Abstract
Purpose
The Patient Dignity Question (PDQ), “What do I need to know about you as a person to give you the best care possible?” is a validated instrument designed to assess patient priorities and stressors. Administration of the PDQ has been demonstrated to improve patient-provider relationships. The PDQ has been evaluated in multiple settings, but never as a standard component of palliative care consultation. The primary objectives of this study were to determine the feasibility of PDQ screening in palliative care consultation and to characterize responses. The secondary objective was to determine patient and disease factors associated with PDQ response among patients diagnosed with cancer.
Methods
PDQ responses were collected from 2015 to 2017, and patient survival data collected through 2018. A codebook was developed to categorize responses using literature review and template analysis; coding was performed until thematic saturation was achieved. We descriptively analyzed thematic distribution among responders and performed multivariable multinomial regression to determine the association between patient characteristics and PDQ response.
Results
Response to the PDQ was documented in 2053/5002 consultations (41.1%); 1877 patient responses were included in final analysis. A total of 544 (29.5%) patients referenced illness-related concerns, 879 (46.8%) shared personal insights, and 283 (15.1%) cited interpersonal relationships. Younger patients frequently reported illness-related concerns; older respondents (age > 65) often responded with insights into their identity. Patients’ responses evaluated less than 1 year before death were more likely to focus upon identity and interpersonal relationships than illness-related concerns.
Conclusion
The PDQ can be used as a means of eliciting values among patients with cancer. Variations in response pattern suggest that approaches to distress may be tailored to age and proximity to death.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00520-022-06938-2.
Keywords: Palliative care, Goals of care, Neoplasms, Feasibility studies, Dignity, Communication
Introduction
Addressing and conserving patient dignity is a key tenet of palliative care providers’ quest to treat the psychosocial and humanistic elements of serious and life-limiting illness [1]. The dignity in care model, developed by H.M. Chochinov in the early 2000s, acknowledged the impact of illness and of interactions with the healthcare system upon end-of-life care [2, 3]. Over time, dignity conservation has expanded to include optimization of patient-provider communication, family support, symptom management, and end-of-life care. The term “dignity-conserving care” was initially intended to highlight the importance of approaching palliative care with a predominant focus on preservation of dignity [4]. As dignity in care evolved and gained traction, the Patient Dignity Question (PDQ) was designed as a means of eliciting patient priorities to be considered when delivering dignity-conserving care. This open-ended question, “What do I need to know about you as a person to give you the best care possible?” can be used by any provider type and in numerous care settings to understand patient values [5]. It has been piloted in multiple clinical settings and by multiple specialties, including in hospitalized patients, tuberculosis clinics, and outpatient palliative care, and has been well-received by patients and clinicians [1, 6, 7]. Use of the PDQ increased patient and family perceptions of person-centered care and improved provider attitudes towards patients [1, 6, 7]. More recently, investigators have sought to elucidate patterns from PDQ responses in psycho-oncology patients in an effort to better characterize core dignity constructs in this group [8]. We deployed the PDQ as a component of routine palliative care consultation in cancer patients and subsequently analyzed responses to evaluate dignity themes and their prevalence. We also measured the association between patient demographic and disease characteristics and dignity theme in a sample of patients receiving palliative care consultation at a major US cancer center.
Methods
Study design
We performed a retrospective cohort study to evaluate the role of the PDQ in routine palliative care consultation (inpatient and outpatient) at a quaternary care cancer center in the USA. Palliative care consultations, conducted primarily in inpatient settings, were ordered for a variety of indications including pain and other symptom management, patient/family support, spiritual distress, discussion of goals of care, and complex psychosocial dynamics related to serious illness. The PDQ was included as a component of a broad-ranging assessment performed by clinicians and trainees on the interprofessional and interdisciplinary palliative care service. PDQ responses were transcribed into a specific field of the palliative care consultant’s regular structured documentation and subsequently extracted from the electronic medical record. The preliminary database was reviewed by a member of the study team (RAH); all responses provided by a patient > 17 years of age were included. Responses were excluded if they were provided by a respondent other than the patient (e.g., a family member), were a duplicate of a prior response, if no response was documented, or if the respondent age was < 18. This study focused on PDQ responses between March 2015 and February 2017. Survival data was collected through March 2018 in order to capture 1-year mortality among all respondents. This study was approved by the Memorial Sloan Kettering Cancer Center Institutional Review Board.
Measures
Primary and secondary themes were derived from direct content analysis of patient responses. Themes were subsequently categorized based on the three main categories of dignity-related concerns [4]: (1) illness-related concerns, (2) dignity conserving repertoire, (3) social dignity inventory, and (4) other.
Direct content analysis, which attempts to validate and/or expand upon an existing framework, was utilized to identify primary and second dignity themes due to its flexibility in the setting of a well-established theory of dignity-preserving care and its methodologic benefit for categorization of data for quantitative analyses. Initial codebook development was iteratively performed by a palliative care physician with extensive qualitative experience (RAH), a palliative care nurse practitioner and doctoral student (WER), and an anesthesia resident (TS). Additional qualitative guidance was provided by a medical anthropologist (JC). Each investigator independently coded an initial fifty transcripts to develop a preliminary codebook. Multiple intermediate consensus meetings were conducted to discuss and arbitrate discrepancies as the group coded an additional one hundred fifty responses throughout which the codebook was refined iteratively to resolve discrepancies, remove redundant categories, and expand/elucidate new categories. Subsequent coding was performed by RAH. TS additionally coded a randomly selected set of 300 responses to verify the prior coding. All codebook revisions were applied to previously coded responses. Each response was ultimately coded into one of seven main dignity themes. Following completion of primary coding, we then evaluated our codebook within the context of existing dignity theory and categorized each pair of primary-secondary dignity themes into one of the three dignity categories [2].
