Abstract
Objectives:
The use of minimally invasive techniques for urgent colectomies remains understudied. This study compares short-term outcomes following urgent minimally invasive colectomies to those following open colectomies.
Methods & Procedures:
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) colectomy database was queried between January 1, 2013 and December 31, 2018. Patients who underwent elective and emergency colectomies, based on the respective NSQIP variables, were excluded. The remaining patients were divided into two groups, minimally invasive surgery (MIS) and open. MIS colectomies with unplanned conversion to open were included in the MIS group. Baseline characteristics and 30-day outcomes were compared using univariable and multivariable regression analyses.
Results:
A total of 29,345 patients were included in the study; 12,721 (43.3%) underwent MIS colectomy, while 16,624 (56.7%) underwent open colectomy. Patients undergoing MIS colectomy were younger (60.6 vs 63.8 years) and had a lower prevalence of either American Society of Anesthesiology (ASA) IV (9.9 vs 15.5%) or ASA V (0.08% vs 2%). After multivariable analysis, MIS colectomy was associated with lower odds of mortality (odds ratio = 0.75, 95% confidence interval: 0.61, 0.91 95% confidence interval), and most short-term complications recorded in the ACS NSQIP. While MIS colectomies took longer to perform (161 vs 140 min), the length of stay was shorter (12.2 vs 14.1 days).
Conclusions:
MIS colectomy affords better short-term complication rates and a reduced length of stay compared to open colectomy for patients requiring urgent surgery. If feasible, minimally invasive colectomy should be offered to patients necessitating urgent colon resection.
Keywords: Colectomy, Colon Resection, Elective, Laparoscopic, Minimally Invasive Surgery, Open, Urgent
INTRODUCTION
Over the last two decades, minimally invasive surgery (MIS) has become the preferred surgical approach for elective colorectal resections.1,2 The benefits of MIS are clear: multiple studies have demonstrated reduced pain and postoperative ileus, oncologic equivalence, shorter hospital length of stay (LOS), and improved short term quality of life associated with MIS.2–7 This has led to a consistent rise in the use of MIS for colorectal resections, with half of all elective colectomies now performed laparoscopically.8
Several studies have evaluated the use of MIS in the nonelective setting. Single institution studies have shown that the use of MIS for nonelective resections is feasible and noninferior to open colectomy.9–15 Reviews of large national databases reveal that the use of MIS in the nonelective setting is associated with a shorter LOS, reduced postoperative morbidity and mortality, and reduced costs.16,17 These studies include both urgent and emergency colorectal resections and a minimally invasive approach was reported in 5% – 30% of total cases.16,17
Patients with a myriad of colorectal conditions often undergo nonoperative treatment prior to ultimately requiring surgery. This can be for a variety of reasons such as further evaluation, medical optimization, or surgical consultation not occurring at the time of admission. Many of these patients ultimately require a colectomy within the hospitalization, albeit in a nonemergency, or not within the first few hours of admission. These patients who undergo urgent (nonelective, nonemergency) operations are distinct from those who require an emergency surgery, as well as from elective ones, and may have a unique rate of postoperative morbidity and mortality.18,19 While the acuity of the illness requiring emergency colon resections, such as hemodynamic instability or overwhelming infection, may preclude the use of MIS, patients undergoing urgent colorectal resections may be better suited for MIS.
Our aim for this study is to focus on patients undergoing urgent (nonemergency, nonelective) inpatient colectomies, and compare 30-day outcomes between MIS and open colorectal resections for these patients. We hypothesize that patients that have their surgery performed in an MIS fashion have improved outcomes compared to those who have it performed in the traditional open fashion.
METHODOLOGY
This retrospective review of a national database was approved by the Institutional Review Board. The American College of Surgeons (ACS) National Surgical Quality Improvement Project (NSQIP) database was used to construct the patient cohort. General and colectomy specific databases were combined to create an aggregate database that included all colectomies performed between January 1, 2013 and December 31, 2018. All patients who underwent emergency or elective colectomy, based on the ‘Emergency Surgery’ or ‘Elective Surgery’ variables, were excluded. Within the database, elective surgery is defined as a procedure performed on a patient who is brought to a medical facility for a scheduled operation. This excludes patients who are inpatient at an acute care hospital, are transferred from an emergency department or clinic, or undergo urgent or emergency surgery. Emergency surgery is any surgery that is designated as such by either the surgeons or the anesthesiologists as part of the American Society of Anesthesiologists (ASA) physical status classification immediately prior to surgery. The final analysis included all adult patients who underwent a default urgent, neither emergency, nor elective colectomy.
