Abstract
Introduction
This study aimed to describe the perspectives of patients from rural communities on access to all forms of kidney replacement therapy to inform strategies to address such inequity.
Methods
Semistructured interviews were conducted. Transcripts were thematically analyzed.
Results
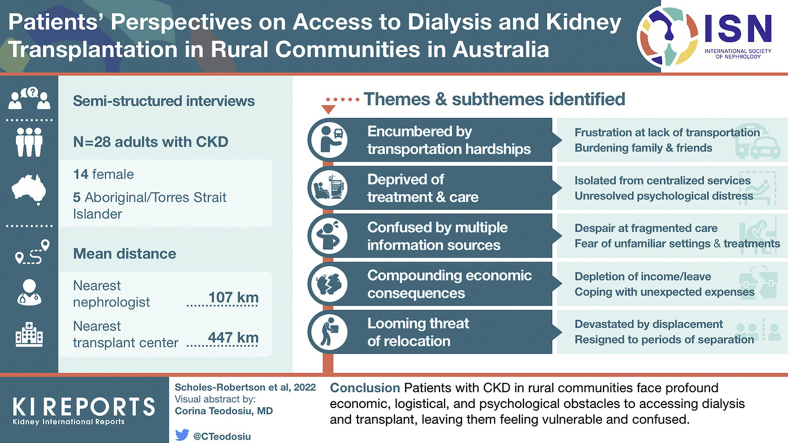
There were 28 participants, of whom, 14 (50%) were female and 5 (17%) Aboriginal or Torres Strait Islander. The mean distance to a nephrologist was 107 km, and transplant center was 447 km. We identified the following 5 themes: encumbered by transportation hardship (burdening of family and friends, frustration at lack of transportation options, heightened vulnerability to road trauma, unrelenting financial strain); deprived of treatment and care (isolated from centralized services, unresolved psychological distress, vulnerable without care, disadvantaged by limited options); confused by multiple information sources (despair at fragmented care, fear of unfamiliar health settings and treatments); compounding economic consequences (depletion of income/leave, coping with unexpected expenses); and the looming threat of relocation (devastated by displacement, resigned to periods of separation, uncertainty in sourcing appropriate accommodation).
Conclusion
Patients with chronic kidney disease (CKD) in rural communities face profound economic, logistical, and psychological obstacles to accessing dialysis and transplant, leaving them feeling vulnerable and confused. To achieve equity of access and improved health outcomes for rural patients with CKD, barriers to dialysis, transplantation, and psychological services in this population require addressing through policy and alternate models of health service delivery, in consultation with rural communities and those families affected by CKD.
Keywords: access, dialysis, qualitative research, rural, transplantation
Graphical abstract
People in rural communities encounter many unique and profound barriers to receiving treatment for CKD that contribute to the increased risk of mortality, morbidity, and hospitalization in this population.1, 2, 3, 4, 5, 6 Limited availability of primary care and specialist services in rural communities can lead to late referral to a nephrologist, increased need to relocate for treatment, and inability to access treatment.4,7,8 Compounding this are socioeconomic disadvantage, increasing remoteness, and poor access despite the greater demand for dialysis and transplantation, which reveals the persistent relevance of the inverse care law in kidney replacement therapy.4,9, 10, 11 In addition, in countries with a history of colonization, there are usually higher numbers of first nations’ people residing in rural and remote locations who require culturally sensitive and safe health care.12
In geographically large countries, such as Canada, the United States, and Australia, longer travel times to dialysis is associated with increased risk of mortality, reduced quality of life, and decreased uptake of some types of kidney replacement therapy.2,13,14 Patients in rural communities are required to spend time away from home for training or surgical procedures needed for home-based dialysis and kidney transplantation15,16 and therefore incur additional costs to those in urban areas, including transport and accommodation.14,17,18 Compounding this is the relative socioeconomic disadvantage experienced in rural communities, including lower household income, lower education attainment, and decreased likelihood of receiving primary health care prevention.19 There are limited policies to redress the inequity of access to care for rural patients with CKD in Australia.20
Despite this, little is known on the perspectives of patients on access to all modalities of kidney replacement therapy in rural communities,21 but more importantly on how they believe it can be improved.22 This study aims to describe the perspectives of patients from rural communities on access to all forms of kidney replacement therapy, which can inform strategies and policy to improve access and reduce inequities and disadvantage experienced by people with CKD in rural areas, thereby improving health outcomes in this group of patients.22
Methods
We followed the Consolidated Criteria for Reporting Qualitative Research framework.23
Context
In Australia, Canada, and the United States combined, >96 million people live in rural settings.22,24,25 Australia has a universal public health insurance scheme, but for some medical consultations, tests, and treatment, there can be a gap payment, which may be substantial.26 When discussing out-of-pocket expenses, we are referring to indirect medical costs, such as transportation, accommodation, but also some direct medical costs, such as medication and any gap payments. In our study, we defined “rural” to include all areas outside of major cities, which represents Modified Monash Classification 2–7 on the Modified Monash Model.27
Participant Selection and Setting
Rural patients with CKD aged >18 years in Australia were eligible. We used purposive sampling to include maximum diversity of characteristics based on demographics (age, sex, geographic location) and current treatment modality. A flyer with information regarding the study was advertised through social media platforms, and participants then contacted researchers whether they were interested in being a part of the study. A snowballing technique was also used whereby participants could nominate other people who they believed could offer a different and relevant perspective on disparities in access to kidney replacement therapy in rural communities. Ethics approval was provided by The University of Sydney (2020-009).
