Abstract
Vaccination against COVID-19 is critical for immuno-compromised individuals, including patients with cancer. Systemic reactogenicity, a manifestation of the innate immune response to vaccines, occurs in up to 69% of patients following vaccination with RNA-based COVID-19 vaccines. Tumor regression can occur following an intense immune-inflammatory response and novel strategies to treat cancer rely on manipulating the host immune system. Here, we report spontaneous regression of metastatic salivary gland myoepithelial carcinoma in a patient who experienced grade 3 systemic reactogenicity, following vaccination with the mRNA-1273 COVID-19 vaccine. Histological and immunophenotypic inspection of the postvaccination lung biopsy specimens showed a massive inflammatory infiltrate with scant embedded tumor clusters (<5%). Highly multiplexed imaging mass cytometry showed that the postvaccination lung metastasis samples had remarkable immune cell infiltration, including CD4+ T cells, CD8+ T cells, natural killer cells, B cells, and dendritic cells, which contrasted with very low levels of these cells in the prevaccination primary tumor and lung metastasis samples. CT scans obtained 3, 6, and 9 months after the second vaccine dose demonstrated persistent tumor shrinkage (50%, 67%, and 73% reduction, respectively), suggesting that vaccination stimulated anticancer immunity. Insight: This case suggests that the mRNA-1273 COVID-19 vaccine stimulated anticancer immunity and tumor regression.
Keywords: COVID-19, tumor microenvironment, translational medical research, immunogenicity, vaccine, head and neck neoplasms
Introduction
Vaccines against COVID-19 are a promising approach to prevent and mitigate COVID-19. Overall, systemic reactogenicity events have been reported by 50% and 69% of patients after the first and second doses of RNA-based COVID-19 vaccines, respectively.1 These events, such as fever, headache, myalgias, and chills, are direct manifestations of the innate immune response to vaccination that results in the production and release of pyrogenic cytokines and inflammatory mediators, activation of complement, and recruitment of immune cells.2
Interestingly, spontaneous tumor regression following an intense immune-inflammatory response, usually triggered by a pathogen infection, has been recognized for centuries and guided the first steps toward immunomodulation of the microenvironment to treat cancer. The first reported immunotherapy against cancer was the inoculation of streptococcal organism into patients with unresectable sarcomas,3 and for over three decades, administration of the BCG vaccine to promote local inflammation has been used to treat non-muscle-invasive bladder cancer.
Here, we describe dramatic tumor regression in a patient with metastatic myoepithelial carcinoma of the parotid who experienced intense reactogenicity following the second dose of the mRNA-1273 COVID-19 vaccine.
Case report
In March 2020, a 61-year-old woman was diagnosed with a T2N0MX (AJCC cancer staging manual, 8th edition) myoepithelial carcinoma of the left parotid. She underwent left parotidectomy and postoperative radiotherapy (60 Gy) to the left neck and tumor bed. CT scans performed in July 2020, after treatment completion, revealed increase in size of bilateral pulmonary nodules suggestive of metastasis (figure 1A). A CT-guided biopsy of a lung lesion confirmed metastatic disease. Given the absence of curative-intent treatment for the metastatic disease, lack of standard systemic therapy for myoepithelial carcinoma, low disease burden, and lack of symptoms, the decision was made to proceed with close surveillance.
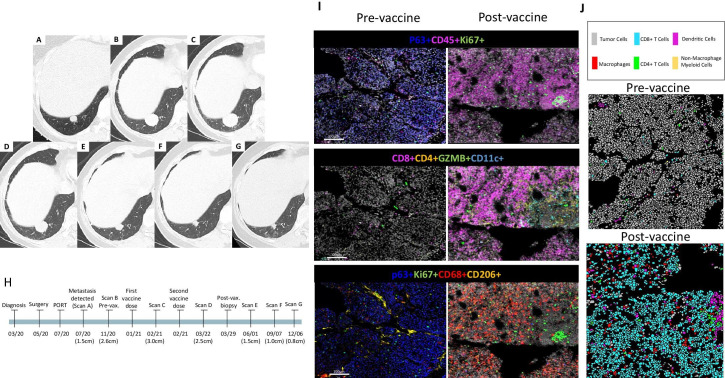
Figure 1.
