Abstract
Complex health policy challenges such as antimicrobial resistance and other emerging infections are driven by activities in multiple sectors. Therefore, addressing these also requires joint efforts from multiple sectors as exemplified in the One Health approach. We undertake a critical review to examine the different ways in which multisector partnerships have been conceptualized across multiple disciplines and thematic areas. We started with a set of six articles from the disciplines of health, nutrition and public administration that reviewed conceptual frameworks within their respective fields. We conducted backward citation tracing using the bibliography of the six articles to identify other articles in the same and related fields that conceptualized multisector partnerships. We identified 58 articles published from 1967 to 2018 from the fields of global health, infectious diseases, management, nutrition and sustainability sciences indicating that multisector partnerships have been a topic of study across different fields for several decades. A thematic analysis of the 58 articles revealed that multisector partnerships assume a variety of forms and have been described in different ways. Partnerships can be categorized by scope, scale, formality and strength. Multisector partnerships emerge in conditions of dynamic uncertainty and sector failure when the information and resources required are beyond the capacities of any individual sector. Such partnerships are inherently political in nature and subsume multiple competing agendas of collaborating actors. Sustaining collaborations over a long period of time will require collaborative approaches like One Health to accommodate competing political perspectives and include flexibility to allow multisector partnerships to respond to changing external dynamics.
Keywords: Multisector, intersectoral, collaboration, partnerships, integration, One Health, AMR
Key messages.
Multisector collaborations are complex political enterprises, which incorporate within themselves, different visions around, objectives, mandates, function and success.
Collaborations can take various forms which allow practitioners to choose the form of collaboration that is most relevant to their requirements.
Most collaborations consist of partners who pursue different individual and institutional agenda and who exercise different amounts of influence. Collaborations should learn how to manage rather than minimize these differences.
While there are no fixed parameters for success, given the dynamic contexts within which multisector collaborations function, they can result in unintended outcomes. Collaborations that are responsive to changing internal and external dynamics are more likely to thrive.
Introduction: need for review
About One Health
The ongoing coronavirus disease-2019 (Covid-19) pandemic has highlighted the importance of and need for multisector action for research, preparedness as well as response to pandemics (Häsler et al., 2020; Ruckert et al., 2020). Consequently, the last 2 years have seen multiple calls for One Health approaches to inform research as well as decision-making at the global level (Amuasi et al., 2020; Department of Health and Social Care, 2021).
The term One Health refers to an approach that seeks to foster interactions among animal, environment and human health sectors, as well as the disciplinary fields associated with them. Initially framed by conservationists in the context of wildlife-origin emerging infectious diseases in 2003, the concept of One Health quickly gained currency, especially in discussion related to pandemic preparedness (Osofsky et al., 2003; IMCAPI, 2010). It was adopted by a tripartite initiative of the Food and Agriculture Organisation (FAO), the World Organisation for Animal Health (OIE) and the World Health Organisation (WHO) as a way of mobilizing joint action, which expanded the ambit of One Health to cover enzootic infections and antimicrobial resistance (AMR) (United Nations, 2008; Food & Agriculture Organization, World Organization for Animal Health, World Health Organization, 2010).
While the term One Health is of recent coinage, the underlying ideas about mutual interdependencies of animal, environment and human health are not. For instance, the One Health approach draws from earlier convergence movements, such as One Medicine and Ecohealth approaches (Zinsstag et al., 2011; Woods et al., 2018). The reasons for repeated calls for One Health in the wake of zoonotic influenza earlier in the millennium, or more recently, AMR and pandemics are not hard to guess, as discussed below.
Wicked problems and One Health
The problems of zoonotic infections, pandemics and AMR have been referred to as key challenges facing humanity in the 21st century and associated with increased risks to global security, poverty, food security, health and development (Perry and Grace, 2009; Davies, 2013; De Bengy Puyvallée and Kittelsen, 2019; Laborde et al., 2020; Ottersen and Engebretsen, 2020). In addition to their magnitude, one of the peculiar challenges of zoonoses and AMR is that the problem emerges from and affects multiple sectors—such as pharmaceuticals, crop and animal agriculture, food processing, water resources and public health, among others. These sectors operate under different incentive structures and are informed from diverse disciplinary perspectives.
The problem of infectious diseases can therefore be framed from a variety of perspectives with often competing, sometimes incompatible, understandings. As such AMR and zoonoses can be viewed as ‘wicked problems’ whose solutions are difficult to clearly define (Waltner-Toews, 2017; Legido-Quigley et al., 2019). As is the case with other similarly deeply entrenched problems that lend themselves to multiple and incomplete characterizations—such as climate change—many believe combating AMR and zoonoses requires the presence of a ‘transdisciplinary imagination’ that can go beyond singular, incomplete perspectives offered within individual disciplines (Harris et al., 2010). In an institutional context, this has been referred to as ‘sector failure’—when the problem is beyond the capacity or complexity for one sector to handle alone (Bryson et al., 2006, p. 46). Acknowledging the multi-sectoral distribution of AMR, for instance, and its ability to spread rapidly across species and countries, Robinson et al. (2016) have termed it as a ‘One Health’ as well as a ‘One World’ issue. Actions to combat a problem that is both multi-sectoral and multi-dimensional in terms of cutting across disciplines require interdisciplinary response—One Health approaches, variously defined in Figure 1, would fit this description. Therefore, not surprisingly, the lead global agencies for global animal, environment and human health identified AMR and zoonoses as ‘Entry Points’ for a One Health approach (Food & Agriculture Organization, World Organization for Animal Health, World Health Organization, 2010), and the UK-funded Fleming Fund programme has adopted One Health as one of its underpinning principles for addressing AMR (UK Department of Health & Social Care, UK Aid, 2018, p. 5).
Figure 1.
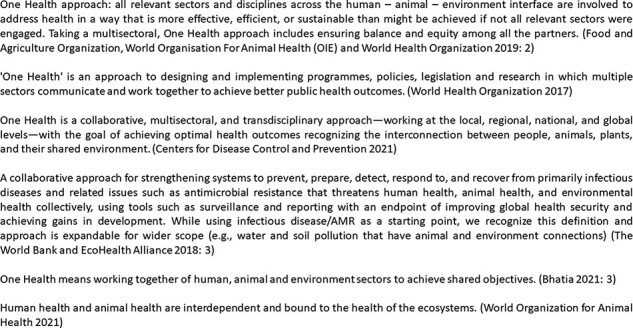
Definitions of One Health advanced by key international agencies
Challenges facing One Health
However, establishing multisector thinking underpinned by an interdisciplinary culture is often challenging as it runs counter to the established cultures of specialization and silo-based compartmentalizations prevalent within academic and governmental bureaucracies (Valeix, 2018; Surdez et al., 2021). This is perhaps why more than 17 years after the term ‘One Health’ was coined (Osofsky et al., 2003), its operationalization continues to be a challenge (Lee and Brumme, 2012; Okello et al., 2014) and there continues to be a strong demand for frameworks to operationalize the approach (United Nations, 2008; Centers For Disease Control and Prevention, 2010; The World Bank, EcoHealth Alliance, 2018; Food and Agriculture Organization, World Organisation For Animal Health (OIE), World Health Organization, 2019).
Most One Health guidelines promote formal, institutional collaborations and a singular health-dominated agenda for action. The increased demand for One Health programmes is in contrast with the limited nature of discussion around the attributes, quality or drivers of One Health collaborations. This simplistic understanding of collaborations runs the risk that One Health is seen more as rhetoric than a series of actions leading to practical solutions (de Garine-wichatitsky et al., 2020).
The differences in the expectations from One Health are borne out of the definitions of One Health advanced by major international agencies which can be assumed to be representative of their respective sectoral interests (see Figure 1). For instance, the Centers for Disease Control and Prevention and WHO definitions of One Health emphasize public health achievements as shared outcomes for One Health partners (World Health Organization, 2021; Centers for Disease Control, 2021). The World Bank definition also gives primacy to global health security but allows for expanding the scope to other non-health outcomes for One Health (The World Bank, EcoHealth Alliance, 2018, p. 3). The definitions from the two non-health agencies, the FAO and OIE, go beyond purely health outcomes and adopt a more open-ended note. While the FAO definition cites ‘shared objectives’ instead of health outcomes, the OIE definition merely recognizes the interconnectedness of different sectors without specifying specific outcomes (Bhatia, 2021; World Organization for Animal Health, 2021). These definitions seem to reflect the remit and interests of their respective organizations and varying levels of interest in purely human health outcomes. Not surprisingly, the apparent lack of clarity in One Health vision has led many commentators to highlight the ‘moral dilemma of One Health’; i.e. whose world and whose health does the framing seek to capture (Galaz et al., 2015; MacGregor and Waldman, 2017; van Herten et al., 2019)?
The limited nature of theorization of collaborations is not unique to AMR or One Health alone, but extends to other avenues for intersectoral action involving health sector as well (Hendriks et al., 2014; Chircop et al., 2015; Dubois et al., 2015; Glandon et al., 2019). Given the limited theorization of collaboration within One Health literature, we cast a wide net to conduct a broad-based review across the disciplines of global health and public administration. In this critical review, we aim to identify what are the different conceptual understandings around collaboration and discuss their relevance to discussions around AMR and zoonoses control.
Accordingly, we have structured the paper in three sections. The Methods section describes and justifies the choice of study design, search strategy, inclusion criteria and analysis plan. The following section on Results describes how multisector collaborations have been discussed in literature around the themes of infectious diseases, global health, nutrition, management studies and public administration. The Discussion section leads with an examination of the diversity and categorization of collaborations. This is followed by a discussion of key drivers of multisector collaborations as viewed from a complex systems lens. The last part of Discussion returns to the themes of AMR and One Health and reflects on possible lessons for developing the field of One Health science and practice.
Methods
Critical review
We use a critical review design to examine the different ways in which multisector collaborations have been conceptualized across multiple disciplines and thematic areas. While standard systematic reviews require a precisely formulated question which are mostly directed towards establishing treatment effect or causality, they do not lend themselves to critically appraising the assumptions and perspectives informing individual studies (Grant and Booth, 2009; Higgins et al., 2019). We found critical reviews to be better suited for our study since our ambition was to hold up ‘each work against a criterion’ and not to ‘summate conclusions or compare the covered works one to another’ (Cooper and Hedges, 2009, p. 5).
This review focusses on conceptual understandings of collaborations, which could help us draw inferences for AMR and disease control policies. Since we were starting from a point of relatively limited theorization and as we were surveying literature from a broad set of areas adopting a critical review approach allowed us to conduct a broad survey of the extant literature ‘to reveal weaknesses, contradictions, controversies, or inconsistencies’ (Paré et al., 2015, p. 190).
