Abstract
On December 18, 2020, US Food and Drug Administration (FDA) approved a supplemental application for ponatinib extending the indication in patients with chronic-phase chronic myeloid leukemia (CP-CML) to patients with resistance or intolerance of at least 2 prior kinase inhibitors. Ponatinib was initially approved in December 2012 but was briefly voluntarily withdrawn due to serious safety concerns including the risk of arterial occlusive events (AOE). It returned to the market in December 2013 with an indication limited to patients with T315I mutation or for whom no other tyrosine kinase inhibitor (TKI) therapy was indicated with revised warnings and precautions. A post-marketing requirement was issued to identify the optimal safe and effective dose for CP-CML. Thus, the OPTIC trial was performed, which randomized patients to 1 of 3 doses, 45 mg, 30 mg, or 15 mg, with a dose reduction to 15 mg on achievement of MR2 (BCR-ABLIS ≤1%). Patients enrolled were treated with at least 2 prior TKIs or had a T315I mutation. Patients with a history of clinically significant, uncontrolled, or active cardiovascular disease were excluded. Efficacy was established on an interim analysis based on the rate of MR2 at 12 months in the modified intent-to-treat population of 261 patients, with 88, 86, and 87 patients in the 45, 30, and 15 mg cohorts, respectively. With a median follow-up of 28 months, the rate of achievement of MR2 at 12 months was 42%, 28%, and 24% in the respective cohorts. The safety profile was consistent with that observed in prior evaluations of ponatinib with notable adverse reactions including pancreatitis, hypertension, hyperlipidemia, liver dysfunction, and AOE. Of patients treated at the 45/15 mg dose, AOEs were seen in 13%, with a higher rate being observed in patients age 65 or older compared to younger patients. A readjudication of AOEs seen on the prior pivotal phase 2 study resulted in a rate of 26%. Overall, the results supported a modification of the recommended dose for patients with CP-CML to 45 mg until the achievement of MR2 followed by a reduction to 15 mg. The expansion of the indication to patients with exposure to 2 prior TKIs was approved given data showing that ponatinib could be successfully used for the treatment of this population with appropriate monitoring and screening for risk factors.
Keywords: ponatinib, chronic-phase chronic myeloid leukemia, FDA approval
This article reviews FDA approval of ponatinib as a supplemental application for patients with chronic-phase chronic myeloid leukemia.
Implications for Practice.
The approval of ponatinib for patients with chronic-phase chronic myeloid leukemia with resistance or intolerance of at least 2 prior kinase inhibitors, with appropriate monitoring and screening for AOE risk factors, provides another treatment option for patients with a poorer prognosis.
Introduction
Chronic myeloid leukemia (CML) is a chronic malignancy characterized by the build-up of immature myeloid precursors in the peripheral blood due to the BCR-ABL fusion protein. Treatment with specific tyrosine kinase inhibitors (TKIs) targeting BCR-ABL results in durable hematologic, cytogenetic, and molecular responses in most patients with CML, with better results if the treatment is initiated during the chronic phase (CP) of the disease.1 Since the approval of TKIs inhibiting BCR-ABL, CML has been considered to have a good prognosis, with life expectancy approaching normal for many patients with this condition.1,2 However, CML which is resistant to multiple targeted therapies or with mutations that confer resistance to BCR-ABL targeting TKIs has a much poorer prognosis.2 The T315I mutation, in which a point mutation in the BCR-ABL fusion gene results in the substitution of isoleucine for threonine in position 315 of the protein (T315I), confers resistance to all first and second-generation TKIs. The T315I mutation is observed in 0-25% of patients with CML in various series,3-5 with higher rates of occurrence in relapsed disease compared to de novo disease.
Ponatinib is a third-generation TKI that is active against CML with mutations in BCR-ABL, including the T315I mutation. It was initially approved under accelerated approval provisions by the US Food and Drug Administration (FDA) in December 2012 for use in CML or Philadelphia chromosome-positive (Ph+) acute lymphoblastic leukemia (ALL) resistant or intolerant to prior TKI therapy (Table 1).6 At the time of approval, a boxed warning was included in the label describing arterial occlusive events (AOE) associated with the use of ponatinib, along with a warning concerning hepatotoxicity. The risk of AOE was estimated to be 8% based on preliminary findings from the pivotal Phase 2 trial of ponatinib in patients with refractory CML and Ph+ ALL (PACE; NCT01207440) trial.7 However, post-marketing data suggested a much higher risk of AOE, including events observed in younger patients with no known risk factors. The product was voluntarily withdrawn by the sponsor from the market in October 2013 due to these findings.8 Ponatinib was reintroduced in December 2013 with revised warnings and precautions, including an updated boxed warning with a higher incidence of vascular occlusion (AOE plus venous thromboembolism [VTE]) of 27%, continued information on hepatotoxicity, new information on heart failure, and a Risk Evaluation and Mitigation Strategy that included a communication plan.9 At the time of reintroduction, the indication was limited to patients with T315I mutation or for whom no other TKI therapy was indicated. Several new post-marketing requirements (PMRs) were added, including PMR 2113-6, which required examination of the efficacy and safety of ponatinib at a variety of doses.10 In November 2016, regular approval was granted to ponatinib based on updated efficacy and safety data from PACE with a minimum of 48 months follow-up.11,12 The incidence of AOEs documented in the label was updated to 35% at this time.12 It was noted that AOEs tended to occur later in the course of treatment, with a median time to cerebrovascular and peripheral vascular events being more than 1 year after the start of treatment.
Table 1.
Ponatinib background information.