Demographic and disease characteristics as well as vital status were abstracted from the electronic medical record. Those categorical variables with sample size < 10 for any response were compiled into an “other” category for model optimization. Vital status was assessed for all patients on March 15, 2018, in order to capture mortality at a minimum of 1 year following response, and time-to-death was calculated by subtracting March 15, 2018, from the date of PDQ evaluation.
Analysis
After identification of dignity theme/subtheme and assignment of dignity theme category, we performed quantitative analysis for frequency of themes in the 1877 coded patient responses. Descriptive statistics were calculated to evaluate the distribution of primary and secondary dignity theme within each of the dignity categories. ANOVA, chi-squared, and Wilcoxon rank sum tests were performed for bivariable analyses to determine the association between sample demographic characteristics (e.g., age, race, ethnicity, religion), disease characteristics (e.g., primary tumor site), vital status, time-to-death, and dignity category. Variables found to be statistically significant predictors of dignity theme in bivariable analyses were included in the multivariable multinomial logistic regression model. All statistical analysis was performed using R Statistical Software (version 4.0.5; R Foundation for Statistical Computing, Vienna, Austria).
Results
Study sample
Among 5002 unique consultations between 2015 and 2017, 2053 included documentation of the PDQ response (41.1%). A total of 176 responses provided by family members were excluded; thus, 1877 patient responses informed these analyses. The mean age of study participants was 58.4 years. Seventy percent of the population self-identified as white (1317/1877), and 92.1% (1728/1877) were not Hispanic/Latinx. Approximately 80% of respondents acknowledged a religious affiliation; almost 60% (58.5%) of the study population described themselves as Christian (1098/1877). The site of primary tumor was categorized by anatomic system: one-quarter of the cohort had primary GI malignancy (479/1877), 13.9% (261/1877) had primary breast or soft tissue cancer, 13.1% of primary tumor sites were unknown, and 12.7% of patients had hematologic malignancies. A total of 1166 (62.1%) patients were dead at follow-up in 2018 with an average time-to-death of 42 days [IQR 18, 93] (Table 1).
Table 1.
Participant characteristics
| Demographic | Category | Frequency, n (%) |
|---|---|---|
| Age (years) | 20–34 | 136 (7.2) |
| 35–44 | 174 (9.3) | |
| 45–54 | 383 (29.4) | |
| 55–64 | 517 (27.5) | |
| 65–74 | 436 (23.2) | |
| 75–84 | 173 (9.2) | |
| 85 + | 58 (3.1) | |
| Religion | Christian | 1098 (58.5) |
| Jewish | 255 (13.6) | |
| Muslim | 47 (2.5) | |
| Buddhist | 22 (1.2) | |
| Hindu | 29 (1.6) | |
| None | 329 (17.5) | |
| Other | 12 (0.6) | |
| Unknown/ declined | 85 (4.5) | |
| Type of encounter | Inpatient | 1523 (81.1) |
| Outpatient | 354 (18.8) | |
| Race | White | 1317 (70.2) |
| Black | 251 (13.4) | |
| Asian | 132 (7.0) | |
| Other | 42 (2.2) | |
| Unknown/declined | 135 (7.2) | |
| Ethnicity | Not Hispanic or Latino | 1728 (92.1) |
| Hispanic or Latino | 145 (7.7) | |
| Unknown | 4 (0.2) | |
| Site of primary tumor | Breast and soft tissue | 261 (13.9) |
| Gastrointestinal | 479 (25.5) | |
| Genitourinary | 162 (8.6) | |
| Gynecologic | 181 (9.6) | |
| Head and neck | 114 (6.1) | |
| Hematologic | 239 (12.7) | |
| Thoracic | 150 (8.0) | |
| Other | 45 (2.4) | |
| Unknown | 246 (13.1) | |
| Deceased at time of follow-up | 1166 (62.1) | |
| Time to death (days) from initial encounter | 42 [18,93] |
Directed content analysis
Qualitative analysis of individual results revealed a variety of attributes, fitting into seven primary themes: fear, physical symptoms, individual identity, coping strategies, goals pertaining to care, interpersonal interaction, and non-response/other (e.g., “I don’t know,” or “Nothing.”). These themes, in turn, aligned with the three major categories of dignity-related experiences identified in earlier work: illness-related concerns, dignity-conserving perspectives and practices, and interactions with others (Table 2) [2, 9].
Illness-related concerns: A large subgroup of respondents responded to the PDQ by expressing concerns directly related to their experience as cancer patient. Many respondents focused upon tangible, disease-related needs and issues, such as symptom burden and its impact upon quality of life. Other respondents expressed anxieties regarding aspects of illness or care, such as opioid side effects, addiction, and dependence upon caregivers. A small cohort acknowledged that their fears centered upon mortality and, particularly, the relationship between hospitalization and death.
-
The dignity-conserving repertoire (dignity-conserving perspectives and practices): Another cohort of respondents engaged with the palliative care team around aspects of their personhood, life experiences, and anticipated legacy. Participants in this category shared professional roles and hobbies as well as other central forms of identity and character traits. They overtly addressed questions of religious identity and belief systems. Some highlighted positive character traits, specifically those which they perceived as impacting care and outcome. Affirmations of personal “goodness,” positivity, and resilience were common. Some respondents in this group explicitly addressed the coping strategies they used to manage their illness, including religion, humor, and acceptance. Another group of patients appeared to struggle with their diagnosis, describing significant distress surrounding the diagnosis and its implications for their life and identity.
Other perspectives included participant motivations and goals, including returning home, experiencing time-dependent milestones, and maintaining independence. Some participants explicitly discussed goals of care, couching their wishes within an understanding of their prognosis. These respondents, while still maintaining focus on their disease, demonstrated a more longitudinal perspective and appeared to utilize the PDQ as a means of sharing insights with the medical team that might impact the direction of care.
The social dignity inventory (interactions with others): A final group of respondents highlighted relationships and their role within familial and social structures. Participants emphasized how strongly they valued their family/support system or expressed concerns regarding the impact of their illness on loved ones. We also included in this category responses from patients whose focus centered on interactions with the healthcare system. These respondents demonstrated significant insight into their interactions with the healthcare team and were able to characterize their needs and wishes based on known needs, prior experiences, and their own expectations. They expressed care needs and provider communication preferences, frequently speaking to a perceived deficit in these areas.
