Abstract
Tendoscopy has been recognized to be a useful technique in the diagnosis and treatment of early tibialis posterior tendon (TPT) dysfunction. Although open surgical procedures for advanced TPT disease have led to excellent outcomes, disagreement persists concerning the correct management algorithm for early TPT dysfunction. Recent developments in needle tendoscopy have provided a minimally invasive option for direct evaluation and intervention throughout the forefoot, midfoot, and hindfoot. The goal of this manuscript is to describe the technique for performing in-office needle tendoscopy targeting the TPT with a discussion of indications and opportunities afforded by an in-office procedure over the traditional operating room suite.
Technique Video
Operative technique demonstrating needle tendoscopy of the tibialis posterior tendon with concomitant intervention. The video demonstrates portal placement, diagnostic arthroscopy, and debridement of the tissue around the tendon and tendon sheath.
Introduction
Adult-acquired flatfoot deformity (AAFD) is a common disorder affecting over 10% of all adults over the age of 65.1 Progressive dysfunction of the tibialis posterior tendon (TPT) has been associated with AAFD.1,2 The tibialis posterior originates off the proximal posterolateral tibia, posteromedial fibula, and interosseous membrane.3,4 Its tendon passes acutely around the medial malleolus and contributes insertion limbs along the hindfoot, midfoot, and forefoot. The most prominent insertions are on the navicular and medial cuneiform, which allow the muscle to function as the primary midfoot inverter and dynamic stabilizer of the medial longitudinal arch. The retromalleolar region is a common site of TPT rupture.5 The anterior aspect of the tendon as it passes around the medial malleolus is avascular, which may limit its healing potential in this area.6 In addition to tendon ruptures, tenosynovitis, and tears have been associated with TPT dysfunction. Although advanced TPT dysfunction often requires open surgical intervention, including tendon transfers, reconstruction techniques, and arthrodesis with excellent outcomes, both conservative and invasive solutions have been attempted for early TPT dysfunction with inconsistent results.7 Tendoscopy is one such technique that has been used as a minimally invasive solution for the diagnosis and management of early TPT dysfunction.
In-office needle arthroscopy (IONA) was first available in the 1990s as a tool for surgeons to visualize and evaluate anatomic structures under local anesthesia.8 The technique was never widely adopted, in part, because of a lack of defined indications, inability to simultaneously treat identified pathologies, and poor picture resolution. Advancements on IONA have led to the release of a new disposable chip-on-tip camera with 400 × 400 resolution and 120° field of view fed through a 13' high-definition monitor.9 Even more important, this system includes operative instrumentation, including punches, graspers, scissors, a retractable probe, shavers, burrs, and resectors that allow for intervention on any identified pathology. Work has now focused on identifying certain pathologies where needle arthroscopy can safely and effectively replace a full operating room suite, as surgeons continuously refine their treatment algorithms to provide high-quality patient care.
This surgical technique guide describes our method for performing a TPT needle tendoscopy with the Arthrex (Naples, FL) Nanoscope nano tendoscopy system. We present our examination room layout, local anesthesia technique, tendoscopy video guide, and perceived benefits and disadvantages of using a needle tendoscopy system to assist other foot and ankle surgeons with deciding whether to adopt this technique into their clinical practices.
Surgical Technique
Preoperative Planning/Positioning
The complete tendoscopy procedure is performed in the office examination room (Video 1). A mayo stand is sterilely draped for the assistant to organize instruments during the procedure. The video monitor and additional equipment are placed on a separate tower within the vicinity of the examination table. The patient is asked to lay in lateral decubitus position on the examination table to provide access to the medial aspect of the operative ankle. Soft padding is provided under the patient’s nonoperative extremity for comfort. Both the assistant and operative surgeon scrub for the procedure and don masks, gowns, and sterile gloves. A solution of chlorhexidine gluconate mixed with isopropyl alcohol is used to sterilely prep the patient’s ankle. Finally, the patient’s ankle is draped to provide a sterile work area on the examination table.