Data Collection
Author NSR conducted semistructured interviews with each participant from February 2020 to October 2020. The interviews were conducted face to face, over the phone, or by Zoom videoconference. The interview guide (Supplementary Appendix S1) was based on a literature review of patient’ and caregivers’ perspectives on access to kidney replacement therapy in rural communities and discussion among the research team.28 Access was defined and discussed in terms of the opportunity to obtain appropriate health care services and receive relevant information pertaining to their health issue.29 We acknowledge that the definition for “rural” varies and may be based on characteristics of a community, availability of health resources, and education and other aspects.30, 31, 32, 33 Interviews were audiorecorded and transcribed. We conducted interviews until data saturation was achieved.34
Analysis
Using thematic analysis, the transcripts were imported into HyperRESEARCH (version 4.0.1, ResearchWare Inc., Randolph, MA), and author NSR read the transcripts, inductively identified preliminary concepts, and grouped similar concepts into initial themes and subthemes. These were reviewed and discussed with NSR and TG, and AT coded the transcripts line by line and identified conceptual links and patterns within the data. Investigator triangulation and member checking helped ensure the findings reflected the full range and depth of the data.
Consumer Involvement
First author NSR has lived experience of both peritoneal dialysis and kidney transplantation and resides in a rural community. NSR conceived the idea for this study and is currently a PhD student with experience in qualitative research.
Results
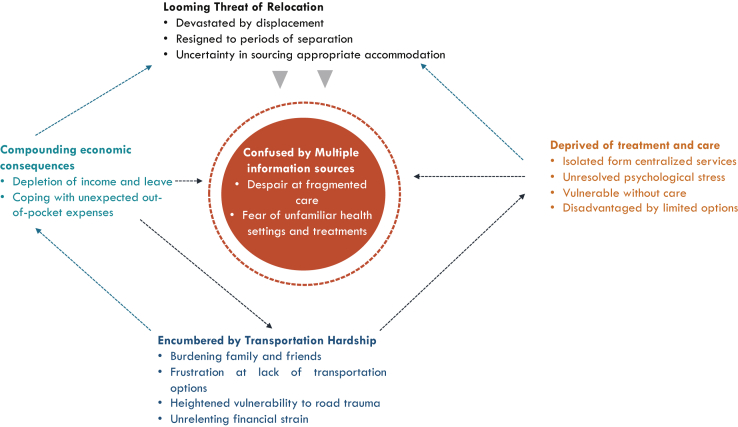
Of the 28 participants, 14 (50%) were female and 5 (17%) identified as Aboriginal or Torres Strait Islander (Table 1). The mean duration of the interview was 28 minutes (range 15–54 minutes). Median distances to services were calculated with highest median distance being to a transplantation center (447 km). We identified the following 5 themes: encumbered by transportation hardship; deprived of treatment and care; confused by multiple information sources; compounding economic consequences; and the looming threat of relocation. The respective subthemes are described subsequently. Figure 1 reveals the relationships between themes and subthemes. Table 2 provides the selected illustrative quotes to support each theme, and Table 3 provides participant suggestions and considerations for practice and policy.
Table 1.
Participant characteristics (n = 28)
| Characteristics | n (%) |
|---|---|
| Female | 14 (50) |
| Age (yr) | |
| <30 | 2 (7) |
| 31–40 | 7 (25) |
| 41–50 | 5 (18) |
| 51–60 | 7 (25) |
| 61–70 | 4 (14) |
| >70 | 3 (11) |
| Current treatment | |
| Kidney transplant | 12 (43) |
| Satellite hemodialysis | 9 (32) |
| Peritoneal dialysis | 4 (14) |
| Home hemodialysis | 3 (11) |
| Marital status | |
| Single | 9 (32) |
| Married/partnered | 16 (58) |
| Separated | 2 (7) |
| Widowed | 1 (3) |
| Ethnicity | |
| Caucasian | 22 (80) |
| Aboriginal | 4 (14) |
| Aboriginal/Torres Strait Islander | 1 (3) |
| Asian | 1 (3) |
| Education level (highest attained) | |
| Postgraduate degree | 1 (3) |
| Undergraduate degree | 10 (35) |
| Professional certificate | 8 (29) |
| Completed 12th grade (ages 17–18 yr) | 3 (11) |
| Completed 10th grade (ages 16 yr) | 3 (11) |
| Before 10th grade | 3 (11) |
| Household income ($AUD) | |
| 0–24,999 | 5 (17) |
| 25,000–49,999 | 13(46) |
| 50,000–74,999 | 5(17) |
| 75,000–99,999 | 3 (10) |
| More than 100,000 | 3(10) |
| Primary cause of kidney disease | |
| Glomerular disease | 11 (39) |
| Genetic | 6 (21) |
| Diabetes | 5 (16) |
| Other | 3 (12) |
| Cancer | 1 (4) |
| Infection | 1 (4) |
| Iatrogenic | 1 (4) |
| Mean distances to health services | Mean, km |
| General practitioner (primary health care) (n = 25) | 15 |
| In-center dialysis unit (n = 16) | 62 |
| Nephrologist (n = 28) | 107 |
| Home dialysis training center (n = 21) | 220 |
| Transplantation center (n = 21) | 447 |
| Interview setting | |
| Zoom (online) | 15 (54) |
| Telephone | 8 (28) |
| In person | 5 (18) |
AUD, Australian dollar.
Figure 1.
Thematic schema.
Table 2.