Table 2.
Dignity themes and subthemes identified in direct content analysis
| Dignity in care domain | Category | Subcategory | Participant response |
|---|---|---|---|
| Illness-related concerns | Fear | Uncertainty |
I’m scared and very concerned that something is wrong I have dealt with so much in my life, and I am scared about what comes next |
| Pain/symptoms |
I am just so scared of suffering, I want the pain and anxiety controlled I’m not scared of dying but I’m afraid of the pain |
||
| Medications/therapies |
Don’t give me an injection I just don’t want to get addicted to pain meds |
||
| Dependence |
I don’t want to burden my family I am concerned about losing control of my life and of being a burden |
||
| Death |
I do not want to die I don’t like to stay in the hospital too long: it makes me think about hospice and scares me I don’t want to die trapped in a web of wires |
||
| Symptoms | Pain |
I would be in so much less distress if you treat my pain. I don’t think it’s even possible to be more comfortable I would really like to have my pain controlled because I feel like I am unable to do anything Normally I can handle pain, but this is unbearable |
|
| Other symptoms | I want my constipation controlled as it is causing me discomfort | ||
| The dignity-conserving repertoire | Identity | Good person/patient |
I am a pretty easygoing person That I am a very peaceful person, not selfish Everybody tells me I’m the sweetest guy in the world. I try to be as friendly as I can |
| Fighter |
I’m a fighter, a tough cookie I’m going to fight my brains out against this cancer. I’m also patient and can take a lot |
||
| Strong |
I’m an Irish bull I’m strong. I’m doing what I have to do |
||
| Optimist |
I am an awesome person… I love life… I love my family… I am a happy and active person and would like to maintain that as long as I can I am an upbeat person, bring sunshine around me and don’t hold grudges |
||
| Other identity | I am a very creative person and I am used to “doing” and “accomplishing”—I don’t know who I am without those things | ||
| Goals | Return to normalcy/recovery of function |
I’d like to get back to my usual regimen and get back to regular life It is important that I see my son conduct the orchestra as well as make it to my planned family vacation with good pain control |
|
| Avoidance of suffering |
I am happy for the time I have been given. I want to make sure my symptoms are as well controlled as possible though the end of my life. I want to die at home I just want to be comfortable. I’m a young guy, I may not look like it but I used to be really strong and now I’m just so weak |
||
| Quality of life |
I want as much quality of life as possible I want to preserve my quality of life for as long as I can |
||
| Independence |
I am learning to ask for help, but I am really a very independent person I am used to being independent. I want to regain control and be able to be comfortable for some period of the day in which I can plan activities that are important to me. I would like to go back to work |
||
| Home | I just want to go back home | ||
| Disease-directed therapy |
I have to have chemotherapy because I have two young children at home I just want to proceed with treatment Well, I’m pretty cut and dry. I want to live, I want more treatment |
||
| Survival/recovery |
I want to live That I am a person who wants to live That I wanna [sic] live. I wanna live life, go back to work, spend time with my family |
||
| Coping strategies | Religion/faith |
I have a very strong faith and know this is in God’s hands. All of this is happening for a purpose I am at peace because my soul is right with God I have a lot of faith, hope, and I want to be a fighter. I believe if I’m of positive mind, irregardless [sic] of what is there, try to think of a higher power |
|
| Humor |
I’ve been through a lot. But I still have a great sense of humor I tend to minimize my symptoms. I also use humor to help me cope |
||
| Acceptance |
I understand that I won’t survive this lymphoma I have had a good life, have grown up children and grandkids, I am in peace with dying |
||
| Distress |
I was a very functional person who was very active and enjoyed doing many things now I am having a hard time even picking up a tissue So much has happened in the past year… it’s been too much. I feel like my life is falling apart I want to get better. I’ve always been so compassionate to people and so kind to people. How could this happen to me? |
||
| Fatigue |
Let me die. I’m so tired of fighting this illness. I am so tired of suffering and pain. I’ve dealt with this illness for 20 years and before that, I worked 15 h a day to support my parents and disabled brother. I am so tired I want this to be done so that my family can move on |
||
| Social dignity inventory | Family/community |
I’m a grandma and need to get back to my life so I can be with my grandchildren My family is the most important thing; [My] sons and grandchildren are everything to [me] I have an 8-year-old son. I’m in so much pain, I can’t even help him with his homework My family makes sure I have no tension. My wife is also very cooperative. I try my best. I have 3 daughters who all act as my nurses and care for me much. I am here because of them |
|
| Care-related | Care needs | I need more help at home. I shouldn’t have to do this by myself and my family shouldn’t have to worry about me so much | |
| Communication preferences |
I am very matter of fact. I like plans and I like to be informed of my medical treatment plan and any changes taking place I’m easy going but I’ll ask a lot of questions. I want to be informed. Sometimes I check Google too much, but I make sure to verify what I know with my doctors I like honest and straight forward information, even if it’s bad |
||
| Non-response/other | Nothing | Nothing | |
| Uncertainty |
I don’t know I’m not sure, I just don’t like being in pain I don’t know. I would like to get my biopsy and get started on treatment |
A small subgroup of patients appeared to be unable to answer the PDQ. Some simply responded, “Nothing;” others “didn’t know” how or what to respond. A few expanded upon their refusal to respond by pointing out untreated symptoms, usually pain, or by implying that the question was delaying delivery of more important answers and next steps,
Quantitative analysis
A total of 879 (46.8%) participants shared a perspective related to identity, coping or goals, 554 (29.5%) responded with illness-related concerns, and 15.1% (n = 283) described interpersonal relationships as the primary dignity-preserving attribute; 161 (8.6%) participants expressed a response categorized as “other” (Table 3).
Table 3.
