Abstract
Background
Age and comorbidities increase COVID-19 related in-hospital mortality risk, but the extent by which comorbidities mediate the impact of age remains unknown.
Methods
In this multicenter retrospective cohort study with data from 45 Dutch hospitals, 4806 proven COVID-19 patients hospitalized in Dutch hospitals (between February and July 2020) from the CAPACITY-COVID registry were included (age 69[58–77]years, 64% men). The primary outcome was defined as a combination of in-hospital mortality or discharge with palliative care. Logistic regression analysis was performed to analyze the associations between sex, age, and comorbidities with the primary outcome. The effect of comorbidities on the relation of age with the primary outcome was evaluated using mediation analysis.
Results
In-hospital COVID-19 related mortality occurred in 1108 (23%) patients, 836 (76%) were aged ≥70 years (70+). Both age 70+ and female sex were univariably associated with outcome (odds ratio [OR]4.68, 95%confidence interval [4.02–5.45], OR0.68[0.59–0.79], respectively;both p< 0.001). All comorbidities were univariably associated with outcome (p<0.001), and all but dyslipidemia remained significant after adjustment for age70+ and sex. The impact of comorbidities was attenuated after age-spline adjustment, only leaving female sex, diabetes mellitus (DM), chronic kidney disease (CKD), and chronic pulmonary obstructive disease (COPD) significantly associated (female OR0.65[0.55–0.75], DM OR1.47[1.26–1.72], CKD OR1.61[1.32–1.97], COPD OR1.30[1.07–1.59]). Pre-existing comorbidities in older patients negligibly (<6% in all comorbidities) mediated the association between higher age and outcome.
Conclusions
Age is the main determinant of COVID-19 related in-hospital mortality, with negligible mediation effect of pre-existing comorbidities.
Trial registration
CAPACITY-COVID (NCT04325412)
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-021-02673-1.
Keywords: COVID-19, Mortality, Hospitalization, Netherlands, Mediation analysis
Background
COVID-19 is a pandemic infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-19), which already accounts for over 5 million deaths worldwide [1]. COVID-19 related mortality is particularly high in the elderly [2–6]. Consequently, in the Netherlands, 90% of the deceased patients is 70 years or older [7].
Pre-existing comorbidities such as hypertension, diabetes mellitus (DM), dyslipidemia, chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), and history of cardiac diseases are also associated with an increased risk of COVID-19 related (in-hospital) mortality [8–12]. However, these comorbidities are also known to be more prevalent in the elderly [8, 9, 13]. It remains unknown to which extent the higher in-hospital mortality rate is mediated by the higher prevalence of these comorbidities in the elderly.
The aim of this study was to explore to which extent existing comorbidities mediate the increased risk of COVID-19 related in-hospital mortality relative to age in a registry of 4806 Dutch COVID-19 patients.
Methods
Study design and population
CAPACITY-COVID (NCT04325412) is an international patient registry established to investigate the role of cardiovascular disease in the COVID-19 pandemic [14, 15]. The details of this registry have been outlined in detail previously [15]. In short, adult patients (≥18 years) with (highly suspected) COVID-19 admitted to one of the participating hospitals were included in this registry [14]. Forty-five Dutch hospitals contributed to the registry. For the current analysis, consecutive patients from all participating Dutch hospitals with proven COVID-19 infection based on at least one positive PCR for SARS-CoV-2 (92% of the included subjects) and/or a chest CT scan strongly suggestive for SARS-CoV-2 infection, hospitalized between January and July 2020 (first COVID-19 wave in the Netherlands), were included [14–16]. In-hospital mortality was defined as a combination of in-hospital mortality or discharge with palliative care. The study was performed according to the Helsinki declaration and local ethics approval was obtained in all participating hospitals. Consent was obtained by either opt-in (when required by the local Medical Research Ethics Committee of the participating center) or opt-out approaches, following local regulations.
