Abstract
Secretion of insulin from pancreatic β-cells is complex, but physiological glucose-dependent secretion is dominated by electrical activity, in turn controlled by ATP-sensitive potassium (KATP) channel activity. Accordingly, loss-of-function mutations of the KATP channel Kir6.2 (KCNJ11) or SUR1 (ABCC8) subunit increase electrical excitability and secretion, resulting in congenital hyperinsulinism (CHI), whereas gain-of-function mutations cause underexcitability and undersecretion, resulting in neonatal diabetes mellitus (NDM). Thus, diazoxide, which activates KATP channels, and sulfonylureas, which inhibit KATP channels, have dramatically improved therapies for CHI and NDM, respectively. However, key findings do not fit within this simple paradigm: mice with complete absence of β-cell KATP activity are not hyperinsulinemic; instead, they are paradoxically glucose intolerant and prone to diabetes, as are older human CHI patients. Critically, despite these advances, there has been little insight into any role of KATP channel activity changes in the development of type 2 diabetes (T2D). Intriguingly, the CHI progression from hypersecretion to undersecretion actually mirrors the classical response to insulin resistance in the progression of T2D. In seeking to explain the progression of CHI, multiple lines of evidence lead us to propose that underlying mechanisms are also similar and that development of T2D may involve loss of KATP activity.
We Understand What KATP Channels Do in β-Cells, Don’t We?
Insulin secretion from pancreatic β-cells is complex, but the dominant role of electrical activity in physiological control of glucose-stimulated insulin secretion (GSIS) is now well understood. Glucose entry leads to a metabolically generated rise in ATP/ADP concentration that initiates β-cell KATP channel closure. This results in action potential firing and elevation of cytosolic calcium (Cai) concentration, which in turn triggers the fusion of exocytotic vesicles (1). Consistent with the paradigm, loss-of-function (LOF) mutations in either the pore-forming Kir6.2 (KCNJ11) or the regulatory SUR1 (ABCC8) subunit of KATP channels cause increased electrical excitability and hyperinsulinism (HI), both in human congenital HI (CHI) (2) and in mice that have incomplete genetic knockout (KO), or knockdown, of KATP channels (3,4). Conversely, KATP gain-of-function (GOF) mutations cause neonatal diabetes mellitus (NDM) as a result of underexcitability and undersecretion (5,6). Accordingly, diazoxide, which activates KATP channels, and sulfonylureas (SUs), which inhibit KATP channels, have proven to be viable therapies for CHI and NDM, respectively (7,8).
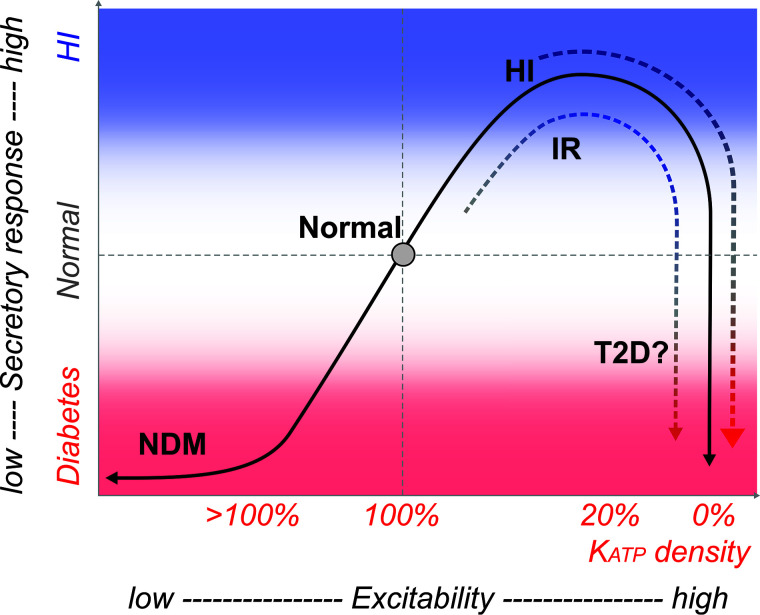
Thus, we have developed a very clear understanding that loss of KATP activity causes HI, as in human CHI, whereas increased KATP activity causes reduced β-cell excitability, undersecretion, and diabetes, as in human NDM (Fig. 1).
Figure 1.
Canonical and paradoxical consequences of reduced KATP activity. A cartoon representation of the relationship between KATP levels, excitability, and secretory response is shown. Supranormal KATP activity (>100%) reduces excitability and secretion, resulting in NDM. Conversely, reduced KATP activity causes hyperexcitability, hypersecretion, and HI. However, when KATP density is reduced substantially, there is a paradoxical crossover to an undersecreting phenotype (the inverse-U relationship [101]), resulting in HI remission or development of diabetes. We propose that increased excitability in response to insulin resistance (IR) will result in hypersecretion but that further reduction of KATP and enhanced excitability may underlie progression to undersecretion in T2D.
Or Do We? Complete Loss of KATP Actually Inhibits Secretion
However, these apparently straightforward yin-yang consequences of KATP LOF and GOF and the simple therapeutic solutions that are provided by KATP activators and inhibitors are complicated by an inconvenient and unexplained realization regarding HI. The KATP closure→elevated Cai→secretion paradigm implies that reduction of KATP levels will shift the insulin secretion curve to the left, i.e., shift the threshold for triggering insulin secretion to increasingly lower glucose concentrations and increase secretion at higher glucose concentrations (Fig. 1). The more KATP is lost, the further the shift and the more severe the hypersecretion will be. When KATP is lost completely, electrical activity will be continuous at all glucose concentrations (β-cells will be “glucose blind”), and there will be maximal secretion of insulin at all glucose concentrations.
Here’s the rub. In mice, partial loss of KATP indeed increases excitability and insulin secretion at lower glucose concentrations (3,9). However, as multiple groups have demonstrated, there is a crossing over to undersecretion, and in vivo insulin secretion is actually dramatically reduced at essentially all glucose concentrations in mice with more complete loss of KATP (10–14). Isolated islets from either SUR1−/− or Kir6.2−/− KATP KO mice are glucose blind, i.e., they are electrically active at all glucose concentrations and lack any marked glucose dependence of secretion, as predicted, but rather than this being because secretion is maximally elevated, almost all studies show it is because secretion stays at a low level, close to the basal level of secretion from normal islets (11–13). Significantly, this undersecretion means that, rather than being hypoglycemic, these animals are actually glucose intolerant as adults (Fig. 1) and become overtly diabetic after high-fat diet (10). The phenomenon is reiterated in mice that express dominant-negative subunits only in β-cells (10,15), obviating the effects of loss of KATP in other cell types. This crossover requires ∼70% loss of KATP activity, since mice with ∼50–70% overall loss of β-cell KATP are hyperinsulinemic (3,4,16) and do not cross over to undersecretion unless challenged with a high-fat diet (10), which may itself cause further lowering of KATP activity.