Distribution of dignity category, main theme, and subtheme among patient-respondents (n = 1877)
| Dignity category | n (%) | Main theme | n (%) | Subtheme | n (%) |
|---|---|---|---|---|---|
| Illness-related concerns | 554 (29.5) | Fears | 86 (4.6) | Death | 11 |
| Dependence | 11 | ||||
| Medications/therapies | 35 | ||||
| Pain/symptoms | 19 | ||||
| Uncertainty | 5 | ||||
| Other | 5 | ||||
| Other | 468 (24.9) | Dyspnea | 3 | ||
| Pain | 413 | ||||
| Other | 52 | ||||
| Dignity conserving repertoire | 879 (46.8) | Coping strategies | 99 (5.3) | Acceptance | 31 |
| Existential distress | 24 | ||||
| Fatigue | 1 | ||||
| Humor | 9 | ||||
| Psychological fatigue | 4 | ||||
| Religion/faith | 28 | ||||
| Other | 2 | ||||
| Goals | 343 (18.3) | Autonomy/independence | 4 | ||
| Comfort/avoid suffering | 56 | ||||
| Disease directed therapy | 22 | ||||
| Home | 66 | ||||
| Quality of life | 15 | ||||
| Return to normalcy | 131 | ||||
| Survival | 46 | ||||
| Other | 3 | ||||
| Not assessed | 0 | ||||
| Identity | 437 (23.3) | Fighter | 63 | ||
| Independent | 36 | ||||
| Nice person | 55 | ||||
| Optimist | 45 | ||||
| Strong | 29 | ||||
| Other | 209 | ||||
| Social dignity inventory | 283 (15.1) | Interpersonal interaction | 283 (15.1) | Care needs | 75 |
| Communication preferences | 83 | ||||
| Family/community | 125 | ||||
| Other | 161 (8.6) | Other | 161 (8.6) | I don’t know | 90 |
| Not sure how-to code | 37 | ||||
| Nothing | 32 | ||||
| Other | 2 | ||||
| Total | 1877 (100.0) | 1877 (100.0) | 1877 |
Age and time-to-death were statistically significantly associated with dignity category in bivariable analysis (Table 4). Illness-related concerns, particularly those related to symptoms and their management, were more common in younger patients, whereas older respondents, particularly those greater than 70 years of age, were more likely to communicate dignity-conserving perspectives and practices in their responses to the PDQ. Although race, ethnicity, religion, and site of primary tumor were not statistically associated with dignity category, religion was statistically significantly associated with primary dignity theme. In this sub-analysis, response category was most similar across the Abrahamic religions. Of participants, 40.9% (9/22) who identified as Buddhist responded to the PDQ with identity-based responses; almost 45% (13/29) of Hindus emphasized interpersonal relations as their primary dignity theme.
Table 4.
Sample characteristics and bivariable statistics by dignity category for patient-respondents (n = 1877)
| All | Illness-related concerns n (%) |
Dignity conserving repertoire n (%) |
Social dignity inventory n (%) |
Other n (%) |
p | |
|---|---|---|---|---|---|---|
| Age (years) | 58.4 (14.7) | 56.6 (14.8) | 60.0 (14.2) | 57.3 (14.3) | 58.0 (16.1) | < 0.001 |
| Age range (decade) | ||||||
| 20–34 | 136 (7.2) | 49 (36.0) | 50 (36.8) | 21 (15.4) | 16 (11.8) | 0.011 |
| 35–44 | 174 (9.3) | 61 (35.1) | 68 (39.1) | 29 (16.7) | 16 (9.2) | |
| 45–54 | 383 (20.4) | 122 (31.9) | 165 (43.1) | 68 (17.8) | 28 (7.3) | |
| 55–64 | 517 (27.5) | 155 (30.0) | 244 (47.2) | 75 (14.5) | 43 (8.3) | |
| 65–74 | 436 (23.2) | 112 (25.7) | 228 (52.3) | 60 (13.8) | 36 (8.3) | |
| 75–84 | 173 (9.2) | 40 (23.1) | 95 (54.9) | 26 (15.0) | 12 (6.9) | |
| 85 + | 58 (3.1) | 15 (25.9) | 29 (50.0) | 4 (6.9) | 10 (17.2) | |
| Race | ||||||
| White | 1317 (70.2) | 396 (30.1) | 610 (46.3) | 202 (15.3) | 109 (8.3) | 0.354 |
| Black | 251 (13.4) | 83 (33.1) | 116 (46.2) | 34 (13.5) | 18 (7.2) | |
| Asian | 132 (7.0) | 30 (22.7) | 67 (50.8) | 21 (15.9) | 14 (10.6) | |
| Other | 42 (2.2) | 16 (38.1) | 17 (40.5) | 6 (14.3) | 3 (7.1) | |
| Unknown/refused | 135 (7.2) | 29 (21.5) | 69 (51.1) | 20 (14.8) | 17 (12.6) | |
| Ethnicity | ||||||
| Not Hispanic or Latino | 1728 (92.1) | 507 (29.3) | 809 (46.8) | 265 (15.3) | 147 (8.5) | 0.706 |
| Hispanic or Latino | 145 (7.7) | 45 (31.0) | 69 (47.6) | 18 (12.4) | 13 (9.0) | |
| Unknown | 4 (0.2) | 2 (50.0) | 1 (25.0) | 0 (0.0) | 1 (25.0) | |
| Religion | ||||||
| Christian | 1098 (58.5) | 324 (29.5) | 521 (47.4) | 163 (14.8) | 90 (8.2) | 0.099 |
| Jewish | 255 (13.6) | 83 (32.5) | 113 (44.3) | 36 (14.1) | 23 (9.0) | |
| Muslim | 47 (2.5) | 15 (31.5) | 19 (40.4) | 6 (12.8) | 7 (14.9) | |
| Buddhist | 22 (1.2) | 7 (31.8) | 12 (54.5) | 2 (9.1) | 1 (4.5) | |
