See Clinical Research on Page 436
The discovery of blood pressure lowering in the 1980s and the use of angiotensin-receptor blockers in the early 2000s were significant advances in protecting the kidney and the cardiovascular system from the ravages of type 2 diabetes. For nearly 2 decades, multiple interventions failed, including the use of combination renin-angiotensin system–blocking drugs.
The clinical observation in phase 2 clinical trials that the sodium-glucose co-transporter 2 (SGLT2) inhibitors lowered albuminuria among patients with type 2 diabetes prompted a phase 3 randomized clinical trial that culminated in the discovery of canagliflozin improving cardiorenal outcomes in this population.1 Soon thereafter, these observations were extended to patients with chronic kidney disease (CKD) without type 2 diabetes and slightly lower levels of albuminuria.2 Specifically, in the DAPA-CKD trial, it was noted that patients with albuminuria ranging between 200 and 5000 mg/g creatinine and estimated glomerular filtration rate between 25 and 75 ml/min per 1.73 m2 with and without type 2 diabetes had reduced cardiorenal outcomes owing to dapagliflozin.2
In 2020, with the nonsteroidal mineralocorticoid receptor antagonist (MRA), finerenone, in the FIDELIO-DKD trial in patients with CKD associated with type 2 diabetes, the kidney-specific adverse clinical outcomes were abrogated by 18% and clinical cardiovascular adverse outcomes were abrogated by 14%.3 In this trial, CKD was defined as albuminuria (30–5000 mg/g creatinine) with estimated glomerular filtration rate between 25 and 75 ml/min per 1.73 m2. Thus, a broader range of patients including all patients with A2 albuminuria were now included. In all the above-mentioned trials, blood pressure was controlled to <140/90 mm Hg and renin-angiotensin system–blocking drugs were prescribed in all patients. Effective cardioprotective therapies, such as statins and platelet-aggregation inhibitors, were used in most patients.
After a hiatus of 2 decades, we had 2 drugs in consecutive years which were approved by the US Food and Drug Administration for cardiorenal protection in patients with CKD associated with type 2 diabetes. The obvious question that emerged was whether the combination of the 2 drugs—finerenone and the SGLT2 inhibitors—will produce greater benefits than either drug alone.
Several considerations are noteworthy. Neither of these 2 trials had stratified randomization by the use of the competing cardiorenal protective drug because at the time the trials were designed, it was unclear whether either therapy was effective. Nevertheless, in the DAPA-CKD trial, including in the finerenone trials, there were a small number of patients who were on combination of the 2 drugs. For example, the DAPA-CKD study used steroidal MRA (spironolactone and eplerenone) in combination with dapagliflozin and FIDELIO-DKD and FIGARO-DKD studies used the SGLT2 inhibitors in combination with finerenone. Therefore, one could ask the question whether patients who received the combination benefited more than either therapy alone.
To address the question whether combination therapy (MRA + an SGLT2 inhibitor) provides as much protection as dapagliflozin alone, in this issue of the KI Reports, Provenzano et al.4 report a post hoc analysis of the moderating effect of use of steroidal MRA, such as eplerenone and spironolactone, on cardiorenal and renal-specific outcomes. In total, 4304 patients with or without type 2 diabetes and CKD were randomized 1:1 to placebo or dapagliflozin 10 mg once daily. Of these, 229 (5.3%) were on MRA at baseline; 109 were on dapagliflozin and 120 on placebo. Among the group of patients not prescribed an MRA, compared with placebo, dapagliflozin had HR of 0.60 (95% CI 0.50–0.72) for the cardiorenal outcome; among patients prescribed an MRA, the hazard ratio was 0.76 (95% CI 0.40–1.47) (Figure 1). There was no evidence of a moderating effect (P interaction = 0.59). Although there was no moderating effect of MRA use, the upper bound of the 95% CI among those prescribed an MRA had a risk that could be 47% greater. The increase in risk for kidney-specific outcome and its components estimated glomerular filtration rate decline > 50% or end-stage kidney disease likewise had an increased risk that could be between 35% and 58% higher. The outcomes of all-cause mortality and hospitalization for heart failure or cardiovascular death include the possibility of even higher risks, 95% and 77% higher, respectively.