Search strategy
The review is not meant to be exhaustive; rather it casts a wide net to capture a breadth of understandings around cross-government collaborations and discuss their relevance to disease control in Low and Middle Income countries (LMICs). We use a selective search strategy with the intention of capturing more visible papers across several disciplinary fields and supplemented these with backward citation tracing.
Citation searching can provide a supplementary or an alternative search strategy to the standard keyword-based search techniques. These are of two types. Backward citation tracing uses the bibliography from a source study to identify additional studies. This is opposed to a ‘forward citation tracing’ which traces articles citing the source study (Briscoe et al., 2020). Citation tracing helps consolidate searches from multiple studies and is therefore likely to yield increased and better-quality search results when compared to structured keyword-based searches (Kuper et al., 2006; Hinde and Spackman, 2015; Hirt et al., 2020).
Citation searches can be especially useful when the core concepts are difficult to define or have been variously defined, as we posit has been the case with multisectoral One Health collaborations (Briscoe et al., 2020). These can be a powerful tool for explorative analysis for small bodies of literature (Akin, 1998). In addition, starting citation searches from an index review tends to yield a limited and relevant body of literature (Kuper et al., 2006).
Accordingly, we started with a small set of papers from a broad set of fields that included global health (infectious diseases, social determinants and nutrition) and public administration disciplines (see Table 1). These were purposively selected articles that reviewed a body of conceptual literature within their respective field as well as presented their own depictions of multisector collaborations. These represented the starting points of our inquiry which would allow us to broaden the scope of our review and overcome the limitations of a backward citation tracing. We then identified the papers cited in the reviews (backward citation tracing) to locate additional papers within their respective fields. These searches were conducted between June 2019 and January 2020.
Table 1.
Review articles selected for backward citation tracing
| Review paper | Domain |
|---|---|
| (Emerson, 2018) | Health and Public Administration |
| (Glandon et al., 2019) | Health (Health systems research) |
| (Harris and Drimie, 2012) | Nutrition |
| (Kuruvilla et al., 2018) | Health (Maternal and Child Health) |
| (Mahlangu et al., 2019) | Health (HIV/AIDS and Public Health) |
| (Thomson et al., 2007) | Public administration |
Inclusion criteria
While recognizing that multisector collaborations might assume different forms, including ad hoc and informal ones, for the purpose of this review, we restricted ourselves to literature around formal, institutional modes of collaborations. This was to reflect the priorities of current One Health guidelines from international technical agencies which promote institutionalized partnership mechanisms (World Health Organization, 2015).
The second inclusion criterion related to conceptual contributions. Original research studies, monographs, reviews, technical reports as well as conceptual papers were all included in the review as long as they contributed to conceptualization of dynamics of multisector collaborations—such as processes, drivers and outcomes. Empirical studies that did not generalize their findings beyond their immediate context were not included.
Since a substantial number of references were published books or programme documents, we excluded those publications whose full text could not be accessed.
Thematic analysis
Thematic analysis offers a flexible approach to organizing and describing qualitative data. In addition, it also allows the researcher to identify patterns and perform interpretations (Braun and Clarke, 2006; Nowell et al., 2017). We used thematic analysis to first organize the data based upon the key domains or topics addressed within them. This allowed us to describe the broad trends on how multisector collaborations have been addressed within the field and identify the key concerns that these debates set out to address.
We describe key debates around multisector collaborations with the fields of infectious diseases, global health (including the topics of women’s and children health, and social determinants of health), nutrition, management studies and public administration. This list of fields does not exactly tally with the domains of the initial list of six articles (Table 1) since we had to accommodate a number of papers and the richness of debates in different often overlapping fields.
The next focus of our inquiry was on examining the diversity of collaborations covered in the literature. We found different ways in which collaborations have been described and chose to focus on two categorizations (formality and strength). Finally, we wanted to understand the functioning of the collaborative process itself. This included an examination of the structure of the collaborative systems—and using a temporal lens—to assess how collaborates originate, operate and sustain. We used the shortlisted publications to structure our inquiries and supplemented these with additional literature as we proceeded to develop our explanations.
Results
Literature landscape
As described in Figure 2, our search generated an initial long list of 344 publications. From these we excluded duplicate references (18) and inaccessible publications (50). The relatively large number of inaccessible publications can be explained by a substantial number of books (30), technical reports (12) and conference presentations (5), included in this figure, which were not accessible electronically.
Figure 2.
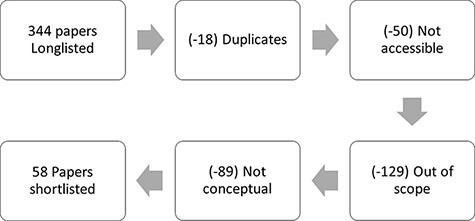
Identifying publications for review
A total of 129 papers were found to be out of scope of our review. These included methodological, contextual or reference literature and did not contribute to conceptual discussions on collaborations. Finally, 89 publications were excluded which were mostly empirical studies or made general observations on collaborations.
While it is difficult to strictly classify the disciplinary fields for these publications, based upon a loosely applied categorization, most of the shortlisted research publications appear to be from public administration and related field of management studies. Most of the publications were published recently; this includes more than half the papers which were published over the last decade (Table 2).
Table 2.
Distribution of shortlisted papers, by domain and decade
| Domain | Publications | Decade | Publications |
|---|---|---|---|
| Public administration | 26 (45%) | 1960–1969 | 1 (2%) |
| Health | 13 (22%) | 1990–1999 | 8 (14%) |
| Management | 12 (21%) | 2000–2009 | 19 (33%) |
| Sustainability sciences | 4 (7%) | 2010–2019 | 30 (52%) |
| Nutrition | 3 (5%) | 2020–2021 | 0 (0%) |
| Total | 58 (100%) | Total | 58 (100%) |
Depictions of multisector collaborations
The idea of multisector collaborations has been variously referred to by related terms such as integration, partnerships and collaboration as well as multi-sector and inter-sector. All these terms refer to related but distinct concepts of working together. In some cases, collaborations are considered akin to partnerships (World Health Organization South East Asian Regional Office, World Health Organization Western Pacific Regional Office, Food & Agriculture Organization et al., 2008) and integration as a more ‘joined-up’ way of working (Davies, 2009; Exworthy and Hunter, 2011). In other contexts, multisectorality refers to a more prescriptive form of alignment of different agendas towards a common goal (Shankardass et al., 2015). Even what is referred to as sectors in ‘multisectoral’ varies a lot. As in the case of One Health or nutrition, sectors could refer simultaneously to economic spheres of activity or to different corresponding disciplines (Parkes et al., 2005; The World Bank, 2013; Okello et al., 2014). In other contexts, sectors could refer to the ownership of the institutions—such as state, non-governmental organizations and citizens, as in the case of collaborative governance literature (Tennyson and Wilde, 2000; Emerson et al., 2012). Finally, while we feel there are differences between multisector and intersector approaches (see Figure 4), in much of programmatic literature they have been used interchangeably (World Health Organization, 2018).
Figure 4.
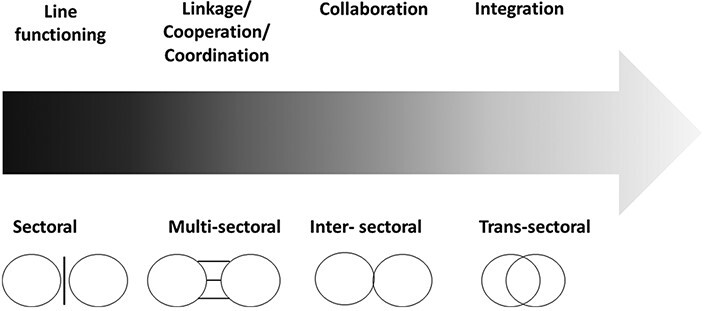
Types of collaborations, by strength; adapted from Harris and Drimie (2012, p. 2)
Therefore, given the lack of established typologies around multisector collaboration, we have considered all the above labels as referring to similar ideas for the purpose of this review. This section explains the different ways in which the multisector collaborations have been addressed in literature relating to infectious diseases, nutrition, global health, management studies and public administration.
Infectious diseases
Given the ubiquitous nature of infectious diseases, the tendency of microbes to cross geographic and species boundaries was well understood from the beginnings of modern medicine (Schultz, 2008; Woods, 2017). It is therefore not surprising that discussions around multisectorality have taken place widely, and for long, across different pathogens. As described below, this includes discussions around integrated disease surveillance, food-borne diseases, Neglected Tropical Diseases (NTDs), Zoonoses, Emerging Infectious diseases (EIDs), Antimicrobial resistance (AMR) as well as Human Immunodeficiency Virus (HIV)/Acquired Immune Deficiency Syndrome (AIDS); at a historical level, the successful eradication of zoonotic diseases such as brucellosis from cattle herds in North America and Europe and the control of tuberculosis in cattle in the same regions. These were multisectoral efforts brought about through crisis or recognition by the private sector that coordination was needed (Olmstead and Rhode, 2015).
The early 2000s witnessed a worldwide push for ‘integrated’ disease surveillance efforts that brought together activities across different diseases, and also, across health and non-health sectors (WHO et al., 2003; Calain, 2007). This was a time when the next pandemic was widely anticipated, and global health agencies had started recognizing the limitations of recognizing the limitations of the pathogen-based funding models which were then prevalent (Shiffman 2006). While the surveillance programmes were very much health centric, the literature on infectious diseases and integration recognized the role of non-health factors in disease causation and the importance of addressing these (Atun et al., 2010; Shigayeva et al., 2010). Similarly, the notion of working with non-health sectors to address NTDs was the motivation for a framework conceptualizing a gradient of progressively stronger collaborations, later also reflected upon by Harris and Drimie (2012) in the context of nutrition (Grépin and Reich, 2008).
The increasing awareness of social origins of HIV/AIDS prompted early thinking on engagement with non-health sectors (Marks, 2002; O’Neil et al., 2004). While many innovative approaches were developed for identifying and engaging with non-health sectors, the objectives of these programmes were largely restricted to outcomes focussed upon single pathogens and within health sector alone (Kar, 2014; Mahlangu et al., 2018). The unique visibility of HIV/ADS programmes, however, resulted in distortion of local health systems priorities in many affected countries (Biesma et al., 2009; Sherr et al., 2012), which was a major factor in call for integrative health systems wide support and integration with local health priorities (Frenk, 2009; Shakarishvili et al., 2009; Gyapong et al., 2010).