| Hindu | 29 (1.6) | 5 (17.2) | 10 (34.5) | 13 (44.8) | 1 (3.4) | |
| None | 329 (17.5) | 91 (27.7) | 156 (47.4) | 53 (16.1) | 29 (8.8) | |
| Other | 12 (0.6) | 4 (33.3) | 5 (41.7) | 1 (8.3) | 2 (16.7) | |
| Unknown/refused | 85 (4.5) | 25 (29.4) | 43 (50.6) | 9 (10.6) | 8 (9.4) | |
| Site of primary tumor | ||||||
| Breast and soft tissue | 261 (13.9) | 80 (30.7) | 118 (45.2) | 41 (15.7) | 22 (8.4) | 0.222 |
| Gastrointestinal | 479 (25.5) | 123 (25.7) | 227 (47.4) | 82 (17.1) | 47 (9.8) | |
| Genitourinary | 162 (8.6) | 41 (25.3) | 84 (51.9) | 20 (12.3) | 17 (10.5) | |
| Gynecologic | 181 (9.6) | 68 (37.6) | 80 (44.2) | 22 (12.2) | 11 (6.1) | |
| Head and neck | 114 (6.1) | 40 (35.1) | 48 (42.1) | 15 (13.2) | 11 (9.6) | |
| Hematologic | 239 (12.7) | 79 (33.1) | 116 (48.5) | 34 (14.2) | 10 (4.2) | |
| Respiratory/thoracic | 150 (8.0) | 49 (32.7) | 61 (40.7) | 25 (16.7) | 15 (10.0) | |
| Other | 45 (2.4) | 13 (28.9) | 21 (46.7) | 7 (15.6) | 4 (8.9) | |
| Unknown | 246 (13.1) | 61 (24.8) | 124 (50.4) | 37 (15.0) | 24 (9.8) | |
| Deceased | 1166 (62.1) | 320 (27.4) | 558 (47.9) | 184 (15.8) | 104 (8.9) | 0.086 |
| Time to death (days) | 42 [18, 93] | 49 [24, 110] | 37 [16, 98] | 39 [18,82] | 42 [14, 81] | 0.023 |
| Total | 1877 (100) | 554 (29.5) | 879 (46.8) | 283 (15.1) | 161 (8.6) | |
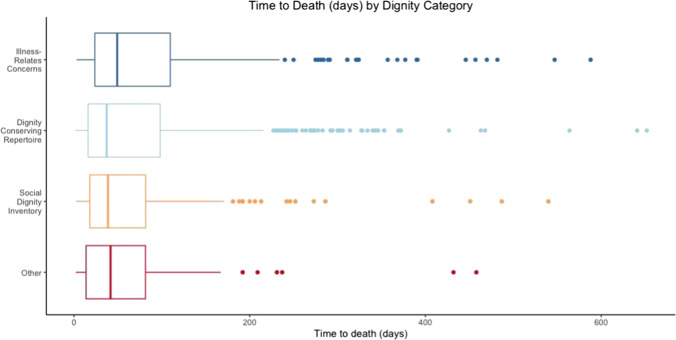
Multivariable multinomial logistic regression was performed to evaluate the independent association between variables significant in bivariable analysis (age and time-to-death) and dignity theme (Table 5). Age remained statistically significant; these data revealed a higher odds of reporting dignity conserving perspectives and practices than illness-related concerns with each progressive age cohort. Patients closer to death were more likely to generate a dignity conserving response than patients farther from death, both independently and in association with age (Fig. 1).
Table 5.
Median [interquartile range, IQR] time to death by participant characteristics (n = 1877)
| All n (%) |
Time to death (d) n [IQR] |
p | |
|---|---|---|---|
| Age | |||
| 20–34 | 136 (7.2) | 71 [27, 181] | 0.005 |
| 35–44 | 174 (9.3) | 57 [19, 114 | |
| 45–54 | 383 (20.4) | 41 [20, 103] | |
| 55–64 | 517 (27.5) | 38 [18, 92] | |
| 65–74 | 436 (23.2) | 42 [16, 79 | |
| 75–84 | 173 (9.2) | 36 [17, 81] | |
| 85 + | 58 (3.1) | 33 [14, 96] | |
| Race | |||
| White | 1317 (70.2) | 40 [17, 90] | 0.024 |
| Black | 251 (13.4) | 45 [18, 92] | |
| Asian | 132 (7.0) | 37 [15, 91] | |
| Other | 42 (2.2) | 34 [12, 76] | |
| Unknown/refused | 135 (7.2) | 70 [23, 180] | |
| Ethnicity | |||
| Not Hispanic or Latinx | 1728 (92.1) | 41 [18, 92] | 0.309 |
| Hispanic or Latinx | 145 (7.7) | 51 [19, 133] | |
| Unknown | 4 (0.2) | - | |
| Religion | |||
| Christian | 1098 (58.5) | 47 [19, 104] | 0.063 |
| Jewish | 255 (13.6) | 38 [16, 87] | |
| Muslim | 47 (2.5) | 49 [29, 72] | |
| Buddhist | 22 (1.2) | 38 [15, 57] | |
| Hindu | 29 (1.6) | 55 [25, 184] | |
| None | 329 (17.5) | 33 [16, 75] | |
| Other | 12 (0.6) | 21 [18, 49] | |
| Unknown/refused | 85 (4.5) | 28 [14, 62] | |
| Site of primary tumor | |||
| Breast and soft tissue | 261 (13.9) | 33 [15, 66] | 0.027 |
| Gastrointestinal | 479 (25.5) | 37 [16, 91] | |
| Genitourinary | 162 (8.6) | 50 [21, 91] | |
| Gynecologic | 181 (9.6) | 43 [19, 87] | |
| Head and neck | 114 (6.1) | 46 [23, 124] | |
| Hematologic | 239 (12.7) | 55 [24, 119] | |
| Respiratory/thoracic | 150 (8.0) | 38 [17, 106] | |
| Other | 45 (2.4) | 51 [24, 126] | |
| Unknown | 246 (13.1) | 48 [17, 104] | |
| Dignity category | |||
| Illness-related concerns | 554 (29.5) | 49 [24, 110] | 0.023 |
| Dignity conserving repertoire | 879 (46.8) | 37 [16, 98] | |
| Social dignity inventory | 283 (15.1) | 39 [18. 82] | |
| Other | 161 (8.6) | 42 [14, 81] | |
| Main dignity theme | |||
| Fears (illness-related concerns) | 86 (4.6) | 46 [28, 87] | 0.033 |
| Symptoms (illness-related concerns) | 468 (24.9) | 53 [23, 110] | |
| Coping (dignity conserving repertoire) | 99 (5.2) | 33 [15, 60] | |
| Goals (dignity conserving repertoire) | 343 (18.3) | 35 [15. 92] | |
| Identity (dignity conserving repertoire) | 437 (23.3) | 42 [16, 106] | |
| Interpersonal interactions (social dignity inventory) | 283 (15.1) | 39 [18, 82] | |
| Other | 161 (8.6) | 42 [14, 81] | |
| Total | 1877 (100) | ||
Fig. 1.
