ABSTRACT
Objectives:
A precise anatomical understanding of the morphology of the spine is indispensable for neck and low back pain therapy including rehabilitation. However, few studies have directly addressed spinal morphology with a focus on the height of the vertebral body and discs. The aim of the current study was to analyze sex- and age-related changes in the spine by measuring the distance between adjacent centers of the intervertebral disc spaces from the posterior aspect in cadavers and by using magnetic resonance imaging (MRI) measurements at the cervical and lumbar vertebral levels.
Methods:
In the cadaveric study, the posterior distance between the adjacent centers of the disc spaces was measured for 58 spinal canals. The equivalent distances were examined using MRI in 370 and 660 subjects who presented with neck pain and back pain, respectively.
Results:
The distance between the adjacent centers of the intervertebral disc spaces in male cadavers was larger than that in female cadavers from C3 to L5/S1. The MRI results showed that the distance between the adjacent centers of the intervertebral disc spaces decreased with age in all spinal areas in men and women. Cadaveric values were significantly lower than the MRI values in men, whereas in women, no significant differences were observed.
Conclusions:
These results suggest that age-related changes in the cervical and lumbar spine are associated with differences between men and women in the degrees of progressive vertebral body and disc degeneration.
Keywords: anatomy, degeneration, gender difference, MRI, spine
INTRODUCTION
The Global Burden of Disease data for noncommunicable diseases indicate that spinal pain has been the leading cause of global disability since 1990.1) Neck and low back pain are the two largest causes of musculoskeletal disability among complaints of spinal pain.2) The prevalence of conditions involving chronic pain is higher among women and older persons.3) Many studies have investigated spinal degeneration with aging by using diagnostic imaging and histochemical studies. The general consensus is that the pathological and morphological changes involved in intervertebral disc degeneration include decreases in proteoglycan level, decreases in water content in the nucleus pulposus, and reduced disc height.4,5,6) As suggested in the 1962 study by Naylor, the intervertebral discs have been shown to undergo an age-related process of degeneration as early as the second decade of life. The nucleus pulposus undergoes transition from a watery gel to a fibrous solid, which reaches a peak in the fourth decade of life.7) Degenerative changes in the discs are always accompanied by osteophyte formation on the margins of the vertebral bodies and arthritic changes in the facet joints. A direct relationship exists between the degree of disc degeneration, marginal osteophyte formation on vertebral bodies, and facet joint changes, which suggests that disc degeneration is the primary event that leads to the clinical condition of degenerative spondylosis.8) Good mobility of the intervertebral disc and the pair of left and right facet joints facilitates free movement of the spine. Experiments using cadaveric lumbar spine specimens revealed that intervertebral disc space constriction caused a significant increase in the peak pressure across the facet joints. Therefore, decreased disc height leads to worse facet osteoarthritis.9) In a healthy spine, only 5%–10% of the load is transmitted through the posterior vertebral arch, including the facet joint; however, the presence of degenerative discs increased the percentage to 40%.10) Using a poroelastic three-dimensional finite element model of the cervical spine, the dimension that most strongly correlated with stress on the facet joint was suggested to be the posterior height of the intervertebral disc and not the anterior height.11) However, it is possible that both the posterior height of the intervertebral disc and the posterior height of the vertebral body have a strong correlation with facet joint load.
The vertebrae are commonly believed to lose some of their mineral content with age, making each bone thinner, and the spinal column becomes curved and compressed.12) A correlation study between vertebral body morphology obtained by computed tomography scans and bone mineral density measured by dual-energy X-ray absorptiometry showed that the age-related lumbar bone mineral density loss was associated with a significant decrease in the posterior height of the vertebral body in both sexes.13) Although the total length of the spine has been shown to decrease with age, the exact degree of change and any sex-related differences remain elusive.14,15)
The present study focused on the height of the vertebral body, including the thickness of half of the disc above and below the vertebral body. This height was measured posteriorly, which is presumed to be more strongly correlated with intervertebral arthropathy. By using magnetic resonance imaging (MRI) and cadaveric measurements at the cervical and lumbar vertebrae levels, we statistically analyzed sex- and age-related changes in the spine, focusing on the distance between the adjacent centers of the intervertebral disc spaces from the posterior aspect.
MATERIALS AND METHODS
Cadaveric Measurements
Subjects
The present study was conducted within the parameters of the written permissions we received from the donors and their surviving relatives, and the present work conformed to the provisions of the Declaration of Helsinki in 1995 (as revised in Edinburgh in 2000). This study was approved by the Institutional Review Board of Nagoya City University Graduate School of Medical Sciences in accordance with the Ethical Guidelines for Epidemiological Research (Approval No. 1156).
A total of 65 adult cadavers (32 male and 33 female) with no known pathological conditions of the spine were examined during educational dissection at Nagoya City University Medical School in 2016–2018. All the cadavers had been perfused with a fixative (10% formalin solution) through the femoral artery, and percolation by 85.5% ethanol solvent (Solmix AP-7, Japan Alcohol Trading, Tokyo, Japan) was achieved through body surfaces via immersion in a solvent pool for >2 weeks. The cadavers were then preserved in a natural posture in the usual manner. The mean age at death was 85.7 years (range, 64–102 years) for the men and 84.8 years (range, 61–101years) for the women. Adequate data could not be obtained from seven specimens because of the poor condition of the spine. After exclusion of those seven cases (three male and four female cadavers), 58 spinal canals (29 male and 29 female) were analyzed.