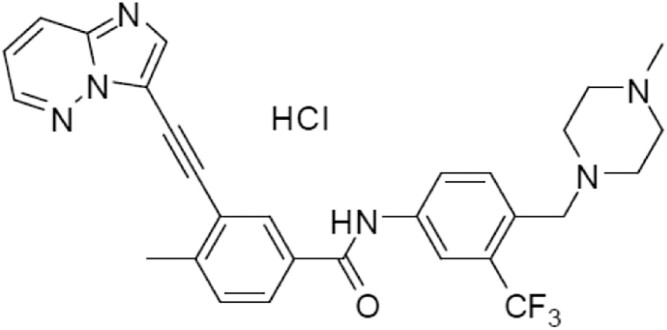
| Structure |
|
|---|---|
| Mechanism of Action | Ponatinib is a kinase inhibitor that inhibits the activity of ABL and T315I mutant ABL |
| Pharmacokinetics | The mean Cmax and AUC(0-24) of ponatinib 45 mg orally once daily at presumed steady state in patients with advanced hematologic malignancies were 73 ng/mL (74%) and 1253 ng·h/mL (73%), respectively. Peak concentrations of ponatinib are observed within 6 hours of oral administration. Food had no clinically significant effect on ponatinib exposure. Ponatinib is 99% plasma bound in vitro with no displacement in vitro by other highly plasma bound medications. The mean terminal elimination half-life was approximately 24 (12-66) hours. At least 64% of a dose undergoes phase I and II metabolism. CYP3A4 and, to a lesser extent, CYP2C8, CYP2D6, and CYP3A5 are involved in the phase I metabolism. Following a single oral dose of radiolabeled ponatinib, 87% of the dose was recovered in the feces and 5% in the urine. |
| Prior Approvals | December 2012: For adults with CML in chronic, accelerated, or blast phase that is resistant or intolerant to prior TKI therapy or Ph+ ALL that is resistant or intolerant to prior TKI therapy; withdrawn. December 2013: For adults with CML in chronic, accelerated, or blast phase or Ph+ ALL withT315I mutation or for whom no other TKI therapy is indicated June 2016: Indications updated to explicitly state that ponatinib is not indicated and not recommended for treatment of patients with newly diagnosed chronic phase CML. |
Abbreviation: TKI, tyrosine kinase inhibitors.
In July 2020, the Sponsor submitted a supplemental NDA to the FDA in which they proposed 2 major changes to the prescribing information. First, a new dosing regimen was proposed for patients with CP-CML based on data from the trial entitled “A Randomized, Open-Label, Phase 2 Trial of Ponatinib in Patients with Resistant Chronic Phase Chronic Myeloid Leukemia to Characterize the Efficacy and Safety of a Range of Doses” (OPTIC trial; NCT02467270), which was initiated to fulfill a safety post-marketing requirement. Second, the Sponsor proposed to revise the ponatinib indication to include an earlier line of therapy.
Assessment of Efficacy and Safety by Dose Schedule
Safety and efficacy results were reviewed across trials of ponatinib in patients with CP-CML using different doses and schedules. The OPTIC study served as the pivotal trial that evaluated new dosing regimens of ponatinib, whereas follow-up from the original PACE study provided long-term efficacy and safety data on the original dose regimen.
Clinical Trials Overview
OPTIC was an open-label, randomized, dose-optimization study of ponatinib in adults with CP-CML whose disease was resistant or resistant/intolerant to at least 2 prior kinase inhibitors or who have the T315I mutation. Patients with uncontrolled hypertension or diabetes and patients with clinically significant, uncontrolled, or active cardiovascular disease, including any history of myocardial infarction, peripheral vascular infarction, revascularization procedure, congestive heart failure (CHF), venous thromboembolism, or clinically significant/ventricular arrhythmias, were excluded. The study randomized patients 1:1:1 to one of 3 doses of ponatinib, 45 mg (cohort A), 30 mg (cohort B), or 15 mg (cohort C). Patients who were randomized to the 45 mg or 30 mg dose reduced their dose to 15 mg daily after the achievement of molecular response with ≤1% BCR-ABLIS (MR2). In addition, dose reduction was allowed for toxicity. The primary efficacy outcome examined was the achievement of MR2 at 12 months after initiation of therapy. Secondary outcomes of interest included safety, ≤0.1% BCR-ABLIS (MR3, also known as a major molecular response or MMR), complete or major cytogenetic response (CCyR or MCyR), duration of response (DOR), and overall survival (OS).
The final analysis was to be performed when all subjects are in the study for at least 12 months. The objective was to test the hypothesis that the rate of MR2 was greater than 20%. With a planned sample size of 276 patients (92 in each of the cohorts) and a true response rate of 35%, the study had 80% power to exclude a 20% response rate, with a 2-sided alpha of 0.0167 (Bonferroni method) in each cohort using an exact binomial test. The application provided results of a preplanned interim analysis performed after all patients enrolled in the study, which was descriptive in nature.
The PACE trial was a single-arm phase 2 study of ponatinib in adults with chronic phase, accelerated phase, or blast phase CML or Ph+ ALL whose disease was resistant or intolerant to either dasatinib or nilotinib or developed the T315I mutation after any TKI therapy. Exclusion criteria regarding cardiovascular risk factors were less restrictive than on OPTIC, with the exclusion of only uncontrolled hypertriglyceridemia and clinically significant or active cardiovascular disease, including the history of clinically significant atrial/ventricular arrhythmias or myocardial infarction, unstable angina, or congestive heart failure (CHF) within 3 months. Further details of the protocol design and endpoints have been described elsewhere.6 The only dose tested in this study was 45 mg daily continuously until progression or unacceptable toxicity. However, dose reductions for adverse events (AEs), particularly AOE, were allowed. Dose modification was common in patients treated on PACE, with 59% of patients requiring a dose reduction to 30 mg or 15 mg daily.7,9 After early evaluation of the data demonstrated a high risk of AOE and VTE, the PACE trial was modified to allow dose reduction to 15 mg for patients with CP-CML in MCyR and 30 mg daily for other patients. A post hoc analysis of the data suggested that dose reduction did not lead to a higher risk of loss of response13; however, this was not part of the prespecified statistical analysis plan. A second post hoc analysis of multiple trials, including PACE, suggested a lower risk of AOE among patients who were dose reduced to 15 mg daily.14 In addition, the risk of other AEs including pancreatitis, rash, and cardiac failure, increased transaminases, and arthralgia were related to dose intensity. Although, there remained uncertainty as to the best starting dose of therapy. The frequent requirement for dose reduction as well as uncertainty about whether a lower dose might be equally efficacious formed the basis for the requirement to study a range of doses, as was done in the OPTIC trial.