As fully expected for secretion in the absence of KATP channel regulation, humans with CHI are glucose blind, i.e., a rise in blood glucose does not stimulate a marked rise in insulin secretion (17). However, this is not because secretion is already maximal at all glucose concentrations. Insulin content may be reduced in CHI islets, and at elevated glucose, insulin secretion may actually be lower than that in normal individuals (17,18). Thus, CHI individuals show essentially the same phenomenon of suppressed maximal secretion as KATP KO mice. Treatment options for CHI are limited, and normoglycemia can frequently only be achieved by near-total pancreatectomy (19). Most of these individuals then eventually develop diabetes, logically attributable to secondary consequences of this drastic surgical intervention. In other cases, particularly in cases that do not cause total loss of KATP, the KATP channel opener diazoxide is effective, and somatostatin analogs can also be effective (20).
The natural long-term outcomes in CHI have not been well studied, but it is increasingly apparent that the symptoms of HI typically lessen with age, including in children with ABCC8 or KCNJ11 LOF mutations (21–23), whether dominantly acting homozygous (Hom) or compound heterozygous (Het) or paternally inherited mutations causing focal CHI. One study of patients with dominant KATP mutations found that in adult carriers, all of whom would be expected to have suffered HI, essentially half (14/29) were symptomless, which indicates preceding remission, and 4/29 carriers in that study had diabetes (24). The authors noted that this is similar to levels of type 2 diabetes (T2D) in the general population, but the possibility that diabetes was related to prior CHI should not be discounted, given other reports of HI patients with dominant ABCC8 LOF mutations who remitted and then progressed to diabetes later in life (25,26). In one intriguing case, a female with HI carrying a heterozygous ABCC8 LOF mutation progressed to marked obesity-associated diabetes at 10 years old (27), consistent with this crossover being linked to insulin resistance.
A similar progression is also seen in an extensive Finnish pedigree (25,28), members of which gradually progress from HI toward glucose intolerance and even frank diabetes. Strikingly, knock-in mice carrying the same (SUR1[E1506K]) mutation showed HI in the neonatal period but also rapidly progressed to an undersecreting phenotype (14). KATP channel activation by MgADP was reduced in β-cells from young Het and more severely from Hom animals, and channel density was reduced significantly as the animals aged (14). Glucose tolerance (GT) was essentially normal in young Het animals, but young Hom animals were glucose intolerant, and GT worsened in both with age. Young Hom E1506K mice exhibited enhanced insulin secretion and lower fasting blood glucose but became diabetic, with greatly reduced insulin secretion and impaired GT by 6 months of age. These mice thus traverse the “inverse U” relationship (Fig. 1) and match the suggestion that progressive reduction of KATP levels to ∼30% of normal will cause hypersecretion, but further reduction will cause crossover.
Interestingly, GOF mutations in glucokinase (GCK), which lead to elevated ATP:ADP ratios and consequent suppression of KATP activity, also cause CHI but, in at least one case, an affected individual subsequently developed diabetes (29). Similarly, GCK activator drugs, which were initially developed with a view to treatment of diabetes by stimulation of glucose metabolism and therefore insulin secretion, reduce fasted and fed glucose levels in the short term (days) (30), but over months, these effects are not sustained (31,32). Paralleling this, constitutive pancreatic β-cell–specific expression of a GOF GCK mutation initially causes persistent hypoglycemia, but by 8 months of age, mutant mice develop impaired GT that is further exacerbated by high-fat/high-sucrose diet (33). Similarly, mutations in hepatocyte nuclear factors 1α and 4α cause CHI, potentially due to reduced KATP channel activity, but this again crosses over to diabetes with age for unknown reasons (34,35). Thus, humans with CHI, due to LOF mutations in KATP or other genetic mechanisms that predispose to reduced KATP channel activity, as well as mice with marked loss or inhibition of KATP all show a very similar progression from hypersecretion to undersecretion, glucose intolerance, and diabetes. As we discuss below, understanding this crossover progression is essential for treatment and management not only of CHI but also potentially of the elephant in the room, T2D itself.
What About a Mechanism: Ca Inhibition of Secretion?
Many β-cell changes have been identified that accompany the crossover to failure of secretion in KATP KO mice. Increased apoptotic markers and increased DNA damage response signals have been reported, as well as evidence of α-cell infiltration, but there is no significant change in islet structure or cell identity. One study, using total internal reflection fluorescence microscopy imaging to assess the secretory mechanism itself, showed an increased number of docked insulin granules and a normal level of t-SNAREs in the plasma membrane of SUR1 KO β-cells, but a markedly reduced number of fusion events (36). In some studies, crossover has been associated with reduction of insulin content (10,14), but this is not a consistent finding and may be insufficient to explain the glucose intolerance, suggesting that downregulation of secretion itself is involved (4,10,11).
Crossover is not simply the result of any obvious changes in other major ion conductances that lead to a compensatory loss of excitation. As a consequence, isolated islets generally are shown to be excitable and firing action potentials at all glucose concentrations, and Cai essentially does what it is predicted to do in the absence of KATP: it stays high at all glucose concentrations (11,37). That said, the work of Henquin and colleagues (38–40) has shown that the Cai signal can be significantly affected by prior culture conditions. When previously cultured in high (10 mmol/L) glucose, KATP KO islets exhibit a relatively high duty cycle of Cai oscillations, but fresh or low (1–5 mmol/L)-glucose cultured islets show a comparably lower duty cycle and lower Cai overall. This culture condition dependence extends to secretion, which is much higher from KO islets cultured in high glucose, suggesting a glucose-dependent adaptation through an unexplained mechanism. Interestingly, it has been shown that KATP levels in CHI islets can themselves be affected by culture conditions (41). Conceivably, there may be subtle changes in other conductances that lead to lowering of the triggering Cai level, and further studies of the details of β-cell excitability in the absence of KATP are warranted.
SU drugs inhibit KATP channels, thereby raising Cai and triggering insulin secretion, and have long been prescribed as T2D treatments. However, they eventually fail as sole therapy for unknown reasons (42–44). We have suggested that this gradual failure to respond to SUs is the result of the same crossover mechanism, i.e., chronic SU-induced inhibition of KATP activity might, by causing the same electrical consequence as KATP KO, cause downregulation of insulin secretory capacity (45). Consistent with this idea, implantation of wild-type mice with pellets that chronically release the SU glibenclamide (glib) initially causes blood glucose to drop as expected, but within a few days, blood glucose rises, and after just 1 week of glib treatment, these mice become as glucose intolerant as adult KATP KO mice (45). Freshly isolated islets from these pellet-implanted mice also show as marked a reduction of secretory capacity as KATP KO islets, but secretory capacity can be restored after overnight incubation, as the drug washes out and KATP channel activity is restored (45). In utilizing an independent pharmacologic route to functionally knock out KATP, these striking results reveal not only that, at least in mice, crossover due to loss of KATP activity develops in vivo within a few days but also that it is rapidly reversible.
