Since the COVID-19 pandemic began over 2 years ago, its global impact has been enormous. Our growing understanding of the pathophysiology of this disease has particular links to hematology. Introduced by Ortel and Berliner, this Review Series provides up-to-date overviews of the many areas in which COVID-19 has implications for hematology practice.
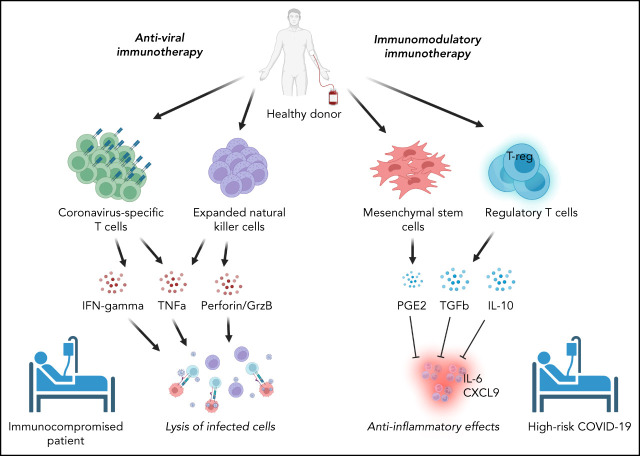
Visual Abstract
Abstract
Patients with blood disorders who are immune suppressed are at increased risk for infection with severe acute respiratory syndrome coronavirus 2. Sequelae of infection can include severe respiratory disease and/or prolonged duration of viral shedding. Cellular therapies may protect these vulnerable patients by providing antiviral cellular immunity and/or immune modulation. In this recent review of the field, phase 1/2 trials evaluating adoptive cellular therapies with virus-specific T cells or natural killer cells are described along with trials evaluating the safety, feasibility, and preliminary efficacy of immune modulating cellular therapies including regulatory T cells and mesenchymal stromal cells. In addition, the immunologic basis for these therapies is discussed.
Introduction
Despite the development of highly efficacious vaccines, the COVID-19 pandemic continues to take a massive toll on populations internationally. Multiple studies have demonstrated elevated hospitalization and mortality rates in immunocompromised patients, including those with inborn errors of immunity, cancer, hematopoietic stem cell transplantation (HSCT), or solid organ transplantation.1-4 Registry reports have indicated that mortality rates in immunocompromised patients requiring hospitalization for severe COVID-19 are as high as 20% despite currently available therapies. Although some individuals with underlying immunodeficiency who become infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) will achieve effective viral clearance,5,6 multiple reports have demonstrated a risk of prolonged shedding of viable virus with intrahost accrual of novel viral variants over time.7-11 Studies of immunocompromised populations have shown suboptimal responses to vaccination,12-17 and although booster vaccines in these populations is required, it is unclear how durable their protective immunity will be compared with immune-competent individuals. Disease severity and the potential for new variants highlight the need for new preventative and therapeutic approaches to protect immunocompromised populations from COVID-19. Adoptive cellular therapy has been used in prior studies to prevent or treat viral infections in the setting of inborn errors of immunity or transplantation, with evidence of safety and efficacy against herpesviruses, polyomaviruses, and some respiratory pathogens such as adenovirus.18-23 Accordingly, adoptive T-cell therapy is being explored as a preventative or therapeutic adjunctive therapy against SARS-CoV-2.
Among adults infected with SARS-CoV-2, severe disease is accompanied by characteristic immunologic profiles, including markedly elevated plasma levels of inflammatory cytokines. Several studies have demonstrated patterns of cytokine elevation, including interleukin 6 (IL-6) and IL-10, which correlate with risk of mortality.24-26 Treatment with dexamethasone among patients requiring respiratory support improves outcomes,27 suggesting that anti-inflammatory agents may be beneficial in some patients with COVID-19. Trials of immunosuppressive agents including tocilizumab,28 Janus kinase inhibitors, and Bruton’s tyrosine kinase inhibitors have yielded mixed results.29-33 In this context, regulatory T cells (Tregs) and mesenchymal stromal cells may be beneficial adjunctive treatments with immune modulatory and tissue reparative properties that could improve outcomes among patients with severe COVID-19.
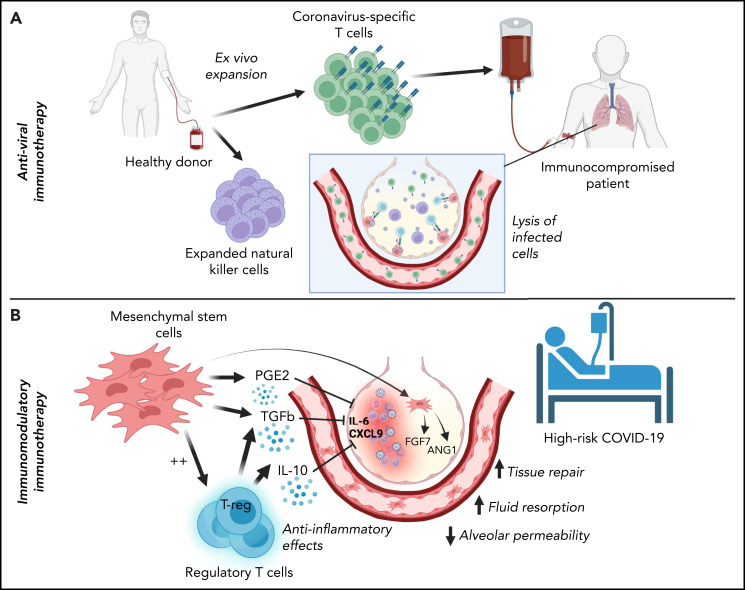
Cellular therapies for SARS-CoV-2 can be conceptually classified based on their intended function as either (1) adoptive immunotherapies designed to enhance viral clearance in patients with ineffective immune responses to SARS-CoV-2 or (2) immune modulatory therapies to correct a dysregulated immune response contributing to clinical deterioration (Figure 1). Within the former category, adoptive immunotherapy may be used for the prevention or treatment of active SARS-CoV-2 infection in immunocompromised patients and includes adoptive immunotherapy with SARS-CoV-2–specific T cells or natural killer (NK) cells. By contrast, immune modulatory cellular therapies include Tregs and mesenchymal stromal cells. Phase 1/2 trials are underway to evaluate these therapies clinically. Hence, this review focuses on the immunologic basis for their development and the results to date.
Figure 1.
Classification of cellular therapies for SARS-CoV-2 infection. Cellular therapy for SARS-CoV-2 can be classified as adoptive anti-viral immunotherapy with CST or NK cells to aid immunocompromised patients with viral clearance (A) or immunomodulatory immunotherapy with Tregs or MSCs to correct dysregulated immune responses in patients with severe COVID-19 (B).
T-cell responses to SARS-CoV-2 infection
The adaptive immune response to SARS-CoV-2 has been an area of intense investigation since the onset of the pandemic. Understanding antigen-specific B-cell, CD4+ T-cell, and CD8+ T-cell responses has been essential for developing effective vaccines and defining the immunopathology that contributes to severity of illness caused by SARS-CoV-2. Although maladaptive immune responses to SARS-CoV-2 remain incompletely understood, several studies to date suggest a link between severe COVID-19 and insufficient early innate immune responses to SARS-CoV-2, resulting in weak or delayed adaptive response,24,34 rather than a primary pathologic role of antigen-specific humoral or cell-mediated adaptive immunity.34-39 Indeed, circulating CD4+ SARS-CoV-2–specific T cells (CSTs) are detected in peripheral blood mononuclear cells (PBMCs) from >90% of convalescent individuals, CD8+ CSTs are detected in >70%, and the presence of CSTs is associated with recovery and decreased severity of illness.40-44 Lymphopenia is associated with poorer outcomes in COVID-19, and analysis of bronchoalveolar lavage (BAL) fluid from patients with varying illness severity indicates decreased clonal T-cell expansion, suggesting a suboptimal CST presence in the lungs of patients with severe or fatal disease.37,45 Moreover, in patients with hematologic malignancies, CD8+ T-cell depletion has been associated with poor outcomes, particularly in patients who also have impaired humoral responses to SARS-CoV-2.46 These findings suggest that T-cell responses, particularly CSTs, are important for effective viral clearance and are associated with improved outcomes in patients with acute infection. Thus, adoptive cellular therapy with CSTs and/or NK cells may be an effective strategy for improving outcomes in immunocompromised patients with or at risk for SARS-CoV-2 infection.
The potential application of immunotherapy could be relevant to many patient groups. For example, immunomodulatory immunotherapy could be applicable to any patient at high risk of severe COVID-19. CST or NK therapy would be most applicable to immunocompromised patients with T-cell deficiency or those receiving immunosuppressive therapies. In these patients, early identification and treatment of those at high risk for immune dysregulation because of SARS-CoV-2 might enhance viral clearance and prevent severe disease, because lower initial viral load,47 early bystander CD8+ T-cell activation,48 and adequate early type I interferon response38,39,49 correlate with decreased mortality related to SARS-CoV-2.35,50 For example, in patients with autoantibodies to type I interferon, CST therapy could theoretically bypass early defects in interferon signaling and restore immune responses to SARS-CoV-2. Additionally, analysis of T-cell subsets has shown that Th1-skewed and CD8+ T-cell responses are associated with decreased COVID-19 severity,51,52 suggesting that enhanced cell therapy products might be manufactured to favor protective T-cell subsets.53 Whether adoptive immunotherapy with CSTs and/or NK cells administered later in the disease course worsens ongoing inflammation and immunopathology is not known but will be addressed by ongoing phase 1/2 trials (Tables 1 and 2).