Demographics and Treatment Characteristics
The OPTIC study randomized a total of 283 patients internationally, including 94 on Cohort A, 95 on Cohort B (one patient in this cohort was not treated), and 94 on Cohort C. Baseline demographic characteristics of the 282 treated patients are presented in Table 2. In general, the cohorts were well balanced with minor variability between arms. Baseline demographics from the 270 patients with CP-CML from the PACE trial are also provided in Table 1 for comparison to OPTIC. The median age on OPTIC was 48 years, which is lower than patients enrolled in the PACE study (60 years for patients with CP-CML). Relatively few patients of minority race or ethnicity were enrolled in either trial. In contrast to PACE, few patients on OPTIC were treated in North America, with the majority being treated in Russia or South America. A small number of patients on both trials were previously treated with only a single TKI, while the majority in both trials were treated with at least 3 prior TKIs, and a considerable number were treated with imatinib plus a second-generation TKI. By design, few patients on OPTIC had a history of arteriovascular disease or risk factors for arteriovascular disease, with the exception of hypertension, which was observed in 29% of patients. In contrast, 18% of patients with CP-CML treated on PACE had a history of ischemic disease, and all examined risk factors except obesity were more commonly seen in PACE compared to OPTIC.
Table 2.
Selected demographic and disease characteristics of patients participating in the OPTIC trial overall and by treatment cohort and in PACE.
| Trial | OPTIC | PACE | ||||
|---|---|---|---|---|---|---|
| Demographic parameters | Cohort A 45 mg → 15 mg (N = 94) |
Cohort B 30 mg → 15 mg (N = 94) |
Cohort C 15 mg (N = 94) |
Total (N = 282) |
CP-CML (N = 270) |
Total (N = 449) |
| Sex | ||||||
| Male | 50 (53%) | 38 (40%) | 53 (56%) | 141 (50%) | 144 (53%) | 238 (53%) |
| Female | 44 (47%) | 56 (60%) | 41 (44%) | 141 (50%) | 126 (47%) | 211 (47%) |
| Age | ||||||
| Median (years) | 46 | 50.5 | 49.0 | 48.0 | 60.0 | 59.0 |
| Min, max (years) | 19, 81 | 21, 77 | 18, 81 | 18, 81 | 18, 94 | 18, 94 |
| Race | ||||||
| White | 73 (78%) | 77 (82%) | 72 (77%) | 222 (79%) | 218 (81%) | 352 (78%) |
| Black or African American | 1 (1%) | 2 (2%) | 3 (3%) | 6 (2%) | 11 (4%) | 25 (6%) |
| Asian | 16 (17%) | 12 (13%) | 15 (16%) | 43 (15%) | 32 (12%) | 59 (13%) |
| Other | 2 (2%) | 1 (1%) | 0 (0%) | 3 (1%) | 3 (1%) | 5 (1%) |
| Unknown/Missing | 2 (2%) | 2 (2%) | 4 (4%) | 8 (3%) | 6 (2%) | 8 (2%) |
| Ethnicity | ||||||
| Hispanic or Latino | 22 (23%) | 26 (28%) | 20 (21%) | 68 (24%) | 21 (8%) | 42 (9%) |
| Not Hispanic or Latino | 70 (75%) | 67 (71%) | 72 (77%) | 209 (74%) | 249 (92%) | 407 (91%) |
| Missing | 2 (2%) | 1 (1%) | 2 (2%) | 4 (1%) | 0 | 0 |
| Region | ||||||
| North America | 10 (11%) | 9 (10%) | 7 (7%) | 26 (9%) | 111 (41%) | 206 (46%) |
| South America | 22 (23%) | 25 (27%) | 16 (17%) | 63 (22%) | 0 | 0 |
| Europe excluding Russia | 10 (11%) | 17 (18%) | 19 (20%) | 46 (16%) | NA | NA |
| Russia | 38 (40%) | 31 (33%) | 38 (40%) | 107 (38%) | NA | NA |
| Asia | 14 (15%) | 12 (13%) | 14 (15%) | 40 (14%) | 27 (10%) | 44 (10%) |
| Europe (all regions)/Australia | NA | NA | NA | NA | 132 (49%) | 199 (44%) |
| Smoker? | ||||||
| Current | 9 (10%) | 14 (15%) | 16 (17%) | 39 (14%) | 21 (8%)a | 23 (5%)a |
| Former | 20 (21%) | 23 (24%) | 17 (18%) | 60 (21%) | NA | NA |
| Never | 65 (69%) | 55 (59%) | 59 (63%) | 179 (63%) | 10 (4%) | 11 (2%)a |
| Unknown | 0 | 2 (2%) | 2 (2%) | 4 (1%) | 239 (89%) | 415 (92%) |
| Prior treatment | ||||||
| Single TKI | 1 (1%) | 1 (1%) | 4 (4%) | 6 (2%) | 18 (7%) | 31 (7%) |
| Imatinib + 2nd+ gen TKI | 37 (39%) | 28 (30%) | 34 (36%) | 99 (35%) | 89 (33%) | 155 (35%) |
| Any 2 2nd gen TKIs | 6 (6%) | 9 (9%) | 8 (9%) | 23 (8%) | 3 (1%) | 6 (1%) |
| At least 3 TKIs | 50 (53%) | 56 (60%) | 48 (51%) | 154 (55%) | 159 (59%) | 38256 (57%) |
| No prior approved TKIs | 0 | 0 | 0 | 0 | 1 (<1%) | 1 (<1%) |
| T315I status | ||||||
| Yes | 25 (27%) | 21 (22%) | 20 (21%) | 66 (23%) | 60 (22%) | 190 (43%) |
| No | 67 (71%) | 73 (77%) | 74 (79%) | 216 (77%) | 188 (70%) | 216 (48%) |
| Missing | 2 | 0 | 0 | 0 | 22 (8%) | 43 (10%) |
| History of ischemic disease | ||||||