The patients were then divided into two groups based on the surgical approach: Minimally Invasive Surgery (MIS) and Open. The MIS group included the following approaches: laparoscopic, laparoscopic with open assist, and laparoscopic with unplanned conversion to open. The open group included all planned open colectomies.
Baseline demographics and comorbidities were compared between the groups. The variables used for baseline comparison are included in Table 1 The primary outcome of interest was 30-day mortality. Secondary outcomes included the incidence of 30-day complications, as well as total hospital LOS and postoperative LOS. All outcomes of interest are outlined in Table 2 and Figure 2.
Table 1.
Patients Baseline Characteristics
| Item | MIS | Open | P Value |
|---|---|---|---|
| (n = 12,721) | (n = 16,624) | ||
| Age (years), mean (SD) | 60.6 (0.2) | 63.8 (0.1) | < 0.0001 |
| Gender, % (n) | 0.005 | ||
| Female | 51.9 (6597) | 53.5 (8894) | |
| Male | 48.1 (6124) | 46.5 (7730) | |
| Race, % (n) | < 0.0001 | ||
| Black | 12 (1532) | 12.8 (2121) | |
| White | 73.2 (9310) | 75.4 (12536) | |
| Other | 3.4 (431) | 2.8 (465) | |
| Unknown | 11.4 (1448) | 9 (1502) | |
| Hispanic, % (n) | 6.2 (789) | 5.6 (931) | 0.024 |
| BMI (kg/m2), % (n) | 0.0001 | ||
| < 18.5 | 4.8 (601) | 5.7 (912) | |
| 18.5 – 24.9 | 33.6 (4175) | 35.4 (5704) | |
| 25 – 29.9 | 30.3 (3766) | 29.3 (4713) | |
| 30 – 34.9 | 17.5 (2177) | 16.4 (2639) | |
| 35 – 39.9 | 7.8 (973) | 7.7 (1239) | |
| ≥ 40 | 5.9 (730) | 5.6 (897) | |
| ASA Score, % (n) | < 0.0001 | ||
| I | 1.8 (225) | 0.9 (142) | |
| II | 32.4 (4121) | 22 (3662) | |
| III | 55.8 (7100) | 61.1 (10161) | |
| IV | 9.9 (1255) | 15.5 (2577) | |
| V | 0.1 (10) | 0.3 (57) | |
| Hypertension, % (n) | 47.4 (6687) | 50.4 (8253) | < 0.0001 |
| Diabetes Mellitus, % (n) | 0.0527 | ||
| Insulin Dependent | 6.6 (840) | 7.3 (1213) | |
| Non-Insulin Dependent | 9.5 (1202) | 9.1 (1517) | |
| Congestive Heart Failure, % (n) | 2.7 (349) | 2.8 (467) | 0.735 |
| Chronic Obstructive Pulmonary Disease, % (n) | 5.8 (738) | 7.9 (1315) | < 0.0001 |
| Renal Failure, % (n) | 0.4 (48) | 1 (171) | < 0.0001 |
| Dialysis Dependent, % (n) | 1.5 (193) | 2.3 (378) | < 0.0001 |
| Recent Weight Loss, % (n) | 10.6 (1349) | 11.2 (1867) | 0.089 |
| Chronic Steroid Use, % (n) | 17.6 (2238) | 12.2 (2034) | < 0.0001 |
| Steroid Use for IBD, % (n) | 15.2 (1922) | 7.9 (1309) | < 0.0001 |
| Smoker, % (n) | 16.9 (2152) | 20.3 (3373) | < 0.0001 |
| Ascites, % (n) | 0.8 (95) | 2.3 (378) | < 0.0001 |
| Disseminated Cancer, % (n) | 7.0 (896) | 11.9 (1991) | < 0.0001 |
| Dyspnea, % (n) | < 0.0001 | ||
| At Rest | 0.7 (85) | 1.1 (189) | |