Portal Placement
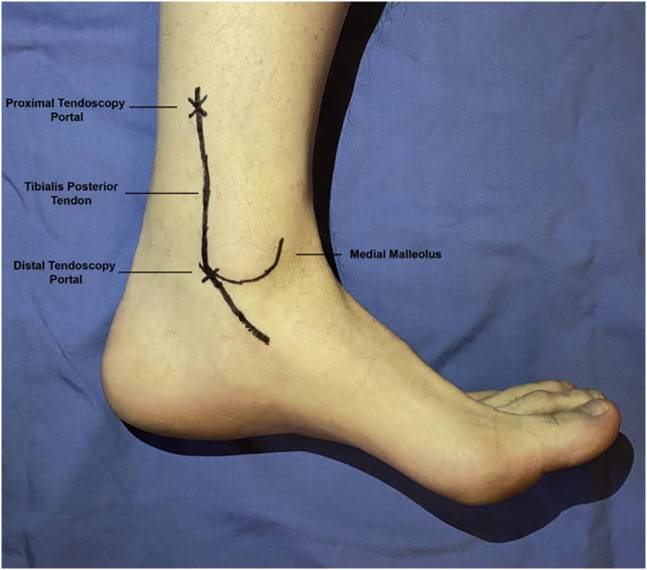
The medial malleolus, distal portal site, and proximal portal site are marked on the skin (Fig 1). The portal sites are superficially injected with 1% lidocaine. After 5-10 minutes, the needle is advanced into the tibialis posterior tendon sheath and 5 mL of 1:1 ratio 0.5% bupivacaine and 1% lidocaine with epinephrine are slowly injected. Emphasis is placed on providing sufficient analgesia to the retromalleolar region. We have found that including epinephrine in the local anesthesia assists with hemostasis.
Fig 1.
The patient is placed in the lateral decubitus position on the examination table such that the medial aspect of the operative ankle is exposed. Pictured here is a surface view of the medial aspect of the left ankle. Portal sites and surface anatomy, including the medial malleolus, talus, and tibialis posterior tendon are marked.
Operative Technique
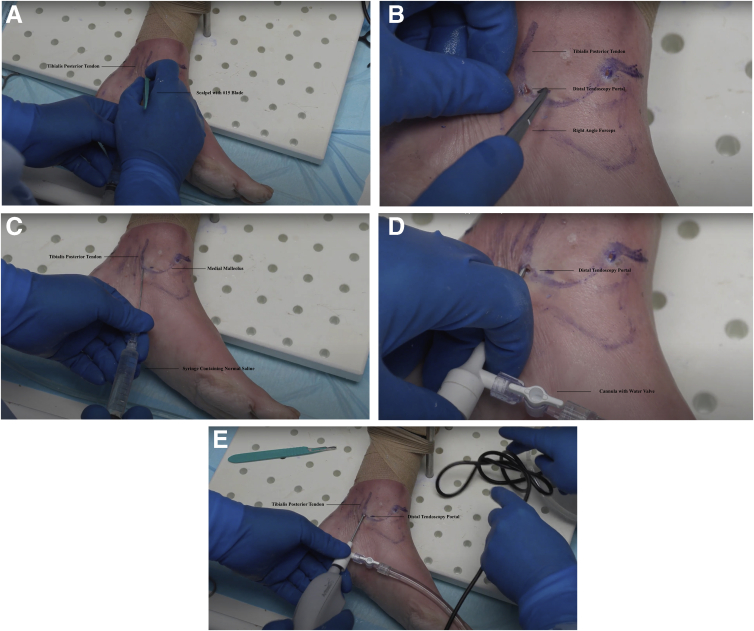
A 22-gauge needle is used to identify the tibialis posterior sheath just inferior and posterior to the medial malleolus (Fig 2). About 5.0 cc of normal saline is injected into the sheath to confirm correct placement. A 2-mm skin incision is then made with an 11-blade, and a blunt trocar is used to enter the tibialis posterior sheath. The camera is exchanged for the trochar and connected to water inflow set to 20 mmHg (Fig 3). A diagnostic tendoscopy is performed to evaluate the length of the tibialis posterior tendon from the retromalleolar region continuing to the proximal myotendinous junction (Figs 4 and 5). Passive ranging of the ankle may be used to assess tendon gliding.
Fig 2.
This is a medial surface view of the left ankle. An 18-gauge spinal needle is placed immediately posterior and inferior to the medial malleolus. We recommend keeping the needle as close as possible to the medial malleolus as you glide into the tibialis posterior tendon space.
Fig 3.
(A-E) This is a medial surface view of the left ankle. (A) 5 cc of normal saline is injected into the tibialis posterior tendon sheath. (B) A scalpel with a #15 blade is used to make an incision just over the medial entry site (C) a right angle forceps is used to develop the portal site (D), the cannula is introduced into the portal, and the water valve is engaged (E). The trocar is finally removed, and the camera is inserted through the portal site and into the tendon sheath.