Supporting quotations
| Theme | Quotations |
|---|---|
| Encumbered by transportation hardships | |
| Burdening family and friends | “I started rounding up family and friends to take me, I hated doing that because everyone works. But my sister in particular took a lot of time off work.” “I do drive myself, unless I’m feeling a bit crap. Then mom will come with me. She does come to most of my doctors’ appointments as well.” “As a single person it’s a bit different. If I had a partner, it would be easier. But I'm lucky to have an adult daughter, she's and I've had to rely on her to be able drive me to Tamworth for those appointments. So, she's working, so she's got to rearrange her schedule.” |
| Frustration at lack of transport options | “If I left my home and headed to XXX for dialysis by bus, I'd get there when the unit closed.” “Getting transport is stressful. If I didn't have my husband, I would not have been able to get to dialysis.” “We don't have really any public transport here. We have taxis, but in the city, you do have that.” |
| Heightened vulnerability to road trauma | “I had to go back to driving myself all the way. And I thought, I just can't do it. Can't do it anymore. I'm a danger on the road.” “We were having to stop halfway for my husband to have a rest, have a ten-minute sleep because it was getting dangerous.” “We thought it was a bit dicey trying to get to XXX. There is black ice, it was so slippery trying to get the unit.” |
| Unrelenting financial strain | “And then Taxis costed anywhere $70. One way.” “The only alternative is to go down in the wheelchair taxi. If I can't find anybody to take me, I can do the wheelchair taxi on my own. Last time I negotiated the cost for that, it was $600 both ways.” “I can't wrap my head around the travel form that you've got to fill out tasks. It's terribly complicated.” (to get reimbursements) |
| Looming threat of relocation | |
| Devastated by displacement | “So, I moved into [a larger town] full time. I ended up selling the farm, which was really difficult.” “We lived there for 30 years and unfortunately when I developed renal failure, we realized we'd have to be near a larger hospital. So, we had to sell of our farm. We left the town where all our friends were and moved, 180 kms away.” “My daughter's crying because we sold the family farm and we had to leave a lovely old home, it does impact and that impacts now on my life and impacts on your relationships.” |
| Uncertainty of sourcing appropriate accommodation | “It's difficult to get accommodation at or very close to the hospital.” “They have some apartments in a motel, and you go on a waiting list for those. So, they didn't come up initially. So, we just had to find private accommodation.” “There isn't really much for kidney patients and the place that we did stay at, wasn't very sanitary.” “You're feeling like a second-class person because they're coming to us. It's for cancer people (the accommodation). It's their priority.” |
| Resigned to periods of relocation | “I went to XXX to dialyse and because my husband was still working at XXX, I got a unit in XXX and he would come and see me on the weekends.” “So, we went down there [to the city] and 12 months later, finally got to come home.” “I went down there for 3 weeks, and I said, I'm getting really homesick, can I go home?” |
| Deprived of treatment and care | |
| Disadvantaged by limited options | “At the time we moved to XXX, there was not a kidney specialist in XXX. And there was no dialysis chair for me, so I had to do it at home.” “It is still difficult because there's no unit where I live. There is renal unit, but there's not a training centre.” “He used to do outreaches in XXX. He stopped that. But I choose to go there and see him because there are no other options.” |
| Isolated form centralized services | “We need to take my supplies [for peritoneal dialysis] from home because the local hospital didn't have anything. There was the continual hassle about did they have enough PD supplies? Only a couple of nurses who'd worked on the renal unit had an understanding of the sterilization issues surrounding peritoneal dialysis.” “It's two and a half hours down. Two and a half hours back. Then four to seven hours on dialysis.” |
| Unresolved psychological distress | “I know that they used to send up a palliative care doctor to see us, I didn't feel like it could help us. I felt like he could only give us antidepressants, but I think the grief and loss counselling would have helped.” “Just to have somebody to kind of vent to, to work out is this just the process or do I need more support? You know, am I coping or not coping?” “I don't know how many times I went to dialysis in those first couple of months thinking I was going to die. And worry about, who's going to look after my son. You know, if I had someone to explain the process to me a bit more, so I would have understood just to help put my mind at ease.” |
| Vulnerable without care availability | “When I presented to our local emergency department in the past and I used to just say, look, I've got Alport syndrome. You just need to ring the specialist [in the city]. don't even bother trying to do any other diagnosis, just ring on. And then they'd come back and say, ‘Can we talk to you? Cause we'd never actually seen anyone with Alport’s.’” “The GP’s really the single hardest thing. Cause basically they are fly in, fly out. You get a different one every time.” |
| Compounding economic consequences | |
| Coping with unexpected out-of-pocket expenses | “But for me to actually travel, it was a bit daunting because sometimes you just can't afford a hotel for five nights.” “How do I spread the tests out and get everything done as you need to be able to fit it into my budget. So, well I'll get that done this month and then I'll get something else done the next month. Um, because that was the only way that I could afford to pay for it. But that means you waiting longer to get all the assessments done. Well, you're not even on the list yet, so it's just putting more wait time on.” “We were able to get some money back from that, then it probably covered half of it. So, we were still 500 bucks a week out of pocket.” |
| Depletion of Income and leave | “I do have to take work off, it's far away, you need to take a couple of days to a week off. You just can't go there for one day and then that's it.” “Obviously, and I ran out of sick leave, so I've got to put more through insurance. I don't know if I'll get it.” “It took about nearly three years to get onto the disability pension.” “And then I didn't go back to work till after the kidney [transplant]. After being in ICU that long, I couldn't move.” |
| Confused by multiple information sources | |
| Despair at fragmented care | “The separation between XXX and XXX [hospitals], a sort of a divide. I was used to having care through there. So, I just thought it was easier to go to a local guy who might want to do it different.” “As a patient we've got complex needs. You're not just got one thing you've got multiple. You want to be within that same health service.” “I went to Brisbane for that. And you couldn't see why that couldn't be done in XXXX through telehealth.” |
| Fear of unfamiliar health settings and treatments | “You hear about the procedure, you people talk about what you do, but actually seeing it in person, like someone on a video showing you how they, what the catheter looks thought, I expected it to be a lot bigger than it was. And even in my head, after I'd been to the first sort of education and she showed me what it looks like, it didn’t seem so daunting.” “I was having a panic attack, because you are so anxious, but you don't always know what all your options are.” “She set up an indigenous kidney patient reference group. She wasn't actually my health worker up there. I just went along to the one session with me and there was only three of us. Yeah. And she showed us a video around PD and then started talking to me about PD, so that’s how I ended up on PD.” |
ICU, intensive care unit; PD, peritoneal dialysis.
