Abstract
Co-infection refers to the simultaneous infection of a host by multiple pathogenic organisms. Experimental co-infection studies using a mutant and its isogenic wild type have proven to be profoundly sensitive to analysis of pathogen factor mutation-associated fitness effects in in vivo models of infectious disease. Here we discuss the use of such co-infection experiments in studying the interaction between Yersinia pestis and its flea vector to more sensitively determine the critical bacterial determinants for Y. pestis survival, adaptation, and transmission from fleas. This chapter comprises two main sections, the first detailing how to infect fleas with mutant and wild type Y. pestis strains, and secondly how to process infected fleas and specifically quantify distinct Y. pestis strain burdens per flea. The Y. pestis competitive fitness co-infection model in fleas is insightful in evaluating the consequence of a mutation which may not be obvious in single-strain flea infections where there is less selective pressure.
Keywords: Yersinia pestis, Co-infection, Competitive fitness, Transmission factors, Flea infection
1. Introduction
Yersinia pestis, the etiological agent of plague, is transmitted to a mammalian host by the bite of a flea. Fleas initially acquire Y. pestis from an infected host through blood feeding. Within the flea digestive tract, Y. pestis preferentially colonizes the foregut proventriculus and/or midgut [1–3]. A short extrinsic incubation period follows acquisition during which Y. pestis adapts to the flea gut physiochemical environment and multiplies to develop into a dense cohesive biofilm in the flea digestive tract. During this process the foregut proventriculus, the valvular organ that pumps the blood meal into the midgut, can become efficiently blocked by biofilm thereby impeding its normal function. It is at this point that the flea is primed for a biofilm-mediated blockage regurgitative transmission event at the next blood feeding. This is the classical biological mechanism of transmission of Y. pestis from fleas [2, 3]. Traditionally, to determine the role a particular bacterial-encoded factor plays in formation of a transmissible infection in fleas, a single infection of fleas with either mutant or wild type bacteria is employed. The dynamics of single infection, such as rate of biofilm gut blockage formation, rate of flea infection, and bacterial burden per flea [4–6] are then compared between the mutant and wild type infections. These studies are extremely useful for the identification of major transmission factors with respect to the biofilm-mediated regurgitation blockage phenotype. Yet such single strain infections of mutants in key transmission factors have rarely, if ever, simultaneously revealed any survival defects associated with the mutation [4–6]. However, the recent use of Y. pestis co-infection experiments in fleas that utilize a mutant competed against an isogenic wild type strain revealed that several mutants exhibiting no survival defects during single-strain infection [6–8] incurred significant fitness defects during competitive co-infection with a wild type strain [7–10]. This illuminated that compensatory effects, in some instances, may mask identification of the true impacts of a specific Y. pestis factor on flea gut infection. Henceforth, flea co-infection studies have been established as a powerful and sensitive means for assessing if a mutant incurs fitness costs or benefits when competing for resources in the flea digestive tract.
In general, the enhanced sensitivity of competitive co-infection models is advantageous in the understanding of subtle, temporally modulated, and host immune system influenced factors that contribute to a pathogen’s ability to infect a host. In fleas, Y. pestis co-infection experiments may represent a realistic experimental infection model for naturally infected wild fleas at plague foci, given that once Y. pestis is ingested it is thought to compete against the flea’s natural microbiota to gain advantage [11]. Fleas reared and maintained under controlled laboratory conditions may not exhibit the same diversity of microbiota as wild fleas, limiting detection of an atypical fitness phenotype in a single-strain infection model [11].
