Abstract
In the treatment of anterior shoulder instability with glenoid bone loss, free bone graft transfers have proven to be a viable anatomic alternative to the commonly performed, nonanatomic Latarjet procedure. Implant-free fixation of the free bone grafts, in particular, has rendered excellent short- and long-term results. However, a drawback remains the source of the graft. We describe an arthroscopic bone block cerclage technique using a tricortical scapular spine autograft, which provides an anatomic arthroscopic glenoid reconstruction with the combined benefit of sparing the subscapularis, metal-free fixation, and intraregional donor site for autograft harvesting.
Technique Video
Arthroscopic bone block cerclage technique using a tricortical scapular spine autograft for glenoid reconstruction in patients with anterior shoulder instability.
The extent of glenoid bone loss is one of the most important risk factors leading to recurrent shoulder instability after soft-tissue stabilization procedures.1 Thus, in the setting of an extensive bony glenoid defect, bony augmentation techniques such as coracoid transfer, iliac crest autograft, or allografts are recommended.2 However, these techniques have drawbacks and complication rates as high as 25%.3, 4, 5 The Latarjet procedure, despite its wide use, violates the normal shoulder anatomy with a permanent split of the subscapularis by the transferred conjoined tendon, with possible structural effects and restriction of the internal rotation.6 Furthermore, Latarjet is associated with damage to neurovascular structures during harvest and fixation.3,5,7 Iliac crest bone graft transfers require an additional surgery site and are associated with donor site morbidity, postoperative pain, immobility, blood loss, hematoma, and nerve injury.8, 9, 10 Further graft options include allogeneic, xenogeneic, and synthetic grafts, with drawbacks including additional costs, potentially lower graft quality and healing potential, higher osteolysis rates, and risk of disease transmission.11, 12, 13 Furthermore, most bony augmentation techniques require application of metal implants for fixation regardless of the graft used, and the presence of metal in implants is associated with hardware failure, residual pain, and graft resorption.14, 15
The scapular spine has recently been identified as an appropriate source for structural bone autografts in glenoid reconstruction.11 Satisfactory results with an autologous scapular spine bone graft were achieved at short-term follow-up in patients with anterior shoulder instability and subcritical bone loss.16 The purpose of this Technical Note is to describe an arthroscopic bone block cerclage technique17 that uses a tricortical scapular spine autograft for reconstruction of the glenoid in patients with anterior shoulder instability and glenoid bone loss.
Surgical Technique
The surgical technique is demonstrated in the Video 1.
Preoperative Assessment and Indications
An elaborate patient history is obtained, and a functional assessment is performed with complete clinical examination to determine the type of instability, functional demand, joint laxity, and possible other pathologies, followed by a detailed radiologic assessment. All patients with multiple episodes of anterior shoulder instability should be evaluated with 3-dimensional computed tomography (CT) to assess humeral and glenoid bone loss. The current technique is indicated in patients with symptomatic anterior shoulder instability and concomitant measured glenoid bone loss >15%.
Patient Positioning and Diagnostic Arthroscopy
Under general anesthesia and with a routine single-shot antibiotic regimen, the patient is placed in the lateral decubitus position using a vacuum bean bag positioner. The affected arm is fixed with the help of a traction device in 30° of abduction and neutral rotation, with axial and lateral traction applied to distend the shoulder joint and improve intraarticular visualization.
Three regular portals are required for this procedure: standard posterior, anterosuperior, and anteroinferior. We recommend the posterior portal be incised in a horizontal fashion to ease the introduction of the drill guide from posterior. A diagnostic arthroscopy is first performed through the posterior portal to identify concomitant pathologies; however, the anterior glenoid rim and capsulolabral complex can be evaluated best through the anterosuperior portal.
Capsulolabral Complex Release and Glenoid Preparation
Looking through the anterosuperior portal, the capsulolabral complex is first carefully mobilized using an arthroscopic periosteal elevator. Then the anterior glenoid defect is debrided and abraded with a motorized burr to achieve a flat plane and induce bleeding for improved glenoid bone graft healing potential (Fig 1).