Table 3.
Participant suggestions and considerations for practice
| Objectives to improve access | Participant suggestions |
|---|---|
| Minimize travel burden |
|
|
|
|
|
|
|
| Provide access to financial support |
|
|
|
|
|
| Minimize need for relocation |
|
|
|
|
|
|
|
| Provide support for patients in navigating multiple health services |
|
|
|
|
|
| Ensure access to psychological and support services |
|
|
|
|
|
|
CKD, chronic kidney disease.
Encumbered by Transportation Hardships
Burdening Family and Friends
Participants felt that they had no other option than to depend on family and friends to attend in-center dialysis, particularly when they are “too unwell” to drive themselves or unable to afford the costs incurred to travel to dialysis. Concern was expressed for those patients without family support as they believed them to be unfairly disadvantaged and “would not be able to do [dialysis] … as they are doing close to 400 kilometers just to do dialysis.” Rural kidney transplant recipients had no choice but to “round up friends and family” to take them to appointments, which could be “seven and a half hours drive, one way.”
Frustration at Lack of Transport Options
Some participants could not access public transport as it was either not available or they would arrive for dialysis “when the unit had closed.” In an emergency, for example fistula access issues, patients felt frustrated that the hospital would arrange their transport to receive treatment in a city hospital, but they had to find their “own way home.”
Heightened Vulnerability to Road Trauma
Participants were aware of the high risk of road accidents while traveling to and from hospital for dialysis, home dialysis training, and transplantation. Fatigue while driving home after dialysis, meant at times needing to stop on the side of the road for a “ten-minute sleep as it was getting dangerous.” Other potential hazards included animals, such as kangaroos, the presence of “black ice,” and the poor conditions of the roads in some rural locations. They had to drive despite feeling unwell as they had no other option.
Unrelenting Financial Strain
Those patients with limited or no other option relied on expensive taxis to attend dialysis. The “terribly complicated” process and paperwork to obtain reimbursement for travel expenses was challenging, often requiring assistance from a social worker. Tests, travel, and accommodation required upfront payments, which were at times difficult to find, and delays in reimbursement added substantially to financial difficulties experienced by rural patients.
Deprived of Treatment and Care
Isolated From Centralized Services
Participants felt anxious as they had to go to the urban center when they encountered complications with their fistulas, often at very short notice. Participants noted a lack of knowledge of peritoneal dialysis at their local rural hospitals, and thus felt vulnerable in having to take on the role as the “expert” in how to do a peritoneal dialysis exchange. For those patients who were being worked up for a transplant, it was a long, often delayed process in the rural setting, with those who could afford it, choosing to go to urban settings to finish “transplant work up that way” as it was quicker.
Unresolved Psychological Distress
For people commencing dialysis, they felt guilt, “grief and loss,” and trauma, indicating there was a “lack of access” to psychological support and social workers. Some were unable to attempt home dialysis owing to their “emotional and mental” state. One participant who moved to an urban dialysis center after a few years at satellite dialysis received weekly psychological support at the urban unit, which enabled her to successfully transition to home hemodialysis.
Vulnerable Without Care Availability
For patients who were transferred to an urban hospital to commence dialysis urgently, the process of returning home was complicated by shortages of dialysis chairs or staff in their local unit, with some unable to receive dialysis in their closest unit. Participants reported that if they had a permcath, local units were apprehensive on those being in place for too long, despite reassurances from specialists in the urban hospital. Specialist bariatric services were required, particularly for those wanting to be eligible for a kidney transplant, were sparsely available in rural areas, and often not covered by universal health care payment.
Disadvantaged by Limited Options
Patients in rural locations without satellite dialysis services had to travel long distances or to sell their home and relocate permanently for dialysis. Owing to limited availability of dialysis chairs in some rural services, moving to a larger rural center did not guarantee a dialysis chair there. Some believed that home dialysis was “too much trouble,” too invasive, and would add to sense of isolation they already experienced. Some expressed concern that transplantation was not “mentioned” by their clinicians in a timely way and patients living “too far away from anything [dialysis unit], every other option [other than transplant] means we have to sell” and relocate. They believed the delay contributed to the difficulty of completing workup for transplantation.
Confused by Multiple Information Sources
Despair at Fragmented Care
The lack of availability of general practitioners in rural communities that predominantly relied on “fly in, fly out” locums disrupted peace of mind among patients, with most preferring to talk to their nephrologist. For those with comorbidities, their specialists were from multiple health services and locations and resulted in the patients receiving conflicting information. Some were confused when they felt that other non-nephrology specialists made erroneous judgment regarding their nephrology care. Patients receiving a transplant experienced differences in communication and priorities between their local hospital and transplant center, leaving them confused on whose advice to follow.
