Abstract
Depression affects over 40% of people with HIV (PHIV) in low- and middle-income countries, and over half of PHIV report HIV-related internalized stigma. However, few longitudinal studies of PHIV have examined the relationship between HIV-related stigma and depression. Data were analyzed from the 2007–15 Uganda AIDS Rural Treatment Outcomes (UARTO) Study, a cohort of 454 antiretroviral therapy (ART)-naïve PHIV (68% women) starting ART. Our primary outcome was depression symptom severity over the first two years of ART, measured using a locally adapted version of the Hopkins Symptom Checklist; our primary exposure was the 6-item Internalized AIDS-Related Stigma Scale. Both scores were measured at enrollment and at quarterly follow-up visits. We fit linear generalized estimating equations (GEE) regression models to estimate the association between stigma and depression symptom severity, adjusting for potential confounders. We included a stigma×time product term to assess the modifying effect of ART on the association between internalized stigma and depression symptom severity. UARTO participants had a median age of 32 years and median enrollment CD4 count of 217 cells/mm3. Both depression symptom severity and internalized stigma declined on ART, particularly during the first treatment year. In multivariable regression models, depression symptom severity was positively associated with internalized stigma (b=0.03; 95% confidence interval [CI], 0.02 to 0.04) and negatively associated with ART duration >6 months (b =− 0.16; 95% CI,− 0.19 to −0.13). The estimated product term coefficient was negative and statistically significant (P = 0.004), suggesting that the association between internalized stigma and depression symptom severity weakened over time on ART. Thus, in this large cohort of PHIV initiating ART in rural Uganda, depression symptom severity was associated with internalized stigma but the association declined with time on ART. These findings underscore the potential value of ART as a stigma reduction intervention for PHIV, particularly during early treatment.
Keywords: Antiretroviral therapy, Depression, Discrimination, HIV, Mental health, Prejudice, Stigma, Sub-saharan africa, Uganda
1. Introduction
Depression is highly prevalent among people with HIV (PHIV), affecting approximately one-third of all PHIV worldwide and over 40% of PHIV in low- and middle-income countries (Kinyanda et al., 2011; Lowther et al., 2014; Nakasujja et al., 2010; Nakimuli-Mpungu et al., 2011; Tsai, 2014). In addition, as many as half of all PHIV report HIV-related internalized stigma (Lowther et al., 2014; Pantelic et al., 2015; Remien & Mellins, 2007; Tsai, 2015), which tends to inhibit serostatus disclosure to partners and family members (Simbayi et al., 2007; Tsai et al., 2013a) and, erodes social support ( Logie& Gadalla, 2009; Rueda et al., 2016; Takada et al., 2014), and is associated with depression (Akena et al., 2012; Ashaba et al., 2018; Boyes et al., 2020; Rueda et al., 2016; Simbayi et al., 2007). Internalized stigma, conceptualized here as self-defacing internal representations of what it means to be a person living with HIV (Kalichman et al., 2009), is negatively associated with other important outcomes, including poor adherence to antiretroviral therapy (ART) and HIV disease control (Earnshaw et al., 2013; Katz et al., 2013; Pantelic et al., 2020; Tsai et al., 2010; Turan et al., 2019), and quality of life (Onyebuchi-Iwudibia & Brown, 2014).
The framework that organizes our conceptualization of the relationship between HIV-related internalized stigma and depression is based on the idea that the internalization of stigma can lead to depressive symptoms, due to a constellation of self-defacing self-perceptions, including feelings of worthlessness, shame, and guilt (Kalichman et al., 2009). There is mounting evidence that HIV-related stigma can become internalized and that, once internalized, stigma can adversely affect mental health (Simbayi et al., 2007; Tsai et al., 2012). Stigma is multifaceted, embedded in social and structural systems, and it is natural for people to internalize negative messages conveyed by people, norms, policies, and/or institutions (Link et al.,; Evans-Lacko et al., 2012; Corrigan et al., 2004; Tsai et al., 2019). Although internalized stigma is only one dimension of stigma, studies conducted in a range of settings suggest that internalized stigma can account for a significant and unique proportion of depressive symptoms, including among PHIV in North America (Lee et al., 2002), South Africa (Simbayi et al., 2007), and Uganda (Tsai et al., 2012). These findings suggest that internalized HIV-related stigma plays a key role in depressive symptoms and emotional wellbeing among PHIV across cultures. People with HIV can also perceive and anticipate rejection from others on the basis of their serostatus (perceived and anticipated stigma) (Tsai et al., 2021); experience behavioral manifestations of stigma directly from others (enacted stigma) (Scambler & Hopkins, 1986); and experience normative or codified manifestations of stigma directly through policies and institutions (Corrigan et al., 2004). All of these facts of stigma are also associated, in the context of HIV, with poor HIV and health care outcomes. Further, the stigma of HIV can also intersect with the stigma attached to other marginalized identities, compounding the nature of the stigma felt or experienced and the resulting adverse health and mental health outcomes (Goodin et al., 2018; Logie et al., 2011, 2019). In this analysis, we focused on one dimension of stigma – internalized stigma – given its substantive role in the genesis of depression among people with HIV(10, 24, 29).
The advent of ART has been conceptualized as a population-level anti-stigma intervention, given its role in attenuating the fear associated with an HIV diagnosis and in transforming HIV from a terminal illness into a chronic illness (Farmer et al., 2001a, 2001b). Consistent with this argument, several population-level studies have found the introduction and scale-up of ART to be associated with decreases in stigmatizing attitudes toward PHIV and in perceived stigma attached to HIV disease (Chan et al., 2015a; Wolfe et al., 2008). In addition to the direct effects of ART on stigma, ART may also modify the relationship between stigma and other psychosocial outcomes of interest, for example, by increasing weight gain, enhancing body self-image, and improving overall health and economic productivity (Thirumurthy et al., 2008; Venkataramani et al., 2014) – and thereby weakening the adverse mental health effects of internalized stigma (Tsai et al., 2013b). Although ART may be an important treatment for HIV-related internalized stigma, larger social and structural contexts amplify stigma, and stigma operates on many levels, intersecting with other identities including gender identity, sexual orientation, socioeconomic status, and work identity. Thus, HIV-related stigma may be mitigated by ART due to reduced fear of morbidity and infection, but is also grounded in pre-existing social inequalities, cultural norms and values, including misinformation and fear, which may act as barriers to ART access (Stangl et al., 172019). Thus, although ART may address some aspects of stigma, other stigma dimensions and intersecting forms of stigma exist.
However, the longitudinal relationship between HIV-related internalized stigma and depression is incompletely characterized. While HIV-related internalized stigma is known to decline during ART in part through improved self-image and feelings of empowerment, particularly in the first 2 years of treatment (Tsai et al., 2013c), and ART is associated with improved psychological wellbeing (Martinez et al., 2014; Tsai et al., 2013c; Wagner et al., 2012), depression remains highly prevalent among PHIV on ART (Tsai, 2014). Further, in some studies depressive symptoms have been shown to increase after 12 months on ART (Pearson et al., 2009; Peltzer & Ramlagan, 2011).
