Abstract
Background:
Public health measures to control the COVID-19 pandemic have led to feelings of loneliness among older adults, which, prior to COVID, has been associated with subsequent morbidity and mortality. We sought to identify differences in feelings of loneliness, sadness, and social disconnection early in the pandemic across racial groups, and possible mitigating factors.
Methods:
We performed a cross-sectional analysis using the weighted nationally-representative Medicare Current Beneficiaries Survey COVID-19 supplement, collected summer 2020. We included all Medicare beneficiaries over 65 who did not respond by proxy. We examined changes in loneliness, sadness, or feelings of social disconnection. Multivariable logistic regression models accounted for sociodemographic variables, access to primary care and the internet, and history of depression or dementia.
Results:
Among 8,125 beneficiaries, representative of 43.7 million Medicare beneficiaries, 22.6% reported loneliness or sadness, and 37.1% feeling socially disconnected. In fully-adjusted models, Hispanic/Latinx beneficiaries were most likely to report loneliness or sadness (OR=1.3, CI: 1.02–1.65; P=0.02) and Black beneficiaries were least likely to report feeling socially disconnected (OR=0.55; CI: 0.42–0.73; P<0.001). Internet access was associated with increased odds of both (OR=1.29, 95 CI: 1.07–1.56; P=0.009; and OR=1.42, 95 CI: 1.24–1.63; P<0.001, respectively). Access to primary care was associated with lower odds of both (OR=0.77, 95 CI: 0.61–0.96; P=0.02; and OR=0.72, 95 CI: 0.61–0.87; P<0.001).
Conclusions:
Loneliness, sadness, and feelings of social disconnection were common among older Medicare beneficiaries early in the COVID-19 pandemic. Differences by race/ethnicity may be driven by different living structures and social networks, and warrant further study. Policy makers and clinicians should consider facilitating connection by phone or in person, as internet access did not diminish feelings of loneliness, particularly for those living alone. Access to primary care, and tools for clinicians to address loneliness should be prioritized.
Introduction:
Efforts to control the COVID-19 pandemic have included distancing measures and stay-at-home orders. While effective for infection control, there is evidence that following these orders has led to increased feelings of loneliness.1–5 Older adults who feel lonely or perceive themselves to be socially isolated are at increased risk of morbidity and mortality,6–8 including from cardiovascular disease,9 mental health,10,11 and dementia.6,12 Even before COVID-19, 20–40% of US adults over 65 years old reported feelings of loneliness.8,13–16 Among older adults, feelings of loneliness and perceived social isolation are more common among women, those who live alone, have low socioeconomic status, or limited English proficiency.13,17,18 Older adults who are women or have low socioeconomic status were also more likely to report sadness.19
Prior to the pandemic, Black and Hispanic/Latinx older adults were less likely to be objectively socially isolated compared with White older adults.14 However, research on racial differences in the subjective feelings of loneliness and social disconnection has been mixed.19–21 Black individuals are most likely to live in multigenerational homes, which could be protective against loneliness and feelings of disconnection.22–25 However, Black and Hispanic/Latinx communities have had higher rates of sickness and death secondary to COVID-19,26,27 which could lead to greater loneliness, sadness, and feelings of social disconnection.
During the COVID-19 pandemic, opportunities to form or reinforce social connections are of particular importance.28,29 Access to the internet may facilitate tangible social connections,6 but studies conducted prior to the pandemic suggest that internet may exacerbate the subjective feeling of loneliness.30,31 Access to primary care may play an important role in identifying and countering isolation.32 The healthcare team itself may serve as a social connection, and physicians can recommend interventions to preempt or address loneliness, sadness, and feelings of social disconnection, such as phone calls with loved ones.6,16,33 However, not all adults have equal access to the internet or primary care, with known disparities by race and ethnicity.34,35
Accordingly, our objective was to characterize self-reported increases in loneliness, sadness, and feelings of social disconnection among Medicare recipients 65 and over since the onset of COVID-19. We sought to determine whether feelings of loneliness, sadness, or social disconnection differed by race or ethnicity, and whether access to the internet or primary care was associated with less loneliness or feelings of disconnection. Given the ongoing COVID-19 pandemic and need for distancing measures, identifying whether modifiable factors such as access to primary care and the internet improve loneliness, sadness or feelings of social disconnection could encourage policy makers to ensure access.
Methods:
Data Source and Population:
We conducted a cross-sectional analysis using publicly-available data from the COVID-19 supplement as part of the Medicare Current Beneficiary Survey (MCBS).36 The MCBS is a rotating panel survey of a nationally representative sample of the Medicare population that has been carried out since 1991 by the non-partisan and objective research organization NORC (formerly the National Opinion Research Center) at the University of Chicago, with oversampling of beneficiaries who are Hispanic/Latinx or over 85 years old. The COVID-19 summer supplement includes data for 11,114 community-dwelling Medicare beneficiaries weighted to be nationally representative of 56,094,955 beneficiaries enrolled in Medicare in 2019 continuously through the Summer of 2020. The overall response rate was 78.9. Interviews were conducted by telephone in June and July of 2020. We excluded beneficiaries under 65 years old and those who responded by proxy, which included beneficiaries whose primary language was neither English nor Spanish. Because these data were publicly available and de-identified, IRB review was not required by Yale University. This study followed the STROBE guideline for reporting for cross-sectional studies.37
Variables:
Our dependent variables were responses to two questions, which both assessed Medicare beneficiaries’ feelings and were similar to questions asked on the 20-item UCLA Loneliness Scale:38 “Since the coronavirus outbreak began, have you felt more lonely or sad, less lonely or sad, or about the same?” and “Since the coronavirus outbreak began, have you felt more socially connected to family and friends, less socially connected to family and friends, or about the same?”. Beneficiaries were asked to choose one of the three options for each question. We included all answers in descriptive analyses, and for regression models collapsed these into dichotomous variables: “more lonely or sad” vs. not and “less socially connected” vs. not. Beneficiaries who used a proxy were not asked these questions. Because the question asking about loneliness also addressed sadness, we examined the correlation between reporting feeling “more lonely or sad” and a history of depression to determine whether this question measured loneliness or sadness distinctly from depression. The correlation coefficient was 0.12 so we treated “more lonely or sad” as a distinct measure.
