Abstract
Achilles tendinopathy is a common inflammatory condition of the Achilles tendon prevalent in the athletic population in which patients present with pain, swelling, and reduced performance exacerbated by physical activity. Operative intervention using either open or percutaneous approaches has traditionally been performed after failure of nonoperative treatment, but less invasive modalities that include endoscopic approaches have been increasingly used. This Technical Note highlights our technique for Achilles paratenon needle tendoscopy in the wide-awake office setting, with accompanying indications for use, advantages, and technical pearls.
Technique Video
Operative technique showing needle tendoscopy of Achilles tendon in left ankle. Portal placement and diagnostic tendoscopy are shown.
Achilles tendinopathy is a common pathology in the athletic population that can present in either an acute or chronic fashion.1 The Achilles tendon measures roughly 12 to 15 cm long and represents the confluence of the aponeuroses of the soleus and gastrocnemius muscles. The conjoined tendon from these 2 muscle groups rotates approximately 90° such that the tendinous portion derived from the soleus inserts anteromedially on the calcaneal tuberosity and the gastrocnemius tendon inserts more posterolaterally.2 At a point about 2 to 6 mm proximal to the calcaneal insertion, a watershed zone exists with limited blood supply to the Achilles tendon.3,4 The Achilles tendon is contained within a tunnel lined with visceral and parietal paratenon layers and is joined anteromedially by the plantaris tendon, which resides within the same fibrous tunnel before it inserts into the calcaneal tuberosity.
Although the etiology of Achilles tendinopathy is not fully understood, failure of proper healing of microtears has been suggested as an explanation for its pathogenesis.5 Chronic tendinopathy of the Achilles tendon is initially managed conservatively. Surgical treatment is usually considered for patients who present with persistent symptoms lasting longer than 3 to 6 months.6, 7, 8, 9 Previous studies have shown that tendoscopy may result in lower complication rates, more favorable clinical outcomes, and a quicker recovery compared with open surgery.10,11
The in-office needle arthroscopy (IONA) procedure was first introduced in the 1990s primarily as a tool for visualization and evaluation of anatomic structures under local anesthesia.12 Inferior image quality resulted in poor diagnostic accuracy and limited the use of IONA for surgical procedures.13 In recent years, the design of nano-arthroscopy devices has improved to a point at which the current system, using an optic chip at the camera tip and no inner rod lenses, provides image quality similar to that of conventional arthroscopy. Additionally, this IONA technology includes various burrs, punches, graspers, scissors, probes, shavers, and resectors that allow the identified pathology to be addressed directly at the time of in-office endoscopy. This improved technology system allows orthopaedic surgeons to perform and complete procedures at the bedside that were once only possible in a full operating room arthroscopy suite.
We present our technique and approach for needle tendoscopy using the Arthrex NanoScope nano-tendoscopy system (Naples, FL) in the treatment of Achilles tendinopathy. Advantages and disadvantages of this surgical technique are listed in Table 1. We share this Technical Note in the hopes that it will provide foot and ankle surgeons with the information needed to incorporate this technique into their own clinical practice. We recommend keeping in mind the advantages, disadvantages, and potential downsides when considering needle arthroscopy to treat a patient and have presented pearls and pitfalls (Table 2), as well as a step-by-step guide for performing our technique (Table 3).
Table 1.
Advantages and Disadvantages of Proposed Technique
| Advantages |
| Minimally invasive with ability to be performed in wide-awake office setting |
| Technique allows patient to undertake active role in understanding his or her pathology |
| Technique avoids placing patient in less desirable prone position while under general anesthesia |
| Potential for quicker recovery, improved cosmesis, decreased risk of iatrogenic injury, decreased blood loss, and decreased wound complications as would be experienced with prone positioning technique under general anesthesia |
| Direct visualization for diagnostic purposes may be better than MRI |
| Reduced cost and resource utilization |
| Disadvantages |
| Difficult to convert to open procedure if necessary |
| Potential for patient pain or discomfort during procedure |
| Learning curve |
MRI, magnetic resonance imaging.
Table 2.