Temporal overview of a metastatic nodule in right lower lobe at different timepoints, before and after COVID-19 vaccination with mRNA-1273. Other bilateral pulmonary metastases (not shown) have presented the same behavior overtime. (A) In July 2020, when metastasis was initially confirmed by biopsy, the nodule measured 1.4 cm. (B) In November 2020, the nodule measured 2.6 cm. (C) In February 2021, a few days after the patient received the first dose of the mRNA-1273 vaccine, the nodule measured 3.0 cm. (D) In March 2021, 1 month after the patient received the second dose of the mRNA-1273 vaccine, the nodule measured 2.5 cm. CT images acquired approximately 3 months (E), 6 months (F), and 9 months (G) after vaccination, show progressive decrease in size of the lesion, measuring 1.5 cm, 1.0 cm, and 0.8 cm, respectively. (H) The timeline at the bottom of the figure shows the timing of events. (I) Representative images demonstrating changes in tumor immune microenvironment composition of the primary parotid tumor (pre vaccine) and the lung metastasis (post vaccine; lung-met II) using imaging mass cytometry (750×750 pixels, length×width, respectively). (J) Imaging mass cytometry cell subpopulation clusters. PORT, postoperative radiation therapy; vax., vaccination.
In January 2021, approximately 10 months after the initial diagnosis of myoepithelial carcinoma, the patient received the first dose of mRNA-1273 COVID-19 vaccine. Adverse events reported were mild injection-site pain on day 1 and mild fatigue on day 2.
In February 2021, a surveillance CT scan of the chest showed a significant increase in the size of the pulmonary nodules compared with their size on the previous CT scan (figure 1B, C), obtained in November 2020. The decision was made to start systemic therapy in a clinical trial.
Later in February 2021, before systemic therapy was initiated, the patient received the second dose of the COVID-19 vaccine. Reported side effects were more severe than after the first dose: the patient reported a fever of 38.3°C and chills that started approximately 9 hours after vaccine administration and lasted for 2 hours. The patient also reported grade 3 fatigue, grade 2 myalgias, grade 2 muscle weakness, grade 2 headache, and mental fogginess; these symptoms persisted for 7 days after vaccination and then subside over an additional 7 days.4
Intriguingly, in March 2021, a CT scan of the chest revealed 13% shrinkage of the pulmonary nodules (figure 1D). Therefore, the decision was made to not proceed with the clinical trial treatment, which had been scheduled to start the day after the CT. A biopsy of a pulmonary nodule was performed at this point. Reverse transcription PCR tests for COVID-19 were performed prior to the CT of the chest and prior to the lung biopsy, both negative for COVID-19 infection.
Persistent tumor shrinkage was demonstrated on follow-up CT scans: 50%, 67%, and 73% reduction (figure 1E–G) at 3, 6, and 9 months, respectively, after the second dose of the vaccine. A timeline summarizing these events is shown in figure 1H. Therefore, we hypothesized that the tumor shrinkage was attributed to a systemic inflammatory response induced by the COVID-19 vaccine.
Methods
The patient gave written informed consent for analysis of tumor specimens and publication of this report. All CT scans were reviewed by the same thoracic radiologist. Details of tumor molecular profiling, including immunohistochemical analysis, targeted-exome sequencing, and imaging mass cytometry, are provided in the online supplemental.
jitc-2021-004371supp001.pdf (367.9KB, pdf)
jitc-2021-004371supp002.pdf (131.9KB, pdf)
jitc-2021-004371supp003.pdf (183KB, pdf)
Results
Molecular profiling and immunohistochemistry suggest a poorly immunogenic tumor
Molecular profiling performed with next-generation sequencing of the primary tumor sample revealed pathogenic somatic mutations in NOTCH3 and TP53 (online supplemental). The tumor was microsatellite stable and mutational burden was low (≤5 mutations/megabase). Histological analysis of H&E-stained sections revealed both primary tumor and lung metastasis prior to COVID-19 vaccination had rare and scattered immune cells restricted to the tumor border (online supplemental figure 1). Consistently, immunohistochemistry showed negative staining for PD-L1 (antibody clone 22C3).
jitc-2021-004371supp004.pdf (4.2MB, pdf)
Imaging mass cytometry reveals robust tumor immune cell infiltration following the second dose of mRNA-1273 vaccine
On histological and immunophenotypic inspection of the tumor samples, a massive inflammatory infiltrate with scant tumor clusters (<5%) embedded in was observed in the postvaccination lung biopsy specimen (online supplemental figure 1), suggesting that the tumor regression was associated with induction of an anticancer immune response.