Table 1.
SARS-CoV-2–specific T-cell trials for treatment or prevention of COVID-19
| Trial | Treatment | Population | Study design | Phase | Estimated enrollment | Blood disorder eligibility |
|---|---|---|---|---|---|---|
| NCT04457726 | Allogeneic CSTs | 1 to 90 y SARS-CoV-2 RT-PCR + within 72 h of enrollment | Arm A: severe COVID-19 Arm B: mild to moderate COVID-19 with high risk of progression to severe disease based on age and/or underlying comorbidity | 1/2 (recruiting) | 18 | Not excluded unless receiving >0.5 mg/kg/d steroid |
| NCT04765449 | Partially HLA-matched banked allogeneic CSTs | ≥18 y SARS-CoV-2 RT-PCR + High risk of severe disease based on age and/or underlying comorbidity No supplemental O2 requirement | Arm A: Treatment with CSTs Arm B: No available HLA-matched product, monitored at home and may receive any standard of care treatment for COVID-19 | 1 (recruiting) | 24 | Included: chemotherapy for malignancy within the prior 24 mo Excluded: prior allogeneic HSCT or solid organ transplant; current chemotherapy, radiation, and/or immunosuppressive drug regimen |
| NCT04742595 | Partially HLA-matched banked allogeneic CSTs | ≥18 y Immunocompromised with cancer SARS-CoV-2 RT-PCR + within 2 wk of enrollment Presence of respiratory symptoms | Patients receive CSTs on day 1 and treatment may repeat every 14 d at investigators' discretion. | 1 (recruiting) | 16 | Yes (required for inclusion) |
| NCT04401410 | Partially HLA-matched banked allogeneic CSTs | ≥18 y SARS-CoV-2 RT-PCR + within 5 d of enrollment Hospitalized for COVID-19 High risk of severe disease based on age and/or underlying comorbidity No supplemental O2 requirement | Phase I: dose finding phase Phase II: randomized pilot study comparing CST treatment at dose determined in phase I to current institutional standard of care treatment for COVID-19 | 1/2 (terminated early) | Final number not yet reported | Yes (inclusion criteria as risk factor for severe disease) |
| NCT04762186 | Allogeneic CSTs | ≥18 y SARS-CoV-2 RT-PCR + within 72 h of enrollment Maximum 14 d between symptom onset and enrollment WHO score 5 or 4 with one additional risk factor for progression | Phase I: dose finding phase Phase II: randomized pilot study comparing CST treatment at dose determined in phase I to current institutional standard of care treatment for COVID-19 | 1/2 (recruiting) | 12 | Yes (inclusion criteria as risk factor for severe disease) |
| NCT04896606 | Family derived HLA-matched allogeneic CSTs | 18 to 65 y SARS-CoV-2 RT-PCR + Hospitalized for mild to moderate COVID-19 disease Risk of progression based on underlying comorbidity HLA-matched family related donor with recent SARS-CoV-2 infection at least 10 d from symptom onset available | Experimental arm: Patients receive family donor derived CSTs up to five times every 2 wk along with standard of care. Active Comparator: Standard of care alone. | 1/2 (recruiting) | 50 | Yes (inclusion criteria as risk factor for severe disease) |
| NCT05141058 | HSCT donor-derived allogeneic CSTs | ≥12 y and <80 y ≥28 d and <4 wk after allogeneic HSCT SARS-CoV-2 RT-PCR negative | Arm A: Adults (≥18 to <80 y) will receive a single infusion of CSTs at escalating doses for prophylaxis against SARS-CoV-2 infection. Arm B: Children (≥12 and <18 y) will receive a single infusion of CSTs at escalating doses for prophylaxis against SARS-CoV-2 infection. | 1 (recruiting) | 24 | Yes (required for inclusion) |
Table 2.
NK-cell immunotherapy trials for COVID-19
| Trial | Treatment | Population | Study design | Phase | Estimated enrollment | Blood disorder eligibility |
|---|---|---|---|---|---|---|
| NCT04900454 | Allogeneic NK cells derived from CD34+ hematopoietic stem cells (DVX201) | 18 to 80 y SARS-CoV-2 RT-PCR + within 7 d of enrollment Hospitalized for COVID-19 Maximum 4L O2 to maintain SO2 ≥93% Inflammatory markers within specified range | Open label, nonrandomized dose-finding study | 1 (recruiting) | 18 | Excluded if receiving systemic immune suppression |
| NCT04280224 | Allogeneic NK cells | 18 to 65 y SARS-CoV-2 RT-PCR + Radiographic evidence of pneumonia | Experimental arm: participants will receive NK cells twice per week, plus conventional therapy No intervention arm: Participants will receive only current standard of care treatment | 1 (recruiting) | 30 | Excluded for malignancy or other serious systemic disorder |
| NCT04365101 | Allogeneic NK cells expanded from human placental CD34+ cells (CYNK-001) | ≥18 y SARS-CoV-2 + using institutionally approved test SO2 ≥92% on supplemental O2 or ≥88% on room air Experiencing any symptom or radiographic finding associated with COVID-19 | Phase 1: evaluate the safety and efficacy of CYNK-001 given on days 1, 4, and 7 in 14 total patients. Phase 2: randomized, open-label assignment to either CYNK-001 or standard of card alone | 1/2 (active, not recruiting) | 86 (14 in phase 1, up to 72 in phase 2) | Excluded for active malignancy and/or immunosuppression |
| NCT04634370 | Allogeneic NK cells | ≥18 y SARS-CoV-2 + using institutionally approved test White or yellow clinical warning criteria174 | Open label, nonrandomized dose-finding study | 1 (not yet recruiting) | 24 | Excluded for malignant blood-borne diseases |
| NCT04363346 | Induced pluripotent stem cell-derived NK cells transduced with high affinity, ADAM17 non-cleavable Fc receptor (CD16) (FT516) | 18 to 76 y old SARS-CoV-2 + Hospitalized for COVID-19 Maximum supplemental O2 requirement 4 L Radiographic evidence of chest infiltrates Inflammatory markers in specified range | Open label sequential assignment dose-finding study | 1 (active, not recruiting) | 5 | Excluded for any known condition requiring systemic immunosuppression |
| NCT04324996 | Cord-blood derived NKG2D-ACE2 CAR-NK cells secreting IL-15 superagonist and GM-CSF neutralizing scFv | ≥18 y Diagnosed with pneumonitis and new coronavirus infection Within 14 d of illness onset | Randomized, parallel assignment with quadruple masking. Arm A: NK cells secreting IL-15 superagonist Arm B: NKG2D CAR-NK cells Arm C: ACE2 CAR-NK cells Arm D: NKG2D-ACE2 CAR NK cells secreting IL-15 superagonist and GM-CSF neutralizing scFv | 1/2 (recruiting) | 90 | Excluded for long-term anti-rejection or immune modulatory drugs |
| NCT04578210 | Allogeneic memory T cells or allogeneic NK cells from convalescent donors | ≤80 y SARS-CoV-2 RT-PCR + within 72 h of enrollment Onset of symptoms within 10 d and <3 d of hospitalization prior to infusion Requiring hospitalization Radiographic evidence of pneumonia Lymphopenia ≤2.5 L O2 requirement | Arm A: single infusion of memory T cells Arm B: single infusion of NK cells | 1/2 (recruiting) | 58 | Not excluded |
Adoptive virus-specific T-cell therapy
Adoptive cellular therapy with virus-specific T cells (VSTs) has been used safely and effectively for more than 25 years to treat and prevent viral infections in patients with immune deficiencies, especially in the post-HSCT setting.22,54-57 Manufacture of VSTs for clinical use involves either selection or ex vivo expansion from donor PBMCs. VST selection uses major histocompatibility complex–antigen multimers or cytokine capture technology to isolate VSTs from PBMCs, whereas ex vivo expansion involves PBMC culture in the presence of growth-enhancing cytokines and viral antigens for 10 to 12 days to generate a product enriched in VSTs targeting 1 or more viruses.21,56 In the post-HSCT population, treatment with donor-derived VSTs results in reconstitution of antiviral immunity with persistence of VSTs for years after infusion.58,59 For patients who have not undergone HSCT or for whom a donor is not available, banking of cryopreserved ex vivo expanded VSTs has developed as an effective “off-the-shelf” approach to VST therapy, allowing for rapid treatment of fulminant viral infections with partially HLA-matched VST products.57,60-62 HLA matching strategies vary across protocols and research continues to determine the optimal approach. Recent studies have demonstrated that small banks using strategically chosen donors based on their HLA type and immunity to the target of interest can provide potential treatment to a large number of referred patients.63 Evidence to date points to increased efficacy if at least 1 shared HLA allele is known to mediate antiviral T-cell immunity.57 Therefore, in the setting of SARS-CoV-2 infection, donor-derived CSTs could be an option as treatment or prophylaxis for high-risk patients after HSCT, and third party partially HLA-matched CSTs could be used as an early treatment for COVID-19 infection in high-risk patients with blood disorders in general.