Design and Procedure
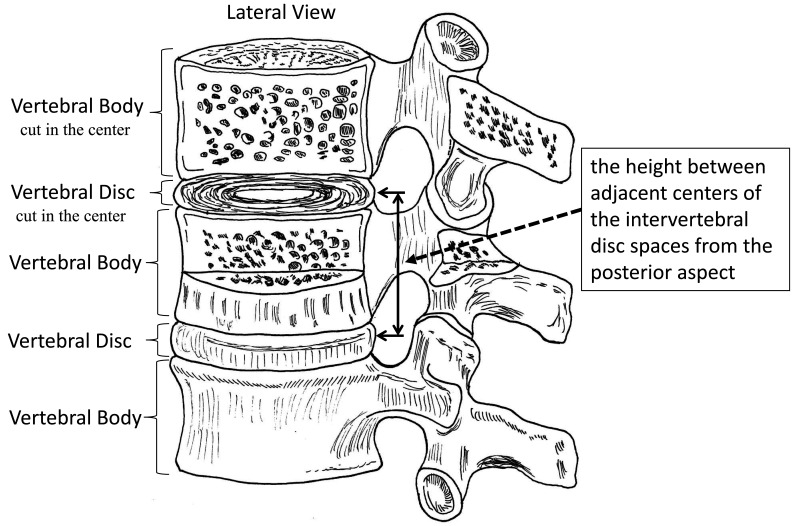
The posterior aspect of the vertebral column was exposed between C3 and L5/S1 by dissection of the postvertebral muscles. The posterior spinal elements were then transected and removed to study the vertebral bodies and intervertebral disc spaces within the spinal canal. After complete dissections of the posterior surface of each intervertebral disc space, morphometric measurements were taken. The distance between the adjacent centers of the intervertebral disc spaces, i.e., the vertebral body and half adjacent disc height (VBAD height), was measured using a Vernier caliper (KSM-15FF, Nakamura Mfg., Tokyo, Japan) at all vertebral and disc levels from C3 to L5/S1 (Fig. 1).
Fig. 1.
The distance between the adjacent centers of the intervertebral disc spaces [(i.e., the vertebral body and half adjacent disc height (VBAD height)] was measured as shown.
Magnetic Resonance Imaging
Subjects
This study was approved by the Institutional Review Board of the participating facility (Approval No. 001). The participants were 370 patients (196 men and 174 women) who presented with neck pain and 660 patients (315 men and 345 women) who presented with low back pain in the Kouyu Orthopaedic Clinic between 2014 and 2020 (Tables 1 and 2). Patients with vertebral body abnormalities or gross spinal pathologies, including spondylolisthesis and disc space collapse, were excluded. Furthermore, patients who had undergone a previous cervical spine operation or lumbar fixation were excluded from the analysis.
Table 1. Cervical spine: age and number of subjects undergoing MRI analysis.
| Age (years) | Men | Mean±SD | Women | Mean±SD |
| 30–39 | 21 | 33.7±3.89 | 20 | 33.7±2.64 |
| 40–49 | 67 | 45.0±2.74 | 50 | 44.6±2.93 |
| 50–59 | 34 | 54.0±2.37 | 28 | 53.7±2.81 |
| 60–69 | 30 | 64.3±2.92 | 25 | 64.9±3.17 |
| 70–79 | 31 | 74.9±3.18 | 38 | 74.4±2.49 |
| 80–89 | 13 | 80.7±1.38 | 13 | 84.1±2.33 |
MRI measurements of the cervical spine were performed in 370 patients (196 men and 174 women) with neck pain.
Table 2. Lumbar spine: age and number of subjects undergoing MRI analysis .
| Age (years) | Men | Mean±SD | Women | Mean±SD |
| 30–39 | 41 | 33.3±3.44 | 40 | 33.0±2.52 |
| 40–49 | 67 | 44.0±2.26 | 50 | 43.5±2.40 |
| 50–59 | 50 | 53.6±2.59 | 56 | 53.8±2.64 |
| 60–69 | 47 | 63.9±2.22 | 69 | 63.9±2.71 |
| 70–79 | 55 | 74.3±3.00 | 55 | 73.6±2.41 |
| 80–89 | 55 | 82.3±2.16 | 75 | 84.4±3.39 |
MRI measurements from the lower thoracic vertebrae to the lumbar vertebrae were performed in 660 patients (315 men and 345 women) with low back pain.
MRI Protocol
All T2-weighted sagittal MRI images were obtained with a 1.5-T superconducting imager (Brivo MR355, GE, Healthcare, Milwaukee, WI, USA) using a fast-recovery fast spin-echo. Imaging protocols for cervical spine MRI were as follows: repetition time (TR)/echo time (TE), 3400/120; echo train length, 19; slice thickness, 4 mm; slice gap, 0.8 mm; field of view, 24 cm; matrix size, 352/0/0/224; number of excitations, 3. Imaging protocols for lumbar spine MRI were as follows: TR/TE, 3400/85; echo train length, 21; slice thickness, 4 mm; slice gap, 0.8 mm; field of view, 30 cm; matrix size, 320/0/0/224; number of excitations, 2.
