Abstract
Treatment options for massive irreparable rotator cuff tears continue to evolve. Recently bursal acromial reconstruction (BAR) has been described as an additional option to reduce pain and improve comfort. As originally described, an acellular dermal allograft is secured to the underside of the acromion as an interposition graft. We describe a modified technique that facilitates suture passage, reduces entanglement, and optimizes contact between the bone-graft interface.
Technique Video
The modified technique for bursal acromial reconstruction is demonstrated.
Introduction
Patients suffering from irreparable rotator cuff tears often experience discomfort resulting from superior translation of the humeral head, as it meets the undersurface of the acromion.1 Surgeons have been exploring treatment options to prevent superior translation by introducing capsular reconstructive methods, such as superior capsular reconstruction (SCR), acellular dermal allograft interfaces (BAR), or spacers (balloon spacer implantation), to prevent contact between the two aforementioned surfaces. SCR requires longer surgical times, more implants, and is technically more difficult to perform. Balloon spacer implantation is not widely accepted in the United States. Thus, BAR has potential advantages over these techniques.
In the original BAR technique, an acellular dermal allograft is secured to the undersurface of the patient’s acromion arthroscopically. Before the graft can be secured, a bursectomy and debridement of the acromion are performed to enhance healing at the bone–graft interface. However, suture management can be challenging with this technique. By modifying the suture placement and using arthroscopic portals, the procedure is simplified, and contact between the acellular dermal allograft (ADA) to the acromion can be improved.
Surgical Technique
The surgical technique is demonstrated in Video 1.
Patient Positioning and Subacromial Preparation
The patient is positioned in the beach chair position and prepared for standard shoulder arthroscopy. Surface landmarks are marked. A diagnostic arthroscopy is performed as well as treatment of any concomitant pathology. Standard arthroscopic viewing and working portals are established. Fig 1 identifies the portals used for the surgical procedure: we start by establishing the posterior (P) anterolateral (AL), posterolateral (PL), and lateral (L) portals as working portals. Once the portals are established, complete bursectomy is performed, the acromion is then debrided until adequate bleeding bone is exposed. Aggressive acromioplasty should be avoided and the coracoacromial (CA) ligament and coracoacromial arch should be preserved. Debridement of the greater tuberosity is also performed to allow a smoother articulating surface on the humeral side, as necessary.
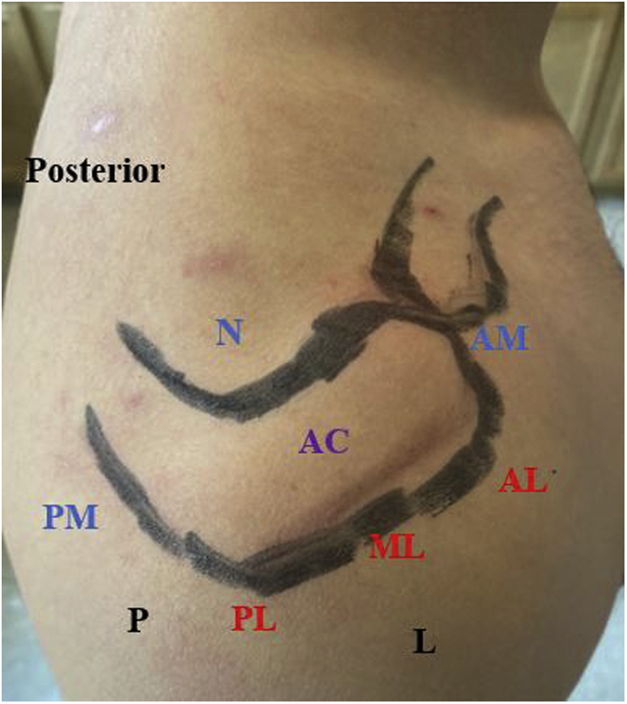
Fig 1.
