Abstract
This technical note describes an arthroscopic technique for treating delayed wound healing after Achilles tendon suture. Ankle arthroscopy is used to clean up the inflammatory tissues and foreign bodies that lead to delayed wound healing, with the advantages of simple postoperative care and low infection risk. This method may provide a less traumatic and low-risk option for the treatment of delayed wound healing after Achilles tendon surgery. The purpose of this technical note is to describe surgical procedures and related recommendations.
Technique Video
Arthroscopic technique for delayed wound healing after Achilles Tendon suture. Patients with delayed wound healing in the Achilles tendon area already have a defect into which the surgical instrument can be inserted. The other port selected is generally located at the top of the other side of the original defect. This approach ensures that the 2 ports are as far away from each other as possible, covers all the suture areas of the Achilles tendon for the first operation, and facilitates full exploration of all surgical suture sites. Recent preoperative magnetic resonance images were used to identify areas with Achilles tendon weakness and degeneration. After the lesion was identified, the damaged tissue was cleaned by curettage. Foreign objects in the tissue may be found, as shown in the video: a nonabsorbable suture is seen and removed.
Achilles tendon rupture is a relatively common type of sports injury. Most Achilles tendon ruptures occur during leisure sports, and the incidence is also showing an increasing trend.1, 2, 3 Regarding the treatment of acute Achilles tendon rupture, there is currently no clear evidence indicating what method is best,4,5 but surgical treatment more effectively reduces the risk of rerupture of the Achilles tendon compared with nonsurgical treatment.6,7 Patients with higher requirements for Achilles tendon function often choose surgical treatment, but they need to also bear the corresponding postoperative complications, including foreign body reaction, skin laceration, skin necrosis, scar adhesion, and delayed wound healing.8, 9, 10 Among these complications, delayed wound healing after Achilles tendon suture11 will hinder the patient’s recovery and affect quality of life.
The occurrence of delayed healing is related to the anatomic characteristics of the Achilles tendon and surrounding skin,12 but some specific conditions are causative, such as local foreign body reactions caused by nonabsorbable sutures,13,14 skin necrosis, or reinjury after surgery. Delayed wound healing may also be caused by deep infection,15,16 which requires special attention.
If conservative treatment cannot be adopted, the conventional treatment is to keep the wound open and perform daily irrigation and routine flushing,17,18 but this approach leaves a larger wound that takes longer to heal and increases the difficulty of postoperative care. We pioneered the use of arthroscopy to treat delayed wound healing after Achilles tendon suture, and our results have been satisfactory.
The purpose of this Technical Note is to introduce the surgical procedure and analyze its clinical significance and advantages over conventional open surgery, to provide an alternative idea for the treatment of patients with delayed healing.
Surgical Technique
Preoperative Evaluation
It is necessary to understand the patient’s medical history before surgery and evaluate the patient’s wound for delayed healing and current condition (Fig. 1). Magnetic resonance imaging is helpful to find inflammatory changes in the surrounding tissues of the Achilles tendon, which can determine the surgical site and the weakened area of the Achilles tendon. Patients are evaluated before surgery to see if they meet the indications and contraindications for surgery (Table 1).
Figure 1.
The dehisced wound after the Achilles tendon suture.
Table 1.
Indications and Contraindications
| Indications |
|
|
| Contraindications |
|
|
|
|
Arthroscopy Technique and Postoperative Management
The patient is placed in a prone position, and the foot is placed at the end of the operating table (Fig. 2). A pneumatic tourniquet is applied to the affected lower extremity. The unhealed part of the original incision (original defect) is selected as the portal to insert the shaver, and the other portal (new portal) for inserting the camera is usually selected at the top of the original incision (Fig. 3). This method ensures that the 2 ports are as far away from each other as possible, covers all the suture areas of the Achilles tendon from the first operation, and allows full exploration of the surgical area (Video 1).
Figure 2.
Prone position and foot placement.
Figure 3.
Endoscopic surgery technique for delayed wound healing after Achilles tendon suture. The shaver and camera were inserted into the existing skin defect and the new portal (NP), respectively, which is generally located at the top of the other side of the original defect (OD). DZ, delayed wound healing zone.
