Abstract
Background
Social Anxiety Disorder (SAD) is among the most common anxiety disorders worldwide with data largely emerging from the Euro-American and Pacific Rim populations. In contrast, there is a dearth of studies among the populations of Arabian Gulf countries including Oman. This study has two interrelated aims: (i) to explore the prevalence of SAD among Omani adults, and (ii) to tease out the links between socio-demographic factors and SAD in Oman.
Methods
A cross-sectional study via an online survey was conducted among 1019 adult Omani nationals residing in Oman. The presence of SAD was assessed using the Arabic version of the Liebowitz Social Anxiety Scale (LSAS).
Results
Nearly half the participants (45.9%, n = 468) exhibited “caseness” for SAD as defined by LSAS. In the multivariate logistic analysis, participants below 40 years of age were 1.6 times (OR = 1.568, p = .026) more likely to have caseness for SAD than those who were 40 and older. Women were 1.3 times (OR = 1.348, p = .038) more likely to exhibit caseness for SAD than men. Participants who had secondary or undergraduate education were respectively 1.5 times (OR = 1.45, p = .014) and 2.5 times (OR = 2.509, p < .001) to have caseness for SAD than those who were graduates.
Conclusion
The present data suggest that 45.9% of the participants reached the cut-off for caseness in LSAS, which is high compared to reports from other populations. The present accrued frequency is discussed within the context of the accrued response rate, socio-cultural factors as well as the tendency for self-reported measures to “produce” spurious results is also highlighted which, in turn, calls for studies that adopt more inclusive survey methods.
Keywords: stress, social anxiety disorder, SAD, social phobia, liebowitz social anxiety scale, focused national survey, adult, Oman
Introduction
Social Anxiety Disorder (SAD), more commonly known as social phobia, is characterized by morbid fears of being the focus of attention, or fear of conducting oneself that would lead to embarrassment or humiliation. 1 The outcome of such preoccupation can be avoidance of social exposure, and if exposed, development of a spectrum of anxiety symptoms as well as physical distress, often manifested as unwarranted trembling, sweating, blushing, palpitations and biliousness. 2 In this context, affected tend to be perceived as “shy-inhibited individuals”. 3 Initially thought to be rare in the general population, 4 this “illness of lost opportunities” is being increasingly recognized as a “hidden epidemic”.5–7 In the USA, a community survey using standardized diagnostic procedures 8 suggested a prevalence of 2%–3% among the general population. In Australia, Lampe et al. reported 1%–2.7%. 9 In Brazil, a community survey found a prevalence of 4.7–7.9%, 10 depending on the psychiatric nomenclature used. In Sweden, a postal survey among nationally representative adults suggested a very high prevalence of 15.6%. 11 The majority of the epidemiology SAD reports have largely emerged from high-income countries of Western Europe, North American, and the Pacific Rim. To fill the gap in the literature, the WHO initiative known as “Data from the World Mental Health Survey Initiative” reported the cross-national epidemiology of SAD. 7 This study conducted community surveys among 28 countries in The World Mental Health Survey Initiative, with 142,405 respondents. The lifetime prevalence estimates were found to range from 1.3–4.0% across all countries. While this study purported to survey prevalence estimates among Eastern Mediterranean, there is no data from Arabian Gulf countries. A few hospitals and college-based studies conducted on the Arabian Gulf population suggest that SAD is common in this region.12,13 These tentative results suggest that wider community studies are warranted in the Gulf region. Additionally, there is increasing evidence to suggest that there are strong sociocultural influences that are critically involved in the expression and experience of shy-inhibited temperament.14,15 It remains to be seen whether the recent globalization and acculturation have an impact on shy-inhibited individuals. Related to this, in Oman, the Arabic word for the concept of shame and shyness is widely articulated using the word khajal, or those with this attribute are known under the name of Khajuul. Likely, in western nosology and psychiatric nomenclature, individuals with something resembling an excessive provision of Khajuul are labeled as having a social phobia or social anxiety disorders. The open question how individuals from such society fare when scrutinized with indices of SAD.
Numerous studies have examined the factors associated with SAD. In terms of gender, various studies have concluded that SAD seemingly more common in females (5.67%) than in males (4.20%).16,17 Studies among college students in Arabian Gulf countries have also endorsed this trend.18–20 However, the literature also yields a few studies which have reported the opposite trend.21,22 More investigation is therefore warranted.
Besides gender, age is also associated with SAD, with likely onset during childhood or adolescence. 23 Shyness in childhood perhaps is a strong determinant of SAD in adulthood and that adult-onset SAD is rare. 24 However, Solmi et al. 25 reported adult-onset SAD among their older subjects. Even though the Arabian Gulf studies have reported that SAD tends to manifest during the formative years, 26 these findings emerged from school- and college-going populations. Studies are needed among the Arabian Gulf adult population to determine the onset and prevalence of SAD among all age groups.
An important characteristic of SAD is that it affects interpersonal relationships. Hart et al. 27 have suggested that “some individuals with social phobia manage to construct a lifestyle that allows them to avoid anxiety-provoking social interactions, but that also leads to loneliness and isolation” (p. 31). This is supported by the observation in Western populations that people with SAD are more likely to be single. 8 As most studies in the Arabian Gulf have focused on pre-adults, the relation of marital status SAD remains unexplored. Addressing this issue would shed light on the sociodemographic factors associated with SAD.
In general, studies from both developed and emerging economies suggest higher prevalence of psychiatric disorders in urban areas which is often attributed to lower social cohesion in cities. 28 Intuitively, one would assume that those with SAD would fare worse in an urban setting. It is also possible that the traditional rural setup consisting of close-knit families with frequent interactions between neighbors might not be preferred by people with SAD. While ample studies are emerging worldwide, throwing light into the urban-rural dichotomy among the psychiatric population, 29 such studies are scant in the Arabian Gulf in the context of SAD.