In this secondary analysis of data from a large cohort of ART-naïve PHIV initiating ART in rural Uganda (Uganda AIDS Rural Treatment Outcomes [UARTO]), we sought to estimate the association between internalized stigma and depression symptom severity during the first two years of treatment. Additional studies of related topics have been carried out in this population (Tsai et al., 2012, 2013a, 2013d). Specifically, our aims were to estimate the association between internalized stigma and depression symptom severity, and to assess the extent to which duration of ART modifies the estimated association. We hypothesized that internalized stigma would be positively associated with depression symptom severity and that the magnitude and strength of this association would decline over time on ART. If shown to be true, our hypothesis would identify improvements in HIV-associated depressive symptoms as a significant collateral benefit of ART, and also emphasize the importance of early and sustained ART treatment, especially in PHIV with clinically significant mental health problems.
2. Material and methods
2.1. Study design
Data for this analysis were obtained from the Uganda AIDS Rural Treatment Outcomes (UARTO, NCT01596322) study, a cohort of treatment-naïve PHIV initiating ART between 2005 and 2013 enrolled to elucidate the social and biological correlates of ART adherence. Participants were recruited from the Mbarara Immune Suppression Syndrome (ISS) Clinic, an ART clinic located in Mbarara, Uganda, 270 km southwest of Kampala. The clinic is representative of other regional HIV clinics, receiving program funding from multilateral programs including the U.S. President's Emergency Plan for AIDS Relief (PEPFAR) (Geng et al., 2010). ISS patients were eligible for UARTO participation if they tested positive for HIV infection, were newly initiating ART, were 18 years of age, and lived within 60 km of the clinic. Participants who declined to initiate ART or who lived outside of the catchment area were excluded. For this analysis we further excluded any participants who were missing data on the primary exposure and outcome of interest within 3 months of ART initiation.
Before initiating ART, participants were required to complete two pre-treatment counseling sessions conducted by clinic staff employees trained as counselors (Siedner et al., 2012). Counseling sessions focused on treatment schedules, potential toxicities, ART resistance resulting from suboptimal adherence, and managing missed doses. Adherence counseling was generally not provided at subsequent visits. At the pre-treatment baseline visit, participants underwent phlebotomy and structured interviews conducted by a research assistant in the local language, Runyankole.
The most common ART regimens at initiation were zidovudine/ lamivudine/nevirapine (AZT/3TC/NVP), stavudine/lamivudine/nevirapine (D4T/3TC/NVP), and tenofovir/lamivudine/efavirenz (TDF/3TC/ EFV), used by 62, 26 and 10% of participants, respectively. Thus, nevirapine- and efavirenz-containing regimens accounted for 98% of all ART. Once a participant was stable on a specific ART regimen, the participant returned at regular intervals for usual care with a medical/clinical officer or a nurse. Every 3–4 months, UARTO participants underwent repeat phlebotomy and a structured interview. Internalized stigma assessments were added to the UARTO study in 2007. All study participants with at least one internalized stigma baseline screen measurement were included in this current analysis. The cohort was followed until 2015 to ensure at least 24 months of follow-up for the participants enrolled in 2013. Written or thumbprint-mark consent was obtained from all study participants. Ethical approval was obtained from the University of California at San Francisco Committee on Human Research, the Partners Human Research Committee, and the Mbarara University of Science and Technology Research Ethics Committee. Consistent with national guidelines, we also obtained clearance for the study from the Uganda National Council of Science and Technology.
2.2. Measures
The primary outcome was depression symptom severity, measured by the depression subscale of the Hopkins Symptom Checklist (HSCL) (Derogatis et al., 1974). The original subscale consists of 15 items. We removed four somatic items (“feeling low in energy, slowed down,” “feeling fidgety,” “poor appetite,” and “having difficulty falling or staying asleep”) to minimize overlap between depressive symptoms of depression and HIV disease (Kalichman et al., 2000), and added one item to capture a locally validated concept indicative of depression in Uganda (“feeling like I don't care what happens to my health”) (Bolton & Ndogoni, 2001). The modified depression subscale is scored by averaging across the 12 items (Bolton & Ndogoni, 2001; Tsai et al., 2012). To define a positive screen for clinically significant symptoms of depression (“probable depression”), we used the cutoff of >1.75 used by Hesbacher et al. (Hesbacher et al., 1980), which has previously been used in this population (Tsai et al., 2012). The primary exposure was internalized stigma, measured by the IARSS (Kalichman et al., 2009), a six-item scale measuring internalized stigma and associated self-defacing internal representations of the self. The IARSS was developed using three independent samples of PHIV in South Africa, Swaziland, and the United States, and has a coherent internal structure, good reliability, and construct validity among PHIV in Uganda (Tsai et al., 2013a, 2013d). Each item has two response options (“Yes” or “No”), and higher IARSS scores indicate a greater degree of internalized stigma. The IARSS is one of the most widely used scales to assess internalized HIV-related stigma (Pantelic et al., 2015) and has been validated in numerous settings throughout sub-Saharan Africa (Geibel et al., 2020; MacLean & Wetherall, 2021).
The HSCL and IARSS were administered at the baseline enrollment visit and subsequent quarterly follow-up visits. For participants missing either measure at enrollment, the score from the earliest visit was used if measured within one month of starting ART. For follow-up visits, measurements within three months of each visit were used. Visits without an HSCL and IARSS score within three months of baseline enrollment were excluded from the analysis.
Socio-demographic variables collected at the baseline visit included age, sex, primary education completion, marital status, household asset wealth (Smith et al., 2020), harmful alcohol consumption (3-item consumption subset of the Alcohol Use Disorders Identification Test [AUDIT-C]) (Adong et al., 2019; Asiimwe et al., 2015; Bradley et al., 2003; Bush et al., 1998; Thakarar et al., 2016), and employment status. For the asset wealth measure, we applied principal components analysis to 25 binary variables for household-owned assets and housing characteristics (Filmer & Pritchett, 2001). The first principal component was retained and used to define the wealth index and was used as a continuous variable in regression models, with higher values indicating greater asset wealth.
For analysis purposes, the cohort was divided into those enrolled during 2007–2009 (earlier group) and those enrolled during 2010–2013 (later group). This stratification was performed because Ugandan National ART Treatment guidelines changed in 2009, increasing the CD4 threshold for ART initiation from <250 to <350 cells/mm3. Starting in 2010, large numbers of participants with CD4 counts >250 cells/mm3 were enrolled into UARTO.
2.3. Statistical analysis
Descriptive statistics were used to characterize the cohort, comparing the earlier (2007–2009) and later (2010–2013) participant groups. For the primary analysis characterizing the relationship between internalized stigma and depression symptom severity, we fit a linear generalized estimating equations (GEE) regression model with HSCL score as a continuous outcome variable and IARSS stigma score as a continuous exposure variable, using cluster-correlated robust estimates of variance to account for repeated measures within participants over time. Time on ART was dichotomized into >6 months versus ≤6 months. In sensitivity analyses, we fit a logistic GEE regression model specifying probable depression (HSCL score >1.75) as the dichotomous outcome and any internalized stigma (IARSS >0) as the dichotomous exposure. An additional linear GEE model was fitted examining depression symptom severity over 4-month intervals after starting ART. We then restricted the GEE analyses to participants with at least 24 months in follow-up on ART, modeling depression and internalized stigma as continuous and categorical variables. All estimates were adjusted for the sociodemographic variables described above, continuous CD4 T-cell count (cells/mm3), ART duration, and year of cohort entry to account for secular trends in HIV-associated internalized stigma over time.
