Abstract
Background
The prevalence of obesity is rising, and obese persons are more likely to use healthcare services and require moving and handling care.
Aims
This study explored the frequency, logistics and barriers to the provision of bariatric patient-handling care including equipment availability in acute hospitals.
Methods
A cross-sectional study design using an anonymous 24-item questionnaire was used to survey 322 clinical nurse managers. Completed hard-copy questionnaires (n = 132) were returned by post.
Results
Most clinical nurse managers (93.1%) provided care for bariatric patients and 85.6% reported barriers to the provision of bariatric care within their clinical area. The principal barriers were lack of equipment (75%), staff (65.2%) and training (57.6%). Only 11.4% owned all the required equipment. Owning equipment provided significantly greater access to a hoist (P = 0.001) and chair (P = 0.032) than renting. Only 9.5% reported that rented equipment always arrives on time. The majority (74.4%) did not have guidelines for caring for bariatric patients, and 46.2% considered this to be a barrier.
Conclusions
Barriers to caring for bariatric patients were identified. Most of the equipment was rented, and significant delays in its delivery were reported. The need for education and training and the dissemination of policies and guidelines were identified.
Keywords: bariatric, barriers, equipment, moving and handling, nurses, obesity
Introduction
The global prevalence of obesity is increasing with worldwide obesity levels almost tripled since 1975 (Di Cesare et al., 2016; World Health Organization, 2018). In keeping with this trend, the proportion of the Irish population who are overweight or obese has increased from 50% in 2008 (Morgan et al., 2008) to 62% in 2017 (Central Statistics Office, 2017). Furthermore, the prevalence of overweight and obesity in Ireland is projected to continue to increase for men and women by 2030 to 89% and 85%, respectively (Keaver et al., 2013). It has also been projected that Ireland will have the highest prevalence of obesity out of 44 European countries by 2025 (Pineda et al., 2018).
Bariatrics is the medical field encompassing the management of patients who are clinically obese. Persons who are obese are more likely to use healthcare services (Dee et al., 2014; Doherty et al., 2012), be admitted to hospital (Musich et al., 2016) and are more likely to be in the intensive care unit (ICU) than those who have a normal weight (Galinsky et al., 2010). Obesity has a detrimental effect on almost all physiological systems (Ortiz and Kwo, 2015), and consequently obese patients’ care needs are many and complex. This also relates to the moving and handling of bariatric patients, in which due to their increased susceptibility to tissue damage or pressure ulcers (Rush and Muir, 2012), they require frequent repositioning in bed (Galinsky et al., 2010) in addition to assistance with general mobility.
The changing patient demographic requires the healthcare sector to regularly review and proactively adapt its approach to providing healthcare. Nursing staff are consistently at the interface of a patient’s hospital admission and subsequent care. Moving and handling of bariatric patients is associated with a higher prevalence of injury among nurses and nursing assistants (Choi and Brings, 2016; Randall et al., 2009) but their safety and the safety and dignity of the patients must be ensured (Gillespie and Lane, 2018). Barriers to safe, dignified moving and handling care have been identified (Booth et al., 2011; Hignett and Griffiths, 2009; McMillan et al., 2018).
Much of the published literature on moving and handling of bariatric patients is narrative and based on expert opinion, and there are limited quantitative data to support evidence-based practice in the area. To date little is known about the proportion of bariatric patients in hospitals or the strategies used to provide, now or in the future, for this population’s specific needs and requirements within the hospital setting. Given the rising prevalence of obesity and projected corresponding hospital admissions there is a need for an evidence-based care strategy. The aim of this study was to explore the provision of moving and handling care for bariatric patients in acute Irish hospital settings. The objectives were to explore: (a) the frequency of nursing staff caring for bariatric patients; (b) the process for obtaining a bariatric patient’s weight; (c) the availability/accessibility of bariatric equipment; (d) the governance and ownership status of bariatric equipment; (e) the perceived bariatric moving and handling training needs of nursing staff.