Pearls and Pitfalls of Proposed Technique
| Pearls |
| Proper support of the patient’s head and nonoperative extremity should be ensured to limit movement during the procedure. |
| A mixture of lidocaine with epinephrine and bupivacaine should be used for injection into the tendon sheath to limit bleeding. |
| The patient should be encouraged to actively range the ankle to ensure the removal of all adhesions. |
| The portal sites should allow for movement of the camera (i.e., medial or lateral to the tendon). Central portal sites can cause difficulty in positioning the camera as a large gastrocnemius-soleus complex may obstruct movement of the camera. |
| Pitfalls |
| Iatrogenic injury to the medial neurovascular bundle during instrument insertion can occur if the instruments are inserted too medially. |
| Incorrect placement of the posterolateral portal can cause sural nerve injury. The surgeon should mark the sural nerve with a marking pen to visualize the course of the nerve especially proximally from medial to lateral. |
Table 3.
Step-by-Step Guide to Performing In-office Achilles Tendoscopy
| Step 1: The patient should be positioned comfortably in the prone position with the operative foot free. The relevant surface anatomy and anticipated portals are marked. The relevant borders are the medial and lateral Achilles borders and the intermalleolar line. Lateral and medial portals are also made relative to the area of presumed pathology over the Achilles tendon. |
| Step 2: Typically, a proximal-medial portal is made first to help visualize areas of tendinopathy. |
| Step 3: Blunt dissection is used to identify the paratenon layer. This layer can then be opened up sharply to access the desired space. |
| Step 4: A second portal is made laterally and is positioned based on the area of relative pathology as seen through MRI or direct visualization. The surgeon may use the transillumination from the medial scope to help locate the portal site. |
| Step 5: Once the surgeon sees the lateral border of the Achilles and paratenon, he or she uses the instrument and pushes medially to ensure a safe distance from the sural nerve. |
| Step 6: On the medial side of the Achilles, one may encounter the plantaris muscle that may run directly anteriorly or posteriorly to the Achilles. |
| Step 7: If the plantaris is adherent or inflamed, a small section can be removed with a biter and the proximal and distal ends can be shaved to prevent re-approximation. |
| Step 8: The shaver and camera portal sites can be exchanged as the pathology dictates. |
| Step 9: Debridement of the tendon circumferentially is performed, and the patient is asked to perform dorsiflexion and plantar flexion of the ankle. |
| Step 10: The procedure is completed after debridement of all adhesions, scarring, and degenerative tissue. |
| Step 11: Wound closure is performed and a soft dressing is applied as indicated. |
MRI, magnetic resonance imaging.
Surgical Technique
Preoperative Planning and Positioning
The entire tendoscopic procedure is performed in the office examination room (Video 1). The equipment for the procedure is organized on a Mayo stand that is draped in a sterile fashion and on which this equipment is organized (Fig 1). The monitor display for the video, as well as the accompanying equipment, is placed within the vicinity of the examination table. The monitor is placed such that it can be seen by both the operating surgeon and the patient. The patient is positioned comfortably on the examination table in the prone position with the foot over the edge of the bed in neutral dorsiflexion–plantar flexion. Soft padding is placed under the patient’s nonoperative extremity for comfort. The operating surgeon and assistant scrub and don standard operating room masks, gowns, and gloves. A solution of chlorhexidine gluconate mixed with isopropyl alcohol is used to sterilely prepare the patient’s ankle. Finally, the patient’s ankle is draped to provide a sterile work area on the examination table.
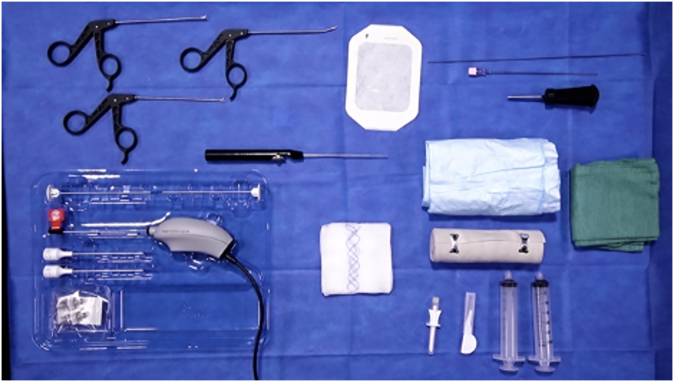
Fig 1.
The equipment for the procedure is organized on a Mayo stand that is draped in a sterile fashion and on which this equipment is organized.