Alongside the above discussions, other convergence movements gathered momentum around infectious diseases. Prominent among these included the Ecohealth movement. It drew connection between human health with different components of ecosystems, including biological and physical environment (Schwabe, 1984; Parkes et al., 2005; Waltner-Toews and Kay, 2005; Charron, 2012). This was closely related to the newly launched One Health approach (Zinsstag et al., 2011). The term ‘One Health’ itself was coined in 2003 and was largely framed as a response to potential threats from wildlife-origin diseases emanating from the risk hotspots of the global south (Leach et al., 2010; Cassidy, 2018).
As pointed out earlier in the paper, much of the One Health literature is still concerned with establishing the need for collaboration (The World Bank, 2010; 2012; Gebreyes et al., 2014), or in advancing standardized frameworks for implementation (World Health Organization South East Asian Regional Office, World Health Organization Western Pacific Regional Office, Food & Agriculture Organization et al., 2008; The World Bank, EcoHealth Alliance, 2018; Food and Agriculture Organization, World Organisation For Animal Health (OIE), World Health Organization, 2019). While there have been some attempts at theorizing One Health such as by the use of socio-ecological models (Wilcox and Kueffer, 2008; Zinsstag et al., 2011; Rüegg et al., 2018a), thinking around the politics and mechanics of One Health continue to lag behind (Lee and Brumme, 2012; Hinchliffe, 2015; Ssennyonjo et al., 2021). Human health priorities tend to dominate most discussions around One Health, and most benefits are still assessed from human health perspective, even in ostensibly One Health analysis (Zinsstag et al., 2007; Fitzpatrick et al., 2016).
Global health
Some of the strongest calls for multisector engagement from the health sector have come from work done on social inequalities, specifically around the social determinants of health (Commission on Social determinants of Health, 2008; Public Health Agency of Canada, Commission on Social Determinants of Health, Regional Network for Equity in Health in East and Southern Africa, 2008). These calls for intersectoral action were reframed by Finland during its European Union presidency as a call to include ‘Health in All Policies’ in 2006. This eventually led to the Helsinki statement during the 8th Global Conference on Health Promotion in 2013 (Puska, 2007; Greszczuk, 2019).
However, despite the visibility of the approach, Health in All Policies has frequently faced implementation challenges. An examination of the governance challenges facing the approach recommended going beyond rigid bureaucracies and adopting a collaborative style of governance (Mcqueen et al., 2012). A recently published assessment identified several challenges to the Health in All Policies approach, such as mismatched incentives and competing priorities of collaborating partners within which it was easy to get the focus on health equity diluted (Greszczuk, 2019). Shankardass et al. (2015), (2018) proposed using systems theory and realist evaluations to characterize the complexity of multi-agency collaborations and capturing the tensions noted above.
The explicit focus on partnerships and convergence within the SDGs, along with the insights from earlier debates described above, have helped inspire a range of new scholarly efforts to think about intersectoral action within the context of child health (Blomstedt et al., 2018; Kuruvilla et al., 2018) and health systems research domains (Dubois et al., 2015; Rasanathan et al., 2015; 2017; Bennett et al., 2018; Graham et al., 2018). Arguably, the key advance in some of these efforts has been increased reflection on the theory (Glandon et al., 2019) as well as incorporation of insights from non-health disciplines including public administration (Rasanathan et al., 2017; Emerson, 2018).
For instance, Glandon et al. (2018), (2019) aimed to develop a research agenda around multisector collaborations. While their initial study on research priorities found a long-held and widespread interest in studying multisector collaborations from a wide range of disciplines and geographies, they found that fundamental questions about initiation, composition, functioning and governance of multisector collaborations remained unclear. Their follow-up study identified the need for development of more theory-driven and outcome-focussed research, and for critical examination of the motivations of collaborating partners within multisector collaborations (Glandon et al., 2018; 2019). Kuruvilla et al. (2018) conducted a theory-driven analysis of 12 country case studies of multisector collaborations to identify the different forms such collaborations could take and develop a model outlining the enabling factors that allowed multisector collaborations to respond to changing external context and internal dynamics.
Nutrition
As a sector that has to interact closely with agriculture and health, nutrition has had a long history of promoting and participating in multisector platforms. Indeed, some of the earliest examples of large-scale integrated programmes came from nutrition, such as the Integrated Child Development Services programme in India (Rajivan, 2006). Multisector collaborations had already had a long history by the 80s, when nutrition scholars were debating the possible ‘demise’ of and relative merits of ‘multisector planning’ in nutrition (Berg, 1987).
Perhaps because of their long-standing practical exposure to collaboration, many nutrition scientists advocate nuanced perspectives on multisectorality. While recognizing the arguments of efficiency and effectiveness underpinning justifications for multisectoral collaborations in nutrition, they point to strong cultural challenges facing such initiatives. Harris and Drimie (2012, p. 1) highlight the presence of many nutrition-specific interventions that tend to be ‘owned’ by health department. This has resulted in many multisector efforts to be conducted piecemeal within individual sectors (Garrett and Natalicchio, 2011, p. 8). However, these scholars also point to the presence of small, under-analysed examples of multisector efforts whose lessons for mechanics of multisector collaborations need to be better understood.
Management studies
Much work around collaborations within private sector management has occurred around team management (Gratton and Erickson, 2007). However, there is a rich vein of literature unpacking the practical elements of collaborations by social management and organizational management scholars.
The efficiency motivation behind collaborations is frequently cited to make a case for donor alignment or for multiple institutions to work together as in the case of PPPs or collaborative management (Kalegaonkar and Brown, 2000; Tennyson, 2003).
Another discussion strand within the management discipline has been around recognizing the differences in powers and interests within collaborating partnerships and how to approach building agreements using consensus-driven and power-aware approaches (Innes, 1999; Brouwer et al., 2013).
Recognizing the challenges involved in creating and sustaining collaborations across organizations, some management scholars describe these as ‘collaborative inertia’. On the other hand, if collaborations are nurtured by addressing issues of conflicting aims, power dynamics and fostering trust, for example it is possible to achieve ‘collaborative advantage’ or a state of synergy that organizations can aspire towards when working together (Huxham, 2003; Huxham and Vangen, 2004; Lank, 2006). They also recognize the transformative potential of such collaborations and offer practical ways for organizations to instil a culture of collaboration (Brouwer et al., 2016).
Public administration
As a discipline that is tasked with the study of ‘organization and management practices in collective or public settings’, public administration scholars have unsurprisingly been studying multisector collaborations deeply and more widely than other fields (Frederickson et al., 2012, p. 1)—an early attempt to develop a theory for collaborations being in 1991 (Gray and Wood, 1991; Wood and Gray, 1991).
Much of the work in the field in the last few decades has led to the recognition of the limitations of the state as an actor. This has accompanied an increasing recognition of the importance of engaging non-state actors, such as civil society organizations, private sector and academia in public policy planning and implementation (Peters and Pierre, 1998; Bourgon, 2011).
This has resulted in new thinking around collaborative public management (McGuire, 2006) and intergovernmental or interagency collaboration (Hudson et al., 1999; Agranoff, 2007; 2013) that seek to encourage local governments to engage with governmental and non-governmental stakeholders (Crosby and Bryson, 2005; Bryson et al., 2006; Page et al., 2015).
As discussed in the section on systems thinking below, many of these scholars have theorized multisector collaborations as complex systems, which has resulted in new insights on how to develop a typology, drivers and elements of such collaborations (Crosby and Bryson, 2005; Bryson et al., 2006; Ansell and Gash, 2007; Emerson et al., 2012; Emerson and Gerlak, 2014; Emerson and Nabatchi, 2015; Page et al., 2015).
Discussion
We have structured the Discussion section in three parts. The first part discusses possible typologies of multisector collaborations. The second part examines possible drivers of multisector collaborations informed by a complex system understanding of collaborations. The last part draws upon the collaboration literature in other fields to draw lessons for the One Health movement.
Collaborations come in different shapes and sizes
Based on an examination of the literature around collaborations cited above, it is clear that the concept has been continued to be discussed in different ways across multiple disciplines and applications. To cite an example, even as Berg and Field were debating the strengths and limitations of multisectoral approaches in nutrition in late eighties (Berg, 1987; Field, 1987), around the same time Gray and Wood were putting together a special journal issue aimed at developing a comprehensive theory of collaborations (Gray and Wood, 1991; Wood and Gray, 1991).
Multisector collaborations have been characterized in many ways in the reviewed literature. The different descriptors can be broadly grouped under four different ways, depicted in Figure 3. Two relatively straightforward ways to categorize collaborations are by describing the scale and scope of their activities. Collaborations can be termed as international, national or subnational depending upon the sphere of their activities, for instance. Similarly, collaborations can also be said to focus on programme, policy or research depending upon their scope of functioning.
Figure 3.
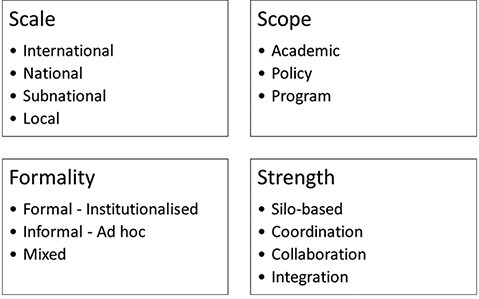
Different ways of characterizing multisector collaborations
The above two ways of categorizing collaborations have the advantage of describing the nature of activities of collaborative enterprises. However, these classifications do not shed any insights on the inner processes of the collaborations themselves, such as the factors precipitating and sustaining collaborations. The two other ways of classifying collaborations—based on their formality and strength can be more informative in this regard, as explained below.
Degree of formality
Even though most analyses of collaborations recognize how collaborations are underpinned by inter-personal dynamics (Agranoff, 2006; Bryson et al., 2006; McGuire, 2006; Ansell and Gash, 2007; Harris and Drimie, 2012) and are shaped by institutional and social norms (Emerson, 2018), the importance of informal collaborations remains a topic of ongoing debate. While some argue about the importance of informal relationships (Bryson et al., 2006; Chenard, 2007), and recognize that formal and informal components are both parts of the ‘collaborative black box’ (Thomson and Perry, 2006), others label informality as ‘Organizational individualism’ that are not appropriate for institutional collaborations (Hudson et al., 1999).
Some management scholars provide a more sophisticated view of formality. For instance, Tennyson (2004, p. 14) recognizes that there can be degrees of informality within collaborations and that there would be relative pros and cons of different levels of formality. An examination of One Health collaborations in India found that formal and informal collaborations often go hand in hand. Formal collaborations are often underpinned by the leadership and agency from participating members, while informal collaborations seldom persist without some level of tacit approvals from the bureaucracy (Abbas, 2018).