Measurements
The distances between the superior and inferior vertebral discs were measured posteriorly from C3 to C7 and from Th11 to L5, i.e., the distances between the adjacent centers of the intervertebral disc spaces. The posterior vertebral body height was measured, including one-half of the height of each of the two adjacent intervertebral discs (Fig. 1).
Statistical Analysis
The sex-related differences in MRI measurements were individually analyzed at each vertebral level from C3 to C7 and from Th11 to L5 by using Student’s t-test. The differences between MRI measurements of the aged patients (80–89 years of age) and cadaveric measurements of aged samples (mean age at death was 85.7 years for the male cadavers and 84.8 years for the female cadavers) were individually analyzed at each vertebral level from C3 to C7 and from Th11 to L5 by using Student’s t-test.
RESULTS
Cadaveric Findings
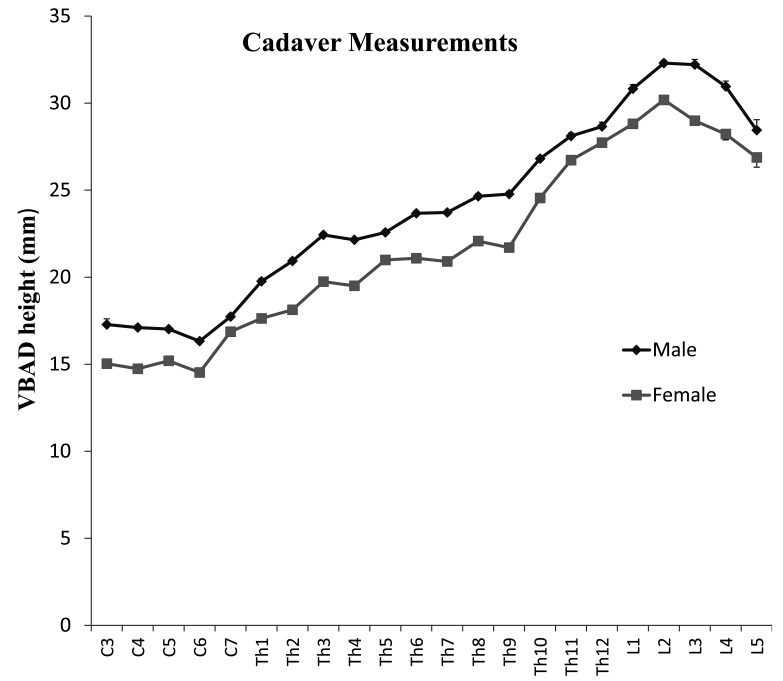
We found no peridural adhesions while removing the posterior spinal elements such as the laminae, pedicles, and spinous processes to expose the dural sac and dissecting the dura to expose the surface of the posterior longitudinal ligament. For example, the anterior meningeal ligament (a small string diagonally connecting the dura mater and posterior longitudinal ligament) could be easily identified and dissected at each attachment point to the posterior longitudinal ligament during the actual process. Because of the old age at death of all cadavers, the intervertebral discs bulged and were convex from the posterior aspect in all samples; in contrast, the surfaces of the vertebral bodies appeared flat. Trial vertebral disc position punctures with a scalpel occasionally resulted in strong resistance, which often indicated partial calcification of the posterior longitudinal ligament at that disc level. We analyzed the measurements and found that the mean VBAD heights were statistically greater in men than in women from C3 to L5/S1. However, no significant differences in VBAD height were found at the C7 and Th12 levels (Fig. 2).
Fig. 2.
In cadaveric measurements, the mean VBAD height was statistically greater (P<0.05) in men than in women from C3 to L5/S1; the exceptions were the C7 and Th12 vertebrae, for which there was no difference. Means and SEs are indicated.
