Abstract
Myocardial infarction has a high mortality rate worldwide. Therefore, clinical intervention in cardiac remodeling after myocardial infarction is essential. Açai pulp is a natural product and has been considered a functional food because of its antioxidant/anti-inflammatory properties. The aim of the present study was to analyze the effect of açai pulp supplementation on cardiac remodeling after myocardial infarction in rats. After 7 days of surgery, male Wistar rats were assigned to six groups: sham animals fed standard chow (SA0, n = 14), fed standard chow with 2% açai pulp (SA2, n = 12) and fed standard chow with 5% açai pulp (SA5, n = 14), infarcted animals fed standard chow (IA0, n = 12), fed standard chow with 2% açai pulp (IA2, n = 12), and fed standard chow with 5% açai pulp (IA5, n = 12). After 3 months of supplementation, echocardiography and euthanasia were performed. Açai pulp supplementation, after myocardial infarction, improved energy metabolism, attenuated oxidative stress (lower concentration of malondialdehyde, P = 0.023; dose-dependent effect), modulated the inflammatory process (lower concentration of interleukin-10, P<0.001; dose-dependent effect) and decreased the deposit of collagen (lower percentage of interstitial collagen fraction, P<0.001; dose-dependent effect). In conclusion, açai pulp supplementation attenuated cardiac remodeling after myocardial infarction in rats. Also, different doses of açai pulp supplementation have dose-dependent effects on cardiac remodeling.
Introduction
Cardiovascular disease (CVD) is a major cause of morbidity and mortality worldwide. Myocardial infarction (MI) is associated with a higher mortality rate than other CVDs [1]. MI is defined as a focus of necrosis resulting from low tissue perfusion, with signs and symptoms consequent to cardiac cell death [2]. Cellular and molecular alterations initiate a cascade of intracellular signaling, which increases inflammation, oxidative stress, apoptosis, and changes in cardiac energy metabolism [3, 4]. Initially, cardiac remodeling is a relevant factor in the progression of CVD because it plays a fundamental role in the pathophysiology of ventricular dysfunction [5, 6].
Therefore, inflammatory processes and oxidative stress are potential targets for attenuating cardiac remodeling and reducing mortality after MI. In this context, specific foods with high antioxidant properties have been used as sources of cardioprotective compounds [7–9]. Açai (Euterpe oleracea Mart.) is a plant in the Arecaceae family and a palm fruit native to the Amazon region of Brazil. Açai seeds have been used in animal foods, plantations and home gardens. Açai pulp is a functional food, consumed in energy drinks, ice cream, juice, and pharmaceutical products; and used in cosmetics [10, 11]. Notably, the consumption of açai pulp has been increasing worldwide.
Açai seed and pulp are rich in several phytochemicals but differ in the degree of richness. Açai seeds contain 65% fiber, 5% protein, 2% lipids, 2% mineral salts, and 28.3% polyphenols (catechin, epicatechin, and polymeric and oligomeric proanthocyanidins) [12]. Açai pulp contains 48% lipids, 25% total sugars, 13% protein, a small amount of fiber, vitamins (A, B1, B2, B3, C, and E), and 25.5% polyphenols (predominantly cyanidin 3-glucoside and cyanidin 3-rutinoside) [13, 14].
In experimental models, açai seed supplementation was performed using hydroalcoholic seed extract (ASE) [15, 16]. Because the seeds are not edible, supplementation has been achieved using açai capsules in clinical studies. Additionally, açai pulp is edible and more attractive than the seeds because of its sensorial characteristics (i.e., appearance, texture, and taste). These characteristics remain unchanged when the pulp is pasteurized and frozen for storage [17]. Thus, açai pulp can be easily used in clinical and experimental studies [18–20].
Studies have shown in experimental models that ASE supplementation has anti-inflammatory [15, 16] and antioxidative activities [21, 22]. This anti-inflammatory activity was also observed in açai pulp supplementation by decreased transcription of nuclear factor kappa B (NF-κB) in the brain [23]. In addition, supplementation with açai pulp decreased the concentration of interferon-gamma (IFN-γ) in individuals with metabolic syndrome [20].
Regarding antioxidative activity, supplementation with açai pulp decreased nitric oxide in microglial cells [24]. Studies performed in different clinical situations reported that açai pulp supplementation increased total antioxidant capacity (TAC) and attenuated exercise-induced muscle damage in junior athletes [25], increased catalase and TAC, and reduced the production of reactive species (RS) and malondialdehyde (MDA) in healthy volunteers [19, 26].
Açai pulp supplementation has also promoted benefits in the heart; for instance, a study of doxorubicin-induced cardiotoxicity in rats found attenuation of this toxicity by decreased oxidative damage (increased glutathione peroxidase and decreased lipid hydroperoxide concentration). Furthermore, açai pulp supplementation improved energy metabolism in the heart (increased β-hydroxyacyl-CoA dehydrogenase, decreased phosphofructokinase; and increased citrate synthase, complex II, and adenosine triphosphate [ATP] synthase enzymatic activities) [27].
In a search of electronic libraries (PubMed, Scopus, and Cochrane) for information on MI and açai supplementation, two articles were found. An experimental model of coronary artery ligation [28], and a global ischemia-reperfusion model in rats [29]. In the first study, açai seed supplementation was performed for 4 weeks, and the rats received 100 mg/kg/day of ASE. The authors observed attenuation in hypertrophy (decreased heart weight), fibrosis (decreased collagen deposition in the left ventricle), and cardiac dysfunction (alterations in arterial and left ventricular pressure) [28]. In the second study, the authors supplemented 5% of açai pulp for 6 weeks and observed an improvement in energy metabolism and attenuation of oxidative stress [29]. Thus far, whether açai pulp supplementation affects cardiac remodeling after MI remains unknown. Although açai pulp has antioxidant and anti-inflammatory activities, its chemical composition differs from that of the seed, as afore mentioned.
Therefore, the aim of this study was to evaluate the effect of açai pulp supplementation in rat chow on cardiac remodeling after MI by modifying oxidative stress, energy metabolism, and inflammatory pathways.
Materials and methods
All experiments and procedures were performed in accordance with the National Institute of Health’s Guide for the Care and Use of Laboratory Animals and with the Ethical Principles in Animal Experimentation adopted by the Brazilian College of Animal Experimentation. The study protocol (n°1066/2013) was submitted and approved by the Botucatu Medical School Animal Research Ethics Committee.
Male Wistar rats weighing from 200 to 250 g. Animals were subjected to MI according to a method previously described [2, 30] or sham surgery. After surgery, rats were housed in individual cages, in a temperature-controlled room (24°C) with a 12-hour light/12-hour dark cycle. Water was supplied ad libitum, and food was controlled.
After the initial echocardiographic exam, animals were allocated into six groups: (1) sham animals fed standard chow (SA0, n = 14); (2) sham animals fed standard chow with 2% açai pulp (SA2, n = 12); (3) sham animals fed standard chow with 5% açai pulp (SA5, n = 14); (4) infarcted animals fed standard chow (IA0, n = 12); (5) infarcted animals fed standard chow with 2% açai pulp (IA2, n = 12); and (6) infarcted animals fed standard chow with 5% açai pulp (IA5, n = 12). Supplementation was performed for 90 days. After this period, the animals were evaluated using the final echocardiographic exam.
Experimental MI
Animals were anesthetized with ketamine (70 mg/kg) and xylazine (1 mg/kg); next, the heart was exteriorized, and the left coronary artery was ligated with 5–0 mononylon between the pulmonary outflow tract and left atrium. Heart was replaced in the thorax, the lungs were inflated by positive pressure, and the thoracotomy was closed [2, 30]. In the sham group, the same MI procedure was performed but without coronary occlusion.
Açai supplementation
Açai pulp was purchased commercially (Icefruit®) from the same batch, homogenized, packed in one-liter bottles, and stored at -80°C for later use in chow. The açai pulp was analyzed, and the total phenolic compounds expressed as a quantity of gallic acid were 170 mg/100 g [31], antioxidant activity was 48.3 g of 2,2-diphenyl-1-picrylhydrazyl (DPPH)/kg [32], and total anthocyanin was 15.6 mg/100g [33]. We also determined fat content (6%) and water content (88%). Supplementation doses of 2% and 5% were chosen based on De Souza et al. (2012) [34] and Fragoso et al. (2013) [35], respectively. Nuvilab chow (Nuvital®) was used for all animals. Chow was initially chopped for the later addition of açai pulp, and the mixture was pelleted and dried at ambient temperature. The chow was stored at -20°C.
Seven days after surgery, an initial echocardiographic exam was performed, and the animals were allocated into groups to start açai supplementation for 3 months. The food intake of all animals was measured periodically. The mean daily intake of each rat was then calculated.