The general strategy of Y. pestis co-infection of fleas is to infect a large cohort of fleas with a 1:1 mixture of a mutant and its isogenic wild type and calculate the ratio of the co-infected strains per flea over time. The strains need to be differentiated by a selection marker. Any selection marker can be used for one of the strains as long as it is verified that this marker does not confer any fitness effect to the strain. In this chapter, we use antibiotic resistance to selectively distinguish between two co-infecting strains. The fleas are fed a blood meal with an equally proportioned mixture of co-infecting strains. The total bacterial load must contain the minimum infectious dose for colonization and maintenance of a persistent infection of the digestive tract of the Xenopyslla cheopis flea species, which is 5 × 108 to 1 × 109 CFU/mL [12]. Fleas are collected immediately after infected blood meal acquisition and at different time points post-infection. The contents of a single co-infected flea are duplicate plated on rich media generally selective for Y. pestis with and without antibiotic selection, allowing enumeration of the antibiotic resistant strain alone, and total Y. pestis per flea respectively. The percentage of each strain in the flea gut can subsequently be determined from fleas collected at different time points post-infection.
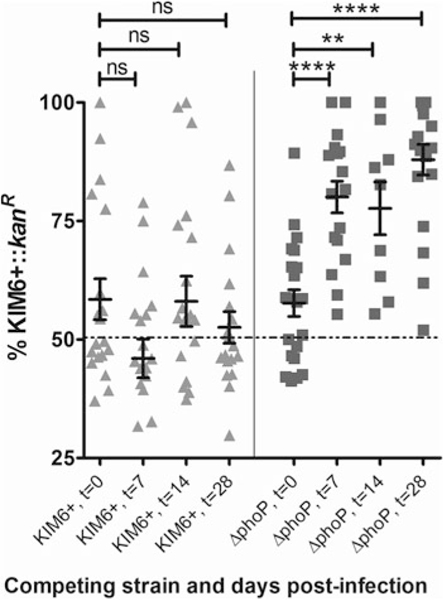
An example of a flea co-infection study in which a mutant in the known critical Y. pestis transmission factor, PhoP [6], and a wild type strain bearing an antibiotic resistance cassette are co-infected is depicted in Fig. 1. A wild type Y. pestis KIM6+ strain genetically marked with a kanamycin resistance cassette in the non-deleterious glmS-pstS site on the chromosome is used as the selective antibiotic strain (KIM6+ glmS-pstS::kanR also called KIM6+::kanR, unpublished data) and represents the isogenic wild type strain that will be competed with the KIM6+ ΔphoP mutant [6]. First a confirmation that the KIM6+::kanR does not confer a fitness impact was made by competing the strain with the isogenic Y. pestis KIM6+ wild type strain. The subsequent co-infection experiment of the KIM6+:: kanR and ΔphoP mutant [6] demonstrates a significant survival fitness defect of the ΔphoP mutant over a week, and this defect is not resolved by 4 weeks post-infection (Fig. 1). This survival fitness defect exhibited by the ΔphoP mutant when co-infected with the wild type recapitulates the observation of a published co-infection study using another PhoP mutant with a wild type strain harboring a plasmid encoding an ampicillin resistance cassette [13]. Generally, a complemented mutant strain should be co-infected with the same wild type strain to verify that this phenotype can be restored in a separate co-infection experiment; such data is not demonstrated here.
Fig. 1.
Mutation in PhoP confers a competitive fitness defect that is apparent when a PhoP mutant is co-infected with a Y. pestis KIM6+ wild type strain in fleas. In two separate co-infection experiments, X. cheopis fleas were co-infected with either a 1:1 ratio of Y. pestis KIM6+::kanR and KIM6+ (triangles) or, KIM6+::kanR and KIM6+ ΔphoP (squares). The Y. pestis bacterial loads were determined for each of 10–20 fleas at time points 0 (1 h following acquisition of the co-infected blood meal), 7, 14 and 28 days post-infection. The percentage of KIM6+::kanR in the co-infection was determined and plotted for each experiment and time point. Error bars represent mean ± SEM. A one-way ANOVA and post-hoc Bonferroni test were used to determine statistical significance between the time point 0 (t = 0) and other time points for each experiment
One potential shortcoming that experimenters may want to be mindful of when infecting with two strains into the same flea is the possibility of synergistic or trans-complementation effects in which no discernable difference in infectivity is observed. In such a case, the predicted or known biological function of the mutated factor might provide a clue as to whether this may be a significant consideration.