MRI Findings
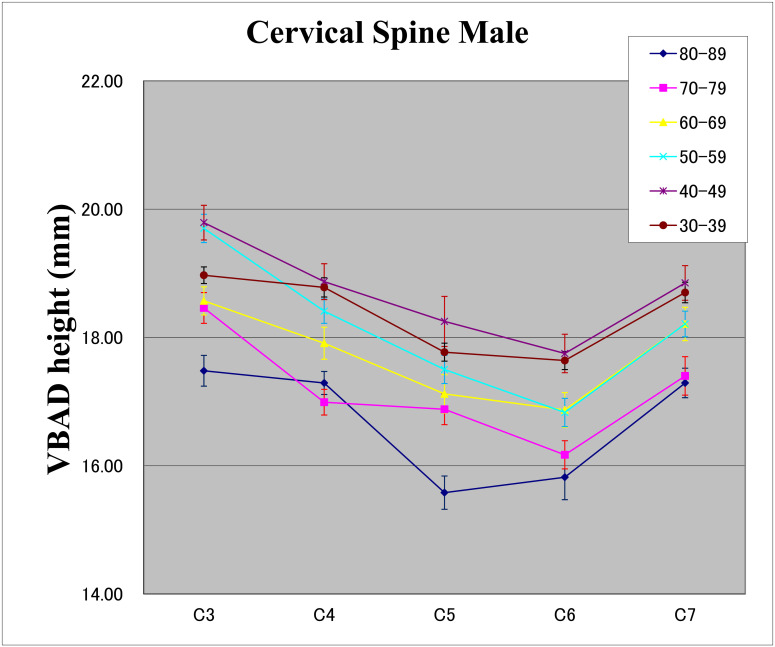
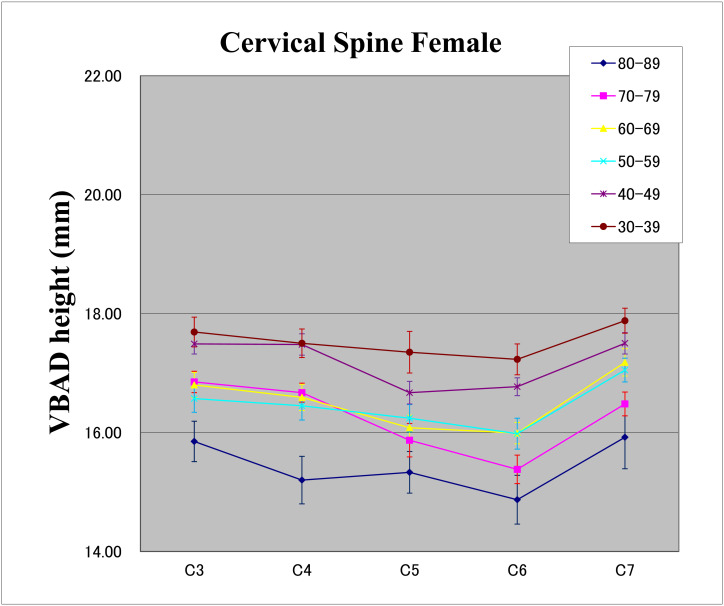
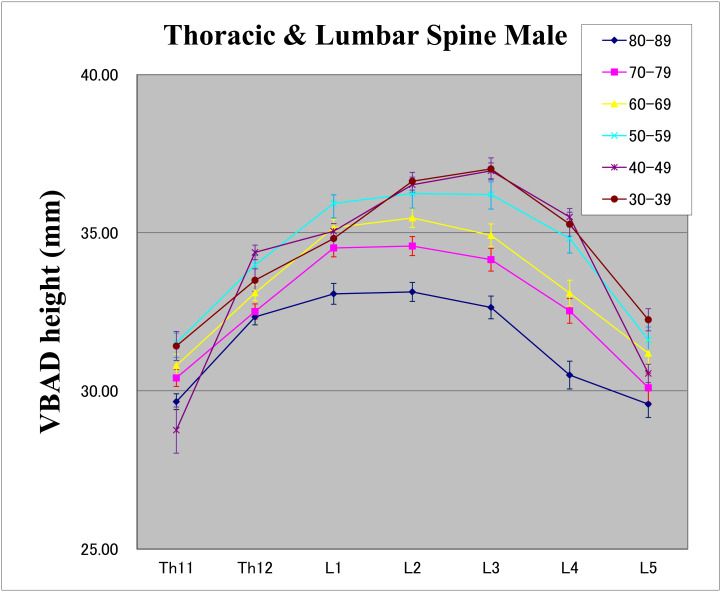
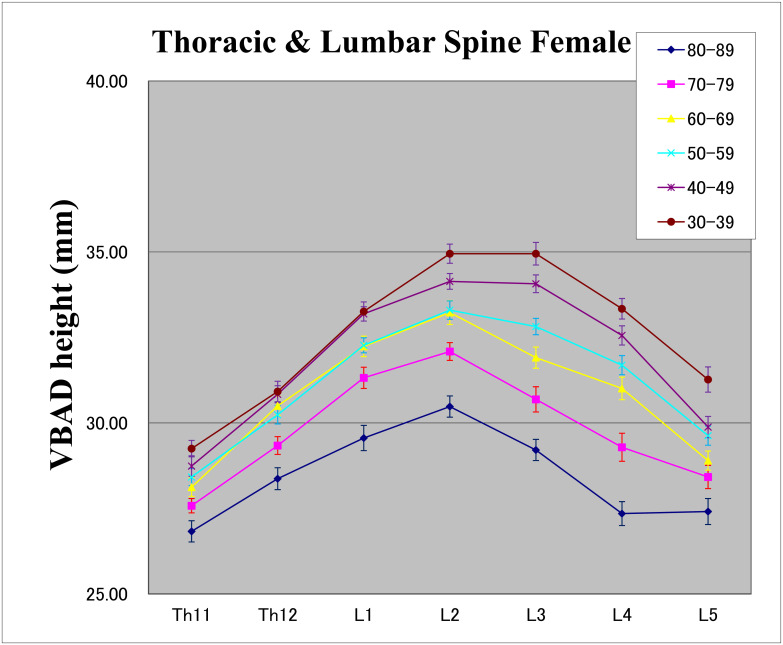
In the cervical spine, C6 had the smallest VBAD heights in men aged 30–79 years, and the VBAD height decreased with age at all sites from C3 to C7. However, in men aged 80–89 years, C5 had the lowest VBAD height, but the C6 height was very similar (Fig. 3). In women, C6 had the minimum VBAD heights in all age groups other than those aged 40–49 years; for all age groups, the C5 and C6 VBAD heights were similar and were close to the minimum value. Moreover, the minimum value at C6 decreased rapidly with age (Fig. 4). For the thoracic and lumbar spine, the maximum values were found at L2 or L3 in all age groups in both men and women, and the VBAD heights for all vertebrae from Th11 to L5 decreased with age (Fig. 5, 6). In women, the values at L3 decreased rapidly with age. MRI measurements indicated sex-related differences in that the mean VBAD height was greater in men than in women in almost all parts of the cervical spine for all age groups. However, C5 and C6 values in those aged 80–89 years, the C4 value in those aged 70–79 years, and C5 and C6 values in those aged 30–39 years showed no significant sex-related differences (Fig. 3, 4). For the lower thoracic vertebrae and the lumbar vertebrae, the mean VBAD heights were significantly greater in men than in women for all age groups (Fig. 5, 6).