Echocardiographic study
At both time points (i.e., initial echocardiographic exam 7 days after surgery and final exam after 90 days of supplementation), animals were evaluated using a transthoracic echocardiographic exam. All measurements were performed according to the method recommended by the American Society of Echocardiography [36] and validated in the infarcted rat model in our laboratory [37]. The equipment used was General Electric Medical Systems, model Vivid S6 (Tirat Carmel, Israel) with a multifrequency transducer of 5 to 11.5 MHz. Mitral inflow and aortic flow were assessed using the same transducer operating at 5.0 MHz.
The initial echocardiographic examination was performed on infarcted animals to check the infarct size and fraction area variation, to homogenize infarct size among the groups. In the final echocardiographic examination, cardiac structures were measured in at least five consecutive cardiac cycles [38, 39].
Morphometric analysis
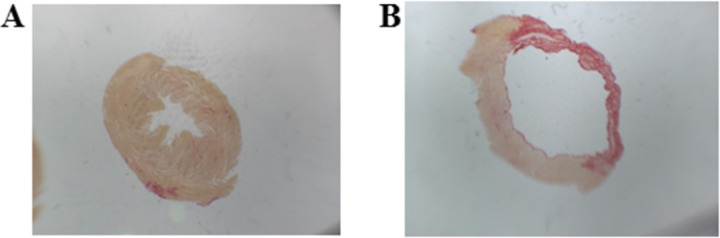
Transverse sections (5 μm) of the left ventricles (LVs) were performed in paraffin blocks and stained with hematoxylin and eosin for cardiomyocyte cross-sectional area (CSA), and with Picrosirius Red Stain for interstitial collagen fraction (ICF) and infarction size calculations. The infarct size was calculated using the following formula: [(endocardial + epicardial circumferences of the infarcted area) / (endocardial + epicardial ventricular circumferences) × 100] (Fig 1). This method is considered more precise than echocardiography analysis because echocardiogram measure only the endocardial perimeter of the infarct, which may be overestimated by the infarction expansion process [40]. In this study, animals with infarcted area smaller than 30% were excluded.
Fig 1. Myocardial infarcted area.
(A) Sham animal heart, (B) Infarcted animal heart.
CSA was measured from 70 cells per ventricle. Digital images were collected (400 × magnification) using a video camera attached to a Leica microscope. ICF was determined in remote cardiac areas free from MI from at least 30 digital images (400 × magnification). All images were collected with a video camera attached to a Leica microscope, and the images were analyzed with the Image-Pro Plus 3.0 software program (Media Cybernetics, Silver Spring, MD, USA).
Lipid hydroperoxide, oxidative stress, and energy metabolism enzymes
Protein extraction was performed on LV samples to determine the lipid hydroperoxide (LH) concentration and enzyme activities. Glutathione peroxidase (GPx, E.C.1.11.1.9), superoxide dismutase (SOD, E.C.1.15.1.1), and catalase (CAT, E.C.1.11.1.6) activities were assessed as previously described [41, 42]. Cardiac energy metabolism was assessed using β-hydroxyacyl coenzyme-A dehydrogenase (β-OHADH, E.C.1.1.1.35.), lactate dehydrogenase (LDH, E.C.1.1.1.27), pyruvate dehydrogenase complex (PDH), citrate synthase (CS; E.C.4.1.3.7.), complex I (NADH: ubiquinone oxidoreductase), complex II (succinate dehydrogenase), and ATP synthase (EC 3.6.3.14) activities, as previously described [42].
Spectrophotometric determinations were performed using a Pharmacia Biotech Spectrophotometer UV/visible Ultrospec 5000 with Swift II Application software for computer system control, 974213 (Cambridge, England, UK) at 560 nm.
Malondialdehyde concentration
Protein extraction was performed on LV samples and quantified using the Bradford method [43]. The extraction was conducted in red light 1 day before the analysis. MDA concentration was determined by the method in (Nielsen et al. [1997]). Fluorometric detection was performed at 527 nm of excitation and 551 nm of emission [44].
Cytokine production and tissue inhibitor of metalloproteinase-1 evaluation
Tumor necrosis factor-α (TNF-α), IFN-γ, interleukin-10 (IL-10) and tissue inhibitor of metalloproteinase-1 (TIMP-1) concentrations were determined. Protein extraction was performed on the LV samples and quantified using the Bradford method [43]. The extraction was evaluated by ELISA, according to the manufacturer’s instructions (R&D Systems, Minneapolis, MN, USA).
Western blot analysis
Nuclear erythroid factor-2 (Nrf-2), NF-κB, and pNF-κB total and phosphorylated (NF-κB and pNF-κB, respectively), collagen I, collagen III, and caspase-3 expression were determined. LV samples were extracted using radioimmunoprecipitation assay buffer or nuclear extraction buffer. Protein content was quantified using the Bradford method [43], and samples containing 50 μg of protein were separated by electrophoresis using a Mini-Protean 3 Electrophoresis Cell (Bio-Rad, Hercules, CA, USA) system and transferred to a nitrocellulose membrane. The membrane was blocked and incubated with primary antibodies. The membrane was then washed with TBS and Tween 20 and incubated with the appropriate secondary peroxidase-conjugated antibody. A SuperSignal® West Pico Chemiluminescent Substrate (Pierce Protein Research Products, Rockford, IL, USA) was used to detect bound antibodies. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) mouse monoclonal (Santa Cruz Biotechnology Inc., Europe) was used for normalization.
Statistical analysis
Data are presented as the mean ± standard error of the mean (SEM). Variables with no normal distribution were normalized using the most suitable mathematical transformation. For data that could not be normalized, we used the Kruskal Wallis test (comparison among sham groups SA0, SA2, and SA5 and among infarcted groups IA0, IA2, and IA5) and the Mann Whitney test (comparison between groups: SA0 and IA0; SA2 and IA2; and SA5 and IA5). Then, Bonferroni correction was performed.
Data were analyzed by 2-factor ANOVA: (1) factor one: presence of MI (I); (2) factor two: açai supplementation (A); and (3) interaction between factors I and A. When a significant interaction between factors was observed, Holm Sidak multiple comparisons were used. When no interaction was found, the factors were separated to assess whether MI animals differed from sham animals and whether supplemented animals differed from those without supplementation.
The results are as follows: (1) changes promoted by MI, corresponding to comparisons between the SA0 and IA0 groups in case of interactions, and comparisons between all animals with or without MI in the absence of interaction between the factors; (2) the effect of açai supplementation in MI animals, corresponding to the comparison among groups IA0, IA2, and IA5 in the presence of interaction; and (3) the effect of açai supplementation in all animals in the absence of interaction between the factors. Thus, in this last situation, we interpreted the results by indicating the effect of açai supplementation in a general action in the heart. In this manner, we also observed this action in MI.
One-factor ANOVA was used to compare infarction size in the infarcted groups. Spearman’s rank correlation coefficient test was performed to compare the dose-dependent effects of açai supplementation. Differences were considered statistically significant if P<0.05. Statistical analyses were performed using SigmaStat for Windows software version 3.5 (Systat Software Inc. San Jose, CA, USA).
Results
Survival, food intake, and body weight
Mortality during the experimental period was as follows: one animal of the sham animals, eight animals from IA0, six from IA2, and five from IA5 (P = 0.728). As expected, no differences were observed in the initial echocardiographic examination (Table 1). In addition, no difference was observed in the infarction size among the infarcted groups in relation to food intake and body weight (Table 2).
Table 1. Initial echocardiographic exam (7 days after surgery).
| Groups | P value | |||
|---|---|---|---|---|
| IA0 (n = 11) | IA2 (n = 12) | IA5 (n = 12) | P | |
| Diastolic area (mm2) | 65.3±3.32 | 66±.2.31 | 60.3±1.66 | 0.209 |
| Sistolic area (mm2) | 44.4±2.74 | 44.8±2.85 | 40.1±2.14 | 0.362 |
| % MI | 38±2.96 | 37.3±2.94 | 36.2±2.38 | 0.899 |
| FAC (%) | 32.3±1.99 | 32.6±2.57 | 33.8±2.39 | 0.890 |
I: infarction; S: sham; A: açai; A0: no supplementation; A2: 2% of açai supplementation; A5: 5% of açai supplementation. FAC: fractional area change. Data are expressed as mean ± SEM. it was performed 1-factor ANOVA.