To estimate the extent to which ART modified the association between internalized stigma and depression symptom severity, we specified time on ART as a continuous variable (in months) and then included a stigma×time product term. A negative coefficient was interpreted as evidence that the estimated association between internalized stigma and depression symptom severity declined (i.e., weakened) over time on ART.
To assess the robustness of our findings to unobserved confounding, we used methods proposed by VanderWeele et al. (VanderWeele & Ding, 2017). We performed an e-value analysis to estimate the minimum strength of association on the risk ratio scale that would be needed for an unobserved confounder to have with both the exposure (internalized stigma) and the outcome (depression symptom severity), assuming the covariates as measured, to explain away the observed association. The e-value quantifies the extent to which unobserved confounding might contribute to the findings. Analyses were conducted using Stata version 16.0 (StataCorp LP, College Station, TX, USA) and the figure was generated using GraphPad Prism 8.4.3 (GraphPad Software, San Diego, CA, USA).
3. Results
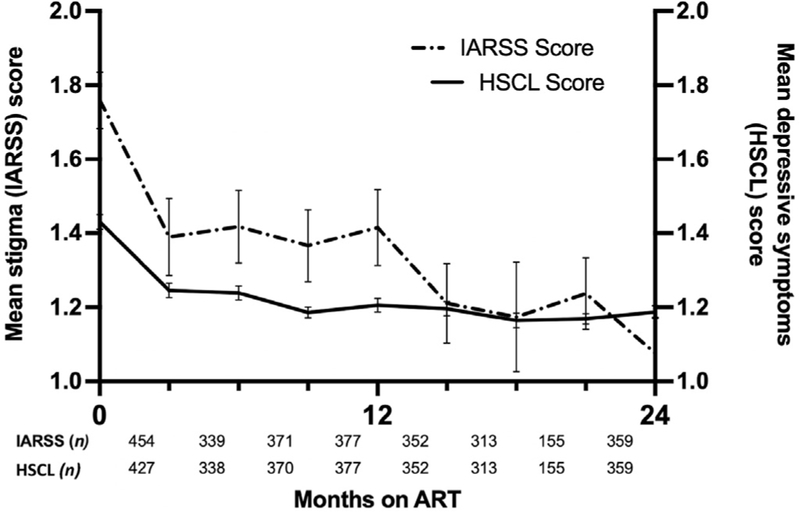
A total of 454 participants were enrolled. Cohort characteristics are presented in Table 1, grouped by year of enrolment (2007–2009 versus 2010–2013). Overall, 407 (90%) participants were retained in follow-up for 24 months or longer, similar for both groups (P=0.95). The median enrollment age was 32 years (interquartile range [IQR] 27–40). Most were women (68%). The median baseline CD4 count was 157 cells/mm3 among participants enrolled in the earlier group versus 292 cells/mm3 among participants enrolled in the later group (P < 0.001). No statistically significant differences were observed in mean log10 viral load (P = 0.16). A total of 427 (94%) participants had a baseline HSCL score, and 413 (91%) had a baseline IARSS score, measured within one month of starting ART. The median baseline IARSS score was 1 among participants enrolled in the earlier group versus 2 among participants enrolled in the later group (P = 0.05). The proportion with probable depression was similar in a comparison of the earlier versus later groups (24% versus 26%, P = 0.63). The overall proportion with probable depression decreased rapidly during the first year of treatment, to 6% at 12 months and to 4% at 24 months. Paralleling this trend, the mean depression symptom severity score declined rapidly during treatment. The mean internalized stigma score also declined during this time (Fig. 1).
Table 1.
Participant characteristics as measured at the baseline interview, by year of enrolment into the UARTO cohort.
| Characteristic | Total cohort n = 454 | 2007–2009 n = 195 | 2010–2013 n = 259 | P-value |
|---|---|---|---|---|
|
| ||||
| Retained in follow-up for ≥12 months on ART | 432 (95) | 181 (93) | 251 (97) | 0.05 |
| Retained in follow-up for ≥24 months on ART | 407 (90) | 175 (90) | 232 (90) | 0.95 |
| Age in years, median (IQR) | 32 (27, 40) | 34 (28, 39) | 31 (26, 40) | 0.19 |
| Women | 308 (68) | 133 (68) | 175 (68) | 0.89 |
| Married | 247 (54) | 90 (46) | 157 (61) | 0.002 |
| Christian religious affiliation | 408 (90) | 175 (90) | 233 (90) | 0.94 |
| Beyond primary education | 123 (27) | 44 (23) | 79 (31) | 0.06 |
| Asset wealth indexa | <0.001 | |||
| Poorest quartile | 110 (24) | 66 (34) | 44 (17) | |
| Poorer | 113 (25) | 50 (26) | 63 (24) | |
| Less poor | 118 (26) | 45 (23) | 73 (28) | |
| Least poor quartile | 113 (25) | 34 (17) | 79 (31) | |
| Employed outside the home | 341 (75) | 135 (69) | 206 (80) | 0.01 |
| Harmful alcohol use in year before starting ART | 172 (38) | 81 (42) | 91 (35) | 0.14 |
| BMI category | 0.005 | |||
| <18 | 41 (9) | 24 (13) | 17 (7) | |
| 18–25 | 316 (70) | 139 (73) | 177 (68) | |
| >25 | 93 (21) | 28 (15) | 65 (25) | |
| CD4 count, median (IQR) | 217 (129, 329) | 157 (95, 220) | 292 (193, 390) | <0.001 |
| CD4 category | <0.001 | |||
| <100 | 76 (17) | 50 (26) | 26 (10) | |
| 100–250 | 191 (42) | 115 (59) | 76 (29) | |
| ≥350 | 94 (21) | 11 (6) | 83 (32) | |
| HIV viral load (log10), mean (SD) | 4.8 (0.9) | 4.9 (0.8) | 4.8 (0.9) | 0.16 |
| Probable depression (HSCL score >1.75) | 107 (25) | 40 (24) | 67 (26) | 0.63 |
| IARSS (stigma) score, median (IQR) | 1 (0, 3) | 1 (0, 3) | 2 (0, 4) | 0.05 |
ART = antiretroviral therapy; BMI = body mass index in kg/m2; CD4 = CD4+ T lymphocyte count in cells/mm3; HSCL = Hopkins Symptom Checklist; IARSS = Internalized AIDS-Related Stigma Scale; IQR = interquartile range; SD = standard deviation; UARTO = Uganda AIDS Rural Treatment Outcomes.
Results listed as n (%) unless otherwise noted. Tests of association were performed using Chi-squared, Wilcoxon rank sum, and t-tests.
The asset index variable was calculated using principal components analysis. By definition, the within-cohort mean is equal to zero. Positive scores indicate increasing wealth, and negative scores indicate decreasing wealth.
Fig. 1.
Unadjusted mean stigma (IARSS) and depressive symptom (HSCL) scores by ART duration.
Depression symptom severity was measured by the HSCL on the continuous scale, with a higher score indicating more severe depressive symptoms. Internalized stigma was measured by the IARSS on the continuous scale, with a higher score indicating a greater degree of internalized stigma. Bars represent standard errors.