Method
A multicentre cross-sectional study design was used to conduct an anonymous questionnaire survey of clinical nurse managers (CNMs) working in acute hospital settings.
Participants
CNMs were chosen as participants in the study as they traditionally play a central decision-making role in the formulation and coordination of individualised patient care including the procurement and allocation of resources, including equipment. Furthermore, CNMs are considered skilled clinicians and are central to the team dynamics of providing patient care in the acute hospital setting. Purposive sampling was applied to identify hospitals with varied geographical locations and sizes for inclusion in the study. All CNMs working in the participating hospitals were eligible for inclusion, except for those working in paediatrics, health promotion or education. CNMs who were on leave at the time of the survey were not included.
Measures
A 24-item questionnaire, based on previous literature (Bulat, 2015; Cowley and Leggett, 2010; Hignett et al., 2007) was developed by the researchers. Experienced clinicians were also involved in the development of the questionnaire in order to strengthen the content validity. The questionnaire comprised 21 closed and three open questions related to six dimensions; (a) care of bariatric patients (three items); (b) ownership and accessibility of bariatric equipment (five items); (c) awareness of policies and guidelines to guide practice (seven items); (d) barriers to the provision of bariatric care (three items); (e) staff education and training (three items); and (f) demographic information (three items). Excluding the demographic questions, closed questions were 4- or 5-point likert scales (n = 7), dichotomous ‘yes/no’ items (n = 6) or multiple response items (n = 5). For example, one multiple response question was: ‘What are the barriers to providing bariatric care within your clinical area?’ and the possible responses were: there are no barriers; lack of guidelines or policies; lack of training; lack of resources/equipment; lack of resources/staff; lack of clinical support; lack of management support; other.
There is no universal definition of the term ‘bariatric’ but it is frequently based on body mass index (BMI), bodyweight, and/or weight-related limitations (Cowley and Leggett, 2011; Galinsky et al., 2010; World Health Organization, 2018). For the purposes of this study, a patient was classified as ‘bariatric’ if their BMI was above 35 kg/m2, or their weight exceeded 159 kg (Health Service Executive, 2012). A pilot study on a convenience sample of 10 CNMs not involved with the study was conducted to test feasibility, face validity and to establish the likely time for completion of the questionnaire. Minor amendments were made based on the feedback and it was established that it would take approximately 10 minutes to complete the questionnaire.
Procedure
The director of nursing in each participating hospital was contacted for permission to distribute the questionnaires, confirmation of the number and locations of the CNMs in their hospital and the nomination of a gatekeeper. The gatekeeper sent an email to potential participants inviting them to participate in the study and to provide them with the participant information leaflet as an attachment. Hardcopy questionnaires were subsequently distributed to the CNMs in their workplace, as the response rate has been shown to be higher with paper questionnaires compared to online surveys (Cho et al., 2013). The CNMs were requested to complete the anonymous questionnaire and return it in the self-addressed envelope to the designated collection point(s) in their hospital. One week later, the gatekeeper sent a combined thank you and reminder email to all the potential participants. The CNMs were reminded that they were under no obligation to participate in the study. Return of the completed questionnaire was considered as consent. Ethics approval for the study was given by the university and the relevant Health Service Executive regions.
Descriptive analysis of frequencies and percentages was performed, and associations were tested using Pearson’s chi-square test. The statistical analysis was conducted using the statistical package for the social sciences (SPSS v. 25; IBM Corp, 2017). Statistical significance at P < 0.05 was assumed.
Results
All hospitals that were approached (n = 7) were included in the study, and 132 out of 322 CNMs participated in the study, giving a response rate of 41%. The majority of CNMs (83.2%) had worked in the current clinical area for more than 3 years. There was wide representation of the clinical areas in which they worked, with the highest proportions working in general medicine (30.3%), ICU/high dependency unit (HDU) (12.1%) and general surgical (11.4%) wards.