| Yes | 3 (3%) | 1 (1%) | 0 | 4 (1%) | 48 (18%) | 67 (15%) |
| No | 91 (97%) | 93 (99%) | 94 (100%) | 278 (99%) | 222 (82%) | 382 (85%) |
| History of hypertension | ||||||
| Yes | 29 (31%) | 27 (29%) | 24 (26%) | 81 (29%) | 102 (38%) | 159 (35%) |
| No | 65 (79%) | 67 (71%) | 70 (74%) | 201 (71%) | 168 (62%) | 290 (65%) |
| History of diabetes | ||||||
| Yes | 5 (5%) | 3 (3%) | 7 (7%) | 15 (5%) | 35 (13%) | 57 (13%) |
| No | 89 (95%) | 91 (97%) | 87 (93%) | 267 (95%) | 235 (87%) | 392 (87%) |
| History of hypercholesterolemia | ||||||
| Yes | 3 (3%) | 4 (4%) | 6 (6%) | 13 (5%) | 65 (24%) | 100 (22%) |
| No | 91 (97%) | 90 (96%) | 88 (94%) | 269 (95%) | 205 (76%) | 349 (78%) |
| History of obesity | ||||||
| Yes | 8 (9%) | 10 (11%) | 4 (4%) | 22 (8%) | 15 (6%) | 19 (4%) |
| No | 86 (91%) | 84 (89%) | 90 (96%) | 260 (92%) | 255 (94%) | 430 (96%) |
Smoking status was described as “yes” or “no” only in the PACE trial.
Abbreviation: TKI, tyrosine kinase inhibitors.
Efficacy Results
Results of the preplanned interim analysis on OPTIC showed an MR2 at 12 months in 29 out of 75 evaluable patients (39%; 95% confidence interval [CI]: 28%-51%) in cohort A, 20 out of 73 (27%; 95% CI: 18%-39%) in cohort B, and 18/68 (27%; 95% CI: 17%-39%) in cohort C. An additional interim efficacy analysis was evaluated with approximately 7.5 months further data on the modified intent to treat (ITT) population of 261 patients (88 on Cohort A, 86 on Cohort B, and 87 on Cohort C) who had b2a2/b3a2 BCR ABL1 transcripts and reached the 12-month timepoint or who had discontinued the study before 12 months, the latter of whom were considered non-responders. With a median follow-up of 28 months, the rate of achievement of MR2 at 12 months was 42% in cohort A, 28% in cohort B, and 24% in cohort C (Table 3). The median duration of response was not reached for all cohorts. Higher rates of MCyR were seen in cohort A as well. The rate of MR3 was similar between the 3 cohorts.
Table 3.
Primary and key secondary efficacy results of OPTIC.
| Cohort A 45 mg → 15 mg |
Cohort B 30 mg → 15 mg |
Cohort C 15 mg |
|
|---|---|---|---|
| MR2/≤1% BCR-ABL1IS at 12 months (N)a,b | 88 | 86 | 87 |
| Number of responders | 37 | 24 | 21 |
| Rate (95% CI), % | 42 (32, 53) | 28 (19, 39) | 24 (16, 35) |
| MR3a,c at 12 months | 88 | 86 | 87 |
| Number of responders | 13 | 17 | 15 |
| Rate (95% CI), % | 15 (8.1, 24) | 20 (12, 30) | 17 (10, 27) |
| MCyRd by 12 months | 86 | 85 | 85 |
| Number of responders | 42 | 22 | 36 |
| Rate (95% CI), % | 49 (38,60) | 26 (17, 37) | 42 (32, 54) |
Includes information from interim efficacy analysis with median duration of follow-up 28 months.
ITT population includes patients who had b2a2/b3a2 BCR ABL1 transcripts. Excludes patients that did not reach the 12-month timepoint while still on study. Patients with MR2 at baseline or patients who discontinued treatment or terminated study before 12 months were treated as a non-responders.
Based on ITT population includes patients who had b2a2/b3a2 BCR ABL1 transcripts. Excludes patients that did not reach the 12-month timepoint and patients with MR3 at baseline.
Based on ITT cytogenetic population defined as patients who had a cytogenetic assessment at baseline with at least 20 metaphases examined. Excludes patients who did not reach the 12-month timepoint and patient with CCyR at baseline.
Abbreviations: CI, confidence interval; MCyR, major cytogenetic response; N, number of evaluable patients.
Exploratory subgroup analyses demonstrated similar rates of achievement of MR2 in cohort A for patients who were treated with 2 prior TKIs versus 3 or more and those with or without T315I mutation (Table 4). The rates of MR2 were lower in cohorts B and C for patients with versus without the T315I mutation. Furthermore, it was noted that patients aged 65 years or older were less likely to achieve MR2 at any dose compared with those aged less than 65. A higher rate of MR2 at 12 months was observed in patients aged 65 years and older treated on cohort A compared to the other cohorts, but the rate (29%) was lower than that for patients aged less than 65 (45%). However, it should be noted that the confidence interval for older patients on cohort A was wide (8.4%-58%) and overlapped with that of younger patients (33%-57%).