Strength of integration
Harris and Drimie (2012) propose a scheme of categorizing collaborations by their strength of integration that resonates with several other conceptualizations of multisector collaborations as well (Kalegaonkar and Brown, 2000; Boon et al., 2004; Grépin and Reich, 2008; Shigayeva et al., 2010).
As described in Figure 4, which is adapted from Harris and Drimie (2012, p. 2), all multisector engagements can be placed on a gradient of progressively more integrative partnerships. This gradient starts from the left where sectors continue to work in individual silos. This leads on to the stage of cooperation or coordination which might involve exchange of information, and possibly joint planning with each sector conducting its own activities in the field independently and maintaining strong sectoral boundaries. The next stage of collaboration moves beyond unstructured cooperation or coordination to conducting joint operations in the field, and even exchange of personnel and use of shared resources. The last stage is termed as integration which is characterized by the physical merging of resources and a blurring of the sectoral boundaries both in terms of resources, as well as sectoral remits.
It is important to note here that the categorizations discussed above provide a vocabulary to help us characterize the diversity in different collaborations and do not imply a value judgement on the desirability or preference for a certain kind of partnerships. It is possible that traditional sectoral boundaries might work better in some contexts than in others, depending upon local institutional and political cultures. Instead, we intend to use these categorizations to make the case against adopting a one-size-fits-all approach and for highlighting the need for designing collaborations that are more relevant to their immediate contexts.
Systems view of multisector collaborations
Multisector collaborations have been frequently described as complex systems consisting of multiple independent parts (Thomson and Perry, 2006; Ansell and Gash, 2007; Emerson et al., 2012; Shankardass et al., 2015; Rüegg et al., 2018b; Mahlangu et al., 2019). This depiction allows us to impose a sequential flow on different collaborative processes—described in one instance as: initiation, consolidation and reflection (Brouwer et al., 2016), or initiation, coordination and durability (De Leeuw, 2017). Others use a systems approach to describe the drivers of collaborations from the lens of inputs, process and outcomes (Thomson et al., 2008; Emerson et al., 2012).
Once we can look past the different sets of terminologies used, there is considerable thematic overlap among the frameworks on the antecedent, starting conditions or system contexts that give rise to collaborations. It is generally accepted that collaborations are initiated or precipitated in crisis situations (Tennyson, 2003) to take advantage of power-resource-knowledge asymmetries among the partners in such a way that the collaboration becomes greater than its sum. Initial trust levels including any prehistory of cooperation or conflict are all useful predictors of collaboration (Ansell and Gash, 2007; Thomson et al., 2007; Emerson et al., 2012).
Emerson et al. (2012) provide possibly the most granular understanding of the collaborative process itself. They distinguish between drivers and system contexts as those responsible for initiating collaborations and describe collaborative dynamics as consisting of principle engagement, shared motivation and capacity for joint action. They also link collaborations to adaptive capacities and provide a typology of outputs and outcomes expected from successful collaborations. In this conceptualization the outputs are focussed on the immediate products from the collaboration focussed on the task at hand. On the other hand, the collaborative outcomes and impact will influence changes at a systemic level, and ultimately lead to some form of adaptation (Emerson and Gerlak, 2014; Emerson and Nabatchi, 2015).
This broadly echoes Thomson and Perry (2006, p. 21) assertion, citing other scholars, that outcomes from collaborative undertakings not only include the achievement of immediate goals, but also a transformation of instrumental transactions among organizations into socially embedded relationships; the creation of ‘new value partnerships’ and ‘self-governing collective action’ (Ostrom, ; Ring and Van De Ven, 1994; Sagawa et al., 1999). These insights have implications on what we understand as successful collaborations, and an acknowledgment of the transformative potential of multisector collaborations, as explained below in the section on sustaining collaborations.
Principles of multisector collaborations
Many frameworks in the reviewed literature adopt a systems approach for describing multisector collaborations. This means that collaborative process is often categorized into development and operational phase, with different sets of factors driving both (Chen, 2010; Tonelli et al., 2018). As mentioned below, there is limited discussion in the literature regarding identifying the expected outcomes of collaborative process itself, which means there are still open-ended questions regarding the long-term ‘success’ of collaborations (Bryson et al., 2006; McGuire, 2006; Ansell and Gash, 2007; Emerson et al., 2012).
Following the conceptual frameworks mentioned in the key publications, we have described below some of the factors of multisector collaborations, grouped into three phases of collaborative process.
Development of collaborations
The conventional wisdom around formal collaborations mentions having a common goal, well-developed prior relationships and ring-fenced objectives. However, most conceptual analysis of multisector collaborations discusses instead the principles of mutual interdependency and complementarity among collaborating partners.
Tennyson et al. (2008, p. 16) describes the need for common vision as an ‘enduring myth’ around collaborations. Instead, many researchers of collaboration posit that even when partners come together to collaborate, they do so only to pursue their individual organizational aims. This usually happens when they are compelled to come together by extraordinary circumstances, such as sector failure (Bryson et al., 2006) and uncertainty (Emerson et al., 2012).
Thus, collaborations tend to work best when the strengths and weaknesses of collaborating agencies complement each other and created mutual interdependencies (Bryson et al., 2006; Ansell and Gash, 2007). This provides strong institutional incentives for collaborations to sustain even in the absence of individual champions.
Performance of collaborations
Once a collaboration comes into existence, the next challenge is to ensure its performance. In the absence of prior relationships, some argue, trust and a sense of achievement can be built by a series of small wins and informal deals that do not require much trust (Bryson et al., 2006; Ansell and Gash, 2007). The collaborative process tends to be iterative (Ansell and Gash, 2007) involving discovery, definition, deliberation and determination (Emerson et al., 2012).
Observations from cases of collaboration often highlight the role of charismatic leadership as a facilitator (Hudson et al., 1999; Ivery, 2010; Brouwer et al., 2016). Yet, it is possible to break this quality down. Indeed, according to some, it is essential to move beyond the notion of individual charisma if the collaboration is to be sustainable (Tennyson, 2003). Leadership of collaborations require skills in boundary spanning (Quick and Feldman, 2014; Pelletier et al., 2018) and knowledge brokering (Bay et al., 2016; Hitziger et al., 2018) to facilitate communication and compromise across different knowledge systems Also importantly, leaders need to recognize power hierarchies that appear in any group so that they can actively address these to ensure multisectoral action (Purdy, 2012; Brouwer et al., 2013). Ran and Qi (2018, p. 836) are more direct when it comes to power hierarchies and state that ‘instead of focusing on the attempt to balance power and share power in collaboration, it will be more fruitful to design and implement collaborative arrangements based on the dynamic contingencies’.
Sustaining collaborations and building resilience
Unlike the descriptions on antecedents and processes of collaborations, discussion is more sparse on the outcomes expected from collaborative processes. This is possibly a reflection of the instrumental nature of most collaborations where the focus is on immediate deliverables rather than longer-term changes. Most sector-specific literature focus on immediate outcomes such as nutritional status (Levinson and Balarajan, 2013) or on surveillance outputs (Ogyu et al., 2020). It can be argued that while these ring-fenced outcomes might allow the goals to be clearly visualized, these run the risk of artificially smoothening the diversity of interests and agendas at play in a multisector collaboration. Huxham and Hibbert (2008) point out that over the course of their activity, collaborations might result in unanticipated results and outcomes flowing from changed external dynamics or as a result of negotiation within the collaboration itself. In such a situation, those collaborations are likely to thrive that have the space to innovate and seize opportunities (Thomson and Perry, 2006; Tennyson et al., 2008).
On the other hand, there is also evidence to show that both congruence as well as divergence in goals might contribute to success of the collaborative enterprise depending upon the local context (Vangen and Huxham, 2012).
Several scholars argue for the need to institute at least limited autonomy within collaborating partners to allow them to redefine their objectives in light of changing circumstances as well as to allow them to navigate their organization aims (which might have limited overlaps with other partners) (Thomson et al., 2008; Emerson and Gerlak, 2014; Brouwer et al., 2016). If a collaboration does not have the space to go beyond its foundational terms of reference, the collaboration itself is likely to die out when the terms become out of sync with external environment (Ramalingam et al., 2008).
This body of work links collaborative governance with adaptive governance (Dietz et al., 2003; Emerson and Gerlak, 2014). As depicted in Figure 5, increased adaptive capacity brought about as a result of multisector collaborations, in turn, is expected to increase the responsiveness and resilience within SES systems (Duit et al., 2010).
Figure 5.
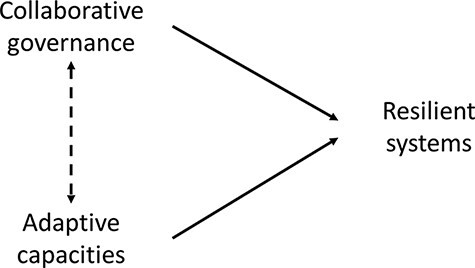
Collaborative systems are resilient systems
On the other hand, adaptive capacities have been associated directly to increasing resilience (within SES). Investing in genuine multisector collaborations and allowing them room to innovate is likely to yield into increasing the responsiveness and resilience of their constituent systems (Dietz et al., 2003; Folke et al., 2005; Duit et al., 2010; Quick and Feldman, 2014).
Implications for the field of One Health
Lessons for One Health science
Having examined the literature around collaborations from other fields, we now return to the domain of One Health. In this section we identify insights from the reviewed literature to examine how we can think about and practice One Health. The complex-systems understanding of multisector collaborations in other fields has broad resonance within One Health as well.
The field of ecosystems approaches to health—which have overlaps with One Health community (Zinsstag, 2012)—has a longstanding tradition of using a socio-ecological lens (Waltner-Toews and Wall, 1997; Charron, 2012) which has informed foundational One Health concepts (Zinsstag et al., 2011; Rüegg et al., 2018a; Rüegg et al., 2018b). However, the enthusiasm for adopting a systems framing has also been tempered by other warnings that these concepts needed to be better internalized across disciplines (Antoine-Moussiaux, 2019; Wilcox et al., 2019; Assmuth et al., 2020). Others have also pointed out the ambiguities in the framing of One Health research and how a lack of recognition of distal causal factors—such as ‘environmental and social injustices driving biodiversity overexploitation and extinction’—will prevent One Health from fulfilling its mandate (de Garine-wichatitsky et al., 2020).
To be sure, recognizing the links between social and ecological systems is merely a starting point in the theorization of One Health. As other examples have shown, more attention to the structural drivers of infections can paint a much richer and more informed picture of how infections occur and are understood by different actors (Wood et al., 2012; Bardosh, 2016; Dzingirai et al., 2017; Wilcox et al., 2019; Thornber et al., 2020). As demonstrated in these examples, in order to design One Health collaborations that better reflect local realities, we will need to have a deep understanding of how different actors perceive diseases and the varying levels of agency exercised by them in order to change their practices.