| Moderate Exertion | 7.8 (986) | 7.2 (1201) | |
| Ventilator Dependent, % (n) | 0.3 (22) | 1.5 (255) | < 0.0001 |
| Sepsis Present at the Time of Surgery, % (n) | 3.5 (446) | 6.6 (1094) | < 0.0001 |
| Wound Infection Present, % (n) | 2.9 (377) | 5.7 (946) | < 0.0001 |
| Recent Transfusion, % (n) | 9.7 (1229) | 9.11 (1514) | 0.106 |
| Functional Status, % (n) | < 0.0001 | ||
| Independent | 93.8 (11935) | 91.4 (15191) | |
| Partially dependent | 4.9 (617) | 6.4 (1064) | |
| Totally Dependent | 1.1 (135) | 1.7 (285) | |
| Recent Chemotherapy Within 30 Days, % (n) | 2.3 (295) | 4.8 (793) | < 0.0001 |
| Wound Classification, % (n) | < 0.0001 | ||
| Clean | 0.8 (96) | 0.6 (105) | |
| Clean/Contaminated | 64.5 (8205) | 52.3 (8686) | |
| Contaminated | 17.1 (2176) | 18.4 (3059) | |
| Dirty/Infected | 17.6 (2244) | 28.7 (4774) | |
| Wound Closure, % (n) | < 0.0001 | ||
| All Layers of Incision | 97.6 (11217) | 90.12 (13220) | |
| Only Deep Layers Closed | 2.1 (240) | 7.9 (1154) | |
| No layers Closed | 0.3 (31) | 2 (296) | |
| Mechanical Bowel Prep, % (n) | 50.7 (5938) | 34.9 (5368) | < 0.0001 |
| Antibiotic Bowel Prep, % (n) | 32.9 (3888) | 21.2 (3305) | < 0.0001 |
| Indication for Surgery, % (n) | < 0.0001 | ||
| Acute Diverticulitis | 10 (1272) | 13.3 (2215) | |
| Chronic Diverticular Stricture | 7.6 (965) | 6.4 (1059) | |
| Bleeding | 1.8 (228) | 1.5 (252) | |
| Colon Cancer | 31.2 (3971) | 21.5 (3581) | |
| Colon Cancer with Obstruction | 10.2 (1296) | 13.1 (2178) | |
| Ulcerative Colitis | 7.4 (946) | 2 (327) | |
| Crohn’s Disease | 9.4 (1193) | 6.8 (1125) | |
| Enterocolitis | 0.4 (47) | 0.8 (129) | |
| Volvulus | 3.1 (400) | 7.2 (1203) | |
| Non-Malignant Polyp | 2.8 (354) | 0.9 (151) | |
| Other ICD Code | 16.1 (2042) | 26.3 (4378) | |
| Unknown | 0.1 (7) | 0.2 (26) |
ASA, American Society of Anesthesiologists Score; BMI, body mass index; IBD, inflammatory bowel disease; ICD, International Classification of Diseases; MIS, minimally invasive surgery.
Table 2.
Postoperative Complications Following Minimally Invasive Surgery in Urgent Colorectal Resections Compared to Open
| Outcome | Mis (n = 12,721) | Open (n = 16,624) | Odds of Complication*(n = 29,345) | Odds of Complication†(n = 23,826) |
|---|---|---|---|---|
| % (n) | % (n) | OR (95% CI) | aOR (95% CI) | |
| Death | 1.5 (195) | 3.8 (624) | 0.40 (0.34, 0.47) | 0.75 (0.61, 0.91) |
| Prolonged stay (> 30 days) | 1.2 (148) | 2.6 (432) | 0.44 (0.37, 0.53) | 0.62 (0.49, 0.78) |
| Bleeding Complications | 14.0 (1179) | 22.0 (3662) | 0.57 (0.54, 0.61) | 0.68 (0.63, 0.73) |
| Septic Shock | 2.4 (306) | 6.1 (1010) | 0.38 (0.34, 0.43) | 0.65 (0.55, 0.75) |
| Systemic Sepsis | 6.6 (841) | 10.8 (1795) | 0.59 (0.54, 0.64) | 0.86 (0.78, 0.95) |