Since the tendency to avoid anxiety-provoking social interactions is the hallmark of people with SAD, the condition can be presumed to impact their educational attainments as well. Some studies have suggested that there is pervasive academic underachievement among people with SAD. Heimberg et al. 30 have suggested that indices such as educational attainment depend on whether the SAD is characterized by “exclusive speaking fears” or “social-evaluative fears”. However, due to insufficient research internationally, the relationship between SAD and educational attainments is still unclear, calling for more studies. Related to education is the issue of employment or labor-force participation. Some studies perceive SAD as a barrier to steady careers and labor-force participation compared to the general population. 31 People with SAD are also likely to endorse the view that their work is stressful and seek earlier retirement. 32
The aforementioned discussion has suggested that while SAD has been reported in the Arabian Gulf population, the majority of them have been focused on hospital-based studies or children and adolescents and particularly those in education streams. There is a dearth of studies conducted on the general population. This study aimed to take advantage of the emerging online research tools to explore the prevalence of SAD among adult Omanis and examine the association between SAD and sociodemographic variables.
Methodology
Setting
The present online survey was conducted from October 2 to November 3, 2019, following the protocol followed elsewhere. 33 During this period there were approximately 3.3 million internet users (∼72% of population total). Oman's high middle-income status, youthful demography, high literacy level (>97%), 34 has resulted in the predominance of people who are well-versed users of online social media. 33 Oman has eleven administrative governorates (muhafazah). The targeted population was stratified according to the population for each administrative governorate. The inclusion criteria included Omani nationals >18 years of age. An electronically signed, printable consent form was sent to the invitees specifying that they needed to give their consent before answering the questions in the study proforma.
Online Survey
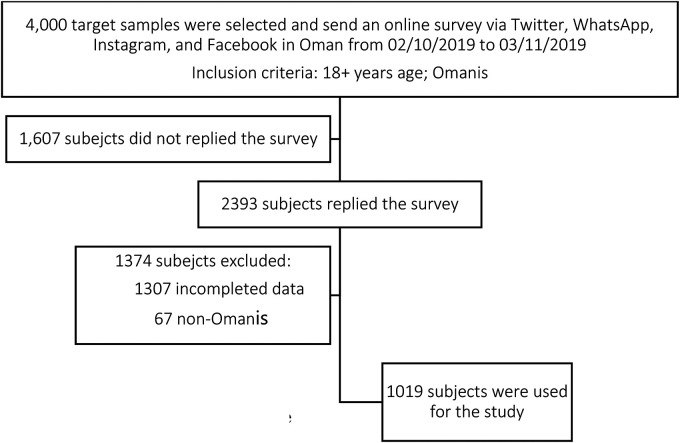
To reach all strata of the society, a video clip of the study and URL of the study proforma was distributed via popular social media platforms such as Twitter, WhatsApp, Instagram and Facebook. All participants were informed that their participation would remain confidential and voluntary, collected data would be aggregated, and could withdraw from the study at any time. Out of 4000 target samples, 1607 subjects did not reply to the survey and thus 2393 subjects replied to the survey. Participants who had sent in incomplete data were excluded, leaving 1086 participants. Among them, 67 non-Omanis were excluded. The final number of participants whose responses were admitted into the study was n = 1019 (see Figure 1).
Figure 1.
Flowchart for the enrolment of subjects.
Outcome Measures
The present study survey has two parts. The first one is sociodemographic data and the other is outcome measures. These are detailed in tandem below.
Sociodemographic Information
The first part of the study questionnaire sought socio-demographic information like gender, marital status, labor-force participation as shown in Table 1. The majority of Oman's population lives in the long, narrow northern coastal region overlooking the Gulf of Oman. The capital Muscat and its satellite towns are also located here which has been duly labeled as an urban part of Oman. The rest of the population lives in/near Al Hajar and Qara Mountains adjacent to the “Empty Quarter” or Rub Al Khali desert. 35 Those participants living outside Muscat and its satellite towns were labeled as rural dwellers. 36 Education level was also explored. In Oman, the educational level is labeled as “secondary education” which constitutes 12 years of formal education, “undergraduate” denotes a 4-year tertiary education known as a bachelor's degree while graduate implies participants who have secured equivalent or above master's degree program.
Table 1.
Sociodemographic Variables of Participants (n = 1019).
| Social Phobia | |||
|---|---|---|---|
| Total (n = 1019) | Yes (n = 468) 45.9% | No (n = 551) 54.1% | |
| Demographics | n (%) | n (%) | n (%) |
| Gender | |||
| Female | 522 (51.2) | 261 (55.8) | 261 (47.4) |
| Male | 497 (48.8) | 207 (44.2) | 290 (52.6) |
| Age (Years) | |||
| 18-39 | 860 (84.4) | 419 (89.5) | 441 (80.0) |
| 40 + | 159 (15.6) | 49 (10.5) | 110 (20.0) |
| Marital Status | |||
| Married | 534 (52.4) | 270 (57.7) | 264 (47.9) |
| Not married, eg, single, divorced, widow | 485 (47.6) | 198 (42.3) | 287 (52.1) |
| Urban-rural dichotomy | |||
| Rural | 562 (55.2) | 271 (57.9) | 291 (52.8) |
| Urban | 457 (44.8) | 197 (42.1) | 260 (47.2) |
| Educational level | |||
| Secondary education | 291 (28.6) | 163 (34.1) | 128 (23.2) |
| Undergraduate | 545 (53.5) | 251 (53.6) | 294 (53.4) |
| Graduate | 183 (18.0) | 54 (11.5) | 129 (23.4) |
| Other, eg, housewife, retired, unemployed | 112 (11.0) | 58 (12.4) | 54 (9.8) |
| Labor-force participation | |||
| Student | 310 (30.4) | 171 (36.5) | 139 (25.2) |
| Employed (ref) | 597 (58.6) | 239 (51.1) | 358 (65.0) |
Social Phobia, Liebowitz Social Anxiety Scale (LSAS): Yes: ≥ 55, No (absent): ≤ 54.