Our primary multivariable linear GEE regression model demonstrated that depression symptom severity was positively associated with greater internalized stigma (b = 0.03; 95% confidence interval [CI], 0.02–0.04) (Table 2). The magnitude of this estimate can be appreciated by comparing it with the mean baseline HSCL of 1.50: an individual with a maximum IARSS score of 6 would have a predicted HSCL score of 1.73, or approximately 15% higher relative to the baseline mean. The depression symptom severity was also negatively associated with ART treatment duration >6 months (b =− 0.16; 95% CI,−0.19 to −0.13). Sensitivity analysis using a dichotomous outcome variable (HSCL score cutoff of >1.75, indicating probable depression) yielded similar results. Additional analysis demonstrated a stigma × gender product term was not statistically significant.
Table 2.
Correlates of depression symptom severity over the first 24 months of antiretroviral therapy (N = 454). Using a multivariable linear GEE regression model, both internalized stigma (IARSS) and depression symptom severity (HSCL) were modeled as continuous variables. The estimated regression coefficient (b) represents the change in depression symptom severity associated with each 1-point change in internalized stigma.
| Variable | b coefficient | 95% Confidence Interval (CI) | P-value |
|---|---|---|---|
|
| |||
| IARSS score | 0.03 | 0.02, 0.04 | <0.001 |
| >6 months on ART (versus ≤6 months) | −0.16 | −0.19, −0.13 | <0.001 |
| Year of cohort enrolment | −0.006 | −0.02, 0.007 | 0.38 |
| Female sex (versus male) | 0.12 | 0.07, 0.17 | <0.001 |
| Age | 0.002 | −0.0003, 0.005 | 0.08 |
| Asset index quartilea | |||
| Poorest quartile | Reference | ||
| Poorer | −0.0008 | −0.07, 0.06 | 0.98 |
| Less poor | −0.04 | −0.10, 0.02 | 0.23 |
| Least poor quartile | −0.05 | −0.11, 0.02 | 0.18 |
| CD4 count | 0.00009 | −0.00004, 0.0002 | 0.19 |
| Primary or no formal education (versus more than primary education) | 0.01 | −0.04, 0.07 | 0.61 |
| Married (versus never married, separated/divorced, or widowed) | 0.002 | −0.04, 0.05 | 0.92 |
CI = confidence interval; HSCL = Hopkins Symptom Checklist; IARSS = Internalized AIDS-Related Stigma Scale; ART = antiretroviral therapy; CD4 = CD4+ T lymphocyte count in cells/mm3.
The asset index variable was calculated using a principal components analysis. By definition, the within-cohort mean is equal to zero. Positive scores indicate increasing wealth, and negative scores indicate decreasing wealth.
When stratified by duration of ART, the estimated association remained statistically significant, but the magnitude decreased over time. In a linear GEE regression model specifying a product term for stigma×ART duration, the interaction was negative and statistically significant (b =−0.02, 95% CI -0.04 to −0.007, P = 0.004), suggesting that the estimated association between internalized stigma and depression symptom severity was modified by ART treatment duration, i.e., the association between internalized stigma and depressive symptoms weakened over time on ART. The estimated association between internalized stigma and depression symptom severity was strongest during months 0–4 of ART (b = 0.04, 95% CI 0.02–0.06, P <0.001) and weakened over successive intervals on ART (Table 3). By 24 months of treatment, the estimated association between internalized stigma and depression symptom severity was no longer statistically significant.
Table 3.
Association between internalized stigma (IARSS) and depressive symptom severity (HSCL) over successive intervals of HIV antiretroviral therapy adjusting for potential confounders, with IARSS score as a continuous exposure, and HSCL score as a continuous outcome (N = 454).
| b coefficient (95% CI) | P-value | |
|---|---|---|
|
|
|
|
| Multivariable adjusted modelsa | ||
|
| ||
| 0–4 months | 0.04 (0.02, 0.06) | 0.001 |
| 4–8 months | 0.03 (0.008, 0.05) | 0.006 |
| 8–12 months | 0.02 (0.001, 0.04) | 0.04 |
| 12–16 months | 0.03 (0.009, 0.05) | 0.004 |
| 16–20 months | 0.03 (0.005, 0.05) | 0.01 |
| 20–24 months | 0.02 (0.003, 0.04) | 0.02 |
| ≥ 24 months | 0.02 (−0.008, 0.04) | 0.20 |
CI = confidence interval; HSCL = Hopkins Symptom Checklist; IARSS = Internalized AIDS-Related Stigma Scale.
each row represents the output of a multivariable regression model, with the cell displaying only the estimated association between internalized stigma (IARSS) and depression symptom severity (HSCL) adjusted for year of enrollment into cohort, age, gender, asset index quartile, CD4 count at baseline, educational level, and marital status.
In a secondary analysis, we fit a multivariable logistic GEE regression model showing that any internalized stigma was positively associated with probable depression (adjusted odds ratio [AOR] = 2.11; 95% CI, 1.56–2.84; P <0.001) (Table 4). Using the odds ratio correction described by VanderWeele (VanderWeele & Ding, 2017), we obtained an e-value of 2.26. Thus, an unobserved confounder would require a strength of association, on the risk ratio scale, with both internalized stigma and probable depression of 2.26 each to shift our estimated association to the null value of 1. This result suggests that confounding by an unmeasured variable would need to be relatively strong in order to fully explain the association between internalized stigma and probable depression observed in our study.
Table 4.
Correlates of probable depression (HSCL >1.75) over the first 24 months of antiretroviral therapy (N = 454). Using a multivariable logistic GEE regression model, both internalized stigma and depression symptom severity were modeled as dichotomous variables (IARSS >0 and HSCL >1.75). The estimated regression coefficients were exponentiated so that they could be interpreted as adjusted odds ratios, which represents the change in odds of probable depression associated with a unit change in the covariates.
| Variable | AOR | 95% Confidence Interval (CI) | P-value |
|---|---|---|---|
|
| |||
| IARSS score >0 (versus 0) | 2.11 | 1.56, 2.84 | <0.001 |
| >6 months’ on ART (versus ≤6 months) | 0.32 | 0.24, 0.41 | <0.001 |
| Year of cohort enrolment | 1.00 | 0.91, 1.11 | 0.92 |
| Female sex (versus male) | 2.70 | 1.65, 4.44 | <0.001 |
| Age | 1.01 | 0.99, 1.03 | 0.37 |
| Asset index quartilea | |||
| Poorest quartile | 0.87 | 0.53, 1.43 | 0.59 |
| Poorer | 0.60 | 0.35, 1.03 | 0.06 |
| Less poor | 0.60 | 0.34, 1.05 | 0.07 |
| CD4 count | 1.00 | 1.00, 1.00 | 0.29 |
| Primary or no formal education (versus more than primary education) | 0.91 | 0.58, 1.41 | 0.66 |
| Married (versus never married, separated/divorced, or widowed) | 1.02 | 0.69, 1.51 | 0.92 |
AOR = adjusted odds ratio; CI = confidence interval; HSCL = Hopkins Symptom Checklist; IARSS = Internalized AIDS-Related Stigma Scale; ART = antiretroviral therapy; CD4 = CD4+ T lymphocyte count (cells/mm3).
The asset index variable was calculated using a principal components analysis. By definition, the within-cohort mean is equal to zero. Positive scores indicate increasing wealth, and negative scores indicate decreasing wealth.