Our independent variables of interest included race/ethnicity, access to the beneficiary’s regular primary care since COVID-19 started, and access to the internet. Race/ethnicity was determined by respondent self-report, and NORC grouped these into “Black”, “Hispanic”, “Other”, and “White”. We defined beneficiaries not able to access their regular primary care as those who said they were “unable to get ‘Treatment for an Ongoing Condition’ or ‘A Regular Check-up’ because of the coronavirus outbreak”. We defined internet access as a “yes” answer to “Do you have access to the internet?”.
Additional covariates of interest included: age, sex, Medicaid eligibility, living in a metropolitan area, limited English proficiency, and living alone. Age was available as two categories: 65–74 years old, and 75 and over. Sex was self-reported as one of two categories: female or male. Medicaid dual-eligibility was used as a proxy for socioeconomic status (SES), because income is a less reliable marker for SES in older, retired individuals.39 Residence in a metropolitan area was categorized as yes or no, using Core Based Statistical Area (CBSA) guidelines: metropolitan statistical areas have at least one urbanized area of 50,000 or more population, plus adjacent territory that has a high degree of social and economic integration with the core as measured by commuting ties. Beneficiaries with limited English proficiency were identified by completing the survey in Spanish. We identified people who lived alone through a response of “beneficiary lives alone” to a question asking if anyone else in the house has been told they have COVID. We also included self-reported history of either dementia or depression.
Data Analysis:
We calculated descriptive statistics on the overall sample, and compared responses to the questions about loneliness or sadness and feeling socially disconnected across sociodemographic characteristics, medical history, and primary care and internet access using chi-squared tests. Next, we constructed two sets of logistic regression models: one to evaluate our dependent variable of increased loneliness or sadness, and one to evaluate increased feelings of social disconnection. To control for the differential rates of COVID-19 throughout the country by region, time and different local government responses, we included the region of the country and interview week in all models. In order to determine which covariates to include in our multivariable models aside from our variables of interest, we first tested each variable independently with our dependent variables. Our multivariable models added all covariates that had a P value of <0.2 in bivariate analysis.
Interactions:
Most public health measures early in the pandemic focused on limiting interactions with people outside of one’s own household.40 Thus, Medicare beneficiaries living alone may have relied more heavily on access to the internet, or may have found change to their regular primary care more disruptive. We tested whether living alone moderated associations between internet access or primary care access and feelings of loneliness, sadness, or social disconnection using interactions in our fully-adjusted models. Specifically, we included interaction terms between living alone and: 1) internet access and 2) primary care access. Finally, given the high proportion of illness and death among Black and Hispanic/Latinx Americans in the Northeast early in the pandemic, we tested an interaction between race/ethnicity and region in our fully-adjusted models.
Sensitivity Analysis:
Beneficiaries with internet access may not use it for social connection. We performed a sensitivity analysis using a yes/no answer to the question “Since the start of the pandemic, have you participated in video or voice calls or conferencing over the internet, such as with Zoom, Skype, or FaceTime?” in place of the internet access variable. Fifty-seven percent of those with internet access responded “yes” to this question.
All analyses accounted for the complex survey design and weighted sampling probabilities of the data source, and were performed using Stata 16.
Results:
Characteristics of MCBS beneficiaries
After excluding beneficiaries under 65 years of age (n=1,901), those who answered questions by proxy (n=1,054), and those missing responses to questions about loneliness or sadness and feeling socially disconnected (n=34), our analysis included 8,125 beneficiaries, weighted to be representative of approximately 43.7 million Medicare recipients. Overall, 79% were White, 21% lived alone, 91.8% were not dual-eligible for Medicaid, 84% reported access to the internet, and 12% did not have access to primary care because of the COVID-19 pandemic (Table 1).
Table 1:
Loneliness, sadness, and feelings of social disconnection in Medicare recipients 65 and older during the covid pandemic who did not respond by proxy.
| Weighted % (95% CI) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Loneliness or Sadness | Feelings of Social Disconnection | ||||||||