Portal Placement
Standard posterior arthroscopic portals are used. A combination of 1% lidocaine and 0.25% bupivacaine hydrochloride is injected around the portal sites, which are made approximately 1 cm above to the fusiform swelling and 3 cm distal to the fusiform swelling (Figs 2 and 3).
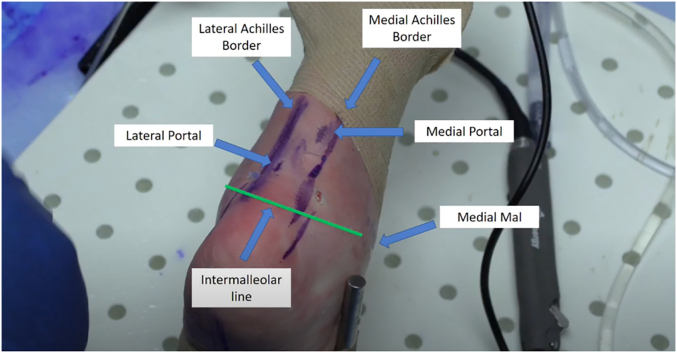
Fig 2.
Tendoscopic approach to the left ankle with the relevant surface anatomy markings and portal locations including the Achilles borders and the intermalleolar line, with the patient in the prone position. The portal sites are made relative to the location of the presumed pathology over the Achilles tendon. Mal, malleolus.
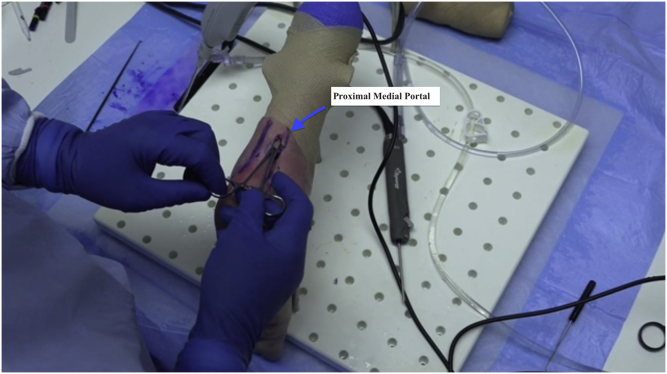
Fig 3.
Tendoscopic approach to the left ankle via the medial portal. Typically, a proximal medial portal is made first to help visualize areas of tendinopathy.
Operative Technique
A tiny incision measuring 2 mm is made using a No. 11 blade. The skin, followed by the subcutaneous tissue and fascia, is incised with special care taken to avoid the sural nerve. After dissection of the subcutaneous layers, the paratenon is visualized (Figs 4 and 5). The scope is placed between the paratenon and the tendon and subsequently advanced in a cephalad fashion. By use of gentle inflow, the space between the tendon and the tendon sheath is inflated and the scope is advanced medially, laterally, and circumferentially. Extensive cicatrization is often a sequela of Achilles tendinopathy and may be visualized along the Achilles and paratenon sheath (Fig 6). A plane can be established between the paratenon and the Achilles tendon using a 2.0-mm shaver. The patient at this time can be asked to perform dorsiflexion and plantar flexion of the ankle to maintain this plane. Debridement of the scar tissue between the Achilles tendon and paratenon is performed using a 3.0-mm resector. From the lateral portal, the surgeon can use transillumination for the scope in the medial portal to help locate the portal site. Generally, the surgeon should aim to place the portals so that they flank the area of the pathology. The portals should never be made midline because the instruments will constantly interfere with one another as the surgeon converges the instruments (Fig 7). Once the camera is through the lateral portal, the surgeon may place instrumentation through the contralateral portal and take down any visible adhesions. One must take special caution regarding the sural nerve on the lateral side because it may appear as a tendinous structure and thus may easily be mistaken for an anomalous band (Fig 8). After visualization of the lateral border of the Achilles and paratenon, the surgeon can use the instrumentation to proceed medially to ensure a safe distance from the sural nerve. From here, the surgeon can start addressing more superficial adhesions in the tendon and then direct the instrumentation to the undersurface of the Achilles tendon (Fig 9). Care should be taken during debridement not to damage the posterior tibial neurovascular bundle distally or the sural nerve proximally at the myotendinous junction. Typically, the inflamed paratenon and the plantaris on the medial side are pain generators in Achilles tendinopathy. Thus, after debridement of the inflamed paratenon, the plantaris can typically be seen tethered to the medial side of the Achilles tendon. Once the plantaris is identified, we use a 2.0-mm resector to debride the tendon to free the tethered connection between the plantaris and Achilles. After complete debridement, the patient is asked to perform dorsiflexion and plantar flexion of the ankle to show the absence of any remaining cicatrization of the Achilles tendon or adhesions between the paratenon and Achilles tendon (Video 1).