Outcome Measures
To identify the presence of SAD, the Liebowitz Social Anxiety Scale (LSAS)-self-report measures- was employed. The LSAS focuses on the way that SAD plays a role in the life of the respondent, in a variety of situations. The respondent is asked to relate to their behavior in the past week. LSAS has 24 items that focus on two aspects of SAD, namely social relationships and performance, on its Likert type questionnaire which gave options to respondents on a 0–3 scale (“none”, “mild”, “moderate”, “severe”). 37 LSAS has undergone extensive validation in various populations and linguist groups including in the Arab population.38–40 Its psychometric properties are adequate, including the presently used Arabic version, which has identified a cut-off of 55 to differentiate between the case and non-case. 41
Data Analysis
Data was analyzed by SPSS v23.0 package and the results of those who were identified as having SAD versus without (LSAS ≥55 vs. LSAS ≤54) were analyzed using descriptive statistics. Univariate analysis was used, and demographic variables were evaluated with the chi-square test and odds ratio to reveal the association between the SAD and normal groups. Next, multiple logistic regression analyses were used, where SAD status was the dependent variable, and those variables in the univariate analysis were the independent variables and concurrently adjusted by each other. This analysis could address the research aim to identify the contributing variables associated with SAD.
Ethical Approval
The study was approved by the Ethics Committee of the College of Medicine at Sultan Qaboos University Hospital (MREC#1749). Informed consent and assent were obtained from all individual participants included in the study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study data that support the findings are available from the corresponding author upon reasonable request.
Results
A total of 1019 participants fulfilled the inclusion criteria. Table 1 shows the results for the subject's demographic variables and their association with the SAD status. Out of 1019 participants, 45.9% (n = 468) fulfilled the presence criteria for caseness for SAD. There were more female participants (51.2%) than males (48.8%). The participants’ average age was 29.9 (SD = 8.4 years) years based on a range from 18 to 60 years. More than 71.0% (n = 728) had university education, and 58.6% (n = 597) of them were employed, 52.4% (n = 534) were married, and 55.2% (n = 562) were not living in an urban setting.
Table 2 shows univariate and multivariate (logistic regression) analysis for SAD in association with demographics. Among the demographic variables, a significant association was found between SAD status and gender (OR = 1.401, p = .008), age (OR = 2.133, p < .001), educational level (graduate vs. secondary, OR = 3.042, p < .001; graduate vs. undergraduate, OR = 2.039, p < .001; graduate vs. other, OR = 1.609, p = .021)), marital status (OR = 1.482, p = .002), and labor-force participation (OR = 1.843, p < .001) except for those living in the urban region (OR = 1.229, p = .103). The multivariate logistic analysis suggested that three demographic variables had significant association with SAD. The model shows that subjects who were of ages below 40 years were 1.6 times (OR = 1.568, p = .026) more likely to have SAD than subjects of 40 years and above. Female subjects were reported as 1.3 times (OR = 1.348, p = .038) more likely to have SAD than males. In education, subjects who have completed only secondary education and undergraduate education were 1.5 times (OR = 1.45, p = .014) and 2.5 times (OR = 2.509, p < .001) respectively, more likely to be more prone to SAD than those who had graduate education.
Table 2.
Univariate and Multivariate (Logistic Regression) Analysis for Social Phobia in the Association of Demographic Factors.
| Demographic | Social Phobia | Univariate Analysis | Multivariate Analysis^ | ||||
|---|---|---|---|---|---|---|---|
| Yes (n = 468) | No (n = 551) | ||||||
| n (%) | n (%) | OR | p-value | OR | p-value | ||
| Gender | Female | 261 (55.8) | 261 (47.4) | 1.401 | .008* | 1.348 | .038* |
| Male (ref) | 207 (44.2) | 290 (52.6) | |||||
| Age (Years) | 18-39 | 419 (89.5) | 441 (80.0) | 2.133 | <.001** | 1.568 | .026* |
| 40 + (ref) | 49 (10.5) | 110 (20.0) | |||||
| Marital Status | Married | 270 (57.7) | 264 (47.9) | 1.482 | .002* | 0.907 | .574 |
| Not married (ref)# | 198 (42.3) | 287 (52.1) | |||||
| Urban-rural dichotomy | Rural | 271 (57.9) | 291 (52.8) | 1.229 | .103 | 1.099 | .483 |
| Urban (ref) | 197 (42.1) | 260 (47.2) | |||||
| Educational level | Secondary | 163 (34.1) | 128 (23.2) | 3.042 | <.001** | 1.45 | .014* |
| Undergraduate | 251 (53.6) | 294 (53.4) | 2.039 | <.001** | 2.509 | <.001** | |
| Other∼ | 58 (12.4) | 54 (9.8) | 1.609 | .021* | 0.97 | .895 | |
| Graduate (ref) | 54 (11.5) | 129 (23.4) | |||||
| Labor-force participation | Students | 171 (36.5) | 139 (25.2) | 1.843 | <.001** | 1.234 | .351 |
| Employed (ref) | 239 (51.1) | 358 (65.0) | |||||
Note: Ref, reference point; OR, Odds Ratio; *, sig., p < .05; **, sig., p < .001; Social Phobia, Liebowitz Social Anxiety Scale (LSAS): Yes: ≥ 55, No (absent): ≤ 54; Enter; Hosmer and Lemeshow Test, c2 = 6.506, p = .591; Sensitivity = 68.8%, Specificity = 50.8%, Overall predicting power = 59.1%; #, included single, divorced, and widowed; ∼, included housewives, retired, unemployed.