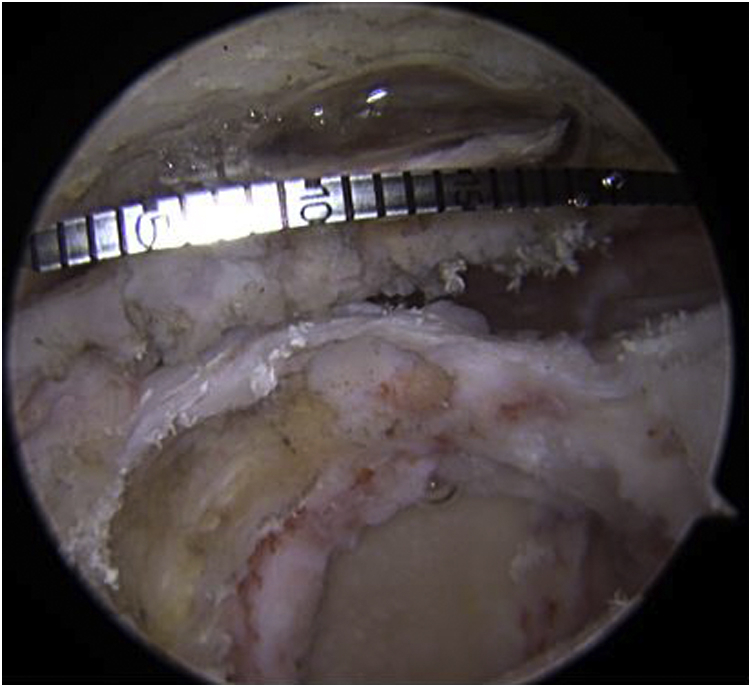
Arthroscopic view, right shoulder, beach chair position, from the posterolateral portal, measurements of the acromion must be taken prior to establishment of percutaneous portals. An arthroscopic measuring device is seen entering the posterior medial (PM) portal directed toward the anterior medial (AM) portal to measure the length of the medial side of the acromion.
Graft Measurement and Portal Preparation
Next, the acromion is measured in both anterior/posterior and medial/lateral dimensions using an arthroscopic measuring device (Arthrex, Naples FL) (Fig 1). Measurement of the length of the acromion in the anterior to posterior direction is performed via the P portal toward the anterior edge of the acromion perpendicular to the medial to lateral axis, and measurement of the acromion in the medial to lateral direction is performed from the L portal toward the medial aspect of the acromion, perpendicular to the anterior to posterior axis of the acromion.
Necessary accessory portals used in addition to standard subacromial arthroscopy portals include the mid-lateral (ML), acromioclavicular joint (AM), posterior medial (PM), posterior lateral (PL) and Neviaser (N), portals. These portals facilitate graft passage throughout the procedure. The superior central entry point for the drill holes through the acromion is not a “portal” and will be labeled acromial (AC). Essentially, there are three medial portals, and three lateral portals each of which will contain a corresponding suture on the graft. In addition, there are two central sutures, which will be tied through the acromial (AC) to two drill holes on the superior aspect of the acromion. Surface landmarks for these portals are shown in Fig 2.
Fig 2.
External view, right shoulder, posterior is to the left. External portal locations for the bursal acromial reconstruction technique. External standard portals are indicated in black as posterior (P), and lateral (L). Lateral portals are indicated in red as posterolateral (PL), midlateral (ML), anterolateral (AL). Medial portals are indicated in blue as posteromeidal (PM), Neviaser (N), and anteromedial (AM). The acromial portal (AC) is indicated in purple.
The three medial portals from anterior to posterior are: 1) the AM located just anterior to the acromioclavicular joint, 2) the N portal located in the notch between the posterior aspect of the acromioclavicular joint and the scapular spine, and 3) the PM portal, which is located medial and superior to the standard posterior viewing portal (P). The AM and N portals are in the same locations typically used to perform an arthroscopic distal clavicle excision. The PM portal is percutaneous and unique to this procedure and is localized with a spinal needle prior to portal creation.
The three corresponding lateral portals from anterior to posterior are: 1) the standard AL portal located at the anterolateral edge of the acromion, 2) the ML portal located just superior to the standard lateral working portal, and 3) the PL portal located at the posterolateral edge of the acromion.
The AC entry point, centered over the midbody of the acromion superiorly, is used for creating two 2.0-mm drill holes. Drilling is first performed anteriorly under direct arthroscopic visualization. After drilling a wire loop (Suture Passing Wire, Arthex, Naples, FL) is then inserted through the drill hole and retrieved with a KingFisher (Arthex) via the AL portal. The tail of a passing suture (Ethibond, GF Mersons Limited, Bridgewater, NJ) is then placed in the wire loop and passed through the drill hole. The process is then repeated through a separate drill hole located approximately 1 cm away posteriorly and passing Ethibond suture is colored and docked in PL portal. These sutures will be used to pass the two ends of the SutureTape placed in a mattress fashion in the central portion of the graft. Once these have been passed and tied, they will provide central reduction of the ADA onto the debrided acromion.