Fig 4.

This is a tendoscopic view from the distal tendoscopy portal site on the medial left ankle. Start with a diagnostic tendoscopy where the tibilias posterior tendon can be visualized.
Fig 5.
Identifiable anatomy during tibialis posterior tendoscopy.
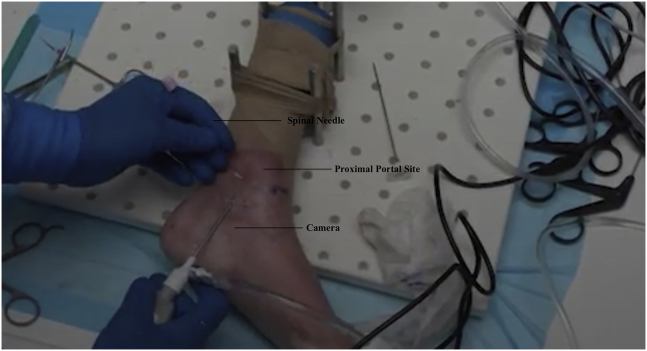
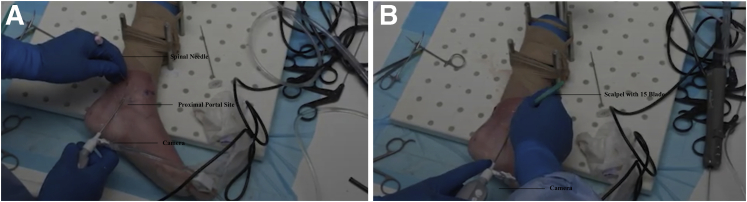
Creation of a second portal may be made under direct visualization using a 25-gauge needle at the proximal aspect of the TPT (Fig 6). This portal is typically used for any concomitant therapeutic procedures. After confirmation of the appropriate portal location, entry into the tendon sheath is completed in a similar fashion as the first portal (Fig 7). A 2-mm shaver or 3-mm burr can be inserted through this portal and onto the tendon sheath (Fig 8). Tendoscopic procedures, such as TPT tear debridement, tenosynovectomy, removal of adhesions, and retromalleolar shaving, may then be completed. Patients have reported feeling vibrations or pressure with the intervention instruments, but pain is generally not experienced with enough time allotted between local anesthesia application and the procedure. Additional bupivacaine and lidocaine should be injected as necessary.
Fig 6.
This is a medial surface view from the medial left ankle. An 18-guage spinal needle is used to find the site of the proximal portal site. This portal is generally placed about 8 cm proximal to the medial malleolus, but the exact distance should be adjusted on the basis of patient characteristics.
Fig 7.
(A and B) This is a medial surface view from the medial left ankle. (A) The camera tip can be adjusted to better visualize insertion of the needle tip. In this figure, the camera was adjusted anteriorly and superiorly until the needle tip was visualized. (B) Another scalpel with a #15 blade can be used to create the proximal portal site.
Fig 8.
This is a tendoscopic view from the distal tendoscopy portal site on the medial left ankle. A 2-mm shaver is introduced through the proximal portal site, where it can be used for debriding tissue around the tendon and tendon sheath.
At the end of the procedure, the patient is asked to actively range his or her ankle to ensure smooth tendon gliding and stability. Any remaining tendoscopy fluid is removed with suction, and the portals are closed with steri-strips. Throughout the procedure, the patient is encouraged watch the viewing monitor and ask questions to learn about their pathology. A sterile soft dressing is applied at the end of the procedure. Patients are allowed to weight bear as tolerated with early range of motion.
Postoperative Protocol
Formal physical therapy consisting of strengthening, range of motion, balance, and proprioceptive exercises is begun immediately after tendoscopy involving only debridement. Ice and elevation are encouraged when patients are not ambulating. We have typically provided pain medication for up to 4 days after the procedure. Patients are expected to return on day 5 after their tendoscopy for the first follow-up appointment (Table 1, Table 2, Table 3).
Table 1.