It is assumed that the researcher has the infrastructure, necessary equipment and knowledge of flea husbandry, so these aspects of the experimentation will not be covered. The experiments described here are performed with biosafety level two designated Y. pestis strains, devoid of the pCD1 plasmid. Appropriate biosafety and regulatory practices will have to be considered if fully virulent strains are to be used.
2. Materials
2.1. Skinning Mice
6+ week old mice (see Note 1).
Sterile 1× Phosphate-Buffered Saline (1× PBS).
Corkboard with push pins.
Plastic spoon.
Rubber bands.
Cling film/Saran wrap.
70% ethanol (EtOH).
2.2. Bacterial Culture
2.3. Flea Infection and Sorting
~300 Xenopsylla cheopis fleas per infection (see Note 3).
Mouse blood (see Note 4).
Water bath set at 42 °C with tubing to attach to water-jacketed feeder.
Peristaltic pump.
Flea cages (see Note 6).
Ultra-fine tip forceps, 0.09 × 0.05 mm tip.
Flea vacuum apparatus.
Dissecting microscope.
8–10 in. tall basin.
Chill table.
Waterproof medical tape.
Electric clippers with 0.25 mm clipper blade.
Glass petri dish.
Columbia blood agar plates.
Ice bucket.
Insect incubator set at 75% relative humidity and 21 °C.
2.4. Determining CFU/Flea
Brain Heart Infusion (BHI) agar plates.
Two water baths set to 42 °C and 46 °C (see Note 7).
BHI broth.
0.7% soft molten BHI agar: Melt 100 mL BHI agar completely in a microwave oven, immediately add an equal volume of BHI broth to it and incubate in the water bath set to 46 °C.
10 mg/mL hemin stock solution. Dissolve 10 mg hemin in 1 mL 0.05 N sodium hydroxide. Store at 4 °C.
1 mg/mL irgasan stock solution: Dissolve 1 mg irgasan in 1 mL 100% EtOH. Store at −20 °C.
Selective antibiotic (e.g. 50 mg/mL kanamycin) (see Note 8).
Sterile 1× PBS.
95% EtOH.
3% Hydrogen peroxide (H2O2).
100 × 15 mm sterile polystyrene petri dish.
Lysing Matrix H tubes (MP Biomedicals) (see Note 9).
Bunsen burner.
Two ultra-fine tipped forceps, 0.09 × 0.05 mm tip.
Bead beater (e.g. MP Biomedicals Fast Prep®−24).
Glass tubes with caps.
3. Methods
3.1. Culturing Y. pestis for Infection
Pick a 2 mm patch of single red-pigmented Y. pestis colonies from a CR plate (see Note 2) and culture, with antibiotic if appropriate, in 3 mL BHI broth overnight, with agitation.
Transfer entire volume of overnight culture into sterile 250 mL glass bottle containing 100 mL of BHI broth, with antibiotic if appropriate, and incubate overnight at 37 °C, without agitation.
3.2. Preparing Mouse Skin
Euthanize a 6+ week old mouse in accordance with IACUC approved protocols (see Note 10).
Spray mouse with 70% EtOH to sterilize the skin surface.
Use scissors to cut the skin around the neck of the mouse. Then, cut the skin from the base of the skull, down the back-bone of the mouse, to the tail.
Gently remove skin from the mouse and retain for experiment. Discard mouse carcass appropriately.
Place the skin, fur-side down, on corkboard. Using push pins, tautly stretch the skin and attach by the far corners to the board (see Note 11).
Put a few drops of 1 × PBS onto the skin surface and scrape off the fat layer of the skin using the side edge of a disposable plastic spoon (see Note 12).