Fig. 3.
MRI measurements of the VBAD height of cervical spines in men with neck pain. Means and SEs are indicated.
Fig. 4.
MRI measurements of the VBAD height of cervical spines in women with neck pain. Means and SEs are indicated.
Fig. 5.
MRI measurements of the VBAD height of lumbar spines in men with low back pain. Means and SEs are indicated.
Fig 6.
MRI measurements of the VBAD height of lumbar spines in women with low back pain. Means and SEs are indicated.
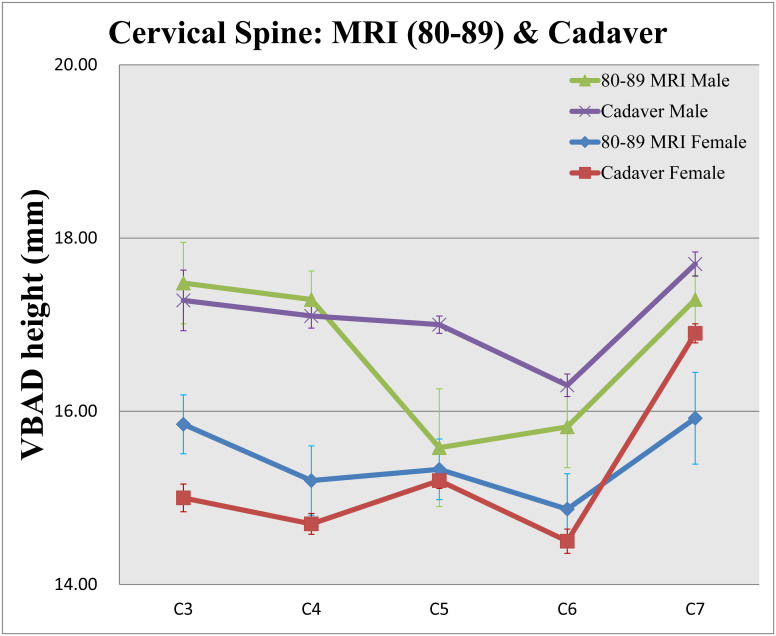
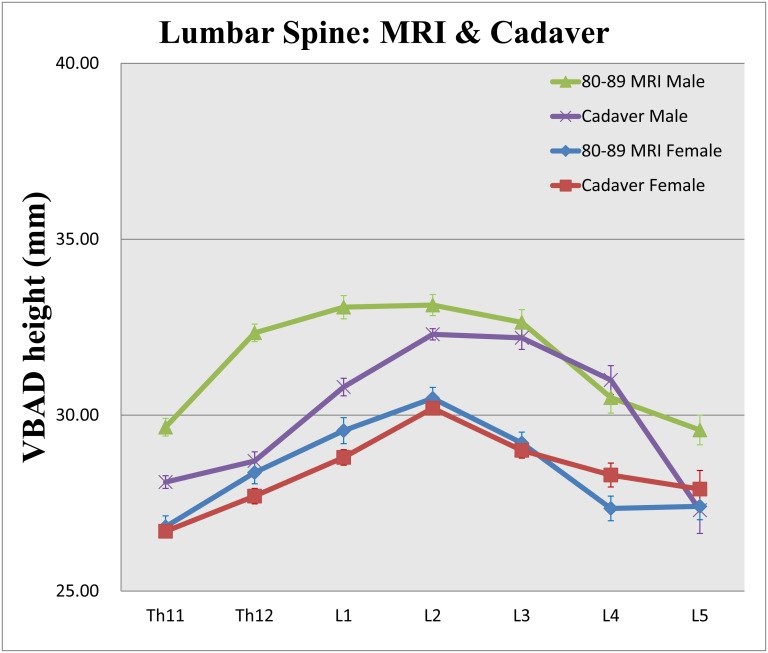
Comparison of the Cadaveric and MRI Measurements
Comparing the data from the cadaveric samples with the outpatient MRI measurements for subjects aged 80–89 years, the VBAD height from cadaveric samples was significantly larger than the MRI value only at the C5 level for men. For women, no significant difference was observed at C3, C4, C5, or C6 between the cadaveric and MRI data, whereas at C7, the cadaveric samples showed slightly higher values than those measured using MRI (Fig. 7). From the lower thoracic vertebrae to the lumbar vertebrae in men, the cadaveric measurements were significantly lower at Th11, Th12, L1, L2, and L5. In contrast, for women, no significant difference was observed at any thoracic or lumbar vertebral level between the cadaveric and MRI data (Fig. 8).