Provision of bariatric care
The majority (93.1%) of CNMs provided care for bariatric patients, with 49.2% stating that they provided care for up to three bariatric patients in the past month. The majority (90.6%) reported that the patient’s weight should be measured within 24 hours of admission/arrival, but only 19.7% stated that this ‘always’ happened and a further 45.6% reported that it ‘frequently’ happened within the time frame. Only 51.5% always know the current weight of the bariatric patients in their care. A staff nurse (97.7%), healthcare assistant (46.2%) or dietitian (18.2%) were most frequently reported as the person responsible for weighing the patient.
Barriers to moving and handling care
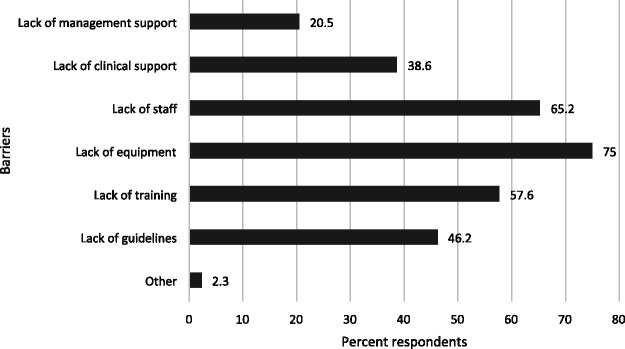
The majority (85.6%) of CNMs stated that there were barriers to the provision of bariatric care within their clinical area. The principal barriers were lack of equipment (75%), lack of staff (65.2%) and lack of training (57.6%), as shown in Figure 1.
Figure 1.
Reported barriers to providing moving and handling care.
Note: As this was a multiple-response item in the questionnaire, participants could choose more than one response.
Accessibility and ownership of bariatric equipment
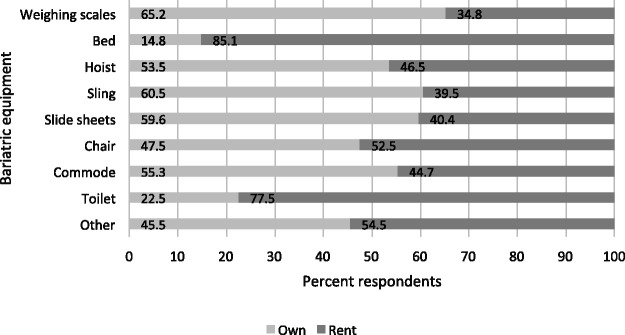
Forty-one per cent reported that they ‘always’ or ‘usually’ have access to bariatric equipment, and the remaining 59% reported that they sometimes (33.9%), seldom (15.7%) or never (9.4%) have access to bariatric equipment. Bariatric beds were available to the greatest proportion of CNMs (62.8%) and a bariatric toilet was available to the least (16.3%), as shown in Figure 2.
Figure 2.
The availability of specific types of bariatric equipment to the participants.
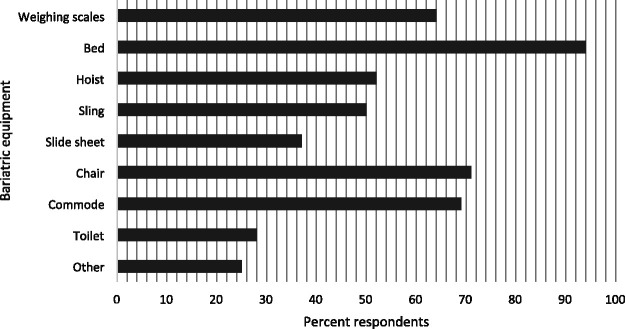
The CNMs were asked if they owned or rented the bariatric equipment they use. Only 11.4% owned all the required equipment and the remaining respondents rented some (79.6%) or all (9%) of the equipment. The ownership status of specific equipment is presented in Figure 3. There was an association between ownership and accessibility, as a Pearson’s chi-square test indicated that those who owned their equipment had significantly greater access to a hoist (χ2 = 10.55, n = 69, df = 1, P = 0.001) and a chair (χ2 = 4.62, n = 77, df = 1, P = 0.032). They also had greater access to scales (χ2 = 2.59, n = 64, df = 1, P = 0.108), a bed (χ2 = 1.87, n = 98, df = 1, P = 0.172) and slide sheets (χ2 = 2.37, n = 51, df = 1, P = 0.124) than those who rented, although the association did not reach statistical significance.