Statistical analyses
Variables are displayed as numbers (percentage), mean ± standard deviation (SD) or median and inter quartile ranges [IQR], as appropriate. Normality was assessed visually using Q-Q plots. Comparisons between groups were performed using chi-square tests for categorical data and for continuous variables by independent sample T-test or Mann Whitney-U test depending on normality of the distribution. Unadjusted binary logistic regression analysis was performed to analyze the associations between sex, age 60+, age 70+, a reported medical history of comorbidities (hypertension, DM, dyslipidemia, CKD, COPD, and a medical history of cardiac disease) and the comorbidity count (a sum of the presence of the before mentioned comorbidities categorized as 0 co-morbidities, 1–2 co-morbidities, and > 2 co-morbidities) with in-hospital mortality. Definitions of pre-existing comorbidities as specified in the case report form are provided in the Supplemental Methods (Additional file 1). Subsequently, adjusted binary logistic regression analysis – with adjustment for age 70+ and sex – was performed to determine the adjusted association between comorbidities and the comorbidity count with in-hospital mortality. Additionally, given the non-linear relationship between age and in-hospital mortality, age-restricted cubic spline adjusted logistic regression models were constructed for sex and the comorbidities [17].
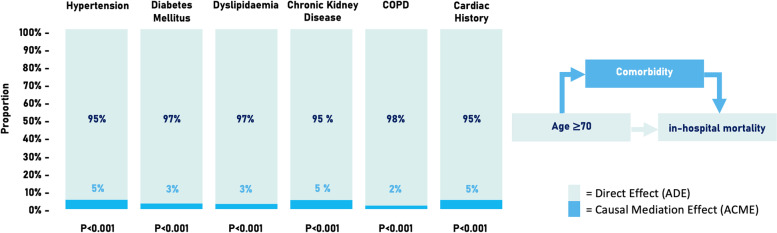
R mediation package 4.5.0 was used to perform the mediation analysis [18]. The mediation analysis tests whether a clinical variable (in this case age 70+) affects outcome through a mediator variable (in this case the co-morbidities) and to which extent. This divides the total effect of the model into a direct effect, called the average direct effect (ADE), and an indirect effect, called the average causal mediation effect (ACME). The proportion of ADE and ACME and the 95% confidence intervals (using 1000x bootstrapping) were calculated and visualized for each comorbidity studied. Statistical analyses were conducted in R, and figures were made using the packages ggplot2 and forest plot [19–21]. Statistical significance was defined as a P value < 0.05.
Results
Patient characteristics
In total, 4806 patients fulfilled the inclusion criteria and were included in this study. Clinical characteristics stratified by age < 70 and ≥ 70 years are outlined in Table 1. The median age was 69 [58–77] years, and approximately two-third were men (63%, N = 3051). All pre-existing comorbidities were more prevalent in the elderly (aged ≥70 years, all p < 0.001). Male patients more often had dyslipidemia (46% vs 39%), a history of cardiac disease (39% vs 30%, especially coronary artery disease and arrhythmias) and presence of two or more comorbidities when compared to women (39% vs 33%, Additional file 2).
Table 1.