Fear of Unfamiliar Health Settings and Treatments
Participants felt extremely vulnerable when attending unfamiliar hospitals in an urban area. One participant reported receiving an “antibiotic that can kill me,” despite warnings on their medical history. They felt alone in the city, unwell, and away from staff and family to “look out for them,” and it was difficult to be in an urban care setting where they were “unknown” to clinicians. Indigenous patients relied on indigenous health workers especially at times of uncertainty and decision-making, particularly on choice of modality.
Compounding Economic Consequences
Depletion of Income and Leave
Participants and their caregivers needed substantial time off work to attend appointments and surgeries in centers located “far away.” They had to use their leave entitlements and income. Some families were able to take “long service leave early and at half pay,” but not all are afforded that option, with families taking years to recover from the financial drain. Transplant recipients, whose specialists provided outreach services to rural areas, expressed relief, “to take an hour or so” off work compared with multiple days required to attend urban appointments.
Coping With Unexpected Out-of-Pocket Expenses
Patients reliant on social security disability benefits did not have “money to splash around on accommodation” for home dialysis training. The burden of medication and supplies for home dialysis, often in addition to existing medical supplies, such as “pump supplies for diabetes” depleted their financial resources. Indigenous participants reported that “closing the gap funding” for medications had reduced their financial burden. For potential transplant recipients, a gap fee to access testing meant scheduling tests over several months to be able to “afford to pay for it,” adding to their anxiety and frustration to “getting on the list.”
Looming Threat of Relocation
Devastated by Displacement
Participants and their families made heartbreaking decisions on relocating as there was no in-center dialysis units within a 100-km radius or they had insufficient water on their farm to do home hemodialysis. Patients felt without choice and “sold the farm,” leaving friends and family to move closer to a dialysis unit. For those people able to do home dialysis or receive a transplant, time away for training or surgeries left them feeling “homesick,” particularly when separated from their children or partners.
Resigned to Periods of Separation
Participants spent lengthy periods of time apart from partners and family, placing strain on their relationships. For patients attending satellite dialysis units in another town, the ongoing travel meant that some families had to be split between the 2 towns, one partner living and working in one, whereas the other attended treatment and lived in another. Patients longed to be able to live in their home with their families to receive care.
Uncertainty in Sourcing Appropriate Accommodation
Difficulty in obtaining and affording hygienic accommodation in close proximity to the urban hospital was a “major concern.” Patients who were allocated accommodation that was primarily for rural patients with cancer felt guilty taking up spaces for “cancer people,” resulting in them “feeling like a second-class person” and wished more specific kidney friendly accommodation was available.
Discussion
Patients with CKD in rural communities face economic, logistical, and psychological obstacles to accessing dialysis and transplant, leaving them feeling vulnerable and confused.
They felt disadvantaged by the limited choices of treatment options and struggled to receive regular ongoing care, particularly in the primary health care setting. Participants feared relocation to larger dialysis or transplant centers and faced ongoing financial burden which was exacerbated by substantial transport and accommodation expenses. For those with no choice except to move, they experienced grief at the loss of friends, family, and homes as a result of the relocation. The ongoing financial outlay over many years leads to depletion of financial resources within households which was compounded by excessive leave from employment required by both the patients and their caregivers to attend appointments in urban areas. Ongoing grief and loss experienced at diagnosis and commencing dialysis affected their decision-making capacity with regard to treatment modality and relocation and noted the lack of psychological services to assist them to adjust at these difficult times. Family and friends played a crucial role for continued coping of patients with the sustained burden of treatment, especially travel over the years, owing to the lack of alternative transport options in rural communities.
Although the findings were broadly consistent across the participants, there were some differences particularly in relation to the modality of treatment sought, the proximity of dialysis units, the remoteness of residence, and the needs of indigenous patients and their families. Home dialysis training and transplant centers had the largest mean distances to travel for the participants (220 and 447 km, respectively), and as such these options were reported to add to the travel, relocation, and financial burden initially but reduced burden overall in the long term. The availability of in-center dialysis units decreases with increasing remoteness, which therefore limits access to this modality for the more remote patients.2,7 Participants with no satellite unit in their community and limited transport or family support to attend the closest unit experienced reduced options to relocation, home modalities, or transplantation. For indigenous patients, the presence of culturally appropriate care and interaction with indigenous health workers, at both their local and urban health centers, was crucial to assist them through the complexities of multiple health care settings, with particular assistance required on modality choice and education.
Disparities in outcomes and access to treatment for rural patients are reported in other areas of health, including cancer and coronary disease.35,36 They share many similar challenges, particularly geographic barriers, transportation concerns, decreased availability of specialist health professionals locally, out-of-pocket expenses, and reporting of vulnerability when in a foreign urban health care setting.36 Owing to the lifelong debilitating nature of CKD, presence of multiple comorbidities, combined with the dependence, burden, and frequency of dialysis and transplantation follow-up, these unrelenting health demands can continue with no hope of a “cure.”37
This study provides in-depth insights from rural patients from a diverse cross-section of the community regarding the barriers and enablers of their access to dialysis and transplantation. Nevertheless, there are some potential limitations. All participants were from rural areas of Australia, a high-income country with universal health care, so we are uncertain of the transferability of the findings beyond this setting. Furthermore, only 1 of the participants was from a non-English-speaking background. All participants were able to access a form of kidney replacement therapy, though this was not always their treatment of choice.