Figure 3.
Ownership status of specific types of bariatric equipment as reported by the participants.
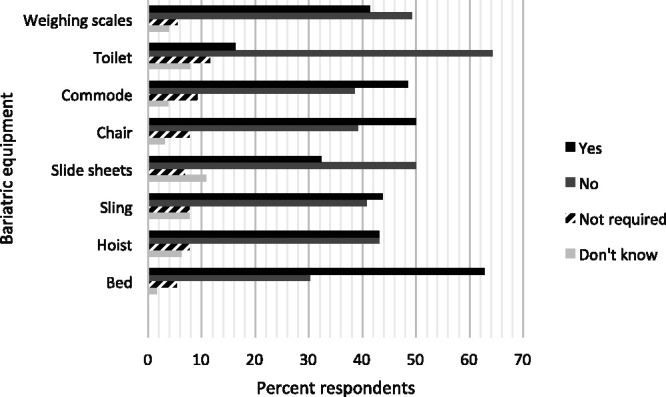
The punctuality of rented equipment deliveries was investigated, and only 9.5% of CNMs reported that rented equipment ‘always’ arrives in a timely manner. Less than half (49.5%) stated that rented equipment ‘usually’ arrives in a timely manner, and a further 32.4%, 5.7% and 2.9% stated that it arrives in a timely manner ‘sometimes’, ‘seldom’ or ‘never’, respectively. Figure 4 presents the frequency of delays for bariatric equipment that was ‘sometimes’, ‘seldom’ and ‘never’ delivered in a timely manner.
Figure 4.
Reported frequency of delays in the delivery of specific types of rented bariatric equipment.
Protocols and guidelines
CNMs were most frequently reported as responsible for ordering bariatric equipment (88.5%), while 32.3% and 27.7% stated that the assistant directors of nursing or staff nurses, respectively, were also responsible. Only 39.7% reported that there was a clear system for ordering bariatric equipment. Those who had a clear system of ordering bariatric equipment reported that it arrived on time more frequently than those who did not (57.7% vs. 41.8%), but the association was not statistically significant (χ2 = 2.96, n = 119, df = 1, P = 0.085).
The majority (74.4%) stated that they did not have guidelines to inform their practice when caring for bariatric patients, although only 46.2% considered it to be a barrier (Figure 1). A greater proportion of less experienced CNMs; that is with 3 years or less in the clinical area (40.9%) than more experienced CNMs (21.7%) had guidelines to inform their practice, but the difference was not significant (χ2 = 3.59, n = 128, df = 1, P = 0.058). Only 11.5% had undertaken education or training in the management of the bariatric patient and 93.2% stated that they would like additional education or training.
Discussion
This study set out to investigate the provision of moving and handling care for bariatric patients in acute hospital settings. Nursing staff are at the interface of patient handling care and were therefore included as participants in this first study. Their inclusion was justified as almost all the respondents had cared for bariatric patients.