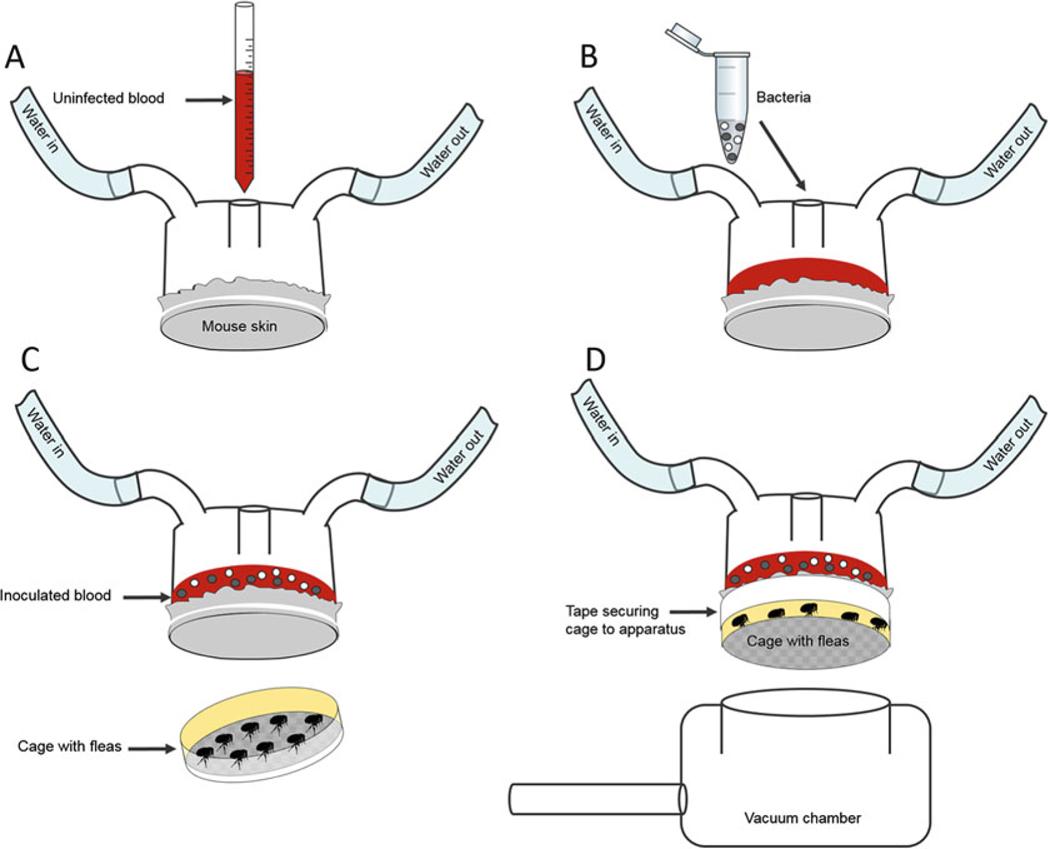
3.3. Preparing Artificial Glass Membrane Feeder (See Fig. 2)
Fig. 2.
Artificial flea feeding schematic. (a) Uninfected blood is added to the opening of the water-jacketed feeder with mouse skin to warm. (b) A 1:1 ratio of mutant strain (open circles) and isogenic wild type (grey circles) are added to blood. (c) The cold immobilized cohort of fleas is placed in the flea cage. (d) The flea cage is secured to the fur-side of the skin on the feeder, then attached to the vacuum chamber for prolonged feeding
Prepare the glass feeder by tautly stretching the mouse skin over the large 62 mm flange opening, fur-side out. Secure skin onto the apparatus with rubber bands.
Using electric clippers, closely shave fur to approximately 1–2 mm length. Assess for leaks in the skin by adding 1 × PBS into the skin covered chamber.
Attach feeder to the tubing of the peristaltic pump. Switch on pump to allow circulation of water to pervade outer jacket of feeder in order to maintain inner chamber at 37 °C (see Note 13).
Spin down the bacterial culture at 7500 × g at 4 °C and resuspend the pellet in 500 μL of sterile 1 × PBS and keep on ice.
Determine concentration of bacteria. Calculate how much is needed for a final concentration of 5 × 108 to 1 × 109 bacteria/mL blood separately for each strain (see Note 14).
Add 5 mL of blood to the inner chamber of the feeder to be pre-warmed approximately 5–10 min prior to bacterial inoculation.
Add equivalent amounts of each strain to 5 mL of pre-warmed blood in the feeder. Swirl blood and bacteria to properly mix together within feeder (see Note 15).