Time to death (days) by dignity category
Discussion
Our results suggest that the PDQ can be leveraged as a component of palliative care assessment in patients undergoing treatment for malignancy and that responses can be used to individualize care. Although prior studies have demonstrated that the PDQ can be utilized as a routine component of care with positive impact on patient and provider-perceived relations [1, 7], this is among the first and, to our knowledge, the largest-scale study to analyze and interpret responses within the complexities of patient- and personhood. We identified several remarkable findings in our analysis of patient responses. Adoption of dignity-conserving practice such as identity work correlated with age: younger patients focused on dignity-threatening experiences, particularly symptoms, whereas older respondents detailed coping mechanisms, goals and personal characteristics. This focus on identity and personhood also applied to patients nearing death across all age ranges, implying that impending death, whether known to the patient or not, may shift attention away from illness-related concerns and redirect it towards legacy-building and interpersonal relationships. This latter finding, in turn, begs the question of how we can better focus end-of-life interventions to address existential needs concurrently with physical ones.
Many individuals experience a cancer diagnosis as profoundly disruptive to preconceived notions of identity, requiring ongoing renegotiation of their self-image, body image, professional identity, and relationships [10–12]. Our findings suggest that the PDQ elicits this identity-specific renegotiation in many, particularly older, patients, and opens an avenue to share this critical shift with the medical team. Although it is not inconceivable that some of this age-related variation in response may be due to differing symptom burdens between age groups [13, 14], it is unlikely that higher symptom burdens in younger patients fully account for our findings. Other research has indicated that older patients demonstrate increased resiliency and lower emotional distress in the face of cancer diagnosis and therapy [15, 16]. Our results suggest that engagement in dignity-conserving practices may contribute to this resilience. The association between age and dignity-conserving practice is unique; similarities we noted across other demographic variables studied suggest that, when faced with serious illness, patients may demonstrate similar values and priorities across racial, ethnic, and religious groups, reinforcing research demonstrating that priorities in care of patients with serious illness should be explored within the context of each patient’s individual narrative [17].
In 2002, Chochinov and colleagues presented a conceptualization of patient dignity derived from open-ended interviews with patients. They highlighted three overarching themes: illness-related concerns, the dignity conserving repertoire, and the social dignity inventory, each with subthemes inviting further examination and, potentially, treatment [2]. Our narrower themes nest well within these broader categories, which in turn can be used to offer potential therapeutic interventions to some of the issues brought up in response to the Patient Dignity Question. The consistency in themes brought up by respondents and their more general alignment with the domains of dignity in care [5] suggest that routine interpretation of responses to the PDQ may have significant value with regards to provision of optimal patient-centered care. Previous studies of PDQ responses from psycho-oncology and hospice patients have identified themes such as personality traits and history, disease-related concerns and goals, spirituality, and familial relationships [8, 18] which are congruent with the seven major themes (fear, physical symptoms, individual identity, goals pertaining to care, coping strategies, and family/community) we identified in our analysis. This similarity of themes suggests that patient concerns and priorities align across multiple facets of the oncology care spectrum and that elicitation of these responses represents a viable means of identifying and acknowledging patient goals and priorities. Our findings support the use of the PDQ as a single-question palliative care assessment, performable by any member of the care team, with responses elucidating patient priorities and preoccupations in a way that may be immediately intervenable or may generate further patient-provider exploration.
Engagement with patient stories has significant impact on both patients and providers [19]. Patient narratives have been used to generate understanding, cement relationships with providers, and draw attention to the experience of patienthood [20]. Analysis of narrative texts in cancer patients has yielded robust insights into the realities of a cancer diagnosis, of an unwanted and painful physiologic process leading to forced embodiment of “sickness” [21]. Our findings, coupled with other work examining this patient experience, provides a route towards building deeper, more existentially supportive, relationships with cancer patients. Routine use of the PDQ in patient interactions provides the clinician with an open-ended mechanism to identify patient priorities and build rapport. Normalization of dignity assessment alongside other components of history and physical exam, coupled with a willingness to use responses to provide targeted treatment (e.g., more effective symptom management strategies, acknowledgement of individual characteristics beyond diagnosis and therapeutic goals), may provide the clinician a toolkit to facilitate dignity-supporting care and to build more overtly empathic relationships with patients [22].
In their responses, many participants highlighted positive character attributes that would further ingratiate them to the medical team as a “good patient,” i.e., one compliant with societal, familial, and medical team norms and dictates [23, 24]. These findings offer two potential explanations: as patients are forced to reassess their lives in the context of malignancy, often late-stage, this self-evaluation as a “good person” and patient is a demonstration of ongoing reevaluation of legacy, identity, and value in the context of their cancer experience. Alternatively, in the context of being asked the PDQ, the patient feels obligated to give a “correct” response highlighting compliance and worthiness of treatment. Other work has demonstrated that reinforcement of “good patient” behaviors adversely impacted quality of death by shifting focus away from the patient’s needs and towards the priorities of the infrastructure surrounding them [23]. Viewed within this context, our findings suggest that the PDQ might best be used as part of a broader approach to identifying priorities in patients with life-limiting illness.