Table 2. Echocardiographic and morphometric data.
| Groups | P values | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| SA0 (n = 14) | SA2 (n = 13) | SA5 (n = 14) | IA0 (n = 12) | IA2 (n = 12) | IA5 (n = 12) | P (I) | P (A) | P (IxA) | |
| Food intake (g) | 23±0.6 | 22.6±0.7 | 23.7±0.6 | 24.8±0.5 | 23.1±0.5 | 23.2±0.8 | 0.257 | 0.254 | 0.194 |
| Initial BW (g) | 266±9 | 260±9 | 275±8 | 252±5 | 260±8 | 258±7 | 0.133 | 0.605 | 0.595 |
| Final BW (g) | 430±10 | 432±14 | 436±11 | 452±11 | 445±13 | 447±13 | 0.127 | 0.949 | 0.906 |
| Infarction size (%) | - | - | - | 42.8±1.9 | 39.7±2.7 | 42.1±1.8 | - | 0.556 | - |
| *LVSD/BW (mm/kg) | 9.52±0.43 | 9.39±0.29 | 8.81±0.33 | 17.5±0.98 | 17.6±1.09 | 18.5±0.84 | <0.0011 | 0.994 | 0.297 |
| *LVDD/BW (mm/kg) | 18.4±0.3 | 18.8±0.5 | 17.8±0.5 | 22.7±0.8 | 22.9±1 | 23.3±0.8 | <0.0011 | 0.901 | 0.428 |
| *LVMI (g/kg) | 1.7±0.04 | 1.8±0.07 | 1.7±0.07 | 3.3±0.21 | 3±0.2 | 3.2±0.22 | <0.0011 | 0.921 | 0.217 |
| #LA/BW (mm/kg) | 12±0.3 | 13±0.4 | 12±0.3 | 16±1 | 15±1.1 | 15±0.9 | 0.0051 | 0.132 | 0.665 |
| #FAC (%) | 69±1.7 | 67±1.1 | 68±1.2 | 32±3 | 33±1.8 | 31±3.3 | <0.0051 | 0.538 | 0.605 |
| *Ejection fraction | 86±1.3 | 87±1.2 | 88±0.7 | 54±3.8 | 55±3.5 | 50±3.2 | <0.0011 | 0.794 | 0.338 |
| E’ media (cm/s) | 3.9±0.2 | 4.1±0.2 | 4.1±0.1 | 3.9±0.2 | 3.6±0.2 | 3.6±0.1 | 0.0121 | 0.988 | 0.176 |
| *A’ media (mm2) | 3.7±0.2 | 3.5±0.2 | 3.3±0.2 | 2.9±0.2 | 2.9±0.3 | 3.5±0.4 | 0.0131 | 0.583 | 0.100 |
| CSA (μm2) | 207±34 | 252±27 | 245±25 | 304±28 | 275±30 | 289±28 | 0.0271 | 0.923 | 0.422 |
I: infarction; S: sham; A: açai; A0: no supplementation; A2: 2% açai supplementation; A5: 5% açai supplementation; BW: body weight; LVSD: left ventricular systolic diameter; LVDD: left ventricular diastolic diameter; LVMI: left ventricular mass index; LA: left atrium; FAC: fractional area change; E’ media: average between early diastolic wave of the mitral annulus lateral and septal; A’ media: average between late diastolic wave of the mitral annulus lateral and septal; CSA: cardiomyocyte cross-sectional area. Data are expressed as mean ± SEM. Bold numbers represents significant effects considered.
1 Comparisons for I factor: infarcted animals different from sham animals.
* variables normalized for 2-factor ANOVA test.
# Mann Whitney and Kruskal Wallis.
Effect of MI in the rat heart
MI promoted myocardial remodeling by morphological changes (higher LV systolic and diastolic diameter adjusted by body weight, higher LV mass index, left atrium, and CSA) and functional changes (systolic: lower fractional area change and ejection fraction; and diastolic: lower E’ media and A’ media) (Table 2).
Changes in energy metabolism were as follows: abnormal oxidation of fatty acids (lower β-OHADH), lower glucose oxidation (lower activity of PDH), lower CS, lower electron transport chain complexes (lower activity of complex I and complex II), lower ATP synthase, and higher lactate production from pyruvate (higher LDH activity). No difference was observed in phosphofructokinase (PFK) activity (Table 3). An antioxidant imbalance was also observed (higher LH and MDA concentrations, higher SOD activity, lower GPx activity, and Nrf-2 expression). No difference was observed in CAT activity (Table 4). MI led to inflammatory alterations (higher IL-10 and lower INF-y concentrations). No differences were observed in NF-κB total and phosphorylated (NF-κB and pNF-κB, respectively) expression (Table 5 and S1 Fig). A higher deposition of collagen was observed after MI (higher concentration of TIMP-1, percentage of ICF, and expression of collagen I). No differences were observed in the expression of collagen III and caspase-3 (Table 6, S2 and S3 Figs).
Table 3. Energy metabolism markers.
| Groups | P values | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| SA0 (n = 8) | SA2 (n = 8) | SA5 (n = 8) | IA0 (n = 8) | IA2 (n = 8) | IA5 (n = 8) | P (I) | P (A) | P (IxA) | |
| β-OHADH (nmol/g) | 33.1±2.02 | 33.6±1.87 | 37.2±1.54 | 20.2±1.45 | 19.0±1.6 | 24.6±1.41 | <0.0011 | 0.0142 | 0.823 |
| #LDH (nmol/g) | 70.3±2.66a | 81.1±7.27 | 65.6±6.42 | 139±6.39a,A,C | 70.1±1.77A | 65.4±2.16C | <0.005 | 0.880 | <0.0053 |
| #PFK (nmol/g) | 143±5.9 | 141±9.2 | 133±9.1 | 155±4.67 | 152±5.4 | 143±9.2 | 0.129 | 0.939 | 0.447 |
| PDH (nmol/g) | 286±12.1 | 300±15.5 | 317±15.5 | 218±15.4 | 293±15.6 | 298±11.4 | 0.0111 | <0.0012 | 0.085 |
| *CS (nmol/g) | 86.3±8.15 | 108±10.2 | 131±9.87 | 51.8±2.37 | 62.6±5.27 | 62.6±3.95 | <0.0011 | 0.0022 | 0.291 |
| *complex I (nmol/g) | 5.19±0.07a | 4.99±0.14b | 5.11±0.10 | 3.39±0.29a,C | 3.37±0.35b,B | 4.78±0.22B,C | <0.001 | 0.015 | 0.0153 |
| complex II (nmol/g) | 5.54±0.34 | 4.66±0.34 | 4.73±0.31 | 3.09±0.16 | 2.99±0.18 | 3.48±0.25 | <0.0011 | 0.208 | 0.094 |
| ATP synthase (nmol/g) | 37.4±0.91a, E | 35.9±1.16b,D | 31.4±1.39c,D,E | 20.6±1.01a | 21.9±1.06b | 20.1±0.98c | <0.001 | 0.007 | 0.049 |
I: infarction; S: sham; A: açai; A0: no supplementation; A2: 2% açai supplementation; A5: 5% açai supplementation. β-OHADH: β-hydroxyacyl coenzyme-A dehydrogenase; LDH: lactate dehydrogenase; PFK: Phosphofructokinase; PDH: pyruvate dehydrogenase complex; CS: citrate synthase. Data are expressed as mean ± SEM. Bold numbers represents significant effects considered.
1 Comparisons for I factor: infarcted animals different from sham animals.
2 Comparisons for açai factor, β-OHADH: animals A0≠animals A5 and animals A2≠animals A5; PDH: animals A0≠animals A2 and animals A0≠animals A5; CS: animals A0≠animals A2 and animals A0≠animals A5.
3 IxA: when interactions are observed, same superscript letters represents differences (P<0.05).
*variables normalized for 2-factor ANOVA test.
#Mann Whitney and Kruskal Wallis.
Table 4. Oxidative stress markers.
| Groups | P values | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| SA0 (n = 8) | SA2 (n = 8) | SA5 (n = 8) | IA0 (n = 8) | IA2 (n = 8) | IA5 (n = 8) | P (I) | P (A) | P (IxA) | |
| *LH (nmol/mg) | 250±10.9 | 241±13.5 | 251±11.9 | 301±15 | 286±15.2 | 254±15.4 | 0.0041 | 0.251 | 0.169 |
| MDA (μmol/g) | 0.35±0.05a | 0.36±0.03b | 0.31±0.04 | 1.32±0.25a,A,C | 0.77±0.12b,A | 0.61±0.12C | <0.001 | 0.013 | 0.0233 |
| CAT (μmol/mg) | 64.5±4.23 | 59.1±5.11 | 56.6±4.04 | 47.8±3.17 | 61±3.62 | 60.5±7 | 0.351 | 0.709 | 0.065 |
| SOD (nmol/mg) | 7.06±0.36a | 7.34±0.36b | 7.59±0.31 | 8.95±0.38a,C | 8.74±0.54b,B | 6.9±0.41B,C | 0.011 | 0.095 | 0.0063 |
| GPx (nmol/mg) | 45.0±3.1 | 43.9±1.87 | 45.6±1.82 | 34.6±1.44 | 39.9±2.31 | 43.6±2.92 | 0.0061 | 0.133 | 0.179 |
| (n) Espression Nrf-2 | (8) 1.45±0.31 | (8) 1.48±0.39 | (7) 1.21±0.38 | (6) 1.05±0.34 | (8) 0.66±0.18 | (8) 0.75±0.16 | 0.0291 | 0.674 | 0.760 |
I: infarction; S: sham; A: açai; A0: no supplementation; A2: 2% açai supplementation; A5: 5% açai supplementation. LH: lipid hydroperoxide; MDA: malondialdehyde; CAT: catalase; SOD: superoxide dismutase; GPx: glutathione peroxidase; Nrf-2: expression of nuclear factor erythroid-2. Data are expressed as mean ± SEM. Bold numbers represents significant effects considered.