| Characteristic | All beneficiaries included in MCBS COVID-19 supplement* no. (weighted %) | Increased | About the Same | Decreased | P value for group | Increased | About the Same | Decreased | P value for group |
| All beneficiaries | 8,159 (100) | 22.6 (21.6–23.6) | 74.9 (73.9– 75.9) | 2.5 (2.2–3.0) | 37.1 (35.5–38.6) | 51.1 (49.5–52.6) | 11.9 (10.9–12.9) | ||
| Age group | 0.049 | <0.001 | |||||||
| 65–74 years | 3,756 (64.7) | 23.3 (21.9–24.7) | 74.0 (72.5–75.4) | 2.7 (2.1–3.3) | 39.1 (37.0–41.1) | 48.7 (46.6–50.7) | 12.3 (10.7–13.8 ) | ||
| 75+ years | 4,403 (35.4) | 21.2 (19.9–22.5) | 76.5 (75.2–77.9) | 2.3 (1.8–2.8) | 33.4 (31.9–34.9) | 55.4 (53.7–57.2) | 11.2 (10.1–12.3) | ||
| Gender | <0.001 | <0.001 | |||||||
| Female | 4,667 (56.5) | 27.8 (26.4–29.3) | 69.5 (68.0–71.0) | 2.7 (2.1–3.3) | 41.0 (39.1–43.0) | 48.3 (46.5–50.0) | 10.7 (9.4–12.0) | ||
| Male | 3,492 (43.5) | 15.7 (14.2–17.2) | 81.9 (80.4–83.5) | 2.3 (1.8–2.9) | 31.9 (30.0–33.8) | 54.7 (52.5–56.9) | 13.4 (12.0–14.8) | ||
| Race/Ethnicity | <0.001 | <0.001 | |||||||
| Black, non-Hispanic | 643 (8.5) | 17.1 (13.9–20.3) | 78.7 (75.6–81.9) | 4.2 (2.6–5.7) | 23.4 (18.5–28.2) | 59.2 (53.5–64.8) | 17.5 (13.7–21.2) | ||
| Hispanic | 698 (6.9) | 28.1 (24.1–32.0) | 67.9 (63.8–72.0) | 4.1 (2.4–5.7) | 33.6 (29.0–38.2) | 52.4 (47.7–57.1) | 14.0 (10.1–17.8) | ||
| Other/Unknown | 401 (5.8) | 21.6 (17.2–25.9) | 74.4 (69.8–78.9) | 4.1 (1.9–6.2) | 35.8 (29.6–42.0) | 49.7 (43.9–55.4) | 14.5 (10.1–18.9) | ||
| White, non-Hispanic | 6,417 (78.8) | 22.7 (21.5–24.0) | 75.1 (73.9–76.4) | 2.1 (1.7–2.6) | 38.9 (37.1–40.1) | 50.2 (48.4–51.9) | 10.9 (9.8–12.0) | ||
| Medicaid eligibility | <0.001 | <0.001 | |||||||
| Full | 508 (5.1) | 25.9 (21.3–30.5) | 67.4 (62.5–72.3) | 6.7 (4.1–9.3) | 26.9 (21.8–32.0) | 58.0 (52.9–63.2) | 15.1 (11.2–18.9) | ||
| Partial | 359 (3.2) | 19.1 (14.3–24.0) | 77.7 (72.7–82.7) | 3.1(0.9–5.4) | 27.8 (22.1–33.4) | 58.9 (52.4–65.4) | 13.3 (8.8–17.9) | ||
| None | 7,292 (91.8) | 22.5 (21.4–23.6) | 75.2 (74.1–76.3) | 2.3 (1.9–2.7) | 37.9 (36.3–39.6) | 50.4 (48.8–52.0) | 11.7 (10.6–12.7) | ||
| Live in metropolitan area | 0.004 | 0.003 | |||||||
| Yes | 6,307 (80.9) | 23.5 (22.4–24.6) | 73.8 (72.7–74.9) | 2.7 (2.2–3.1) | 37.8 (36.0–39.5) | 49.9 (48.1–51.8) | 12.3 (11.1–13.5) | ||
| No | 1,847 (19.2) | 18.7 (16.5–20.9) | 79.4 (77.0–81.8) | 1.9 (0.8–3.0) | 34.0 (30.9–37.2) | 55.9 (52.8–58.9) | 10.1 (8.6–11.6) | ||
| Limited English Proficiency (LEP) | <0.001 | <0.001 | |||||||
| Yes | 333 (2.7) | 22.6 (21.5–23.6) | 70.4 (65.3–75.4) | 7.2 (3.4–10.9) | 24.9 (19.6–30.1) | 57.1 (50.8–63.5) | 18.0 (12.9–23.1) | ||
| No | 7,826 (97.3) | 22.6 (21.5–23.6) | 75.0 (74.0–76.1) | 2.4 (2.0–2.8) | 37.4 (35.8–39.0) | 50.9 (49.3–52.5) | 11.7 (10.7–12.7) | ||
| Live alone | <0.001 | 0.06 | |||||||
| Yes | 2,012 (21.5) | 29.9 (27.5–32.4) | 67.5 (64.9–70.2) | 2.5 (1.6–3.5) | 34.6 (32.0–37.1) | 54.2 (51.3–57.0) | 11.3 (9.5–13.0) | ||
| No | 6,132 (78.5) | 20.5 (19.4–21.7) | 76.9 (75.7–78.1) | 2.5 (2.1–3.0) | 37.8 (36.0–40.0) | 50.2 (48.4–52.0) | 12.0 (10.8–13.2) | ||
| Prior depression diagnosis | <0.001 | 0.001 | |||||||
| Yes | 1,667 (21.5) | 33.4 (30.7–36.1) | 63.1 (60.3–65.8) | 3.6 (2.4–4.7) | 42.1 (39.2–45.1) | 45.6 (42.5–48.7) | 12.2 (9.9–14.6) | ||
| No | 6,472 (78.6) | 19.6 (18.4–20.8) | 78.2 (77.0–79.3) | 2.3 (1.9–2.7) | 35.7 (33.9–37.5) | 52.5 (50.8–54.3) | 11.8 (10.6–12.9) | ||
| Prior dementia diagnosis | 0.21 | 0.008 | |||||||
| Yes | 162 (1.5) | 26.5 (18.5–34.6) | 69.2 (61.1–77.3) | 4.3 (0.9–7.7) | 30.0 (21.8–38.2) | 63.2 (54.9–71.4) | 6.8 (3.8–9.8) | ||
| No | 7,985 (98.5) | 22.5 (21.5–23.5) | 75.0 (74.0–76.0) | 2.5 (2.1–2.9) | 37.2 (35.6–38.8 | 50.9 (49.3–52.4) | 12.0 (10.9–13.0) | ||
| Internet access | 0.01 | <0.001 | |||||||
| Yes | 6,437 (84.5) | 23.2 (22.1–24.3) | 74.4 (73.3–75.5) | 2.5 (2.0–2.9) | 39.0 (37.4–40.7) | 48.8 (47.2–50.5) | 12.1 (11.0–13.3) | ||
| No | 1,682 (15.6) | 19.2 (16.8–21.6) | 77.7 (75.0–80.3) | 3.1 (2.2–3.9) | 26.4 (24.0–28.7) | 63.2 (60.2–66.1) | 10.5 (8.5–12.4) | ||
| Access to primary care during COVID pandemic | 0.007 | <0.001 | |||||||
| Yes | 7,253 (88.3) | 21.8 (20.7–22.8) | 75.8 (74.7–76.8) | 2.5 (2.1–2.9) | 35.9 (34.3–37.5) | 52.3 (50.7–53.9) | 11.8 (10.7–12.9) | ||
| No | 871 (11.7) | 28.2 (24.2–32.2) | 69.0 (64.7–73.3) | 2.8 (1.1–4.5) | 45.6 (41.6–50.0) | 41.9 (37.7–46.1) | 12.5 (9.8–15.3) | ||
Weighted percentages reflect MCBS complex survey weighting and do not perfectly match the raw numbers
Loneliness or Sadness
Since the pandemic began, 22.6% of beneficiaries reported increased loneliness or sadness, 74.9% reported no change, and 2.5% reported decreased loneliness or sadness. Rates of loneliness or sadness were higher among women (27.8% vs. 15.7% men), those with lower SES (25.9% with full Medicaid eligibility vs 22.5% without Medicaid), who live alone (29.9% vs. 20.5% who live with others), and with a history of depression (33.4% vs. 19.6% without) (Table 1).