Fig. 7.
Comparison of the cadaveric and MRI VBAD heights of the cervical spine. Means and SEs are indicated.
Fig. 8.
Comparison of the cadaveric and MRI VBAD heights from the lower thoracic vertebrae to the lumbar vertebrae. Means and SEs are indicated.
DISCUSSION
Age-related disc degeneration and subsequent vertebral body degeneration have been studied using various methods and indicate some sex-related differences.16,17,18,19) Among the previous findings from Japan, one investigation reported that from the second to the eighth decades of life, nearly all developmental spinal canal dimensions were smaller in women than in men. Radiographic data from Japanese people (1230 asymptomatic volunteers with at least 100 men and 100 women in each decade of life between the third and eighth decades) showed that the central vertebral body height of men was larger than that of women between the C3 and C7 levels. The disc height in men was also higher than that in women between the C2/C3 and C5/C6 disc levels from the second to the eighth decades of life.16) Lumbar spine radiography has indicated that disc space narrowing proceeds to a greater degree in women than in men, based on the investigation of the prevalence of lumbar disc space narrowing in elderly (age >65 years) Chinese men and women.17) By using MRI, Teraguchi et al. reported the prevalence and distribution of intervertebral disc degeneration over the entire spine (975 participants; 324 men, mean age of 67.2 years; 651 women, mean age of 66.0 years) and focused on the sex-related differences. That study revealed that the prevalence of disc degeneration was highest at C5/C6 (men: 51.5%, women: 46%), T6/T7 (men: 32.4%, women: 37.7%), and L4/L5 (men: 69.1%, women: 75.8%).18) Miękisiak et al. reported that the vertebral body height decreases whereas the vertebral disc height increases with age. This finding was based on the retrospective analysis of collected computed tomography (CT) data of the lumbar spine from 31 men aged 20–73 years and 31 women aged 20–78 years.19)
Many studies have investigated the sex- and age-related differences in spinal degeneration, focusing on the posterior vertebral body height; we identified studies that used direct measurements from plain X-ray radiographs,20,21) CT scans,22) MRI scans,23,24) adult human cadavers,25) and vertebral samples of a human osteological collection.26) By using data obtained from cervical spine X-ray radiographs of 120 adults (69 men and 51 women; age range, 20–80 years), Liguoro et al. reported that the posterior vertebral body height was higher in men than in women.20) Focusing on postmenopausal effects, Diacinti et al. reported measurements from lumbar spine X-ray radiographs from 50 healthy premenopausal and 76 healthy postmenopausal women (age range, 39–74 years) and found that the posterior vertebral body height decreased significantly in postmenopausal women.21) On the basis of lumbar spine CT image data of 126 patients who presented with low back pain (55 men, mean age 50±13.60 years; 71 women, mean age 49±12.04 years), Zhou et al. reported that the posterior height of the vertebral discs was higher in men than in women.22)
Other studies used MRI measurements.23,24) For example, Hong et al. used MRI to investigate the intervertebral spaces of relatively young patients. From their MRI measurements of subjects with the chief complaint of lumbar pain (138 men, mean age 20.51 years; 40 women, mean age 21.38 years), Hong et al. found that the size of the posterior intervertebral space was larger in women than in men.23) Hegazy and Hegazy reported that the mean MRI-measured posterior height of vertebral bodies from L1 to L5 was greater in men than in women. Moreover, they also reported that the mean posterior disc height at L1/L2 was greater in women than in men, whereas those from L2/L3 to L5/S1 were greater in men than in women.24) Twomey and Taylors’ study of 206 cadavers showed that, in most individuals, small decreases in marginal intervertebral disc height (anterior and posterior) were countered by an increase in central height. Young adults of both sexes were, on average, taller than the old adults.25)
One report analyzed 4080 thoracic and lumbar vertebrae obtained from 240 normal complete spines in adult human skeletons that were part of the Hamann–Todd Human Osteological Collection housed at the Cleveland Museum of Natural History, Cleveland, OH, USA. The data obtained from lumbar spine skeletal specimens indicated that the posterior vertebral body height was larger in men than in women.26)
For the cervical spine, the present study found that C6 had the smallest VBAD height in all age groups for men and that the VBAD height at C6 rapidly decreased with age in women. Regarding the lumbar spine, both men and women had maximum VBAD heights at L2 or L3 for all ages, but in the women, the L3 and L4 values rapidly decreased with age. These MRI results suggest some possible differences between men and women in age-related changes in both cervical and lumbar vertebrae. The present study confirmed the previous findings that nearly all developmental spinal canal dimensions were smaller in women than in men, taking into account age-related changes.