Clinical characteristics of patients aged < 70 and aged ≥70 (70+) years
| < 70 (N = 2504) |
70+ (N = 2302) |
Total (N = 4806) |
P-value | |
|---|---|---|---|---|
| Clinical Presentation | ||||
| Age, years | 58 [51–64] | 77 [73–82] | 69 [58–77] | < 0.001 |
| Female | 910 (36%) | 845 (37%) | 1755 (37%) | 0.793 |
| BMI, kg/m2 | 27.9 [25.1–31.2] | 26.7 [24.0–30.1] | 27.3 [24.5–30.8] | < 0.001 |
| Temperature, °C | 37.9 ± 1.1 | 37.7 ± 1.1 | 37.8 ± 1.1 | < 0.001 |
| Heart rate, bpm | 91 [80–103] | 86 [75–99] | 89 [77–101] | < 0.001 |
| Systolic BP, mmHg | 133 ± 21 | 136 ± 24 | 135 ± 23 | < 0.001 |
| Diastolic BP, mmHg | 78 ± 14 | 75 ± 15 | 77 ± 15 | < 0.001 |
| Breathing rate, rpm | 22 [18–26] | 21 [18–26] | 22 [18–26] | 0.620 |
| Oxygen saturation, So2% | 95 [92–97] | 95 [92–96] | 95 [92–97] | < 0.001 |
| Medical History, n (%) | ||||
| Hypertension | 1036 (41%) | 1720 (75%) | 2756 (57%) | < 0.001 |
| Diabetes Mellitus | 512 (20%) | 701 (31%) | 1213 (25%) | < 0.001 |
| Dyslipidemia | 764 (31%) | 1303 (57%) | 2067 (43%) | < 0.001 |
| Chronic Kidney Disease | 127 (5%) | 392 (17%) | 519 (11%) | < 0.001 |
| COPD | 206 (8%) | 373 (16%) | 579 (12%) | < 0.001 |
| Cardiac disease | 488 (20%) | 1218 (53%) | 1706 (36%) | < 0.001 |
| Arrhyth./Conduc. | 160 (6%) | 612 (27%) | 772 (16%) | < 0.001 |
| Heart Failure | 46 (2%) | 228 (10%) | 274 (6%) | < 0.001 |
| Coronary Artery Disease | 249 (10%) | 574 (25%) | 823 (17%) | < 0.001 |
| Valvular Heart Disease | 50 (2%) | 201 (9%) | 251 (5%) | < 0.001 |
| Comorbidity count | < 0.001 | |||
| 0 comorbidities | 1073 (43%) | 250 (11%) | 1323 (28%) | |
| 1–2 comorbidities | 896 (36%) | 842 (37%) | 1738 (36%) | |
| > 2 comorbidities | 535 (21%) | 1210 (53%) | 1745 (36%) | |
Arrhyth arrhythmias, BMI body mass index, BP blood pressure, Conduc conduction disorders, COPD chronic obstructive pulmonary disease
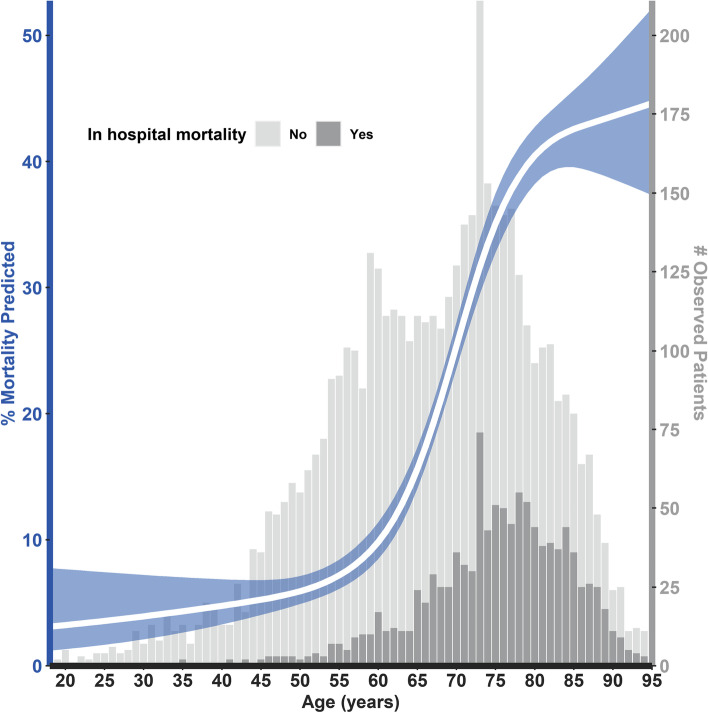
Median duration of hospitalization was 7 [4 - 15] days. In-hospital mortality (N = 1066, 96%) or palliative discharge (N = 42, 4%) occurred in 1108 (23%) patients, of which 836 (76%) were aged 70+ and 272 (24%) were aged < 70 (p < 0.001; Table 2). The observed and predicted association between age (splined adjusted) and in-hospital mortality are shown in Fig. 1. Male sex and the individual comorbidities were more prevalent, and comorbidity count per patient was higher in the in-hospital mortality group (p < 0.001, Table 2). In total, 1312 (27%) patients were referred to the intensive care unit (ICU) during hospitalization, of which 446 were aged 70+ (34%) and 866 (66%) were aged < 70 (p < 0.001).