Lastly, a 12 × 4 mm soft cannula (PassPort Button Cannula, Arthrex) is placed at the AL portal in preparation for graft passage through this portal. This device assists in graft passage because it is flexible, relatively short, and prevents soft tissue bridges that may inhibit graft and suture passage.
Graft Preparation
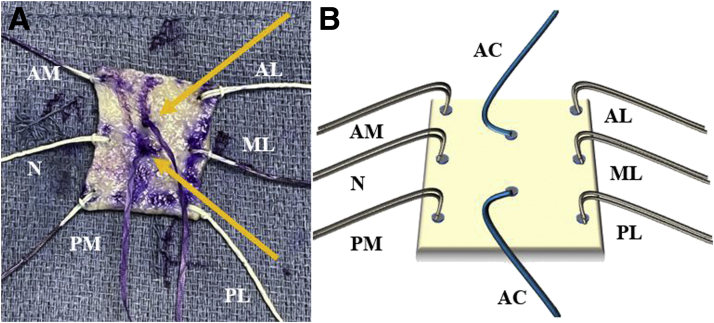
When considering the preparation of an ADA, standard graft sizing (35 × 25 mm) may be used for most patients. However, measurement of the acromial surface area should be made to ensure proper sizing of the graft, similar to the technique for superior capsular reconstruction. Placement of sutures is demonstrated in Fig 3. Six cinched FiberSnares (Arthrex) are placed evenly around the borders of the allograft. Passage of suture through the ADA can be accomplished with a suture passing device (SutureLasso, Arthrex). A SutureTape is passed in a mattress fashion at the center of the graft.
Fig 3.
(A) Open view, acellularvdermal allograft superior view demonstrating the appropriate sutures for graft preparation prior to graft passage. The two central sutures are colored purple and are marked with yellow arrows. (B) Schematic of the dermal allograft prior to graft passage with sutures plaed for passage through the corresponding portals. Acromial (AC). Latearl portal sutures are anterolateral (AL), midlateral (ML), and posterolateral (PL). Medial portal sutures are anteromedial (AM), Neviaser (N), and posteromedial (PM).
Graft Passage
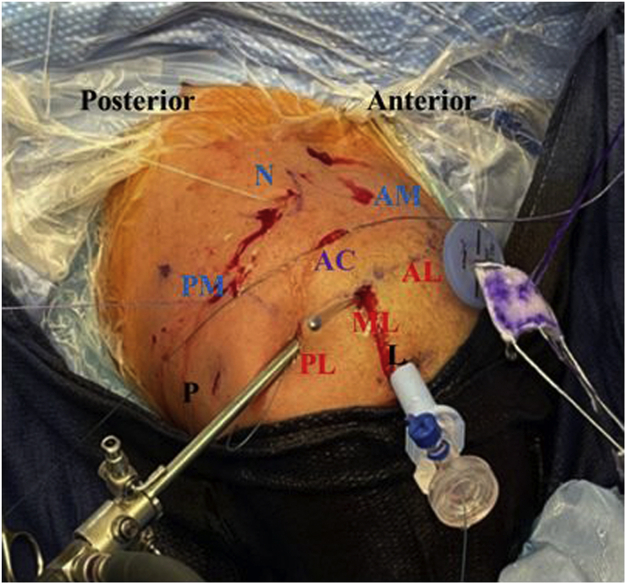
The completed graft is placed on a blue towel in the anatomic position in which it will be placed in the shoulder adjacent to the AL portal. A suture grasper is used to retrieve the corresponding sutures from the medial side of the graft to their corresponding medial portals: AM, N, and PM. Suture passage is performed sequentially to mitigate the risk of entanglement of the sutures. Final suture position prior to graft passage is demonstrated in Fig 4.
Fig 4.
Open view right shoulder, beach chair position, posterior is to the left. The graft is seen entering the anterolateral (AL) portal). The arthroscope is viewing from the posterolateral portal (PL). Medially based reduction sutures from the graft are docked out the corresponding posteromedial (PM), Neviaser (N), and anteromedial (AM) portals. The central sutures from the graft will be shuttled with the ethibond passing sutures through the acromial portal (AC). The remaining lateral sutures seen to the right of the image will be retrieved via the posterolateral (PL), midlateral (ML), and anterolateral (AL) portals once the graft is fully inserted into the shoulder.