Discussion
To our knowledge, this is the first focused national survey of Omani adults to examine the prevalence of SAD using an online survey. The related aim has been to examine the factors which influence the development of SAD. Previous studies in Oman have focused on these factors only in educational settings. Using LSAS, Al-Hinai et al. identified 37% of college students to meet the caseness of SAD. 20 Among school-going pupils, using the “Composite International Diagnostic Interview” (CIDI), 42 Al-Sharbati et al. reported 36.6% of the sample as having SAD. 41 In the other Arabian Gulf countries also, there was a SAD prevalence of 11.7% using LSAS 43 and 16.3% using the “Social Phobia Inventory”. 44 While such data are welcome, they do not cover the higher age groups, which is what the current study has attempted. The present results revealed that nearly half the sample, 45.9% (n = 468) had SAD. This figure is higher than the international rates reported from community surveys where prevalence estimates were found to range from 1.3–4.0% across all countries.
Therefore, it is essential to speculate on the factors that could contribute to the presently found higher rate. First, this focused national survey only accrued less than 45% of target respondents that was included in the analysis. This may explain the high prevalence of SAD in this report. One factor that could contribute to low response is that only those with shy-inhibited individuals made attempted to fill the study survey since their temperament may lead them to find the items of the LSAS as salient. The online survey may have contributed to the present high rate. Despite its limitations, the online survey can be fast and cost-effective in reaching a wider community. In addition, there is a heuristic value for the online survey for people with SAD who are known to prefer social media instead of face-to-face communication. 45 However, nonresponses as shown in this study appear to be high. Studies are therefore needed to disentangle on whether online surveys or personalized ones tend to attract all strata of the society. Second, the high rate could stem from the screening tools. The presently used measure, LSAS, constitutes a self-report measure. In community surveys, it has been consistently shown that standardized diagnostic procedures such as those derived by ICD and DSM are more reliable compared to self-report measures. 46 Takada et al. 47 have examined the likelihood of LSAS to have measurement error among the Japanese general adult population (n = 1300). The result suggested LSAS tends to produce high fault positives. More studies are needed to examine whether self-report measures tend to produce spurious results in particular in the non-western population where idioms of distress are different from the western-derived psychiatric nomenclature.
Third, one particular hypothesis suggests that growing up in “collective” societies as those in the Arabian Gulf tend to influence the development of shy-inhibited temperament and conduct which is reinforced by “disciplinarian” or “authoritarian” parental style. 48 Such type of socialization has the net effect of rendering a member of the society to be interdependent rather than independent as prescribed in Euro-American culture. 49 To reinforce interdependence and the resultant conformity, shame is one of the instruments that are likely to be used to foster such sociocultural patterning. 49 Shame, as an instrument to foster interdependence, implies that individuals would embrace external locus of control and become “watchful to the eyes of others”. 50 This may lead to a vulnerable individual being occupied with fears of being the focus of attention, or fear of conducting oneself which in turn could lead to the development of shy-inhibited individuals. 51 There is evidence that such temperaments are more condoned in the collective society. 52 If this assumption is valid, then it is likely that such a society to have the preponderance of shy-inhibited individuals. This hypothesis would require further scrutiny in light of the present figure where nearly half the sample exhibited propensity towards SAD.
The second aim of this study is to establish the correlates of SAD. This study has examined sociodemographic variables such as gender, age, marital status, educational attainment, urban-rural dichotomy, and labor-force participation. While using logistic regression, three variables emerged to be significantly associated with SAD, namely being ≤40 years old, educational level, and female gender. These sociodemographic variables are discussed below in tandem within the background literature.
Vast empirical studies are suggesting that temperament is known as the behavioral inhibition system (BIS), colloquially known as “shyness,” is often associated with SAD. 53 Such a temperament often appears in childhood and may persist into adulthood 23 and the entrance of the diathesis-stress model as postulated 54 may apply to the individuals who are likely to manifest SAD. When SAD is adult-onset, it is likely to be associated with adverse life events and the resultant depression and episodic paroxysmal anxiety. 55 In the present cohort, which was divided into two age groups (<40 vs. >40), SAD is strongly associated with the former. If SAD is mostly childhood-onset, it remains to be seen whether age has the potential to mitigate the symptoms of SAD. This study was not equipped to address this issue. Longitudinal studies are needed to assess the durability of SAD.
Conceptually, if one tends to avoid interpersonal relationships and perceives unfamiliar social behavior as threatening, one would assume that such temperament would hamper one from academic excellence. However, evidence on the link between the pursuit of education and SAD has been generally mixed. Popular author Cain 56 has pointed out a tendency in Euro-American culture to underestimate the capabilities of introverts and the socially timid. In support of such a view, a longitudinal study among Finnish adolescents suggested that teens with SAD are likely to academically underperform their non-SAD peers. 57 Kessler, 58 drawing from the United States National Comorbidity Survey, concluded that teens with SAD are less likely to make a smooth transition from school to higher education. While SAD is perceived as a culturally devalued temperament in the West, in non-western societies, an extroverted individual is more likely to be perceived as selfish and marked with the tendency to disrupt social modesty. 41 Within such a background, the question remains in the relationship between SAD and educational attainment in non-Western cultures such as Oman. Being an online survey, by definition, this study has likely been over-represented by people who are well-versed in social media and educated. Therefore, it is not surprising that the majority of the participants, 53.5%, are undergraduates. In terms of the association between education and SAD, the present study suggests that secondary school and undergraduate education are strongly related to the presence of SAD. The question remains whether the temperament that is intimately related to SAD is a significant dampener in a young person's academic performance and later as an adult, in persons integration into the labor force. More studies are needed to clearly understand this vital issue so that remedial measures can be contemplated.