In unadjusted analyses, Hispanic beneficiaries had the highest odds of feeling lonely or sad (28.1% vs. 17.1% Black, 21.6% other, and 22.7% White; OR=1.28 vs. White; 95% CI: 1.03–1.60) to the internet was associated with higher odds of feeling lonely or sad (23.2% vs. 19.2%; OR=1.23; 95% CI: 1.04–1.45; p=0.02), whereas access to regular primary care during the pandemic was associated with lower odds of feeling lonely or sad (21.8% vs. 28.2%; Odds Ratio [OR]=0.73, 95% confidence interval [CI], 0.59–0.90; P=0.004) (Figure 1; Table 2).
Figure 1:
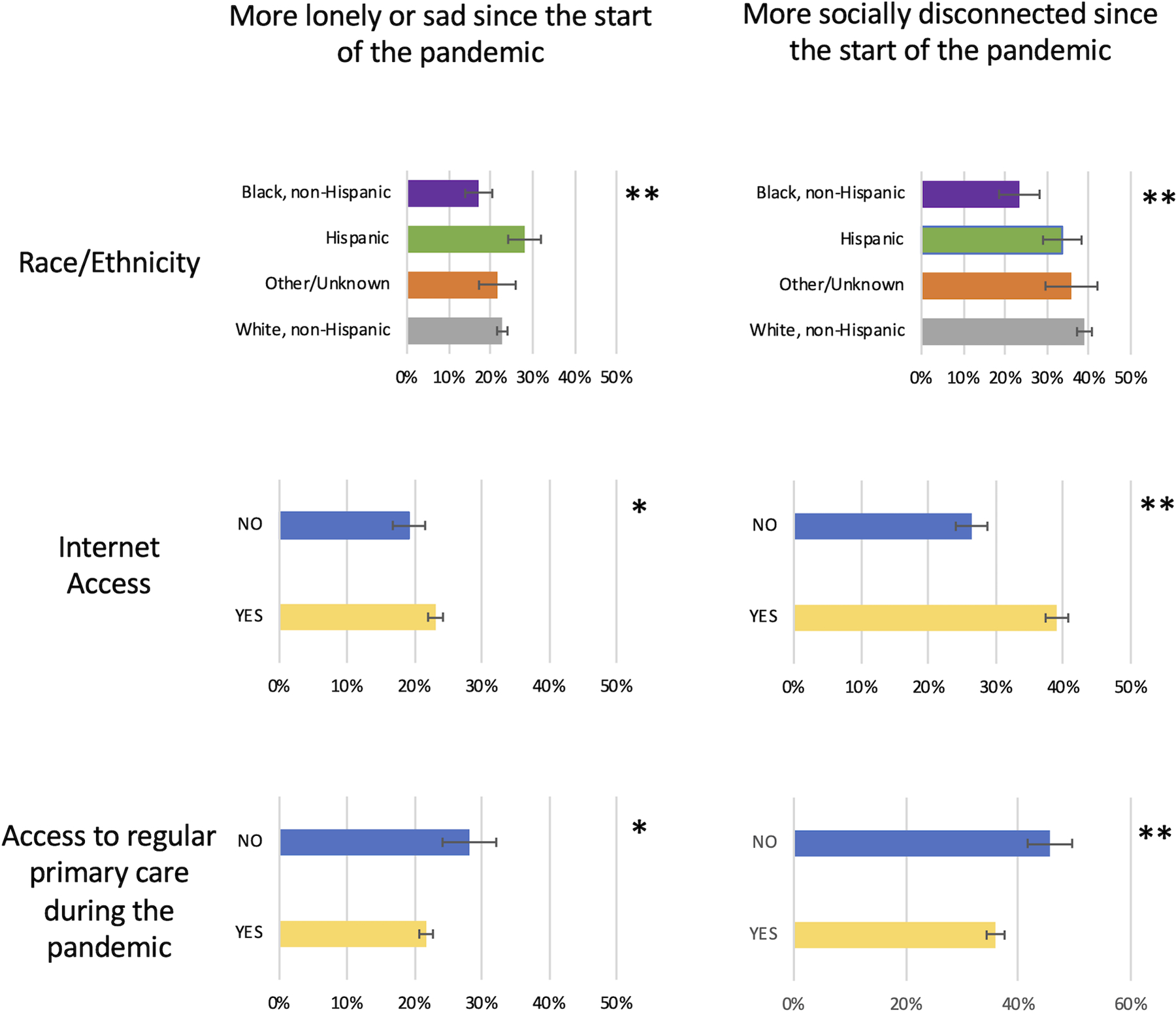
Self-reported loneliness or sadness and feelings of social disconnection among Medicare beneficiaries >65 years old since the start of the COVID-19 pandemic
* p<.05
** p<.001
Table 2.