Just prior to the graft being placed into the shoulder, a suture grasper is used to retrieve the more posterior of the two central SutureTape limbs out the AL portal. This process is repeated with the more anterior limb, which is taken out the same AL portal. The previously passed Ethibond sutures are then tied into a loop and used to shuttle the SutureTape limbs out of the two AC drill holes. Traction on these suture limbs reduces the graft centrally and will improve visualization for subsequent steps.
A specialized Back Grasper (Arthex) is used to grasp the central medial portion of the graft. This device provides a rigid pushing force, which is assisted by sequentially pulling on the three medial cinched FiberSnares. The remaining laterally based FiberSnare graft cinched sutures are then retrieved to their corresponding lateral portals, AL, ML, and PL with a suture grasper. Final suture tying can then commence.
The central SutureTapes are tied first with an arthroscopic knot pusher through the AC drill holes. A crossing pattern is then used to secure the six FiberSnares to each other. Ultimately, the AM FiberSnare will be tied to the PL, the ML to the N, and the AL to the PM. This pattern places the subcutaneous knots first superiorly, posterolaterally, medially, and posteromedially.
In each case a suture grasper is introduced from one end and is maneuvered subcutaneously over the superior aspect of the acromion. It will exit the corresponding opposite portal (i.e., AM to PL), where the suture tail can be grasped and retrieved. These sutures can then be tied to each other through the medially based portal with an arthroscopic knot-tying device. The AL to PM portal is secured last, and the Passport cannula is removed to allow easier suture retrieval of the final lateral suture.
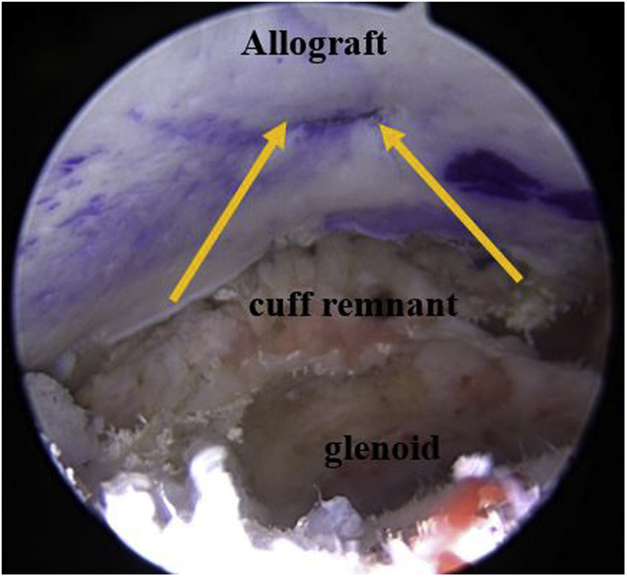
The final construct is demonstrated in Fig 5.
Fig 5.
Arthroscopic view of right shoulder, while patient is in the beach chair position. Final construct and alignment of acellular dermal allograft are secured to undersurface of acromion. Acromial sutures are indicated with yellow arrows.
Postoperative Care and Rehabilitation
Even though treatment regiments may be individualized on the basis of their healing ability and level of activity, postoperative rehabilitation goals follow simple guidelines, such as the preservation of flexible movements within the joint, prevention of shearing or tearing of the dermal allograft, and eventual strengthening of both the deltoid and rotator cuff muscles.
General guidelines include the restriction of active range of motion (AROM) for the first 3 weeks, while encouraging patients to remain in a sling during this initial phase. Lateral passive rotation should begin as soon as possible following the completion of the surgery. AROM nonresistance open chain exercises are advised at week 4 through week 6. Following week 6, patients can continue their open chain exercises but may add resistance for further strengthening of supportive rotator cuff and shoulder accessory muscles.2
The pearls and pitfalls of this technique are summarized in Table 1.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Appropriate patient selection would entail choosing patients who may not be candidates for reverse shoulder arthroplasty or superior capsular reconstruction. | Inadequate tension when tying knots in the subcutaneous layer may lead to a loss of tension across the allograft, ultimately causing it to sag, which may impact healing and incorporation. |
| Minimal acromioplasty should be performed to reduce the risk of acromial fracture. | Early range of motion and cyclical loading may lead to knot failure and graft displacement, which could cause early failure. |
| The coracoacromial ligament and arch should be left intact to prevent anterior superior escape and mitigate the risk of complication in the care of revision surgery. | |
| The addition of two portals for SutureTape management lowers the probability of suture entanglement. |
Discussion
Massive irreparable rotator cuff tears continue to be problematic for the active, elderly population and their treating orthopedic surgeon. Determining correct indications and patient selection is critical (Table 2). While certain surgical treatments have gained popularity, including superior capsular reconstruction (SCR), balloon spacing, and reverse shoulder arthroplasty (RSA), none of these treatments is ideally indicated for all patients. The ideal candidate for BAR is an elderly patient who is most likely over the age of 75, has a massive irreparable rotator cuff tear, and is not a good candidate for reverse shoulder arthroplasty. Shared decision making should guide a detailed conversation with the patient about the risks and benefits of various treatment options. Patients should be informed that currently, there is limited evidence to support BAR, and peer-reviewed literature is evolving.