There are contradictory views on whether gender is strongly associated with SAD. Xu et al. 16 have explored gender differences in SAD among US adult population (n = 43,093). Females appear to surpass their male counterpart in the lifetime prevalence of SAD (5.67% for female vs. 4.20% for male). Further analysis of the data suggested that affected females tend to be marked with internalizing disorders and are more apt to receive pharmacotherapy for SAD. In contrast, the males with SAD have a poor social life and externalizing disorders thus are likely to be pursuing self-medication (alcohol and illicit drugs) to relieve symptoms of SAD. Caballo et al. 17 have examined gender differences in SAD among South and Latin countries (Argentina, Bolivia, Brazil, Colombia, Costa Rica, Chile, Dominican Republic, El Salvador, Guatemala, Honduras, Mexico, Paraguay, Peru, Portugal, Puerto Rico, Uruguay, and Venezuela) and Europe (Spain, and Portugal). The catchment areas were both community and clinical samples. While females scored significantly higher than men in the indices of SAD, when the magnitude of the differences was explored, the authors noted that the differences were not statistically significant. Asher et al. 59 have reviewed extant literature on gender differences and associated factors as functioning, comorbidity, prognostic indicator, healthcare utilization, and biological parameter including the status of oxytocin. The review concluded that SAD tends to affect both genders equally. In the Arab population, there are conflicting views on gender. Ahmed & Alansari 18 have surveyed anxiety using a culturally sensitive measure for tapping anxiety symptoms, Kuwait University Anxiety Scale (KUAS), 60 the region of interest include students in tertiary education (n = 3064) from 10 Arab countries [six from Arabian Gulf, five from the fertile crescent, and one from North Africa]. The study found the mean score of KUAS were higher among female participants in only some of these participating countries (7 out 10). The authors speculated that the preponderance of females in SAD might stem from the socialization process including sex-typing and gender roles. While this study accrued participants in the wider Arab population, it is not clear whether KUAS is equipped to tap into SAD. Previous studies from Oman appear to circumvent the limitation of KUAS. Among school-going pupils in Oman, it is reported more female pupils to be affected than male pupils. 41 Among the college-going population in Oman, Al-Hinai et al. 20 found equal distribution in the endorsement of SAD for both genders. Among the clinical population, Chaleby & Raslan 61 have reported that more males are presenting with symptoms akin to SAD in their clinical practice in Saudi Arabia. Taken together, there are reasons to believe that SAD is more common among women in the education stream yet the trend may change in clinical settings. Our study, the first of its kind in the Omani community also suggests that females are more likely to endorse themselves with the symptoms of SAD than their male counterparts. Oman, in the past decade, has undergone a rapid pace of modernization, the spread of education, and female empowerment. Due to these factors, both tertiary education and the labor force have undergone “feminization” in Oman's society in many spheres of life. 62 Such trend has rendered females to juggle between the traditional sex-typing and gender roles and newly acquired empowerment. Consequently we need to examine the effect of social transition often common in the emerging economies in the global south.
Limitations
Apart from the above discussion, it would be essential to highlight other factors that may hamper the generalizability of the present study, the following seem most important. Firstly, with a presumptive higher rate of SAD, future studies could employ two phase survey whereby the first comprises of screening SAD using self-report measures (eg, LSAS) while the second would follow up with standardized diagnostic procedures. 63 Secondly, the utility of international psychiatric nosology tends to be hampered because of different idioms use. 64 Thus, when screening using international psychiatric nomenclature, the accrued distresses are likely to appear as “atypical”, “unlisted” or “not otherwise classified”. 65 Concerted efforts are needed to develop culture-free measures. Finally, SAD is often associated with the spectrum of psychiatric disorders panic disorder, posttraumatic stress disorder, depression, and substance use disorder. 66 Being a focused national LSAS survey, this possible confounder was not addressed.
Conclusion
This study found the prevalence of SAD among a sample of Omani adults to be at 45.9%. This is much higher than that of international trends. The demographic variables that were positively associated with the endorsement of SAD were female gender, younger age (<40 years), and lower-to-mid strata of education. Further studies are needed on whether sociocultural factors, response rate, and self-reported outcome measures contribute to the high prevalence of SAD in the present region of interest. Replicating this study with a more robust methodology than an online survey alone would be valuable. Rather than self-report measures, it would be more viable to use standardized diagnostic procedures. If this finding withstands scrutiny, then it is essential to mitigate such a high prevalence of SAD as this hidden epidemic may lead to chronic opportunity costs and loss of productivity at individual and national levels.
Acknowledgment
The authors want to thank their respective institutions for their support. The authors also would like to thank all who participated in this study.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: The study was approved by the Ethics Committee of the College of Medicine at Sultan Qaboos University Hospital (MREC#1749). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed Consent: Informed consent and assent were obtained from all individual participants included in the study.