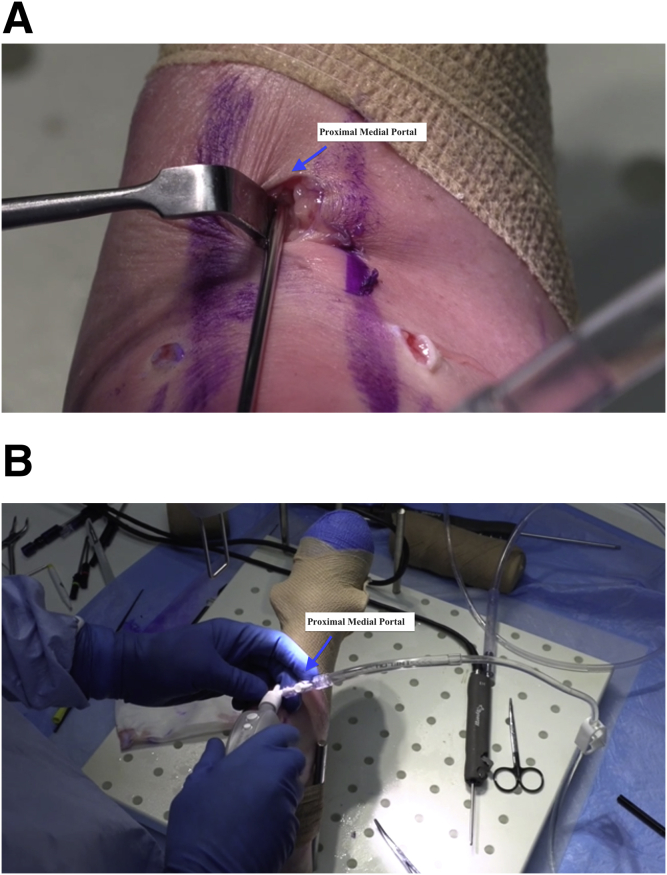
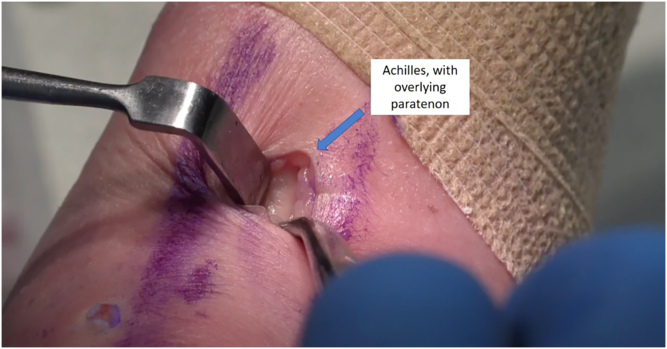
Fig 4.
Tendoscopic approach to the left ankle via the medial portal. (A) The scope is placed between the paratenon and the Achilles tendon and subsequently advanced in a cephalad fashion. (B) The tendon and the tendon sheath are inflated, and the scope is advanced medially, laterally, and circumferentially.
Fig 5.
Tendoscopic approach to the left ankle via the medial portal. Blunt dissection is used to identify the paratenon layer. This layer can then be opened up sharply to access the desired space. The Achilles tendon is typically located just under the skin, so identification of the subcutaneous tissue of the paratenon should be fairly easy. The surface view of the Achilles tendon is shown, with the overlying paratenon identified.