Lessons for the practice of One Health
As the Covid-19 pandemic has demonstrated, decision-making around infectious diseases is often conducted in an environment characterized by uncertainty, dynamism and multi-scale interactions where multiple framings of the disease coexist and compete for attention (Macgregor et al., 2019; Leach et al., 2020). Given the scale and rapidity with which Covid-19 overwhelmed global governance arrangements, this has resulted in increased calls for realignment and coordinated responses—many of which cite One Health as an important tool for responding to the current and future pandemics (Cable et al., 2021; Lal et al., 2021; The Lancet Microbe, 2021).
The current instruments for assessing capacities to respond to disease events such as the International Health Regulations checklist and Performance of Veterinary Services pathways do refer to intersectoral collaborations. While these overlaps have been further enhanced in recent years using the One Health approach (De La Rocque and Formenty, 2014), the ongoing pandemic has led to calls for revisions in the global governance frameworks, and greater coordination among them (Blinken and Becerra, 2021; Lal et al., 2021). In addition, multilateral agencies have developed specific One Health centric guidance to help countries develop their own One Health collaborations (World Health Organization South East Asian Regional Office, World Health Organization Western Pacific Regional Office, Food & Agriculture Organization et al., 2008; The World Bank, EcoHealth Alliance, 2018; Food and Agriculture Organization, World Organisation For Animal Health (OIE), World Health Organization, 2019; Bhatia, 2021).
However, the current One Health guidance is exclusively focussed on formal, institutional mechanisms for initiating multisectoral activities, as illustrated by the example of the AMR Coordination Committee (Seale et al., 2017; Department of Health and Social Care, 2020). Other ways of encouraging interaction and dialogue across bureaucratic silos remain absent in the official literature. Another limitation of the standardized approaches to advocating One Health at the national level is that these fail to take the local context into account. While the newer guidance such as the Tripartite Zoonoses Guide does acknowledge the need for the country programme managers to adapt the approach to their local contexts, there is limited guidance on how to do so (Food and Agriculture Organization, World Organisation For Animal Health (OIE), World Health Organization, 2019).
Given the complex political economy of AMR and zoonoses, disease risks are likely to be understood and responded differently by each of the many different actors affected by them (Leach et al., 2010; Waltner-Toews, 2017; Spruijt and Petersen, 2020). Standardized and formal approaches of One Health governance that fail to recognize these differences in perspectives and operate within bureaucratic hierarchies that do not take into account power imbalances between the partners run the risk of developing blind spots in their management of disease risks. Therefore, the resultant One Health collaborations are not likely to sustain over a long time.
Country-based studies that have examined bureaucratic politics, economic incentives and structural factors governing disease risks have highlighted the importance of these factors in shaping local and national response to disease risks (Hinchliffe et al., 2021; Asaaga et al., 2021; Surdez et al., 2021). Therefore, in order for One Health collaborations to be relevant to local needs, their design and operation should adapt to the role of local politics and informal relationships. In short, for One Health collaborations to succeed, they need to be designed to be locally relevant, be aware of the diversity of interests and influence exercised by the actors involved and allow space for deliberation and adaptation to accommodate changing circumstances and partner needs.
Conclusions
This review demonstrates that, in addition to the themes of AMR and infectious diseases, multisector collaborations have been proposed and enacted as a policy response to a range of policy challenges that emerge from and impact multiple sectors. These multisector collaborations differ in formats and some will suit a specific context better than others. In their nature, multisector collaborations are complex political enterprises, that incorporate different visions around objectives, mandates, function, and success. Collaborating partners are likely to approach the partnership through their own aims and agenda which might compete or even conflict with the collaborative interests. Therefore, for collaborations to sustain, there will need to be pragmatism and some room for these to manoeuvre and adapt in order to accommodate partner needs or changing circumstances. Such adaptation is more likely to take place when boundaries of the collaboration remain relatively fluid.
Building upon observations from our review, we find several lessons for One Health movement. We suggest that One Health discourse needs to move beyond a one-size-fits-all approach and embrace multiple forms of multisector partnerships that are open to adaptation. In addition, One Health literature should recognise and respond to the politics involved in the development and conduct of multisector collaborations. This includes the diversity of framings within One Health, wherein different partners come to the collaboration with different expectations and agenda. The reference to politics also includes a reference to the different levels of influence enjoyed by the partners to effect change as well as the power dynamics operating among themselves.
A successful collaboration needs to be smart about working with and accommodating this politics instead of ignoring it. We recommend researchers to examine the role of politics in influencing multisector collaborations and that guidance around One Health partnerships from technical agencies being explicit about the political agenda they work in. Rather than standardized approaches, we suggest that the international guidelines on One Health should develop capacities and empower national programme managers to be flexible in choosing a form of One Health that best suits their requirements, and which can accommodate the agenda of different collaborating actors within their respective political landscapes. If the One Health movement can allow and encourage such an adaptive and responsive approach, we suggest, it is more likely that we will see sustainable forms of One Health collaborations to emerge.
Supplementary Material
Acknowledgements
We remain grateful to all those who have supported our efforts to develop the paper in different ways. Thanks to Dr Manu Mathur for his advice on methods. The literature review that informed the paper was developed to inform the One Health evaluation strategy for UK Fleming Fund (FF)—a complex multisectoral—One Health, UK aid programme around AMR funded by the UK Department for Health and Social Care. All three authors are part of the Itad team that is undertaking an independent evaluation of the FF. The authors used discussions with the FF team—specifically within the UK Department of Health and Social Care, Mott MacDonald (FF Management Agent) and Itad to seek feedback and programme inputs to the preliminary findings. These took the part of two formal meetings (in August 20 and January 21). The views expressed in this publication are those of the author(s) and not necessarily those of the Department of Health and Social Care.
Contributor Information
Syed Shahid Abbas, Institute of Development Studies, University of Sussex, Falmer, Brighton BN1 9RE, UK; Public Health Foundation of India, Plot No. 47, Sector 44, Institutional Area Gurugram 122002, India.
Tim Shorten, Independent Priory Farm, Half Moon Lane, Redgrave, Suffolk IP22 1RX, UK.
Jonathan Rushton, Institute of Infection, Veterinary and Ecological Sciences, University of Liverpool, Neston, Liverpool CH64 7TE, UK.
Supplementary data
Supplementary data are available at Health Policy and Planning online.
Data availability
The details of reviewed articles in this paper are available as online supplementary material.
Funding
S.A., T.S. and J.R. were a part of a team evaluating UK Fleming Fund—a complex multisectoral—One Health, UK aid programme around AMR funded by the UK Department for Health and Social Care. In addition, S.A. was supported by the UK Research and Innovation Global Challenges Research Fund One Health Poultry Hub (BB/S011269/1), one of 12 interdisciplinary research hubs funded through the UK Government’s Global Challenges Research Fund.
Author contributions
S.A. designed the study, conducted the literature review and developed the first draft of the manuscript. T.S. and J.R. contributed to the analysis and to revising the manuscript.
Ethical approval.
This study did not require ethical approval from our institutions.
Conflict of interest statement.
None declared.
References
- Abbas SS. 2018. Working Together for Prevention and Control of Zoonoses in India. [Google Scholar]
- Agranoff R. 2006. Inside collaborative networks: ten lessons for public managers. PublicAdministration Review 66: 56–65. [Google Scholar]
- Agranoff R. 2007. Intergovernmental policy management: cooperative practices in federal systems. In: Pagano MA, Leonardi R (eds). The Dynamics of Federalism in National and Supranational Political Systems. Basingstoke: Palgrave Macmillan, 248–83. [Google Scholar]
- Agranoff R. 2013. Local governments in multilevel systems: emergent public administration challenges. The American Review ofPublicAdministration 44: 47S–62S. [Google Scholar]
- Akin L. 1998. Methods for examining small literatures: explication, physical analysis, and citation patterns. Library & Information Science Research 20: 251–70. [Google Scholar]
- Amuasi JH, Walzer C, Heymann D et al. 2020. Calling for a COVID-19 one health research coalition. The Lancet 395: 1543–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansell C, Gash A. 2007. Collaborative governance in theory and practice. Journal ofPublicAdministration Research andTheory 18: 543–71. [Google Scholar]
- Antoine-Moussiaux N, Janssens de Bisthoven L, Leyens S et al. 2019. The good, the bad and the ugly: framing debates on nature in a One Health community. Sustainability Science 14: 1729–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asaaga FA, Rahman M, Kalegowda SD et al. 2021. “None of my ancestors ever discussed this disease before!” How disease information shapes adaptive capacity of marginalised rural populations in India. PLOSNeglected Tropical Diseases 15: e0009265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assmuth T, Chen X, Degeling C et al. 2020. Integrative concepts and practices of health in transdisciplinary social ecology. Socio-EcologicalPractice Research 2: 71–90. [Google Scholar]
- Atun RA, de Jongh T, Secci F et al. 2010. Integration of targeted health interventions into health systems: a conceptual framework for analysis. Health Policyand Planning 25: 104–11. [DOI] [PubMed] [Google Scholar]
- Bardosh KL. (ed.) 2016. One Health: Science, Politics and Zoonotic Disease in Africa. Abingdon, UK: Routledge. [Google Scholar]
- Bay J, Morton S, Vickers M. 2016. Realizing the potential of adolescence to prevent transgenerational conditioning of noncommunicable disease risk: multi-sectoral design frameworks. Healthcare 4: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett S, Glandon D, Rasanathan K. 2018. Governing multisectoral action for health in low-income and middle-income countries: unpacking the problem and rising to the challenge. BMJGlobal Health 3: e000880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg A. 1987. Rejoinder: nutrition planning is alive and well, thank you. Food Policy 12: 365–75. [DOI] [PubMed] [Google Scholar]
- Bhatia R. 2021. National Framework for One Health. New Delhi: FAO. [Google Scholar]
- Biesma RG, Brugha R, Harmer A et al. 2009. The effects of global health initiatives on country health systems: a review of the evidence from HIV/AIDS control. Health Policyand Planning 24: 239–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blinken AJ, Becerra X. 2021. Strengthening global health security and reforming the international health regulations. JAMA 326: 1255. doi: 10.1001/jama.2021.15611 [DOI] [PubMed] [Google Scholar]
- Blomstedt Y, Bhutta ZA, Dahlstrand J et al. 2018. Partnerships for child health: capitalising on links between the sustainable development goals. BMJ 360: 1–8. [DOI] [PubMed] [Google Scholar]
- Boon H, Verhoef M, O’Hara D et al. 2004. From parallel practice to integrative health care: a conceptual framework. BMC HealthServices Research 4: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgon J. 2011. A New Synthesis of Public Administration: Serving in the 21st Century. Montreal: McGill-Queen’s University Press. [Google Scholar]
- Braun V, Clarke V. 2006. Using thematic analysis in psychology. Qualitative Research in Psychology 3: 77–101. [Google Scholar]
- Briscoe S, Bethel A, Rogers M. 2020. Conduct and reporting of citation searching in Cochrane systematic reviews: a cross-sectional study. Research SynthesisMethods 11: 169–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwer H, Hiemstra W, va Vugt S et al. 2013. Analysing stakeholder power dynamics in multi-stakeholder processes: insights of practice from Africa and Asia. Knowledge Management for Development Journal 9: 11–31. [Google Scholar]
- Brouwer H, Woodhill J, Hemmati M et al. 2016. The MSP guide: how to design and facilitate multi-stakeholder partnerships. In: The MSP Guide: How to Design and Facilitate Multi-Stakeholder Partnerships. Wageningen: Practical Action Publishing, i–1. [Google Scholar]
- Bryson JM, Crosby BC, Stone MM. 2006. The design and implementation of cross-sector collaborations: propositions from the literature. PublicAdministration Review 66: 44–55. [Google Scholar]
- Cable J, Heymann DL, Uzicanin A et al. 2021. Pandemic diseases preparedness and response in the age of COVID‐19—a symposium report. Annals of the New York Academy of Sciences 1489: 17–29. [DOI] [PubMed] [Google Scholar]
- Calain P. 2007. Exploring the international arena of global public health surveillance. Health Policyand Planning 22: 2–12. [DOI] [PubMed] [Google Scholar]
- Cassidy A. 2018. Humans, other animals and ‘one health’ in the early twenty-first century. In: Timmermann C, Worboys M (eds). Animals and the Shaping of Modern Medicine. Cham: Springer International Publishing, 193–236. [Google Scholar]
- Centers for Disease Control and Prevention . 2021. Atlanta: One Health. cdc.gov/onehealth, accessed 9 June 2021.