| Gastrointestinal Ileus | 17.5 (2228) | 30.4 (5035) | 0.49 (0.46, 0.52) | 0.60 (0.56, 0.64) |
| Return to Operating Room | 5.6 (715) | 7.7 (1278) | 0.72 (0.65, 0.79) | 0.80 (0.72, 0.90) |
| Wound Dehiscence | 0.9 (115) | 2.1 (348) | 0.43 (0.35, 0.53) | 0.59 (0.46, 0.76) |
| Anastomotic Leak | 3.3 (422) | 4.6 (758) | 0.72 (0.63, 0.81) | 0.84 (0.72, 0.97) |
| Renal Failure | 0.6 (77) | 1.2 (193) | 0.52 (0.40, 0.68) | 0.74 (0.54, 1.01) |
| Myocardial Infarction | 0.9 (108) | 1.2 (206) | 0.68 (0.54, 0.86) | 0.81 (0.60, 1.08) |
| Reintubation | 2.1 (272) | 4.1 (678) | 0.52 (0.45, 0.59) | 0.70 (0.59, 0.83) |
| Deep Venous Thrombosis | 2.0 (260) | 3.0 (505) | 0.67 (0.57, 0.78) | 0.77 (0.65, 0.92) |
| Organ Space SSI | 6.1 (774) | 9.6 (1592) | 0.62 (0.56, 0.67) | 0.75 (0.68, 0.84) |
| Deep SSI | 0.9 (117) | 1.5 (255) | 0.60 (0.48, 0.74) | 0.72 (0.55, 0.93) |
| Superficial SSI | 4.7 (601) | 4.9 (1146) | 0.67 (0.61, 0.74) | 0.72 (0.63, 0.81) |
| Cerebrovascular Accident | 0.3 (40) | 0.5 (86) | 0.61 (0.42, 0.88) | 0.70 (0.46, 1.10) |
| Pulmonary Embolism | 0.9 (116) | 1.4 (225) | 0.67 (0.54, 0.84) | 0.61 (0.47, 0.79) |
| Cardiac Arrest | 0.7 (84) | 1.2 (203) | 0.54 (0.42, 0.69) | 0.74 (0.55, 0.99) |
| Urinary Tract Infection | 2.4 (307) | 3.4 (561) | 0.71 (0.62, 0.82) | 0.80 (0.67, 0.94) |
| Readmission | 15.8 (1579) | 17.1 (2325) | 0.91 (0.85, 0.98) | 0.87 (0.79, 0.95) |
| Colostomy | 14.5 (1663) | 35.6 (5577) | 0.31 (0.29, 0.33) | 0.43 (0.39, 0.46) |
OR, adjusted odds ratio; OR, odds ratio; SSI, superficial site infection; MIS, minimally invasive surgery.
Bolded estimates were statistically significant different from 1 (P < .05).
Unadjusted odds of complication.
Multivariable analysis adjusting for propensity score and including year of operation as random effect.
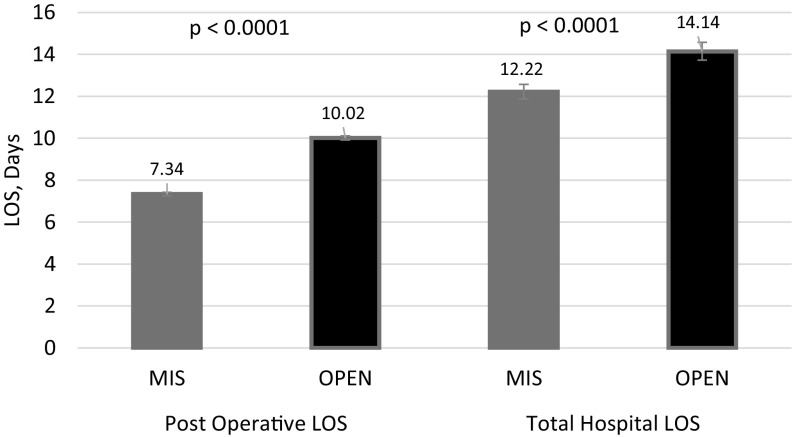
Figure 2.
Total hospital length of stay and postoperative length of stay were significantly decreased for minimally invasive surgery group (P < .0001).
Data were analyzed using SAS/STAT software (version 90.4) Copyright© 2014 SAS Institute Inc., Cary, North Carolina, USA. Baseline characteristics were compared using χ2 test for categorical variables, and t test for continuous variables. Median operative time was compared using Wilcoxon Rank-Sum test. Univariable comparison of postoperative outcomes was performed using χ2 test and logistic regression, followed by a multivariable logistic regression analysis. The multivariable logistic regression adjusted for propensity scores and the year of surgery to account for changes over time. A P-value of < 0.05 was chosen to denote statistical significance.