3.4. Infecting Fleas (See Fig. 2)
Chill fleas to immobilize for at least 5 min on ice.
Place immobile fleas into the bottom of a flea cage.
Securely attach cage to skin covered flange opening of feeder with surgical tape (see Note 16).
Place feeder with attached cage under weak suction from a vacuum (see Note 17).
Allow fleas to feed for approximately 1 h in a darkened area (see Note 18).
Disassemble and detach the cage from the feeder by removing the surgical tape, collect fleas in a tube and place them on ice for 10 min (see Note 19).
Select only well-fed fleas that have acquired a fresh infectious blood meal. This can be determined under the microscope by the presence of bright red blood filling ≥75% of the gut volume (see Note 20). Collect 20 of these fleas in a microfuge tube to represent the time point of day 0; time at which the infectious blood meal was acquired. Place the rest of the well-fed fleas into a labeled flea cage in an insect incubator. Collected fleas are stored at −80 °C until processed in Subheading 3.6.
Collect 100 μL of blood from the feeder upon completion of flea feeding. Serially dilute and plate blood from dilutions 10−6 to 10−7 onto Columbia blood agar plates with and without selective antibiotic.
Incubate plates for ~48 h in a 28 °C incubator and count colonies to determine colony forming units (CFU) of Y. pestis per mL blood. Verify CFU is within desired infectious dose range and that both strains are equally represented.
Fleas should be fed twice a week on a fresh blood meal for the duration of the experiment according to established lab protocols for flea maintenance. Collect fleas at required time points post-infection and store at −80 °C until processing according to Subheading 3.6 (see Note 21).
3.5. Preparing Top Layer Molten Agar
The following materials are enough for processing 10 co-infected fleas.
Allow 20 BHI plates to warm to room temperature (see Note 22).
Place two separate bottles of 100 mL melted 0.7% BHI soft agar in a 46 °C water bath (see Note 23).
Label 10 Lysing Matrix H tubes, 1 through 10, and sterilely add 1 mL of 1× PBS to each tube.
Place 20 capped glass test tubes into a 42 °C water bath.
Add hemin and irgasan to a final concentration of 10 μg/mL and 1 μg/mL, respectively, to each of the two molten agar bottles and swirl to mix.
Add appropriate selective antibiotic to one of the bottles and label.
Sterilely add 4 mL of the molten soft agar without selective antibiotic to 10 warmed glass test tubes resting in the water bath. Repeat with another 10 warmed glass test tubes using the molten agar containing selective antibiotic. Keep tubes in the 42 °C water bath.
3.6. Sterilizing Flea Surface and Preparing Flea Triturate
Fleas must be surface sterilized prior to processing to eliminate surface contaminants, and specifically quantify Y. pestis in the flea digestive tract. The following methods will be carried out using aseptic technique. Light a Bunsen burner to create a sterile environment on the laboratory bench.
Retrieve 10 co-infected fleas from −80 °C freezer storage.
Add 1 mL of 3% H2O2 to tube containing fleas and incubate for 2 min. Mix gently by inverting tube 2–3 times during incubation.
Gently draw off the H2O2 with a pipetman.
Add 1 mL of 95% EtOH to tube containing fleas and incubate for 1 min. Mix gently by inverting tube 2–3 times during incubation.
Gently draw off EtOH using a pipetman and add another 1 mL of 95% EtOH to tube containing fleas.
Pour fleas and EtOH onto a sterile petri plate. Draw off as much EtOH by tipping plate to a 45° angle to collect EtOH.
Separate the fleas using flame sterilized fine tipped forceps. Allow fleas to air dry in the petri dish (see Note 24).
Rinse fleas once by adding 10 mL sterile distilled water to petri dish. Gently remove water with a pipet.
Separate the fleas with sterilized forceps as before and allow them to air dry again for ~10 min.
Carefully transfer one flea into each of the 10 labeled Lysing Matrix H tube using sterilized forceps.