Table 4.
| Cohort A 45 mg → 15 mg (N = 88) |
Cohort B 30 mg → 15 mg (N = 86) |
Cohort C 15 mg (N = 87) |
|
|---|---|---|---|
| MR2 at 12 months by the number of prior TKI therapies | |||
| For those having 2 prior TKIs | 39 | 35 | 38 |
| Number of responders | 15 | 12 | 11 |
| Rate (95% CI), % | 38 (23, 55) | 34 (19, 52) | 29 (15, 46) |
| For those having 3+ prior TKIs | 48 | 51 | 45 |
| Number of responders | 22 | 12 | 10 |
| Rate (95% CI), % | 46 (31, 61) | 24 (13, 37) | 22 (11, 37) |
| MR2 at 12 months by T315I mutation status | |||
| For those with T315I mutation | 24 | 20 | 18 |
| Number of responders | 10 | 4 | 2 |
| Rate (95% CI), % | 42 (22, 63) | 20 (5.7, 44) | 11 (1.4, 35) |
| For those without T315I mutation | 64 | 66 | 69 |
| Number of responders | 27 | 20 | 19 |
| Rate (95% CI), % | 42 (30, 55) | 30 (20, 43) | 28 (17, 40) |
| MR2 by age cohort | |||
| Age < 65 years | 74 | 75 | 80 |
| Number of responders | 33 | 23 | 20 |
| Rate (95% CI), % | 45 (33, 57) | 31 (21, 42) | 25 (16, 36) |
| Age ≥ 65 years | 14 | 11 | 7 |
| Number of responders | 4 | 1 | 1 |
| Rate (95% CI), % | 29 (8.4, 58) | 9.1 (0.2, 41) | 14 (0.4, 58) |
Includes information from interim efficacy analysis with median duration of follow-up 28 months.
ITT population includes patients who had b2a2/b3a2 BCR ABL1 transcripts. Excludes patients that did not reach the 12-month timepoint while staying on study.
Abbreviations: CI, confidence interval; MR2, ≤1% BCR-ABL1IS; N, number of evaluable patients; TKI, tyrosine kinase inhibitors.
The submission provided updated efficacy data from PACE, which minimally impacted results already contained in labeling for ponatinib. An analysis of efficacy data with a median follow-up of 40.5 months was performed on the modified ITT population of 267 patients with CP-CML, excluding patients without confirmation of T315I mutation status and patients who had not received prior dasatinib or nilotinib. Although not a prespecified endpoint on the PACE trial, FDA performed an exploratory analysis of MR2 at 12 months for comparison to the OPTIC trial. MR2 at 12 months was achieved by 34% (95% CI 29%-40%) of 267 CP-CML patients on PACE. MR3 at any time was 40% (95% CI 35%-47%). With a minimum follow-up of 60 months, the median duration of MR3 (range: 1 day to 67.8 months) had not been reached.
Safety Results
On OPTIC, the review of the safety focused on an analysis across cohorts A, B, and C. At least one treatment-emergent adverse event (TEAE) was observed in 96% of patients on the study and 100% of patients in cohort A. Common (≥10%) nonhematological adverse reactions and adverse events of special interest are listed in Table 5 and notable laboratory abnormalities are listed in Tables 6 and 7. Events more common on cohort A (>5 percentage points difference compared to other cohorts) included thrombocytopenia, rash, neutropenia, infection, hepatic dysfunction, hyperlipidemia, pyrexia, cardiac failure, dry skin, and cardiac arrhythmias. A smaller dose/response effect was observed for AOE, pancreatitis, and abdominal pain. Hypertension was more common in patients on cohort A and B compared to cohort C. Laboratory abnormalities seen more commonly in cohort A included hemoglobin decreased, lipase increased, transaminases increased, glucose increased, and triglycerides increased. Only a single treatment-emergent venous thromboembolic event, occurring in cohort A, was observed in patients treated on OPTIC.
Table 5.
Common (≥10%) treatment emergent adverse events and adverse events of special interest in patients on the OPTIC trial, excluding laboratory terms.
| Eventa | Cohort A 45 mg → 15 mg (n = 94) |
Cohort B 30 mg → 15 mg (n = 94) |
Cohort C 15 mg (n = 94) |
Total (N = 282) |
|---|---|---|---|---|
| Any | 94 (100%) | 88 (94%) | 88 (94%) | 270 (96%) |
| Rash | 48 (51%) | 34 (36%) | 26 (28%) | 108 (38%) |
| Arthralgia/myalgia | 26 (28%) | 31 (33%) | 21 (22%) | 78 (28%) |
| Hypertensionb | 31 (33%) | 34 (36%) | 24 (26%) | 87 (31%) |
| Infection | 29 (31%) | 18 (19%) | 23 (24%) | 70 (25%) |
| Abdominal painc | 26 (28%) | 23 (24%) | 19 (20%) | 68 (24%) |
| Hepatic dysfunction | 23 (25%) | 15 (16%) | 24 (26%) | 62 (22%) |
| Pancreatitis | 22 (23%) | 18 (19%) | 14 (15%) | 54 (19%) |
| Headache | 16 (17%) | 16 (17%) | 17 (18%) | 49 (17%) |
| AOEd | 16 (17%) | 14 (15%) | 11 (12%) | 41 (15%) |
| Constipation | 10 (11%) | 11 (12%) | 14 (15%) | 35 (12%) |
| Eye disorderse | 10 (11%) | 13 (14%) | 9 (10%) | 32 (11%) |
| Hemorrhage | 11 (12%) | 14 (15%) | 6 (6%) | 31 (11%) |
| Cardiac arrythmias (SMQ) | 14 (15%) | 9 (10%) | 5 (5%) | 28 (10%) |
| Pyrexia | 15 (16%) | 4 (4%) | 9 (10%) | 28 (10%) |
| Fatigue/asthenia | 9 (10%) | 11 (12%) | 6 (6%) | 26 (9%) |
| Edema | 5 (5%) | 8 (9%) | 11 (12%) | 24 (9%) |
| Cardiac failure | 11 (12%) | 4 (4%) | 3 (3%) | 18 (6%) |
| Dry skin | 11 (12%) | 5 (5%) | 4 (4%) | 20 (7%) |
| Neuropathy | 7 (7%) | 5 (5%) | 10 (11%) | 22 (7%) |
| Venous thromboembolism | 1 (1%) | 0 | 0 | 1 (<1%) |
See supplemental documents for grouped terms
Varies slightly from label due to inclusion of white coat hypertension
Varies slightly from label due to inclusion of preferred term dyspepsia
Includes all search terms. See also AOE discussion in the section below for further information
Excluding vascular
Table 6.