Unadjusted logistic regression models, by primary variables of interest*
| Characteristic (P value for group) | Increased loneliness or sadness Odds Ratio (CI) N = 8,117 |
Increased feelings of social disconnection Odds Ratio (CI) N = 8,122 |
|---|---|---|
| Race/Ethnicity | P=0.002 | P<0.001 |
| Black, non-Hispanic | 0.74 (0.57–0.96) | 0.51 (0.38–0.67) |
| Hispanic | 1.28 (1.03–1.60) | 0.80 (0.64–1.00) |
| Other/Unknown | 0.91 (0.69–1.21) | 0.88 (0.67–1.16) |
| White, non-Hispanic | ref | ref |
| Internet Access | P=0.02 | P<0.001 |
| Yes | 1.23 (1.04–1.45) | 1.75 (1.54–2.00) |
| No | ref | ref |
| Access to primary care during COVID-19 pandemic | P=0.004 | P<0.001 |
| Yes | 0.73 (0.59–0.90) | 0.68 (0.58–0.80) |
| No | ref | ref |
All models control for region and interview week.
In the fully-adjusted model, beneficiaries who identified as Hispanic/Latinx had higher odds of feeling lonely or sad (OR: 1.30; CI: 1.02–1.65; P value for joint test of race/ethnicity = 0.02). Those with access to the internet also had higher odds (OR: 1.29; CI: 1.07–1.56; P=0.009), whereas those with access to regular primary care had lower odds of feeling lonely or sad (OR=0.77; 95% CI, 0.61–0.96; P=0.02). Several other characteristics were associated with higher odds of loneliness or sadness, including female gender (OR: 1.89; CI: 1.63–2.19; P<0.001), living in a metropolitan area (OR: 1.33; CI: 1.15–1.55; P<0.001), living alone (OR: 1.61; CI: 1.38–1.88, P<0.001), and having a history of depression (OR: 1.86; CI: 1.57–2.19), P<0.001) (Table 3).
Table 3.
Fully adjusted logistic regression models showing odds of increased loneliness or sadness, by beneficiary characteristics*
| Characteristic (P value for group) | Odds Ratio (CI) N= 8,011 |
|---|---|
| Race/Ethnicity | P=0.02 |
| Black, non-Hispanic | 0.78 (0.60–1.02) |
| Hispanic | 1.30 (1.02–1.65) |
| Other/Unknown | 1.02 (0.75–1.39) |
| White, non-Hispanic | ref |
| Access to internet | P=0.009 |
| Yes | 1.29 (1.07–1.56) |
| No | ref |
| Access to primary care during COVID-19 pandemic | P=0.02 |
| Yes | 0.77 (0.61–0.96) |
| No | ref |
| Age group | P=0.06 |
| 65–74 years | ref |
| 75+ years | 0.89 (0.80–1.00) |
| Gender | P<0.001 |
| Female | 1.89 (1.63–2.19) |
| Male | ref |
| Medicaid eligibility | P=0.22 |
| Full | 1.06 (0.80–1.43) |
| Partial | 0.76 (0.53–1.08) |
| None | ref |
| Live in metropolitan area | P<0.001 |
| Yes | ref |
| No | 0.75 (0.64–0.87) |
| Live alone | P<0.001 |
| Yes | 1.61 (1.38–1.88) |
| No | ref |
| Prior depression diagnosis | P<0.001 |
| Yes | 1.86 (1.57–2.19) |
| No | ref |
All models control for region and interview week.
Feelings of Social Disconnection
Overall, 37.1% of beneficiaries reported feeling more disconnected since the start of the COVID-19 pandemic, 51.1% reported no change, and 11.9% reported feeling less disconnected. Feeling socially disconnected was more common among younger people (39.1% ages 65–74 vs. 33.4% of >75-year-olds), women (41.1% vs. 31.9% of men), those with higher socioeconomic status (37.9% of those with no Medicaid eligibility vs. 26.9% with full Medicaid), those whose primary language is English (37.4% vs. 24.9% with limited English proficiency), and those with a history of depression (42.1% vs. 35.7% without) (Table 1).
In unadjusted analyses, Black beneficiaries had the lowest odds of feeling socially disconnected (23.4% vs. 33.6% Hispanic, 35.8% other, and 38.9% White; OR=0.51 vs. White; 95% CI: 0.38–0.67) access to the internet was associated with higher odds of feeling disconnected (39.0% vs. 26.4%; OR=1.75; 95% CI: 1.54–2.00; P<0.001), whereas access to primary care during the pandemic was associated with lower odds of feeling disconnected (35.9% vs 45.6%; OR=0.68, CI: 0.58–0.81, P<0.001) (Figure 1; Table 2).
In the fully-adjusted model, Black beneficiaries had lower odds of feeling disconnected (OR: 0.55; CI: 0.42–0.73; P value for joint test of race/ethnicity <0.001). Those with access to their regular primary care also had lower odds of feeling disconnected (OR: 0.73; CI: 0.61–0.87, P=0.001), and those with access to the internet had higher odds of feeling disconnected (OR: 1.42; CI: 1.24–1.63; P<0.001). Several other sociodemographic characteristics were associated with higher odds of feeling disconnected, including younger age (OR for 65–74 years old: 1.19; CI: 1.08–1.32; P=0.001), female gender (OR: 1.52; CI: 1.36–1.71; P<0.001), living in a metropolitan area (OR: 1.22; CI: 1.04–1.44; P=0.02), and having a history of depression (OR: 1.23; CI: 1.05–1.43); P=0.01). (Table 4).
Table 4.