ORCID iD: M. Walid Qoronfleh https://orcid.org/0000-0001-6757-1922
Trial Registration: Not applicable, because this article does not contain any clinical trials.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- 2.Havranek MM, Volkart F, Bolliger Bet al. The fear of being laughed at as additional diagnostic criterion in social anxiety disorder and avoidant personality disorder? PLoS One. 2017; 12(11): e0188024. doi: 10.1371/journal.pone.0188024. PMID: 29176893; PMCID: PMC5703445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poole KL, Van Lieshout RJ, Schmidt LA. Exploring relations between shyness and social anxiety disorder: the role of sociability. Pers Individ Dif. 2017; 110: 55–59. doi: 10.1016/j.paid.2017.01.020 [DOI] [Google Scholar]
- 4.Moutier CY, Stein MB. The history, epidemiology, and differential diagnosis of social anxiety disorder. J Clin Psychiatry. 1999; 60(Suppl 9): 4–8. PMID: 10335673. [PubMed] [Google Scholar]
- 5.Jenike MA. Obsessive-compulsive and related disorders: a hidden epidemic. N Engl J Med. 1989; 321(8): 539–541. doi: 10.1056/NEJM198908243210811. PMID: 2761591. [DOI] [PubMed] [Google Scholar]
- 6.Vilaplana-Pérez A, Pérez-Vigil A, Sidorchuk Aet al. Much more than just shyness: the impact of social anxiety disorder on educational performance across the lifespan. Psychol Med. 2021; 51(5): 861–869. doi: 10.1017/S0033291719003908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stein DJ, Lim C, Roest AMet al. The cross-national epidemiology of social anxiety disorder: data from the world mental health survey initiative. BMC Med. 2017; 15(1): 143. doi: 10.1186/s12916-017-0889-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schneier FR, Johnson J, Hornig CD, Liebowitz MR, Weissman MM. Social phobia. Comorbidity and morbidity in an epidemiologic sample. Arch Gen Psychiatry. 1992; 49(4): 282–288. doi: 10.1001/archpsyc.1992.01820040034004 [DOI] [PubMed] [Google Scholar]
- 9.Lampe L, Slade T, Issakidis C, Andrews G. Social phobia in the Australian national survey of mental health and well-being (NSMHWB). Psychol Med. 2003; 33(4): 637–646. doi: 10.1017/s0033291703007621. PMID: 12785465. [DOI] [PubMed] [Google Scholar]
- 10.Rocha FL, Vorcaro CM, Uchoa E, Lima-Costa MF. Comparing the prevalence rates of social phobia in a community according to ICD-10 and DSM-III-R. Braz J Psychiatry. 2005; 27(3): 222–224. doi: 10.1590/s1516-44462005000300011. Epub 2005 Oct 4. PMID: 16224610. [DOI] [PubMed] [Google Scholar]
- 11.Furmark T, Tillfors M, Everz P, Marteinsdottir I, Gefvert O, Fredrikson M. Social phobia in the general population: prevalence and sociodemographic profile. Soc Psychiatry Psychiatr Epidemiol. 1999; 34(8): 416–424. doi: 10.1007/s001270050163. PMID: 10501711. [DOI] [PubMed] [Google Scholar]
- 12.Alsamghan AS. Social anxiety symptoms and quality of life of secondary school students of Abha, Saudi Arabia. J Genet Psychol. 2021; 182(1): 18–30. [DOI] [PubMed] [Google Scholar]
- 13.Eapen V, Ghubash R, Salem MO, Sabri S. Familial predictors of childhood shyness: a study of the United Arab Emirates population. Public Health Genomics 2005; 8(1): 61–64. [DOI] [PubMed] [Google Scholar]
- 14.Okano K. Shame and social phobia: a transcultural viewpoint. Bull Menninger Clin. 1994; 58(3): 323–338. PMID 7920372. [PubMed] [Google Scholar]
- 15.Carvalho FR, Nóbrega CDR, Martins AT. Mapping gene expression in social anxiety reveals the main brain structures involved in this disorder. Behav Brain Res. 2020; 394: 112808. doi: 10.1016/j.bbr.2020.112808. Epub 2020 Jul 22. PMID: 32707139. [DOI] [PubMed] [Google Scholar]
- 16.Xu Y, Schneier F, Heimberg RGet al. et al. Gender differences in social anxiety disorder: results from the national epidemiologic sample on alcohol and related conditions. J Anxiety Disord. 2012; 26(1): 12–19. [DOI] [PubMed] [Google Scholar]
- 17.Caballo VE, Salazar IC, Irurtia MJ, Arias B, Hofmann SG, Ciso-A Research Team. Differences in social anxiety between men and women across 18 countries. Pers Individ Dif. 2014; 64: 35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahmed MAK, Alansari BM. Gender differences in anxiety among undergraduates from ten arab countries. Soc Behav Pers Int J. 2004; 32(7): 649–655. [Google Scholar]
- 19.Elhadad AA, Alzaala MA, Alghamdi RS, Asiri SA, Algarni AA, Elthabet MM. Social phobia among Saudi medical students. Middle East Current Psychiatry 2017; 24(2): 68–71. [Google Scholar]
- 20.Al-Hinai SS, Al-Saidy O, Dorvlo ASSet al. Culture and prevalence of social phobia in a college population in Oman. In: Landow MV, ed. College Students: Mental Health and Coping Strategies. Nova Science Publishers; 2006: 2–19. [Google Scholar]
- 21.Mohammadi MR, Salehi M, Khaleghi Aet al. Social anxiety disorder among children and adolescents: a nationwide survey of prevalence, socio-demographic characteristics, risk factors and co-morbidities. J Affect Disord. 2020; 263: 450–457. doi: 10.1016/j.jad.2019.12.015 [DOI] [PubMed] [Google Scholar]
- 22.Canino G, Shrout PE, Rubio-Stipec Met al. The DSMIV rates of child and adolescent disorders in Puerto Rico. Arch Gen Psychiatry. 2004; 61(1): 85–93. [DOI] [PubMed] [Google Scholar]
- 23.Nelson EC, Grant JD, Bucholz KKet al. et al. Social phobia in a population-based female adolescent twin sample: co-morbidity and associated suicide-related symptoms. Psychol Med. 2000; 30(4): 797–804. [DOI] [PubMed] [Google Scholar]