4. Discussion
In this secondary analysis of data from a large cohort of ART-naïve PHIV initiating ART in rural Uganda, we estimated a strong and statistically significant association between internalized stigma and depression symptom severity over the first two years of treatment. As hypothesized, we found that internalized stigma was robustly associated with depression symptom severity at baseline, and that the magnitude and strength of this association declined over time on ART. Our primary finding is consistent with other reports that HIV-related internalized stigma declines during ART, particularly in the first two years of treatment (Tsai et al., 2013c). Multiple factors likely contribute to this decline, including acceptance of HIV diagnosis, increasing medical and social support over time, and improved physical health with ART and ensuing economic and social reintegration (Thirumurthy et al., 2008; Tsai et al., 2013b; Venkataramani et al., 2014). However, in contrast to other studies demonstrating that depression continues to be prevalent among PHIV on ART (Pearson et al., 2009; Peltzer & Ramlagan, 2011; Tsai, 2014), we found a low (6%) prevalence of probable depression at 12 months, which remained low at 24 months (4%). In our analyses, we did not see evidence of rebounding depressive symptoms at 24 months’ follow-up. The prevalence of probable depression at baseline enrollment in this sample (24–26%) was comparable to other studies conducted in sub-Saharan Africa (Tsai, 2014). It remains important to identify and treat depressive symptoms among PHIV, because depression treatment has been associated with improved mental health and, potentially, HIV-related outcomes including improved ART uptake and adherence and lower HIV viral load in several studies (Pence et al., 2015; Safren et al., 2016; Tsai et al., 2010, 2013e).
The decrease in depressive symptoms we observed over time could be due to ART therapy itself (Martinez et al., 2014), which could have a positive impact on feelings of agency and hope among PHIV (Chan et al., 2015a; Chan & Tsai, 2016; Tsai et al., 2013b). Furthermore, ART may improve depressive symptoms through biologic and immunologic pathways. One such mechanism is through switching off the indoleamine 2, 3-dioxygenase-1 pathway activated by HIV viral products, leading to reversal of tryptophan catabolism and a decreasing kynurenine:-tryptophan ratio (Martinez et al., 2014). It is also possible that depressive symptoms declined over time due to changes in ART regimens, based on prior studies noting differences in depressive symptoms associated with nevirapine-based ART compared to efavirenz-based ART (Chan et al., 2015b; Chang et al., 2018). In this cohort, 88% of participants initiated ART containing nevirapine, a proportion which likely decreased over time as efavirenz use increased. However, decreases in depressive symptoms could also be mediated by other explanatory factors, including weight gain (which is viewed favorably in this setting (Wittenberg, 2013)) and attendant improvements in self-esteem, positive relationships between clinic staff and caregivers, other components of the total ‘package’ of HIV care, and disclosure. It is nonetheless important to note that time on ART and calendar time are collinear (Chan et al., 2015a; Chan & Tsai, 2016), and thus regression to the mean as a potential explanation for the observed reductions in depressive symptoms cannot be completely ruled out. However, we believe this to be less likely given that depression is known to impede engagement with HIV care (Cichowitz et al., 2017; Gardner et al., 2016; Kinyanda et al., 2018; Nakimuli-Mpungu et al., 2015; Zuniga et al., 2016). Nevertheless, given the way in which the effect of internalized stigma on depression waned over time on ART, we advocate for early and sustained ART adherence (Haberer et al., 2017) and stigma reduction interventions for all PHIV (Stangl et al., 2013). In addition to the negative correlation between depressive symptoms and ART adherence, higher baseline internalized stigma scores also predict poor adherence to ART over time (Turan et al., 2019), reinforcing our conclusion that early interventions to reduce internalized stigma in PHIV could lead to better outcomes over time. Fundamental interventions are needed to identify and treat HIV infection early; to promote increased access to ART, especially amongst socially marginalized groups; and to sustain uninterrupted ART therapy over at least the first two years after initiation. Interventions should be multi-level, challenge stigmatizing community and institutional norms, and incorporate bi-directional learning involving stigmatized people in the process (Rao et al., 2019). Such interventions may also need to account for intersecting stigmas by incorporating outreach to specific marginalized groups experiencing varying degrees of structural oppression in order to engage PHIV in advocacy and leverage their strengths in coping, social support, and solidarity (Charurat et al., 2015; Ogunbajo et al., 2020; Papworth et al., 2013; Schwartz et al., 2015). However, even in populations where ART has decreased internalized HIV-related stigma, disclosure concerns may persist, especially among PHIV taking ART (Chan et al., 2019). Furthermore, medication adherence may still be affected by HIV-related internalized stigma, limiting the effectiveness of ART on reducing stigma (Blake Helms et al., 2017; Katz et al., 2013; Tsai et al., 2013a).
Strengths of our study include the large cohort size, high retention in care over two years of follow-up, and regular assessment of both internalized stigma and depressive symptoms, reducing the potential to miss rebounding depressive symptoms over time on ART. Furthermore, mental health outcomes have been understudied in our study population, PHIV in rural areas of sub-Saharan Africa. Limitations of our study include the lack of an untreated control group and incomplete measurement of other possible confounders of both internalized stigma and depressive symptoms over time. The e-value quantifies the extent to which unobserved confounding could potentially explain away the observed findings. As a concrete example, data on coping/self-efficacy were not collected in this cohort, so we could not adjust our estimates for this important (and potentially confounding) variable. However, in previously published studies (albeit conducted in different settings), the estimated associations between coping and depression (AOR = 0.54) (Chaudoir et al., 2012) and between self-efficacy and internalized stigma (AOR = 0.65) (Li et al., 2011), when inverted, were smaller than the estimated e-value of 2.26 – suggesting that our failure to adjust for coping/self-efficacy would be unlikely to completely explain the observed association. BMI data were also insufficient to integrate into the manuscript analysis and make conclusions about the relationship between BMI and internalized stigma and related depressive symptoms. Furthermore, we were unable to assess mediators of depressive symptoms, or to determine the impact of ART on depressive symptoms independent of other elements of the HIV care ‘package’. In addition, we focused on internalized stigma for this analysis, which represents only one dimension of stigma. This focus provides a unidimensional and individual-level picture of one aspect of stigma, one facet of the social and structural production of stigma and its consequences. Additional studies focused on other aspects of stigma will help provide a more complete picture of HIV-related stigma in all its forms. Lastly, the original study providing data for this analysis ended in 2015. Thus, although HIV-associated stigma remains a significant problem for PHIV, it is possible that internalization of stigma and its relationship to depressive symptoms has changed with time.
5. Conclusions
Higher degree of internalized stigma was longitudinally associated with higher depression scores in this large cohort of PHIV initiating ART. Both depression symptom severity and internalized stigma declined on ART, particularly during the first treatment year. The association between internalized stigma and depression symptom severity weakened over time on ART. Our findings underscore the need for early and sustained ART adherence for PHIV. Future research should examine the separate contributions of ART and stigma reduction measures to reducing depressive symptoms among PHIV, longer-term associations between internalized stigma, ART, and depressive symptoms beyond two years on ART; and how the relationship between internalized stigma and depressive symptoms has evolved over time.
Acknowledgements
The authors would like to thank the individuals who participated in the UARTO study and the ISS clinic staff.
Funding
The project and analysis was supported by the following grants from the National Institutes of Health: R01MH054907, K24AA015287, K23AI138856, R01MH113494, and K23MH108440.