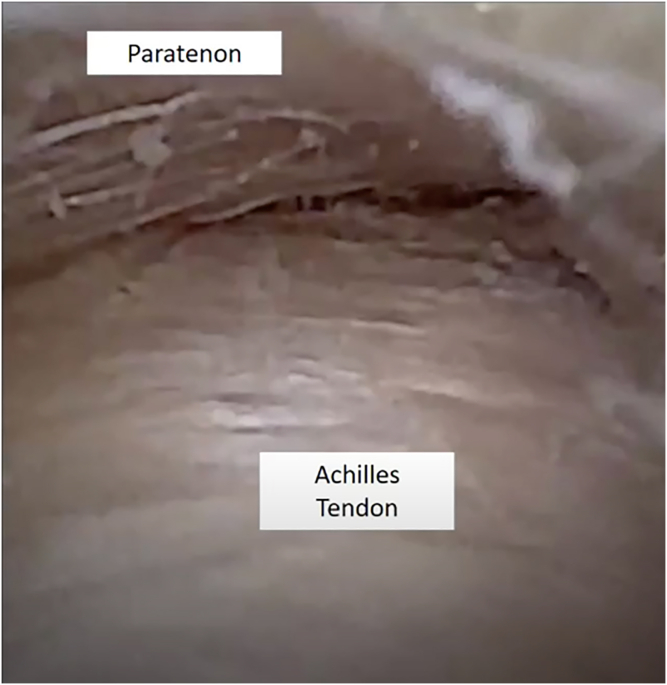
Fig 6.
Tendoscopic approach to the left ankle via the medial portal. Once the plane established between the paratenon and the Achilles tendon is identified, the surgeon may visualize the posterior border of the Achilles tendon and the paratenon on the top of the screen.
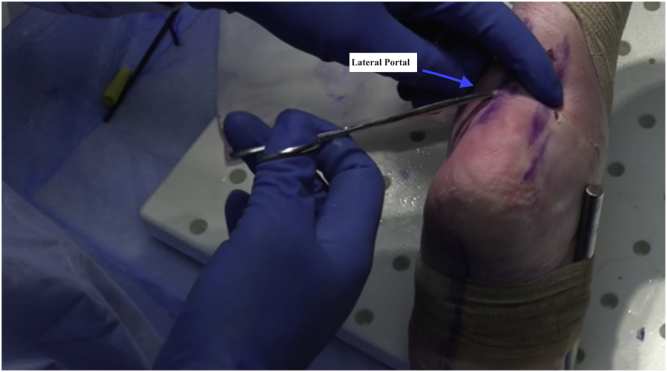
Fig 7.
Tendoscopic approach to the left ankle via the lateral portal. A second portal site is made relative to the area of presumed pathology based on magnetic resonance imaging and direct visualization. The surgeon can use transillumination for the scope in the medial portal to help locate the portal site. Generally, one should aim to place the portals so that they flank the area of the pathology. The portals should never be made midline because the instruments will constantly interfere with one another as the surgeon converge instruments.
Fig 8.
Tendoscopic approach to the left ankle via the lateral portal. Once the camera is through the lateral portal, the surgeon may place instrumentation through the contralateral portal and take down any visible adhesions. One must take special caution regarding the sural nerve on the lateral side because it may appear as a tendinous structure and thus may easily be mistaken for an anomalous band.
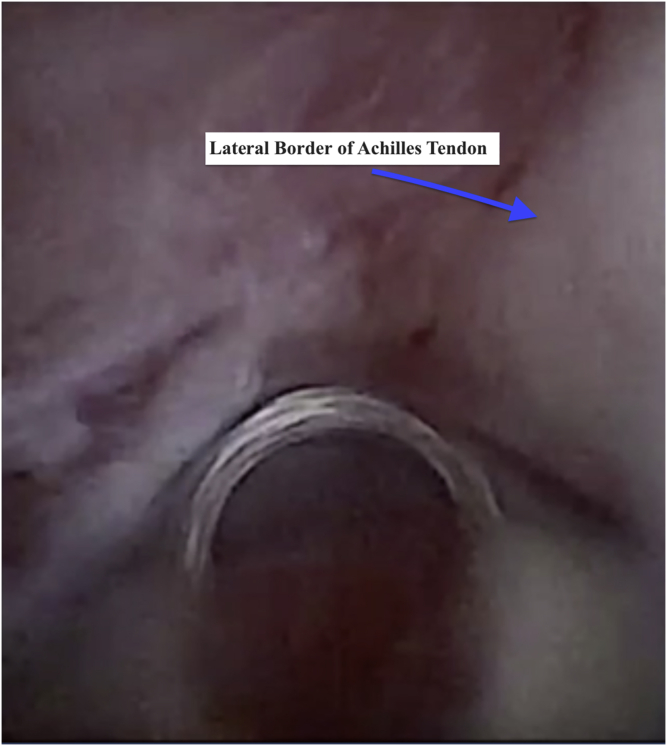
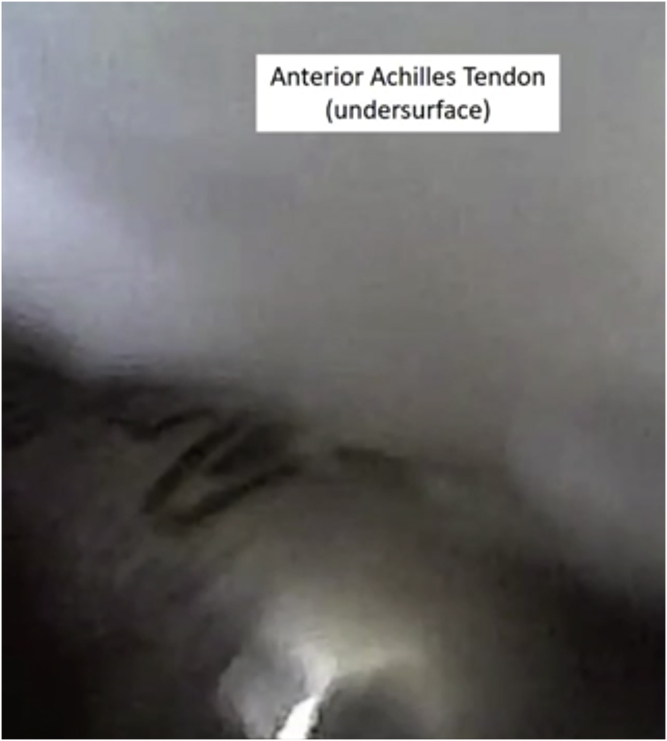
Fig 9.
Tendoscopic approach to the left ankle via the lateral portal. After visualization of the lateral border of the Achilles and paratenon, the surgeon can use the instrumentation to proceed medially to ensure a safe distance from the sural nerve. From here, the surgeon can start addressing more superficial adhesions in the tendon and then direct the instrumentation to the undersurface of the Achilles tendon.
The portals are now sealed with adhesive wound closure strips (Steri-Strip; 3M, Saint Paul, MN). A dry, sterile dressing and a compression bandage are applied.