Grade 3+ hematologic laboratory abnormalities of >5% incidence in patients on OPTIC.
| Laboratory test | Cohort A 45 mg → 15 mg (n = 94) |
Cohort B 30 mg → 15 mg (n = 94) |
Cohort C 15 mg (n = 94) |
Total (N = 282) |
|---|---|---|---|---|
| Platelet count decreased | 29 (31%) | 29 (31%) | 27 (29%) | 27 (29%) |
| Neutrophil count decreased | 21 (22%) | 19 (20%) | 22 (23%) | 63 (22%) |
| Hemoglobin decreased | 13 (14%) | 6 (6%) | 5 (5%) | 22 (8%) |
| WBC decreased | 12 (13%) | 12 (13%) | 6 (6%) | 30 (11%) |
| Lymphocyte decreased | 7 (7%) | 8 (9%) | 6 (6%) | 21 (7%) |
Table 7.
All-grade non-hematologic laboratory abnormalities occurring in >20% of patients on OPTIC.
| Laboratory test | Cohort A 45 mg → 15 mg (n = 94) |
Cohort B 30 mg → 15 mg (n = 94) |
Cohort C 15 mg (n = 94) |
Total (N = 282) |
|---|---|---|---|---|
| Liver Function Tests | ||||
| ALT increased | 46 (49%) | 29 (31%) | 37 (39%) | 112 (40%) |
| AST increased | 38 (40%) | 22 (23%) | 26 (28%) | 86 (31%) |
| Alkaline phosphatase increased | 22 (23%) | 18 (19%) | 20 (21%) | 60 (21%) |
| Pancreatic Enzymes | ||||
| Lipase increased | 32 (34%) | 26 (28%) | 22 (23%) | 80 (28%) |
| Other Chemistry | ||||
| Glucose increased | 43 (46%) | 35 (37%) | 37 (39%) | 115 (41%) |
| Triglycerides increased | 39 (42%) | 29 (31%) | 27 (29%) | 95 (36%) |
| BNP | 36 (38%) | 29 (31%) | 22 (23%) | 87 (31%) |
| Cholesterol | 33 (35%) | 17 (18%) | 22 (23%) | 72 (26%) |
| Phosphate decreased | 25 (27%) | 27 (29%) | 21 (22%) | 73 (26%) |
| Bicarbonate decreased | 25 (27%) | 19 (20%) | 24 (26%) | 68 (24%) |
Abbreviations: ALT, alanine transferase; AST, aspartate aminotransferase; BNP, B-type natriuretic peptide.
A review of PACE safety data confirmed the previously identified risks documented in the label. Serious adverse events (SAEs) occurred in 304/449 (68%) of patients on PACE, with the most common SAEs (>5%) being AOE, pneumonia, abdominal pain, cardiac failure, pancreatitis, arrhythmias, and hemorrhage. Twenty-seven (6%) malignant neoplasms other than the condition under treatment were observed in patients on PACE, including skin cancers (including melanoma) seen in 13 patients. The other malignancies observed were varied without a single dominant condition being seen. Malignancies other than CML were seen only rarely on OPTIC (2 patients); however, the follow-up time is too short to draw conclusions for that study.
Dose modifications and discontinuations due to adverse events (AEs) occurred commonly in patients treated on OPTIC, in 70%, 64%, and 58% of patients on cohorts A, B, and C, respectively, including discontinuation in 18%, 15%, and 16% of patients, respectively. The most common events leading to discontinuation included thrombocytopenia, AOE, other cytopenias, infection, and other cardiac or vascular events including hypertension, sudden death, and cardiac failure. FDA concluded that a total of 4 (1%) deaths on OPTIC were possibly resulted from the toxicity of ponatinib. Two deaths, both characterized as sudden death, occurred in cohort A and 2, both attributed to infection, in cohort C. No deaths on treatment were observed in cohort B.
The Sponsor submitted long-term safety data from PACE, which included independent adjudication of AOE and venous thromboembolism events to better characterize the risk of thrombotic events in this population. The company proposed that some events considered to be AOEs in prior labeling may have been miscategorized, leading to overestimation of the risk of AOEs in the label. To assess the proposal, events identified as possible or probable AOE in PACE and OPTIC by included AE terms were adjudicated by the company and the FDA.
AOEs were identified using AE terms in 156 (35%) of patients on the PACE study. Adjudication of all events was performed using information obtained from clinical narratives, safety reports describing the events, laboratory and vital signs data surrounding the events, and associated AEs. Events that were judged to be unlikely to represent true AOEs included atypical chest pain without concomitant troponin elevation or EKG changes, Raynaud’s phenomenon in the absence of other signs of vascular disease, and non-specific complaints of coldness in limbs. In addition, grade 1 events without concurrent AEs, ECG, or laboratory findings were considered unlikely to represent true AOEs. However, any event coded as a term consistent with arterial occlusion (ie, angina, transient ischemic attack) was considered to be a true AOE. After adjudication by the Sponsor and FDA, 41 of these events were deemed unlikely to represent true AOE, resulting in a final rate of AOE of 115 (26%) in the PACE trial. Of these, fatal AOE occurred in 9 (2%) of patients. Events occurred as early as one day and as late as 4.9 years after initiation of therapy, with the median time to onset being 1 year for cardiovascular events, 1.4 years for cerebrovascular events, and 2 years for peripheral vascular events. Events were more common in patients with pre-existing risk factors but occurred in patients with no known risk factors for AOE before start of the study.