In many nations, the out-of-pocket costs borne by patients are increasing despite the presence of universal health care.38 For rural patients, this is magnified with substantial additional costs than those faced by urban patients, particularly for transportation, accommodation, and relocation if required, and further compounded by excessive leave requirements, to attend appointments and surgeries.18,39,40 There is a scarcity of information available as to the extent of rural financial hardship in people with CKD, and this requires further research, especially to evaluate the impact the financial hardship exerts on decision-making and access to all forms of treatment.41
The extent of depression and anxiety in the CKD population has been discussed previously, though there is little in the way of research on rural populations and the ongoing impact that this has on their access to treatment, decision-making, and their quality of life.18,42,43 They face many stresses, including financial, “grief and loss,” and yet, there is limited opportunity to discuss with health professionals or other rural patients with CKD who can offer support or assistance throughout this time.44 Participants may benefit from referral to psychologists and social workers with appropriate awareness and training in CKD. More work is required to look at the impacts of these psychological issues, and its impact on access to dialysis and transplantation, and methods such as telehealth, that ensure it is delivered to the vast geographic spread of patients requiring it.45, 46, 47
Novel to this study are suggestions and considerations from the patient perspective, based on their lived experiences (Table 3). The suggestions cover a broad range of suggestions from increased telehealth, instigation of patient navigator and indigenous health workers specifically for patients with CKD, simplification of travel reimbursement schemes, and further research into the models of care for rural patients with CKD, especially satellite services in communities with no current availability. It is essential when revising rural service delivery models to improve access for rural patients, that patients lead, or at a minimum, be a part of the redesign process, and that patient-prioritized outcomes are comparable with urban patients.48,49 Examples of this can be found in health services models introduced by the Northern Territory Government, Purple House, and Manitoba's Local Centre Program, providing dialysis services to remote areas; however, there are ongoing issues of access and equity in relation to transplantation.50,51 The Purple house has led the way in innovative models of service delivery, is indigenous consumer led, and has bought changes in health policy and funding with the introduction of a new Medicare Benefits Schedule item for dialysis treatment in a very remote location.50
CKD and its ongoing treatment regimens place an exhausting burden physically, financially, and psychologically on rural patients. There are many barriers to access reported by patients, including geography, especially transport, the need for relocation owing to limited availability of some essential services, the ongoing financial stress, and out-of-pocket expenses, together with the difficulties of navigating the complexities of multiple health services. To achieve equity and improved health outcomes for rural patients with CKD, barriers to dialysis, transplantation, and psychological services in this population require addressing through policy and alternate models of health service delivery, in consultation with rural communities and those families affected by CKD.
Disclosure
NSR is supported by a National Health and Medical Research Council Postgraduate Scholarship (ID1190850). TG is supported by a National Health and Medical Research Council Postgraduate Scholarship (ID1169149). AT is supported by a National Health and Medical Research Council (NHMRC) fellowship (1106716). All the other authors declared no competing interests.
Acknowledgments
The authors thank all the participants for their willingness and time to share their perspectives and experiences. With their written permission, the authors acknowledge the following, by name: Colin Ahoy, Kerry Armstrong, Janet Bailey, Nicole Barnes, Geoff Cutter, Karrin Davidson, Halley Griffin, Anthony Halstead, Maree Hayes, Justine Heaslip, David Hibbert, Kaye Kelly, Mark Lawlor, Chris Markham, Peter Marshall, Simone Monez, Peter Murko, Colleen Rockliff, Brad Rossiter, Ray Sambo, Paul Sanderson, Jason Size, Janet Stewart, and Katherine Widders. The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Appendix S1. Interview guide.
Supplementary Material
Appendix S1. Interview guide.
STROBE Statement (PDF)
References
- 1.United Nations 2018 revision of world urbanization prospects. Published May 16, 2018. https://www.un.org/development/desa/publications/2018-revision-of-world-urbanization-prospects.html#:∼:text=Today%2C%2055%25%20of%20the%20world's,increase%20to%2068%25%20by%202050 Accessed September 15, 2021.
- 2.Kashima S., Matsumoto M., Ogawa T., Eboshida A., Takeuchi K. The impact of travel time on geographic distribution of dialysis patients. PLoS One. 2012;7:e47753. doi: 10.1371/journal.pone.0047753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kotwal S., Gallagher M., Cass A., Webster A. Effects of health service geographic accessibility in patients with treated end stage kidney disease: cohort study 2000–2010. Nephrology (Carlton) 2017;22:1008–1016. doi: 10.1111/nep.12913. [DOI] [PubMed] [Google Scholar]
- 4.Bello A.K., Hemmelgarn B., Lin M., et al. Impact of remote location on quality care delivery and relationships to adverse health outcomes in patients with diabetes and chronic kidney disease. Nephrol Dial Transplant. 2012;27:3849–3855. doi: 10.1093/ndt/gfs267. [DOI] [PubMed] [Google Scholar]
- 5.Tonelli M., Klarenbach S., Rose C., Wiebe N., Gill J. Access to kidney transplantation among remote- and rural-dwelling patients with kidney failure in the United States [published correction appears in JAMA. 2009;301:2329] [published correction appears in JAMA. 2009;301:1882] JAMA. 2009;301:1681–1690. doi: 10.1001/jama.2009.545. [DOI] [PubMed] [Google Scholar]
- 6.Australian Institute of Health and Welfare Chronic kidney disease: regional variation in Australia. https://www.aihw.gov.au/reports/chronic-disease/chronic-kidney-disease-regional-variation-in-aust/contents/table-of-contents Published October 17, 2013. Accessed September 15, 2021.