Logistic regression models showing odds of increased feelings of social disconnection, by beneficiary characteristics*
| Characteristic (P value for group) | Model 2c Odds Ratio (CI) N = 8,016 |
|---|---|
| Race/Ethnicity | P<0.001 |
| Black, non-Hispanic | 0.55 (0.42–0.73) |
| Hispanic | 1.01 (0.73–1.40) |
| Other/Unknown | 0.92 (0.70–1.21) |
| White, non-Hispanic | ref |
| Internet access | P<0.001 |
| Yes | 1.42 (1.24–1.63) |
| No | ref |
| Access to primary care during COVID pandemic | P=0.001 |
| Yes | 0.73 (0.61–0.87) |
| No | Ref |
| Age group | P=0.001 |
| 65–74 years | Ref |
| 75+ years | 0.84 (0.76–0.93) |
| Gender | P<0.001 |
| Female | 1.52 (1.36–1.71) |
| Male | Ref |
| Medicaid eligibility | P=0.17 |
| Full | 0.80 (0.59–1.08) |
| Partial | 0.79 (0.57–1.08) |
| None | Ref |
| Limited English proficiency | P=0.05 |
| Yes | 0.63 (0.40–1.00) |
| No | Ref |
| Live in metropolitan area | P=0.02 |
| Yes | Ref |
| No | 0.82 (0.69–0.97) |
| Live alone | P=0.05 |
| Yes | 0.87 (0.75–1.00) |
| No | Ref |
| Prior depression diagnosis | P=0.01 |
| Yes | 1.23 (1.05–1.43) |
| No | Ref |
| Prior dementia diagnosis | P=0.40 |
| Yes | 0.83 (0.54–1.28) |
| No | Ref |
All models control for region and interview week.
Interactions
In the fully-adjusted models, those who lived alone were significantly more likely to report loneliness or sadness if they had access to the internet (P<0.001). There was no association between internet access and loneliness or sadness for those who did not live alone. This interaction was not significant for feelings of social disconnection. Living alone did not moderate the association between primary care access and feelings of loneliness, sadness, or social disconnection. There was no significant interaction between race and region.
Sensitivity Analysis:
In our full models for loneliness or sadness and feelings of social disconnection, substituting use of internet for video or voice calls for our internet access variable did not change our findings. In addition, the interaction between living alone and using internet for video or voice calls was not significant.
Discussion:
In this analysis of data from the nationally-representative Medicare Current Beneficiary Survey, our findings support prior research demonstrating increases in loneliness and feeling socially disconnected since the start of the COVID-19 pandemic.1–5 We expand upon previous findings by looking specifically at those 65 and over using nationally-representative data. We find differences across racial groups, further contextualize associations with internet access, and offer new insights related to access to regular primary care.
Research conducted prior to the COVID-19 pandemic has been inconsistent regarding racial/ethnic differences in loneliness and feeling socially disconnected.19–21 A study conducted during the pandemic using a nationally-representative sample over 50 years old found that Black and Hispanic/Latinx respondents were less likely than White respondents to report loneliness.1 Our findings were consistent with regard to Black Americans, who were least likely to report loneliness, sadness, or feelings of social disconnection. Prior work is consistent in the finding that Black Americans are more likely to live in multigenerational homes,21–25 and there is evidence that older Black Americans are most likely to participate in religious activities,41,42 which may have been an important social network during the pandemic and protective against feelings of loneliness. In contrast, Hispanic/Latinx beneficiaries in our sample of over 65-year-olds were most likely to report loneliness or sadness, which differs from findings in the over 50 age group.1 Prior to the COVID-19 pandemic, one study found that Hispanic/Latinx older adults were least likely to report their mental health as good, and most likely to have negative mental health effects from objective social isolation compared with White and Black older adults.21 Thus, our findings of more loneliness or sadness among Hispanic/Latinx beneficiaries could be related to the high prevalence of SARS-CoV-2 infections and mortality among Hispanic/Latinx communities.26 One pre-pandemic abstract suggested that social ties to friends were more important for preventing loneliness in older Hispanic/Latinx adults than ties to family,43 and ties to friends may have been more disrupted by COVID-19 precautions.
Internet access was associated with more loneliness and feelings of disconnection, which is in line with several studies conducted prior to the pandemic.30,31 Interestingly, this finding was driven by Medicare beneficiaries who lived alone. Internet access was not associated with a difference in loneliness for those who did not live alone. This is in contrast to findings from a pre-pandemic cross-sectional study among a large European sample, which found that internet access mitigated loneliness in adults over 50.44 It may be that older adults in particular benefit from guidance on using it for social connection. For example, a study conducted prior to the pandemic that introduced internet to older adults living in assisted living facilities for the explicit purpose of social connection found that those taught to use the internet were less likely to report both loneliness and perceived social isolation.45 Guidance on appropriate internet use may also be helpful as older adults increasingly rely on technology for health information.46 Other studies conducted during the pandemic suggest that internet is inadequate to replace in-person contact.2,5 Indeed, phone calls appear to be a more effective way of facilitating feelings of social connection.47,48
Those who had access to their regular primary care provider during the pandemic were less likely to report increased loneliness or sadness and feelings of disconnection than those who had to forego their regular care. Prior work has shown that lonely people are more likely to utilize health care.33,49,50 Thus, having to forego primary care appointments during the pandemic may have exacerbated loneliness and feelings of disconnection for those who rely on this outlet for connection. It is also possible that those who retained access to their PCP during the pandemic had earlier interventions to mitigate loneliness or feelings of disconnection. For example, the care team could encourage safe ways of remaining connected.32 Finally, it may be that this finding is the result of confounding, for example due to barriers to access to care that also increase risk of loneliness, such as geographic or transportation barriers or residual confounding from SES. Those who were able to maintain their regular primary care may have had better social connections in the first place. Nonetheless, clinicians should ask patients about feelings of loneliness, particularly older adults.32
Limitations
Our study has several limitations. First, our results may not be generalizable to Medicare beneficiaries who live in nursing homes or who have severe dementia. The survey only included Medicare beneficiaries who live in the community and not nursing homes, and we limited analyses to beneficiaries who did not require a proxy. Second, beneficiaries were asked about their experiences of “loneliness or sadness” in one question, but the low correlation between responses to this question and depression suggests this is measuring a distinct phenomenon. Further, both domains, loneliness and sadness, reflect important aspects of patient experience, and these findings were broadly consistent with feelings of social disconnection. Third, we could not control for factors related to living situation, including family structure, because those data were not available. We did account for living alone, which is associated with loneliness and social isolation. Fourth, this study was conducted early in the pandemic, and one study demonstrated attenuation of feelings of loneliness as time progressed from initial shelter in place orders.2
Conclusions
Loneliness, sadness, and feelings of social disconnection are increasing among older adults in the United States as a result of the COVID-19 pandemic. Surprisingly, Black Americans, who have had the highest rates of sickness and death from COVID-19, are least likely to report feelings of loneliness and social disconnection. This may be the result of multigenerational households or religious networks. Hispanic/Latinx older adults were most likely to report loneliness or sadness, and this finding warrants further exploration. Internet access is not a universal solution, and policy makers should consider telephone-based interventions to build community and decrease loneliness. Access to regular primary care may help to alleviate loneliness and feelings of social disconnection. Health systems should provide tools to clinicians to address loneliness and prioritize maintaining access to primary care. This may include ongoing support for telehealth or video visits, which would be helpful for patients with limited access to care. Patients report a desire to speak with their physicians about loneliness,20 and clinicians should prompt these discussions by asking their patients about these feelings.32
Key points:
Feelings of loneliness and social disconnection differed by race
Those with internet were more lonely
Access to primary care mitigated loneliness
Why this paper matters?