Initial review using AE terms identified 41 (15%) patients with AOE on the OPTIC trial, including 16 (18%) of patients on cohort A. After adjudication of AOEs in cohort A, 4 events were found to be unlikely to represent AOEs, leaving a final rate of identified AOEs of 12 (13%) of patients in this cohort. The most common AOE on Cohort A was cardiovascular events (eg, myocardial infarction, angina, chest pain), occurring in 9% of patients. The median time to onset for the first event was 4.5 months for cardiovascular events, 1 year for cerebrovascular events, and 3.6 months for peripheral vascular events. At the time of data cutoff, the median follow-up time was 28 months. Patients aged 65 years and older were more likely to experience AOE compared to younger patients, with 6/78 (8%) of patients under age 65 and 6/16 (38%) of patients aged 65 years or older treated on cohort A experiencing an AOE during treatment.
A single event of venous thromboembolism was observed in the OPTIC trial and therefore no further adjudication of this trial was required. VTE was adjudicated in PACE with a final rate of VTE events confirmed to be 6%.
Clinical Pharmacology
Pharmacokinetics
Ponatinib exhibits dose-proportional increases in steady-state Cmax and AUC0-24h from 2 to 60 mg once daily, demonstrates a mean (range) terminal half-life of 24 (12-66) hours after a dose of 45 mg once daily for 28 days and is primarily metabolized in the liver involving CYP3A4 (major), and 2C8, 2D6, 3A5. It is also metabolized by esterases and/or amidases. Population pharmacokinetic analysis showed that age (19-85 years), body weight (41-152 kg), and mild-to-moderate renal impairment (creatinine clearance 30-89 mL/minute) has no clinically meaningful effects on the pharmacokinetics of ponatinib. The effects of severe renal impairment (creatinine clearance 15-29 mL/minute) on the pharmacokinetics of ponatinib are unknown. Hepatic impairment of any severity (Child-Pugh A, B, or C) had no significant effect on ponatinib exposure following a single dose of 30 mg; however, subjects with hepatic impairment had increased incidence of adverse reactions and should therefore receive a lower starting dose of ponatinib. Given the metabolism of ponatinib via CYP metabolism enzymes, coadministration of strong CYP3A inhibitors or inducers with ponatinib should be avoided to prevent changes in exposure which may increase the risk of adverse events with inhibitors or reduce efficacy with inducers. If coadministration cannot be avoided, reduce the dose of ponatinib with inhibitors or monitor for reduced efficacy with inducers.
Exposure-Response Relationships
Exposure-response relationships for efficacy based on data from the OPTIC study showed that increasing ponatinib concentrations were associated with an increased probability of transitioning to an improved response (eg, from MR1 to MR2 or better) and a decrease in the probability of transitioning to a poorer response (eg, from MR1 to NR). Age was identified as a statistically significant covariate with older age associated with a poorer response rate.
Exposure-response relationships for safety based on data from the OPTIC study identified a statistically significant relationship between increased ponatinib exposure and adverse reactions including AOE and Grade 3 or higher thrombocytopenia. Baseline hypercholesterolemia was a statistically significant risk factor for Grade 3 or higher AOE. Other previously identified risk factors for AOE (including age and history of ischemia, hypertension, or diabetes) could not be identified as significant risk factors for AOE in the OPTIC study given the small number of patients with those cardiovascular risk factors included in the study due to the strict eligibility criteria compared to the PACE trial.
Discussion
The OPTIC trial provided substantial evidence of efficacy and safety to support approval of the 45 mg starting dose of ponatinib with a reduction to 15 mg upon achievement of MR2 to patients with CP-CML with resistance or intolerance to at least 2 prior kinase inhibitors. Regular approval was granted based on the rate of MR2 at 12 months of 42% in patients treated with this dosing regimen, as well as MCyR rate by 12 months, duration of response, and a tolerable safety profile. Efficacy was comparable to that demonstrated with the previously approved ponatinib dosing regimen of 45 mg daily, continuously, on the PACE trial. Furthermore, there was a lower incidence of AOE events at 13% on OPTIC in cohort A compared to 26% observed on PACE after adjudication.
Ponatinib has a complex regulatory history. It was withdrawn from the market due to the high AOE rate in both clinical trials and in the post-marketing setting, as well as the finding of multiple other serious toxic effects including pancreatitis, hepatotoxicity, myelosuppression, and risk of RPLS. However, in the absence of other available TKI treatment for the T315I mutation, it was returned to the market after revision of the label to delineate the risks and limit use to patients with T315I mutation or who were not eligible for other TKI therapy. The optimal dose of ponatinib was not felt to be identified by prior studies, including PACE, leading to the PMR for examination of the efficacy and safety at a variety of doses.10 The OPTIC trial was thus initiated to examine a variety of initial doses with efficacy-adapted dose reduction and determine the dose with the best benefit-risk ratio. It was hoped that the decrease in dose after an MR2 was obtained would reduce the risk of AOE.
Efficacy results from the OPTIC study demonstrate a higher rate of achievement of MR2 at 12 months in patients who were randomized to the 45 mg starting dose. An analysis by the Sponsor showed a dose-response relationship as well.12 Because of this, 45 mg remains the recommended starting dose for ponatinib in patients with chronic phase CML. The effect of dose reduction to 15 mg after the achievement of MR2 has not yet been completely characterized and the approval was issued with a new PMR for long-term safety follow-up from OPTIC. Of note, the OPTIC study enrolled only patients who were in the chronic phase of CML. Therefore, the recommended dose for patients in accelerated or blast phase or with Philadelphia chromosome-positive ALL remains 45 mg daily continuously.
The overall safety profile observed in OPTIC was generally consistent with the known safety profile of ponatinib. Of note, the AOE incidence was lower than on PACE.15 However, this may be related to the lower baseline risk of patients enrolled on OPTIC compared to PACE. In addition, it is difficult to directly compare the rate of AOE in OPTIC versus PACE due to the difference in follow-up time for each study. The median follow-up time for patients on OPTIC is less than the median time to AOE for patients treated on the PACE study, which may have resulted in a lower apparent incidence. Further follow-up is needed to definitively determine the risk. However, it is noted that the risk of AOE was lower in the lower dose cohorts on OPTIC so the dose decrease to 15 mg after the achievement of MR2 may reduce this risk. Similarly, the risk of VTE was lower on OPTIC, possibly due to a lower risk population and more aggressive prophylaxis.