- Centers For Disease Control and Prevention . Operationalizing “One Health”: a policy perspective—taking stock and shaping an implementation roadmap: In: Meeting Overview: May 4–6, 2010: Stone Mountain, Georgia; 2010. [Google Scholar]
- Charron DF. (ed.) 2012. Ecohealth Research in Practice: Innovative Applications of an Ecosystem Approach to Health. Ottawa: International Development Research Centre. [Google Scholar]
- Chen B. 2010. Antecedents or processes? Determinants of perceived effectiveness of interorganizational collaborations for public service delivery. InternationalPublicManagement Journal 13: 381–407. [Google Scholar]
- Chenard HJ. 2007. Intersectoral Partnerships for Sustainable Development : The Case of Community Forest Management in Brazil. London: London School of Economics & Political Science. [Google Scholar]
- Chircop A, Bassett R, Taylor E. 2015. Evidence on how to practice intersectoral collaboration for health equity: a scoping review. CriticalPublic Health 25: 178–91. [Google Scholar]
- Commission on Social determinants of Health . 2008. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health. Geneva. [Google Scholar]
- Cooper H, Hedges LV. 2009. Research synthesis as a scientific process. In: Hedges LV, Cooper H, Valentine JC (eds). The Handbook of Research Synthesis and Meta-Analysis. 2nd edn New York: Russell Sage Foundation, 3–16. [Google Scholar]
- Crosby BC, Bryson JM. 2005. A leadership framework for cross-sector collaboration. PublicManagement Review 7: 177–201. [Google Scholar]
- Davies JS. 2009. The limits of joined up governance: towards a political analysis. PublicAdministration 87: 80–96. [Google Scholar]
- Davies SC. 2013. Infections and the Rise of Antimicrobial Resistance. In: Walker D, Fowler T (eds). London: Department of Health, 11–25. [Google Scholar]
- de Bengy Puyvallée A, Kittelsen S. 2019. “Disease knows no borders”: pandemics and the politics of global health security. In: Bjørkdahl K, Carlsen B (eds). Pandemics, Publics, and Politics. Singapore: Springer Singapore, 59–73. [Google Scholar]
- de Garine-wichatitsky M, Binot A, Morand S et al. 2020. Will the COVID-19 crisis trigger a One Health coming-of-age? TheLancetPlanetary Health 4: e377–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de La Rocque S, Formenty P. 2014. Applying the One Health principles: a trans-sectoral coordination framework for preventing and responding to Rift Valley fever outbreaks. Revue Scientifique et Technique de l’OIE 33: 555–67. [DOI] [PubMed] [Google Scholar]
- de Leeuw E. 2017. Engagement of sectors other than health in integrated health governance, policy, and action. Annual Review ofPublic Health 38: 329–49. [DOI] [PubMed] [Google Scholar]
- Department of Health and Social Care . 2020. Fleming fund annual review: January to December 2019. UKGOV. [Google Scholar]
- Department of Health and Social Care . 2021. G7 health ministers’ meeting, communique. 4 June, 2021. Oxford: GOVUK. [Google Scholar]
- Dietz T, Ostrom E, Stern PC. 2003. The struggle to govern the commons. Science 302: 1907–12. [DOI] [PubMed] [Google Scholar]
- Dubois A, St-Pierre L, Veras M. 2015. A scoping review of definitions and frameworks of intersectoral action. Ciência & Saúde Coletiva 20: 2933–42. [DOI] [PubMed] [Google Scholar]
- Duit A, Galaz V, Eckerberg K et al. 2010. Governance, complexity, and resilience. Global Environmental Change 20: 363–8. [Google Scholar]
- Dzingirai V, Bett B, Bukachi S et al. 2017. Zoonotic diseases: who gets sick, and why? Explorations from Africa. CriticalPublic Health 27: 97–110. [Google Scholar]
- Emerson K. 2018. Collaborative governance of public health in low- and middle-income countries: lessons from research in public administration. BMJGlobal Health 3: e000381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emerson K, Gerlak AK. 2014. Adaptation in collaborative governance regimes. Environmental Management 54: 768–81. [DOI] [PubMed] [Google Scholar]
- Emerson K, Nabatchi T. 2015. Evaluating the productivity of collaborative governance regimes: a performance matrix. PublicPerformance & Management Review 38: 717–47. [Google Scholar]
- Emerson K, Nabatchi T, Balogh S. 2012. An integrative framework for collaborative governance. Journal ofPublicAdministration Research andTheory 22: 1–29. [Google Scholar]
- Exworthy M, Hunter DJ. 2011. The challenge of joined-up government in tackling health inequalities. International Journal ofPublicAdministration 34: 201–12. [Google Scholar]
- Field JO. 1987. Multisectoral nutrition planning: a post-mortem. Food Policy 12: 15–28. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick MC, Shah HA, Pandey A et al. 2016. One Health approach to cost-effective rabies control in India. Proceedings of the National Academy of Sciences 113: 14574–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folke C, Hahn T, Olsson P et al. 2005. Adaptive governance of social - ecological systems. Annual Review of Environment and Resources 30: 441–73. [Google Scholar]
- Food & Agriculture Organization, World Organization for Animal Health, World Health Organization . 2010. The FAO-OIE-WHO Collaboration: Sharing Responsibilities and Coordinating Global Activities to Address Health Risks at the Animal-Human-Ecosystems Interfaces: A Tripartite Concept Note. Geneva. [Google Scholar]
- Food and Agriculture Organization, World Organisation For Animal Health (OIE), World Health Organization . 2019. Taking A Multisectoral, One Health Approach: A Tripartite Guide to Addressing Zoonotic Diseases in Countries Taking A Multisectoral, One Health Approach. Geneva: Food and Agriculture Organization, World Organisation For Animal Health (OIE), World Health Organization. [Google Scholar]
- Frederickson HG, Smith KB, Larimer CW et al. 2012. The Public Administration Theory Primer. 2nd edn Boulder, CO: Westview Press. [Google Scholar]
- Frenk J. 2009. Reinventing primary health care: the need for systems integration. TheLancet 374: 170–3. [DOI] [PubMed] [Google Scholar]
- Galaz V, Leach M, Scoones I et al. 2015. The Political Economy of One Health Research and Policy. Brighton: Institute of Development Studies. [Google Scholar]
- Garrett J, Natalicchio M (eds). 2011. Working Multisectorally in Nutrition Principles, Practices, and Case Studies. Washington, DC: International Food Policy Research Institute. [Google Scholar]
- Gebreyes WA, Dupouy-Camet J, Newport MJ et al. 2014. The global one health paradigm: challenges and opportunities for tackling infectious diseases at the human, animal, and environment interface in low-resource settings. PLoSNeglected Tropical Diseases 8: e3257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glandon D, Meghani A, Jessani N et al. 2018. Identifying health policy and systems research priorities on multisectoral collaboration for health in low-income and middle-income countries. BMJGlobal Health 3: e000970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glandon D, Mondal S, Okeyo I et al. 2019. Methodological gaps and opportunities for studying multisectoral collaboration for health in low- and middle-income countries. Health Policyand Planning 34: ii7–17. [DOI] [PubMed] [Google Scholar]
- Graham WJ, Kuruvilla S, Hinton R et al. 2018. Multisectoral collaboration for health and sustainable development. BMJ 363: k4868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant MJ, Booth A. 2009. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Information and Libraries Journal 26: 91–108. [DOI] [PubMed] [Google Scholar]
- Gratton L, Erickson TJ. 2007. Ways to build collaborative teams. Harvard Business Review 85: 86–94. [PubMed] [Google Scholar]
- Gray B, Wood DJ. 1991. Collaborative alliances: moving from practice to theory. The Journal of Applied Behavioral Science 27: 3–22. [Google Scholar]
- Grépin KA, Reich MR. 2008. Conceptualizing integration: a framework for analysis applied to neglected tropical disease control partnerships. Utzinger J (ed.). PLoSNeglected Tropical Diseases 2: e174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greszczuk C. (ed.) 2019. Implementing Health in All Policies: Lessons from around the World. London: The Health Foundation. [Google Scholar]
- Gyapong JO, Gyapong M, Yellu N et al. 2010. Integration of control of neglected tropical diseases into health-care systems: challenges and opportunities. TheLancet 375: 160–5. [DOI] [PubMed] [Google Scholar]
- Harris J, Brown VA, Russell J. (eds). 2010. Tackling Wicked Problems. 1st edn London: Routledge. [Google Scholar]
- Harris J, Drimie S. 2012. Toward an Integrated Approach for Addressing Malnutrition in Zambia: A Literature Review and Institutional Analysis. Washington, DC: International Food Policy Research Institute. [Google Scholar]
- Häsler B, Bazeyo W, Byrne AW et al. 2020. Reflecting on One Health in action during the COVID-19 response. Frontiers in Veterinary Science 7: 578649. doi: 10.3389/fvets.2020.578649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriks A-M, Habraken J, Jansen MWJ et al. 2014. ‘Are we there yet?’ – operationalizing the concept of integrated public health policies. Health Policy 114: 174–82. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Thomas J, Chandler J et al. (eds). 2019. Cochrane Handbook for Systematic Reviews of Interventions. Wiley. [Google Scholar]
- Hinchliffe S. 2015. More than one world, more than one health: re-configuring interspecies health. Social Science & Medicine 129: 28–35. [DOI] [PubMed] [Google Scholar]
- Hinchliffe S, Butcher A, Rahman MM et al. 2021. Production without medicalisation: risk practices and disease in Bangladesh aquaculture. The Geographical Journal 187: 39–50. [Google Scholar]
- Hinde S, Spackman E. 2015. Bidirectional citation searching to completion: an exploration of literature searching methods. Pharmacoeconomics 33: 5–11. [DOI] [PubMed] [Google Scholar]
- Hirt J, Nordhausen T, Appenzeller-Herzog C et al. 2020. Using citation tracking for systematic literature searching - study protocol for a scoping review of methodological studies and an expert survey. F1000Research 9: 1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitziger M, Esposito R, Canali M et al. 2018. Knowledge integration in One Health policy formulation, implementation and evaluation. Bulletin of theWorld HealthOrganization 96: 211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson B, Hardy B, Henwood M et al. 1999. In pursuit of inter-agency collaboration in the public sector. PublicManagement:AnInternational Journal of Research andTheory 1: 235–60. [Google Scholar]