Loneliness and feelings of disconnection are risk factors for morbidity and mortality; maintaining access to primary care may help
ACKNOWLEDGEMENTS:
Funding:
LH is supported by the VA Office of Academic Affiliations through the VA/National Clinician Scholars Program and Yale University and through NIA (T32AG066598). SM is supported through the National Clinician Scholars Program and Yale University. This publication was made possible by CTSA Grant Number TL1 TR001864 from the National Center for Advancing Translational Science (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH. CO receives funding from NHLBI (1K01HL145347–01A1). BR receives funding from NHLBI (1K08 HL143133–01A1). JR currently receives research support through Yale University from Johnson and Johnson to develop methods of clinical trial data sharing, from the Medical Device Innovation Consortium as part of the National Evaluation System for Health Technology (NEST), from the Food and Drug Administration for the Yale-Mayo Clinic Center for Excellence in Regulatory Science and Innovation (CERSI) program (U01FD005938); from the Agency for Healthcare Research and Quality (R01HS022882), from the National Heart, Lung and Blood Institute of the National Institutes of Health (NIH) (R01HS025164, R01HL144644), and from the Laura and John Arnold Foundation to establish the Good Pharma Scorecard at Bioethics International.
Footnotes
Conflict of Interest Summary: All authors report no conflicts of interest.
Sponsor’s Role: No funder/sponsor had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and the decision to submit the manuscript for publication.
References
- 1.Choi EY, Farina MP, Wu Q, Ailshire J. COVID-19 Social Distancing Measures and Loneliness Among Older Adults. J Gerontol B Psychol Sci Soc Sci 2021. [DOI] [PMC free article] [PubMed]
- 2.Kotwal AA, Holt-Lunstad J, Newmark RL, et al. Social Isolation and Loneliness Among San Francisco Bay Area Older Adults During the COVID-19 Shelter-in-Place Orders. J Am Geriatr Soc 2021;69(1):20–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoffman GJ, Malani PN, Solway E, Kirch M, Singer DC, Kullgren JT. Changes in activity levels, physical functioning, and fall risk during the COVID-19 pandemic. J Am Geriatr Soc 2021. [DOI] [PubMed]
- 4.Wong SYS, Zhang D, Sit RWS, et al. Impact of COVID-19 on loneliness, mental health, and health service utilisation: a prospective cohort study of older adults with multimorbidity in primary care. Br J Gen Pract 2020;70(700):e817–e824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hawkley LC, Finch LE, Kotwal AA, Waite LJ. Can remote social contact replace in-person contact to protect mental health among older adults? J Am Geriatr Soc 2021. [DOI] [PMC free article] [PubMed]
- 6.Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. The Lancet Public Health 2020;5(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Courtin E, Knapp M. Social isolation, loneliness and health in old age: a scoping review. Health Soc Care Community 2017;25(3):799–812. [DOI] [PubMed] [Google Scholar]
- 8.Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med 2012;172(14):1078–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart 2016;102(13):1009–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging 2010;25(2):453–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav 2009;50(1):31–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson RS, Krueger KR, Arnold SE, et al. Loneliness and risk of Alzheimer disease. Arch Gen Psychiatry 2007;64(2):234–240. [DOI] [PubMed] [Google Scholar]
- 13.Ong AD, Uchino BN, Wethington E. Loneliness and Health in Older Adults: A Mini-Review and Synthesis. Gerontology 2016;62(4):443–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cudjoe TKM, Roth DL, Szanton SL, Wolff JL, Boyd CM, Thorpe RJ. The Epidemiology of Social Isolation: National Health and Aging Trends Study. J Gerontol B Psychol Sci Soc Sci 2020;75(1):107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kotwal AA, Cenzer IS, Waite LJ, et al. The epidemiology of social isolation and loneliness among older adults during the last years of life. J Am Geriatr Soc 2021. [DOI] [PMC free article] [PubMed]
- 16.National Academies of Sciences E, Medicine. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System Washington, DC: The National Academies Press; 2020. [PubMed] [Google Scholar]
- 17.Valtorta N, Hanratty B. Loneliness, isolation and the health of older adults: do we need a new research agenda? J R Soc Med 2012;105(12):518–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coyle CE, Dugan E. Social isolation, loneliness and health among older adults. J Aging Health 2012;24(8):1346–1363. [DOI] [PubMed] [Google Scholar]
- 19.Skarupski KA, Mendes de Leon CF, Bienias JL, et al. Black-white differences in depressive symptoms among older adults over time. J Gerontol B Psychol Sci Soc Sci 2005;60(3):P136–142. [DOI] [PubMed] [Google Scholar]
- 20.Mullen RA, Tong S, Sabo RT, et al. Loneliness in Primary Care Patients: A Prevalence Study. Ann Fam Med 2019;17(2):108–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miyawaki CE. Association of social isolation and health across different racial and ethnic groups of older Americans. Ageing Soc 2015;35(10):2201–2228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beck RW, Beck SH. The incidence of extended households among middle-aged black and white women: estimates from a 15-year panel study. J Fam Issues 1989;10(2):147–168. [DOI] [PubMed] [Google Scholar]