Lyse and homogenize fleas using a Fastprep bead beater (see Note 25). Machine settings: one cycle of 20 s at speed 6 (see Note 26).
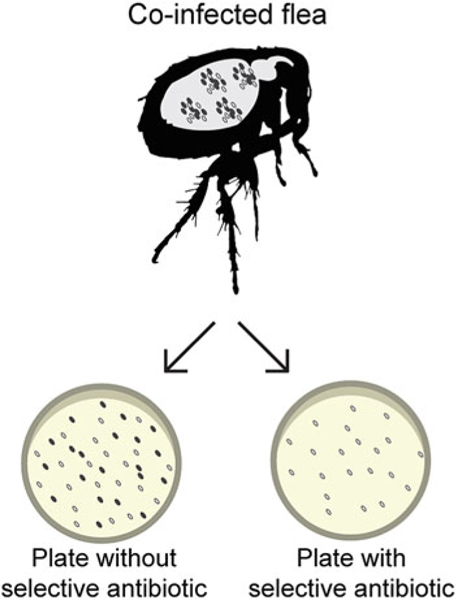
3.7. Plating Flea Triturate (See Fig. 3)
Fig. 3.
Co-infected flea plating schematic. The flea triturate is mixed with molten agar and plated as a top layer on an agar plate. For molten agar containing no selective antibiotic, both strains (open circles for antibiotic resistance marker encoding strain, closed circles for unmarked strain) grow providing a total CFU count per flea while selective antibiotic containing media allows for CFU enumeration of the strain that contains an antibiotic selective marker
Mix contents of crushed fleas by inverting tube 3–4 times.
Transfer 25 μL of crushed flea triturate to one glass tube containing molten agar without selective antibiotic (see Note 27).
Vortex the molten agar containing flea triturate, briefly flame the mouth of tube and pour entire contents onto the center of one appropriately labeled BHI agar plate. Rock the plate gently to distribute the agar evenly over the surface.
Set the plate on a flat surface and repeat for the remaining nine samples using molten agar tubes without selective antibiotic. Allow the plates to solidify for approximately 15 min.
Repeat steps 2–4 for selective antibiotic medium (see Note 28).
Add 3–4 mL of remaining molten soft agar (with or without selective antibiotic as appropriate) to overlay on each plate.
Allow the overlay layer to solidify for approximately 15 min.
Invert and incubate plates at 28 °C for 48–72 h.
Count colonies on plates using colony counter and multiply by the dilution factor to determine CFU Y. pestis per flea (see Note 29).
For each flea, calculate the percent selective marker strain over the total CFU per flea by dividing the selective antibiotic CFU count over total CFU count and multiply by 100. Plot and compare these percentages between different days post-infection. Apply statistical analyses. This should identify a significant advantage or disadvantage in fitness between compared strains (Fig. 1).
4. Notes
It is easier to see fleas on white-furred mice, i.e. Swiss Webster or CD-1.
For flea infections, hmsHFRS+ Y. pestis strains are usually used because these strains form a biofilm, which is important for persistent colonization of the flea gut in X. cheopis fleas [4]. Picking colonies from CR agar plates allows for confirmation of this phenotype prior to flea infection.
Co-infection studies described here are optimized for infection of X. cheopis fleas for which the dynamics of persistent Y. pestis infection has been well-established. Not all fleas may exhibit persistent colonization of the digestive tract by Y. pestis.
The blood is treated with sodium-heparin, but defibrinated blood can also be used [1]. Commercially purchased blood should be used as fresh as possible, i.e. within ~24–48 h of arrival.
The glass feeder is a patented invention (https://patents.google.com/patent/US4850305). The outer chamber forms the water jacket through which water at 42 °C can be circulated. This heated water can maintain the blood that is filled into the inner chamber at the physiologically relevant temperature of 37 °C. This feeder is commercially available through Lillie Glass Blowers, Inc. (Smyrna, USA).