Lack of equipment was reported to be the main barrier to providing bariatric moving and handling care, with continuous availability of all required equipment reported by less than 15% of the respondents. Inadequate bariatric equipment has also been reported to be a barrier to providing care for patients in an acute care setting (Drake et al., 2005) and in varied practice settings (Drake et al., 2008), in primary healthcare (Cowley and Leggett, 2011), in emergency departments (Geary and Collins, 2012), and across a regional health board (Murray, 2012). In studies in which the clinical setting or site was a variable, it was reported that specialised bariatric equipment was more readily available in hospitals compared to the community setting (Drake et al., 2008; Rose et al., 2008). The current study was undertaken in the hospital setting only, but if the pattern of availability of specialised bariatric equipment is similar in the current study to others there could be an even greater cause for concern for nurses working in the community.
Establishing the patient’s weight is a fundamental component of a moving and handling risk assessment in order to determine the level of assistance required and the need for equipment. With this in mind, the safe working load of the available moving and handling equipment must be known (Health Service Executive, 2018). However, this will only be relevant if the patient’s weight is known. The majority of CNMs stated that the patient’s weight should be measured within 24 hours of admission/arrival; however, less than half had weighing scales available to them. This is significantly fewer than reported in a state-wide survey by Gardner (2013), but greater than the availability in emergency departments (Geary and Collins, 2012). The lack of such basic equipment prevents a comprehensive risk assessment being performed and may contribute to delays in the commencement of the optimum treatment of the patient.
The frequency of moving and handling care of bariatric patients by nurses was explored in this study, but the proportion of patients who have bariatric requirements is yet unknown. Insufficient staffing levels were reported to be a barrier to providing care, similar to the findings of Drake et al. (2005), Drake et al. (2008) and Gardner (2013). Furthermore, Drake et al. (2008) concluded that adequate staffing levels were also related to the satisfaction of nurses working with bariatric patients in outpatients. This issue has also been raised in the past as narrative debate and opinion (Gallagher, 2012; Gallagher et al., 2014). The current survey examined factors related to bariatric patient handling care at an exploratory level. Limited information was gathered regarding the specifics of inadequate staffing, but the findings highlight the necessity of further investigation, potentially including participants at a corporate or management level. Further research is required to quantify the frequency and pattern of bariatric patient hospital admissions so that sufficient numbers of well-informed staff are employed.
Most of the bariatric equipment used by the respondents was rented. This is possibly due to the short-term cost implications whereby renting is more affordable than buying, or due to insufficient storage facilities (Rose et al., 2008). Similar to Gardner (2013), many hospitals both rent and own bariatric equipment. From a work practice point of view, it may not be important if the equipment is rented or owned, provided it is available for use when required. In this study, the respondents had better access to equipment when it was owned compared to when it was rented, although few owned all their required equipment. The CMNs were asked about the promptness of rented equipment deliveries, and they reported that there were significant delays in the delivery of rented equipment. Bariatric beds were most likely to be rented but a very low proportion of CNMs reported that the equipment was always delivered in a timely manner. The length of time required to secure rented equipment was also highlighted by Gardner (2013). Any delays in the procurement of specialised equipment have negative implications for the safety of staff and for the safety and dignity of the patient. Therefore, this is an issue that requires further investigation and more importantly the development of a system that provides a solution. Furthermore, most respondents reported that CNMs were responsible for ordering bariatric equipment. Despite this, almost two-thirds of them reported not having a clear system for ordering bariatric equipment and this may have contributed to the delays.
Only one quarter of the respondents reported having guidelines to inform their practice when caring for bariatric patients. Similarly in other studies, it has been stated that institutions did not have guidelines to inform their practice when caring for bariatric patients (Hignett and Griffiths, 2009a), or that policies and protocols for bariatric patients were absent (Rose et al., 2008), insufficient or not adhered to (Gardner, 2013). In a general healthcare setting, knowledge of workplace guidelines and the presence of specific protocols for using lifting devices have been shown to have the greatest influence on nurses’ behaviour in relation to the use of the devices (Koppelaar et al., 2013). Those findings could possibly also apply to a bariatric setting.