RESULTS
A total of 193,507 colectomy cases were identified over the 6-year study period. After the exclusion of elective (134,165) cases, emergency (29,331) cases, and ‘other surgical approaches’ (995), the final cohort included 29,345 colectomy cases. Of these, 12,721 (43.3%) were performed using MIS and 16,624 (56.7%) were performed using a planned open approach (Figure 1). Among patients in the MIS group, 2,722 (21.4%) required unplanned conversion to open.
Figure 1.
Group allocation.
At baseline, patients undergoing open surgery were older (63.8 years vs 60.6 years, P < .0001). Women were more likely to have open surgery (53.5% vs 51.9%, P = .0052). Patients who were overweight and obese were more likely to undergo MIS colectomy (P < .0001, Table 1). More American Society of Anesthesiology (ASA) I or II patients underwent MIS compared to those with ASA III or higher (P < .0001). Patients who underwent open surgery were more likely to have comorbid conditions (P < .0001, Table 1). There was no significant difference between the prevalence of diabetes mellitus, congestive heart failure, recent weight loss, or recent blood transfusion between the groups (Table 1). More patients in the MIS group completed mechanical (50.7% vs 34.9%) and antibiotic (32.9% vs 21.2%) bowel preparation (P < .0001). More MIS cases were classified as clean or clean/contaminated, while more open cases were classified as contaminated or dirty (P < .0001, Table 1). Partial wound closure was applied more often in open cases compared to MIS (P < .0001).
The most common indications for surgery were colon cancer, obstructing colon cancer, and acute diverticulitis. Patients who underwent MIS colectomy were most likely to have a diagnosis of colon cancer, obstructing colon cancer, chronic diverticular stricture, inflammatory bowel disease, bleeding or nonmalignant polyps. Conversely, patients who underwent open colectomy were more likely to have acute diverticulitis or volvulus (P < .0001, Table 1). Compared to open colectomy, the median time to complete a MIS colectomy was 21 minutes longer (161 vs 140 min, P < .0001).
On univariable analysis, 30-day mortality following MIS colectomy was significantly lower than that following open surgery (1.5% vs 3.8% P < .05). Similarly, the incidence of all recorded adverse outcomes was lower for patients who underwent MIS colectomy (Table 2).
After adjusting for baseline variances, the difference in the likelihood of mortality favored for the MIS group (odds ratio [OR] 0.75, 95% confidence interval [CI] 0.61, 0.91). The odds of prolonged stay (> 30 days), bleeding complications, septic shock, systemic sepsis, ileus, reoperation, wound dehiscence, anastomotic leak, reintubation, venous thrombosis (DVT), surgical site infections (SSI) (superficial, deep, and organ space), pulmonary embolism (PE), cardiac arrest, urinary tract infection (UTI), and readmission were lower for the patients undergoing MIS colectomy (Table 2). The odds of renal failure, myocardial infarction, and cerebrovascular accident were similar between groups.
Finally, patients who underwent MIS colectomy had a shorter total hospital LOS (12.2 vs 14.1 days, P < .0001), as well as postoperative LOS (7.2 vs 10 days, P < .0001) (Figure 2).
DISCUSSION/CONCLUSIONS
The benefits of MIS in elective colorectal surgery are clear. These benefits likely extend to nonelective surgeries as well. This study highlights that MIS techniques can be beneficial in a subset of nonelective surgeries. For patients undergoing urgent inpatient colectomy, the use of MIS was associated with a decrease in mortality, prolonged hospitalization, gastrointestinal ileus, dehiscence, SSI, DVT, and PE, as well as readmission rate.