List of abbreviations
- ART
Antiretroviral therapy
- BMI
Body mass index
- CD4
CD4+ T-cell count
- CI
Confidence interval
- GEE
Generalized estimating equations
- HIV
Human immunodeficiency virus type 1
- HSCL
Hopkins Symptom Checklist
- IASS
Internalized AIDS Stigma Scale
- IQR
Interquartile range
- OR
Oddsratio
- PEPFAR
President's Emergency Fund for AIDS Relief
- PHIV
People with HIV
- SD
Standard deviation
- UARTO
Uganda AIDS Rural Treatment Outcomes
Footnotes
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Disclaimer
The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
References
- Adong J, Fatch R, Emenyonu NI, Cheng DM, Muyindike WR, Ngabirano C, et al. (2019). Social desirability bias impacts self-reported alcohol use among persons with HIV in Uganda. Alcoholism: Clinical and Experimental Research, 43(12), 2591–2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akena D, Musisi S, Joska J, & Stein DJ (2012). The association between aids related stigma and major depressive disorder among HIV-positive individuals in Uganda. PLoS One, 7(11), Article e48671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashaba S, Cooper-Vince C, Maling S, Rukundo GZ, Akena D, & Tsai AC (2018). Internalized HIV stigma, bullying, major depressive disorder, and high-risk suicidality among HIV-positive adolescents in rural Uganda. Glob Ment Health (Camb), 5, e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asiimwe SB, Fatch R, Emenyonu NI, Muyindike WR, Kekibiina A, Santos GM, et al. (2015). Comparison of traditional and novel self-report measures to an alcohol biomarker for quantifying alcohol consumption among HIV-infected adults in sub-saharan Africa. Alcoholism: Clinical and Experimental Research, 39(8), 1518–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake Helms C, Turan JM, Atkins G, Kempf MC, Clay OJ, Raper JL, et al. (2017). Interpersonal mechanisms contributing to the association between HIV-related internalized stigma and medication adherence. AIDS and Behavior, 21(1), 238–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton P, & Ndogoni L (2001). In Cross-cultural assessment of trauma-related mental illness (Zhase II): A report of research conducted by World vision Uganda and the Johns Hopkins University. US agency for international development, the Johns Hopkins University, and world vision International. [Google Scholar]
- Boyes ME, Pantelic M, Casale M, Toska E, Newnham E, & Cluver LD (2020). Prospective associations between bullying victimisation, internalised stigma, and mental health in South African adolescents living with HIV. Journal of Affective Disorders, 276, 418–423. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, et al. (2003). Two brief alcohol-screening tests from the alcohol use disorders identification test (AUDIT): Validation in a female veterans affairs patient population. Archives of Internal Medicine, 163(7), 821–829. [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, & Bradley KA (1998). The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory care quality improvement project (ACQUIP). Alcohol use disorders identification test. Archives of Internal Medicine, 158(16), 1789–1795. [DOI] [PubMed] [Google Scholar]
- Chang JL, Tsai AC, Musinguzi N, Haberer JE, Boum Y, Muzoora C, et al. (2018). Depression and suicidal ideation among HIV-infected adults receiving efavirenz versus nevirapine in Uganda: A prospective cohort study. Annals of Internal Medicine, 169(3), 146–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan BT, Maughan-Brown BG, Bogart LM, Earnshaw VA, Tshabalala G, Courtney I, et al. (2019). Trajectories of HIV-related internalized stigma and disclosure concerns among ART initiators and non-initiators in South Africa. Stigma Health, 4(4), 433–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan BT, & Tsai AC (2016). HIV stigma trends in the general population during antiretroviral treatment expansion: Analysis of 31 countries in sub-saharan Africa, 2003–2013. Journal of Acquired Immune Deficiency Syndromes, 72(5), 558–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan BT, Tsai AC, & Siedner MJ (2015). HIV treatment scale-up and HIV-related stigma in sub-saharan Africa: A longitudinal cross-country analysis. American Journal of Public Health, 105(8), 1581–1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan BT, Weiser SD, Boum Y, Haberer JE, Kembabazi A, Hunt PW, et al. (2015). Declining prevalence of probable depression among patients presenting for antiretroviral therapy in rural Uganda: The role of early treatment initiation. AIDS and Behavior, 19(1), 19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charurat ME, Emmanuel B, Akolo C, Keshinro B, Nowak RG, Kennedy S, et al. (2015). Uptake of treatment as prevention for HIV and continuum of care among HIV-positive men who have sex with men in Nigeria. Journal of Acquired Immune Deficiency Syndromes, 68(Suppl 2), S114–S123. Suppl 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudoir SR, Norton WE, Earnshaw VA, Moneyham L, Mugavero MJ, & Hiers KM (2012). Coping with HIV stigma: Do proactive coping and spiritual peace buffer the effect of stigma on depression? AIDS and Behavior, 16(8), 2382–2391. [DOI] [PubMed] [Google Scholar]
- Cichowitz C, Maraba N, Hamilton R, Charalambous S, & Hoffmann CJ (2017). Depression and alcohol use disorder at antiretroviral therapy initiation led to disengagement from care in South Africa. PLoS One, 12(12), Article e0189820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan PW, Markowitz FE, & Watson AC (2004). Structural levels of mental illness stigma and discrimination. Schizophrenia Bulletin, 30(3), 481–491. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, & Covi L (1974). The Hopkins Symptom Checklist (HSCL). A measure of primary symptom dimensions. Modern Problems of Pharmacopsychiatry, 7,79–110, 0. [DOI] [PubMed] [Google Scholar]
- Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, & Copenhaver MM (2013). HIV stigma mechanisms and well-being among PLWH: A test of the HIV stigma framework. AIDS and Behavior, 17(5), 1785–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Lacko S, Brohan E, Mojtabai R, & Thornicroft G (2012). Association between public views of mental illness and self-stigma among individuals with mental illness in 14 European countries. Psychological Medicine, 42(8), 1741–1752. [DOI] [PubMed] [Google Scholar]
- Farmer P, Leandre F,Mukherjee JS,Claude M,Nevil P,Smith-Fawzi MC,et al. (2001). Community-based approaches to HIV treatment in resource-poor settings. Lancet, 358(9279), 404–409. [DOI] [PubMed] [Google Scholar]
- Farmer P, Léandre F,Mukherjee J, Gupta R,Tarter L,&Kim JY(2001). Community-based treatment of advanced HIV disease: Introducing DOT-HAART (directly observed therapy with highly active antiretroviral therapy). Bulletin of the World Health Organization, 79(12), 1145–1151. [PMC free article] [PubMed] [Google Scholar]
- Filmer D, & Pritchett LH (2001). Estimating wealth effects without expenditure data– or tears: An application to educational enrollments in states of India. Demography, 38(1), 115–132. [DOI] [PubMed] [Google Scholar]
- Gardner LI, Marks G, Shahani L, Giordano TP, Wilson TE, Drainoni ML, et al. (2016). Assessing efficacy of a retention-in-care intervention among HIV patients with depression, anxiety, heavy alcohol consumption and illicit drug use. AIDS, 30(7), 1111–1119. [DOI] [PubMed] [Google Scholar]
- Geibel S, Gottert A, Friedland BA, Jeremiah K, McClair TL, Mallouris C, et al. (2020). Internalized stigma among people living with HIV: Assessing the internalized AIDS-related stigma scale in four countries. AIDS, 34(Suppl 1), S33–s41. [DOI] [PubMed] [Google Scholar]