We also compared the MRI data from elderly patients (those aged 80–90 years) with the direct measurements on cadavers with a similar age at death. Treatment with formalin and ethanol is considered to result in atrophy of the vertebral body and intervertebral disc tissue. Despite the lifelike appearance of cadavers treated using this method, preservation has a major drawback. Fixation in ethanol causes shrinkage of bone tissue specimens,27) and all preservation methods cause some morphological, biomechanical, and histological changes in soft tissue such as vertebral discs, including shrinkage effects.28) Ten percent formalin solution has been commonly used as a fixative solution since 1893 without much modification.29) Formaldehyde is an excellent fixative, disinfectant, and preservative; however, its use is generally associated with extreme rigidity.30) In the embalming setting, ethanol is also widely used as an alcoholic solvent and anti-infective agent. In addition, some authors have suggested that excess formaldehyde can be washed away by ethanol31)
In the present study, the cadaveric measurements of VBAD height were significantly smaller than the MRI measurements in men at Th11, Th12, L1, L2, and L5. In women, no significant differences were found at any level of the thoracic or lumbar spine. From these findings, the most noteworthy observation was that a sharp decrease in VBAD height compared with the MRI measurements, which could be attributed to postmortem fixation, was observed at the lower thoracic and upper lumbar levels in men but not in women. Considering that fixation causes the spinal structure to shrink, areas that have significantly lower values than that indicated by MRI data may not yet have much degeneration of the vertebral body and disc tissue in vivo. These results are likely to indicate that lower thoracic and upper lumbar spinal mobility is more restricted in aged women. Therefore, care must be taken not to use excessive dynamic exercise during rehabilitation, and older female patients may require more gentle manipulation procedures.
CONCLUSIONS
We statistically analyzed the sex- and age-related changes of the posterior VBAD height of the spine. By using cadaveric and MRI measurements, the present study suggested that age-related changes of the cervical and lumbar spine are associated with differences between men and women in the degrees of progressive vertebral body and disc degeneration.
Footnotes
CONFLICTS OF INTEREST: None of the authors have any conflicts of interest or disclosures in relation to this work.
REFERENCES
- 1.Briggs AM,Woolf AD,Dreinhöfer K,Homb N,Hoy DG,Kopansky-Giles D,Åkesson K,March L: Reducing the global burden of musculoskeletal conditions. Bull World Health Organ 2018;96:366–368. 10.2471/BLT.17.204891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators: Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1211–1259. 10.1016/S0140-6736(17)32154-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsang A,Von Korff M,Lee S,Alonso J,Karam E,Angermeyer MC,Borges GL,Bromet EJ,de Girolamo G,de Graaf R,Gureje O,Lepine JP,Haro JM,Levinson D,Oakley Browne MA,Posada-Villa J,Seedat S,Watanabe M,Watanabe M: Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain 2008;9:883–891. 10.1016/j.jpain.2008.05.005 [DOI] [PubMed] [Google Scholar]
- 4.Antoniou J,Steffen T,Nelson F,Winterbottom N,Hollander AP,Poole RA,Aebi M,Alini M: The human lumbar intervertebral disc: evidence for changes in the biosynthesis and denaturation of the extracellular matrix with growth, maturation, ageing, and degeneration. J Clin Invest 1996;98:996–1003. 10.1172/JCI118884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frobin W,Brinckmann P,Kramer M,Hartwig E: Height of lumbar discs measured from radiographs compared with degeneration and height classified from MR images. Eur Radiol 2001;11:263–269. 10.1007/s003300000556 [DOI] [PubMed] [Google Scholar]
- 6.Adams MA,Roughley PJ: What is intervertebral disc degeneration, and what causes it? Spine 2006;31:2151–2161. 10.1097/01.brs.0000231761.73859.2c [DOI] [PubMed] [Google Scholar]
- 7.Naylor A: The biophysical and biochemical aspects of intervertebral disc herniation and degeneration. Ann R Coll Surg Engl 1962;31:91–114. [PMC free article] [PubMed] [Google Scholar]
- 8.Twomey L,Taylor J: The lumbar spine: structure, function, age changes and physiotherapy. Aust J Physiother 1994;40:19–30. 10.1016/S0004-9514(14)60620-6 [DOI] [PubMed] [Google Scholar]
- 9.Dunlop RB,Adams MA,Hutton WC: Disc space narrowing and the lumbar facet joints. J Bone Joint Surg Br 1984;66-B:706–710. 10.1302/0301-620X.66B5.6501365 [DOI] [PubMed] [Google Scholar]
- 10.Pollintine P,Dolan P,Tobias JH,Adams MA: Intervertebral disc degeneration can lead to “stress-shielding” of the anterior vertebral body: a cause of osteoporotic vertebral fracture? Spine 2004;29:774–782. 10.1097/01.BRS.0000119401.23006.D2 [DOI] [PubMed] [Google Scholar]