1 Comparisons for I factor: infarcted animals different from sham animals.
3 IxA: when interactions are observed, same superscript letters represents differences (P<0.05).
*variables normalized for 2-factor ANOVA test.
Table 5. Production of cytokines inflammatory.
| Groups | P values | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| SA0 | SA2 | SA5 | IA0 | IA2 | IA5 | P (I) | P (A) | P (IxA) | |
| (n) IL-10 (pg/mg) | (6) 3.21±0.47a,E | (6) 4.81±0.71D | (6) 8.49±1.c,D,E | (6) 6.83±0.44a,A,C | (6) 4.75±0.62A,B | (6) 2.48±0.27c,B,C | 0.123 | 0.529 | <0.0013 |
| INF-γ (pg/mg) | (6) 0.48±0.19 | (5) 1.05±0.32 | (5) 1.33±0.22 | (6) 0.48±0.18 | (6) 0.62±0.27 | (4) 0.13±0.08 | 0.0081 | 0.276 | 0.054 |
| #TNF-α (pg/mg) | (6) 0.10±0.01 | (6) 0.02±0.02 | (6) 0.78±0.47 | (6) 0.24±0.16 | (6) 0.92±0.49 | (6) 0.53±00.33 | 0.699 | 0.250 | 0.427 |
| Expression p NF-κB | (8) 0.85±0.10 | (8) 1.24±0.14 | (6) 1.08±0.21 | (6) 1.25±0.21 | (6) 1.03±0.27 | (7) 1.06±0.16 | 0.696 | 0.872 | 0.222 |
| Expression NF-κB | (8) 0.94±0.16 | (8) 1.16±0.12 | (6) 1.09±0.25 | (6) 1.20±0.17 | (6) 0.96±0.20 | (7) 1.03±0.17 | 0.990 | 0.997 | 0.415 |
| *Expression p NF-κB / NF-κB | (8) 1.00±0.10 | (8) 1.05±0.05 | (6) 0.97±0.13 | (6) 1.02±0.07 | (6) 0.86±0.06 | (7) 0.91±0.11 | 0.191 | 0.663 | 0.377 |
I: infarction; S: sham; A: açai; A0: no supplementation; A2: 2% açai supplementation; A5: 5% açai supplementation. IL-10: interleukin 10; INF-γ: interferon γ; TNF-α: tumor necrosis factor-α, NF-κB: nuclear factor kappa B. Data are expressed as mean ± SEM. Bold numbers represents significant effects considered.
1 Comparisons for I factor: infarcted animals different from sham animals.
3 IxA: when interactions are observed, same superscript letters represents differences (P<0.05).
*variables normalized for 2-factor ANOVA test.
#Mann Whitney and Kruskal Wallis.
Table 6. Collagen degradation markers and caspase-3.
| Groups | P values | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| SA0 | SA2 | SA5 | IA0 | IA2 | IA5 | P (I) | P (A) | P (IxA) | |
| *TIMP-1 (pg/mg) | (6) 8.94±2.48a | (4) 9.42±0.90 | (2) 18.1±8.85 | (4) 51.4±13.5a,A,C | (4) 12.3±1.62A | (4) 8.25±1.95C | 0.055 | 0.049 | <0.0013 |
| *ICF (%) | (8) 2.19±0.3a,E,F | (8) 3.09±0.9b,F | (8) 3.08±0.3c,E | (8) 10.4±1.5a,C | (8) 10.2±1.4b,B | (8) 8.07±1.8c,B,C | <0.001 | 0.090 | <0.0013 |
| Expression Collagen I | (8) 0.73±0.13 | (6) 0.87±0.17 | (6) 0.73±0.16 | (6) 1.22±0.21 | (6) 1.18±0.29 | (6) 0.85±0.14 | 0.0501 | 0.439 | 0.603 |
| Expression Collagen III | (7) 0.84±0.09 | (6) 1.04±0.14 | (6) 1.26±0.24 | (6) 1.14±0.17 | (6) 1.00±0.07 | (6) 1.25±0.14 | 0.503 | 0.164 | 0.464 |
| Expression Caspase-3 | (8) 1.88±0.58 | (7) 2.81±0.73 | (8) 3.21±0.65 | (7) 1.58±0.42 | (8) 2.63±0.68 | (7) 2.36±0.65 | 0.397 | 0.182 | 0.853 |
I: infarction; S: sham; A: açai; A0: no supplementation; A2: 2% açai supplementation; A5: 5% açai supplementation. TIMP-1: tissue inhibitor of metalloproteinase-1; ICF: interstitial collagen fraction. Data are expressed as mean ± SEM. Bold numbers represents significant effects considered.
1 Comparisons for I factor: infarcted animals different from sham animals.
3 IxA: when interactions are observed, same superscript letters represents differences (P<0.05).
*variables normalized for 2-factor ANOVA test.
#Mann Whitney and Kruskal Wallis.
Effect of açai supplementation after MI
Açai supplementation in infarcted animals improved cardiac energy metabolism (higher activity of β-OHADH, PDH, CS, complex I, and lower LDH activity) (Table 3 and Fig 2) and attenuated oxidative stress (lower concentration of MDA and SOD activity) (Table 4 and Fig 3). Furthermore, açai supplementation modulated the inflammatory process (lower concentration of IL-10) (Table 5 and Fig 4) and decreased the deposition of collagen (lower concentration of TIMP-1 and percentage of ICF) (Table 6 and Fig 4).
Fig 2. Energy metabolism enzymes in sham and infarcted rats with and without açai supplementation.
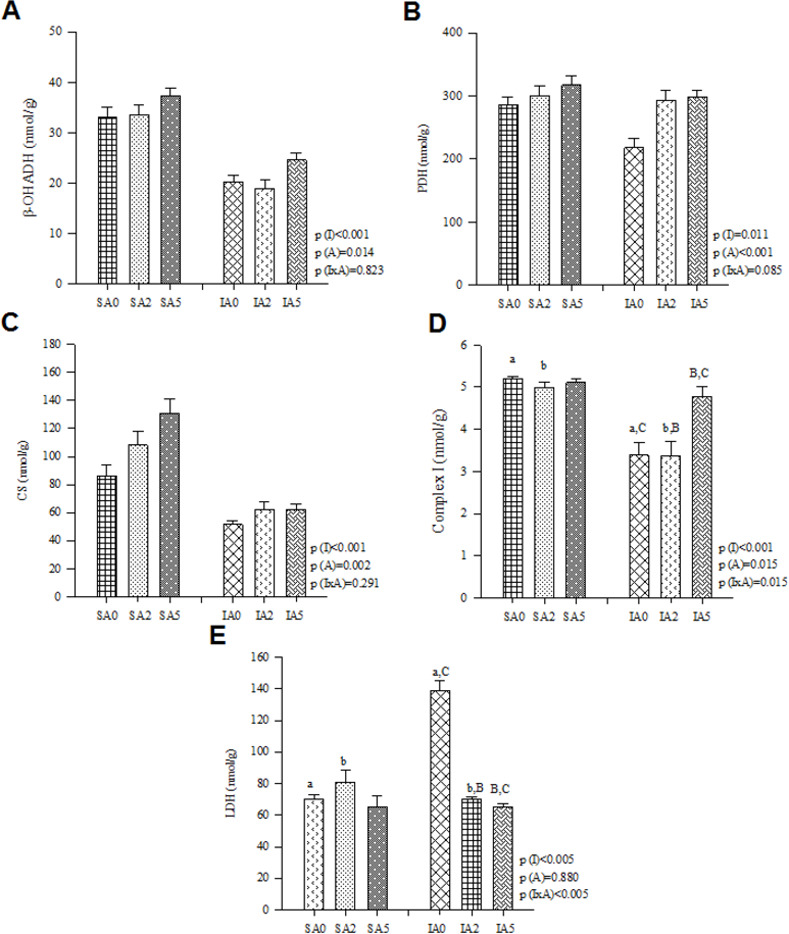
(A) β-OHADH: β-hydroxyacyl coenzyme-A dehydrogenase, (B) PDH: pyruvate dehydrogenase complex, (C) CS: citrate synthase, (D) Complex I, (E) LDH: lactate dehydrogenase. Data are expressed as mean ± SEM. Same letter represents a significant difference between groups (p<0.005). Sample size: SA0 = 8; SA2 = 8; SA5 = 8; IA0 = 8; IA2 = 8; IA5 = 8.
Fig 3. Oxidative stress markers in sham and infarcted rats with and without açai supplementation.