Clinical use of SARS-CoV-2–specific T cells
CSTs can be expanded from the PBMCs of most convalescent donors, along with some individuals who have not been infected with SARS-CoV-2, likely because of cross-reactivity with common cold coronaviruses.40,64-66 Epitope mapping has established immunogenic hot spots within SARS-CoV-2, including multiple regions of the spike and nucleocapsid proteins, as well highly conserved regions of the membrane protein, allowing for design of peptide pools for rapid expansion of CSTs for clinical use.64,65 Convalescent donors who have seroconverted display broader T-cell antigenic responsiveness, but even seronegative convalescent individuals can elicit an expandable CST population.64 Spike-directed T-cell responses have also been demonstrated in individuals who have been vaccinated against SARS-CoV-2, thus providing a large pool of potential donors for the generation of CST banks.67-71 Moreover, these spike-directed T-cell responses elicited from vaccinated but previously uninfected donors against peptide pools created from the Wuhan strain have shown cross reactivity to other variant strains, thereby broadening the applicability of this approach.72
Currently, there are 7 registered phase 1/2 trials evaluating allogeneic CSTs for the treatment or prevention of COVID-19, 4 of which are actively recruiting patients (Table 1). Six trials are designed to test third party allogeneic CSTs for treatment of SARS-CoV-2 infection in high-risk patients (based on illness severity score, underlying comorbidities, and/or age) and 1 (NCT05141058) tests HSCT donor-derived CSTs for prophylaxis against SARS-CoV-2 infection in SARS-CoV-2–negative participants after allogeneic HSCT. Two trials (NCT05141058 and NCV04745295) specifically target immunocompromised patients with blood disorders; 3 others include malignancy and/or immune suppression as risk factors for severe disease, which are required for eligibility (Table 1). To date, data from 1 trial (NCT04401410) have been presented detailing 4 patients who were treated with partially HLA-matched CSTs to treat SARS-CoV-2 infection in high-risk individuals. One patient experienced symptoms consistent with cytokine release syndrome but recovered. Three of the 4 treated patients achieved resolution of their infection after CST infusion,73 but without results from the control group, the extent of the CST effect is unclear. Unfortunately, this trial was terminated early because of feasibility concerns with insufficient numbers of patients meeting inclusion criteria.
As SARS-CoV-2 variants arise, CSTs generated for therapeutic use must be evaluated for cross-reactivity against new circulating viral strains. Studies to date demonstrate moderate to high T-cell cross-reactivity against circulating variants, including the omicron variant,74-76 with strong reactivity particularly in the CD4+ compartment.67,70,72,77-79 Indeed, T-cell epitopes identified in CSTs from convalescent patients span the viral proteome40,50,80-82 and stimulate T-cell responses to viral variants that are partially resistant to vaccine-induced humoral spike-specific responses.83-85 Importantly, high-throughput systematic analysis of CD8+ T-cell activity in response to mutant peptides from SARS-CoV-2 variants of concern, including alpha, beta, and delta variants, has suggested decreased ability of some mutant epitopes to bind to certain HLA,86,87 which highlights the need to ensure that CSTs generated for clinical use maintain activity against circulating strains as new variants arise.72 SARS-CoV-2–specific T cells are long-lasting in convalescent individuals, retaining activation and proliferation capacity ex vivo for at least 10 months,88 and supporting the assertion that CSTs may provide durable protection against severe illness due to SARS-CoV-2, even as humoral immunity wanes.89
Limitations/effect of concomitant steroid treatment on adoptive cellular therapy efficacy
Although many groups have classified T-cell immunity to SARS-CoV-2 and demonstrated the feasibility of CST generation, the hyperinflammatory nature of critical COVID-19 calls into question whether T-cell therapy may be beneficial in the setting of pneumonia or acute respiratory distress syndrome (ARDS). Dexamethasone is standard treatment for hypoxic patients following the demonstration of a survival advantage in randomized controlled trials, and this therapy is highly likely to inactivate both endogenous lymphocytes and any unmodified adoptive cell therapies. Basar et al90 showed that corticosteroid-resistant T cells targeting SARS-CoV-2 could be generated via CRISPR/Cas9 knockout of the glucocorticoid receptor (NR3C1), and the resulting cells maintain viability and effector function in the presence of dexamethasone in vitro. These and similar approaches may facilitate the use of cell therapy even when immunosuppressive pharmacotherapy must be administered simultaneously.
NK-cell immunotherapy for COVID-19
NK cells are an essential component of antiviral defense, as demonstrated by many inborn errors of immunity in which NK cell defects result in viral susceptibility.91,92 Studies of COVID-19 have demonstrated that NK lymphopenia is common in acute illness, with loss of CD56dim effector NK cells in patients with severe cases.93 Reports have revealed inverse correlations between NK counts and serum IL-6 level,94 as well as interleukin-2 receptor alpha.95 Robust NK activation has been observed in both peripheral blood and BAL samples from patients with COVID-19, although elevation of adaptive NK cells (NKG2C+/Ksp37+/perforin+) was exclusively seen in severe disease.96 A recent study suggested that the IL-15–IL-15R axis may be a key driver of immune dysfunction in COVID-19 infection, with excess signaling resulting in NK dysfunction.97 Ma et al98 also demonstrated that NK cells modified with a chimeric antigen receptor (CAR) using a single chain variable fragment (scFv) derived from the spike-targeting S309 monoclonal antibody killed spike-expressing targets and had cross-reactivity with common spike variants.
Presently, there are 7 clinical trials evaluating allogeneic NK cell immunotherapy as adjunctive treatment for COVID-19, as well as 1 trial of NK CAR immunotherapy targeting SARS-CoV-2 (Table 2); none specifically target immunocompromised populations. No study results have been published to date and at least 1 such trial is no longer recruiting (NCT04365101).
Cell therapy targeting immune dysregulation in COVID-19
Although characterization of COVID-19 immunopathology has been complicated by the dynamic nature of the immune response over time, distinct immunologic profiles are associated with progression to severe disease in patients infected with SARS-CoV-2.24,39,99,100 Elevated plasma markers of inflammation, including C-reactive protein (CRP), ferritin, IL-6, IL-8, and tumor necrosis factor-α are associated with risk of progression to severe disease and mortality.26,101-104 Additionally, severe COVID-19 is characterized by circulating T-cell lymphopenia and an activated, exhausted T-cell phenotype,105-108 Treg dysfunction,109 and myeloid cell activation in blood and bronchoalveolar samples.37,45,110-112 Multisystem inflammatory syndrome in children, an inflammatory complication of SARS-CoV-2 infection in children, seems to be associated with increased CST responses compared with children who have uncomplicated SARS-CoV-2 infection113 and has an inflammatory profile unique from severe COVID-19 in adults.114,115 Additionally, this syndrome has been associated with activation of CX3CR1+ vascular patrolling T cells.116 These immunologic signatures may allow for targeting of immune modulatory treatments to the patients most likely to benefit from them and point to the potential utility of immune modulation in treating COVID-19.
Multiple immune modulators, including IL-1 and IL-6 receptor blockers and systemic corticosteroids, have been used to target the hyperinflammatory phenomena in severe COVID-19 and multisystem inflammatory syndrome in children, which have recently been reviewed.117,118 Cellular treatments with ex vivo expanded Tregs and/or mesenchymal stromal cells (MSCs) may offer a targeted and less broadly immunosuppressive approach. In addition, Tregs and MSCs have shown promise in preclinical and early clinical trials for the treatment of ARDS,119-124 a hallmark of severe COVID-19.
Use of Treg and MSC therapies in ARDS
ARDS is a syndrome of lung injury defined by the acute development of hypoxemia resulting from alveolar injury and loss of vectorial fluid transport out of the airspaces. This is accompanied by dysregulated alveolar inflammatory cell infiltration that perpetuates the injury, although the exact immunologic responses are only partially understood. The therapeutic potential of Tregs and MSCs in ARDS centers around their immune modulatory and tissue reparative properties. In preclinical models, Tregs attenuate markers of inflammation, promote tissue repair, and shorten time to recovery from lung injury, although Tregs have not been trialed clinically in ARDS before their use in SARS-CoV-2 infection.120 MSCs attenuate systemic inflammation and lung injury in murine models of ARDS, and phase 1 and 2a trials among adults with ARDS have shown them to be safe and well tolerated.122,125 In viral ARDS specifically, preclinical results with MSC treatment have been mixed.126-128 Whether the therapeutic effect of MSCs changes depending on the viral pathogen remains an open question.
Both MSCs and Tregs have been used safely to treat steroid-refractory graft-versus-host disease (GVHD). In this setting, treatment aims to dampen a damaging graft-versus-host immune response by suppressing cytotoxic T cells along with elements of the innate immune response including dendritic and NK cells.129,130 Similar immune modulatory targets may explain the therapeutic potential of these biologics for the treatment of viral ARDS, which is exacerbated by a damaging inflammatory response.131
Treg treatment for COVID-19
The full phenotype and function of Tregs in vivo is well reviewed elsewhere132-134 and is beyond the scope of this review. In brief, Tregs are characteristically CD4+CD25hiCD127lo T lymphocytes that express the transcription factor Forkhead Box Protein 3 and inhibit the activation and proliferation of inflammatory effector cells, including CD4+ and CD8+ effector T lymphocytes, macrophages, B cells, neutrophils, and dendritic cells.132,135,136 Treg products for cellular therapy may be either autologous or allogeneic depending on the clinical context and have been safely administered to patients for the treatment of GVHD, solid organ transplant rejection, and autoimmune diseases in phase 1/2 clinical trials.137-141
In the setting of an acute and life-threatening viral infection, such as severe COVID-19, rapid availability of an “off-the-shelf” product is needed. Thus, clinical trials of Tregs in COVID-19 (Table 3) are evaluating banked, partially HLA-matched allogeneic Treg products. The manufacture of Tregs for treatment of SARS-CoV-2 infection requires expansion from donor cord blood (CB) or peripheral blood, as Tregs comprise only 5% to 10% of the CD4+ population in these sources.