- 23.Aquilino WS. The Likelihood of Parent-Adult Child Coresidence: Effects of Family Structure and Parental Characteristics. Journal of Marriage and Family 1990;52(2):405–419. [Google Scholar]
- 24.Amorim M, Dunifon R, Pilkauskas N. The magnitude and timing of grandparental coresidence during childhood in the United States. Demographic Research 2017;37:1695–1706. [Google Scholar]
- 25.Cross CJ. Extended family households among children in the United States: Differences by race/ethnicity and socio-economic status. Popul Stud (Camb) 2018;72(2):235–251. [DOI] [PubMed] [Google Scholar]
- 26.Gross CP, Essien UR, Pasha S, Gross JR, Wang SY, Nunez-Smith M. Racial and Ethnic Disparities in Population-Level Covid-19 Mortality. J Gen Intern Med 2020;35(10):3097–3099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rossen LM, Branum AM, Ahmad FB, Sutton P, Anderson RN. Excess Deaths Associated with COVID-19, by Age and Race and Ethnicity - United States, January 26-October 3, 2020. MMWR Morb Mortal Wkly Rep 2020;69(42):1522–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Escalante E, Golden RL, Mason DJ. Social Isolation and Loneliness: Imperatives for Health Care in a Post-COVID World. JAMA 2021;325(6):520–521. [DOI] [PubMed] [Google Scholar]
- 29.Meier DE, Morrison RS. All you need is love: Yet another social determinant of health. J Am Geriatr Soc 2021. [DOI] [PMC free article] [PubMed]
- 30.Amichai-Hamburger Y, Ben-Artzi E. Loneliness and Internet Use. Computers in Human Behavior 2003(19):71–80. [Google Scholar]
- 31.Nowland R, Necka EA, Cacioppo JT. Loneliness and Social Internet Use: Pathways to Reconnection in a Digital World? Perspect Psychol Sci 2018;13(1):70–87. [DOI] [PubMed] [Google Scholar]
- 32.Cudjoe TKM, Kotwal AA. “Social Distancing” Amid a Crisis in Social Isolation and Loneliness. J Am Geriatr Soc 2020;68(6):E27–E29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gerst-Emerson K, Jayawardhana J. Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. American journal of public health 2015;105(5):1013–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Internet/Broadband Fact Sheet https://www.pewresearch.org/internet/fact-sheet/internet-broadband/. Published 2019. Accessed 12/01/2020, 2020.
- 35.Shi L, Chen CC, Nie X, Zhu J, Hu R. Racial and socioeconomic disparities in access to primary care among people with chronic conditions. J Am Board Fam Med 2014;27(2):189–198. [DOI] [PubMed] [Google Scholar]
- 36.Medicare Current Beneficiary Survey (MCBS). Centers for Medicare & Medicaid Services https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MCBS. Published 2020. Accessed 11/20/2020, 2020.
- 37.von Elm E, Altman DG, Egger M, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335(7624):806–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess 1996;66(1):20–40. [DOI] [PubMed] [Google Scholar]
- 39.Social Risk Factors and Performance Under Medicare’s Value-Based Purchasing Programs Washington D.C. : United States Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation; December 2016 2016. [Google Scholar]
- 40.Polisena J, Ospina M, Sanni O, et al. Public health measures to reduce the risk of SARS-CoV-2 transmission in Canada during the early days of the COVID-19 pandemic: a scoping review. BMJ open 2021;11(3):e046177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Taylor RJ, Chatters LM, Taylor HO. Race and Objective Social Isolation: Older African Americans, Black Caribbeans, and Non-Hispanic Whites. J Gerontol B Psychol Sci Soc Sci 2019;74(8):1429–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taylor RJ, Chatters LM, Jackson JS. Religious and spiritual involvement among older african americans, Caribbean blacks, and non-Hispanic whites: findings from the national survey of american life. J Gerontol B Psychol Sci Soc Sci 2007;62(4):S238–250. [DOI] [PubMed] [Google Scholar]
- 43.Peek MK. Loneliness in Older Hispanics: Who Matters More—Friends or Family? Innovation in Aging 2017;1(suppl_1):1030–1030. [Google Scholar]
- 44.Silva P, Matos AD, Martinez-Pecino R. Can the internet reduce the loneliness of 50+ living alone? Information, Communication & Society 2020:1–17.
- 45.Cotten SR, Anderson WA, McCullough BM. Impact of internet use on loneliness and contact with others among older adults: cross-sectional analysis. J Med Internet Res 2013;15(2):e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee DR, Lo JC, Ramalingam N, Gordon NP. Understanding the Uptake of Digital Technologies for Health-Related Purposes in Frail Older Adults. J Am Geriatr Soc 2021;69(1):269–272. [DOI] [PubMed] [Google Scholar]
- 47.Kahlon MK, Aksan N, Aubrey R, et al. Effect of Layperson-Delivered, Empathy-Focused Program of Telephone Calls on Loneliness, Depression, and Anxiety Among Adults During the COVID-19 Pandemic: A Randomized Clinical Trial. JAMA Psychiatry 2021. [DOI] [PMC free article] [PubMed]
- 48.Chatterjee P, Yatnatti SK. Intergenerational Digital Engagement: A Way to Prevent Social Isolation During the COVID-19 Crisis. J Am Geriatr Soc 2020;68(7):1394–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jovicic A, McPherson S. To support and not to cure: general practitioner management of loneliness. Health Soc Care Community 2020;28(2):376–384. [DOI] [PubMed] [Google Scholar]
- 50.Ellaway A, Wood S, Macintyre S. Someone to talk to? The role of loneliness as a factor in the frequency of GP consultations. British Journal of General Practice 1999. [PMC free article] [PubMed]