- 7.Cheikh Hassan H.I., Chen J.H.C., Murali K. Incidence and factors associated with geographical relocation in patients receiving renal replacement therapy. BMC Nephrol. 2020;21:1–249. doi: 10.1186/s12882-020-01887-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rucker D., Hemmelgarn B.R., Lin M., et al. Quality of care and mortality are worse in chronic kidney disease patients living in remote areas. Kidney Int. 2011;79:210–217. doi: 10.1038/ki.2010.376. [DOI] [PubMed] [Google Scholar]
- 9.Tudor Hart J. The inverse care law. Lancet. 1971;297:405–412. doi: 10.1016/s0140-6736(71)92410-x. [DOI] [PubMed] [Google Scholar]
- 10.Beard J.R., Tomaska N., Earnest A., Summerhayes R., Morgan G. Influence of socioeconomic and cultural factors on rural health. Aust J Rural Health. 2009;17:10–15. doi: 10.1111/j.1440-1584.2008.01030.x. [DOI] [PubMed] [Google Scholar]
- 11.Andreasyan K., Hoy W.E. Renal-related deaths in Indigenous people in Queensland, Australia [published correction appears in Nephrology (Carlton). 2008;13:753-754] Nephrology (Carlton) 2007;12:514–519. doi: 10.1111/j.1440-1797.2007.00834.x. [DOI] [PubMed] [Google Scholar]
- 12.Ritchie S.D., Jo Wabano M., Beardy J., et al. Community-based participatory research with Indigenous communities: the proximity paradox. Health Place. 2013;24:183–189. doi: 10.1016/j.healthplace.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 13.Moist L.M.M.D., Bragg-Gresham J.L.M.S., Pisoni R.L.P., et al. Travel time to dialysis as a predictor of health-related quality of life, adherence, and mortality: the dialysis outcomes and practice patterns study (DOPPS) Am J Kidney Dis. 2008;51:641–650. doi: 10.1053/j.ajkd.2007.12.021. [DOI] [PubMed] [Google Scholar]
- 14.Klein M.G., Verter V., Moses B.G. Designing a rural network of dialysis facilities. Eur J Oper Res. 2020;282:1088–1100. [Google Scholar]
- 15.Gray N.A., Grace B.S., McDonald S.P. Peritoneal dialysis in rural Australia. BMC Nephrol. 2013;14:278. doi: 10.1186/1471-2369-14-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Hare A.M., Johansen K.L., Rodriguez R.A. Dialysis and kidney transplantation among patients living in rural areas of the United States. Kidney Int. 2006;69:343–349. doi: 10.1038/sj.ki.5000044. [DOI] [PubMed] [Google Scholar]
- 17.McGrath P., Holewa H. 'It's a regional thing': Financial impact of renal transplantation on live donors. Rural Remote Health. 2012;12 2144-2144. [PubMed] [Google Scholar]
- 18.Gunn K.M., Skrabal Ross X., McLoughlin M., McDonald S., Olver I. The psychosocial experiences and supportive care preferences of organ transplant recipients and their carers who live in regional Australia. Aust J Rural Health. 2021;29:92–105. doi: 10.1111/ajr.12693. [DOI] [PubMed] [Google Scholar]
- 19.Blumenthal S.J., Kagen J. The effects of socioeconomic status on health in rural and urban America. JAMA. 2002;287:109. [PubMed] [Google Scholar]
- 20.Dominello A., Howell M., Craig J.C., et al. Equity in national policies for Australians with kidney disease. Aust N Z J Public Health. 2021;45:370–375. doi: 10.1111/1753-6405.13096. [DOI] [PubMed] [Google Scholar]
- 21.Rogers A., Flowers J., Pencheon D. Improving access needs a whole systems approach. And will be important in averting crises in the millennium winter. 1999;319:866–867. doi: 10.1136/bmj.319.7214.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Douthit N., Kiv S., Dwolatzky T., Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129:611–620. doi: 10.1016/j.puhe.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 23.Tong A., Sainsbury P., Craig J.C. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 24.Welfare A. IoHa. Australia’s health 2018. Australia’s Health Series. 2018;No 16(Aus 221) https://www.aihw.gov.au/reports/rural-remote-australians/rural-remote-health Accessed September 15, 2021.
- 25.Axelrod D.A., Guidinger M.K., Finlayson S., et al. Rates of solid-organ wait-listing, transplantation, and survival among residents of rural and urban areas. JAMA. 2008;299:202–207. doi: 10.1001/jama.2007.50. [DOI] [PubMed] [Google Scholar]
- 26.Jan S., Leeder S.R., Leeder S.R. Falling through the cracks: the hidden economic burden of chronic illness and disability on Australian households. Med J Aust. 2012;196:29–31. doi: 10.5694/mja11.11105. [DOI] [PubMed] [Google Scholar]
- 27.Australian Institute of Health and Welfare Rural and remote health. https://www.aihw.gov.au/reports/australias-health/rural-and-remote-health Published July 23, 2020. Accessed September 15, 2021.