Table 3.
Treg-cell immunotherapy trials for COVID-19
| Trial | Treatment | Population | Study design | Phase | Estimated enrollment | Blood disorder eligibility |
|---|---|---|---|---|---|---|
| NCT05027815 | Cryopreserved ex vivo expanded polyclonal CD4+CD127loCD25+ cells | 18 to 70 y SARS-CoV-2 + RT-PCR Diagnosis of ARDS requiring intubation within 72 h of enrollment Chest imaging consistent with COVID-19 pneumonia | Nonrandomized, open label, dose escalation trial at 3 doses (100, 200, 400 × 106 cells) | 1/2 (recruiting) | 18 | Excluded for known or suspected immune suppression and/or a history of bone marrow or stem cell transplantation |
| NCT04468971 | CK0802 | ≥18 y SARS-CoV-2 RT-PCR positive Moderate to severe ARDS Intubated for less than 120 h | Multicenter, double blinded, randomized, placebo-controlled safety and early efficacy trial Arm 1: placebo Arm 2: CK0802 at 1 × 108 cells Arm 3: CK0802 at 3 × 108 cells | 1 (active, not recruiting) | 45 | Not excluded |
In July 2020, Gladstone et al142 published a case series of 2 adult patients with COVID-19 and ARDS who were treated with 2 to 3 doses of 1 × 108 cells per dose of cryopreserved, allogeneic, HLA-matched Tregs, ex vivo expanded from CB. Neither patient experienced adverse events related to the treatment, and both experienced improvement in symptoms and a decrease in inflammatory markers (including IL-6, IL-12, interferon-γ, tumor necrosis factor-α) that was temporally associated with Treg infusion.142 This CB-derived Treg product, termed CK0802, is now under investigation in a multicenter, double-blinded, placebo-controlled, phase 1 trial (NCT04468971) targeting moderate-to-severe ARDS caused by COVID-19. NCT05027815 is also evaluating treatment with allogeneic ex vivo expanded polyclonal CD4+CD127loCD25hi Tregs for treatment of COVID-19 and ARDS in an open label, nonrandomized dose-escalation study. Results from these trials have not yet been reported.
MSC production for treatment of COVID-19
MSCs currently in use in phase 1/2 clinical trials for the treatment of COVID-19 ARDS are derived from bone marrow, adipose tissue, or umbilical cord and then expanded in vitro for manufacture of a clinical product. Similar products have been used safely and effectively in phase 1, 2, and 3 trials to modulate the graft-versus-host response in acute and chronic GVHD.143-148 Their low MHC-II surface expression allows for allogeneic infusion without HLA matching. Although cell-to-cell contact mediates some aspects of potential therapeutic benefit of MSCs,149-151 their immune modulatory, antimicrobial, and tissue reparative properties are largely mediated by paracrine factors collectively referred to as the MSC “secretome.”152-157 MSC-secreted hepatocyte growth factor,124 keratinocyte growth factor,154,158 and angiopoietin-1155,159 have all been linked to protection against lung injury, as have extracellular vesicle-associated RNAs.157 As such, MSC-derived extracellular vesicles are also under investigation for the treatment of severe COVID-19.
Although MSCs show efficacy in preclinical disease models and safety in early clinical trials, the results of phase 3 trials have been mixed. This is likely in part because of variation in tissue source and manufacturing protocols, including culture conditions and number of passages, which can lead to functional and phenotypic differences in MSCs that might go undetected based on minimal release criteria.160 Furthermore, best methods of isolation (plastic adherence vs selection) and ex vivo expansion are also unclear, as head-to-head studies of clinical outcomes using differing manufacturing methods have not been performed.161
Use of MSCs for treatment of COVID-19
Based on preclinical and early clinical data supporting their use in ARDS and observation of the inflammatory response to SARS-CoV-2, several groups completed pilot studies using MSCs to treat severe COVID-19, with no observed treatment-related adverse events.162-167 These included an open-label, individually randomized pilot study conducted by Shu et al,162 in which 41 patients diagnosed with severe COVID-19 were assigned to treatment with a single IV dose of 2 × 106 cells/kg human umbilical cord (hUC)-MSCs (n = 12) or standard treatment (n = 29), with a decline in CRP and IL-6 and more rapid improvement in hypoxemia in the treatment compared with control group. Leng et al164 treated 7 patients diagnosed with COVID-19 with 1 × 106 cells/kg of hUC-MSCs with subsequent clinical improvement and decreased CRP and confirmed that their hUC-MSC product was ACE2 negative and thus unlikely to be infected by SARS-CoV-2, a finding that has been confirmed elsewhere.164,168,169 Guo et al165 treated 31 patients with severe COVID-19 pneumonia with 1 × 106 cells/kg hUC-MSCs with a trend toward improvement in oxygenation and decreased inflammatory markers (IL-6, CRP, procalcitonin) after treatment. Sengupta et al170 treated patients with severe COVID-19 and moderate-to-severe ARDS (n = 24) with MSC-derived exosomes (ExoFlo) in a nonrandomized, open-label cohort study and found an improvement in oxygenation and a survival rate of 83% after treatment, along with an increase in lymphocyte counts and a decrease in CRP.
Results from early randomized controlled trials of MSCs for treatment of COVID-19 have shown promising preliminary efficacy results, although their samples sizes are small. In a double-blinded, randomized, placebo-controlled trial of 40 critically ill adults with COVID-19, 20 of whom were treated with hUC-MSCs, Dilogo et al171 (NCT04457609) reported a survival rate in patients treated with hUC-MSCs that was 2.5 times higher than those who received placebo (P = .047). Lanzoni et al172 (NCT04355728) also performed a double-blinded, randomized, placebo-controlled phase 1/2a study in which 24 patients with COVID-19 ARDS were allocated 1:1 to either treatment with 2 doses of 100 ± 20 × 106 hUC-MSCs or vehicle solution and found significantly improved patient survival (91% vs 42%, P = .015), serious adverse event-free survival, and time to recovery in the hUC-MSC group. Shi et al173 (NCT04288102) treated 101 patients who had been hospitalized for COVID-19, most of whom were classified as being in the convalescent phase of illness at enrollment, with either hUC-MSCs (n = 66) or placebo (n = 35). This study identified an improvement in a 6-minute walk test and computed tomography lung lesion burden in the MSC group compared with placebo. There are currently more than 30 registered clinical trials evaluating safety, feasibility, and efficacy of MSCs for the treatment of COVID-19.
Limitations and future directions
Although multiple studies of cellular therapy targeting COVID-19 are underway or planned, there remain many potential hurdles for these treatments. Although some of the current studies include control groups, randomized controlled studies of cellular therapies are difficult to carry out, particularly when focused on rare patient populations. Cellular therapies can be costly because of the manufacturing requirements. However, current antiviral cell therapies are roughly on par with the cost of IV antiviral medications, and if effective in reducing hospitalization time, they may be economical. As SARS-CoV-2 infection has the potential to progress rapidly, both antiviral and anti-inflammatory cellular therapies would likely require rapid turnaround (likely on the order of days) to be feasible as treatment options. This would likely eliminate individualized cellular therapies for treatment in most cases. Furthermore, the standard use of immunosuppressive medications including corticosteroids in patients with severe respiratory disease may inactivate infused cellular therapies. Gene-engineered products may overcome this limitation but would add to the cost of product generation. Use of previously generated cell banks from healthy donors could overcome many of these hurdles.
Conclusion
There remains a need for novel therapies to protect vulnerable populations from SARS-CoV-2 and future emerging infectious diseases, and adoptive cellular therapy may play a role in the prevention of disease in patients with blood disorders who are unable to mount a vaccine response. In addition, cell-based therapies are a potential treatment for these patients and high-risk individuals with complicated COVID-19. Randomized controlled trials of antiviral and anti-inflammatory immunotherapy are, however, required to help determine whether these therapies will have an established place in our armamentarium against COVID-19.
Supplementary Material
Acknowledgments
Funding support for this article was provided by the Leukemia and Lymphoma Society (6632-21) and the Board of Visitors at Children's National Hospital, the Katzen Foundation, and the Connor Family Foundation.
Authorship
Contribution: S.R.C. conducted the literature review and wrote the paper; M.D.K. conducted the literature review and edited the paper; and C.M.B. oversaw the literature review and edited the paper.
Conflict-of-interest disclosure: C.M.B. is a cofounder and on the scientific advisory boards for Catamaran Bio and Mana Therapeutics with stock and/or ownership, is on the board of directors for Caballeta Bio with stock options, and has stock in Neximmune and Repertoire Immune Medicines. M.D.K. is on a scientific advisory panel for Enzyvant. C.M.B. and M.D.K. have filed a patent related to SARS-CoV-2 T cell therapy. S.R.C. declares no competing financial interests.
Correspondence: Catherine M. Bollard, Children’s National Hospital, 111 Michigan Ave NW, Washington, DC 20010; e-mail: cbollard@childrensnational.org.