- 24.Zeytinoglu S, Neuman KJ, Degnan KAet al. Pathways from maternal shyness to adolescent social anxiety. J Child Psychol Psychiatry. 2021 Jun 28. doi: 10.1111/jcpp.13477. Epub ahead of print. PMID: 34184279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Solmi M, Radua J, Olivola Met al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. 2021 Jun 2. doi: 10.1038/s41380-021-01161-7. Epub ahead of print. PMID: 34079068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fox AS, Kalin NH. A translational neuroscience approach to understanding the development of social anxiety disorder and its pathophysiology. Am J Psychiatry. 2014; 171(11): 1162–1173. doi: 10.1176/appi.ajp.2014.14040449. PMID: 25157566; PMCID: PMC4342310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hart TA, Turk CL, Heimberg RG, Liebowitz MR. Relation of marital status to social phobia severity. Depress Anxiety. 1999; 10(1): 28–32. doi:. PMID: 10499187. [DOI] [PubMed] [Google Scholar]
- 28.Peen J, Schoevers RA, Beekman AT, Dekker J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr Scand. 2010; 121(2): 84–93. doi: 10.1111/j.1600-0447.2009.01438.x. Epub 2009 Jul 13. PMID: 19624573. [DOI] [PubMed] [Google Scholar]
- 29.Breslau J, Marshall GN, Pincus HA, Brown RA. Are mental disorders more common in urban than rural areas of the United States? J Psychiatr Res. 2014; 56: 50–55. doi: 10.1016/j.jpsychires.2014.05.004. Epub 2014 May 14. PMID: 24857610. [DOI] [PubMed] [Google Scholar]
- 30.Heimberg RG, Stein MB, Hiripi E, Kessler RC. Trends in the prevalence of social phobia in the United States: a synthetic cohort analysis of changes over four decades. Eur Psychiatry. 2000; 15(1): 29–37. doi: 10.1016/s0924-9338(00)00213-3. PMID: 10713800. [DOI] [PubMed] [Google Scholar]
- 31.Bruch MA, Fallon M, Heimberg RG. Social phobia and difficulties in occupational adjustment. J Couns Psychol. 2003; 50(1): 109. [Google Scholar]
- 32.Butterworth P, Gill SC, Rodgers B, Anstey KJ, Villamil E, Melzer D. Retirement and mental health: analysis of the Australian national survey of mental health and well-being. Soc Sci Med. 2006; 62(5): 1179–1191. doi: 10.1016/j.socscimed.2005.07.013. Epub 2005 Sep 19. PMID: 16171915. [DOI] [PubMed] [Google Scholar]
- 33.Al-Alawi M, Al-Sinawi H, Al-Adawi S, Jeyaseelan L, Murthi S. Public perception of mental illness in Oman: a cross sectional study. Int J Cult Ment Health. 2017; 10(4): 389–399. [Google Scholar]
- 34.Kumaraswamy PR, Quamar MM. Oman. In: Persian Gulf 2019. Palgrave Macmillan; 2020: 135–155. [Google Scholar]
- 35.Al Kindi M, Pickford M, Gommery D, Qatan A. Stratigraphy, palaeoclimatic context and fossils of the Southern Rub Al Khali (the empty quarter): results of a geo-archaeological survey around the area of maitan in the Sultanate of Oman. Hist Biol. 33; 9: 1534–1555. doi: 10.1080/08912963.2020.1717485 [DOI] [Google Scholar]
- 36.Alshekaili M, Hassan W, Al Said Net al. Factors associated with mental health outcomes across healthcare settings in Oman during COVID-19: frontline versus non-frontline healthcare workers. BMJ open. 2020; 10(10): e042030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liebowitz MR. Social phobia. Mod Probl Pharmacopsychiatry. 1987; 22: 141–173. doi: 10.1159/000414022. PMID: 2885745. [DOI] [PubMed] [Google Scholar]
- 38.Zubeidat I, Salinas JM, Sierra JC, Fernández-Parra A. Psychometric properties of the social interaction anxiety scale and separation criterion between Spanish youths with and without subtypes of social anxiety. J Anxiety Disord. 2007; 21(5): 603–624. doi: 10.1016/j.janxdis.2006.09.010. Epub 2006 Nov 3. PMID: 17084589. [DOI] [PubMed] [Google Scholar]
- 39.Terra MB, Barros HM, Stein ATet al. Internal consistency and factor structure of the Portuguese version of the liebowitz social anxiety scale among alcoholic patients. Braz J Psychiatry. 2006; 28(4): 265–269. PMID: 17242804. [PubMed] [Google Scholar]
- 40.Soykan C, Ozgüven HD, Gençöz T. Liebowitz social anxiety scale: the Turkish version. Psychol Rep. 2003; 93(3 Pt 2): 1059–1069. doi: 10.2466/pr0.2003.93.3f.1059. PMID: 14765570. [DOI] [PubMed] [Google Scholar]
- 41.Al-Sharbati M, Al-Adawi S, Petrini Ket al. Two-phase survey to determine social anxiety and gender differences in Omani adolescents. Asia Pac Psychiatry. 2012; 4(2): 131–139. doi: 10.1111/j.1758-5872.2012.00181.x. [DOI] [PubMed] [Google Scholar]
- 42.World Health Organization. Composite International Diagnostic Interview. WHO; 1993. [Google Scholar]
- 43.Ghazwani JY, Khalil SN, Ahmed RA. Social anxiety disorder in Saudi adolescent boys: prevalence, subtypes, and parenting style as a risk factor. J Family Community Med. 2016; 23(1): 25–31. doi: 10.4103/2230-8229.172226. PMID: 26929726; PMCID: PMC4745198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Taha AA, El-shereef EA, Abdullah TIM, Abdullah RIM, Aldahasi WAM. Social anxiety disorder and its correlates among female students at Taif University, Saudi Arabia. Res Psychol Behav Sci. 2017; 5(2): 50–56. [Google Scholar]
- 45.Joseph N, Rasheeka VP, Nayar V, Gupta P, Manjeswar MP, Mohandas A. Assessment of determinants and quality of life of university students with social phobias in a coastal city of south India. Asian J Psychiatr. 2018; 33: 30–37. doi: 10.1016/j.ajp.2018.02.008. Epub 2018 Feb 13. PMID: 29514122. [DOI] [PubMed] [Google Scholar]