Here, the story has reached something of an impasse. Given that crossover is not a developmental phenomenon and can be rapidly induced and rapidly reversed, it is possible that the mechanism involves a physiological adjustment of Ca-dependent processes, such as Ca/calmodulin-dependent kinases (CaMKs), calcineurin, or other Ca-dependent proteins, which can cause immediate physiological effects and can modulate G-protein-coupled signaling through cAMP, the recognized primary modulator of secretion. It could also involve changes in gene expression: transcriptomic analysis of SUR1 KO islet cells, in normal diet or after high-fat diet, demonstrates extensive gene reprogramming, with 4,000–7,000 genes affected (46,47). In addition to genes associated with mitochondrial biogenesis and metabolism, there are gene changes consistent with altered β-cell identity and regulation of β-cell epigenetic and transcriptional programs. How many, if any, of these changes are a developmental consequence of the global gene KO, and how many relate to secretion crossover specifically, is not clear. To test this, it will be important to assess whether any of these transcript changes are reversibly induced during short-term induction of crossover, i.e., in glib-pelleted mice or from inducible KO animals, and it remains a possibility that the rapidity of induction and reversal reflects a pathophysiological response to chronic depolarization and elevated Cai that involves only a few or no changes in gene expression.
These issues need sorting out. As we discuss below, the implications of this crossover phenomenon are potentially enormous and demand mechanistic explanation.
Implications for T2D Mechanisms
As discussed above, crossover in response to loss of KATP provides a ready scenario for remission and development of diabetes that can occur in the rare individuals with KATP-dependent CHI. Could it also have a role in the development of T2D, the overwhelmingly important form of diabetes? The textbook progression of T2D involves development of insulin resistance, which is generally associated with obesity and which is initially compensated by increased insulin secretion from pancreatic β-cells. As insulin resistance increases, β-cells eventually fail to “keep up,” gradually crossing over to an undersecreting phenotype, and hyperglycemia develops, in turn worsening β-cell function. We cannot do justice to it here, but an enormous body of work has identified multiple genetic and nongenetic contributors to the development of β-cell dysfunction in T2D (48,49). In response to insulin resistance, β-cell mass expansion provides one mechanism of compensatory increase in secretion, by cellular proliferation and hypertrophy (50,51).
Subsequent crossover from an adaptive hypersecreting state to an uncompensated undersecreting state has been the focus of many studies, and multiple pathways have been implicated. Genome-wide association studies show that the majority of T2D-linked genes play a role in β-cell function or mass, including Wnt-regulated transcription factors, cell cycle and division regulators, and pancreatic transcription factors (52,53). In addition to a potentially synergistic glucolipotoxic role of chronic hyperglycemia and elevated free fatty acids (54), elevated amino acids and related metabolites (55) may induce deleterious effects on β-cell mass and function. Generation of reactive oxygen species (ROS), activation of endoplasmic reticulum stress, upregulation of chronic hexosamine signaling pathway/O-GlcNAcylation, and induction of proinflammatory cytokines in islets may all reduce β-cell proliferation, insulin secretion, or insulin gene expression and promote β-cell apoptosis (56–58). In addition, β-cell dedifferentiation and transdifferentiation can occur under glucolipotoxic conditions (59) but may be reversible, as we showed for dedifferentiation seen in inexcitable β-cells with no GSIS, if glucotoxicity is reversed by exogenous control (60).
Thus, at the organism level, progression from compensated hyperinsulinemia to uncompensated diabetes can involve a lot of well-studied processes. Significantly, there is no specific role ascribed to changes in KATP channel activity in these proposed mechanisms, and a role for altered KATP channel activity, if any, in the typical progression of T2D remains essentially unknown, an important gap given the clear importance of these channels for normal secretion. Multiple lines of evidence lead us to suggest that altered KATP activity may in fact be a significant component. Interestingly, KCNJ11 was one of the earliest T2D-associated genes, with the coding variant (Kir6.2[E23K]) repeatedly being identified (61,62), but the mechanistic link is still not clear. The mutation is in linkage disequilibrium with a second missense mutation (encoding SUR1[S1369A]) in the adjacent ABCC8 gene. Which is the relevant variant is not clear; at the level of channel function, SUR1[S1369A] may enhance MgATP activation of the channel (63), while Kir6.2[E23K] causes a small decrease in ATP sensitivity (64–66). Either effect might predispose to diabetes via the same mechanism as KATP-dependent NDM, i.e., by reducing excitability and secretion (67). However, a Hom knock-in mouse model of Kir6.2[E23K] (68) showed no effect on body weight or blood glucose, and insignificant reduction of GSIS and GT, on a normal diet. On a high-fat diet, there was sexual divergence, with a trend toward greater weight gain in E23K females, associated with slightly worsened GT but an unexplained enhancement of secretion (68).
Further studies may reveal compounding effects of other variants, but these contradictory results provide little support for the idea that KATP GOF contributes directly to failure of secretion in T2D by inhibiting excitation. Moreover, the textbook progression of T2D (Fig. 1) suggests this is not a likely scenario: initial increase of insulin secretion in compensation for insulin resistance is more likely to be associated with reduced KATP activity and enhanced excitability (69). Could reduced β-cell KATP activity really be a causal component of crossover to secretory failure in T2D? As blood glucose is elevated, glucose metabolism in the β-cell will reduce KATP activity by inhibition, but there is also evidence that hyperglycemia can drive a reduction of KATP channel levels, and maximal KATP density is significantly reduced in wild-type β-cells chronically incubated in high glucose in vitro (70). This suggests a positive feedback relationship between loss of KATP and hyperglycemia that could become important under glucolipotoxic conditions. Partly through activation of protein kinase C, high glucose may promote endocytosis of KATP channels, reducing levels of SUR1 protein in the membrane and increasing excitability (71). Conversely, under glucose-deprived conditions, or in the presence of leptin, phosphorylated AMPK induces recruitment of KATP to the plasma membrane (72,73). Thus, both protein kinase C–mediated endocytosis and loss of AMPK-mediated trafficking to the membrane would be predicted to reduce surface KATP density under hyperglycemic conditions. Leptin promotion of KATP trafficking to the membrane provides a mechanism by which insulin secretion could normally be suppressed (74,75). Conceivably, this mechanism may be inhibited in obese individuals with leptin resistance and contribute to crossover progression and development of diabetes.