- Geng EH, Bwana MB, Kabakyenga J, Muyindike W, Emenyonu NI, Musinguzi N, et al. (2010). Diminishing availability of publicly funded slots for antiretroviral initiation among HIV-infected ART-eligible patients in Uganda. PLoS One, 5(11), Article e14098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodin BR, Owens MA, White DM, Strath LJ, Gonzalez C, Rainey RL, et al. (2018). Intersectional health-related stigma in persons living with HIV and chronic pain: Implications for depressive symptoms. AIDS Care, 30(sup2), 66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haberer JE, Sabin L, Amico KR, Orrell C, Galarraga O,Tsai AC,et al. (2017). Improving antiretroviral therapy adherence in resource-limited settings at scale: A discussion of interventions and recommendations. Journal of the International AIDS Society, 20(1), 21371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesbacher PT, Rickels K, Morris RJ, Newman H, & Rosenfeld H (1980). Psychiatric illness in family practice. Journal of Clinical Psychiatry, 41(1), 6–10. [PubMed] [Google Scholar]
- Kalichman SC, Rompa D, & Cage M (2000). Reliability and validity of self-reported CD4 lymphocyte count and viral load test results in people living with HIV/AIDS. International Journal of STD & AIDS, 11(9), 579–585. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, & Ginindza T (2009). Measuring AIDS stigmas in people living with HIV/AIDS: The internalized AIDS-related stigma scale. AIDS Care, 21(1), 87–93. [DOI] [PubMed] [Google Scholar]
- Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. (2013). Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. Journal of the International AIDS Society, 16(3 Suppl 2), 18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinyanda E, Hoskins S, Nakku J, Nawaz S, & Patel V (2011). Prevalence and risk factors of major depressive disorder in HIV/AIDS as seen in semi-urban Entebbe district, Uganda. BMC Psychiatry, 11, 205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinyanda E, Levin J, Nakasujja N, Birabwa H, Nakku J, Mpango R, et al. (2018). Major depressive disorder: Longitudinal analysis of impact on clinical and behavioral outcomes in Uganda. Journal of Acquired Immune Deficiency Syndromes, 78(2), 136–143. [DOI] [PubMed] [Google Scholar]
- Lee R, Kochman A, & Sikkema K (2002). Internalized stigma among people living with HIV/AIDS. AIDS and Behavior, 6, 309–319. [Google Scholar]
- Li X, Huang L, Wang H, Fennie KP, He G, & Williams AB (2011). Stigma mediates the relationship between self-efficacy, medication adherence, and quality of life among people living with HIV/AIDS in China. AIDS Patient Care and STDs, 25(11), 665–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental Disorders: An empirical assessment. [Google Scholar]
- Logie C, & Gadalla TM (2009). Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care, 21(6), 742–753. [DOI] [PubMed] [Google Scholar]
- Logie CH, James L, Tharao W, & Loutfy MR (2011). HIV, gender, race, sexual orientation, and sex work: A qualitative study of intersectional stigma experienced by HIV-positive women in ontario, Canada. PLoS Medicine, 8(11), Article e1001124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie CH, Williams CC, Wang Y, Marcus N, Kazemi M, Cioppa L, et al. (2019). Adapting stigma mechanism frameworks to explore complex pathways between intersectional stigma and HIV-related health outcomes among women living with HIV in Canada. Social Science & Medicine, 232(1982), 129–138. [DOI] [PubMed] [Google Scholar]
- Lowther K, Selman L, Harding R, & Higginson IJ (2014). Experience of persistent psychological symptoms and perceived stigma among people with HIV on antiretroviral therapy (ART): A systematic review. International Journal of Nursing Studies, 51(8), 1171–1189. [DOI] [PubMed] [Google Scholar]
- MacLean JR, & Wetherall K (2021). The association between HIV-stigma and depressive symptoms among people living with HIV/AIDS: A systematic review of studies conducted in South Africa. Journal of Affective Disorders, 287, 125–137. [DOI] [PubMed] [Google Scholar]
- Martinez P, Tsai AC, Muzoora C, Kembabazi A, Weiser SD, Huang Y, et al. (2014). Reversal of the Kynurenine pathway of tryptophan catabolism may improve depression in ART-treated HIV-infected Ugandans. Journal of Acquired Immune Deficiency Syndromes, 65(4), 456–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakasujja N, Skolasky RL, Musisi S, Allebeck P, Robertson K, Ronald A, et al. (2010). Depression symptoms and cognitive function among individuals with advanced HIV infection initiating HAART in Uganda. BMC Psychiatry, 10,44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakimuli-Mpungu E, Musisi S, Katabira E, Nachega J, & Bass J (2011). Prevalence and factors associated with depressive disorders in an HIV+ rural patient population in southern Uganda. Journal of Affective Disorders, 135(1–3), 160–167. [DOI] [PubMed] [Google Scholar]
- Nakimuli-Mpungu E, Wamala K, Okello J, Alderman S, Odokonyero R, Mojtabai R, et al. (2015). Group support psychotherapy for depression treatment in people with HIV/AIDS in northern Uganda: A single-centre randomised controlled trial. The lancet HIV, 2(5), e190–e199. [DOI] [PubMed] [Google Scholar]
- Ogunbajo A, Iwuagwu S, Williams R, Biello KB, Kahler CW, Sandfort TGM, et al. (2020). Experiences of minority stress among gay, bisexual, and other men who have sex with men (GBMSM) in Nigeria, Africa: The intersection of mental health, substance use, and HIV sexual risk behavior. Global Public Health,1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onyebuchi-Iwudibia O, & Brown A (2014). HIV and depression in eastern Nigeria: The role of HIV-related stigma. AIDS Care, 26(5), 653–657. [DOI] [PubMed] [Google Scholar]
- Pantelic M, Casale M, Cluver L, Toska E, & Moshabela M (2020). Multiple forms of discrimination and internalized stigma compromise retention in HIV care among adolescents: Findings from a South African cohort. Journal of the International AIDS Society, 23(5), Article e25488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pantelic M, Shenderovich Y, Cluver L, & Boyes M (2015). Predictors of internalised HIV-related stigma: A systematic review of studies in sub-saharan Africa. Health Psychology Review, 9(4), 469–490. [DOI] [PubMed] [Google Scholar]
- Papworth E, Ceesay N, An L, Thiam-Niangoin M, Ky-Zerbo O, Holland C, et al. (2013). Epidemiology of HIV among female sex workers, their clients, men who have sex with men and people who inject drugs in West and Central Africa. Journal of the International AIDS Society, 16(4 Suppl 3), 18751. Suppl 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson CR, Micek MA, Pfeiffer J, Montoya P, Matediane E, Jonasse T, et al. (2009). One year after ART initiation: Psychosocial factors associated with stigma among HIV-positive Mozambicans. AIDS and Behavior, 13(6), 1189–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peltzer K, & Ramlagan S (2011). Perceived stigma among patients receiving antiretroviral therapy: A prospective study in KwaZulu-natal, South Africa. AIDS Care, 23(1), 60–68. [DOI] [PubMed] [Google Scholar]
- Pence BW, Gaynes BN, Adams JL, Thielman NM, Heine AD, Mugavero MJ, et al. (2015). The effect of antidepressant treatment on HIV and depression outcomes: Results from a randomized trial. AIDS, 29(15), 1975–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao D, Elshafei A, Nguyen M, Hatzenbuehler ML, Frey S, & Go VF (2019). A systematic review of multi-level stigma interventions: State of the science and future directions. BMC Medicine, 17(1), 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remien RH, & Mellins CA (2007). Long-term psychosocial challenges for people living with HIV: let's not forget the individual in our global response to the pandemic. AIDS, 21(Suppl 5), S55–S63. [DOI] [PubMed] [Google Scholar]