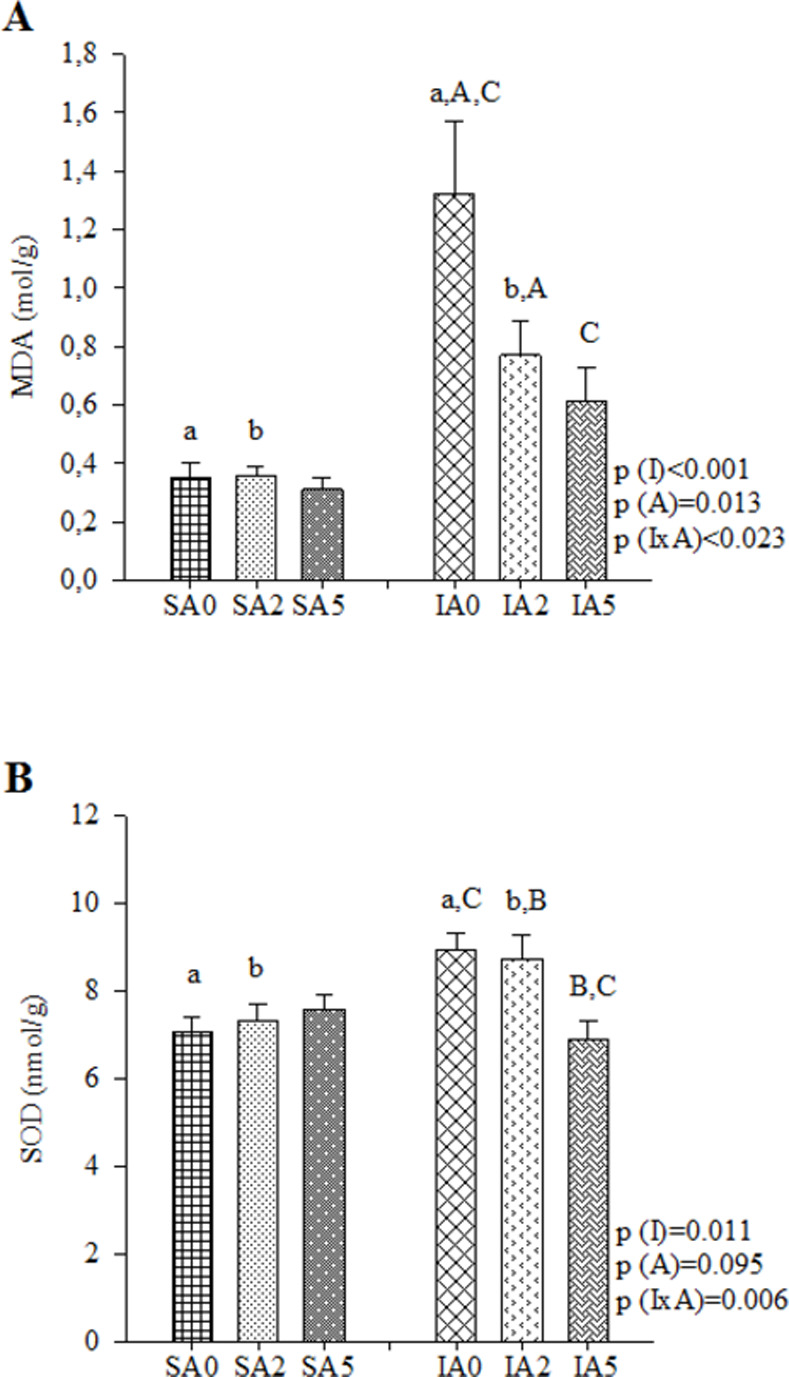
(A) MDA: malondialdehyde, (B) SOD: superoxide dismutase. Data are expressed as mean ± SEM. The same letter represents a significant difference between groups (p<0.005). Sample size: SA0 = 8; SA2 = 8; SA5 = 8; IA0 = 8; IA2 = 8; IA5 = 8.
Fig 4. Inflammatory process and collagen deposit in sham and infarcted rats with and without açai supplementation.
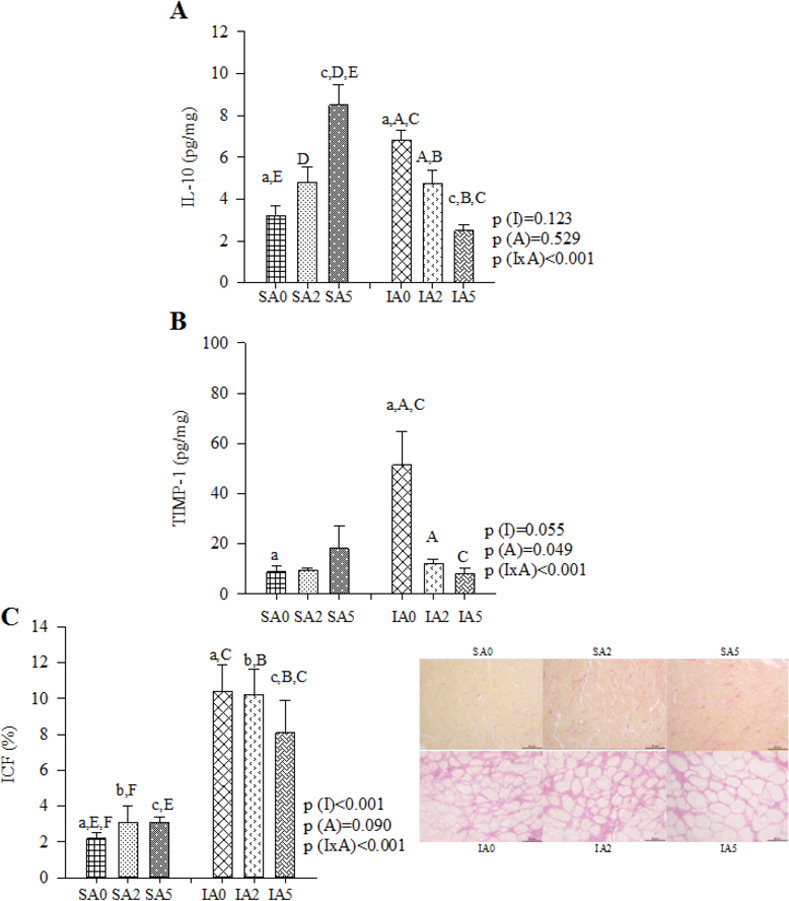
(A) IL-10: interleukin 10. Sample size: SA0 = 6; SA2 = 6; SA5 = 6; IA0 = 6; IA2 = 6; IA5 = 6. (B) TIMP-1: tissue inhibitor of metalloproteinase-1. Sample size: SA0 = 6; SA2 = 4; SA5 = 2; IA0 = 4; IA2 = 4; IA5 = 4. (C) ICF: interstitial collagen fraction. Sample size: SA0 = 8; SA2 = 8; SA5 = 8; IA0 = 8; IA2 = 8; IA5 = 8. Data are expressed as mean ± SEM. The same letter represents a significant difference between groups (p<0.005).
Dose-dependent effects of açai supplementation after MI
Different doses of açai supplementation led to dose-dependent effects. This effect can be observed in antioxidant enzymes: lower SOD activity (P = 0.005), and higher GPx activity (P = 0.014); lipid peroxidation markers: lower concentration of LH (P = 0.034), and MDA (P = 0.009); in energy metabolism enzymes: higher activity of PDH (P = 0.001), CS (P = 0.043), and complex I (P = 0.003); and lower activity of LDH (P<0.001); anti-inflammatory cytokine: lower concentration of IL-10 (P<0.001); and collagen deposit markers: lower percentage of ICF (P = 0.016), and lower concentration of TIMP-1 (P<0.001) (S1 Table).
Discussion
The aim of this study was to analyze the influence of açai supplementation on cardiac remodeling after MI in rats. Our data showed that MI promoted morphological and functional cardiac alterations, altered energy metabolism, increased oxidative stress, worsened the inflammatory process, and increased collagen deposition in the heart. These alterations are characteristic of cardiac remodeling and have been observed in other studies [7–9]. Supplementation of açai in infarcted animals improved energy metabolism, attenuated oxidative stress, modulated the inflammatory process, and decreased fibrosis. Furthermore, açai supplementation resulted in a dose-dependent response.