- 28.Scholes-Robertson N.J., Howell M., Gutman T., et al. Patients’ and caregivers’ perspectives on access to kidney replacement therapy in rural communities: systematic review of qualitative studies. BMJ Open. 2020;10:e037529. doi: 10.1136/bmjopen-2020-037529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Evans D.B., Hsu J., Boerma T. Universal health coverage and universal access. Bull World Health Organ. 2013;91 doi: 10.2471/BLT.13.125450. 546-546A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kulig J.C., Andrews M.E., Stewart N.L., et al. How do registered nurses define rurality? [published correction appears in Aust J Rural Health. 2009;17:350] Aust J Rural Health. 2008;16:28–32. doi: 10.1111/j.1440-1584.2007.00947.x. [DOI] [PubMed] [Google Scholar]
- 31.Miller R. More than “not urban”: seeking a quantifiable definition of rural. Berkeley Plan J. 2013;26:39–62. [Google Scholar]
- 32.Couper I.D. Rural hospital focus: defining rural. Rural Remote Health. 2003;3:205. [PubMed] [Google Scholar]
- 33.Australian Institute of Health and Welfare Rural, regional and remote health: a guide to remoteness classifications. https://www.aihw.gov.au/reports/rural-remote-australians/guide-to-remoteness-classifications/summary Published March 19, 2004. Accessed September 15, 2021.
- 34.Tong A., Winkelmayer W.C., Craig J.C. Qualitative research in CKD: an overview of methods and applications. Am J Kidney Dis. 2014;64:338–346. doi: 10.1053/j.ajkd.2014.02.026. [DOI] [PubMed] [Google Scholar]
- 35.Afshar N., English D.R., Milne R.L. Rural–urban residence and cancer survival in high-income countries: a systematic review. Cancer. 2019;125:2172–2184. doi: 10.1002/cncr.32073. [DOI] [PubMed] [Google Scholar]
- 36.Brundisini F., Giacomini M., DeJean D., Vanstone M., Winsor S., Smith A. Chronic disease patients’ experiences with accessing health care in rural and remote areas: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess S. 2013;13:1–33. [PMC free article] [PubMed] [Google Scholar]
- 37.Nordio M., Limido A., Maggiore U., Nichelatti M., Postorino M., Quintaliani G. Survival in patients treated by long-term dialysis compared with the general population. Am J Kidney Dis. 2012;59:819–828. doi: 10.1053/j.ajkd.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 38.Yusuf F., Leeder S. Recent estimates of the out-of-pocket expenditure on health care in Australia. Aust Health Rev. 2020;44:340–346. doi: 10.1071/AH18191. [DOI] [PubMed] [Google Scholar]
- 39.Newton J., Johnson C., Hohnen H., et al. Out-of-pocket expenses experienced by rural Western Australians diagnosed with cancer. Support Care Cancer. 2018;26:3543–3552. doi: 10.1007/s00520-018-4205-2. [DOI] [PubMed] [Google Scholar]
- 40.Ginetta S., Len K., Bruce M. Perspectives on health: experiences of First Nations dialysis patients relocated from remote communities for treatment. Can J Rural Med. 2003;8:19. [Google Scholar]
- 41.Newton J.C., Hohnen H., Johnson C.E., et al. ‘… If I don’t have that sort of money again, what happens?’: adapting a qualitative model to conceptualize the consequences of out-of-pocket expenses for cancer patients in mixed health systems. Aust Health Rev. 2020;44:355–364. doi: 10.1071/AH18250. [DOI] [PubMed] [Google Scholar]
- 42.Damery S., Brown C., Sein K., Nicholas J., Baharani J., Combes G. The prevalence of mild-to-moderate distress in patients with end-stage renal disease: results from a patient survey using the emotion thermometers in four hospital Trusts in the West Midlands, UK. BMJ Open. 2019;9:e027982. doi: 10.1136/bmjopen-2018-027982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nataatmadja M, Evangelidis N, Manera KE, et al. Perspectives on mental health among patients receiving dialysis. Nephrol Dial Transplant. Published online December 29, 2020. https://doi.org/10.1093/ndt/gfaa346 [DOI] [PubMed]
- 44.Scholes-Robertson N. The empty chair. Am J Kidney Dis. 2021;78:A11. doi: 10.1053/j.ajkd.2021.03.015. [DOI] [PubMed] [Google Scholar]
- 45.Meyer C., Becot F., Burke R., Weichelt B. Rural telehealth use during the COVID-19 pandemic: how long-term infrastructure commitment may support rural health care systems resilience. J Agromedicine. 2020;25:362–366. doi: 10.1080/1059924X.2020.1814921. [DOI] [PubMed] [Google Scholar]
- 46.Perle J.G., Langsam L.C., Randel A., et al. Attitudes toward psychological telehealth: current and future clinical psychologists’ opinions of internet-based interventions. J Clin Psychol. 2013;69:100–113. doi: 10.1002/jclp.21912. [DOI] [PubMed] [Google Scholar]
- 47.Khanal N., Lawton P.D., Cass A., McDonald S.P. Disparity of access to kidney transplantation by indigenous and non-indigenous Australians [published correction appears in Med J Aust. 2018;209:475] Med J Aust. 2018;209:261–266. doi: 10.5694/mja18.00304. [DOI] [PubMed] [Google Scholar]
- 48.Bate P., Robert G. Experience-based design: from redesigning the system around the patient to co-designing services with the patient. Qual Saf Health Care. 2006;15:307–310. doi: 10.1136/qshc.2005.016527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hughes J.T., Freeman N., Beaton B., et al. My experiences with kidney care: a qualitative study of adults in the Northern Territory of Australia living with chronic kidney disease, dialysis and transplantation. PLoS One. 2019;14 doi: 10.1371/journal.pone.0225722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brown S. Remote possibilities: from a Pintupi dream to Medicare funding. Ren Soc Australas J. 2018;14:105–107. [Google Scholar]
- 51.Gorham G., Majoni S.W., Lawton P., et al. Interesting times—evolution of dialysis in Australia’s Northern Territory (1980–2014) Ren Soc Australas J. 2018;14:108–117. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.