- Rueda S, Mitra S, Chen S, Gogolishvili D, Globerman J, Chambers L, et al. (2016). Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: A series of meta-analyses. BMJ open, 6(7), Article e011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, Bedoya CA, O'Cleirigh C, Biello KB, Pinkston MM, Stein MD, et al. (2016). Cognitive behavioural therapy for adherence and depression in patients with HIV: A three-arm randomised controlled trial. The lancet HIV, 3(11), e529–e538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scambler G, & Hopkins A (1986). Being epileptic: Coming to terms with stigma. Sociology of Health & Illness, 8(1), 226–243. [Google Scholar]
- Schwartz SR, Nowak RG, Orazulike I, Keshinro B, Ake J, Kennedy S, et al. (2015). The immediate eff ect of the same-sex marriage prohibition act on stigma, discrimination, and engagement on HIV prevention and treatment services in men who have sex with men in Nigeria: Analysis of prospective data from the TRUST cohort. The lancet HIV, 2(7), e299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siedner MJ, Lankowski A, Haberer JE, Kembabazi A, Emenyonu N, Tsai AC, et al. (2012). Rethinking the "pre" in pre-therapy counseling: No benefit of additional visits prior to therapy on adherence or viremia in Ugandans initiating ARVs. PLoS One, 7(6), Article e39894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, & Mqeketo A (2007). Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Social Science & Medicine, 64(9), 1823–1831, 1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ML, Kakuhikire B, Baguma C, Rasmussen JD, Bangsberg DR, & Tsai AC (2020). Do household asset wealth measurements depend on who is surveyed? Asset reporting concordance within multi-adult households in rural Uganda. J Glob Health, 10(1), Article 010412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stangl AL, Earnshaw VA, Logie CH, van Brakel W,LCS, Barre I,et al.(2019). The health stigma and discrimination framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Medicine, 17,31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stangl AL, Lloyd JK, Brady LM, Holland CE, & Baral S (2013). A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: How far have we come? Journal of the International AIDS Society, 16(3 Suppl 2), 18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada S, Weiser SD, Kumbakumba E, Muzoora C, Martin JN, Hunt PW, et al. (2014). The dynamic relationship between social support and HIV-related stigma in rural Uganda. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine, 48(1), 26–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakarar K, Asiimwe SB, Cheng DM, Forman L, Ngabirano C, Muyindike WR, et al. (2016). Alcohol consumption in Ugandan HIV-infected household-brewers versus non-brewers. AIDS and Behavior, 20(10), 2408–2417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thirumurthy H, Zivin JG, & Goldstein M (2008). The economic impact of AIDS treatment: Labor supply in western Kenya. Journal of Human Resources, 43(3), 511–552. [PMC free article] [PubMed] [Google Scholar]
- Tsai AC (2014). Reliability and validity of depression assessment among persons with HIV in sub-saharan Africa: Systematic review and meta-analysis. Journal of Acquired Immune Deficiency Syndromes, 66(5), 503–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC (2015). Socioeconomic gradients in internalized stigma among 4,314 persons with HIV in sub-Saharan Africa. AIDS and Behavior, 19(2), 270–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, Bwana M, Haberer JE, Frongillo EA, Muzoora C, et al. (2013). How does antiretroviral treatment attenuate the stigma of HIV? Evidence from a cohort study in rural Uganda. AIDS and Behavior, 17(8), 2725–2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, Frongillo EA, Hunt PW, Muzoora C, Martin JN, et al. (2012). Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Social Science & Medicine, 74(12), 2012–2019, 1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, Kegeles SM, Katz IT, Haberer JE, Muzoora C, et al. (2013). Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine, 46(3), 285–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, & Weiser SD (2013). Harnessing poverty alleviation to reduce the stigma of HIV in Sub-Saharan Africa. PLoS Medicine, 10(11), Article e1001557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Kakuhikire B, Perkins JM, Vorechovska D, Ogburn EL, Downey JM, et al. (2021). Normative vs. personal attitudes toward persons with HIV, and the mediating role of perceived HIV stigma in rural Uganda. J Glob Health (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Karasic DH, Hammer GP, Charlebois ED, Ragland K, Moss AR, et al. (2013). Directly observed antidepressant medication treatment and HIV outcomes among homeless and marginally housed HIV-positive adults: A randomized controlled trial. American Journal of Public Health, 103(2), 308–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Kiang MV, Barnett ML, Beletsky L, Keyes KM, McGinty EE, et al. (2019). Stigma as a fundamental hindrance to the United States opioid overdose crisis response. PLoS Medicine, 16(11), Article e1002969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Weiser SD, Petersen ML, Ragland K, Kushel MB, & Bangsberg DR (2010). A marginal structural model to estimate the causal effect of antidepressant medication treatment on viral suppression among homeless and marginally housed persons with HIV. Archives of General Psychiatry, 67(12), 1282–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Weiser SD, Steward WT, Mukiibi NF, Kawuma A, Kembabazi A, et al. (2013). Evidence for the reliability and validity of the internalized AIDS-related stigma scale in rural Uganda. AIDS and Behavior, 17(1), 427–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan B, Rice WS, Crockett KB, Johnson M, Neilands TB, Ross SN, et al. (2019). Longitudinal association between internalized HIV stigma and antiretroviral therapy adherence for women living with HIV: The mediating role of depression. AIDS, 33(3), 571–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ, & Ding P (2017). Sensitivity analysis in observational research: Introducing the E-value. Annals of Internal Medicine, 167(4), 268–274. [DOI] [PubMed] [Google Scholar]
- Venkataramani AS, Thirumurthy H, Haberer JE, Ii YB, Siedner MJ, Kembabazi A, et al. (2014). CD4+ cell count at antiretroviral therapy initiation and economic restoration in rural Uganda. AIDS, 28(8), 1221–1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner GJ, Ghosh-Dastidar B, Garnett J, Kityo C, & Mugyenyi P (2012). Impact of HIV antiretroviral therapy on depression and mental health among clients with HIV in Uganda. Psychosomatic Medicine, 74(9), 883–890. [DOI] [PubMed] [Google Scholar]
- Wittenberg M (2013). The weight OF success: The body mass index and economic wellbeing IN southern africa. Review of Income and Wealth, 59(Suppl 1), S62–s83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe WR, Weiser SD, Leiter K, Steward WT, Percy-de Korte F, Phaladze N, et al. (2008). The impact of universal access to antiretroviral therapy on HIV stigma in Botswana. American Journal of Public Health, 98(10), 1865–1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuniga JA, Yoo-Jeong M, Dai T, Guo Y, & Waldrop-Valverde D (2016). The role of depression in retention in care for persons living with HIV. AIDS Patient Care and STDs, 30(1), 34–38. [DOI] [PMC free article] [PubMed] [Google Scholar]