Influence of açai pulp supplementation in MI heart
Under physiological conditions, fatty acids are used as the main energy substrate. However, after MI, cardiac metabolism changes and glucose oxidation increase energy production [45]. Açai supplementation increased fatty acid oxidation and decreased the glycolytic pathway after MI. These data show that açai increased the use of fatty acids as an energy substrate, which is similar to what occurs in the heart under normal conditions [45]. Moreover, as afore mentioned, açai pulp has a high lipid content (48% of lipids) [13, 14], which may have contributed to the increased use of fatty acids. Furthermore, açai supplementation improved the citric acid cycle and electron transport chain. In the citric acid cycle, acetyl coenzyme A (acetyl CoA) and oxaloacetate are catalyzed by citrate synthase to citrate. At the end of this cycle, it generates additional coenzymes, which are responsible for the electron transport that occurs in the inner membrane of mitochondria to the intermembrane space. Moreover, this electron transfer is mediated by specific complexes I to IV and provides protons for complex V to produce ATP [45, 46]. Thus, açai supplementation improved energy metabolism in the heart. Two other studies have also observed that açai pulp supplementation improves cardiac energy metabolism in the heart in a doxorubicin-induced cardiotoxicity model [27] and in a global ischemia-reperfusion model [29].
After MI, there is an imbalance between RS production and myocardial antioxidant reserves [47]. In addition, changes in cardiac metabolism, increase the generation of superoxide radicals and increase oxidative stress [45]. In oxidative stress, the membrane is one of the cell components most affected by lipid peroxidation in its phospholipids, which causes changes in cell structure and permeability. This lipid peroxidation produces MDA, which is the most abundant end product of lipid peroxidation chain reactions and is commonly used as an indicator of oxidative damage [48, 49]. In our study, açai supplementation decreased the MDA concentration in the heart, leading to an improvement in oxidative stress. In addition, açai supplementation decreased the SOD activity. SOD is an antioxidant enzyme that protects mitochondria against deleterious superoxide radicals in pathophysiological and pathological conditions [50]. Other authors have also observed lower SOD activity in animals supplemented with açai. They suggested that the high levels of antioxidant compounds present in the açai pulp can reduce RS, maintaining redox balance, without the physiological need to increase antioxidant enzyme activity [51–53]. Therefore, the presence of phytochemical compounds, especially polyphenols, has been associated with the effects of açai as an antioxidant via both direct [13] and indirect effects [53–55] in different experimental models. Thus, in this study, the decreased MDA concentration and SOD activity promoted by açai supplementation suggest a reduction in RS in these animals, maintaining redox balance. Decreased SOD activity has also been reported with infarcted animals and supplementation of natural products with antioxidant/anti-inflammatory properties [7, 8].
Regarding the inflammatory response, MI activates innate immunity, characterized by an increase in proinflammatory cytokines (TNF-α, interleukin-1 β (IL-1β), and interleukin-6 (IL-6)) [56]. An anti-inflammatory repair response is initiated, characterized by the activation and accelerated proliferation of fibroblasts [57, 58]. Finally, repairing macrophages are recruited and release inhibitory mediators (i.e., transforming growth factor-β and IL-10), which suppress inflammation and activate profibrotic processes [59]. Thus, the acute inflammatory process after MI is followed by inflammatory balance and tissue repair with stabilization of the healing process [60]. Therefore, the decreased concentration of the anti-inflammatory cytokine IL-10, observed in groups supplemented with açai, suggests that the inflammatory process is balanced and that there is no reason to increase the production of anti-inflammatory cytokines. This balance in the inflammatory process can also be confirmed by the normal values of TNF-α and NF-κB (phosphorylated, total, and its relation).
The participation of the extracellular matrix and its structural elements, such as collagen and other proteins, is also relevant in the remodeling process. The ECM is upregulated by matrix metalloproteinases (MMPs) and downregulated by tissue inhibitors of metalloproteinases (TIMPs) [61]. A study reported that MI promoted an increase in MMP-2 [8]. Therefore, an increase in TIMP-1 in infarcted animals is expected to be a consequence of the increase in MMPs [61]. In our study, açai supplementation decreased TIMP-1 concentration and ICF percentage. Thus, açai supplementation led to a decrease in extracellular matrix degradation and, consequently, a decrease in fibrosis.
This study did not observe an improvement in morphological and functional variables, as evaluated by echocardiography, promoted by açai supplementation. Our study supplemented açai for 3 months after MI, as prior studies performed in our laboratory with an experimental model of infarction have done [7, 8]. Considering these results with açai supplementation, we observed important biochemical improvements. We suggest that an increased supplementation time, would result in improvements in morphological and functional variables. In addition, açai supplementation doses had dose-dependent effects. Thus, increasing the dose of açai supplementation, would improvement the morphological and functional variables.
In this study, açai supplementation with 2% and 5% had a dose-dependent effect on post-MI cardiac remodeling. Regarding the açai dose, concentrations of 2% and 5% in rat chow were equivalent to 15.6 g (1 tablespoons daily) and 39 g (2.5 tablespoons daily) for humans, respectively [62]. Therefore, the amount is not large, açai is a product that can be easily found year-round in Brazil, and the price is affordable.
Conclusion
Açai supplementation attenuated cardiac remodeling after MI in rats. The mechanism involved reduced oxidative stress, improved energy metabolism, modulated the inflammatory process, and decreased fibrosis. Different doses of açai supplementation had dose-dependent effects on cardiac remodeling.
Supporting information
(DOCX)
(A) NF-κB total: nuclear factor kappa B, (B) pNF-κB: nuclear factor kappa B: phosphorylated nuclear factor kappa B. Sample size: SA0 = 8; SA2 = 8; SA5 = 6; IA0 = 6; IA2 = 6; IA5 = 7.
(TIF)
(A) Collagen I. Sample size: SA0 = 8; SA2 = 6; SA5 = 6; IA0 = 6; IA2 = 6; IA5 = 6. (B) Collagen III. Sample size: SA0 = 7; SA2 = 6; SA5 = 6; IA0 = 6; IA2 = 6; IA5 = 6.
(TIF)
(A) Nrf-2: expression of nuclear factor erythroid-2. Sample size: SA0 = 8; SA2 = 8; SA5 = 7; IA0 = 6; IA2 = 8; IA5 = 8. (B) Caspase-3. Sample size: SA0 = 8; SA2 = 7; SA5 = 8; IA0 = 7; IA2 = 8; IA5 = 7.
(TIF)
Acknowledgments
We thank Mario B. Bruno, José Georgette and Antonio Carlos de Lalla for animal management and technical assistance. AMF, SARP, BFP, MFM, LAMZ and PSAG designed the research; AMF, ACC, BPMR, RACS, AFG, TFB, LLI, BCO, BLBP, AAHF and KO conducted the research; AMF and SARP analyzed the data and wrote the paper. SARP had primary responsibility for final content. All authors read and approved the final manuscript.
Data Availability
All files are available from the UNESP database https://repositorio.unesp.br/bitstream/handle/11449/136446/figueiredo_am_me_bot.pdf?sequence=3&isAllowed=y.
Funding Statement
This research was supported in part by Coordenação de Aperfeiçoamento Pessoal de Nível Superior (CAPES), Brazil. The funding source had no involvement in study design, in the collection, analysis and interpretation of data, in the writing of the report, and in the decision to submit the article for publication. There was no additional external funding received for this study.