Postoperative Protocol
Range of motion and weight-bearing exercises are encouraged immediately after surgery with an emphasis on ranging the ankle to prevent recurrence of scar tissue. The patient transitions to a regular shoe at approximately 2 weeks or when tolerated as dictated by pain and swelling. Driving is prohibited for the first 2 weeks. Formal physiotherapy is usually not required.
Discussion
Achilles tendinopathy is the most frequently encountered tendinous condition of the foot and/or ankle in athletes.14 Recent advancements in needle arthroscopy have provided foot and ankle surgeons with the tools to directly diagnose and treat pathologies in the office setting while providing an enhanced patient experience. Patients are able to understand their pathology by observing the procedure while wide awake, effectively enhancing their rehabilitation process.
When conservative measures fail, operative treatment for Achilles tendinopathy may include the open approach, percutaneous approach, or endoscopic approach.15, 16, 17 The endoscopic approach has been shown to allow for better operative control than the percutaneous technique and to yield fewer complications than the open approach.11,18 Endoscopy has been described as a safe treatment for Achilles tendinopathy, allowing for the treatment of diffuse Achilles tendinopathy and concomitant paratenon involvement.
In a small case series by Maquirriain et al.,19 7 patients with chronic Achilles tendinopathy underwent endoscopic surgical treatment, and the final clinical outcomes improved in all patients from 39 ± 16 points preoperatively to 89 ± 20 points postoperatively using the Achilles tendinopathy scoring system. Vega et al.11 performed a small series in 8 patients who underwent endoscopic surgical treatment for chronic Achilles tendinopathy. They reported that the procedure was safe and yielded satisfactory results with lower morbidity than other reported techniques.