- 11.Hussain M,Natarajan RN,An HS,Andersson GB: Patterns of height changes in anterior and posterior cervical disc regions affects the contact loading at posterior facets during moderate and severe disc degeneration: a poroelastic C5-C6 finite element model study. Spine 2010;35:E873–E881. 10.1097/BRS.0b013e3181dc60a9 [DOI] [PubMed] [Google Scholar]
- 12.Dobbs MB,Buckwalter J,Saltzman C: Osteoporosis: the increasing role of the orthopaedist. Iowa Orthop J 1999;19:43–52. [PMC free article] [PubMed] [Google Scholar]
- 13.Kwok AW,Wang YX,Griffith JF,Deng M,Leung JC,Ahuja AT,Leung PC: Morphological changes of lumbar vertebral bodies and intervertebral discs associated with decrease in bone mineral density of the spine: a cross-sectional study in elderly subjects. Spine 2012;37:E1415–E1421. 10.1097/BRS.0b013e31826f561e [DOI] [PubMed] [Google Scholar]
- 14.Birrell F,Pearce MS,Francis RM,Parker L: Self-report overestimates true height loss: implications for diagnosis of osteoporosis. Clin Rheumatol 2005;24:590–592. 10.1007/s10067-005-1112-y [DOI] [PubMed] [Google Scholar]
- 15.Xu W,Perera S,Medich D,Fiorito G,Wagner J,Berger LK,Greenspan SL: Height loss, vertebral fractures, and the misclassification of osteoporosis. Bone 2011;48:307–311. 10.1016/j.bone.2010.09.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yukawa Y,Kato F,Suda K,Yamagata M,Ueta T: Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: Radiographic data from over 1,200 asymptomatic subjects. Eur Spine J 2012;21:1492–1498. 10.1007/s00586-012-2167-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang YX,Griffith JF,Zeng XJ,Deng M,Kwok AW,Leung JC,Ahuja AT,Kwok T,Leung PC: Prevalence and sex difference of lumbar disc space narrowing in elderly Chinese men and women: osteoporotic fractures in men (Hong Kong) and osteoporotic fractures in women (Hong Kong) studies. Arthritis Rheum 2013;65:1004–1010. 10.1002/art.37857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Teraguchi M,Yoshimura N,Hashizume H,Muraki S,Yamada H,Minamide A,Oka H,Ishimoto Y,Nagata K,Kagotani R,Takiguchi N,Akune T,Kawaguchi H,Nakamura K,Yoshida M: Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: The Wakayama Spine Study. Osteoarthritis Cartilage 2014;22:104–110. 10.1016/j.joca.2013.10.019 [DOI] [PubMed] [Google Scholar]
- 19.Miękisiak G,Łątka D,Janusz W,Urbański W,Załuski R,Kubaszewski Ł: The change of volume of the lumbar vertebrae along with aging in asymptomatic population: a preliminary analysis. Acta Bioeng Biomech 2018;20:25–30. [PubMed] [Google Scholar]
- 20.Liguoro D,Vandermeersch B,Guérin J: Dimensions of cervical vertebral bodies according to age and sex. Surg Radiol Anat 1994;16:149–155. 10.1007/BF01627588 [DOI] [PubMed] [Google Scholar]
- 21.Diacinti D,Acca M,D’Erasmo E,Tomei E,Mazzuoli GF: Aging changes in vertebral morphometry. Calcif Tissue Int 1995;57:426–429. 10.1007/BF00301945 [DOI] [PubMed] [Google Scholar]
- 22.Zhou SH,McCarthy ID,McGregor AH,Coombs RR,Hughes SP: Geometrical dimensions of the lower lumbar vertebrae – analysis of data from digitised CT images. Eur Spine J 2000;9:242–248. 10.1007/s005860000140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hong CH,Park JS,Jung KJ,Kim WJ: Measurement of the normal lumbar intervertebral disc space using magnetic resonance imaging. Asian Spine J 2010;4:1–6. 10.4184/asj.2010.4.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hegazy AA,Hegazy RA: Midsagittal anatomy of lumbar lordosis in adult Egyptians: MRI study. Anat Res Int 2014;2014:1–12. 10.1155/2014/370852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Twomey L,Taylor J: Age changes in lumbar intervertebral discs. Acta Orthop Scand 1985;56:496–499. 10.3109/17453678508993043 [DOI] [PubMed] [Google Scholar]
- 26.Masharawi Y,Salame K,Mirovsky Y,Peleg S,Dar G,Steinberg N,Hershkovitz I: Vertebral body shape variation in the thoracic and lumbar spine: characterization of its asymmetry and wedging. Clin Anat 2008;21:46–54. 10.1002/ca.20532 [DOI] [PubMed] [Google Scholar]
- 27.Gedrange T,Mai R,Mack F,Zietek M,Borsos G,Vegh A,Spassov A,Gredes T: Evaluation of shape and size changes of bone and remodelled bone substitute after different fixation methods. J Physiol Pharmacol 2008;59(Suppl 5):87–94. [PubMed] [Google Scholar]
- 28.Beger O,Karagül Mİ,Koç T,Kayan G,Cengiz A,Yılmaz ŞN,Olgunus ZK: Effects of different cadaver preservation methods on muscles and tendons: a morphometric, biomechanical and histological study. Anat Sci Int 2020;95:174–189. 10.1007/s12565-019-00508-z [DOI] [PubMed] [Google Scholar]
- 29.Brenner E: Human body preservation – old and new techniques. J Anat 2014;224:316–344. 10.1111/joa.12160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hopwood D: Fixatives and fixation: a review. Histochem J 1969;1:323–360. 10.1007/BF01003278 [DOI] [PubMed] [Google Scholar]
- 31.Björkman N,Nielsen P,Møller VH: Removing formaldehyde from embalmed cadavers by percolating the body cavities with dilute ethanol. Cells Tissues Organs 1986;126:78–83. 10.1159/000146192 [DOI] [PubMed] [Google Scholar]