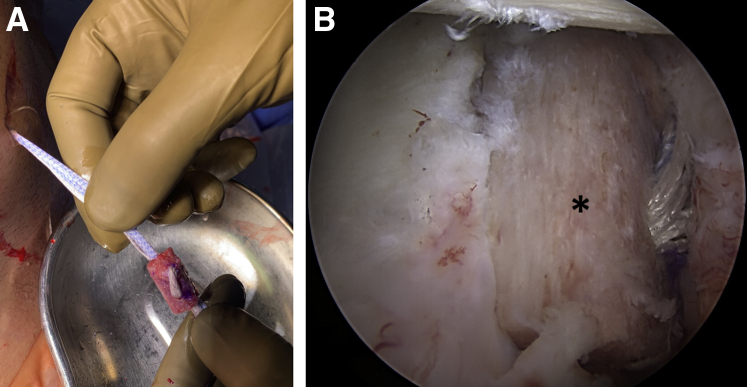
Fig 1.

Arthroscopic view of the left shoulder from anterosuperior portal. Patient in lateral decubitus position; after mobilization of the capsulolabral complex and debridement and abrasion of the anterior glenoid defect (∗) with a motorized burr to achieve a plane surface. Note the remaining hardware (arrow) from previous stabilization surgery.
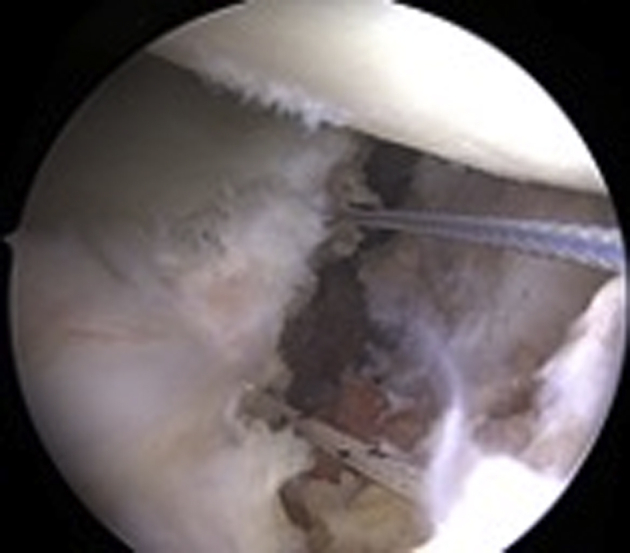
Glenoid Drilling
An arthroscopic posterior drilling guide (Arthrex, Naples, FL) is introduced into the joint through the posterior portal, and the hook component is placed parallel to the articular surface of the glenoid, as close as possible to the center of the defect and ∼5 mm medial of the cartilage surface (Fig 2A). With the help of the drill guide, two 2.4-mm tunnels are drilled from the posterior scapula neck to the glenoid defect on the anterior scapula neck, parallel to the articular surface and parallel to each other with a 10-mm distance. After removal of the central pins of the cannulated drills, 2 nitinol wires with loops (1 for each tunnel) are passed and retrieved from the anteroinferior portal (Fig 2B). The drill guide, hook, and drills are then removed. Two loop sutures (FiberLink/TigerLink; Arthrex), one with the loop anterior and the other with the loop posterior, are passed through the tunnels using the nitinol wires (Fig 3).
Fig 2.
Arthroscopic view of the left shoulder from anterosuperior portal. Patient in lateral decubitus position. (A) Positioning of the drill guide from the posterior portal with the hook position 5 mm deep from the articular surface and parallel to glenoid for correct placement of the drill tunnels. (B) Intraoperative view of nitinol wires shuttled through the drill holes.
Fig 3.
Arthroscopic view of the left shoulder from anterosuperior portal. Patient in lateral decubitus position. Exchange of nitinol wires with FiberLink (blue) and TigerLink (white) sutures for FiberTape-TigerTape Cerclage passage through glenoid and graft tunnels.