The plantaris tendon has been identified as a potential cause of midportion Achilles tendinopathy owing to differential movement and shear stress between the tendon and Achilles itself, leading to an inflammatory response in or near the Achilles tendon.20,21 In a prospective study by Bedi et al.,22 elite athletes underwent open ventral paratenon scraping and plantaris release for non-insertional Achilles tendinopathy.15 Of 15 patients, 13 returned to full athletic competition at 12 weeks postoperatively, and at a final follow-up of 25 months, there was a 93.3% satisfaction rate. In a randomized controlled trial by Kaalund et al.,23 patients with midportion Achilles tendinopathy (nonresponsive to >6 months of conservative treatment) were randomly assigned to receive either tendoscopic peritendon shaving or placebo tendoscopic treatment. The primary outcome measure—the total score on the Victorian Institute of Sport Assessment Achilles (VISA-A) questionnaire—indicated a faster recovery from tendoscopic treatment compared with placebo for the 23 patients included in the study.
Patients are now increasingly willing to undergo procedures that minimize time spent in the operating room. They also prefer less exposure to general anesthesia. Patient feedback thus far has been largely positive in response to treatment with IONA with a high rate of willingness to undergo similar treatment.24,25 Ultimately, advances in needle arthroscopy have the potential to redefine minimally invasive procedures and help orthopaedic surgeons to be better equipped to respond to the increased demands of today’s patients.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.W.S. is a board or committee member of AANA. J.G.K. is a paid consultant for Isto Biologics, receives research support from Isto Biologics, and is a consultant for Arthrex, United States, outside the submitted work. In addition, J.G.K. is a board or committee member of American Orthopaedic Foot & Ankle Society, AANA, European Society of Sports Traumatology, Knee Surgery & Arthroscopy Ankle and Foot Associates, and International Society for Cartilage Repair of the Ankle. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Operative technique showing needle tendoscopy of Achilles tendon in left ankle. Portal placement and diagnostic tendoscopy are shown.
References
- 1.Carreira D., Ballard A. Achilles tendoscopy. Foot Ankle Clin. 2015;20:27–40. doi: 10.1016/j.fcl.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Edama M., Kubo M., Onishi H., et al. Structure of the Achilles tendon at the insertion on the calcaneal tuberosity. J Anat. 2016;229:610–614. doi: 10.1111/joa.12514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carr A.J., Norris S.H. The blood supply of the calcaneal tendon. J Bone Joint Surg Br. 1989;71:100–101. doi: 10.1302/0301-620X.71B1.2914976. [DOI] [PubMed] [Google Scholar]
- 4.Gilbert P.J., Shmon C.L., Linn K.A., Singh B. Macroscopic and microvascular blood supply of the canine common calcaneal tendon. Vet Comp Orthop Traumatol. 2010;23:81–86. doi: 10.3415/VCOT-09-05-0057. [DOI] [PubMed] [Google Scholar]
- 5.Aicale R., Oliviero A., Maffulli N. Management of Achilles and patellar tendinopathy: What we know, what we can do. J Foot Ankle Res. 2020;13:59. doi: 10.1186/s13047-020-00418-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clancy W.G., Jr., Neidhart D., Brand R.L. Achilles tendonitis in runners: A report of five cases. Am J Sports Med. 1976;4:46–57. doi: 10.1177/036354657600400202. [DOI] [PubMed] [Google Scholar]
- 7.Maffulli N., Sharma P., Luscombe K.L. Achilles tendinopathy: Aetiology and management. J R Soc Med. 2004;97:472–476. doi: 10.1258/jrsm.97.10.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nelen G., Martens M., Burssens A. Surgical treatment of chronic Achilles tendinitis. Am J Sports Med. 1989;17:754–759. doi: 10.1177/036354658901700605. [DOI] [PubMed] [Google Scholar]
- 9.Schepsis A.A., Wagner C., Leach R.E. Surgical management of Achilles tendon overuse injuries. A long-term follow-up study. Am J Sports Med. 1994;22:611–619. doi: 10.1177/036354659402200508. [DOI] [PubMed] [Google Scholar]