Glucagon-like peptide 1 (GLP-1) agonists, but not glucose-dependent insulinotropic polypeptide (GIP) agonists, are effective at maintaining insulin secretion in human T2D, and pharmacological studies indicate that GLP-1–induced insulin secretion is similarly retained, while GIP-induced secretion is severely diminished, in KATP KO mice (15,76) due to a relative shift from Gs to Gq signaling. The same shift reportedly occurs when isolated islets are chronically depolarized, whether by inhibiting KATP with the SU tolbutamide or by incubation in high glucose (15). These parallels are consistent with a switch in incretin efficiency being driven by loss of KATP in both KATP KO animals and human T2D. Are there any data to link the development of T2D to loss of KATP? First established in the 1950s (77), the KK mouse is an in-bred strain exhibiting obesity, insulin resistance, and predisposition to diabetes. Introduction of the yellow obese (Ay) gene to generate the KK-Ay strain resulted in a mouse that developed severe diabetes from an early age (78), and many studies have since been carried out using these mice as polygenic T2D models. Oduori et al. (15) recently reported that β-cells from nondiabetic KK mice respond normally to high glucose with electrical activity and GSIS, but severely hyperglycemic KK-Ay β-cells lack KATP activity and are depolarized under all conditions, with loss of GSIS. Oduori et al. further showed that GLP-1 secretion was amplified in the latter, but GIP was without effect. The authors proposed that the switched incretin sensitivity in diabetic KK-Ay islets was a consequence of the loss of β-cell KATP, and that this could explain incretin bias in human T2D. For this to be the case, of course, human T2D must then involve loss of KATP (79).
If this implication is correct, it is of the utmost fundamental importance, but is it a reasonable idea? Tentatively, we argue that the answer is yes, given that 1) hyperglycemia will reduce KATP levels and that 2) loss of KATP activity could be marked enough to cause glucose intolerance and overt diabetes when insulin resistance is imposed. We acknowledge that this is a bold contention, but given the extent of these correlated facts and the implications discussed below, it is one that needs to be carefully examined.
Potential Implications for T2D Therapeutics
If loss of KATP activity does indeed trigger β-cell crossover as one of the pathological mechanisms in the development of T2D, the potential for reversibility by restoration of KATP conductance implies a potential mechanism to reverse secretory failure in T2D. By activating β-cell KATP, the KATP channel opener diazoxide suppresses electrical activity and inhibits insulin secretion. Under normal circumstances, such an action should exacerbate a diabetic state. However, there is evidence for counterintuitively beneficial effects of diazoxide treatment in T2D (80,81). Exactly how diazoxide does this is not clear. It may reduce β-cell apoptosis via increased mitogen-activated protein kinase activity (82) and may affect endogenous glucose production via central nervous system KATP channels (83). However, extensive studies of Björklund and colleagues (80) suggest that the most likely scenario is indeed one in which activation of β-cell KATP channels reverses crossover. Based on the demonstration that prior in vivo diazoxide treatment preserved GSIS in pancreas taken from hyperglycemic rats (84), treatment of insulin-dependent T2D subjects with additional bedtime diazoxide, at doses too low to cause the typical side effects of high dosing, resulted in considerable improvement in stimulated C-peptide and insulin levels (85). Interestingly, in a second study in which the protocol was repeated on insulin-naive T2D subjects (86), glycemic control was, if anything, slightly worsened. In this case, it is tempting to speculate that these subjects had not yet crossed over, and, therefore, activating KATP would simply serve to inappropriately suppress insulin secretion. Similarly, a trial of diazoxide in newly diagnosed type 1 diabetes patients could have failed to result in better preservation of β-cell function for the same reasons (87).
Further consistent with the general idea that restoration of KATP channel activity is beneficial in T2D is recent clinical evidence that intermittent fasting (IF) can reverse T2D (88). The primary goal of such dietary interventions is to improve insulin resistance by reducing average caloric intake and causing weight loss, but some animal studies suggest that IF (versus simple caloric restriction with equivalent caloric intake) induces additional beneficial outcomes, and some human studies have shown beneficial effects of IF in the absence of any weight loss (89–91). While simply restricting caloric intake may reduce blood glucose levels and inhibition of KATP, the possibility that this also regulates KATP levels is unexplored.
As an alternative to exercise and dietary modification, bariatric surgery to reduce the functional volume of the stomach is now recognized as effective therapy in T2D (92,93). It can result in impressive improvement in HbA1c levels and reduction of medication needs, associated with rapid improvement of insulin secretion, particularly meal-stimulated secretion. Loss of first-phase insulin release occurs early in development of T2D, and the effectiveness of gastric bypass for correcting T2D clearly involves recovery of β-cell function. In one study, recovery of first-phase insulin secretion rate (ISR) in i.v. glucose tolerance test (GTT) and β-cell glucose sensitivity during oral GTT was found to be greater in subjects with high β-cell function (i.e., with better glycemic control and with shorter duration of T2D) prior to Roux-en-Y gastric bypass surgery than in those with low function prior to surgery (94). Postoperative postprandial GLP-1 concentrations also increased similarly in both groups, supporting the idea that the primary improvement was in β-cell function. Perhaps reversal of crossover underlies the improvement in β-cell function following gastric bypass? Interestingly, one serious potential complication is the occurrence of hypoglycemia with inappropriately high insulin and C-peptide levels, reflecting hyperstimulation of insulin secretion (95–97). As with CHI, many such individuals can be effectively treated by diazoxide, i.e., by activating KATP, but partial pancreatectomy may be needed to achieve significant improvements in symptom control (96,98). We suggest the simple possibility that bariatric surgery in an individual with a pre-existing state of reduced KATP levels could, by reducing the metabolic signal for KATP inhibition, cause a reversal of crossover, back onto the ascending limb of the inverse-U relationship (Fig. 1), explaining inappropriate hypersecretion of insulin until and unless normal levels of KATP activity are restored.
By pharmacologically suppressing KATP activity, SUs hyperstimulate secretion and can enhance control of glycemia for an extended period in T2D, but SU therapies inevitably fail over months or years (42–44). We suggest that such treatment, by exaggerating the loss of KATP activity, accelerates crossover, but at least initially, this may be reversible. In one intriguing clinical study, nonobese T2D patients with secondary failure of SU therapies regained significant insulin secretory activity after 3 months of intensive insulin therapy (99). In these patients, therefore, control of blood glucose with insulin, reducing stimulatory demand on β-cells, restored secretory capacity. This result parallels the observation that removal of a high-fat diet leads to recovery of secretion and glycemic control in mice with loss of KATP channels (10).