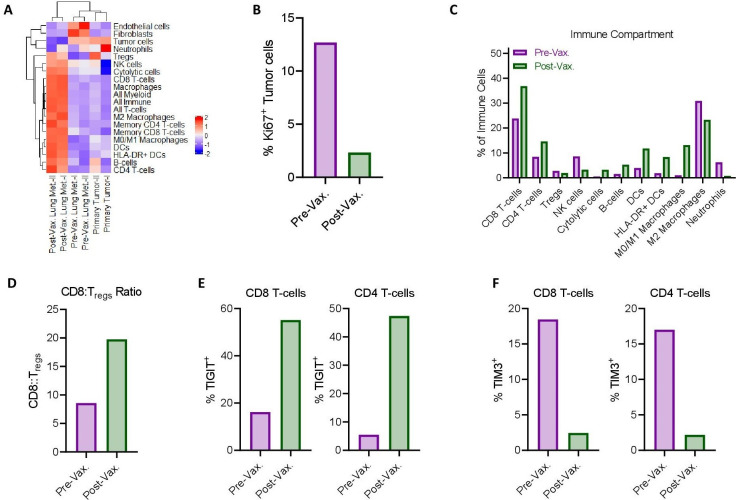
To comprehensively profile the tumor immune microenvironment (TIME), we performed highly multiplexed imaging mass cytometry on representative prevaccination (primary tumor and lung metastasis) and postvaccination (lung metastasis) samples (figure 1I–J). Notably, the postvaccination lung metastasis samples had remarkable immune cell infiltration, including infiltration by CD4+ T cells, CD8+ T cells, natural killer cells, B cells, and dendritic cells, which contrasted with very low levels of these cells in the prevaccination samples (figure 2A). As results for replicate biopsies for each condition clustered together, we pooled data for each condition for further analysis. In the tumor cell compartment, the fraction of proliferating tumor cells was reduced fivefold following vaccination (figure 2B). In the lung metastases, the postvaccination samples exhibited higher fractions of T cells, granzyme B+ cells, B cells, and dendritic cells (figure 2C), as well as a higher ratio of CD8+ T cells to regulatory T cells (figure 2D). In contrast, the prevaccination samples exhibited higher fractions of M2 macrophages and neutrophils (figure 2C). Further phenotypic analysis of T cells demonstrated that the percentage of cells expressing T-cell immunoglobulin and ITIM domain (TIGIT) was increased following vaccination (figure 2E), potentially indicative of antigen exposure.5 Conversely, the percentage of T cells expressing the inhibitory receptor T-cell immunoglobulin and mucin domain-containing protein 3 (TIM3)6 was decreased following vaccination (figure 2F). Taken together, these results suggest a robust anticancer immune response stimulated by COVID-19 vaccination with mRNA-1273.
Figure 2.
Imaging mass cytometry indicates robust anti-tumor immune response following COVID-19 vaccination. (A) Clustergram of imaging mass cytometry quantification in biopsy specimens from primary tumor and prevaccination (Pre-Vax.), and postvaccination (Post-Vax.) lung metastases (Lung Met.). I and II indicate specimens from different regions taken at the same time. Color axis represents each phenotype subpopulation frequency (z-normalized density [cells/mm2] values), red for high frequency and blue for low frequency or absence (−2); (B) Percentage of proliferative (Ki67+) tumor cells (pan-CK+ and/or p63+) in Pre-Vax. and Post-Vax. lung metastasis specimens. (C) Percentage of indicated immune cell populations as percentage of total immune cells in Pre-Vax. and Post-Vax. lung metastasis specimens. (D–F) Comparison of Pre-Vax. and Post-Vax. lung metastasis specimens for (D) ratio of CD8+ T cells to regulatory T cells (Tregs), (E) percentages of CD8+ T cells and CD4+ T cells positive for TIGIT, and (F) percentages of CD8+ T cells and CD4+ T cells positive for TIM3. +, positive.
Discussion
Severe hyperinflammatory response occurs in a fraction of patients with COVID-19.7 Similarly, COVID-19 vaccines have the potential to evoke intense immunologic responses.8 Here, we describe a case of an anticancer response after COVID-19 vaccination. Histology analysis and tumor molecular profiling suggested that the primary tumor was poorly immunogenic, which is associated with poor responses to the most commonly used cancer immunotherapy. Notably, the patient reported grade 3 systemic adverse events after the second dose of the COVID-19 vaccine, which was preceded by spontaneous tumor regression, indicating that an intense inflammatory host response stimulated by the vaccine may have promoted an antitumor response.
The changes we observed in the TIME between the prevaccination and postvaccination tumor specimens, including increases in CD8+ and CD4+ T cell tumor infiltration and granzyme B+ cytolytic cells, are associated with immune cell activation. Moreover, we found notable reduction in the absolute number of tumor cells and the fraction of remaining cells actively proliferating, indicating an effective anti-cancer response, consistent with the patient’s radiological findings.
CD8+ cytotoxic T cells have a pivotal role in the anti-cancer immune response; in fact, enhancing their activity is the main strategy of current successful cancer immunotherapies. Interestingly, although the efficacy of most vaccines is largely related to induction of antibody responses, T-cell-mediated immunity has emerged as an important mechanism of host defense against severe respiratory syndrome coronavirus-29; COVID-19 vaccine has been shown to induce both virus-specific antibodies and T-cell responses,9 which align with the TIME changes found in our analysis.