In the current study, the absence of guidelines was not always considered to be a barrier to providing bariatric care. Other factors such as lack of equipment, staff and training were more frequently considered to be barriers than the lack of guidelines. Recent guidance on manual handling for bariatric patients has been produced (Health Service Executive, 2018). However, to date the guidelines do not appear to have been disseminated among staff. In this study, the more experienced CNMs were less likely to have guidelines to inform their practice than their less experienced colleagues. This is a disappointing finding for two reasons. Firstly, for their own safety and that of their patients, and secondly because the more experienced staff may have a leadership and mentoring role for younger staff. This also has implications for targeted future strategies aimed at informing CNMs and other medical personnel about bariatric patient management. The low level of clinical education in bariatric moving and handling reported by the CNMs in this study is a further issue that needs to be addressed. A positive finding is that most respondents expressed an interest in training in this area.
Limitations
The low response rate of the questionnaire survey is a limitation, although similar to Murray (2012) and considerably higher than Hignett and Griffiths (2009b). Every effort was made to obtain a high response rate, such as a guarantee of anonymity (Jobber and O’Reilly, 1998), pre-paid mail survey (Cho et al., 2013; Jobber and O’Reilly, 1998) and follow-up (Cho et al., 2013). Circumstances beyond the control of the researchers (snowstorms and industrial action) occurred at the time of survey distributions and were likely to have influenced the response rate. The small number of hospitals (n = 7) included in the study is a further limitation, but a purposive sampling method was used that included mostly teaching hospitals. Given the emphasis on good practice in teaching hospitals, the results may in fact represent an overestimation of the situation nationally. It is also possible that selection bias affected the response rate, as nurses who did not care for bariatric patients may have been less likely to complete the questionnaire.
Conclusions
Nursing staff worldwide are consistently at the interface of patient handling care and are regularly caring for bariatric patients. Barriers to caring for bariatric patients were identified in this study and are similar to those identified by others previously. The emphasis was placed on factors that are readily amenable to change at a clinical level, including the logistics of providing patient handling care, the availability of equipment and basic staff training. The limited access to bariatric equipment, lack of staff and the dearth of clinical education are of concern. Most of the equipment was rented, but significant delays in the delivery of rented equipment were reported. The need for education and training and the dissemination of policies and guidelines were identified. Such policies and pathways have the potential to enhance and optimise patient handling care for persons with obesity and facilitate favourable healthcare outcomes for this cohort. The enthusiasm for specific bariatric training and guidelines is a positive finding that can be acted on by those involved in moving and handling in an advisory or educational capacity.
Future research should include surveys of the service users and healthcare professionals, in order to contribute to evidence-based strategic planning for the optimum care of bariatric patients in the hospital setting.
Key points for policy, practice and/or research
Barriers to caring for bariatric patients were identified in this study.
Most of the equipment was rented, and significant delays in its delivery were reported.
The need for education and training and the dissemination of policies and guidelines were identified.
Acknowledgements
The author(s) would like to thank the clinical nurse managers who participated in the study, the gatekeepers who contacted potential participants, the directors of nursing who facilitated the study and the research assistants who were involved in the distribution and collection of questionnaires.
Biography
Sara Dockrell is an Assistant Professor in the discipline of Physiotherapy, Trinity College Dublin and a chartered physiotherapist. Her research interests include moving and handling of patients, with particular focus on the provision of safe and dignified moving and handling for bariatric patients in healthcare.
Graham Hurley is a chartered Physiotherapist and moving and handling training co-ordinator, Centre for Learning and Development, St James’s Hospital. His research and practice focus on moving and handling in the healthcare sector.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics: The study was approved by the School of Medicine, Trinity College Dublin (app. no. 20170910); Nursing Research Access Committee, and the Health Service Executive (HSE South East; HSE North East; and HSE North West).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Sara Dockrell https://orcid.org/0000-0002-5838-7805
References
- Booth CMA, Moore CE, Eddleston J, et al. (2011) Patient safety incidents associated with obesity: A review of reports to the National Patient Safety Agency and recommendations for hospital practice. Postgraduate Medical Journal 87: 694–699. [DOI] [PubMed] [Google Scholar]
- Bulat T (2015) Bariatric Toolkit. Available at: https://www.pdffiller.com/jsfiller-desk15/?projectId=324906482&expId=5355&expBranch=1#8d4277af53929c7614dcb27d97c1bcea (accessed 7 June 2017).