Advantages and Disadvantages of Proposed Technique
| Advantages | Disadvantages |
|---|---|
| Minimally invasive procedure with smaller instruments than standard tendoscopy | Dependent on local anesthesia for pain control during procedure |
| Direct visualization of the tendon may allow for identification of pathology not detected by MRI. | Unable to convert to open procedure in the office if identified pathology is not reparable through tendoscopy |
| Decreased cost and resource utilization without the need for a full operating room suite | Learning curve with wide-awake patient present |
| Patient is wide awake and allowed to learn about their condition in real-time. | Only a 0° camera is currently available with the needle tendoscopy system. |
| Less invasive procedure provides opportunity for quicker recovery, minimal scarring, and limited wound complications |
MRI, magnetic resonance imaging.
Table 2.
Pearls and Pitfalls of the Proposed Technique
| Pearls | Pitfalls |
|---|---|
| Ensure proper support for the patient’s head and nonoperative extremity to limit movement during the procedure. | Incorrect placement of inferior and superior portal may cause tibial nerve injury. |
| Inject lidocaine at both portal sites and just posterior to the medial malleolus | Too inferior and anterior placement of the inferior portal may lead to difficulties in assessing the retromalleolar and proximal TPT |
| Use a mixture of lidocaine with epinephrine and bupivacaine for injection into the tendon sheath to limit bleeding. | Debridement before a full diagnostic evaluation may lead to iatrogenic injury. |
| “Walk” step-wise with the 18-gauge spinal needle posterior to the medial malleolus to identify the proper location for the inferior portal. | Maintain constant visualization of the shaver to limit iatrogenic injury to the TPT. |
| Identifying the “glistening tendon” with right-angle forceps assists with correct cannula placement | |
| Injection of 5 cc of normal saline into the tendon sheath allows for easier cannula introduction. | |
| Instruct patient to actively range his or her ankle to assess TPT gliding and identify any missed adhesions. |
Table 3.
Step-by-Step Guide to Performing In-Office Tibialis Posterior Tendoscopy
| Step 1: Position the patient in lateral decubitus on an examination table to make the medial aspect of the operative ankle easily accessible. |
| Step 2: Use a chlorhexidine gluconate/isopropyl alcohol sponge-stick to sterilely prepare the ankle. |
| Step 3: Drape the ankle to create a sterile field along the distal half of the examination table. |
| Step 4: Inject local anesthesia superficially into the anticipated portals and deep along the tibialis posterior tendon. |
| Step 5: Establish portals with a superficial stab incision followed by blunt dissection. Start with the retromalleolar portal and finish with the more proximal portal under direct visualization. |
| Step 6: Carefully debride fatty tissue around the tendon to allow for full visualization. |
| Step 7: Perform a diagnostic tendoscopy along the length of the tendon from just inferior to the medial malleolus up to the myotendinous junction. |
| Step 8: Treat the tibialis posterior tendon as necessary. This step may include tenosynovectomy, debridement of frayed tissue, removal of adhesions, or shaving of the retromalleolar bone to produce local bleeding. |
| Step 9: Ask the patient to actively range their ankle to assess tendon function. |
| Step 10: Perform wound closure with steri-strips and apply soft dressing or splint as indicated. |
Discussion
Advancements in needle tendoscopy have provided foot and ankle surgeons with an invaluable tool to identify and intervene on select pathology in the office under local anesthesia. We prepared this article to describe a technique for performing wide-awake TPT needle tendoscopy for the management of early TPT dysfunction.
Few studies have investigated TPT tendoscopy outcomes. Chow et al. performed a small series of TPT tendoscopies with synovectomies for patients with stage 1 TPT dysfunction.10 The authors demonstrated that the procedure was safe, and all patients reported pain improvement by the 2-month follow-up visit. Bulstra et al. used TPT tendoscopy to treat a diverse set of pathology in 33 patients. No complications were encountered during the tendoscopies and patients were able to mobilize early with minimal postoperative pain.11 Khazen and Khazen similarly used TPT tendoscopy to treat stage 1 TPT dysfunction in 9 patients.12 Of these 9 patients, 3 patients had tendon tears requiring open repair, but 5 of the 6 remaining patients treated with only tendoscopy did not have progression of their TPT dysfunction by a mean of 3 years follow-up (range, 10-38 months). Gianakos et al. compared preoperative MRI findings to intraoperative TPT tendoscopy findings in a small case series and found that MRI missed TPT pathology in 33% (4/12) of patients.13 Finally, Bernasconi et al. prospectively investigated management of stage 2 TPT dysfunction with tendoscopy.14 One patient was lost to follow-up, but the remaining 15 patients reported improvements in VAS pain, SF-36 physical, and SF-36 mental scores at a mean 25.6 months. Needle tendoscopy has already been demonstrated to be capable of safely visualizing all relevant structures for evaluation of the TPT, including the entire length of the tendon and sheath in a cadaver model.15 Although further work is necessary, needle tendoscopy is expected to build upon the positive results achieved by traditional tendoscopy for TPT dysfunction by allowing the procedure to be performed under local anesthesia.