Table 2.
Clinical characteristics of patients with and without event
| No mortality or Palliative Care (N = 3698) |
Mortality or Palliative Care (N = 1108) |
Total (N = 4806) |
P-value | |
|---|---|---|---|---|
| Clinical Presentation | ||||
| Age, years | 65 [56–74] | 76 [70–82] | 69 [58–77] | < 0.001 |
| Female | 1423 (39%) | 332 (30%) | 1755 (37%) | < 0.001 |
| BMI, kgm−2 | 27.5 [24.7–30.8] | 26.8 [24.1–30.5] | 27.3 [24.5–30.8] | 0.010 |
| Temperature, °C | 37.8 ± 1.1 | 37.8 ± 1.1 | 37.8 ± 1.1 | 0.454 |
| Heart rate, bpm | 89 [78–100] | 90 [77–103] | 89 [77–101] | 0.087 |
| Systolic BP, mmHg | 135 ± 22 | 134 ± 25 | 135 ± 23 | 0.301 |
| Diastolic BP, mmHg | 77 ± 14 | 73 ± 16 | 77 ± 15 | < 0.001 |
| Breathing rate, rpm | 20 [17–25] | 24 [19–28] | 22 [18–26] | < 0.001 |
| Oxygen saturation, So2% | 95 [93–97] | 94 [91–96] | 95 [92–97] | < 0.001 |
| Medical History | ||||
| Hypertension | 1979 (54%) | 777 (70%) | 2756 (57%) | < 0.001 |
| Diabetes Mellitus | 835 (23%) | 378 (34%) | 1213 (25%) | < 0.001 |
| Dyslipidemia | 1479 (40%) | 588 (53%) | 2067 (43%) | < 0.001 |
| Chronic Kidney Disease | 311 (8%) | 208 (19%) | 519 (11%) | < 0.001 |
| COPD | 389 (11%) | 190 (17%) | 579 (12%) | < 0.001 |
| Cardiac disease | 1170 (32%) | 536 (48%) | 1706 (36%) | < 0.001 |
| Arrhyth./Conduc. | 509 (14%) | 263 (24%) | 772 (16%) | < 0.001 |
| Heart Failure | 168 (5%) | 106 (10%) | 274 (6%) | < 0.001 |
| Coronary Artery Disease | 540 (15%) | 283 (26%) | 823 (17%) | < 0.001 |
| Valvular Heart Disease | 155 (4%) | 96 (9%) | 251 (5%) | < 0.001 |
| Comorbidity count | < 0.001 | |||
| 0 comorbidities | 1164 (32%) | 159 (14%) | 1323 (28%) | |
| 1–2 comorbidities | 1354 (37%) | 384 (35%) | 1738 (36%) | |
| > 2 comorbidities | 1180 (32%) | 565 (51%) | 1745 (36%) | |
Arrhyth arrhythmias, BMI body mass index, BP blood pressure, Conduc conduction disorders, COPD chronic obstructive pulmonary disease
Fig. 1.