- Central Statistics Office (2017) The Wellbeing of the Nation 2017. Available at: https://www.cso.ie/en/releasesandpublications/ep/p-wbn/thewellbeingofthenation2017/hlt/ (accessed 20 June 2019).
- Cho YI, Jojnson TP, Vangeest JB. (2013) Enhancing surveys of health care professionals: a meta-analysis of techniques to improve response. Evaluation and the Health Professions 36: 382–407. [DOI] [PubMed] [Google Scholar]
- Choi SD, Brings K. (2016) Work-related musculoskeletal risks associated with nurses and nursing assistants handling overweight and obese patients: a literature review. Work: A Journal of Prevention Assessment & Rehabilitation 53: 439–448. [DOI] [PubMed] [Google Scholar]
- Cowley SP, Leggett S. (2010) Manual handling risks associated with the care, treatment and transportation of bariatric patients and clients in Australia. International Journal of Nursing Practice 16: 262–267. [DOI] [PubMed] [Google Scholar]
- Cowley SP, Leggett S. (2011) Manual handling risks associated with the care, treatment and transportation of bariatric (severely obese) clients in Australia. Work: A Journal of Prevention Assessment & Rehabilitation 39: 477–483. [DOI] [PubMed] [Google Scholar]
- Dee A, Kearns K, O’Neill C, et al. (2014) The direct and indirect costs of both overweight and obesity: a systematic review. BMC Research Notes 7: 242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Cesare M, Bentham J, Stevens GA, et al. (2016) Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 387: 1377–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doherty E, Dee A, O’Neill C. (2012) Estimating the amount of overweight and obesity related health-care use in the Republic of Ireland using SLAN data. Economic and Social Review 43: 227–250. [Google Scholar]
- Drake D, Baker G, Engelke MK, et al. (2008) Challenges in caring for the morbidly obese: differences by practice setting. Southern Online Journal of Nursing Research 8: 1–13. [Google Scholar]
- Drake D, Dutton K, Engelke M, et al. (2005) Challenges that nurses face in caring for morbidly obese patients in the acute care setting. Surgery for Obesity and Related Diseases 1: 462–466. [DOI] [PubMed] [Google Scholar]
- Galinsky T, Hudock S, Streit J. (2010) Addressing the need for research on bariatric patient handling. Rehabilitation Nursing 35: 242–247. [DOI] [PubMed] [Google Scholar]
- Gallagher S. (2012) Safety, the nursing shortage and the bariatric nurse: is this an ethical debate? Bariatric Nursing and Surgical Patient Care 7: 10–12. [Google Scholar]
- Gallagher S, Hilton T, Monaghan H, et al. (2014) Safe patient handling and movement: bariatric considerations. American Journal of Safe Patient Handling and Movement June: 1–16. [Google Scholar]
- Gardner LA. (2013) Caring for class III obese patients. American Journal of Nursing 113: 66–70. [DOI] [PubMed] [Google Scholar]
- Geary B, Collins N. (2012) Are we prepared for a growing population? Morbid obesity and its implications in Irish emergency departments. European Journal of Emergency Medicine 19: 117–120. [DOI] [PubMed] [Google Scholar]
- Gillespie T, Lane S. (2018) Moving the bariatric patient. Critical Care Nursing Quarterly 41: 297–301. [DOI] [PubMed] [Google Scholar]
- Health Service Executive (2012) Manual handling and people handling policy, Dublin: Health Service Executive. [Google Scholar]
- Health Service Executive (2018) Managing the manual handling issues of service users with bariatric needs. Available at: http://13.94.105.41/eng/staff/safetywellbeing/healthsafetyand%20wellbeing/bariatric%20guidelines%20re%20manual%20handling%20issues.pdf (accessed 20 June 2019).