Flea cages are custom made with a 62 mm diameter opening on the upper side that matches the diameter of the flange on the glass membrane feeder. A fine-pored nylon breathable mesh composes the base of the cage and top of the lid of the cage. Infected fleas can be maintained in the cage or a pint Mason glass jar lined at the bottom with a thin layer of sawdust. Instead of the solid aluminum flat cap on the Mason jar, a fine-pored mesh is glued to the screw band to prevent flea egress while maintaining airflow.
The water bath temperature must provide a balance of preventing molten agar from solidifying and death of Y. pestis.
We have successfully used 100 μg/mL carbenicillin for selection with strains harboring an ampicillin resistance cassette. However, each antibiotic used should be pre-tested to ensure absence of synergistic activity with irgasan.
Lysing Matrix H tubes have 2 mm glass and 2 mm zirconium beads that break through the flea’s chitinous exoskeleton, disrupt the midgut tissue, and break up the biofilm matrix without causing bacterial death under the optimized settings used.
The IACUC approved euthanization method used should keep the skin intact.
Make sure not to pierce or tear the main surface area of the skin.
The spoon should glide over the skin, there is no need for excessive dousing with PBS. Use enough force to scrape off the fat, without tearing the skin. Skins are typically prepared a day ahead and store at −20 °C wrapped in Saran wrap inside a sealed plastic container.
The 42 °C temperature of the water is sufficient to ensure that blood temperature is maintained at 37 °C. Blood is warmed within 10 min and ready for inoculation with bacteria.
This can be calculated using a Petroff-Hausser counting chamber. A pre-determined OD600 reading that represents the required Y. pestis CFU can also be used.
Blood may also be pre-warmed in a 37 °C incubator for 10 min before adding bacteria. Once bacteria are added, the inoculum should be mixed well and then placed into the feeder.
We use surgical tape to attach the bottom of the flea cage to the skin covering the feeder. The surgical tape adheres better to the mouse skin, and prevents tearing during disassembly of the feeder after infection.
The light suction from the vacuum pulls the blood against the mouse skin, and creates a humid micro-environment ideal for fleas feeding that mimics natural feeding conditions on a live host.
We cover the entire vacuum system and feeder with attached fleas with an opaque cover, like a black garbage bag.
When fleas are first placed on ice, simultaneously place a glass petri dish on the chilling table under the microscope to pre-chill in preparation to sort immobile fleas.
Fleas that have not fed well will sometimes clear the infection because they have not acquired an appropriate infectious dose. Such fleas will not be useful for your study and should be discarded.
We feed fleas on days 5, 8, 12, 15, 19, 22, and 26 post-infection. We collect fleas to analyze on day of infection and days 7, 14, and 28 post-infection.
Label plates 1 through 10 that normal agar will be added to and another 10 plates labeled 1 through 10 for adding agar containing selective marker antibiotic. The numbers of these plates should correspond to the same flea triturate tube.
If using solidified BHI soft agar, melt in the microwave by placing bottle of agar in a pan of water and microwave to prevent boiling over of agar.
Be careful not to pierce fleas because this may allow infiltration of EtOH, resulting in bacterial death.
If using another type of lysing tube or bead beater, optimization may be required to assure adequate crushing of flea without lysing bacteria.
Check each tube to make sure the flea has been crushed open to expel gut contents.
For fleas collected on day 0, transferring 25 μL flea triturate directly from the lysis matrix tube constitutes a 1:40 dilution of the flea triturate. The same is done for fleas collected at ≥7 days post-infection, except that flea triturate is diluted 1:10 in 1 × PBS first to obtain a final 1:400 dilution. This dilution series usually captures the countable range of colonies.
It is important to match a specific flea to a single number because the CFU calculated from the plate without antibiotics will be subtracted from the CFU from the corresponding plate with antibiotics.
Plates will frequently have many colonies that can be more accurately counted using a colony counter, i.e. Reichert™ Darkfield Quebec™ Colony Counter.
Acknowledgments
This work was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health Grants 1R21AI097974-01 and 1R01 AI117016-01A1 to V.V.