The use of MIS in nonelective colorectal resections has been studied previously. Single institution studies have demonstrated that the use of MIS is not only noninferior to open, but in some cases, has superior outcomes.9,10,12 A more recent retrospective review by Stulberg et al. showed a similar mortality rate between open and MIS cases, and decreased blood loss and LOS for the MIS groups.11 The benefit of MIS in urgent and emergency colorectal resections was confirmed by larger studies. Vallance et al. studied patients who underwent urgent and emergency colectomies in the National Bowel Cancer Audit and showed that MIS was associated with a shorter LOS and a lower 90-day mortality.16 Keller et al. reviewed the Premier national inpatient database and found that although less than 5% of the nonelective colectomies were performed using MIS, when performed, MIS was associated with improved outcomes and decreased hospital costs.17
We have focused on the patients undergoing urgent inpatient colectomy, who require a surgical resection within the index hospital admission, but in a nonemergency fashion. An ‘urgent’ status has previously been shown to be an independent risk factor for morbidity and mortality for general surgery operations, as well as colon resections.18,19 The present study shows that the benefits of MIS extend to this patient population as well. 43.3% of the patients underwent an MIS colectomy in this patient cohort, which is higher than previously reported, and could be explained by the exclusion of emergency cases.16,17 Although higher than previously reported, the use of MIS in the urgent group still lags behind its use in the elective colorectal resections.8 Keller et al. found that while the vast majority of the nonelective resections were performed by general surgeons, fellowship trained colorectal surgeons were more likely to perform nonelective cases using MIS.17 While increased specialization and MIS training during fellowship may translate into greater utilization of MIS in nonelective settings, this cannot be substantiated in this study given the lack of information regarding surgeon specialty within the database. There are many other factors including, but not limited to, teaching status of the hospital and rural versus urban setting, that may influence the utilization of MIS in nonelective setting. As experience with laparoscopy increases, hopefully its utilization in urgent colorectal resections will follow.
Infectious complications following colectomy are of a particular interest, and nonelective colectomies are associated with an increased incidence of deep and organ space infections.20 The present study reveals that the odds of SSI (superficial, deep, and organ space) were significantly lower for the MIS Group (Table 2). SSIs confer a significant burden on the patients as well as the healthcare system. SSI after nonelective colorectal surgery is associated with a significantly longer LOS, a cost increase of $20,890.21,22 This has led to implementation of financial penalties for hospitals that have an increased SSI rate following colectomies.23,24 An increase in the use of MIS in this setting would likely help ameliorate the SSI.
The current study demonstrates that MIS was associated with a shorter hospital LOS by 2 days, and a shorter postoperative LOS by 3 days (Figure 2). This is consistent with previous findings in large retrospective reviews.16,17 In addition, patients undergoing MIS colectomy were also less likely to be readmitted (Table 2). Readmissions following colectomy has been shown to be associated with an increase in inpatient mortality as well as reduced 3-year survival.25 Additionally, each readmission following colorectal resection is associated with a cost of $9,000, leading to an annual cost of $300 million for colorectal readmissions nationwide.26 Hospital readmission rate has emerged as an important quality metric, and under Hospital Readmission Reduction Program, hospitals are financially penalized for excess 30-day readmission rate for certain conditions and procedures.27 The present study demonstrates that patients undergoing MIS colectomy in the urgent setting were less likely to be readmitted to the hospital. Patient comorbidities as well as perioperative complications have been shown to impact the risk of readmission.25 In the present study, a reduction in nearly all short-term complications following MIS may have led to a decrease in readmission rates.
This is the largest study to our knowledge that evaluated the use of MIS for urgent inpatient colectomies. However, there are several limitations to our study. This is a retrospective review of a large database, and as such, is vulnerable to inherent limitations to that design, particularly selection bias and errors in coding. Less than 1% of patients in both groups had a “clean” wound class. Given that colon resection are considered “clean contaminated” at minimum, these may represent cases not requiring resection (e.g. Rectopexy) or an error in coding. Furthermore, “emergency” status was designated by the operating surgeon or anesthesiologist immediately preceding the surgery. While this may lead to a selection bias, it provides a pragmatic example of patient classification. Clearly there were differences in the patients that underwent MIS colectomy compared to open. Patients who underwent MIS colectomy were less likely to have hypertension, chronic obstructive pulmonary disease, renal failure, dialysis, smoking, sepsis at the time of surgery, functional independence, as well as significant contamination. Generally sicker patients were more likely to undergo open surgery, which is consistent with previous reports.16,17 This was mitigated by the use of multivariable logistic regression using propensity scores. Lack of information for certain variables included in the multivariable model decreased the final number of patients in the multivariable model to 23,826. We believe that this is still a substantial dataset with adequate power to support the analysis. Given the large number of patients included in the analysis, some baseline variances, while statistically different, may not be clinically significant.