Predicted and observed in-hospital mortality (univariable age-restricted cubic spline adjusted). % Mortality predicted: The white line represents the predicted mortality rates at different ages, accompanied by 95% confidence intervals in blue. # Observed patients: The grey bars represent the number of patients observed within the different age categories. The light grey bars are the patients that were discharged without palliative care. The dark grey bars are the patients in which in-hospital mortality (or palliative discharge) occurred
Univariable and multivariable associations and mediation effect of comorbidities and in-hospital mortality
Higher age (70+), male sex, and the individual comorbidities were all significantly associated with in-hospital mortality in univariable analysis (all p < 0.001; Fig. 2A). Hypertension, DM, CKD, COPD and a history of cardiac disease remained significantly associated after adjustment for age 70+ and sex (hypertension odds ratio [OR] 1.29, 95% confidence interval [CI] 1.10–1.51, p = 0.001; DM OR 1.55 [1.33–1.81], p < 0.001; dyslipidemia OR 1.15 [1.00–1.34], p = 0.053; CKD OR 1.74 [1.43–2.13], p < 0.001; COPD OR 1.41 [1.15–1.72], p < 0.001; history of cardiac disease OR 1.22 [1.05–1.41], p = 0.010, Fig. 2B). Additionally, given the non-linear relationship between age and in-hospital mortality, age-spline adjusted analysis was performed for the association of sex and all comorbidities with in-hospital mortality (Fig. 2C). The effects were attenuated after age-spline adjustment, only leaving sex, DM, CKD, and COPD significantly associated with in-hospital mortality (female OR 0.65 [0.55–0.75], p < 0.001; DM OR 1.47 [1.26–1.72], p < 0.001; CKD OR 1.61 [1.32–1.97], p < 0.001; COPD OR 1.30 [1.07–1.59], p = 0.010, Fig. 2C).
Fig. 2.
Associations of age and comorbidities with in-hospital mortality. A) Univariable association of age 70+, sex, and comorbidities with in-hospital mortality; B) Association of all comorbidities after adjustment for age 70+ and sex; C) Association of sex and all comorbidities after age spline adjustment. COPD = chronic obstructive pulmonary disease
Uni- and multivariable (spline-adjusted) analysis of comorbidity count revealed a significant, univariable association with in-hospital mortality (p < 0.001; Additional file 3), which remained significant in the multivariable model with an attenuated effect. In the age-spline multivariable adjusted analysis, the association of the comorbidity count was not significant for a comorbidity count of 1–2 (OR 1.15 [0.9–1.4]) and attenuated for > 2 comorbidity count (OR 1.4 [1.1–1.7]).
All individual comorbidities significantly mediated the association between age 70+ and in-hospital mortality (ACME; Fig. 3). However, the proportion of this eff ect was below 6% for all comorbidities, and thereby the increased risk of in-hospital mortality in the elderly was explained mainly by the direct effect (ADE; Fig. 3) of age 70+ within this analysis (Fig. 3). Additionally, a mediation analysis was performed to quantify the mediation effect of a comorbidity count > 2 on the association between age and in-hospital mortality. Although the proportion of this effect was higher than the comorbidities separately, it remained minimal (8%, p < 0.001, Additional file 4).
Fig. 3.
Mediation analysis with age ≥ 70 years as independent predictor, the individual comorbidities as mediator and in-hospital mortality as outcome. All comorbidities partly mediated the effect of age on in-hospital mortality (all p-values < 0.001). The mediation effect was 5% (95% CI 2–9%) for hypertension, 3% (95% CI 2–4%) for diabetes mellitus, 3% (95% CI 0.4–6%) for dyslipidemia, 5% (95% CI 3–7%) for chronic kidney disease, 2% (95% CI 1–3%) for COPD, and 5% (95% CI 2–9%) for history of cardiac disease. COPD = chronic obstructive pulmonary disease
Age-spline plots showed a steep increase in the predicted risk of in-hospital mortality from 60 years and higher (Fig. 1; analysis stratified by sex and the individual comorbidities is shown in Additional file 5). Correspondingly, in-hospital mortality rates were significantly lower in patients < 60 years when compared to the older patients (age 60+ years, 6% (N = 87) vs 30% (N = 1021), p < 0.001; Additional file 6). All comorbidities also occurred less frequently in this younger patient group (Additional file 6). None of the co-morbidities, except for history of cardiac disease, were significantly associated with in-hospital mortality in univariable analysis in patients < 60 years (hypertension OR 1.31 [0.83–2.06], p = 0.240; DM OR 1.38 [0.82–2.35], p = 0.228; dyslipidemia OR 1.26 [0.76–2.10], p = 0.367; CKD OR 2.33 [0.96–5.66], p = 0.062; COPD OR 0.62 [0.19–2.00], p = 0.421; history of cardiac disease OR 1.90 [1.10–3.27], p = 0.021, Additional file 7). In the total patient population, age 60+ was significantly associated with in-hospital mortality (OR 6.35[5.05–7.98], p < 0.001; Additional file 7A).