Table 2.
Decision-Making Algorithm Table for the BAR Technique and Other Associated Procedures
| Age <60 Years | Age 65-75 Years | Age >75 Years | Infraspinatus | Osteoarthritis | Compensated | Treatment Option |
|---|---|---|---|---|---|---|
| ✓ | X | X | If supraspinatus is absent, rotate graft. | None | X | SCR + BAR |
| ✓ | ✓ | ? | Present | Mild | ✓ | SCR |
| X | X | ✓ | + / − | Mild | ✓ | BAR |
| X | X | ✓ | N/A | Mild | X | RSA |
| X | ? | ✓ | N/A | Severe | + / − | RSA |
BAR, bursal acromial reconstruction; N/A, not applicable; RSA, reverse shoulder arthroplasty; SCR, superior capsular reconstruction.
SCR was first introduced in 2012 by Mihata et al. and has grown in popularity with evolving techniques and grafts.3 Mihata’s early results showed excellent promise using a fascia lata autograft with American Shoulder and Elbow Surgeons (ASES) scores improving from 23 to 92 and recently reported maintained positive results at 5 years postoperatively.4,5 Techniques for SCR have continued to evolve since being introduced and have further developed to use dermal allografts, which significantly reduces donor site morbidity.6, 7, 8 However, SCR is not ideal for all patients. This procedure requires either intact or at least repairable infraspinatus and subscapularis tendons, involves an extensive recovery, and is not immune to failures due to the fastening of multiple anchors required for fixation.9 These fixation concerns are only amplified in elderly patients who often harbor poor anatomical qualities and bone health. SCR is also a technically complex and time-consuming procedure, which could be seen as beyond the practice of many surgeons. While SCR is an increasingly used option for irreparable rotator cuff tears, it is not always the best treatment option for all patients. Specifically, elderly patients with particularly lower-demand lifestyles may struggle with the recovery and may not have clinical healing of the graft, which can affect clinical outcomes.
The implementation of subacromial copolymer balloon spacers to treat irreparable rotators cuff tears is still in clinical evaluation and remains under review. Wright has described positive results using a copolymer balloon filled with saline to create a space between the humeral head and acromion, which ultimately reduces the forces across the glenohumeral joint.10 This procedure does not involve debridement of the acromion, nor does it require any general anesthesia. Another study found balloon spacer implementation can be technically simple and have favorable patient outcomes, but currently, the long-term efficacy of the procedure remains undetermined.11 As described by Wright, another pitfall is the limitation of the surgeon’s view.10 A final consideration is this procedure is not Food and Drug Administration-approved at this time for patients in the United States.
In elderly patients with significant glenohumeral arthritis and in reasonable medical condition, RSA has become an excellent option with good clinical outcomes.12,13 Even though patients who have received RSA have experienced respectable positive outcomes and recoveries, not all elderly patients may be good candidates for undergoing a shoulder arthroplasty. This may be because of either their medical comorbidities or simply a desire to avoid arthroplasty. Consequently, there is still a population of patients with irreparable rotator cuff tears who may not be good candidates for either SCR or RSA, and there remains a need for additional treatment options for irreparable rotator cuff tears, particularly, for the lower-demand population.
Comparison of Original and Modified BAR Technique
Use of an acellular dermal allograft is effective to treat symptoms experienced by patients suffering from irreparable rotator cuff tears. However, the previously described technique for placement for SutureTapes and FiberSnares may pose complications for surgeons when attempting to secure the graft to the undersurface of the acromion. This complication can increase operation times. Additionally, this complication may cause the BAR technique to be considered as more technically challenging to surgeons who are not experienced with its use. Our method using two centrally placed sutures with alternating FiberSnares prevents suture entanglement and maintains stability of the ADA to the undersurface of the acromion.