First, the Achilles tendon and surrounding tissues are explored to identify lesions, which includes inflammatory tissues, infected tissues under the skin or around the Achilles tendon, and necrotic tendons. The shaver is then used to remove these lesions. In this process, it is necessary to avoid excessive damage to the surrounding soft tissues, blood vessels, and nerves. The point of this is to carefully identify whether the tissue has completely lost its biological activity and needs to be removed.
Next, all the weak areas of the Achilles tendon need to be identified. In our experience, most of the weak areas will have healed, but some cavities may still exist. These cavities of Achilles tendon wounds need to be cleaned by shaver. If foreign bodies (nonabsorbable sutures) are found, they should be removed with nucleus pulposus forceps, which can be inserted from the original defect (Fig. 4). If necessary, another portal can be established at the distal end of the scar, so that the distal area of the Achilles tendon can also be accessed by surgery. The operation process is the same as described above (Table 2).
Figure 4.
Nonabsorbable suture can be seen in the arthroscopy; it was removed.
Table 2.
Pearls and pitfalls
| Pearls |
|
|
|
|
| Pitfalls |
|
|
Finally, the subcutaneous tissue is processed. The planer is used to remove the inflamed tissue and scar tissue. Skin tissue that has lost bioactivity around the wound also needs to be cut off, and the skin edge of the wound should be trimmed neatly.
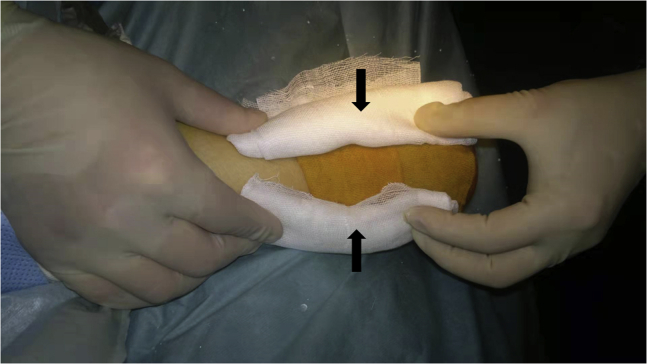
Primary suturing of the wounds is performed (Fig. 5). Roll gauze pads are placed on both sides of the Achilles tendon incision, and a pressure bandage is applied to the surgical area (Fig. 6). The purpose of the pads is to avoid fluid accumulation on the left and right sides of the Achilles tendon. For patients who are in good condition and have no wound infection, there is no need to use antibiotics or plaster fixation after surgery, which is also conducive to allowing exercise of the patient’s motor functions. If the blood circulation around the wound is poor and slow to heal, or infection is prone to occur, short-term preventive antibiotics can be used after the operation, and a short leg plaster can be used to fix the foot in natural plantarflexion for 2 weeks. Sutures can be removed 2 to 3 weeks after surgery. The rehabilitation plan can refer to the treatment of acute Achilles tendon rupture.
Figure 5.
Primary suture of the wounds.
Figure 6.
Roll gauze pads are placed on both sides of the Achilles tendon incision.
Discussion
Achilles tendon rupture occurs mainly in young and middle-aged men.19 If delayed wound healing and infection occur after surgical treatment, the patient will subjectively feel pain around the wound and worry that the wound will not heal. The function of the lower limb will also be greatly affected. The natural properties of trauma and surgical repair have already affected the healing of the wound,15 and the patient’s own condition and surgery-related treatment are also factors that lead to postoperative complications.20
Nonabsorbable sutures are widely used after Achilles tendon ruptures because they are considered to provide sufficient fixation strength during the critical healing period.21,22 However, they can also cause a certain degree of inflammation of the soft tissues23 or may cause infections, which will affect the healing of the wound. Influence. Itoga et al.24 reported a case of foreign body granuloma caused by nonabsorbable sutures, which had poor therapeutic effect with antibiotics alone. Surgical treatment was required, an incision was made on the basis of the original scar, and the granuloma was removed.
If the ruptured wound is not covered, the exposed tendon will become dry and subject to secondary adhesions.10 Although this process does not necessarily cause infection, the treatment methods are similar. Liles and Adams15 recommended early surgical intervention (irrigation and debridement) to avoid secondary deep infections.