One final implication, regarding SU therapy, is that although supranormal reduction of β-cell KATP and, hence, overstimulation of hyperexcitability will, by causing crossover, be self-limiting in the use of SU to trigger an increase in insulin secretion in T2D, the same need not be true for KATP-dependent NDM. In the latter case, the underlying problem is too much β-cell KATP activity due to the KCNJ11/ABCC8 GOF mutations. Conceivably, the correct SU dose will only serve to reduce channel activity to an essentially normal level, allowing the glucose-dependent amplifying pathway to produce quasi-normal, glucose-dependent insulin secretion. This can explain how successful SU treatment provides better glucose control than bolus insulin therapy in NDM patients (8). If the dose is carefully titrated to avoid excess KATP inhibition (and, hence, avoid hyperelevation of Cai), this can also explain why SU therapy in patients with KATP-dependent NDM, in contrast to those with T2D, is proving to be a sustainable, long-term therapy (100).
Conclusions
Despite the paradigmatic role of KATP channels in normal control of insulin secretion, reflected in the CHI and neonatal diabetes that result from LOF and GOF KATP mutations, respectively, significant loss of KATP channel activity paradoxically is associated with reduced insulin secretability that can be significant enough to cause glucose intolerance, and even frank diabetes, in the presence of insulin resistance. The implications of this crossover are significant. First, it provides a potential explanation for the progression of HI patients from HI to impaired GT and even frank diabetes. Second, the possibility that insulin resistance and hyperglycemia leads to downregulation of KATP channels provides a potential explanation for the critical transition from glucose intolerance and HI to undersecretion in the development of T2D. Third, rapid reversibility of crossover, back to normal secretion, as a consequence of reducing excitability implies a mechanism for reversing this pathology in T2D. Such a mechanism might underlie the remission of T2D that can follow diazoxide treatment or when demand for insulin secretion is reduced following gastric bypass.
Article Information
Funding. C.G.N. is supported by the Center for Scientific Review, National Institutes of Health, grant HL140024, and M.S.R. is supported by National Institutes of Health grant DK123163.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
References
- 1. Ashcroft FM, Rorsman P. Electrophysiology of the pancreatic beta-cell. Prog Biophys Mol Biol 1989;54:87–143 [DOI] [PubMed] [Google Scholar]
- 2. Henwood MJ, Kelly A, Macmullen C, et al. Genotype-phenotype correlations in children with congenital hyperinsulinism due to recessive mutations of the adenosine triphosphate-sensitive potassium channel genes. J Clin Endocrinol Metab 2005;90:789–794 [DOI] [PubMed] [Google Scholar]
- 3. Koster JC, Remedi MS, Flagg TP, et al. Hyperinsulinism induced by targeted suppression of beta cell KATP channels. Proc Natl Acad Sci U S A 2002;99:16992–16997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Remedi MS, Rocheleau JV, Tong A, et al. Hyperinsulinism in mice with heterozygous loss of K(ATP) channels. Diabetologia 2006;49:2368–2378 [DOI] [PubMed] [Google Scholar]
- 5. Koster JC, Marshall BA, Ensor N, Corbett JA, Nichols CG. Targeted overactivity of beta cell K(ATP) channels induces profound neonatal diabetes. Cell 2000;100:645–654 [DOI] [PubMed] [Google Scholar]
- 6. Gloyn AL, Pearson ER, Antcliff JF, et al. Activating mutations in the gene encoding the ATP-sensitive potassium-channel subunit Kir6.2 and permanent neonatal diabetes. N Engl J Med 2004;350:1838–1849 [DOI] [PubMed] [Google Scholar]
- 7. Palladino AA, Bennett MJ, Stanley CA. Hyperinsulinism in infancy and childhood: when an insulin level is not always enough. Clin Chem 2008;54:256–263 [DOI] [PubMed] [Google Scholar]
- 8. Pearson ER, Flechtner I, Njølstad PR, et al.; Neonatal Diabetes International Collaborative Group . Switching from insulin to oral sulfonylureas in patients with diabetes due to Kir6.2 mutations. N Engl J Med 2006;355:467–477 [see comment] [DOI] [PubMed] [Google Scholar]
- 9. Remedi MS, Nichols CG, Koster JC. The mitochondria and insulin release: Nnt just a passing relationship. Cell Metab 2006;3:5–7 [DOI] [PubMed] [Google Scholar]
- 10. Remedi MS, Koster JC, Markova K, et al. Diet-induced glucose intolerance in mice with decreased beta-cell ATP-sensitive K+ channels. Diabetes 2004;53:3159–3167 [DOI] [PubMed] [Google Scholar]
- 11. Miki T, Nagashima K, Tashiro F, et al. Defective insulin secretion and enhanced insulin action in KATP channel-deficient mice. Proc Natl Acad Sci U S A 1998;95:10402–10406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Seghers V, Nakazaki M, DeMayo F, Aguilar-Bryan L, Bryan J. Sur1 knockout mice. A model for K(ATP) channel-independent regulation of insulin secretion. J Biol Chem 2000;275:9270–9277 [DOI] [PubMed] [Google Scholar]
- 13. Shiota C, Larsson O, Shelton KD, et al. Sulfonylurea receptor type 1 knock-out mice have intact feeding-stimulated insulin secretion despite marked impairment in their response to glucose. J Biol Chem 2002;277:37176–37183 [DOI] [PubMed] [Google Scholar]
- 14. Shimomura K, Tusa M, Iberl M, et al. A mouse model of human hyperinsulinism produced by the E1506K mutation in the sulphonylurea receptor SUR1. Diabetes 2013;62:3797–3806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Oduori OS, Murao N, Shimomura K, et al. Gs/Gq signaling switch in β cells defines incretin effectiveness in diabetes. J Clin Invest 2020;130:6639–6655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rocheleau JV, Remedi MS, Granada B, et al. Critical role of gap junction coupled KATP channel activity for regulated insulin secretion. PLoS Biol 2006;4:e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Li C, Ackermann AM, Boodhansingh KE, et al. Functional and metabolomic consequences of KATP channel inactivation in human islets. Diabetes 2017;66:1901–1913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Henquin JC, Nenquin M, Sempoux C, et al. In vitro insulin secretion by pancreatic tissue from infants with diazoxide-resistant congenital hyperinsulinism deviates from model predictions. J Clin Invest 2011;121:3932–3942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. De León DD, Stanley CA. Mechanisms of disease: advances in diagnosis and treatment of hyperinsulinism in neonates. Nat Clin Pract Endocrinol Metab 2007;3:57–68 [DOI] [PubMed] [Google Scholar]