REFERENCES
- 1.Dai M, Liu D, Liu M, et al. Patients with cancer appear more vulnerable to SARS-CoV-2: a multicenter study during the COVID-19 outbreak. Cancer Discov. 2020;10(6):783-791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deng G, Yin M, Chen X, Zeng F. Clinical determinants for fatality of 44,672 patients with COVID-19. Crit Care. 2020;24(1):179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuderer NM, Choueiri TK, Shah DP, et al. ; COVID-19 and Cancer Consortium . Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395(10241):1907-1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma A, Bhatt NS, St Martin A, et al. Clinical characteristics and outcomes of COVID-19 in haematopoietic stem-cell transplantation recipients: an observational cohort study. Lancet Haematol. 2021;8(3):e185-e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah GL, DeWolf S, Lee YJ, et al. Favorable outcomes of COVID-19 in recipients of hematopoietic cell transplantation. J Clin Invest. 2020; 130(12):6656-6667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kinoshita H, Durkee-Shock J, Jensen-Wachspress M, et al. Robust antibody and T cell responses to SARS-CoV-2 in patients with antibody deficiency. J Clin Immunol. 2021;41(6):1146-1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aydillo T, Gonzalez-Reiche AS, Aslam S, et al. Shedding of viable SARS-CoV-2 after immunosuppressive therapy for cancer. N Engl J Med. 2020;383(26):2586-2588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kemp SA, Collier DA, Datir RP, et al. ; COVID-19 Genomics UK (COG-UK) Consortium . SARS-CoV-2 evolution during treatment of chronic infection. Nature. 2021;592(7853):277-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Avanzato VA, Matson MJ, Seifert SN, et al. Case study: prolonged infectious SARS-CoV-2 shedding from an asymptomatic immunocompromised individual with cancer. Cell. 2020;183(7):1901-1912.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCarthy KR, Rennick LJ, Nambulli S, et al. Recurrent deletions in the SARS-CoV-2 spike glycoprotein drive antibody escape. Science. 2021;371(6534):1139-1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Truong TT, Ryutov A, Pandey U, et al. Increased viral variants in children and young adults with impaired humoral immunity and persistent SARS-CoV-2 infection: a consecutive case series. EBioMedicine. 2021;67:103355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agha ME, Blake M, Chilleo C, Wells A, Haidar G. Suboptimal response to coronavirus disease 2019 messenger RNA vaccines in patients with hematologic malignancies: a need for vigilance in the postmasking era. Open Forum Infect Dis. 2021;8(7):ofab353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barrière J, Chamorey E, Adjtoutah Z, et al. Impaired immunogenicity of BNT162b2 anti-SARS-CoV-2 vaccine in patients treated for solid tumors. Ann Oncol. 2021;32(8):1053-1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hagin D, Freund T, Navon M, et al. Immunogenicity of Pfizer-BioNTech COVID-19 vaccine in patients with inborn errors of immunity. J Allergy Clin Immunol. 2021;148(3):739-749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mamez AC, Pradier A, Giannotti F, et al. Antibody responses to SARS-CoV2 vaccination in allogeneic hematopoietic stem cell transplant recipients. Bone Marrow Transplant. 2021;56(12):3094-3096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Delmonte OM, Bergerson JRE, Burbelo PD, et al. Antibody responses to the SARS-CoV-2 vaccine in individuals with various inborn errors of immunity. J Allergy Clin Immunol. 2021;148(5):1192-1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Apostolidis SA, Kakara M, Painter MM, et al. Cellular and humoral immune responses following SARS-CoV-2 mRNA vaccination in patients with multiple sclerosis on anti-CD20 therapy. Nat Med. 2021;27(11):1990-2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blyth E, Clancy L, Simms R, et al. Donor-derived CMV-specific T cells reduce the requirement for CMV-directed pharmacotherapy after allogeneic stem cell transplantation. Blood. 2013;121(18):3745-3758. [DOI] [PubMed] [Google Scholar]
- 19.Gerdemann U, Keirnan JM, Katari UL, et al. Rapidly generated multivirus-specific cytotoxic T lymphocytes for the prophylaxis and treatment of viral infections. Mol Ther. 2012;20(8):1622-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muftuoglu M, Olson A, Marin D, et al. Allogeneic BK virus-specific T cells for progressive multifocal leukoencephalopathy. N Engl J Med. 2018;379(15):1443-1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Papadopoulou A, Gerdemann U, Katari UL, et al. Activity of broad-spectrum T cells as treatment for AdV, EBV, CMV, BKV, and HHV6 infections after HSCT. Sci Transl Med. 2014;6(242):242ra83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feucht J, Opherk K, Lang P, et al. Adoptive T-cell therapy with hexon-specific Th1 cells as a treatment of refractory adenovirus infection after HSCT. Blood. 2015;125(12):1986-1994. [DOI] [PubMed] [Google Scholar]
- 23.Bollard CM, Heslop HE. T cells for viral infections after allogeneic hematopoietic stem cell transplant. Blood. 2016;127(26):3331-3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lucas C, Wong P, Klein J, et al. ; Yale IMPACT Team . Longitudinal analyses reveal immunological misfiring in severe COVID-19. Nature. 2020;584(7821):463-469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abers MS, Delmonte OM, Ricotta EE, et al. ; NIAID COVID-19 Consortium . An immune-based biomarker signature is associated with mortality in COVID-19 patients. JCI Insight. 2021;6(1):e144455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Del Valle DM, Kim-Schulze S, Huang HH, et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat Med. 2020;26(10):1636-1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Horby P, Lim WS, Emberson JR, et al. ; RECOVERY Collaborative Group . Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693-704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gordon AC, Mouncey PR, Al-Beidh F, et al. ; REMAP-CAP Investigators . Interleukin-6 receptor antagonists in critically ill patients with Covid-19. N Engl J Med. 2021;384(16):1491-1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cao Y, Wei J, Zou L, et al. Ruxolitinib in treatment of severe coronavirus disease 2019 (COVID-19): a multicenter, single-blind, randomized controlled trial. J Allergy Clin Immunol. 2020;146(1):137-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kalil AC, Patterson TF, Mehta AK, et al. ; ACTT-2 Study Group Members . Baricitinib plus remdesivir for hospitalized adults with Covid-19. N Engl J Med. 2021;384(9):795-807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spinelli FR, Conti F, Gadina M. HiJAKing SARS-CoV-2? The potential role of JAK inhibitors in the management of COVID-19. Sci Immunol. 2020;5(47):eabc5367. [DOI] [PubMed] [Google Scholar]
- 32.Roschewski M, Lionakis MS, Sharman JP, et al. Inhibition of Bruton tyrosine kinase in patients with severe COVID-19. Sci Immunol. 2020;5(48):eabd0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Treon SP, Castillo JJ, Skarbnik AP, et al. The BTK inhibitor ibrutinib may protect against pulmonary injury in COVID-19-infected patients [correction published in Blood. 2021;137(11):1561]. Blood. 2020;135(21):1912-1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bastard P, Rosen LB, Zhang Q, et al. ; COVID Human Genetic Effort . Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science. 2020;370(6515):eabd4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sette A, Crotty S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell. 2021;184(4):861-880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhou R, To KK, Wong YC, et al. Acute SARS-CoV-2 infection impairs dendritic cell and T cell responses. Immunity. 2020;53(4):864-877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Szabo PA, Dogra P, Gray JI, et al. Longitudinal profiling of respiratory and systemic immune responses reveals myeloid cell-driven lung inflammation in severe COVID-19. Immunity. 2021;54(4):797-814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang Q, Bastard P, Liu Z, et al. ; NIAID-USUHS/TAGC COVID Immunity Group . Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science. 2020;370(6515):eabd4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blanco-Melo D, Nilsson-Payant BE, Liu WC, et al. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell. 2020;181(5):1036-1045.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grifoni A, Weiskopf D, Ramirez SI, et al. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. 2020;181(7):1489-1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dan JM, Mateus J, Kato Y, et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science. 2021;371(6529):eabf4063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rydyznski Moderbacher C, Ramirez SI, Dan JM, et al. Antigen-specific adaptive immunity to SARS-CoV-2 in acute COVID-19 and associations with age and disease severity. Cell. 2020;183(4):996-1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Le Bert N, Clapham HE, Tan AT, et al. Highly functional virus-specific cellular immune response in asymptomatic SARS-CoV-2 infection. J Exp Med. 2021;218(5):e20202617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tan AT, Linster M, Tan CW, et al. Early induction of functional SARS-CoV-2-specific T cells associates with rapid viral clearance and mild disease in COVID-19 patients. Cell Rep. 2021;34(6):108728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liao M, Liu Y, Yuan J, et al. Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19. Nat Med. 2020;26(6):842-844. [DOI] [PubMed] [Google Scholar]