- 46.Wu Y, Levis B, Ioannidis JPA, Benedetti A, Thombs BD; DEPRESsion Screening Data (DEPRESSD) Collaboration. Probability of Major depression classification based on the SCID, CIDI, and MINI diagnostic interviews: a synthesis of three individual participant data meta-analyses. Psychother Psychosom. 2021; 90(1): 28–40. doi: 10.1159/000509283. Epub 2020 Aug 19. PMID: 32814337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Takada K, Takahashi K, Hirao K. Measurement error in the liebowitz social anxiety scale: results from a general adult population in Japan. Int J Psychiatry Clin Pract. 2018; 22(4): 289–295. doi: 10.1080/13651501.2018.1426772. Epub 2018 Jan 17. PMID: 29338470. [DOI] [PubMed] [Google Scholar]
- 48.Hendaus MA, Alozeib R, Saied Let al. et al. Parenting style in a rapidly developing country: a report from the state of Qatar. J Family Med Prim Care. 2021; 10(8): 2947–2951. doi: 10.4103/jfmpc.jfmpc_1462_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Al-Saadoon M, Al-Adawi M, Al-Adawi S. Socio-cultural constraints in protecting child rights in a society in transition: a review and synthesis from Oman. Child Indic Res. 2020; 14(1): 1–29. doi: 10.1007/s12187-020-09759-z. Epub ahead of print. PMID: 32837628; PMCID: PMC7412292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Spokas M, Heimberg RG. Overprotective parenting, social anxiety, and external locus of control: cross-sectional and longitudinal relationships. Cognit Ther Res. 2009; 33(6): 543–551. [Google Scholar]
- 51.Swee MB, Hudson CC, Heimberg RG. Examining the relationship between shame and social anxiety disorder: a systematic review. Clin Psychol Rev. 2021; 90: 102088. doi: 10.1016/j.cpr.2021.102088. Epub 2021 Sep 22. PMID: 34598054. [DOI] [PubMed] [Google Scholar]
- 52.Zhu J, Fu R, Li Y, Wu M, Yang T. Shyness and adjustment in early childhood in Southeast China: the moderating role of conflict resolution skills. Front Psychol. 2021; 12: 644652. doi: 10.3389/fpsyg.2021.644652. PMID: 33868117; PMCID: PMC804766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lan X, Wang W. To be Shy or avoidant? Exploring the longitudinal association between attachment and depressive symptoms among left-behind adolescents in rural China. Pers Individ Dif. 2020; 155: 109634. doi: 10.1016/j.paid.2019.109634 [DOI] [Google Scholar]
- 54.Ingram RE, Luxton DD. Vulnerability-Stress models. In Hankin BL, Abela JRZ, eds. Development of Psychopathology: A Vulnerability Stress Perspective. Sage Publications Inc; 2005: 32–46. [Google Scholar]
- 55.Rapee RM, Spence SH. The etiology of social phobia: empirical evidence and an initial model. Clin Psychol Rev. 2004; 24(7): 737–767. doi: 10.1016/j.cpr.2004.06.004. PMID: 15501555. [DOI] [PubMed] [Google Scholar]
- 56.Cain S. Quiet: The Power of Introverts in a World That Can’t Stop Talking. Broadway Books; 2013. [Google Scholar]
- 57.Ranta K, La Greca AM, Kaltiala-Heino R, Marttunen M. Social phobia and educational and interpersonal impairments in adolescence: a prospective study. Child Psychiatry Hum Dev. 2016; 47(4): 665–677. doi: 10.1007/s10578-015-0600-9. PMID: 26514560. [DOI] [PubMed] [Google Scholar]
- 58.Kessler RC. The impairments caused by social phobia in the general population: implications for intervention. Acta Psychiatr Scand Suppl. 2003; 417: 19–27. doi: 10.1034/j.1600-0447.108.s417.2.x. PMID: 12950433. [DOI] [PubMed] [Google Scholar]
- 59.Asher M, Asnaani A, Aderka IM. Gender differences in social anxiety disorder: a review. Clin Psychol Rev. 2017; 56: 1–12. doi: 10.1016/j.cpr.2017.05.004. Epub 2017 May 30. PMID: 28578248. [DOI] [PubMed] [Google Scholar]
- 60.Abdel-Khalek AM. The Kuwait University anxiety scale: psychometric properties. Psychol Rep. 2000; 87(2): 478–492. doi: 10.2466/pr0.2000.87.2.478. PMID: 11086592. [DOI] [PubMed] [Google Scholar]
- 61.Chaleby KS, Raslan A. Delineation of social phobia in Saudia Arabians. Soc Psychiatry Psychiatr Epidemiol. 1990; 25(6): 324–327. doi: 10.1007/BF00782888. PMID: 2291136. [DOI] [PubMed] [Google Scholar]
- 62.Mohamed NA, Abdulhadi NN, Al-Maniri AA, Al-Lawati NR, Al-Qasmi AM. The trend of feminization of doctors’ workforce in Oman: is it a phenomenon that could rouse the health system? Hum Resour Health. 2018; 16(1): 19. doi: 10.1186/s12960-018-0283-y. PMID: 29699562; PMCID: PMC5921264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shaw CM, Creed F, Tomenson B, Riste L, Cruickshank JK. Prevalence of anxiety and depressive illness and help seeking behaviour in African caribbeans and white europeans: two phase general population survey. Br Med J. 1999; 318(7179): 302–305. doi: 10.1136/bmj.318.7179.302. PMID: 9924059; PMCID: PMC27715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ng LC, Solomon JS, Ameresekere M, Bass J, Henderson DC, Chakravarty S. Development of the South Sudan mental health assessment scale. Transcult Psychiatry. 2021: 13634615211059711. doi: 10.1177/13634615211059711. Epub ahead of print. PMID: 34898333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Alfalahi M, Mahadevan S, Balushi RAet al. et al. Prevalence of eating disorders and disordered eating in Western Asia: a systematic review and meta-analysis. Eat Disord. 2021: 1–30. doi: 10.1080/10640266.2021.1969495. Epub ahead of print. PMID: 34486495. [DOI] [PubMed] [Google Scholar]
- 66.Lydiard RB. Social anxiety disorder: comorbidity and its implications. J Clin Psychiatry. 2001; 62(Suppl 1): 17–24. [PubMed] [Google Scholar]