For patients with infection at the wound site, Bae et al.25 used open debridement. The wound was kept open after debridement for patients with poor wound condition, and daily irrigation and changing of dressing were performed. The result of a deep infection can be catastrophic. Surgery requires removal of the infected and necrotic tendon. The patient may completely lose the Achilles tendon during treatment.26
These days, the use of endoscopic technology in Achilles tendon surgery is normal, and the arthroscopic technique used in Achilles tendon repair was first described by Maquirriain27 in 1998. This technology is not difficult for those who have mastered conventional endoscopy technology, increasing its suitability. Arthroscopy itself has a slighter “second blow” to the wound site, relatively. It has smaller incisions compared with traditional treatment. In addition, after the lesion is cleared, the wound can be primary sutured to avoid the complications that may be caused by an open wound. Depending on the doctor’s evaluation, the application of antibiotics and plaster fixation is not even necessary after the operation, which demonstrates the benefits of this technology (Table 3). Patients can perform early postoperative functional exercises.
Table 3.
Advantages and limitations
| Advantages |
|
|
|
|
|
| Limitations |
|
|
During the operation, care to detect whether there is a foreign body left around the Achilles tendon is necessary, because this may cause the patient’s delayed healing. Because of the limited surgical field, and perhaps lack of adequate experience, it may be difficult to find during the operation.
The remaining nonabsorbable sutures may cause relapse, which means that although the wound is completely healed after treatment, inflammation around the Achilles tendon will appear later, which is manifested as redness, swelling, and pain. FiberWire is known to have the risk of causing foreign body reactions,28 which may require surgery. If it is considered that these symptoms are caused by foreign body reactions, there is no need to perform arthroscopic surgery again. Instead, a small incision can be made directly under local anesthesia, and the sutures can be taken out. Therefore, when using this technology to treat patients, the risk needs to be communicated to patients in advance. In addition, taking into account the difficulty of arthroscopic surgery and supplies, there will be a higher cost compared with conventional open surgery.
Conclusions
This technical note describes an arthroscopic technique for delayed wound healing after Achilles tendon suture. Compared with conventional open surgery, it has the characteristics of lower risk of intraoperative injury and postoperative infection, easier postoperative care, and faster wound recovery.
Footnotes
The study was supported by Integrated application of technology and comprehensive demonstration Project of Scientific and Technological Winter Olympics of Zhangjiakou in 2020 (20110004D) and 2021 (21110006D).
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic technique for delayed wound healing after Achilles Tendon suture. Patients with delayed wound healing in the Achilles tendon area already have a defect into which the surgical instrument can be inserted. The other port selected is generally located at the top of the other side of the original defect. This approach ensures that the 2 ports are as far away from each other as possible, covers all the suture areas of the Achilles tendon for the first operation, and facilitates full exploration of all surgical suture sites. Recent preoperative magnetic resonance images were used to identify areas with Achilles tendon weakness and degeneration. After the lesion was identified, the damaged tissue was cleaned by curettage. Foreign objects in the tissue may be found, as shown in the video: a nonabsorbable suture is seen and removed.