- 46.Bange EM, Han NA, Wileyto P, et al. CD8+ T cells contribute to survival in patients with COVID-19 and hematologic cancer. Nat Med. 2021;27(7):1280-1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pujadas E, Chaudhry F, McBride R, et al. SARS-CoV-2 viral load predicts COVID-19 mortality. Lancet Respir Med. 2020;8(9):e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bergamaschi L, Mescia F, Turner L, et al. ; Cambridge Institute of Therapeutic Immunology and Infectious Disease-National Institute of Health Research (CITIID-NIHR) COVID BioResource Collaboration . Longitudinal analysis reveals that delayed bystander CD8+ T cell activation and early immune pathology distinguish severe COVID-19 from mild disease. Immunity. 2021;54(6):1257-1275.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hadjadj J, Yatim N, Barnabei L, et al. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science. 2020;369(6504):718-724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moss P. The T cell immune response against SARS-CoV-2. Nat Immunol. 2022;23(2):186-193. [DOI] [PubMed] [Google Scholar]
- 51.Notarbartolo S, Ranzani V, Bandera A, et al. Integrated longitudinal immunophenotypic, transcriptional and repertoire analyses delineate immune responses in COVID-19 patients. Sci Immunol. 2021;6(62):eabg5021. [DOI] [PubMed] [Google Scholar]
- 52.Su Y, Chen D, Yuan D, et al. ; ISB-Swedish COVID19 Biobanking Unit . Multi-omics resolves a sharp disease-state shift between mild and moderate COVID-19. Cell. 2020;183(6):1479-1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lazarski CA, Datar AA, Reynolds EK, Keller MD, Bollard CM, Hanley PJ. Identification of new cytokine combinations for antigen-specific T-cell therapy products via a high-throughput multi-parameter assay. Cytotherapy. 2021;23(1):65-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Heslop HE, Ng CY, Li C, et al. Long-term restoration of immunity against Epstein-Barr virus infection by adoptive transfer of gene-modified virus-specific T lymphocytes. Nat Med. 1996;2(5):551-555. [DOI] [PubMed] [Google Scholar]
- 55.Rooney CM, Smith CA, Ng CY, et al. Infusion of cytotoxic T cells for the prevention and treatment of Epstein-Barr virus-induced lymphoma in allogeneic transplant recipients. Blood. 1998;92(5):1549-1555. [PubMed] [Google Scholar]
- 56.Leen AM, Myers GD, Sili U, et al. Monoculture-derived T lymphocytes specific for multiple viruses expand and produce clinically relevant effects in immunocompromised individuals. Nat Med. 2006;12(10):1160-1166. [DOI] [PubMed] [Google Scholar]
- 57.O’Reilly RJ, Prockop S, Hasan AN, Koehne G, Doubrovina E. Virus-specific T-cell banks for ‘off the shelf’ adoptive therapy of refractory infections. Bone Marrow Transplant. 2016;51(9):1163-1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Keller MD, Darko S, Lang H, et al. T-cell receptor sequencing demonstrates persistence of virus-specific T cells after antiviral immunotherapy. Br J Haematol. 2019;187(2):206-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Heslop HE, Slobod KS, Pule MA, et al. Long-term outcome of EBV-specific T-cell infusions to prevent or treat EBV-related lymphoproliferative disease in transplant recipients. Blood. 2010;115(5):925-935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Leen AM, Bollard CM, Mendizabal AM, et al. Multicenter study of banked third-party virus-specific T cells to treat severe viral infections after hematopoietic stem cell transplantation. Blood. 2013;121(26):5113-5123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tzannou I, Papadopoulou A, Naik S, et al. Off-the-shelf virus-specific T cells to treat BK virus, human herpesvirus 6, cytomegalovirus, Epstein-Barr virus, and adenovirus infections after allogeneic hematopoietic stem-cell transplantation. J Clin Oncol. 2017;35(31):3547-3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vickers MA, Wilkie GM, Robinson N, et al. Establishment and operation of a Good Manufacturing Practice-compliant allogeneic Epstein-Barr virus (EBV)-specific cytotoxic cell bank for the treatment of EBV-associated lymphoproliferative disease. Br J Haematol. 2014;167(3):402-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tzannou I, Watanabe A, Naik S, et al. “Mini” bank of only 8 donors supplies CMV-directed T cells to diverse recipients. Blood Adv. 2019;3(17):2571-2580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Keller MD, Harris KM, Jensen-Wachspress MA, et al. SARS-CoV-2-specific T cells are rapidly expanded for therapeutic use and target conserved regions of the membrane protein. Blood. 2020;136(25):2905-2917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cooper RS, Fraser AR, Smith L, et al. Rapid GMP-compliant expansion of SARS-CoV-2-specific T cells from convalescent donors for use as an allogeneic cell therapy for COVID-19. Front Immunol. 2021;11:598402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mateus J, Grifoni A, Tarke A, et al. Selective and cross-reactive SARS-CoV-2 T cell epitopes in unexposed humans. Science. 2020;370(6512):89-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Goel RR, Painter MM, Apostolidis SA, et al. ; UPenn COVID Processing Unit‡ . mRNA vaccines induce durable immune memory to SARS-CoV-2 and variants of concern. Science. 2021;374(6572):abm0829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sadoff J, Le Gars M, Shukarev G, et al. Interim results of a phase 1-2a trial of Ad26.COV2.S Covid-19 vaccine. N Engl J Med. 2021;384(19):1824-1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Folegatti PM, Ewer KJ, Aley PK, et al. ; Oxford COVID Vaccine Trial Group . Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet. 2020;396(10249):467-478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tarke A, Sidney J, Methot N, et al. Impact of SARS-CoV-2 variants on the total CD4+ and CD8+ T cell reactivity in infected or vaccinated individuals. Cell Rep Med. 2021;2(7):100355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Painter MM, Mathew D, Goel RR, et al. Rapid induction of antigen-specific CD4+ T cells is associated with coordinated humoral and cellular immunity to SARS-CoV-2 mRNA vaccination. Immunity. 2021;54(9):2133-2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Stanojevic M, Geiger A, Ostermeier B, et al. Spike-directed vaccination elicits robust spike-specific T-cell response, including to mutant strains. Cytotherapy. 2022;24(1):10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Vasileiou S, Kuvalekar M, Workineh A, et al. 37. Allogeneic, Off-the-Shelf, SARS-CoV-2-specific T Cells Demonstrate Reactivity Against Emerging Variant Strains. Open Forum Infectious Diseases. 2021; 8(Supplement_1):S27–S27. [Google Scholar]
- 74.Choi SJ, Kim DU, Noh JY, et al. T cell epitopes in SARS-CoV-2 proteins are substantially conserved in the Omicron variant. Cell Mol Immunol. 2022;19(3):447-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Keeton R, Tincho MB, Ngomti A, et al. T cell responses to SARS-CoV-2 spike cross-recognize Omicron. Nature. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mazzoni A, Vanni A, Spinicci M, et al. SARS-CoV-2 spike-specific CD4+ T cell response is conserved against variants of concern, including omicron. Front Immunol. 2022;13:801431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Geers D, Shamier MC, Bogers S, et al. SARS-CoV-2 variants of concern partially escape humoral but not T-cell responses in COVID-19 convalescent donors and vaccinees. Sci Immunol. 2021;6(59):eabj1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Keeton R, Richardson SI, Moyo-Gwete T, et al. Prior infection with SARS-CoV-2 boosts and broadens Ad26.COV2.S immunogenicity in a variant-dependent manner. Cell Host Microbe. 2021;29(11):1611-1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hamelin DJ, Fournelle D, Grenier JC, et al. The mutational landscape of SARS-CoV-2 variants diversifies T cell targets in an HLA-supertype-dependent manner. Cell Syst. 2022;13(2):143-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tarke A, Sidney J, Kidd CK, et al. Comprehensive analysis of T cell immunodominance and immunoprevalence of SARS-CoV-2 epitopes in COVID-19 cases. Cell Rep Med. 2021;2(2):100204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Quadeer AA, Ahmed SF, McKay MR. Landscape of epitopes targeted by T cells in 852 individuals recovered from COVID-19: meta-analysis, immunoprevalence, and web platform. Cell Rep Med. 2021;2(6):100312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Grifoni A, Sidney J, Vita R, et al. SARS-CoV-2 human T cell epitopes: adaptive immune response against COVID-19. Cell Host Microbe. 2021;29(7):1076-1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kuhlmann C, Mayer CK, Claassen M, et al. Breakthrough infections with SARS-CoV-2 omicron despite mRNA vaccine booster dose. Lancet. 2022;399(10325):625-626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.GeurtsvanKessel CH, Geers D, Schmitz KS, et al. Divergent SARS CoV-2 Omicron-reactive T- and B cell responses in COVID-19 vaccine recipients [published online ahead of print 3 February 2022]. Sci Immunol. doi:10.1126/sciimmunol.abo2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Skelly DT, Harding AC, Gilbert-Jaramillo J, et al. ; C-MORE/PHOSP-C Group . Two doses of SARS-CoV-2 vaccination induce robust immune responses to emerging SARS-CoV-2 variants of concern. Nat Commun. 2021;12(1):5061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhang H, Deng S, Ren L, et al. Profiling CD8+ T cell epitopes of COVID-19 convalescents reveals reduced cellular immune responses to SARS-CoV-2 variants. Cell Rep. 2021;36(11):109708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.de Silva TI, Liu G, Lindsey BB, et al. ; ISARIC4C Investigators . The impact of viral mutations on recognition by SARS-CoV-2 specific T cells. iScience. 2021;24(11):103353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jung JH, Rha MS, Sa M, et al. SARS-CoV-2-specific T cell memory is sustained in COVID-19 convalescent patients for 10 months with successful development of stem cell-like memory T cells. Nat Commun. 