A further limitation is that there is no defined urgent category in the ACS NSQIP, and the urgent category is arrived at by default by excluding patients not categorized as emergency or elective. Previous studies evaluating patients undergoing colectomies in NSQIP have demonstrated that an urgent status derived using this methodology was found to be an independent risk factor for short term morbidity and mortality.18,19 While some patients including in this cohort may have been admitted for financial or logistical reasons, the overall cohort is at an increased risk of short term complications and remains relatively understudied.19 Although the ACS NSQIP collects data from over 600 hospitals, it may not be a nationally representative sample. While NSQIP does not publish data regarding surgical volumes, we speculate that larger tertiary care centers with higher volumes are more likely to participate in NSQIP and may not be applicable to all practice settings. Finally, this study evaluates overall trends across a large and heterogeneous population. The pathophysiology of the disease processes encompassed in the analysis differ significantly, limiting generalizability. Further studies may focus on the evaluation the benefit of MIS for specific disease processes.
Despite these limitations, this study demonstrates that the use of MIS for urgent inpatient colectomies is associated with improved mortality, morbidity rates including infectious complications, LOS, as well as readmission rates. Further expansion of the use of MIS for this population should be considered to optimize patient care and improve healthcare utilization. Whenever feasible, MIS should be offered to patients necessitating urgent inpatient colectomies.
Footnotes
Disclosure: none.
Funding sources: none.
Conflict of interests: none.
Informed consent: Dr. Luv N. Hajirawala declares that written informed consent was obtained from the patient/s for publication of this study/report and any accompanying images.
Contributor Information
Luv N. Hajirawala, Section of Colorectal Surgery, Department of Surgery Louisiana State University Health Sciences Center, New Orleans, LA, USA..
Varun Krishnan, Section of Colorectal Surgery, Department of Surgery Louisiana State University Health Sciences Center, New Orleans, LA, USA..
Claudia Leonardi, School of Public Health, Louisiana State University Health Sciences Center, New Orleans, LA, USA..
Elyse R. Bevier-Rawls, Section of Colorectal Surgery, Department of Surgery Louisiana State University Health Sciences Center, New Orleans, LA, USA..
Guy R. Orangio, Section of Colorectal Surgery, Department of Surgery Louisiana State University Health Sciences Center, New Orleans, LA, USA..
Kurt G. Davis, Section of Colorectal Surgery, Department of Surgery Louisiana State University Health Sciences Center, New Orleans, LA, USA..
Aaron L. Klinger, Section of Colorectal Surgery, Department of Surgery Louisiana State University Health Sciences Center, New Orleans, LA, USA..
Jeffrey S. Barton, Department of Surgery, NW Permanente, Clackamas, OR..
References:
- 1.Bonjer HJ, Nelson H, Sargent DJ, et al. Laparoscopically assisted versus open colectomy for colon cancer. Arch of Surg. 2007;142(3), 298. [DOI] [PubMed] [Google Scholar]
- 2.Veldkamp D, Kuhry E, Hop WCJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. The Lancet Oncol. 2005;6(7), 477–484. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy GD, Heise C, Rajamanickam V, et al. Laparoscopy decreases postoperative complication rates after abdominal colectomy: results from the national surgical quality improvement program. Ann Surg. 2009;249(4):596–601. [DOI] [PubMed] [Google Scholar]
- 4.Schwenk W, Haase O, Neudecker JJ, Müller JM. Short term benefits for laparoscopic colorectal resection. Cochrane Database of Syst Rev. 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lacy AM, García-Valdecasas JC, Delgado S, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359(9325):2224–2229. [DOI] [PubMed] [Google Scholar]
- 6.Delaney CP, Kiran RP, Senagore AJ, Brady K, Fazio VW. Case-matched comparison of clinical and financial outcome after laparoscopic or open colorectal surgery. Ann Surg. 2003;238(1):67–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Delaney CP, Marcello PW, Sonoda T, Wise P, Bauer J, Techner L. Gastrointestinal recovery after laparoscopic colectomy: results of a prospective, observational, multicenter study. Surg Endosc. 2010;24(3):653–661. [DOI] [PubMed] [Google Scholar]