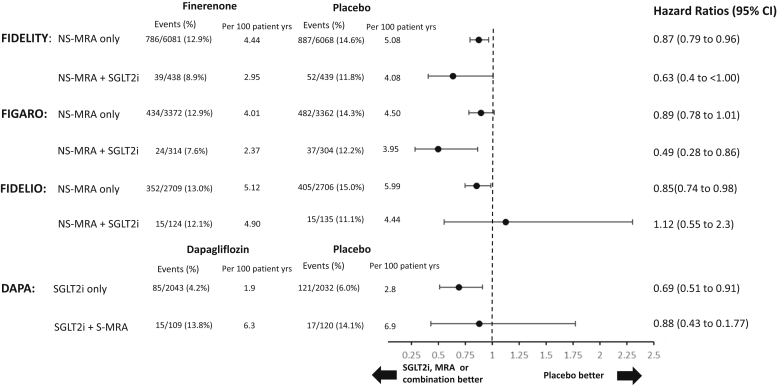
Figure 1.
Forest plot for cardiovascular outcomes in studies with the use of SGLT-2i, NS-MRA, and S-MRAs individually or in combination. MRA, mineralocorticoid receptor antagonist; NS-MRA, nonsteroidal mineralocorticoid antagonist; SGLT2i, sodium-glucose co-transporter 2 inhibitor; S-MRA, steroidal mineralocorticoid receptor antagonist.
In the FIDELIO-DKD studies, among a group of 259 of 5674 patients (4.6%) who received an SGLT2 inhibitor at baseline, compared with placebo, finerenone had HR of 1.38 (95% CI 0.61–3.10) for the primary composite kidney outcome.5 For the group who did not receive SGLT2 inhibitors at baseline, the HR was 0.82 (95% CI 0.72–0.92). There was no statistical evidence of a moderating effect of SGLT2 inhibitor use on the kidney composite outcomes (P interaction = 0.21)
Figure 1 illustrates the hazard ratios for the cardiovascular outcomes in the various trials. In the FIDELIO-DKD randomized clinical trial, evaluation of the 95% CI indicates that the cardiovascular risk associated with SGLT2 inhibitor use could be 130% greater. In the FIGARO-DKD randomized clinical trial, which used the same cardiovascular end point in patients with an earlier stage of CKD associated with type 2 diabetes, 618 of 7352 patients (8.4%) were on SGLT2 inhibitors.6 Finerenone use mitigated the cardiovascular risk among users of SGLT2 inhibitor use; among nonusers, the upper bound of the 95% CI exceeded 1. In the pooled analysis of the 2 trials, FIDELITY, in which 877 of 13,026 patients (6.7%) were on SGLT2 inhibitors, the HR for cardiovascular composite among SGLT2 inhibitor users was 0.63.7 The HR was 24% higher at 0.87 in nonusers. The combined analysis failed to detect a moderating influence of SGLT2 inhibitor use (P interaction = 0.41).
At first glance, comparing the HRs of cardiovascular outcomes in FIDELIO-DKD and FIGARO-DKD which provide disparate results—SGLT2 inhibitor use was associated with harms in FIDELIO-DKD and benefits in FIGARO-DKD. Nevertheless, the width of the CI is more important than the point estimate of the HR itself. When data were pooled in FIDELITY, the CIs shrink and both users and nonusers of SGLT2 inhibitors now have benefits. An increase in sample size reduced the width of the CIs. In a trial of 13,026 patients, only 6.7% were on SGLT2 inhibitors, and despite a difference of 24% in the HR, there was no statistically significant effect of moderation found. Despite that there were 13,026 patients, this can be interpreted as lack of power to detect a clinically meaningful effect owing to limited number of patients who received combination therapies of an MRA and an SGLT2 inhibitor in these trials. As pointed out by Kraemer et al.,8 “P values are not and should not be used to define moderators and mediators of treatment, because then moderator or mediator status would change with sample size”.
MRA and SGLT2 inhibitors act through different pathways to abrogate cardiovascular and kidney disease progression. It is therefore biologically plausible that the combination therapy is additive or even synergistic. At least one line of evidence found in the clinical trials points us in that direction. The baseline prescription of either an SGLT2 inhibitor or an MRA does not remove the ability of the complementary drug for reducing urine albumin-to-creatinine ratio. For example, reduction in urine albumin-to-creatinine ratio with finerenone was found with SGLT2 inhibitor at baseline was noted to be 31% (95% CI 29%–34%) and 25% (95% CI 10%–38%) when given by itself. Although the authors do not report the exact reductions in DAPA-CKD, the background use of MRA did not remove the ability of dapagliflozin to reduce urine albumin-to-creatinine ratio more. Furthermore, the use of SGLT2 inhibitor in combination with finerenone was associated with a reduced incidence of hyperkalemia (8.1% in users of SGLT2 inhibitor vs. 18.7% in nonusers of SGLT2 inhibitors). This might be another reason to use these 2 medications in combination.