- 10.Stornebrink T., Stufkens S.A.S., Appelt D., Wijdicks C.A., Kerkhoffs G.M.M.J. 2-Mm diameter operative tendoscopy of the tibialis posterior, peroneal, and Achilles tendons: A cadaveric study. Foot Ankle Int. 2020;41:473–478. doi: 10.1177/1071100719895504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vega J., Cabestany J.M., Golanó P., Pérez-Carro L. Endoscopic treatment for chronic Achilles tendinopathy. Foot Ankle Surg. 2008;14:204–210. doi: 10.1016/j.fas.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Zhang K., Crum R.J., Samuelsson K., et al. In-office needle arthroscopy: A systematic review of indications and clinical utility. Arthroscopy. 2019;35:2709–2721. doi: 10.1016/j.arthro.2019.03.045. [DOI] [PubMed] [Google Scholar]
- 13.McMillan S., Schwartz M., Jennings B., et al. In-office diagnostic needle arthroscopy: Understanding the potential value for the US healthcare system. Am J Orthop (Belle Mead NJ) 2017;46:252–256. [PubMed] [Google Scholar]
- 14.Akoh C.C., Phisitkul P. Minimally invasive and endoscopic approach for the treatment of noninsertional Achilles tendinopathy. Foot Ankle Clin. 2019;24:495–504. doi: 10.1016/j.fcl.2019.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Fares M.Y., Khachfe H.H., Salhab H.A., Zbib J., Fares Y., Fares J. Achilles tendinopathy: Exploring injury characteristics and current treatment modalities. Foot (Edinb) 2020;46:101715. doi: 10.1016/j.foot.2020.101715. [DOI] [PubMed] [Google Scholar]
- 16.Nordio A., Chan J.J., Guzman J.Z., Hasija R., Vulcano E. Percutaneous Zadek osteotomy for the treatment of insertional Achilles tendinopathy. Foot Ankle Surg. 2020;26:818–821. doi: 10.1016/j.fas.2019.10.011. [DOI] [PubMed] [Google Scholar]
- 17.Steenstra F., van Dijk C.N. Achilles tendoscopy. Foot Ankle Clin. 2006;11:429–438. doi: 10.1016/j.fcl.2006.02.001. viii. [DOI] [PubMed] [Google Scholar]
- 18.Paavola M., Orava S., Leppilahti J., Kannus P., Järvinen M. Chronic Achilles tendon overuse injury: Complications after surgical treatment: An analysis of 432 consecutive patients. Am J Sports Med. 2000;28:77–82. doi: 10.1177/03635465000280012501. [DOI] [PubMed] [Google Scholar]
- 19.Maquirriain J., Ayerza M., Costa-Paz M., Muscolo D.L. Endoscopic surgery in chronic Achilles tendinopathies: A preliminary report. Arthroscopy. 2002;18:298–303. doi: 10.1053/jars.2002.30065b. [DOI] [PubMed] [Google Scholar]
- 20.Lintz F., Higgs A., Millett M., et al. The role of plantaris longus in Achilles tendinopathy: A biomechanical study. Foot Ankle Surg. 2011;17:252–255. doi: 10.1016/j.fas.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 21.Maquirriain J. Endoscopic release of Achilles peritenon. Arthroscopy. 1998;14:182–185. doi: 10.1016/s0749-8063(98)70038-6. [DOI] [PubMed] [Google Scholar]
- 22.Bedi H.S., Jowett C., Ristanis S., Docking S., Cook J. Plantaris excision and ventral paratendinous scraping for Achilles tendinopathy in an athletic population. Foot Ankle Int. 2016;37:386–393. doi: 10.1177/1071100715619989. [DOI] [PubMed] [Google Scholar]
- 23.Kaalund S, Kjaer SG, Rathleff MS, Fredberg U. Tendoscopic peritendon shaving of midportion Achilles tendinopathy: A randomised, placebo-controlled study [published online October 25, 2021]. Scand J Med Sci Sports. https://doi.org/10.1111/sms.14078. [DOI] [PubMed]
- 24.Gunasagaran J., Sean E.S., Shivdas Amir S., Ahmad T.S. Perceive comfort during minor hand surgeries with wide awake local anesthesia no tourniquet (WALANT) versus local anesthesia (LA)/tourniquet. J Orthop. Surg. 2017;25:1–4. doi: 10.1177/2309499017739499. [DOI] [PubMed] [Google Scholar]
- 25.Rhee P.C., Fischer M.M., Rhee L.A., et al. Cost savings and patient experiences of a clinic-based, wide-awake hand surgery program at a military medical center: A critical analysis of the first 100 procedures. J Hand Surg. 2017;42:139–147. doi: 10.1016/j.jhsa.2016.11.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Operative technique showing needle tendoscopy of Achilles tendon in left ankle. Portal placement and diagnostic tendoscopy are shown.
Operative technique showing needle tendoscopy of Achilles tendon in left ankle. Portal placement and diagnostic tendoscopy are shown.