References
- 1.Leppilahti J., Orava S. Total Achilles tendon rupture. A review. Sports Med. 1998;25:79–100. doi: 10.2165/00007256-199825020-00002. [DOI] [PubMed] [Google Scholar]
- 2.Ganestam A., Kallemose T., Troelsen A., Barfod K.W. Increasing incidence of acute Achilles tendon rupture and a noticeable decline in surgical treatment from 1994 to 2013. A nationwide registry study of 33,160 patients. Knee Surg Sports Traumatol Arthrosc. 2016;24:3730–3737. doi: 10.1007/s00167-015-3544-5. [DOI] [PubMed] [Google Scholar]
- 3.Lantto I., Heikkinen J., Flinkkilä T., Ohtonen P., Leppilahti J. Epidemiology of Achilles tendon ruptures: Increasing incidence over a 33-year period. Scand J Med Sci Sports. 2015;25:e133–e138. doi: 10.1111/sms.12253. [DOI] [PubMed] [Google Scholar]
- 4.Ochen Y., Beks R.B., van Heijl M., Hietbrink F., Leenen L.P.H., van der Velde D., Heng M., van der Meijden O., Groenwold R.H.H., Houwert R.M. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: Systematic review and meta-analysis. BMJ. 2019;364 doi: 10.1136/bmj.k5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nilsson-Helander K., Silbernagel K.G., Thomeé R., Faxén E., Olsson N., Eriksson B.I., Karlsson J. Acute achilles tendon rupture: A randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38:2186–2193. doi: 10.1177/0363546510376052. [DOI] [PubMed] [Google Scholar]
- 6.Zhou K., Song L., Zhang P., Wang C., Wang W. Surgical versus non-surgical methods for acute Achilles tendon rupture: A meta-analysis of randomized controlled trials. J Foot Ankle Surg. 2018;57:1191–1199. doi: 10.1053/j.jfas.2018.05.007. [DOI] [PubMed] [Google Scholar]
- 7.Wilkins R., Bisson L.J. Operative versus nonoperative management of acute Achilles tendon ruptures: A quantitative systematic review of randomized controlled trials. Am J Sports Med. 2012;40:2154–2160. doi: 10.1177/0363546512453293. [DOI] [PubMed] [Google Scholar]
- 8.Reda Y., Farouk A., Abdelmonem I., El Shazly O.A. Surgical versus non-surgical treatment for acute Achilles’ tendon rupture. A systematic review of literature and meta-analysis. Foot Ankle Surg. 2020;26:280–288. doi: 10.1016/j.fas.2019.03.010. [DOI] [PubMed] [Google Scholar]
- 9.Deng S., Sun Z., Zhang C., Chen G., Li J. Surgical treatment versus conservative management for acute achilles tendon rupture: A systematic review and metaanalysis of randomized controlled trials. J Foot Ankle Surg. 2017;56:1236–1243. doi: 10.1053/j.jfas.2017.05.036. [DOI] [PubMed] [Google Scholar]
- 10.Young J.S., Kumta S.M., Maffulli N. Achilles tendon rupture and tendinopathy: Management of complications. Foot Ankle Clin. 2005;10:371–382. doi: 10.1016/j.fcl.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 11.Schipper O., Cohen B. The acute injury of the Achilles: Surgical options (open treatment, and, minimally invasive surgery) Foot Ankle Clin. 2017;22:689–714. doi: 10.1016/j.fcl.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 12.Dayton P. Anatomic, vascular, and mechanical overview of the Achilles tendon. Clin Podiatr Med Surg. 2017;34:107–113. doi: 10.1016/j.cpm.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 13.Kara A., Celik H., Seker A., Uysal M.A., Uzun M., Malkoc M. Granuloma formation secondary to Achilles tendon repair with nonabsorbable suture. Int J Surg Case Rep. 2014;5:720–722. doi: 10.1016/j.ijscr.2014.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahluwalia R., Zourelidis C., Guo S., Dega R. Chronic sinus formation using non absorbable braided suture following open repair of Achilles tendon. Foot Ankle Surg. 2013;19:e7–e9. doi: 10.1016/j.fas.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Liles J., Adams S.B., Jr. Management of complications of Achilles tendon surgery. Foot Ankle Clin. 2019;24:447–457. doi: 10.1016/j.fcl.2019.04.008. [DOI] [PubMed] [Google Scholar]
- 16.Mosser P., Kelm J., Anagnostakos K. Negative pressure wound therapy in the management of late deep infections after open reconstruction of Achilles tendon rupture. J Foot Ankle Surg. 2015;54:2–6. doi: 10.1053/j.jfas.2014.09.040. [DOI] [PubMed] [Google Scholar]