References
- 1.Bland DM, Jarrett CO, Bosio CF, Hinnebusch BJ (2018) Infectious blood source alters early foregut infection and regurgitative transmission of Yersinia pestis by rodent fleas. PLoS Pathog 14(1):e1006859. 10.1371/journal.ppat.1006859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bacot AW, Martin CJ (1914) LXVII. Observations on the mechanism of the transmission of plague by fleas. J Hyg 13(Suppl):423–439 [PMC free article] [PubMed] [Google Scholar]
- 3.Jarrett CO, Deak E, Isherwood KE, Oyston PC, Fischer ER, Whitney AR, Kobayashi SD, DeLeo FR, Hinnebusch BJ (2004) Transmission of Yersinia pestis from an infectious biofilm in the flea vector. J Infect Dis 190(4):783–792. 10.1086/422695 [DOI] [PubMed] [Google Scholar]
- 4.Hinnebusch BJ, Perry RD, Schwan TG (1996) Role of the Yersinia pestis hemin storage (hms) locus in the transmission of plague by fleas. Science 273(5273):367–370 [DOI] [PubMed] [Google Scholar]
- 5.Sun YC, Koumoutsi A, Jarrett C, Lawrence K, Gherardini FC, Darby C, Hinnebusch BJ (2011) Differential control of Yersinia pestis biofilm formation in vitro and in the flea vector by two c-di-GMP diguanylate cyclases. PLoS One 6(4):e19267. 10.1371/journal.pone.0019267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rebeil R, Jarrett CO, Driver JD, Ernst RK, Oyston PC, Hinnebusch BJ (2013) Induction of the Yersinia pestis PhoP-PhoQ regulatory system in the flea and its role in producing a transmissible infection. J Bacteriol 195 (9):1920–1930. 10.1128/JB.02000-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vadyvaloo V, Hinz AK (2015) A LysR-type transcriptional regulator, RovM, senses nutritional cues suggesting that it is involved in metabolic adaptation of Yersinia pestis to the flea gut. PLoS One 10(9):e0137508. 10.1371/journal.pone.0137508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rempe KA, Hinz AK, Vadyvaloo V (2012) Hfq regulates biofilm gut blockage that facilitates flea-borne transmission of Yersinia pestis. J Bacteriol 194(8):2036–2040. 10.1128/JB.06568-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fukuto HS, Svetlanov A, Palmer LE, Karzai AW, Bliska JB (2010) Global gene expression profiling of Yersinia pestis replicating inside macrophages reveals the roles of a putative stress-induced operon in regulating type III secretion and intracellular cell division. Infect Immun 78(9):3700–3715. 10.1128/IAI.00062-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aoyagi KL, Brooks BD, Bearden SW, Montenieri JA, Gage KL, Fisher MA (2015) LPS modification promotes maintenance of Yersinia pestis in fleas. Microbiology 161 (Pt 3):628–638. 10.1099/mic.0.000018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones RT, Vetter SM, Montenieiri J, Holmes J, Bernhardt SA, Gage KL (2013) Yersinia pestis infection and laboratory conditions alter flea-associated bacterial communities. ISME J 7 (1):224–228. 10.1038/ismej.2012.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lorange EA, Race BL, Sebbane F, Hinnebusch BJ (2005) Poor vector competence of fleas and the evolution of hypervirulence in Yersinia pestis. J Infect Dis 191(11):1907–1912. 10.1086/429931 [DOI] [PubMed] [Google Scholar]
- 13.Fukuto HS, Vadyvaloo V, McPhee JB, Poinar HN, Holmes EC, Bliska JB (2018) A single amino acid change in the response regulator PhoP acquired during Yersinia pestis evolution affects PhoP target gene transcription and polymyxin B susceptibility. J Bacteriol 200(9): e00050–18. 10.1128/JB.00050-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Surgalla MJ, Beesley ED (1969) Congo red-agar plating medium for detecting pigmentation in Pasteurella pestis. Appl Microbiol 18 (5):834–837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wade SE, Georgi JR (1988) Survival and reproduction of artificially fed cat fleas, Ctenocephalides felis bouche (Siphonaptera: Pulicidae). J Med Entomol 25:186–190 [DOI] [PubMed] [Google Scholar]