In situ measurement of the anterior glenoid defect is crucial to achieve a perfect fit of the autograft. This is performed by using an arthroscopic measuring probe (220 mm, 60°; Arthrex) from the anteroinferior portal to measure the craniocaudal and mediolateral width of the defect and the exact localization of the drill holes within the defect.
Scapular Spine Preparation
A harvest location 4 to 5 cm lateral to the medial scapular border is selected that provides the largest cross-sectional graft size while avoiding the acromial base.11 A 5-cm horizontal incision is then made along the scapular spine, and the posterior deltoid and trapezius fascia are dissected to expose the scapular spine (Fig 4A). A tricortical bone graft with a length of 20 mm and a thickness of 8 mm is harvested using an oscillating saw. The width of the graft is predefined by the maximum width of the spina scapulae. The fascia is repaired with resorbable sutures after placing a hemostatic sponge in the harvest area (Fig 4B). After freeing the graft from soft tissue, a slight reshaping can be performed, and two 2.4-mm drill tunnels are made through the graft based on the measurements obtained before.
Fig 4.
(A) Harvest location 4 to 5 cm lateral to the medial scapular border is selected, which provides the largest cross-sectional graft size while avoiding the acromial base. A horizontal incision is made along the scapular spine, and the posterior deltoid and trapezius fascia are dissected to expose the scapular spine. (B) A tricortical bone graft is harvested from a left shoulder using an oscillating saw. Patient in lateral decubitus position.
Fixation of the Scapular Spine Bone Graft
Digital dilation of the anteroinferior portal is performed for better graft passage. Using the inferior FiberLink loop, 2 ultra-high-strength suture tapes (FiberTape Cerclage System; Arthrex) are passed from posterior to the anterior side of the glenoid and retrieved through the anteroinferior portal. The suture tapes are then passed through the inferior tunnel of the autograft from the cancellous side to the cortical side and from the cortical side to the cancellous side through the superior tunnel of the autograft (Fig 5A). The superior TigerLink loop is then loaded with both FiberTape Cerclage sutures to pass them from anterior to the posterior glenoid side. The scapular spine autograft is introduced in the joint through the anteroinferior portal and through the rotator interval by pulling the FiberTape Cerclage sutures while holding the graft with a Kocher clamp.
Fig 5.
(A) Tricortical scapular spine autograft after FiberTape-TigerTape passage before insertion through the anteroinferior portal and the rotator interval. (B) Arthroscopic view of the left shoulder from anterosuperior portal after positioning of the graft (∗) on the anterior glenoid rim. Patient in lateral decubitus position.
After insertion and proper positioning of the scapular spine graft (Fig 5B), the FiberTape sutures are interconnected to create a continuous loop. For that purpose, the tail of the FiberTape suture is loaded through the pretied racking hitch knot of the TigerTape and vice versa. To apply sufficient traction on each suture limb in a controlled fashion, a cerclage tensioner set to 60 to 80 N is used. Sutures are then knotted with ≥4 alternating knots, and finally the graft fixation is checked with an arthroscopic probe.
Capsulolabral Repair
The capsulolabral complex is reattached to the glenoid around the graft with 3 cinch stitches and 3 single-loaded 2.9-mm knotless suture anchors (PushLock; Arthrex) placed in the native glenoid, thus partially covering the graft to restore anatomy (Fig 6). Alternatively, other suture and anchor configurations can be used.
Fig 6.
Arthroscopic view of the left shoulder from anterosuperior portal. Patient in lateral decubitus position. Fixation of the capsulolabral complex on the native glenoid around the transferred graft with cinch stitches and knotless suture anchors (A), thus partially covering the graft (B).