Wide-awake surgical procedures have been successfully used to manage select upper and lower extremity pathology.16, 17, 18, 19, 20 Patient feedback after these interventions has been overall positive with a high rate willing to undergo a similar treatment.21,22 Indeed, our own patients have been grateful to have an opportunity to watch their arthroscopy in real-time and interact with the operative team. Additionally, quality evaluations have demonstrated that wide-awake procedures are often less expensive than equivalent surgeries requiring a full operating suite.22, 23, 24 We are now conducting studies to investigate outcomes after in-office needle arthroscopy for TPT dysfunction.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.W.S. reports being a board or committee member of Arthroscopy Association of North America. J.G.K. reports grants from Isto Biologics and Arthrex, outside the submitted work. He is a board or committee member of American Orthopaedic Foot and Ankle Society, Arthroscopy Association of North America, European Society for Sports Traumatology, Knee Surgery and Arthroscopy, Ankle and Foot Associates, and International Society for Cartilage Repair of the Ankle. He has also received support from Ohnell Family Foundation and Mr. and Mrs. Michael J. Levitt. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Operative technique demonstrating needle tendoscopy of the tibialis posterior tendon with concomitant intervention. The video demonstrates portal placement, diagnostic arthroscopy, and debridement of the tissue around the tendon and tendon sheath.
References
- 1.Henry J.K., Shakked R., Ellis S.J. Adult-acquired flatfoot deformity. Foot Ankle Ortho. 2019;4:1–17. doi: 10.1177/2473011418820847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ling S.K., Lui T.H. Posterior tibial tendon dysfunction: an overview. Open Orthop J. 2017;11:714–723. doi: 10.2174/1874325001711010714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaye R.A., Jahss M.H. Tibialis posterior: a review of anatomy and biomechanics in relation to support of the medial longitudinal arch. Foot Ankle. 1991;11:244–247. doi: 10.1177/107110079101100414. [DOI] [PubMed] [Google Scholar]
- 4.Guelfi M., Pantalone A., Mirapeix R.M., et al. Anatomy, pathophysiology, and classification of posterior tibial tendon dysfunction. Europ Rev Med Pharmacol Sci. 2017;21:13–19. [PubMed] [Google Scholar]
- 5.Petersen W., Hohmann G., Pufe T., et al. Structure of the human tibialis posterior tendon. Arch Orthop Trauma Surg. 2004;124:237–242. doi: 10.1007/s00402-003-0500-5. [DOI] [PubMed] [Google Scholar]
- 6.Petersen W., Hohmann G., Tillman B. The blood supply of the posterior tibial tendon. J Bone Joint Surg (Br) 2002;84:141–144. doi: 10.1302/0301-620x.84b1.11592. [DOI] [PubMed] [Google Scholar]
- 7.Edwards M.R., Singh J.S.K. Tibialis posterior dysfunction. Current Orthop. 2008;22:185–192. [Google Scholar]
- 8.Zhang K, Crum RJ. Samuelsson K, et al. In-office needle arthroscopy: a systematic review of indications and clinical utility. Arthroscopy. 2019;35:2709–2721. doi: 10.1016/j.arthro.2019.03.045. [DOI] [PubMed] [Google Scholar]
- 9.Hand Held Arthroscopic Instruments. Arthrex, Inc. https://www.arthrex.com/knee/hand-held-arthroscopic-instruments [Accessed 2/21/2021]
- 10.Chow H.T., Chan K.B., Lui T.H. Tendoscopic debridement for stage 1 posterior tibial tendon dysfunction. Knee Surg Sports Traumato Arthrosc. 2005;13:695–698. doi: 10.1007/s00167-005-0635-8. [DOI] [PubMed] [Google Scholar]
- 11.Bulstra G.H., Olsthoorn P.G.M., van Dijk C.N. Tendoscopy of the posterior tibial tendon. Foot Ankle Clin N Am. 2006;11:421–427. doi: 10.1016/j.fcl.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 12.Khazen G., Khazen C. Tendoscopy in stage 1 posterior tibial tendon dysfunction. Foot Ankle Clin N Am. 2021;17:399–406. doi: 10.1016/j.fcl.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Gianakos A.L., Ross K.A., Hannon C.P., et al. Function outcomes of tibialis posterior tendoscopy with comparison to magnetic resonance imaging. Foot Ankle Int. 2015;36:812–819. doi: 10.1177/1071100715576485. [DOI] [PubMed] [Google Scholar]