Nevertheless, subgroup analyses such as these are associations, and before we take combination therapy of SGLT2 inhibitor and finerenone as the standard of care, some cautions are important. First, the SGLT2-inhibitor drugs in the finerenone trial or steroidal MRA use in the dapagliflozin trials was not randomly assigned. Therefore, imbalances may exist between therapies which often are not adjusted or accounted for. For example, in the finerenone trials, compared with patients not prescribed with SGLT2 inhibitors, the prescription of these drugs among people who had type 2 diabetes and CKD might have indicated more access to care, greater use of other cardioprotective medications, better delivery of care, greater adherence to therapy by the patients, and socioeconomic factors that all can influence cardiorenal outcomes. In the DAPA-CKD trial, compared with patients not treated with an MRA, patients treated with an MRA were also more likely to be treated with other cardiovascular therapies, such as diuretics, beta-blockers, statins, and antithrombotic agents. They were also more likely to have type 2 diabetes, a history of heart failure, a higher body mass index, and a higher urine albumin-to-creatinine ratio. Second, despite the large numbers of patients evaluated in these trials, the fraction of patients on a combination of MRA and an SGLT2 inhibitor was small. As noted previously, none of these trials were powered adequately to evaluate the interaction effect adequately. In fact, evaluation of the CIs reveals that there could be potential harms with the use of the combination therapy. In the DAPA-CKD study, for every clinical outcome evaluated, the upper bound of the CI in the combination therapy exceeded substantially over one. This may be a play of chance because of small numbers. Whether there could be a true harm cannot be answered owing to the post hoc nature of these analyses and limited power of the studies. Third, these trials do not tell us the consequences of simultaneously initiating MRA and the SGLT2 inhibitors. The combination therapies—when concurrently initiated—might elicit greater blood pressure declines, greater elevations in serum creatinine concentrations, and possibly faster progression. The subgroup analyses do not address these concerns.
Animal data suggest that compared with either drug alone, the combination of empagliflozin and finerenone might protect the kidney more.9 Now, we need randomized clinical trials to evaluate the value of combination therapies—compared with either alone—in protecting both the heart and the kidneys in patients with CKD associated with type 2 diabetes.
Disclosure
RA has served as a consultant, member of clinical trial steering committee, adjudication committee, and/or data safety monitoring committees of the following companies: Akebia, Bayer, Boehringer Ingelheim, Vifor, Reata, Diamedica, Chinook, and Vertex. BR declared no competing interests.
Acknowledgments
RA is supported by grants from the National Institutes of Health (R01HL126903) and the Veterans Affairs (5I01CX001753).
References
- 1.Perkovic V., Jardine M.J., Neal B., et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380:2295–2306. doi: 10.1056/NEJMoa1811744. [DOI] [PubMed] [Google Scholar]
- 2.Heerspink H.J.L., Stefansson B.V., Correa-Rotter R., et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383:1436–1446. doi: 10.1056/NEJMoa2024816. [DOI] [PubMed] [Google Scholar]
- 3.Bakris G.L., Agarwal R., Anker S.D., et al. Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes. N Engl J Med. 2020;383:2219–2229. doi: 10.1056/NEJMoa2025845. [DOI] [PubMed] [Google Scholar]
- 4.Provenzano M., Jongs N., Vart P., et al. The kidney protective effects of the sodium–glucose cotransporter-2 inhibitor, dapagliflozin, are present in patients with CKD treated with mineralocorticoid receptor antagonists. Kidney Int Rep. 2022;7:436–443. doi: 10.1016/j.ekir.2021.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rossing P., Filippatos G., Agarwal R., et al. Finerenone in predominantly advanced CKD and type 2 diabetes with or without sodium-glucose cotransporter-2 inhibitor therapy. Kidney Int Rep. Published online October 13, 2021 doi: 10.1016/j.ekir.2021.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pitt B., Filippatos G., Agarwal R., et al. Cardiovascular events with finerenone in kidney disease and type 2 diabetes. N Engl J Med. 2021;385:2252–2263. doi: 10.1056/NEJMoa2110956. [DOI] [PubMed] [Google Scholar]
- 7.Agarwal R, Filippatos G, Pitt B, et al. Cardiovascular and kidney outcomes with finerenone in patients with type 2 diabetes and chronic kidney disease: the FIDELITY pooled analysis. Eur Heart J. Forthcoming 2022. [DOI] [PMC free article] [PubMed]
- 8.Kraemer H.C., Wilson G.T., Fairburn C.G., Agras W.S. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 9.Kolkhof P., Hartmann E., Freyberger A., et al. Effects of finerenone combined with Empagliflozin in a model of hypertension-induced end-organ damage. Am J Nephrol. 2021;52:642–652. doi: 10.1159/000516213. [DOI] [PMC free article] [PubMed] [Google Scholar]