Several limitations may impact the generalizability of this study. Respondents were drawn from a single large academic quaternary care medical center and were exclusively being treated for cancer, primarily in the inpatient setting. The study population predominantly identified as white and non-Hispanic; further investigation with more heterogenous populations may be warranted. Furthermore, although the study population is characterized in terms of self-reported race, ethnicity, age, and religion, our team was unable to provide information on sexual orientation or gender identity due to inconsistent or unavailable data. Sexual and gender minority groups may warrant more targeted investigation related to dignity conservation in the face of bias, fear of mistreatment, and disenfranchised relationships and grief, among other discriminatory factors and experiences [25–29]. While directed content analysis permitted rapid thematic saturation, it is possible that categories of concerns and priorities experienced by patients in other care settings were missed in our analysis. We did not perform formal member checking, although interrater reliability was assessed at multiple intervals. In addition, limited information is available about the approximately 2500 patients who underwent palliative care consultation but did not respond to the PDQ during this same time period, thus contributing to a potential selection bias in our results. We suspect that the majority may not have been asked the PDQ due to patient mental status, disease acuity, urgency of attention to immediate health issues, time or provider discomfort; however, we are unable to compare these groups to determine whether these characteristics may have influenced participation. Similarly, there is little understanding about the category of patients who followed the PDQ with “other” responses, such as a focus on symptomatic complaints or “not knowing” how to answer. Finally, the PDQ was asked by providers with a variety of training levels, backgrounds, and degrees of comfort with using this tool. Patient-centered verbal and non-verbal techniques, such as active listening, therapeutic presence, and empathic communication competencies, are also considered foundational to how the question is delivered and the ways patients and families experience the provider [22, 30]. Given the sheer volume of responses, we do not anticipate that any single questioner would have unduly influenced response; however, the extent to which questioner characteristics might have altered responses is unclear. Additional exploration will be needed to better understand how to ensure holistic psychosocial support for these patients and foster the care environments needed to elicit the full existential narrative.
Conclusions
The PDQ provides an easily adopted means of ascertaining priorities and goals among cancer patients that can readily be employed by various provider types to further person-centered care. Responses shed light on shifts in priorities with age and proximity to death. Further work is needed to ascertain the effectiveness of using the PDQ as a trigger for needed interventions in communication and care and to strengthen the evidence base around dignity conserving care, particularly for underserved groups and throughout the systemic constraints associated with the COVID-19 crisis.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to recognize the contributions of Toby Steinberg, MD, who assisted with codebook development and data coding, as well as Justin Clapp, PhD, MPH, who provided methodological guidance. We would also like to recognize the patients and families whose responses were included in this study—without their contributions, this work would not exist.
Author contribution
Dr. Hadler and Dr. Nelson conceptualized this project. Drs. Hadler, Rosa, and Goldshore contributed to data analysis. Drs. Hadler and Goldshore both contributed to original manuscript development; they, as well as Drs. Rosa and Nelson, participated in review and editing of the finalized manuscript.
Funding
Drs. Rosa and Nelson received the NIH/NCI Cancer Center Support Grant P30 CA008748. Dr. Rosa is also supported by the NCI award number T32 CA009461. No other authors have anything to disclose.
Data availability
Data available on request.
Code availability
Not applicable.
Declarations
Ethics approval
This study was approved by the Memorial Sloan Kettering Institutional Review Board.
Consent to participate
A waiver of informed consent was approved by the Memorial Sloan Kettering Institutional Review Board.
Consent for publication
Not applicable.
Competing interests
Not applicable.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
R. A. Hadler, Email: Rachel-hadler@uiowa.edu
M. Goldshore, Email: Matthew.goldshore@pennmedicine.upenn.edu
W. E. Rosa, Email: Rosaw@mskcc.org
J. Nelson, Email: Nelsonj@mskcc.org
References
- 1.Chochinov HM, McClement S, Hack T, Thompson G, Dufault B, Harlos M. Eliciting personhood within clinical practice: effects on patients, families, and health care providers. J Pain Symptom Manage. 2015;49(6):974–80.e2. doi: 10.1016/j.jpainsymman.2014.11.291. [DOI] [PubMed] [Google Scholar]
- 2.Chochinov HM, Hack T, McClement S, Kristjanson L, Harlos M. Dignity in the terminally ill: a developing empirical model. Soc Sci Med. 2002;54(3):433–443. doi: 10.1016/S0277-9536(01)00084-3. [DOI] [PubMed] [Google Scholar]
- 3.Dignity in care: the model in detail. Dignity in Care. https://www.dignityincare.ca/en/the-model-in-detail.html (2016). Accessed February 22 2022.