Conclusion
This technique demonstrates a modified technique, which may facilitate graft passage and suture management in performance of BAR for appropriately indicated patients.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.O, S.M., and H.L. has shared article processing fees from Mammoth Orthopedic Institute Research Foundation. B.G. has received financial support for research and scholarly activities from the Mammoth Orthopedic Institute and has received medical education from Reno Regenerative Medicine and Mammoth Sports Medicine. He has received research support, outside the submitted work, from Arthrex. He has shared article processing fees from the Taos Orthopedic Institute Research Foundation. He is a member of the Clinical Advisor Board of Smart Medical Devices, as well as a member of AANA committees and editorial board member of the Arthroscopy Journal. He owns stock in ROM3 and Doximity. D.G. has received grants from Arthrex, Medacta, Stryker, Smith & Nephew, Donjoy, and Breg. He has shared article processing fees from Mammoth Orthopedic and Institute Research Foundation. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The modified technique for bursal acromial reconstruction is demonstrated.
References
- 1.Ravenscroft M., Barnes M.W., Muench L.N., Mazzocca A.D., Berthold D.P. Bursal acromial reconstruction (BAR) using an acellular dermal allograft as a surgical solution for the treatment of massive irreparable rotator cuff tears. Arthrosc Tech. 2021;10:e877–e885. doi: 10.1016/j.eats.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Curtis D.M., Pullen W.M., Helenius K., Freehill M.T. The evolution and role of the bursal acromial reconstruction. Video J Sports Med. 2021;1 26350254211001367. [Google Scholar]
- 3.Mihata T., McGarry M.H., Pirolo J.M., Kinoshita M., Lee T.Q. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am J Sports Med. 2012;40:2248–2255. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 4.Mihata T., Lee T.Q., Watanabe C., et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 5.Mihata T., Lee T.Q., Hasegawa A., et al. Five-year follow-up of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. J Bone Joint Surg Am. 2019;101:1921–1930. doi: 10.2106/JBJS.19.00135. [DOI] [PubMed] [Google Scholar]
- 6.Hirahara A.M., Adams C.R. Arthroscopic superior capsular reconstruction for treatment of massive irreparable rotator cuff tears. Arthrosc Tech. 2015;4:e637–e641. doi: 10.1016/j.eats.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Denard P.J., Brady P.C., Adams C.R., Tokish J.M., Burkhart S.S. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy. 2018;34:93–99. doi: 10.1016/j.arthro.2017.08.265. [DOI] [PubMed] [Google Scholar]
- 8.Loy B.N., Owen M.T., Reid J.B., III, Guttmann D. Technique for double row superior capsule reconstruction with dermal allograft. Arthrosc Tech. 2020;9:e91–e96. doi: 10.1016/j.eats.2019.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mihata T., Lee T.Q., Hasegawa A., et al. Arthroscopic superior capsule reconstruction for irreparable rotator cuff tears: comparison of clinical outcomes with and without subscapularis tear. Am J Sports Med. 2020;48:3429–3438. doi: 10.1177/0363546520965993. [DOI] [PubMed] [Google Scholar]
- 10.Wright M.A., Abboud J.A., Murthi A.M. Subacromial balloon spacer implantation. Curr Rev Musculoskel Med. 2020;13:1–8. doi: 10.1007/s12178-020-09661-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stewart R.K., Kaplin L., Parada S.A., Graves B.R., Verma N.N., Waterman B.R. Outcomes of subacromial balloon spacer implantation for massive and irreparable rotator cuff tears: A systematic review. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119875717. 2325967119875717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mulieri P., Dunning P., Klein S., Pupello D., Frankle M. Reverse shoulder arthroplasty for the treatment of irreparable rotator cuff tear without glenohumeral arthritis. J Bone Joint Surg Am. 2010;92:2544–2556. doi: 10.2106/JBJS.I.00912. [DOI] [PubMed] [Google Scholar]
- 13.Petrillo S., Longo U.G., Papalia R., Denaro V. Reverse shoulder arthroplasty for massive irreparable rotator cuff tears and cuff tear arthropathy: A systematic review. Musculoskel Surg. 2017;101:105–112. doi: 10.1007/s12306-017-0474-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The modified technique for bursal acromial reconstruction is demonstrated.
The modified technique for bursal acromial reconstruction is demonstrated.