Dendritic cells, macrophages, and B cells are major populations of antigen-presenting cells critical for the initiation of adaptive immune response through T-cell activation, which is crucial for both vaccine-induced and anti-cancer immunity. Our finding of a substantial increase in antigen-presenting cell tumor infiltration in postvaccination samples is consistent with the robust innate and adaptative anticancer responses experienced by this patient.
Notably, we observed a shift in the TIME composition from myeloid predominant to lymphocytic predominant. Fractions of immune suppressive cells, represented by M2-macrophages, regulatory T cells, and cancer-associated fibroblasts, were higher in prevaccination samples than in postvaccination samples, which align with previous literature showing that immune suppressive cells are associated with immune evasion and worse prognosis in cancer.10 Finally, dysfunctional and exhausted T cells, represented by expression for TIM3,6 were also more prevalent in the pre-vaccination samples, whereas TIGIT expression in T cells was higher after vaccination and may be associated with T-cell activation.
In summary, this patient’s clinical course and the analysis of prevaccination and postvaccination tumor samples support the hypothesis that stimulation of the innate immune system by the mRNA-1273 COVID-19 vaccine induced systemic immune activation and led to a robust and persistent anticancer response, represented by radiological tumor shrinkage and an ‘anticancer’ TIME composition. To our knowledge, this is the first reported case of COVID-19 vaccine-induced tumor regression and the first report of spontaneous tumor regression in a patient with salivary myoepithelial carcinoma. Host and tumor characteristics that led to this phenomenon remain unclear.
Acknowledgments
We thank Stephanie Deming, scientific editor, Research Medical Library, for editing this article.
Footnotes
Twitter: @LGSousaMD
LGdS and DJM contributed equally.
Contributors: LGdS and DJM contibuted equally. All authors actively contributed to the manuscript development.
Funding: DJM was supported by NCI grant K99CA240689. This work was supported by the National Institutes of Health/National Cancer Institute under award number P30CA016672, which supports the MD Anderson Cancer Center Imaging Core Facility and Research Histology Core Laboratory. JB is further supported by the NCI’s Research Specialist 1 R50 CA243707-01A1. Bethyl Laboratories and Cell Signaling Technologies donated antibodies to the MD Anderson Flow Cytometry and Cellular Imaging Facility for use in IMC.
Competing interests: RF: reports personal fees from Regeneron-Sanofi, Ayala Pharmaceuticals, Prelude Pharmaceuticals, Bicara Therapeutics, Klus Pharma, Medscape, Carevive, Merck, and Guidepoint Global and institutional fees from AstraZeneca, Merck, Genentech, Pfizer, EMD-Serono, Ayala Pharmaceuticals, Prelude Pharmaceuticals, and Rakuten Medical not related to the topic of the submitted work.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Chapin-Bardales J, Gee J, Myers T. Reactogenicity following receipt of mRNA-based COVID-19 vaccines. JAMA 2021;325:2201–2. 10.1001/jama.2021.5374 [DOI] [PubMed] [Google Scholar]
- 2.Hervé C, Laupèze B, Del Giudice G, et al. The how's and what's of vaccine reactogenicity. NPJ Vaccines 2019;4:39. 10.1038/s41541-019-0132-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coley WB. The treatment of malignant tumors by repeated inoculations of erysipelas: with a report of ten original cases. Am J Med Sci 1893;105:487. [PubMed] [Google Scholar]
- 4.Guidance for industry: toxicity grading scale for healthy adult and adolescent volunteers enrolled in preventive vaccine clinical trials 2007. [DOI] [PubMed]
- 5.Chauvin J-M, Zarour HM. TIGIT in cancer immunotherapy. J Immunother Cancer 2020;8:e000957. 10.1136/jitc-2020-000957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolf Y, Anderson AC, Kuchroo VK. TIM3 comes of age as an inhibitory receptor. Nat Rev Immunol 2020;20:173–85. 10.1038/s41577-019-0224-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel P, DeCuir J, Abrams J, et al. Clinical characteristics of multisystem inflammatory syndrome in adults: a systematic review. JAMA Netw Open 2021;4:e2126456. 10.1001/jamanetworkopen.2021.26456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nune A, Iyengar KP, Goddard C, et al. Multisystem inflammatory syndrome in an adult following the SARS-CoV-2 vaccine (MIS-V). BMJ Case Rep 2021;14. 10.1136/bcr-2021-243888. [Epub ahead of print: 29 Jul 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhuang Z, Lai X, Sun J. Mapping and role of T cell response in SARS-CoV-2-infected mice. J Exp Med 2021;218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whiteside TL. The tumor microenvironment and its role in promoting tumor growth. Oncogene 2008;27:5904–12. 10.1038/onc.2008.271 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2021-004371supp001.pdf (367.9KB, pdf)
jitc-2021-004371supp002.pdf (131.9KB, pdf)
jitc-2021-004371supp003.pdf (183KB, pdf)
jitc-2021-004371supp004.pdf (4.2MB, pdf)