- 14.Bernasconi A., Sadile F., Welck M., et al. Role of tendoscopy in treating stage II posterior tibial tendon dysfunction. Foot Ankle Int. 2018;39:433–442. doi: 10.1177/1071100717746192. [DOI] [PubMed] [Google Scholar]
- 15.Stornebrink T., Stufkens S.A.S., Appelt D., et al. 2-mm diameter operative tendoscopy of the tibialis posterior, peroneal, and achilles tednons: A cadaveric study. Foot Ankle Int. 2021;41:473–478. doi: 10.1177/1071100719895504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tahir M., Chaudhry E.A., Ahmed N., et al. Ankle fracture fixation with use of WALANT (wide awake local anesthesia with no tourniquet) technique: An attractive alternative for the austere environment. J. Bone Joint Surg. Am. 2021;103:397–404. doi: 10.2106/JBJS.20.00196. [DOI] [PubMed] [Google Scholar]
- 17.Wright J., MaCNeill A.L., Mayich D.J. A prospective comparison of wide-awake local anesthesia and general anesthesia for forefoot surgery. Foot Ankle Surg. 2019;25:211–214. doi: 10.1016/j.fas.2017.10.015. [DOI] [PubMed] [Google Scholar]
- 18.Turcotte J.J., Petre B.M., Jones C.M., Gelfand J.M. Maintaining access to orthopaedic surgery during periods of operating room resource constraint: Expanded used of wide-awake surgery during the COVID-19 pandemic. J Am Acad Orthop Surg Glob Res Rev. 2020;4:1–8. doi: 10.5435/JAAOSGlobal-D-20-00100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grandizio L.C., Graham J., Klena J.C. Current trends in WALANT surgery: A survery of American Society for Surgery of the Hand members. J Hand Surg Global Online. 2020;2:186–190. doi: 10.1016/j.jhsg.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ilyas A.M., Lennings J.D., Banner L., Matzon J.L. Wide-awake surgery with local anesthesia and epinephrine is safe. Orthopedics. 2020;43:529–532. doi: 10.3928/01477447-20200827-03. [DOI] [PubMed] [Google Scholar]
- 21.Gunasagaran J., Sean E.S., Shivdas Amir S., Ahmad T.S. Perceive comfort during minor hand surgeries with wide awake local anesthesia no tourniquet (WALANT) versus local anesthesia (LA)/tourniquet. J Orthop Surg. 2017;25:1–4. doi: 10.1177/2309499017739499. [DOI] [PubMed] [Google Scholar]
- 22.Rhee P.C., Fischer M.M., Rhee L.A., et al. Cost savings and patient experiences of a clinic-based, wide-awake hand surgery program at a military medical center: A critical analysis of the first 100 procedures. J Hand Surg. 2017;42:139–147. doi: 10.1016/j.jhsa.2016.11.019. [DOI] [PubMed] [Google Scholar]
- 23.Tahir M, Chaudhry EA, Zaffar Z, et al. Fixation of distal radius fractures using wide-awake local anaesthesia with no tourniquet (WALANT) technique: A randomized control trial of a cost-effective and resource-friendly procedure. Bone Joint Res. 2020;9:429–439. doi: 10.1302/2046-3758.97.BJR-2019-0315.R1. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 24.Maliha S.G., Cohen O., Jacoby A., Sharma S. A cost and efficiency analysis of the WALANT technique for the management of trigger finger in a procedure room of a major city hospital. Plastic and Recon Surg Global Open. 2019;7:1–5. doi: 10.1097/GOX.0000000000002509. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Operative technique demonstrating needle tendoscopy of the tibialis posterior tendon with concomitant intervention. The video demonstrates portal placement, diagnostic arthroscopy, and debridement of the tissue around the tendon and tendon sheath.
Operative technique demonstrating needle tendoscopy of the tibialis posterior tendon with concomitant intervention. The video demonstrates portal placement, diagnostic arthroscopy, and debridement of the tissue around the tendon and tendon sheath.