- 17.Fourniols E., Lazennec J.Y., Rousseau M.A. Salvage technique for postoperative infection and necrosis of the Achilles tendon. Orthop Traumatol Surg Res. 2012;98:915–920. doi: 10.1016/j.otsr.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 18.Saku I., Kanda S., Saito T., Fukushima T., Akiyama T. Wound management with negative pressure wound therapy in postoperative infection after open reconstruction of chronic Achilles tendon rupture. Int J Surg Case Rep. 2017;37:106–108. doi: 10.1016/j.ijscr.2017.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raikin S.M., Garras D.N., Krapchev P.V. Achilles tendon injuries in a United States population. Foot Ankle Int. 2013;34:475–480. doi: 10.1177/1071100713477621. [DOI] [PubMed] [Google Scholar]
- 20.Yang Y.P., Chen H.Y., Cui G.Q., Xiu X.L., Liu X.P., An H., Ao Y.F. Endoscopic surgery for delayed wound healing after achilles tendon suture repair: A report of three cases. Orthop Surg. 2021;13:1126–1131. doi: 10.1111/os.12995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carmont M.R., Kuiper J.H., Grävare Silbernagel K., Karlsson J., Nilsson-Helander K. Tendon end separation with loading in an Achilles tendon repair model: Comparison of non-absorbable vs. absorbable sutures. J Exp Orthop. 2017;4:26. doi: 10.1186/s40634-017-0101-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barber F.A., Herbert M.A., Richards D.P. Sutures and suture anchors: Update 2003. Arthroscopy. 2003;19:985–990. doi: 10.1016/j.arthro.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 23.Cho J., Kim H.J., Lee J.S., Kim J., Won S.H., Yi Y., Chun D.I. Comparing absorbable and nonabsorbable suture materials for repair of Achilles tendon rupture: A magnetic resonance imaging-based study. Diagnostics (Basel) 2020;10:1085. doi: 10.3390/diagnostics10121085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Itoga R., Matsuoka M., Onodera T., Shimizu A., Iwasaki K., Matsubara S., Hishimura R., Kondo E., Iwasaki N. Delayed onset of infectious foreign body granuloma for nonabsorbable sutures after open Achilles tendon repair: A case report. J Foot Ankle Surg. 2021 doi: 10.1053/j.jfas.2021.04.025. S1067-251600258-1. [DOI] [PubMed] [Google Scholar]
- 25.Bae S.H., Lee H.S., Seo S.G., Kim S.W., Gwak H.C., Bae S.Y. Debridement and functional rehabilitation for Achilles tendon infection following tendon repair. J Bone Joint Surg Am. 2016;98:1161–1167. doi: 10.2106/JBJS.15.01117. [DOI] [PubMed] [Google Scholar]
- 26.Pajala A., Kangas J., Ohtonen P., Leppilahti J. Rerupture and deep infection following treatment of total Achilles tendon rupture. J Bone Joint Surg Am. 2002;84:2016–2021. doi: 10.2106/00004623-200211000-00017. [DOI] [PubMed] [Google Scholar]
- 27.Maquirriain J. Endoscopic release of Achilles peritenon. Arthroscopy. 1998;14:182–185. doi: 10.1016/s0749-8063(98)70038-6. [DOI] [PubMed] [Google Scholar]
- 28.Barp E.A., Reese E.R., Jones N.E.H., Bliek Z.J. Heel complications. Clin Podiatr Med Surg. 2021;38:183–191. doi: 10.1016/j.cpm.2020.12.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic technique for delayed wound healing after Achilles Tendon suture. Patients with delayed wound healing in the Achilles tendon area already have a defect into which the surgical instrument can be inserted. The other port selected is generally located at the top of the other side of the original defect. This approach ensures that the 2 ports are as far away from each other as possible, covers all the suture areas of the Achilles tendon for the first operation, and facilitates full exploration of all surgical suture sites. Recent preoperative magnetic resonance images were used to identify areas with Achilles tendon weakness and degeneration. After the lesion was identified, the damaged tissue was cleaned by curettage. Foreign objects in the tissue may be found, as shown in the video: a nonabsorbable suture is seen and removed.
Arthroscopic technique for delayed wound healing after Achilles Tendon suture. Patients with delayed wound healing in the Achilles tendon area already have a defect into which the surgical instrument can be inserted. The other port selected is generally located at the top of the other side of the original defect. This approach ensures that the 2 ports are as far away from each other as possible, covers all the suture areas of the Achilles tendon for the first operation, and facilitates full exploration of all surgical suture sites. Recent preoperative magnetic resonance images were used to identify areas with Achilles tendon weakness and degeneration. After the lesion was identified, the damaged tissue was cleaned by curettage. Foreign objects in the tissue may be found, as shown in the video: a nonabsorbable suture is seen and removed.