Second malignant neoplasms were observed in 6% of patients treated with ponatinib on the PACE study, with skin neoplasms being seen most frequently and no other single primary predominating. A risk of second neoplasms has not previously been identified in patients treated with ponatinib. The mechanism of action by which ponatinib is associated with an increased risk of the second neoplasm is unclear since it was not noted to be mutagenic in non-clinical studies. The observation may be due to off-target effects, immune system changes, or the underlying disease. Further observation is needed to explore this issue.
Based on the demonstrated efficacy and manageable safety profile in patients previously treated with 2 or more TKIs, the indication was expanded to include adults with CP-CML who have failed at least 2 prior therapies. However, several caveats should be noted. First, patients with clinically significant, uncontrolled, or active cardiovascular disease were excluded from the OPTIC study. Patients with cardiovascular disease may be at higher risk for AOE or venous thrombosis and thus the benefit-risk ratio should be considered carefully before starting treatment with ponatinib in these patients. Second, dose reductions for toxicity were common in patients who started treatment at the 45 mg dose. Careful clinical and laboratory monitoring and dose modification, if necessary, are essential to the safe use of ponatinib. Third, patients age 65 and over had a higher risk of AOE than younger patients and were less likely to achieve MR2 compared to younger patients. In addition, the median age of patients treated on OPTIC was lower than the median age for patients with CML in the general population15 and the number of patients aged 65 years or older in OPTIC was small. Thus, the optimal dose in this population is uncertain and the benefit-risk ratio should be considered carefully in this population before treatment is initiated. Finally, the long-term efficacy and safety of the 45/15 dosing regimen will need to be explored. To gain insight into the long-term outcomes of patients treated with this regimen, patients on OPTIC will be followed for up to 5 years.
Conflict of Interest
The authors indicated no financial relationships.
Author Contributions
Conception/design: All authors. Provision of study material or patients: All authors. Collection and/or assembly of data: All authors. Data analysis and interpretation: All authors. Manuscript writing: All authors. Final approval of manuscript: All authors.
Data Availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. Sasaki K, Strom SS, O’Brien S, et al. Prospective analysis: Relative survival in patients with chronic myeloid leukemia in chronic phase in the era of tyrosine kinase inhibitors. Lancet Haematol. 2015;2(5):e186–e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bower H, Björkholm M, Dickman PW, Höglund M, Lambert PC, Andersson TM.. Life expectancy of patients with chronic myeloid leukemia approaches the life expectancy of the general population. J Clin Oncol. 2016;34(24):2851-2857. [DOI] [PubMed] [Google Scholar]
- 3. Kim H, Kim S, Kim HJ, et al. Comparison of frequency and sensitivity of BCR-ABL1 kinase domain mutations in Asian and white patients with imatinib-resistant chronic-phase chronic myeloid leukemia. Clin Lymphoma Myeloma Leuk. 2018;18(10):e391-e399. [DOI] [PubMed] [Google Scholar]
- 4. Liu J, Yang H, Xu X, Yi S, Meng L.. Mutations in the BCR-ABL1 kinase domain in patients with chronic myeloid leukaemia treated with TKIs or at diagnosis. Oncol Lett. 2020;20(2):1071-1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wongboonma W, Thongnoppakhun W, Auewarakul CU.. BCR-ABL kinase domain mutations in tyrosine kinase inhibitors-naïve and -exposed Southeast Asian chronic myeloid leukemia patients. Exp Mol Pathol. 2012;92(2):259-265. [DOI] [PubMed] [Google Scholar]
- 6. US Food and Drug Administration. ICLUSIG® (ponatinib) tablets for oral use (2012). Accessed May 24, 2021. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/203469lbl.pdf
- 7. Cortes JE, Kim DW, Pinilla-Ibarz J, et al. ; PACE Investigators . A phase 2 trial of ponatinib in Philadelphia chromosome-positive leukemias. N Engl J Med. 2013;369(19):1783-1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kim J, Nair A, Keegan P, et al. Evaluation of serious Postmarket safety signals within 2 years of FDA approval for new cancer drugs. Oncologist. 2020;25(4):348-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. US Food and Drug Administration. ICLUSIG® (ponatinib) tablets for oral use (2013). Accessed May 24, 2021. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/203469s007s008lbl.pdf
- 10. US Food and Drug Administration. ICLUSIG® (ponatinib) tablets for oral use (2016). Accessed May 24, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/203469s022lbl.pdf
- 11. US Food and Drug Administration. Iclusig® (ponatinib) Tablets, 15 mg, 30 mg, and 45 mg. Accessed May 24, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2016/203469Orig1s022ltr.pdf
- 12. Hanley M, Diderichsen P, Rich B, et al. Exposure-response (ER) analyses of the optic interim analysis data to support the response-adjusted dosing regimen for Ponatinib (PIV-014). Clin Pharmacol Ther. 2021;109(Supplement S1):S66. [Google Scholar]
- 13. Cortes JE, Kim DW, Pinilla-Ibarz J, et al. Ponatinib efficacy and safety in Philadelphia chromosome-positive leukemia: final 5-year results of the phase 2 PACE trial. Blood. 2018;132(4):393-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dorer DJ, Knickerbocker RK, Baccarani M, et al. Impact of dose intensity of ponatinib on selected adverse events: multivariate analyses from a pooled population of clinical trial patients. Leuk Res. 2016;48:84-91. [DOI] [PubMed] [Google Scholar]
- 15. Mendizabal AM, Younes N, Levine PH.. Geographic and income variations in age at diagnosis and incidence of chronic myeloid leukemia. Int J Hematol. 2016;103(1):70-78. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.