- 4.Chochinov HM. Dignity-conserving care–a new model for palliative care: helping the patient feel valued. JAMA. 2002;287(17):2253–2260. doi: 10.1001/jama.287.17.2253. [DOI] [PubMed] [Google Scholar]
- 5.Chochinov HM. Dignity and the essence of medicine: the A, B, C, and D of dignity conserving care. BMJ (Clinical research ed) 2007;335(7612):184–187. doi: 10.1136/bmj.39244.650926.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lopez C, Bertram-Farough A, Heywood D, Dawson L, Dillon M, Chochinov HM, et al. Knowing about you: eliciting dimensions of personhood within tuberculosis care. Int J Tuberc Lung Dis. 2017;21(2):149–153. doi: 10.5588/ijtld.16.0630. [DOI] [PubMed] [Google Scholar]
- 7.Johnston B, Pringle J, Gaffney M, Narayanasamy M, McGuire M, Buchanan D. The dignified approach to care: a pilot study using the patient dignity question as an intervention to enhance dignity and person-centred care for people with palliative care needs in the acute hospital setting. BMC Palliat Care. 2015;14:9. doi: 10.1186/s12904-015-0013-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meier EA, Naqvi JB, Xiao J, Montross LP. Conversations regarding personhood: use of the patient dignity question in an outpatient psycho-oncology clinic. J Palliat Med. 2019;22(12):1574–1577. doi: 10.1089/jpm.2018.0256. [DOI] [PubMed] [Google Scholar]
- 9.Arantzamendi M, Belar A, Martinez M. Promoting patient-centred palliative care: a scoping review of the patient dignity question. Curr Opin Support Palliat Care. 2016;10(4):324–329. doi: 10.1097/spc.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 10.Mathieson CM, Stam HJ. Reneotiating identity: cancer narratives. Sociol Health Illn. 1995;17(3):283–306. doi: 10.1111/1467-9566.ep10933316. [DOI] [Google Scholar]
- 11.Van Der Molen B (2000). Relating information needs to the cancer experience. 2. Themes from six cancer narratives*. Eur J Cancer Care. 9(1):48–54. 10.1046/j.1365-2354.2000.00190.x. [DOI] [PubMed]
- 12.Rosenblatt L. Being the monster: women’s narratives of body and self after treatment for breast cancer. Med Humanit. 2006;32(1):53. doi: 10.1136/jmh.2004.000212. [DOI] [PubMed] [Google Scholar]
- 13.Walsh D, Donnelly S, Rybicki L. The symptoms of advanced cancer: relationship to age, gender, and performance status in 1,000 patients. Support Care Cancer. 2000;8(3):175–179. doi: 10.1007/s005200050281. [DOI] [PubMed] [Google Scholar]
- 14.McMillan SC. The relationship between age and intensity of cancer-related symptoms. Oncol Nurs Forum. 1989;16(2):237–241. [PubMed] [Google Scholar]
- 15.Cohen M, Baziliansky S, Beny A. The association of resilience and age in individuals with colorectal cancer: an exploratory cross-sectional study. J Geriatr Oncol. 2014;5(1):33–39. doi: 10.1016/j.jgo.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 16.Gagliese L, Jovellanos M, Zimmermann C, Shobbrook C, Warr D, Rodin G. Age-related patterns in adaptation to cancer pain: a mixed-method study. Pain Med. 2009;10(6):1050–1061. doi: 10.1111/j.1526-4637.2009.00649.x. [DOI] [PubMed] [Google Scholar]
- 17.Volandes AE, Paasche-Orlow M, Gillick MR, Cook EF, Shaykevich S, Abbo ED, et al. Health literacy not race predicts end-of-life care preferences. J Palliat Med. 2008;11(5):754–762. doi: 10.1089/jpm.2007.0224. [DOI] [PubMed] [Google Scholar]
- 18.McDermott P. Patient Dignity Question. Feasible, dignity-conserving intervention in a rural hospice. Can Fam Physician 2019;65(11):812–9. [PMC free article] [PubMed]
- 19.Kalitzkus V, Matthiessen PF. Narrative-based medicine: potential, pitfalls, and practice. Perm J. 2009;13(1):80–86. doi: 10.7812/tpp/08-043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Charon R. What to do with stories. Can Fam Physician. 2007;53(8):1265. [PMC free article] [PubMed] [Google Scholar]
- 21.Skott C (2002) Expressive metaphors in cancer narratives. Cancer Nurs. 25(3). [DOI] [PubMed]
- 22.Sanders JJ, Dubey M, Hall JA, Catzen HZ, Blanch-Hartigan D, Schwartz R (2021). What is empathy? Oncology patient perspectives on empathic clinician behaviors. Cancer. 10.1002/cncr.33834 [DOI] [PubMed]
- 23.Proulx K, Jacelon C. Dying with dignity: the good patient versus the good death. Am J Hosp Palliat Med. 2004;21(2):116–20. doi: 10.1177/104990910402100209. [DOI] [PubMed] [Google Scholar]
- 24.Jadad AR, Rizo CA, Enkin MW. I am a good patient, believe it or not. BMJ. 2003;326(7402):1293–1295. doi: 10.1136/bmj.326.7402.1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harding R, Epiphaniou E, Chidgey-Clark J. Needs, experiences, and preferences of sexual minorities for end-of-life care and palliative care: a systematic review. J Palliat Med. 2012;15(5):602–611. doi: 10.1089/jpm.2011.0279. [DOI] [PubMed] [Google Scholar]
- 26.Bristowe K, Marshall S, Harding R. The bereavement experiences of lesbian, gay, bisexual and/or trans* people who have lost a partner: a systematic review, thematic synthesis and modelling of the literature. Palliat Med. 2016;30(8):730–744. doi: 10.1177/0269216316634601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stein GL, Berkman C, O’Mahony S, Godfrey D, Javier NM, Maingi S. Experiences of lesbian, gay, bisexual, and transgender patients and families in hospice and palliative care: perspectives of the palliative care team. J Palliat Med. 2020;23(6):817–824. doi: 10.1089/jpm.2019.0542. [DOI] [PubMed] [Google Scholar]
- 28.Bristowe K, Hodson M, Wee B, Almack K, Johnson K, Daveson BA, et al. Recommendations to reduce inequalities for LGBT people facing advanced illness: ACCESSCare national qualitative interview study. Palliat Med. 2018;32(1):23–35. doi: 10.1177/0269216317705102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haviland K, Burrows Walters C, Newman S. Barriers to palliative care in sexual and gender minority patients with cancer: a scoping review of the literature. Health Soc Care Community. 2021;29(2):305–318. doi: 10.1111/hsc.13126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schwartz R, Dubey M, Blanch-Hartigan D, Sanders JJ, Hall JA. Physician empathy according to physicians: a multi-specialty qualitative analysis. Patient Educ Couns. 2021 doi: 10.1016/j.pec.2021.07.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available on request.
Not applicable.