Discussion
In the treatment of anterior shoulder instability with glenoid bone loss, free bone graft transfers have proven to be a viable anatomic alternative to the commonly performed, nonanatomic Latarjet procedure.6,18 In particular, implant-free fixation of the free bone grafts has rendered excellent short- and long-term results.6 However, a drawback remains the source of the graft. Grafts are commonly harvested from the iliac crest, with the associated risk of postoperative pain, immobility, blood loss, hematoma, and nerve injury.8, 9, 10 Additionally, many patients understandably would like to avoid having a procedure performed in a second body region. The alternative option, allografts, can be associated with additional costs, potentially lower graft quality and healing potential, higher osteolysis rates, and risk of disease transmission.11, 12, 13,18
The arthroscopic bone block cerclage technique using a tricortical scapular spine autograft provides an anatomic arthroscopic glenoid reconstruction with the combined benefit of sparing the subscapularis, metal-free fixation, and intraregional donor site for autograft harvesting. The advantages and disadvantages, as well as some pearls and pitfalls of the technique, are described in Tables 1 and 2. Although the size of the graft is limited, CT-based studies have shown that the scapular spine has dimensions similar to the coracoid, and even the iliac crest, in the majority of patients11 and therefore is suitable as a graft choice for bony glenoid reconstruction in anterior shoulder instability. Not only does the use of grafts with smaller size make it technically easier to transfer the graft into the joint and attach the capsulolabral complex around the graft, but it has also been shown that, most of the time, iliac crest bone grafts are too large and therefore augment rather than reconstruct the glenoid, which leads to extensive resorption due to remodeling processes based on Wolff’s law.19 Furthermore, in the case of failure, revision surgery with an iliac-crest bone graft transfer or Latarjet is easily possible, as the donor sites are still available, no metal implants were used, and the subscapularis was spared.
Table 1.
Advantages and Disadvantages
| Advantages |
|
|
|
|
|
| Disadvantages |
|
|
Table 2.
Pearls and Pitfalls
| Pearls |
|
|
|
| Pitfalls |
|
|
|
Footnotes
The authors report the following potential conflicts of interest or sources of funding: P.M. reports grants, personal fees, and nonfinancial support, Arthrex GmbH. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic bone block cerclage technique using a tricortical scapular spine autograft for glenoid reconstruction in patients with anterior shoulder instability.
References
- 1.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 2.Bushnell B.D., Creighton R.A., Herring M.M. Bony instability of the shoulder. Arthroscopy. 2008;24:1061–1073. doi: 10.1016/j.arthro.2008.05.015. [DOI] [PubMed] [Google Scholar]
- 3.Shah A.A., Butler R.B., Romanowski J., Goel D., Karadagli D., Warner J.J. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am. 2012;94:495–501. doi: 10.2106/JBJS.J.01830. [DOI] [PubMed] [Google Scholar]
- 4.Degen R.M., Camp C.L., Werner B.C., Dines D.M., Dines J.S. Trends in bone-block augmentation among recently trained orthopaedic surgeons treating anterior shoulder instability. J Bone Joint Surg Am. 2016;98:e56. doi: 10.2106/JBJS.15.01478. [DOI] [PubMed] [Google Scholar]
- 5.Griesser M.J., Harris J.D., McCoy B.W., et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: A systematic review. J Shoulder Elbow Surg. 2013;22:286–292. doi: 10.1016/j.jse.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 6.Moroder P., Schulz E., Wierer G., et al. Neer Award 2019: Latarjet procedure vs. iliac crest bone graft transfer for treatment of anterior shoulder instability with glenoid bone loss: a prospective randomized trial. J Shoulder Elbow Surg. 2019;28:1298–1307. doi: 10.1016/j.jse.2019.03.035. [DOI] [PubMed] [Google Scholar]