2021;12(1):4043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Noh JY, Yang JS, Hwang SY, et al. Duration of humoral immunity and cross-neutralizing activity against the Alpha, Beta, and Delta variants after wild-type SARS-CoV-2 infection: a prospective cohort study. J Infect Dis. 2022;jiac050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Basar R, Uprety N, Ensley E, et al. Generation of glucocorticoid-resistant SARS-CoV-2 T cells for adoptive cell therapy. Cell Rep. 2021;36(3):109432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Orange JS. Natural killer cell deficiency. J Allergy Clin Immunol. 2013;132(3):515-525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lisco A, Hsu AP, Dimitrova D, et al. Treatment of relapsing HPV diseases by restored function of natural killer cells. N Engl J Med. 2021;385(10):921-929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wilk AJ, Rustagi A, Zhao NQ, et al. A single-cell atlas of the peripheral immune response in patients with severe COVID-19. Nat Med. 2020;26(7):1070-1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang F, Nie J, Wang H, et al. Characteristics of peripheral lymphocyte subset alteration in COVID-19 pneumonia. J Infect Dis. 2020;221(11):1762-1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Osman M, Faridi RM, Sligl W, et al. Impaired natural killer cell counts and cytolytic activity in patients with severe COVID-19. Blood Adv. 2020;4(20):5035-5039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Maucourant C, Filipovic I, Ponzetta A, et al. ; Karolinska COVID-19 Study Group . Natural killer cell immunotypes related to COVID-19 disease severity. Sci Immunol. 2020;5(50):eabd6832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sahoo D, Katkar GD, Khandelwal S, et al. AI-guided discovery of the invariant host response to viral pandemics. EBioMedicine. 2021;68:103390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ma MT, Badeti S, Chen CH, et al. CAR-NK cells effectively target SARS-CoV-2-spike-expressing cell lines in vitro. Front Immunol. 2021;12:652223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mathew D, Giles JR, Baxter AE, et al. ; UPenn COVID Processing Unit . Deep immune profiling of COVID-19 patients reveals distinct immunotypes with therapeutic implications. Science. 2020;369(6508):eabc8511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Laing AG, Lorenc A, Del Molino Del Barrio I, et al. A dynamic COVID-19 immune signature includes associations with poor prognosis [corrections published in Nat Med. 2020;26:1663 and 2020;26;1951]. Nat Med. 2020;26(10):1623-1635. [DOI] [PubMed] [Google Scholar]
- 101.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242. [DOI] [PubMed] [Google Scholar]
- 102.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ; HLH Across Speciality Collaboration, UK . COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033-1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gong J, Dong H, Xia QS, et al. Correlation analysis between disease severity and inflammation-related parameters in patients with COVID-19: a retrospective study. BMC Infect Dis. 2020;20(1):963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chen G, Wu D, Guo W, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130(5):2620-2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Diao B, Wang C, Tan Y, et al. Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19). Front Immunol. 2020;11:827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kalfaoglu B, Almeida-Santos J, Tye CA, Satou Y, Ono M. T-cell hyperactivation and paralysis in severe COVID-19 infection revealed by single-cell analysis. Front Immunol. 2020;11:589380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ronit A, Berg RMG, Bay JT, et al. Compartmental immunophenotyping in COVID-19 ARDS: a case series. J Allergy Clin Immunol. 2021;147(1):81-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.De Biasi S, Meschiari M, Gibellini L, et al. Marked T cell activation, senescence, exhaustion and skewing towards TH17 in patients with COVID-19 pneumonia. Nat Commun. 2020;11(1):3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Meckiff BJ, Ramírez-Suástegui C, Fajardo V, et al. Imbalance of regulatory and cytotoxic SARS-CoV-2-reactive CD4+ T Cells in COVID-19. Cell. 2020;183(5):1340-1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Merad M, Martin JC. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages [correction published in Nat Rev Immunol. 2020;20:448]. Nat Rev Immunol. 2020;20(6):355-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chua RL, Lukassen S, Trump S, et al. COVID-19 severity correlates with airway epithelium-immune cell interactions identified by single-cell analysis. Nat Biotechnol. 2020;38(8):970-979. [DOI] [PubMed] [Google Scholar]
- 112.Schulte-Schrepping J, Reusch N, Paclik D, et al. ; Deutsche COVID-19 OMICS Initiative (DeCOI) . Severe COVID-19 is marked by a dysregulated myeloid cell compartment. Cell. 2020;182(6):1419-1440.e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Conway SR, Lazarski CA, Field NE, et al. SARS-CoV-2-specific T cell responses are stronger in children with multisystem inflammatory syndrome compared to children with uncomplicated SARS-CoV-2 infection. Front Immunol. 2022;12:793197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Consiglio CR, Cotugno N, Sardh F, et al. ; CACTUS Study Team . The immunology of multisystem inflammatory syndrome in children with COVID-19. Cell. 2020;183(4):968-981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Huang JJ, Gaines SB, Amezcua ML, et al. Upregulation of type 1 conventional dendritic cells implicates antigen cross-presentation in multisystem inflammatory syndrome. J Allergy Clin Immunol. 2022;149(3):912–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Vella LA, Giles JR, Baxter AE, et al. ; UPenn COVID Processing Unit . Deep immune profiling of MIS-C demonstrates marked but transient immune activation compared to adult and pediatric COVID-19. Sci Immunol. 2021;6(57):eabf7570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Meyerowitz EA, Sen P, Schoenfeld SR, et al. Immunomodulation as treatment for severe coronavirus disease 2019: a systematic review of current modalities and future directions. Clin Infect Dis. 2021;72(12):e1130-e1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.McArdle AJ, Vito O, Patel H, et al. ; BATS Consortium . Treatment of multisystem inflammatory syndrome in children. N Engl J Med. 2021;385(1):11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.D’Alessio FR, Tsushima K, Aggarwal NR, et al. CD4+CD25+Foxp3+ Tregs resolve experimental lung injury in mice and are present in humans with acute lung injury. J Clin Invest. 2009;119(10):2898-2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Arpaia N, Green JA, Moltedo B, et al. A distinct function of regulatory T cells in tissue protection. Cell. 2015;162(5):1078-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Fulton RB, Meyerholz DK, Varga SM. Foxp3+ CD4 regulatory T cells limit pulmonary immunopathology by modulating the CD8 T cell response during respiratory syncytial virus infection. J Immunol. 2010;185(4):2382-2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Matthay MA, Calfee CS, Zhuo H, et al. Treatment with allogeneic mesenchymal stromal cells for moderate to severe acute respiratory distress syndrome (START study): a randomised phase 2a safety trial. Lancet Respir Med. 2019;7(2):154-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wilson JG, Liu KD, Zhuo H, et al. Mesenchymal stem (stromal) cells for treatment of ARDS: a phase 1 clinical trial. Lancet Respir Med. 2015;3(1):24-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hu S, Li J, Xu X, et al. The hepatocyte growth factor-expressing character is required for mesenchymal stem cells to protect the lung injured by lipopolysaccharide in vivo. Stem Cell Res Ther. 2016;7(1):66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Liu KD, Wilson JG, Zhuo H, et al. Design and implementation of the START (STem cells for ARDS Treatment) trial, a phase 1/2 trial of human mesenchymal stem/stromal cells for the treatment of moderate-severe acute respiratory distress syndrome. Ann Intensive Care. 2014;4(1):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chan MC, Kuok DI, Leung CY, et al. Human mesenchymal stromal cells reduce influenza A H5N1-associated acute lung injury in vitro and in vivo. Proc Natl Acad Sci USA. 2016;113(13):3621-3626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Darwish I, Banner D, Mubareka S, et al. Mesenchymal stromal (stem) cell therapy fails to improve outcomes in experimental severe influenza. PLoS One. 2013;8(8):e71761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Gotts JE, Abbott J, Matthay MA. Influenza causes prolonged disruption of the alveolar-capillary barrier in mice unresponsive to mesenchymal stem cell therapy. Am J Physiol Lung Cell Mol Physiol. 2014;307(5):L395-L406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hong J, Hueckelhoven A, Wang L, et al. Indoleamine 2,3-dioxygenase mediates inhibition of virus-specific CD8(+) T cell proliferation by human mesenchymal stromal cells. Cytotherapy. 2016;18(5):621-629. [DOI] [PubMed] [Google Scholar]
- 130.Cheung TS, Bertolino GM, Giacomini C, Bornhäuser M, Dazzi F, Galleu A. Mesenchymal stromal cells for graft versus host disease: mechanism-based biomarkers. Front Immunol. 2020;11:1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Newton AH, Cardani A, Braciale TJ. The host immune response in respiratory virus infection: balancing virus clearance and immunopathology. Semin Immunopathol. 2016;38(4):471-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Romano M, Fanelli G, Albany CJ, Giganti G, Lombardi G. Past, present, and future of regulatory T cell therapy in transplantation and autoimmunity. Front Immunol. 2019;10:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Lucca LE, Dominguez-Villar M. Modulation of regulatory T cell function and stability by co-inhibitory receptors. Nat Rev Immunol. 2020;20(11):680-693. [DOI] [PubMed] [Google Scholar]