- Huxham C. 2003. Theorizing collaboration practice. PublicManagement Review 5: 401–23. [Google Scholar]
- Huxham C, Hibbert P. 2008. Hit or myth? Stories of collaborative success. In: O’Flynn J, Wanna J (eds). Collaborative Governance: A New Era of Public Policy in Australia? Canberra: ANU Press, 45–50. [Google Scholar]
- Huxham C, Vangen S. 2004. Managing to Collaborate: The Theory and Practice of Collaborative Advantage. New York: Routledge. [Google Scholar]
- IMCAPI . Hanoi Declaration at the International Ministerial Conference: “Animal and Pandemic Influenza: The Way Forward”. Hanoi, Vietnam: 19–21 April 2010. [Google Scholar]
- Innes JE. 1999. Evaluating Consensus Building. In: Susskind L, McKearnan S, Book JT-L (eds). Thousand Oaks, CA: SAGE Publications, Inc, 631–76. [Google Scholar]
- Ivery JM. 2010. Partnerships in transition: managing organizational and collaborative change. Journal of Human Behavior in the Social Environment 20: 20–37. [Google Scholar]
- Kalegaonkar A, Brown LD. 2000. Intersectoral Cooperation: Lessons for Practice. Boston: Institute for Development Research. [Google Scholar]
- Kar M. 2014. Governance of HIV/AIDS: implications for health sector response. International Journal of HealthPolicyand Management 2: 39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuper H, Nicholson A, Hemingway H. 2006. Searching for observational studies: what does citation tracking add to PubMed? A case study in depression and coronary heart disease. BMCMedical Research Methodology 6: 4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuruvilla S, Hinton R, Boerma T et al. 2018. Business not as usual: how multisectoral collaboration can promote transformative change for health and sustainable development. BMJ 363: k4771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laborde D, Martin W, Swinnen J et al. 2020. COVID-19 risks to global food security. Science 369: 500–2. [DOI] [PubMed] [Google Scholar]
- Lal A, Erondu NA, Heymann DL et al. 2021. Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage. The Lancet 397: 61–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Lancet Microbe . 2021. G7 leaders commit to greater pandemic preparedness (again). The Lancet Microbe 2: e276. [DOI] [PubMed] [Google Scholar]
- Lank E. 2006. Collaborative Advantage: How Organizations Work Together. New York: Palgrave Macmillan. [Google Scholar]
- Leach M, MacGregor H, Scoones I et al. 2020. Post-pandemic transformations: how and why COVID-19 requires us to rethink development. WorldDevelopment 138: 105233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leach M, Scoones I, Stirling A. 2010. Governing epidemics in an age of complexity: narratives, politics and pathways to sustainability. Global Environmental Change 20: 369–77. [Google Scholar]
- Lee K, Brumme ZL. 2012. Operationalizing the One Health approach: the global governance challenges. Health Policy and Planning 28: 778–85. doi: 10.1093/heapol/czs127 [DOI] [PubMed] [Google Scholar]
- Legido-Quigley H, Khan MS, Durrance-Bagale A et al. 2019. Something borrowed, something new: a governance and social construction framework to investigate power relations and responses of diverse stakeholders to policies addressing antimicrobial resistance. Antibiotics 8: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson FJ, Balarajan Y. 2013. Addressing Malnutrition: What Have We Learned from Recent International Experience? New York: UNICEF and MDG Achievement Fund. [Google Scholar]
- Macgregor H, Ripoll S, Leach M. 2019. Disease outbreaks: navigating uncertainties in preparedness and response. In: Scoones I, Stirling A (eds). The Politics of Uncertainty: Challenges of Transformation. London: Routledge. [Google Scholar]
- MacGregor H, Waldman L. 2017. Views from many worlds: unsettling categories in interdisciplinary research on endemic zoonotic diseases. Philosophical Transactions of the Royal SocietyB: Biological Sciences 372: 20160170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahlangu P, Goudge J, Vearey J. 2019. Towards a framework for multisector and multilevel collaboration: case of HIV and AIDS governance in South Africa. GlobalHealth Action 12: 1617393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahlangu P, Vearey J, Goudge J. 2018. Multisectoral (in)action: towards effective mainstreaming of HIV in public sector departments in South Africa. AfricanJournal ofAIDSResearch 17: 301–12. [DOI] [PubMed] [Google Scholar]
- Marks S. 2002. An epidemic waiting to happen? The spread of HIV/AIDS in South Africa in social and historical perspective. African Studies 61: 13–26. [Google Scholar]
- McGuire M. 2006. Collaborative public management: assessing what we know and how we know it. PublicAdministration Review 66: 33–43. [Google Scholar]
- Mcqueen DV, Wismar M, Lin V et al. (eds). 2012. Intersectoral Governance for Health in All Policies: Structures, Actions and Experiences. Copenhagen: World Health Organization. [Google Scholar]
- Nowell LS, Norris JM, White DE et al. 2017. Thematic analysis: striving to meet the trustworthiness criteria. International Journal of QualitativeMethods 16: 1–13. [Google Scholar]
- O’Neil J, Orchard T, Swarankar RC et al. 2004. Dhandha, dharma and disease: traditional sex work and HIV/AIDS in rural India. Social Science & Medicine 59: 851–60. [DOI] [PubMed] [Google Scholar]
- Ogyu A, Chan O, Littmann J et al. 2020. National action to combat AMR: a One-Health approach to assess policy priorities in action plans. BMJ Global Health 5: e002427. doi: 10.1136/bmjgh-2020-002427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okello AL, Bardosh K, Smith J et al. 2014. One Health: past successes and future challenges in three african contexts. Zinsstag J (ed.). PLoSNeglected Tropical Diseases 8: e2884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olmstead AL, Rhode PW. 2015. Arresting Contagion: Science, Policy, and Conflicts over Animal Disease Control. Cambridge, MA: Harvard University Press. [Google Scholar]
- Osofsky SA, Karesh WB, Kock R et al. 2003. AHEAD invitees briefing packet. Wildlife Conservation Society. http://www.wcs-ahead.org/wpcongress.html. [Google Scholar]
- Ostrom E. 1990. Governing the Commons: The Evolution of Institutions for Collective Action. In: Alt JE, North DC (eds). Cambridge University Press. [Google Scholar]
- Ottersen OP, Engebretsen E. 2020. COVID-19 puts the sustainable development goals center stage. Nature Medicine 26: 1672–3. [DOI] [PubMed] [Google Scholar]
- Page SB, Stone MM, Bryson JM et al. 2015. Public value creation by cross-sector collaborations: a framework and challenges of assessment. PublicAdministration 93: 715–32. [Google Scholar]
- Paré G, Trudel MC, Jaana M et al. 2015. Synthesizing information systems knowledge: a typology of literature reviews. Information & Management 52: 183–99. [Google Scholar]
- Parkes MW, Bienen L, Breilh J et al. 2005. All hands on deck: transdisciplinary approaches to emerging infectious disease. Ecohealth 2: 258–72. [Google Scholar]
- Pelletier D, Gervais S, Hafeez-ur-Rehman H et al. 2018. Boundary-spanning actors in complex adaptive governance systems: the case of multisectoral nutrition. The International Journal ofHealthPlanning and Management 33: e293–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry BD, Grace D. 2009. The impacts of livestock diseases and their control on growth and development processes that are pro-poor. Philosophical Transactions of the Royal SocietyB: Biological Sciences 364: 2643–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters BG, Pierre J. 1998. Governance without government? Rethinking public administration. Journal ofPublicAdministration Research andTheory 8: 223–43. [Google Scholar]
- Public Health Agency of Canada, Commission on Social Determinants of Health, Regional Network for Equity in Health in East and Southern Africa . 2008. Crossing Sectors – Experiences in Intersectoral Action, Public Policy and Health. Toronto: Public Health Agency of Canada. [Google Scholar]
- Purdy JM. 2012. A framework for assessing power in collaborative governance processes. PublicAdministration Review 72: 409–17. [Google Scholar]
- Puska P. 2007. Health in all policies. The European Journal ofPublic Health 17: 328–328. [DOI] [PubMed] [Google Scholar]
- Quick KS, Feldman MS. 2014. Boundaries as junctures: collaborative boundary work for building efficient resilience. Journal ofPublicAdministration Research andTheory 24: 673–95. [Google Scholar]
- Rajivan AK. 2006. Tamil Nadu: ICDS with a difference. Economic and Political Weekly 41: 3684–8. [Google Scholar]
- Ramalingam B, Jones H, Reba T et al. 2008. Exploring the Science of Complexity: Ideas and Implications for Development and Humanitarian Efforts Results of ODI Research Presented in Preliminary Form for Discussion and Critical Comment. 2nd edn London: Overseas Development Institute. [Google Scholar]
- Ran B, Qi H. 2018. Contingencies of power sharing in collaborative governance. The American Review ofPublicAdministration 48: 836–51. [Google Scholar]
- Rasanathan K, Bennett S, Atkins V et al. 2017. Governing multisectoral action for health in low- and middle-income countries. PLoSMedicine 14: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasanathan K, Damji N, Atsbeha T et al. 2015. Ensuring multisectoral action on the determinants of reproductive, maternal, newborn, child, and adolescent health in the post-2015 era. BMJ 351: h4213. [DOI] [PubMed] [Google Scholar]
- Ring PS, Van De Ven AH. 1994. Developmental processes of cooperative interorganizational relationships. Academy of Management Review 19: 90–118. [Google Scholar]
- Robinson TP, Bu DP, Carrique-Mas J et al. 2016. Antibiotic resistance is the quintessential One Health issue. Transactions of the Royal Society of Tropical Medicine and Hygiene 110: 377–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruckert A, Zinszer K, Zarowsky C et al. 2020. What role for One Health in the COVID-19 pandemic? Canadian Journal ofPublicHealth 111: 641–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rüegg SR, Häsler B, Zinsstag J. (eds). 2018a. Integrated Approaches to Health: A Handbook for the Evaluation of One Health. The Netherlands: Wageningen Academic Publishers. [Google Scholar]