- 7.Longo U.G., Loppini M., Rizzello G., Ciuffreda M., Maffulli N., Denaro V. Latarjet, Bristow, and Eden-Hybinette procedures for anterior shoulder dislocation: Systematic review and quantitative synthesis of the literature. Arthroscopy. 2014;30:1184–1211. doi: 10.1016/j.arthro.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 8.Loeffler B.J., Kellam J.F., Sims S.H., Bosse M.J. Prospective observational study of donor-site morbidity following anterior iliac crest bone-grafting in orthopaedic trauma reconstruction patients. J Bone Joint Surg Am. 2012;94:1649–1654. doi: 10.2106/JBJS.K.00961. [DOI] [PubMed] [Google Scholar]
- 9.Myeroff C., Archdeacon M. Autogenous bone graft: Donor sites and techniques. J Bone Joint Surg Am. 2011;93:2227–2236. doi: 10.2106/JBJS.J.01513. [DOI] [PubMed] [Google Scholar]
- 10.Armaghani S.J., Even J.L., Zern E.K., Braly B.A., Kang J.D., Devin C.J. The evaluation of donor site pain after harvest of tricortical anterior iliac crest bone graft for spinal surgery: A prospective study. Spine (Phila) 2016;41:E191–E196. doi: 10.1097/BRS.0000000000001201. [DOI] [PubMed] [Google Scholar]
- 11.Rohman E., Gronbeck K., Tompkins M., Mittelsteadt M., Kirkham J.A., Arciero R.A. Scapular spine dimensions and suitability as a glenoid bone graft donor site. Am J Sports Med. 2019;47:2469–2477. doi: 10.1177/0363546519861965. [DOI] [PubMed] [Google Scholar]
- 12.Sayegh E.T., Mascarenhas R., Chalmers P.N., Cole B.J., Verma N.N., Romeo A.A. Allograft reconstruction for glenoid bone loss in glenohumeral instability: A systematic review. Arthroscopy. 2014;30:1642–1649. doi: 10.1016/j.arthro.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Provencher M.T., Frank R.M., Golijanin P., et al. Distal tibia allograft glenoid reconstruction in recurrent anterior shoulder instability: Clinical and radiographic outcomes. Arthroscopy. 2017;33:891–897. doi: 10.1016/j.arthro.2016.09.029. [DOI] [PubMed] [Google Scholar]
- 14.Provencher M.T., Peebles L.A., Aman Z.S., et al. Management of the failed Latarjet procedure: Outcomes of revision surgery with fresh distal tibial allograft. Am J Sports Med. 2019;47:2795–2802. doi: 10.1177/0363546519871896. [DOI] [PubMed] [Google Scholar]
- 15.Magone K., Luckenbill D., Goswami T. Metal ions as inflammatory initiators of osteolysis. Arch Orthop Trauma Surg. 2015;135:683–695. doi: 10.1007/s00402-015-2196-8. [DOI] [PubMed] [Google Scholar]
- 16.Xiang M., Yang J., Chen H., et al. Arthroscopic autologous scapular spine bone graft combined with bankart repair for anterior shoulder instability with subcritical (10%-15%) glenoid bone loss. Arthroscopy. 2021;37:2065–2074. doi: 10.1016/j.arthro.2021.01.061. [DOI] [PubMed] [Google Scholar]
- 17.Hachem A.I., Del Carmen M., Verdalet I., Rius J. Arthroscopic bone block cerclage: A fixation method for glenoid bone loss reconstruction without metal implants. Arthrosc Tech. 2019;8:e1591–e1597. doi: 10.1016/j.eats.2019.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boehm E., Minkus M., Moroder P., Scheibel M. Arthroscopic iliac crest bone grafting in recurrent anterior shoulder instability: Minimum 5-year clinical and radiologic follow-up. Knee Surg Sports Traumatol Arthrosc. 2021;29:266–274. doi: 10.1007/s00167-020-05986-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moroder P., Hitzl W., Tauber M., Hoffelner T., Resch H., Auffarth A. Effect of anatomic bone grafting in post-traumatic recurrent anterior shoulder instability on glenoid morphology. J Shoulder Elbow Surg. 2013;22:1522–1529. doi: 10.1016/j.jse.2013.03.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic bone block cerclage technique using a tricortical scapular spine autograft for glenoid reconstruction in patients with anterior shoulder instability.
Arthroscopic bone block cerclage technique using a tricortical scapular spine autograft for glenoid reconstruction in patients with anterior shoulder instability.