- 8.Davis CH, Shirkey BA, Moore LW, et al. Trends in laparoscopic colorectal surgery over time from 2005–2014 using the NSQIP database. J Surg Res. 2018;223:16–21. [DOI] [PubMed] [Google Scholar]
- 9.Champagne B, Stulberg JJ, Fan Z, Delaney CP. The feasibility of laparoscopic colectomy in urgent and emergent settings. Surg Endosc. 2009;23(8):1791–1796. [DOI] [PubMed] [Google Scholar]
- 10.Nash GM, Bleier J, Milsom JW, Trencheva K, Sonoda T, Lee SW. Minimally invasive surgery is safe and effective for urgent and emergent colectomy. Colorectal Dis. 2010;12(5):480–484. [DOI] [PubMed] [Google Scholar]
- 11.Stulberg JJ, Champagne BJ, Fan Z, et al. Emergency laparoscopic colectomy: does it measure up to open? Am J Surgy. 2009;197(3):296–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Catani M, De Milito R, Romagnoli F, Romeo V, Modini C. Laparoscopic colorectal surgery in urgent and emergent settings. Surg Laparosc Endosc Percutan Tech. 2011;21(5):340–343. [DOI] [PubMed] [Google Scholar]
- 13.Marcello PW, Milsom JW, Wong SK, Brady K, Goormastic M, Fazio VW. Laparoscopic total colectomy for acute colitis. Dis Colon Rectum. 2001;44(10):1441–1445. [DOI] [PubMed] [Google Scholar]
- 14.Koea JB, Guillem JG, Conlon KC, Minsky B, Saltz L, Cohen A. Role of laparoscopy in the initial multimodality management of patients with near-obstructing rectal cancer. J Gastrointest Surg. 2000;4(1):105–108. [DOI] [PubMed] [Google Scholar]
- 15.Bleier JI, Moon V, Feingold D, et al. Initial repair of iatrogenic colon perforation using laparoscopic methods. Surg Endosc. 2008;22(3):646–649. [DOI] [PubMed] [Google Scholar]
- 16.Vallance AE, Keller DS, Hill J, et al. Role of emergency laparoscopic colectomy for colorectal cancer. Ann Surg. 2019;270(1):172–179. [DOI] [PubMed] [Google Scholar]
- 17.Keller DS, Pedraza R, Flores-Gonzalez JR, LeFave JP, Mahmood A, Haas EM. The current status of emergent laparoscopic colectomy: a population-based study of clinical and financial outcomes. Surg Endosc. 2016;30(8):3321–3326. [DOI] [PubMed] [Google Scholar]
- 18.Mullen MG, Michaels AD, Mehaffey JH, et al. Risk associated with complications and mortality after urgent surgery vs elective and emergency surgery. JAMA Surg. 2017;152(8):768–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hajirawala L, Leonardi C, Orangio G, Davis K, Barton J. Urgent inpatient colectomy carries a higher morbidity and mortality than elective surgery. J Surg Res. 2021;268:394–404. [DOI] [PubMed] [Google Scholar]
- 20.Benjamin E, Siboni S, Haltmeier T, Inaba K, Lam L, Demetriades D. Deep organ space infection after emergency bowel resection and anastomosis. J Trauma Acute Care Surg. 2015;79(5):805–811. [DOI] [PubMed] [Google Scholar]
- 21.Gantz O, Zagadailov P, Merchant AM. The cost of surgical site infections after colorectal surgery in the United States from 2001 to 2012: a longitudinal analysis. Am Surg. 2019;85(2):142–149. [PubMed] [Google Scholar]
- 22.Cologne KG, Byers S, Rosen DR, et al. Factors associated with a short (<2 days) or long (>10 days) length of stay after colectomy: a multivariate analysis of over 400 patients. Am Surg. 2016;82(10):960–963. [PubMed] [Google Scholar]
- 23.Hospital-Acquired Condition Reduction Program (HACRP). Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/HAC-Reduction-Program. Accessed July 2, 2021.
- 24.Morgan DM, Kamdar N, Regenbogen SE, et al. Evaluation of the methods used by Medicare's Hospital-Acquired Condition Reduction Program to identify outlier hospitals for surgical site infection. J Am Coll Surg. 2018;227(3):346–356. [DOI] [PubMed] [Google Scholar]
- 25.Schneider EB, Hyder O, Brooke BS, et al. Patient readmission and mortality after colorectal surgery for colon cancer: impact of length of stay relative to other clinical factors. J Am Coll Surg. 2012;214(4):390–398. [DOI] [PubMed] [Google Scholar]
- 26.Wick EC, Shore AD, Hirose K, et al. Readmission rates and cost following colorectal surgery. Dis Colon Rectum. 2011;54(12):1475–1479. [DOI] [PubMed] [Google Scholar]
- 27.Hospital Readmissions Reduction Program (HRRP). CMS. Available at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program. Accessed July 2, 2021.