References
- 1.Minicucci MF, Azevedo PS, Matsubara BB, Matsubara LS, Paiva SA, et al. (2010) [Association between sphericity, ventricular function and size of the infarction in rats]. Arq Bras Cardiol 94: 645–650. doi: 10.1590/s0066-782x2010005000023 [DOI] [PubMed] [Google Scholar]
- 2.Zornoff LA, Paiva SA, Minicucci MF, Spadaro J (2009) Experimental myocardium infarction in rats: analysis of the model. Arq Bras Cardiol 93: 434–440, 426–432. doi: 10.1590/s0066-782x2009001000018 [DOI] [PubMed] [Google Scholar]
- 3.Opie LH, Commerford PJ, Gersh BJ, Pfeffer MA (2006) Controversies in ventricular remodelling. Lancet 367: 356–367. doi: 10.1016/S0140-6736(06)68074-4 [DOI] [PubMed] [Google Scholar]
- 4.Stanley WC, Recchia FA, Lopaschuk GD (2005) Myocardial substrate metabolism in the normal and failing heart. Physiol Rev 85: 1093–1129. doi: 10.1152/physrev.00006.2004 [DOI] [PubMed] [Google Scholar]
- 5.Zornoff LA, Paiva SA, Duarte DR, Spadaro J (2009) Ventricular remodeling after myocardial infarction: concepts and clinical implications. Arq Bras Cardiol 92: 150–164. doi: 10.1590/s0066-782x2009000200013 [DOI] [PubMed] [Google Scholar]
- 6.Pfeffer JM, Pfeffer MA, Braunwald E (1985) Influence of chronic captopril therapy on the infarcted left ventricle of the rat. Circ Res 57: 84–95. doi: 10.1161/01.res.57.1.84 [DOI] [PubMed] [Google Scholar]
- 7.Pereira BLB, Reis PP, Severino FE, Felix TF, Braz MG, et al. (2017) Tomato (Lycopersicon esculentum) or lycopene supplementation attenuates ventricular remodeling after myocardial infarction through different mechanistic pathways. J Nutr Biochem 46: 117–124. doi: 10.1016/j.jnutbio.2017.05.010 [DOI] [PubMed] [Google Scholar]
- 8.Murino Rafacho BP, Portugal Dos Santos P, Goncalves AF, Fernandes AAH, Okoshi K, et al. (2017) Rosemary supplementation (Rosmarinus oficinallis L.) attenuates cardiac remodeling after myocardial infarction in rats. PLoS One 12: e0177521. doi: 10.1371/journal.pone.0177521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oliveira BC, Santos PP, Figueiredo AM, Rafacho BPM, Ishikawa L, et al. (2021) Influence of Consumption of Orange Juice (Citrus Sinensis) on Cardiac Remodeling of Rats Submitted to Myocardial Infarction. Arq Bras Cardiol 116: 1127–1136. doi: 10.36660/abc.20190397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodrigues RB, Lichtenthaler R, Zimmermann BF, Papagiannopoulos M, Fabricius H, et al. (2006) Total oxidant scavenging capacity of Euterpe oleracea Mart. (acai) seeds and identification of their polyphenolic compounds. J Agric Food Chem 54: 4162–4167. doi: 10.1021/jf058169p [DOI] [PubMed] [Google Scholar]
- 11.de Moura RS, Resende AC (2016) Cardiovascular and Metabolic Effects of Acai, an Amazon Plant. J Cardiovasc Pharmacol 68: 19–26. doi: 10.1097/FJC.0000000000000347 [DOI] [PubMed] [Google Scholar]
- 12.de Oliveira PR, da Costa CA, de Bem GF, Cordeiro VS, Santos IB, et al. (2015) Euterpe oleracea Mart.-Derived Polyphenols Protect Mice from Diet-Induced Obesity and Fatty Liver by Regulating Hepatic Lipogenesis and Cholesterol Excretion. PLoS One 10: e0143721. doi: 10.1371/journal.pone.0143721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schauss AG, Wu X, Prior RL, Ou B, Huang D, et al. (2006) Antioxidant capacity and other bioactivities of the freeze-dried Amazonian palm berry, Euterpe oleraceae mart. (acai). J Agric Food Chem 54: 8604–8610. doi: 10.1021/jf0609779 [DOI] [PubMed] [Google Scholar]
- 14.Silva DF, Vidal FC, Santos D, Costa MC, Morgado-Diaz JA, et al. (2014) Cytotoxic effects of Euterpe oleracea Mart. in malignant cell lines. BMC Complement Altern Med 14: 175. doi: 10.1186/1472-6882-14-175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou J, Zhang J, Wang C, Qu S, Zhu Y, et al. (2018) Acai (Euterpe oleracea Mart.) attenuates alcohol-induced liver injury in rats by alleviating oxidative stress and inflammatory response. Exp Ther Med 15: 166–172. doi: 10.3892/etm.2017.5427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alessandra-Perini J, Perini JA, Rodrigues-Baptista KC, de Moura RS, Junior AP, et al. (2018) Euterpe oleracea extract inhibits tumorigenesis effect of the chemical carcinogen DMBA in breast experimental cancer. BMC Complement Altern Med 18: 116. doi: 10.1186/s12906-018-2183-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.da Silva PP, Casemiro RC, Zillo RR, de Camargo AC, Prospero ET, et al. (2014) Sensory descriptive quantitative analysis of unpasteurized and pasteurized jucara pulp (Euterpe edulis) during long-term storage. Food Sci Nutr 2: 321–331. doi: 10.1002/fsn3.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fragoso MF, Romualdo GR, Vanderveer LA, Franco-Barraza J, Cukierman E, et al. (2018) Lyophilized acai pulp (Euterpe oleracea Mart) attenuates colitis-associated colon carcinogenesis while its main anthocyanin has the potential to affect the motility of colon cancer cells. Food Chem Toxicol 121: 237–245. doi: 10.1016/j.fct.2018.08.078 [DOI] [PubMed] [Google Scholar]
- 19.Pala D, Barbosa PO, Silva CT, de Souza MO, Freitas FR, et al. (2018) Acai (Euterpe oleracea Mart.) dietary intake affects plasma lipids, apolipoproteins, cholesteryl ester transfer to high-density lipoprotein and redox metabolism: A prospective study in women. Clin Nutr 37: 618–623. doi: 10.1016/j.clnu.2017.02.001 [DOI] [PubMed] [Google Scholar]
- 20.Kim H, Simbo SY, Fang C, McAlister L, Roque A, et al. (2018) Acai (Euterpe oleracea Mart.) beverage consumption improves biomarkers for inflammation but not glucose- or lipid-metabolism in individuals with metabolic syndrome in a randomized, double-blinded, placebo-controlled clinical trial. Food Funct 9: 3097–3103. doi: 10.1039/c8fo00595h [DOI] [PubMed] [Google Scholar]
- 21.de Bem GF, da Costa CA, da Silva Cristino Cordeiro V, Santos IB, de Carvalho L, et al. (2018) Euterpe oleracea Mart. (acai) seed extract associated with exercise training reduces hepatic steatosis in type 2 diabetic male rats. J Nutr Biochem 52: 70–81. doi: 10.1016/j.jnutbio.2017.09.021 [DOI] [PubMed] [Google Scholar]
- 22.Martinez RM, Guimaraes DAB, Berniz CR, Abreu JP, Rocha A, et al. (2018) Acai (Euterpe oleracea Mart.) Seed Extract Induces Cell Cycle Arrest and Apoptosis in Human Lung Carcinoma Cells. Foods 7. doi: 10.3390/foods7110178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Poulose SM, Bielinski DF, Carey A, Schauss AG, Shukitt-Hale B (2017) Modulation of oxidative stress, inflammation, autophagy and expression of Nrf2 in hippocampus and frontal cortex of rats fed with acai-enriched diets. Nutr Neurosci 20: 305–315. doi: 10.1080/1028415X.2015.1125654 [DOI] [PubMed] [Google Scholar]
- 24.Carey AN, Miller MG, Fisher DR, Bielinski DF, Gilman CK, et al. (2017) Dietary supplementation with the polyphenol-rich acai pulps (Euterpe oleracea Mart. and Euterpe precatoria Mart.) improves cognition in aged rats and attenuates inflammatory signaling in BV-2 microglial cells. Nutr Neurosci 20: 238–245. doi: 10.1080/1028415X.2015.1115213 [DOI] [PubMed] [Google Scholar]
- 25.Sadowska-Krepa E, Klapcinska B, Podgorski T, Szade B, Tyl K, et al. (2015) Effects of supplementation with acai (Euterpe oleracea Mart.) berry-based juice blend on the blood antioxidant defence capacity and lipid profile in junior hurdlers. A pilot study. Biol Sport 32: 161–168. doi: 10.5604/20831862.1144419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barbosa PO, Pala D, Silva CT, de Souza MO, do Amaral JF, et al. (2016) Acai (Euterpe oleracea Mart.) pulp dietary intake improves cellular antioxidant enzymes and biomarkers of serum in healthy women. Nutrition 32: 674–680. doi: 10.1016/j.nut.2015.12.030 [DOI] [PubMed] [Google Scholar]
- 27.Mathias L, Alegre PHC, Dos Santos IOF, Bachiega T, Figueiredo AM, et al. (2019) Euterpe oleracea Mart. (Acai) Supplementation Attenuates Acute Doxorubicin-Induced Cardiotoxicity in Rats. Cell Physiol Biochem 53: 388–399. doi: 10.33594/000000145 [DOI] [PubMed] [Google Scholar]
- 28.Zapata-Sudo G, da Silva JS, Pereira SL, Souza PJ, de Moura RS, et al. (2014) Oral treatment with Euterpe oleracea Mart. (acai) extract improves cardiac dysfunction and exercise intolerance in rats subjected to myocardial infarction. BMC Complement Altern Med 14: 227. doi: 10.1186/1472-6882-14-227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alegre P, Mathias L, Lourenco MA, Santos PPD, Goncalves A, et al. (2019) Euterpe Oleracea Mart. (Acai) Reduces Oxidative Stress and Improves Energetic Metabolism in Myocardial Ischemia-Reperfusion Injury in Rats. Arq Bras Cardiol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pfeffer JM, Finn PV, Zornoff LA, Pfeffer MA (2000) Endothelin-A receptor antagonism during acute myocardial infarction in rats. Cardiovasc Drugs Ther 14: 579–587. doi: 10.1023/a:1007890126061 [DOI] [PubMed] [Google Scholar]