- 134.Sakaguchi S, Yamaguchi T, Nomura T, Ono M. Regulatory T cells and immune tolerance. Cell. 2008;133(5):775-787. [DOI] [PubMed] [Google Scholar]
- 135.Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Science. 2003;299(5609):1057-1061. [DOI] [PubMed] [Google Scholar]
- 136.Śledzińska A, Vila de Mucha M, Bergerhoff K, et al. Regulatory T cells restrain interleukin-2- and blimp-1-dependent acquisition of cytotoxic function by CD4+ T cells. Immunity. 2020;52(1):151-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Bluestone JA, Buckner JH, Fitch M, et al. Type 1 diabetes immunotherapy using polyclonal regulatory T cells. Sci Transl Med. 2015;7(315):315ra189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Brunstein CG, Miller JS, Cao Q, et al. Infusion of ex vivo expanded T regulatory cells in adults transplanted with umbilical cord blood: safety profile and detection kinetics. Blood. 2011;117(3):1061-1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Marek-Trzonkowska N, Myśliwiec M, Dobyszuk A, et al. Therapy of type 1 diabetes with CD4(+)CD25(high)CD127-regulatory T cells prolongs survival of pancreatic islets: results of one year follow-up. Clin Immunol. 2014;153(1):23-30. [DOI] [PubMed] [Google Scholar]
- 140.Martelli MF, Di Ianni M, Ruggeri L, et al. HLA-haploidentical transplantation with regulatory and conventional T-cell adoptive immunotherapy prevents acute leukemia relapse. Blood. 2014;124(4):638-644. [DOI] [PubMed] [Google Scholar]
- 141.Mathew JM, H-Voss J, LeFever A, et al. A phase I clinical trial with ex vivo expanded recipient regulatory t cells in living donor kidney transplants. Sci Rep. 2018;8(1):7428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Gladstone DE, Kim BS, Mooney K, Karaba AH, D’Alessio FR, Regulatory T. Regulatory T cells for treating patients with COVID-19 and acute respiratory distress syndrome: two case reports. Ann Intern Med. 2020;173(10):852-853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Boberg E, von Bahr L, Afram G, et al. Treatment of chronic GvHD with mesenchymal stromal cells induces durable responses: a phase II study. Stem Cells Transl Med. 2020;9(10):1190-1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kebriaei P, Hayes J, Daly A, et al. A phase 3 randomized study of remestemcel-L versus placebo added to second-line therapy in patients with steroid-refractory acute graft-versus-host disease. Biol Blood Marrow Transplant. 2020;26(5):835-844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Chen S, Zhao K, Lin R, et al. The efficacy of mesenchymal stem cells in bronchiolitis obliterans syndrome after allogeneic HSCT: a multicenter prospective cohort study. EBioMedicine. 2019;49:213-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Dotoli GM, De Santis GC, Orellana MD, et al. Mesenchymal stromal cell infusion to treat steroid-refractory acute GvHD III/IV after hematopoietic stem cell transplantation. Bone Marrow Transplant. 2017;52(6):859-862. [DOI] [PubMed] [Google Scholar]
- 147.Gao L, Zhang Y, Hu B, et al. Phase II multicenter, randomized, double-blind controlled study of efficacy and safety of umbilical cord-derived mesenchymal stromal cells in the prophylaxis of chronic graft-versus-host disease after HLA-haploidentical stem-cell transplantation. J Clin Oncol. 2016;34(24):2843-2850. [DOI] [PubMed] [Google Scholar]
- 148.Muroi K, Miyamura K, Okada M, et al. Bone marrow-derived mesenchymal stem cells (JR-031) for steroid-refractory grade III or IV acute graft-versus-host disease: a phase II/III study. Int J Hematol. 2016;103(2):243-250. [DOI] [PubMed] [Google Scholar]
- 149.Jackson MV, Morrison TJ, Doherty DF, et al. Mitochondrial transfer via tunneling nanotubes is an important mechanism by which mesenchymal stem cells enhance macrophage phagocytosis in the in vitro and in vivo models of ARDS. Stem Cells. 2016;34(8):2210-2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Feng Y, Zhu R, Shen J, et al. Human bone marrow mesenchymal stem cells rescue endothelial cells experiencing chemotherapy stress by mitochondrial transfer via tunneling nanotubes. Stem Cells Dev. 2019;28(10):674-682. [DOI] [PubMed] [Google Scholar]
- 151.Islam MN, Das SR, Emin MT, et al. Mitochondrial transfer from bone-marrow-derived stromal cells to pulmonary alveoli protects against acute lung injury. Nat Med. 2012;18(5):759-765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Bruno S, Grange C, Collino F, et al. Microvesicles derived from mesenchymal stem cells enhance survival in a lethal model of acute kidney injury. PLoS One. 2012;7(3):e33115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Stone ML, Zhao Y, Robert Smith J, et al. Mesenchymal stromal cell-derived extracellular vesicles attenuate lung ischemia-reperfusion injury and enhance reconditioning of donor lungs after circulatory death. Respir Res. 2017;18(1):212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Zhu YG, Feng XM, Abbott J, et al. Human mesenchymal stem cell microvesicles for treatment of Escherichia coli endotoxin-induced acute lung injury in mice. Stem Cells. 2014;32(1):116-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Fang X, Neyrinck AP, Matthay MA, Lee JW. Allogeneic human mesenchymal stem cells restore epithelial protein permeability in cultured human alveolar type II cells by secretion of angiopoietin-1. J Biol Chem. 2010;285(34):26211-26222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Can A, Coskun H. The rationale of using mesenchymal stem cells in patients with COVID-19-related acute respiratory distress syndrome: What to expect. Stem Cells Transl Med. 2020;9(11):1287-1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Khatri M, Richardson LA, Meulia T. Mesenchymal stem cell-derived extracellular vesicles attenuate influenza virus-induced acute lung injury in a pig model. Stem Cell Res Ther. 2018;9(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Lee JW, Krasnodembskaya A, McKenna DH, Song Y, Abbott J, Matthay MA. Therapeutic effects of human mesenchymal stem cells in ex vivo human lungs injured with live bacteria. Am J Respir Crit Care Med. 2013;187(7):751-760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Tang XD, Shi L, Monsel A, et al. Mesenchymal stem cell microvesicles attenuate acute lung injury in mice partly mediated by Ang-1 mRNA. Stem Cells. 2017;35(7):1849-1859. [DOI] [PubMed] [Google Scholar]
- 160.Yin JQ, Zhu J, Ankrum JA. Manufacturing of primed mesenchymal stromal cells for therapy. Nat Biomed Eng. 2019;3(2):90-104. [DOI] [PubMed] [Google Scholar]
- 161.Debacq-Chainiaux F, Erusalimsky JD, Campisi J, Toussaint O. Protocols to detect senescence-associated beta-galactosidase (SA-betagal) activity, a biomarker of senescent cells in culture and in vivo. Nat Protoc. 2009;4(12):1798-1806. [DOI] [PubMed] [Google Scholar]
- 162.Shu L, Niu C, Li R, et al. Treatment of severe COVID-19 with human umbilical cord mesenchymal stem cells. Stem Cell Res Ther. 2020;11(1):361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Liang B, Chen J, Li T, et al. Clinical remission of a critically ill COVID-19 patient treated by human umbilical cord mesenchymal stem cells: a case report. Medicine (Baltimore). 2020;99(31):e21429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Leng Z, Zhu R, Hou W, et al. Transplantation of ACE2- mesenchymal stem cells improves the outcome of patients with COVID-19 pneumonia. Aging Dis. 2020;11(2):216-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Guo Z, Chen Y, Luo X, He X, Zhang Y, Wang J. Administration of umbilical cord mesenchymal stem cells in patients with severe COVID-19 pneumonia. Crit Care. 2020;24(1):420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Chen X, Shan Y, Wen Y, Sun J, Du H. Mesenchymal stem cell therapy in severe COVID-19: a retrospective study of short-term treatment efficacy and side effects. J Infect. 2020;81(4):647-679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Meng F, Xu R, Wang S, et al. Human umbilical cord-derived mesenchymal stem cell therapy in patients with COVID-19: a phase 1 clinical trial. Signal Transduct Target Ther. 2020;5(1):172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Avanzini MA, Mura M, Percivalle E, et al. Human mesenchymal stromal cells do not express ACE2 and TMPRSS2 and are not permissive to SARS-CoV-2 infection. Stem Cells Transl Med. 2021;10(4):636-642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Hernandez JJ, Beaty DE, Fruhwirth LL, Lopes Chaves AP, Riordan NH. Dodging COVID-19 infection: low expression and localization of ACE2 and TMPRSS2 in multiple donor-derived lines of human umbilical cord-derived mesenchymal stem cells. J Transl Med. 2021;19(1):149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Sengupta V, Sengupta S, Lazo A, Woods P, Nolan A, Bremer N. Exosomes derived from bone marrow mesenchymal stem cells as treatment for severe COVID-19. Stem Cells Dev. 2020;29(12):747-754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Dilogo IH, Aditianingsih D, Sugiarto A, et al. Umbilical cord mesenchymal stromal cells as critical COVID-19 adjuvant therapy: a randomized controlled trial. Stem Cells Transl Med. 2021;10(9):1279-1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Lanzoni G, Linetsky E, Correa D, et al. Umbilical cord mesenchymal stem cells for COVID-19 acute respiratory distress syndrome: a double-blind, phase 1/2a, randomized controlled trial. Stem Cells Transl Med. 2021;10(5):660-673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Shi L, Huang H, Lu X, et al. Effect of human umbilical cord-derived mesenchymal stem cells on lung damage in severe COVID-19 patients: a randomized, double-blind, placebo-controlled phase 2 trial. Signal Transduct Target Ther. 2021;6(1):58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Liao X, Wang B, Kang Y. Novel coronavirus infection during the 2019-2020 epidemic: preparing intensive care units-the experience in Sichuan Province, China. Intensive Care Med. 2020;46(2):357-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.