- 20. Rosenfeld E, Ganguly A, De Leon DD. Congenital hyperinsulinism disorders: genetic and clinical characteristics. Am J Med Genet C Semin Med Genet 2019;181:682–692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Salomon-Estebanez M, Flanagan SE, Ellard S, et al. Conservatively treated congenital hyperinsulinism (CHI) due to K-ATP channel gene mutations: reducing severity over time. Orphanet J Rare Dis 2016;11:163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mazor-Aronovitch K, Gillis D, Lobel D, et al. Long-term neurodevelopmental outcome in conservatively treated congenital hyperinsulinism. Eur J Endocrinol 2007;157:491–497 [DOI] [PubMed] [Google Scholar]
- 23. Martinez R, Fernandez-Ramos C, Vela A, et al. Clinical and genetic characterization of congenital hyperinsulinism in Spain. Eur J Endocrinol 2016;174:717–726 [DOI] [PubMed] [Google Scholar]
- 24. Pinney SE, MacMullen C, Becker S, et al. Clinical characteristics and biochemical mechanisms of congenital hyperinsulinism associated with dominant KATP channel mutations. J Clin Invest 2008;118:2877–2886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Huopio H, Otonkoski T, Vauhkonen I, Reimann F, Ashcroft FM, Laakso M. A new subtype of autosomal dominant diabetes attributable to a mutation in the gene for sulfonylurea receptor 1. Lancet 2003;361:301–307 [DOI] [PubMed] [Google Scholar]
- 26. Kapoor RR, Flanagan SE, Arya VB, Shield JP, Ellard S, Hussain K. Clinical and molecular characterisation of 300 patients with congenital hyperinsulinism. Eur J Endocrinol 2013;168:557–564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Abdulhadi-Atwan M, Bushman J, Tornovsky-Babaey S, et al. Novel de novo mutation in sulfonylurea receptor 1 presenting as hyperinsulinism in infancy followed by overt diabetes in early adolescence. Diabetes 2008;57:1935–1940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Huopio H, Reimann F, Ashfield R, et al. Dominantly inherited hyperinsulinism caused by a mutation in the sulfonylurea receptor type 1. J Clin Invest 2000;106:897–906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Glaser B, Kesavan P, Heyman M, et al. Familial hyperinsulinism caused by an activating glucokinase mutation. N Engl J Med 1998;338:226–230 [DOI] [PubMed] [Google Scholar]
- 30. Bonadonna RC, Heise T, Arbet-Engels C, et al. Piragliatin (RO4389620), a novel glucokinase activator, lowers plasma glucose both in the postabsorptive state and after a glucose challenge in patients with type 2 diabetes mellitus: a mechanistic study. J Clin Endocrinol Metab 2010;95:5028–5036 [DOI] [PubMed] [Google Scholar]
- 31. Meininger GE, Scott R, Alba M, et al. Effects of MK-0941, a novel glucokinase activator, on glycemic control in insulin-treated patients with type 2 diabetes. Diabetes Care 2011;34:2560–2566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wilding JP, Leonsson-Zachrisson M, Wessman C, Johnsson E. Dose-ranging study with the glucokinase activator AZD1656 in patients with type 2 diabetes mellitus on metformin. Diabetes Obes Metab 2013;15:750–759 [DOI] [PubMed] [Google Scholar]
- 33. Tornovsky-Babeay S, Weinberg-Corem N, Ben-Haroush Schyr R, et al. Biphasic dynamics of beta cell mass in a mouse model of congenital hyperinsulinism: implications for type 2 diabetes. Diabetologia 2021;64:1133–1143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Arya VB, Rahman S, Senniappan S, Flanagan SE, Ellard S, Hussain K. HNF4A mutation: switch from hyperinsulinaemic hypoglycaemia to maturity-onset diabetes of the young, and incretin response. Diabet Med 2014;31:e11–e15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Stanescu DE, Hughes N, Kaplan B, Stanley CA, De León DD. Novel presentations of congenital hyperinsulinism due to mutations in the MODY genes: HNF1A and HNF4A. J Clin Endocrinol Metab 2012;97:E2026–E2030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kikuta T, Ohara-Imaizumi M, Nakazaki M, et al. Docking and fusion of insulin secretory granules in SUR1 knock out mouse beta-cells observed by total internal reflection fluorescence microscopy. FEBS Lett 2005;579:1602–1606 [DOI] [PubMed] [Google Scholar]
- 37. Nenquin M, Szollosi A, Aguilar-Bryan L, Bryan J, Henquin JC. Both triggering and amplifying pathways contribute to fuel-induced insulin secretion in the absence of sulfonylurea receptor-1 in pancreatic beta-cells. J Biol Chem 2004;279:32316–32324 [DOI] [PubMed] [Google Scholar]
- 38. Szollosi A, Nenquin M, Aguilar-Bryan L, Bryan J, Henquin JC. Glucose stimulates Ca2+ influx and insulin secretion in 2-week-old β-cells lacking ATP-sensitive K+ channels. J Biol Chem 2007;282:1747–1756 [DOI] [PubMed] [Google Scholar]
- 39. Szollosi A, Nenquin M, Henquin JC. Overnight culture unmasks glucose-induced insulin secretion in mouse islets lacking ATP-sensitive K+ channels by improving the triggering Ca2+ signal. J Biol Chem 2007;282:14768–14776 [DOI] [PubMed] [Google Scholar]
- 40. Ravier MA, Nenquin M, Miki T, Seino S, Henquin JC. Glucose controls cytosolic Ca2+ and insulin secretion in mouse islets lacking adenosine triphosphate-sensitive K+ channels owing to a knockout of the pore-forming subunit Kir6.2. Endocrinology 2009;150:33–45 [DOI] [PubMed] [Google Scholar]
- 41. Powell PD, Bellanné-Chantelot C, Flanagan SE, et al. In vitro recovery of ATP-sensitive potassium channels in β-cells from patients with congenital hyperinsulinism of infancy. Diabetes 2011;60:1223–1228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Matthews DR, Cull CA, Stratton IM, Holman RR; UK Prospective Diabetes Study (UKPDS) Group . UKPDS 26: sulphonylurea failure in non-insulin-dependent diabetic patients over six years. Diabet Med 1998;15:297–303 [DOI] [PubMed] [Google Scholar]
- 43. Bretzel RG, Voigt K, Schatz H. The United Kingdom Prospective Diabetes Study (UKPDS) implications for the pharmacotherapy of type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes 1998;106:369–372 [PubMed] [Google Scholar]
- 44. Birkeland KI, Furuseth K, Melander A, Mowinckel P, Vaaler S. Long-term randomized placebo-controlled double-blind therapeutic comparison of glipizide and glyburide. Glycemic control and insulin secretion during 15 months. Diabetes Care 1994;17:45–49 [DOI] [PubMed] [Google Scholar]