- 31.Kim DO, Chun OK, Kim YJ, Moon HY, Lee CY (2003) Quantification of polyphenolics and their antioxidant capacity in fresh plums. J Agric Food Chem 51: 6509–6515. doi: 10.1021/jf0343074 [DOI] [PubMed] [Google Scholar]
- 32.Brand-Williams W CM, Berset C (1995) Use of a free radicalmethod to evaluate antioxidant activity. LWT-Food Sci Technol 28: 25–30. [Google Scholar]
- 33.Teixeira LN SP, Oliveira FA (2008) Comparison of methods for quantification of anthocyanins. Ceres 55: 297–304. [Google Scholar]
- 34.de Souza MO, Souza ESL, de Brito Magalhaes CL, de Figueiredo BB, Costa DC, et al. (2012) The hypocholesterolemic activity of acai (Euterpe oleracea Mart.) is mediated by the enhanced expression of the ATP-binding cassette, subfamily G transporters 5 and 8 and low-density lipoprotein receptor genes in the rat. Nutr Res 32: 976–984. doi: 10.1016/j.nutres.2012.10.001 [DOI] [PubMed] [Google Scholar]
- 35.Fragoso MF, Romualdo GR, Ribeiro DA, Barbisan LF (2013) Acai (Euterpe oleracea Mart.) feeding attenuates dimethylhydrazine-induced rat colon carcinogenesis. Food Chem Toxicol 58: 68–76. doi: 10.1016/j.fct.2013.04.011 [DOI] [PubMed] [Google Scholar]
- 36.Sahn DJ, DeMaria A, Kisslo J, Weyman A (1978) Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation 58: 1072–1083. doi: 10.1161/01.cir.58.6.1072 [DOI] [PubMed] [Google Scholar]
- 37.Zornoff LA, Matsubara BB, Matsubara LS, Azevedo PS, Minicucci MF, et al. (2006) Beta-carotene supplementation results in adverse ventricular remodeling after acute myocardial infarction. Nutrition 22: 146–151. doi: 10.1016/j.nut.2005.05.008 [DOI] [PubMed] [Google Scholar]
- 38.Slama M, Ahn J, Peltier M, Maizel J, Chemla D, et al. (2005) Validation of echocardiographic and Doppler indexes of left ventricular relaxation in adult hypertensive and normotensive rats. Am J Physiol Heart Circ Physiol 289: H1131–1136. doi: 10.1152/ajpheart.00345.2004 [DOI] [PubMed] [Google Scholar]
- 39.Tei C, Nishimura RA, Seward JB, Tajik AJ (1997) Noninvasive Doppler-derived myocardial performance index: correlation with simultaneous measurements of cardiac catheterization measurements. J Am Soc Echocardiogr 10: 169–178. doi: 10.1016/s0894-7317(97)70090-7 [DOI] [PubMed] [Google Scholar]
- 40.Minicucci MF, Azevedo PS, Polegato BF, Paiva SA, Zornoff LA (2011) Heart failure after myocardial infarction: clinical implications and treatment. Clin Cardiol 34: 410–414. doi: 10.1002/clc.20922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ewing JF, Janero DR (1995) Microplate superoxide dismutase assay employing a nonenzymatic superoxide generator. Anal Biochem 232: 243–248. doi: 10.1006/abio.1995.0014 [DOI] [PubMed] [Google Scholar]
- 42.Burneiko RC, Diniz YS, Galhardi CM, Rodrigues HG, Ebaid GM, et al. (2006) Interaction of hypercaloric diet and physical exercise on lipid profile, oxidative stress and antioxidant defenses. Food Chem Toxicol 44: 1167–1172. doi: 10.1016/j.fct.2006.01.004 [DOI] [PubMed] [Google Scholar]
- 43.Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72: 248–254. doi: 10.1006/abio.1976.9999 [DOI] [PubMed] [Google Scholar]
- 44.Nielsen F, Mikkelsen BB, Nielsen JB, Andersen HR, Grandjean P (1997) Plasma malondialdehyde as biomarker for oxidative stress: reference interval and effects of life-style factors. Clin Chem 43: 1209–1214. [PubMed] [Google Scholar]
- 45.Azevedo PS, Minicucci MF, Santos PP, Paiva SA, Zornoff LA (2013) Energy metabolism in cardiac remodeling and heart failure. Cardiol Rev 21: 135–140. doi: 10.1097/CRD.0b013e318274956d [DOI] [PubMed] [Google Scholar]
- 46.Lopaschuk GD, Ussher JR, Folmes CD, Jaswal JS, Stanley WC (2010) Myocardial fatty acid metabolism in health and disease. Physiol Rev 90: 207–258. doi: 10.1152/physrev.00015.2009 [DOI] [PubMed] [Google Scholar]
- 47.Sun Y (2009) Myocardial repair/remodelling following infarction: roles of local factors. Cardiovasc Res 81: 482–490. doi: 10.1093/cvr/cvn333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Daiber A, Hahad O, Andreadou I, Steven S, Daub S, et al. (2021) Redox-related biomarkers in human cardiovascular disease—classical footprints and beyond. Redox Biol 42: 101875. doi: 10.1016/j.redox.2021.101875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li G, Ye Y, Kang J, Yao X, Zhang Y, et al. (2012) l-Theanine prevents alcoholic liver injury through enhancing the antioxidant capability of hepatocytes. Food Chem Toxicol 50: 363–372. doi: 10.1016/j.fct.2011.10.036 [DOI] [PubMed] [Google Scholar]
- 50.Liu T, Chen L, Kim E, Tran D, Phinney BS, et al. (2014) Mitochondrial proteome remodeling in ischemic heart failure. Life Sci 101: 27–36. doi: 10.1016/j.lfs.2014.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barbosa PO, Souza MO, Silva MPS, Santos GT, Silva ME, et al. (2021) Acai (Euterpe oleracea Martius) supplementation improves oxidative stress biomarkers in liver tissue of dams fed a high-fat diet and increases antioxidant enzymes’ gene expression in offspring. Biomed Pharmacother 139: 111627. doi: 10.1016/j.biopha.2021.111627 [DOI] [PubMed] [Google Scholar]
- 52.de Freitas Carvalho MM, Lage NN, de Souza Paulino AH, Pereira RR, de Almeida LT, et al. (2019) Effects of acai on oxidative stress, ER stress, and inflammation-related parameters in mice with high fat diet-fed induced NAFLD. Sci Rep 9: 8107. doi: 10.1038/s41598-019-44563-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.de Souza MO, Silva M, Silva ME, Oliveira Rde P, Pedrosa ML (2010) Diet supplementation with acai (Euterpe oleracea Mart.) pulp improves biomarkers of oxidative stress and the serum lipid profile in rats. Nutrition 26: 804–810. doi: 10.1016/j.nut.2009.09.007 [DOI] [PubMed] [Google Scholar]
- 54.Guerra JF, Magalhaes CL, Costa DC, Silva ME, Pedrosa ML (2011) Dietary acai modulates ROS production by neutrophils and gene expression of liver antioxidant enzymes in rats. J Clin Biochem Nutr 49: 188–194. doi: 10.3164/jcbn.11-02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Xie C, Kang J, Burris R, Ferguson ME, Schauss AG, et al. (2011) Acai juice attenuates atherosclerosis in ApoE deficient mice through antioxidant and anti-inflammatory activities. Atherosclerosis 216: 327–333. doi: 10.1016/j.atherosclerosis.2011.02.035 [DOI] [PubMed] [Google Scholar]
- 56.Nian M, Lee P, Khaper N, Liu P (2004) Inflammatory cytokines and postmyocardial infarction remodeling. Circ Res 94: 1543–1553. doi: 10.1161/01.RES.0000130526.20854.fa [DOI] [PubMed] [Google Scholar]
- 57.Christia P, Bujak M, Gonzalez-Quesada C, Chen W, Dobaczewski M, et al. (2013) Systematic characterization of myocardial inflammation, repair, and remodeling in a mouse model of reperfused myocardial infarction. J Histochem Cytochem 61: 555–570. doi: 10.1369/0022155413493912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Turillazzi E, Di Paolo M, Neri M, Riezzo I, Fineschi V (2014) A theoretical timeline for myocardial infarction: immunohistochemical evaluation and western blot quantification for Interleukin-15 and Monocyte chemotactic protein-1 as very early markers. J Transl Med 12: 188. doi: 10.1186/1479-5876-12-188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Frangogiannis NG (2015) Inflammation in cardiac injury, repair and regeneration. Curr Opin Cardiol 30: 240–245. doi: 10.1097/HCO.0000000000000158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Prabhu SD, Frangogiannis NG (2016) The Biological Basis for Cardiac Repair After Myocardial Infarction: From Inflammation to Fibrosis. Circ Res 119: 91–112. doi: 10.1161/CIRCRESAHA.116.303577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Spinale FG (2007) Myocardial matrix remodeling and the matrix metalloproteinases: influence on cardiac form and function. Physiol Rev 87: 1285–1342. doi: 10.1152/physrev.00012.2007 [DOI] [PubMed] [Google Scholar]
- 62.Reagan-Shaw S, Nihal M, Ahmad N (2008) Dose translation from animal to human studies revisited. FASEB J 22: 659–661. doi: 10.1096/fj.07-9574LSF [DOI] [PubMed] [Google Scholar]