- Rüegg SR, Nielsen LR, Buttigieg SC et al. 2018b. A systems approach to evaluate One Health initiatives. Frontiers in Veterinary Science 5: 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagawa S, Segal E, Kanter RM. 1999. Common Interest, Common Good: Creating Value through Business and Social Sector Partnerships. Boston: Harvard University Press. [Google Scholar]
- Schultz M. 2008. Rudolf virchow. Emerging Infectious Diseases 14: 1480–1. [Google Scholar]
- Schwabe CW. 1984. Veterinary Medicine and Human Health. 3rd edn Baltimore: Lippincott Williams and Wilkins. [Google Scholar]
- Seale AC, Gordon NC, Islam J et al. 2017. AMR surveillance in low and middle-income settings - a roadmap for participation in the Global Antimicrobial Surveillance System (GLASS). Wellcome OpenResearch 2: 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakarishvili G, Atun RA, Berman P. 2009. Building on Health Systems Frameworks for Developing a Common Approach to Health: Draft for Discussion. Washington, DC: The World Bank. [Google Scholar]
- Shankardass K, Muntaner C, Kokkinen L et al. 2018. The implementation of health in all policies initiatives: a systems framework for government action. Health ResearchPolicyand Systems 16: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankardass K, Renahy E, Muntaner C et al. 2015. Strengthening the implementation of health in all policies: a methodology for realist explanatory case studies. Health Policy and Planning 30: 462–73. [DOI] [PubMed] [Google Scholar]
- Sherr K, Mussa A, Chilundo B et al. 2012. Brain drain and health workforce distortions in mozambique. Miranda JJ (ed.). PLoS One 7: e35840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman J. 2006. Donor funding priorities for communicable disease control in the developing world. Health Policyand Planning 21: 411–20. [DOI] [PubMed] [Google Scholar]
- Shigayeva A, Atun R, McKee M et al. 2010. Health systems, communicable diseases and integration. Health Policyand Planning 25: i4–20. [DOI] [PubMed] [Google Scholar]
- Spruijt P, Petersen AC. 2020. Multilevel governance of antimicrobial resistance risks: a literature review. Journal ofRiskResearch 0: 1–14. [Google Scholar]
- Ssennyonjo A, Van Belle S, Titeca K et al. 2021. Multisectoral action for health in low-income and middle-income settings: how can insights from social science theories inform intragovernmental coordination efforts? BMJGlobal Health 6: e004064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surdez M, Piquerez L, Hobeika A. 2021. Torn between responsibility and loyalty: how the veterinarian profession designs antibiotic resistance policies that shake its foundations. Review of Agricultural,Foodand Environmental Studies 102: 191–211. [Google Scholar]
- Tennyson R. 2003. Institutionalising Partnerships: Lessons from the Front Line. London: International Business Leaders Forum (IBLF). [Google Scholar]
- Tennyson R. 2004. The Partnering Toolbook. In: Torggler B, Hill A (eds). London: International Business Leaders Forum (IBLF), 14. [Google Scholar]
- Tennyson R, Harrison T, Alzaga C et al. 2008. Under the Spotlight: Building a Better Understanding of Global Business-NGO Partnerships. In: Hodges A, Joyce R (eds). London: International Business Leaders Forum (IBLF), 16–18. [Google Scholar]
- Tennyson R, Wilde L. 2000. The Guiding Hand: Brokering Partnerships for Sustainable Development. McManus S (ed.) London: United Nations Department of Public Information. [Google Scholar]
- Thomson AM, Perry JL. 2006. Collaboration processes: inside the black box. PublicAdministration Review 66: 20–32. [Google Scholar]
- Thomson AM, Perry JL, Miller TK. 2007. Conceptualizing and measuring collaboration. Journal ofPublicAdministration Research andTheory 19: 23–56. [Google Scholar]
- Thomson AM, Perry JL, Miller TK. 2008. Linking collaboration processes and outcomes: foundations for advancing empirical theory. In: Big Ideas in Collaborative Public Management. 1st edn London: Routledge, 97–120. [Google Scholar]
- Thornber K, Verner-Jeffreys D, Hinchliffe S et al. 2020. Evaluating antimicrobial resistance in the global shrimp industry. Reviews in Aquaculture 12: 966–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonelli DF, Sant’Anna L, Barcelar Abbud E et al. 2018. Antecedents, process, and equity outcomes: a study about collaborative governance. CogentBusiness & Management 5: 1–17. [Google Scholar]
- UK Department of Health & Social Care, UK Aid . 2018. Fleming fund overview. Fleming Fund. https://www.flemingfund.org/wp-content/uploads/91b22cc0262e93091bd0ae1edbafcae2.pdf, accessed 20 May 2021. [Google Scholar]
- United Nations . 2008. Contributing to One World, One Health- A Strategic Framework for Reducing Risks of Infectious Diseases at the Animal – Human – Ecosystems Interface. Geneva: United Nations. [Google Scholar]
- Valeix SF. 2018. One Health integration: a proposed framework for a study on veterinarians and zoonotic disease management in Ghana. Frontiers in Veterinary Science 5: 85. doi: 10.3389/fvets.2018.00085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Herten J, Bovenkerk B, Verweij M. 2019. One Health as a moral dilemma: towards a socially responsible zoonotic disease control. Zoonoses andPublic Health 66: 26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vangen S, Huxham C. 2012. The tangled web: unraveling the principle of common goals in collaborations. Journal ofPublicAdministration Research andTheory 22: 731–60. [Google Scholar]
- Waltner-Toews D. 2017. Zoonoses, One Health and complexity: wicked problems and constructive conflict. Philosophical Transactions of the Royal SocietyB: Biological Sciences 372: 20160171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waltner-Toews D, Kay J. 2005. The evolution of an ecosystem approach: the diamond schematic and an adaptive methodology for ecosystem sustainability and health. Ecology and Socity 10. [Google Scholar]
- Waltner-Toews D, Wall E. 1997. Emergent perplexity: in search of post-normal questions for community and agroecosystem health. Social Science & Medicine 45: 1741–9. [DOI] [PubMed] [Google Scholar]
- Wilcox B, Kueffer C. 2008. Transdisciplinarity in EcoHealth: status and future prospects. Ecohealth 5: 1–3. [DOI] [PubMed] [Google Scholar]
- Wilcox BA, Aguirre AA, De Paula N et al. 2019. Operationalizing one health employing social-ecological systems theory: lessons from the greater Mekong sub-region. Front Public Health 7: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood DJ, Gray B. 1991. Toward a comprehensive theory of collaboration. The Journal of Applied Behavioral Science 27: 139–62. [Google Scholar]
- Wood JLN, Leach M, Waldman L et al. 2012. A framework for the study of zoonotic disease emergence and its drivers: spillover of bat pathogens as a case study. Philosophical Transactions of the Royal SocietyB: Biological Sciences 367: 2881–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods A. 2017. From one medicine to two: the evolving relationship between human and veterinary medicine in England, 1791–835. Bulletin of the History of Medicine 91: 494–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods A, Bresalier M, Cassidy A et al. 2018. Animals and the Shaping of Modern Medicine: One Health and Its Histories. In: Timmermann C, Worboys M (eds). Cham, Switzerland: Springer International Publishing, 193–226. [Google Scholar]
- The World Bank . 2010. People, Pathogens and Our Planet Volume 1: Towards a One Health Approach for Controlling Zoonotic Diseases. Washington, DC: The World Bank. [Google Scholar]
- The World Bank . 2012. People, Pathogens and Our Planet: Volume 2: The Economics of One Health. Washington, DC: The World Bank. [Google Scholar]
- The World Bank . 2013. Improving Nutrition through Multisectoral Approaches. Washington, DC: The World Bank. [Google Scholar]
- The World Bank, EcoHealth Alliance . 2018. Operational Framework for Strengthening Human, Animal and Environmental Public Health Systems at Their Interface. Washington, DC: The World Bank. [Google Scholar]
- World Health Organization . 2015. WHO Global Action Plan on Antimicrobial Resistance. Geneva: World Health Organization. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2017. Geneva: One Health. Q&A. [Google Scholar]
- World Health Organization . 2018. Multisectoral and Intersectoral Action for Improved Health and Well-Being for All: Mapping of the WHO European Region Governance for a Sustainable Future: Improving Health and Well-Being for All. Copenhagen: World Health Organization. [Google Scholar]
- World Health Organization South East Asian Regional Office, World Health Organization Western Pacific Regional Office, Food & Agriculture Organization et al. 2008. Zoonotic Diseases: A Guide to Establishing Collaboration between Animal and Human Health Sectors at the Country Level. Manila: World Health Organization. [Google Scholar]
- World Health Organization, United Nations Foundation Interagency Partnership, Centres for Disease Control and Prevention et al. 2003. The Implementation of Integrated Disease Surveillance and Response in the African and Eastern Mediterranean Regions: Synthesis Report: Nov 17, 2002 to December 7, 2002. Geneva: World Health Organization. [Google Scholar]
- World Organization for Animal Health . 2021. Paris: One Health. OIE.Int. [Google Scholar]
- Zinsstag J. 2012. Convergence of EcoHealth and One Health. Ecohealth 9: 371–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinsstag J, Schelling E, Roth F et al. 2007. Human benefits of animal interventions for zoonosis control. Emerging Infectious Diseases 13: 527–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinsstag J, Schelling E, Waltner-Toews D et al. 2011. From “one medicine” to “one health” and systemic approaches to health and well-being. Preventive Veterinary Medicine 101: 148–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The details of reviewed articles in this paper are available as online supplementary material.