- 45. Remedi MS, Nichols CG. Chronic antidiabetic sulfonylureas in vivo: reversible effects on mouse pancreatic beta-cells. PLoS Med 2008;5:e206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Stancill JS, Cartailler JP, Clayton HW, et al. Chronic β-cell depolarization impairs β-cell identity by disrupting a network of Ca2+-regulated genes. Diabetes 2017;66:2175–2187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Osipovich AB, Stancill JS, Cartailler JP, Dudek KD, Magnuson MA. Excitotoxicity and overnutrition additively impair metabolic function and identity of pancreatic β-cells. Diabetes 2020;69:1476–1491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Alejandro EU, Gregg B, Blandino-Rosano M, Cras-Méneur C, Bernal-Mizrachi E. Natural history of β-cell adaptation and failure in type 2 diabetes. Mol Aspects Med 2015;42:19–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Prentki M, Nolan CJ. Islet beta cell failure in type 2 diabetes. J Clin Invest 2006;116:1802–1812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Dor Y, Brown J, Martinez OI, Melton DA. Adult pancreatic beta-cells are formed by self-duplication rather than stem-cell differentiation. Nature 2004;429:41–46 [DOI] [PubMed] [Google Scholar]
- 51. Montanya E, Nacher V, Biarnés M, Soler J. Linear correlation between beta-cell mass and body weight throughout the lifespan in Lewis rats: role of beta-cell hyperplasia and hypertrophy. Diabetes 2000;49:1341–1346 [DOI] [PubMed] [Google Scholar]
- 52. Dupuis J, Langenberg C, Prokopenko I, et al.; DIAGRAM Consortium; GIANT Consortium; Global BPgen Consortium; Anders Hamsten on behalf of Procardis Consortium; MAGIC Investigators . New genetic loci implicated in fasting glucose homeostasis and their impact on type 2 diabetes risk. Nat Genet 2010;42:105–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zeggini E, Scott LJ, Saxena R, et al.; Wellcome Trust Case Control Consortium . Meta-analysis of genome-wide association data and large-scale replication identifies additional susceptibility loci for type 2 diabetes. Nat Genet 2008;40:638–645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Poitout V, Robertson RP. Glucolipotoxicity: fuel excess and beta-cell dysfunction. Endocr Rev 2008;29:351–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Newgard CB. Interplay between lipids and branched-chain amino acids in development of insulin resistance. Cell Metab 2012;15:606–614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Del Guerra S, Lupi R, Marselli L, et al. Functional and molecular defects of pancreatic islets in human type 2 diabetes. Diabetes 2005;54:727–735 [DOI] [PubMed] [Google Scholar]
- 57. Tanaka Y, Gleason CE, Tran PO, Harmon JS, Robertson RP. Prevention of glucose toxicity in HIT-T15 cells and Zucker diabetic fatty rats by antioxidants. Proc Natl Acad Sci USA 1999;96:10857–10862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Tanaka Y, Tran PO, Harmon J, Robertson RP. A role for glutathione peroxidase in protecting pancreatic beta cells against oxidative stress in a model of glucose toxicity. Proc Natl Acad Sci USA 2002;99:12363–12368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Talchai C, Xuan S, Lin HV, Sussel L, Accili D. Pancreatic β cell dedifferentiation as a mechanism of diabetic β cell failure. Cell 2012;150:1223–1234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Wang Z, York NW, Nichols CG, Remedi MS. Pancreatic β cell dedifferentiation in diabetes and redifferentiation following insulin therapy. Cell Metab 2014;19:872–882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Hani EH, Boutin P, Durand E, et al. Missense mutations in the pancreatic islet beta cell inwardly rectifying K+ channel gene (KIR6.2/BIR): a meta-analysis suggests a role in the polygenic basis of type II diabetes mellitus in Caucasians. Diabetologia 1998;41:1511–1515 [DOI] [PubMed] [Google Scholar]
- 62. Gloyn AL, Hashim Y, Ashcroft SJ, Ashfield R, Wiltshire S; UK Prospective Diabetes Study (UKPDS 53) . Association studies of variants in promoter and coding regions of beta-cell ATP-sensitive K-channel genes SUR1 and Kir6.2 with type 2 diabetes mellitus (UKPDS 53). Diabet Med 2001;18:206–212 [DOI] [PubMed] [Google Scholar]
- 63. Fatehi M, Raja M, Carter C, Soliman D, Holt A, Light PE. The ATP-sensitive K+ channel ABCC8 S1369A type 2 diabetes risk variant increases MgATPase activity. Diabetes 2012;61:241–249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Schwanstecher C, Meyer U, Schwanstecher M. K(IR)6.2 polymorphism predisposes to type 2 diabetes by inducing overactivity of pancreatic beta-cell ATP-sensitive K+ channels. Diabetes 2002;51:875–879 [DOI] [PubMed] [Google Scholar]
- 65. Riedel MJ, Steckley DC, Light PE. Current status of the E23K Kir6.2 polymorphism: implications for type-2 diabetes. Hum Genet 2005;116:133–145 [DOI] [PubMed] [Google Scholar]
- 66. Hamming KS, Soliman D, Matemisz LC, et al. Coexpression of the type 2 diabetes susceptibility gene variants KCNJ11 E23K and ABCC8 S1369A alter the ATP and sulfonylurea sensitivities of the ATP-sensitive K+ channel. Diabetes 2009;58:2419–2424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Villareal DT, Koster JC, Robertson H, et al. Kir6.2 variant E23K increases ATP-sensitive K+ channel activity and is associated with impaired insulin release and enhanced insulin sensitivity in adults with normal glucose tolerance. Diabetes 2009;58:1869–1878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Sachse G, Haythorne E, Hill T, et al. The KCNJ11-E23K gene variant hastens diabetes progression by impairing glucose-induced insulin secretion. Diabetes 2021;70:1145–1156 [DOI] [PubMed] [Google Scholar]
- 69. Velasco M, Larqué C, Gutiérrez-Reyes G, Arredondo R, Sanchez-Soto C, Hiriart M. Metabolic syndrome induces changes in KATP-channels and calcium currents in pancreatic β-cells. Islets 2012;4:302–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Shyr ZA, Wang Z, York NW, Nichols CG, Remedi MS. The role of membrane excitability in pancreatic β-cell glucotoxicity. Sci Rep 2019;9:6952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Han YE, Chun JN, Kwon MJ, et al. Endocytosis of KATP channels drives glucose-stimulated excitation of pancreatic β cells. Cell Rep 2018;22:471–481 [DOI] [PubMed] [Google Scholar]
- 72. Park SH, Ho WK, Jeon JH. AMPK regulates K(ATP) channel trafficking via PTEN inhibition in leptin-treated pancreatic β-cells. Biochem Biophys Res Commun 2013;440:539–544 [DOI] [PubMed] [Google Scholar]