- Hignett S, Griffiths P. (2009. a) Manual handling risks in the bariatric (obese) patient pathway in acute sector, community and ambulance care and treatment. Work: A Journal of Prevention Assessment & Rehabilitation 33: 175–180. [DOI] [PubMed] [Google Scholar]
- Hignett S, Griffiths P. (2009. b) Risk factors for moving and handling bariatric patients. Nursing Standard (Royal College of Nursing (Great Britain) 24: 40–48. [DOI] [PubMed] [Google Scholar]
- Hignett S, Chipchase S, Tetley A, et al. (2007) Risk assessment and process planning for bariatric patient handling pathways. Available at: http://www.hse.gov.uk/research/rrpdf/rr573.pdf (accessed 26 June 2019).
- IBM Corp (2017) IBM Statistical Package for the Social Sciences (SPSS) for Windows, New York: Armonk. [Google Scholar]
- Jobber D, O’Reilly D. (1998) Industrial mail surveys – a methodological update. Industrial Marketing Management 27: 95–107. [Google Scholar]
- Keaver L, Webber L, Dee A, et al. (2013) Application of the UK foresight obesity model in Ireland: the health and economic consequences of projected obesity trends in Ireland. PLoS One 8: e79827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koppelaar E, Knibbe JJ, Miedema HS, et al. (2013) The influence of individual and organisational factors on nurses’ behaviour to use lifting devices in healthcare. Applied Ergonomics 44: 532–537. [DOI] [PubMed] [Google Scholar]
- McMillan J, Moo A, Newnam S, et al. (2018) Improvements in patient handling for worker and patient safety. Available at: https://research.iscrr.com.au/__data/assets/pdf_file/0004/1321771/Environmental-Scan_Improvements-in-patient-handling-for-worker-and-patient-safety.pdf (accessed 28 June 2019).
- Morgan K, McGee H, Watson D, et al. (2008) Slan 2007: Survey of lifestyle, attitudes and nutrition in Ireland: Main report, Dublin: Department of Health and Children; Available at: http://epubs.rcsi.ie/psycholrep/3/ (accessed 8 March 2019). [Google Scholar]
- Murray A. (2012) Managing people with severe and complex obesity in health care. Equipment Services April: 30–34. [Google Scholar]
- Musich S, MacLeod S, Bhattarai GR, et al. (2016) The impact of obesity on health care utilization and expenditures in a Medicare supplement population. Gerontology and Geriatric Medicine 2: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz VE, Kwo J. (2015) Obesity: physiologic changes and implications for preoperative management. BMC Anesthesiology 15: 97.DOI: 10.1186/s12871-015-0079-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pineda E, Sanchez-Romero LM, Brown M, et al. (2018) Forecasting future trends in obesity across Europe: the value of improving surveillance. Obesity Facts 11: 360–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randall SB, Pories WJ, Pearson A, et al. (2009) Expanded occupational safety and health administration 300 log as metric for bariatric patient-handling staff injuries. Surgery for Obesity and Related Diseases 5: 463–468. [DOI] [PubMed] [Google Scholar]
- Rose MA, Drake DJ, Baker G, et al. (2008) Caring for morbidly obese patients: safety considerations for nurse administrators. Nursing Management 39: 47–50. [DOI] [PubMed] [Google Scholar]
- Rush A, Muir M. (2012) Maintaining skin integrity bariatric patients. British Journal of Community Nursing 17: 156–159. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2018) Obesity and overweight: Key facts. Available at: http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed 1 June 2019).