- 73. Chen PC, Kryukova YN, Shyng SL. Leptin regulates KATP channel trafficking in pancreatic β-cells by a signaling mechanism involving AMP-activated protein kinase (AMPK) and cAMP-dependent protein kinase (PKA). J Biol Chem 2013;288:34098–34109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Cochrane V, Shyng SL. Leptin-induced trafficking of KATP channels: a mechanism to regulate pancreatic β-cell excitability and insulin secretion. Int J Mol Sci 2019;20:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Seufert J, Kieffer TJ, Leech CA, et al. Leptin suppression of insulin secretion and gene expression in human pancreatic islets: implications for the development of adipogenic diabetes mellitus. J Clin Endocrinol Metab 1999;84:670–676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Miki T, Seino S. Roles of KATP channels as metabolic sensors in acute metabolic changes. J Mol Cell Cardiol 2005;38:917–925 [DOI] [PubMed] [Google Scholar]
- 77. Kondo K, Nozawa K, Tomita T, Ezaki K. Inbred strains resulting from Japanese mice. Bull Exp Anim 1957;6:107–112 [Google Scholar]
- 78. Ikeda H. KK mouse. Diabetes Res Clin Pract 1994;24(Suppl.):S313–S316 [DOI] [PubMed] [Google Scholar]
- 79. Nichols CG, York NW, Remedi MS. Preferential Gq signaling in diabetes: an electrical switch in incretin action and in diabetes progression? J Clin Invest 2020;130:6235–6237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Grill V, Radtke M, Qvigstad E, Kollind M, Björklund A. Beneficial effects of K-ATP channel openers in diabetes: an update on mechanisms and clinical experiences. Diabetes Obes Metab 2009;11(Suppl. 4):143–148 [DOI] [PubMed] [Google Scholar]
- 81. Greenwood RH, Mahler RF, Hales CN. Improvement in insulin secretion in diabetes after diazoxide. Lancet 1976;1:444–447 [DOI] [PubMed] [Google Scholar]
- 82. Huang Q, Bu S, Yu Y, et al. Diazoxide prevents diabetes through inhibiting pancreatic beta-cells from apoptosis via Bcl-2/Bax rate and p38-beta mitogen-activated protein kinase. Endocrinology 2007;148:81–91 [DOI] [PubMed] [Google Scholar]
- 83. Carey M, Lontchi-Yimagou E, Mitchell W, et al. Central KATP channels modulate glucose effectiveness in humans and rodents. Diabetes 2020;69:1140–1148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Sako Y, Grill VE. Diazoxide infusion at excess but not at basal hyperglycemia enhances beta-cell sensitivity to glucose in vitro in neonatally streptozotocin-diabetic rats. Metabolism 1992;41:738–743 [DOI] [PubMed] [Google Scholar]
- 85. Qvigstad E, Kollind M, Grill V. Nine weeks of bedtime diazoxide is well tolerated and improves beta-cell function in subjects with type 2 diabetes. Diabet Med 2004;21:73–76 [DOI] [PubMed] [Google Scholar]
- 86. Radtke M, Kollind M, Qvigstad E, Grill V. Twelve weeks’ treatment with diazoxide without insulin supplementation in type 2 diabetes is feasible but does not improve insulin secretion. Diabet Med 2007;24:172–177 [DOI] [PubMed] [Google Scholar]
- 87. Ortqvist E, Björk E, Wallensteen M, et al. Temporary preservation of beta-cell function by diazoxide treatment in childhood type 1 diabetes. Diabetes Care 2004;27:2191–2197 [DOI] [PubMed] [Google Scholar]
- 88. Furmli S, Elmasry R, Ramos M, Fung J. Therapeutic use of intermittent fasting for people with type 2 diabetes as an alternative to insulin. BMJ Case Rep 2018. DOI: 10.1136/bcr-2017-221854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Anson RM, Guo Z, de Cabo R, et al. Intermittent fasting dissociates beneficial effects of dietary restriction on glucose metabolism and neuronal resistance to injury from calorie intake. Proc Natl Acad Sci U S A 2003;100:6216–6220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Hatori M, Vollmers C, Zarrinpar A, et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab 2012;15:848–860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Halberg N, Henriksen M, Söderhamn N, et al. Effect of intermittent fasting and refeeding on insulin action in healthy men. J Appl Physiol (1985) 2005;99:2128–2136 [DOI] [PubMed] [Google Scholar]
- 92. Dixon JB, O’Brien PE, Playfair J, et al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA 2008;299:316–323 [DOI] [PubMed] [Google Scholar]
- 93. Rubino F, Schauer PR, Kaplan LM, Cummings DE. Metabolic surgery to treat type 2 diabetes: clinical outcomes and mechanisms of action. Annu Rev Med 2010;61:393–411 [DOI] [PubMed] [Google Scholar]
- 94. Lund MT, Hansen M, Skaaby S, et al. Preoperative β-cell function in patients with type 2 diabetes is important for the outcome of Roux-en-Y gastric bypass surgery. J Physiol 2015;593:3123–3133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Service GJ, Thompson GB, Service FJ, Andrews JC, Collazo-Clavell ML, Lloyd RV. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. N Engl J Med 2005;353:249–254 [DOI] [PubMed] [Google Scholar]
- 96. Patti ME, McMahon G, Mun EC, et al. Severe hypoglycaemia post-gastric bypass requiring partial pancreatectomy: evidence for inappropriate insulin secretion and pancreatic islet hyperplasia. Diabetologia 2005;48:2236–2240 [DOI] [PubMed] [Google Scholar]
- 97. Marsk R, Jonas E, Rasmussen F, Näslund E. Nationwide cohort study of post-gastric bypass hypoglycaemia including 5,040 patients undergoing surgery for obesity in 1986-2006 in Sweden. Diabetologia 2010;53:2307–2311 [DOI] [PubMed] [Google Scholar]
- 98. Mathavan VK, Arregui M, Davis C, Singh K, Patel A, Meacham J. Management of postgastric bypass noninsulinoma pancreatogenous hypoglycemia. Surg Endosc 2010;24:2547–2555 [DOI] [PubMed] [Google Scholar]
- 99. Torella R, Salvatore T, Cozzolino D, Giunta R, Quatraro A, Giugliano D. Restoration of sensitivity to sulfonylurea after strict glycaemic control with insulin in non-obese type 2 diabetic subjects. Diabete Metab 1991;17:443–447 [PubMed] [Google Scholar]
- 100. Bowman P, Sulen Å, Barbetti F, et al.; Neonatal Diabetes International Collaborative Group . Effectiveness and safety of long-term treatment with sulfonylureas in patients with neonatal diabetes due to KCNJ11 mutations: an international cohort study. Lancet Diabetes Endocrinol 2018;6:637–646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Remedi MS, Nichols CG. Hyperinsulinism and diabetes: genetic dissection of beta cell metabolism-excitation coupling in mice. Cell Metab 2009;10:442–453 [DOI] [PMC free article] [PubMed] [Google Scholar]