Discussion
This study reveals that higher age is the main determinant of COVID-19 related in-hospital mortality in the Netherlands. While pre-existing comorbidities (including hypertension, DM, dyslipidemia, CKD, COPD, and cardiac diseases) are more prevalent in the elderly, their mediation effect on COVID-19 related in-hospital mortality is minimal.
Over the last months, studies revealed multiple risk factors independently associated with COVID-19 related (in-hospital) mortality, including higher age, pre-existing co-morbidities, and male sex, which is in line with current findings [9, 10, 22–25]. A recent study of 2273 COVID-19 hospitalized Dutch patients showed that a mortality prediction model using ten clinical features including age, number of home medications, admission blood values urea nitrogen/LDH/albumin, oxygen saturation, blood gas pH and history of chronic cardiac disease, improved discrimination over age-based decision rules only [26]. Nonetheless, no data regarding to which extent age and cardiovascular comorbidities contributed to the mortality risks were provided. We show that the contributing effect of pre-existing comorbidities is minimal relative to age.
In the Netherlands, the vast majority (90%) of deceased patients due to COVID-19 is over 70 years of age. The prevalence of comorbidities among hospitalized COVID-19 patients is particularly high, especially in the elderly [7, 8]. The current study included 4806 patients from 45 Dutch - both academic and local - hospitals, accounting for around 40% of all COVID-19 related hospitalizations between January 2020 and July 2020 in the Netherlands [7]. Therefore, this study population adequately represents the total hospitalized population during the first COVID-19 pandemic wave in the Netherlands. The higher prevalence of male COVID patients observed in the current registry and the increased mortality risk of males is in line with previous findings and likely due to a less effective viral control of the immune system in males [24, 27], together with the higher comorbidity rates in males compared to females [24, 28]. The observed association between a medical history of a cardiac disease and in-hospital mortality in the young has been studied and discussed before by current consortium, which is mainly driven by the presence of severe (NYHA≥3) heart failure [29].
It is important to notice that during the first wave of COVID-19, the median age of people referred to the ICU department decreased when the total number of patients referred to the ICU department increased [30]. Younger (< 70+) patients were possibly more likely to be referred to the ICU department due to bed shortages. However, the percentage of patients aged 70+ in the COVID-19 related mortality group in the current study (76%) is lower than the overall percentage of subjects aged 70+ of the COVID-19 related deaths in the Netherlands in 2020 (90%) [31]. This likely results from fewer referrals of elderly patients to the hospitals (possibly even independent of the presence of comorbidities) due to the overwhelming stress on hospitals during the first COVID-19 wave. Nonetheless, even in the group aged < 60 years - in whom likely no or limited referral “restrictions” were present - the effect of pre-existing comorbidities on mortality was limited in the current study, indicating that age as such is likely the main driver of COVID-19 related in-hospital mortality.
Our study revealed that pre-existing co-morbidities, highly prevalent in the elderly, contributed minimally to in-hospital mortality when compared to age. Moreover, the contribution of the comorbidities to outcome in patients aged < 60 years was limited to a history of cardiac disease without any significant association for DM, CKD, and COPD. As a result, the present study stresses the need for primary preventive efforts to protect the elderly (males) from an infection with SARS-CoV-19.
Limitations
There are some study limitations that need to be addressed, including its retrospective design. Additionally, data concerning the patients’ frailty and the reasons for not referring patients to the hospital or the ICU, were not collected within this registry. To which extent the lower hospital and ICU referral rate of the elderly and frailty contributed to the in-hospital mortality rate could therefore not be assessed and requires further research. Such research could help to better understand the association of higher age and in-hospital mortality beyond the comorbidities and might guide decision making on treatment, counselling and admission to high care facilities in the future.
Conclusion
Age is the main determinant of COVID-19 related in-hospital mortality, which is negligibly mediated by pre-existing comorbidities in the Netherlands.
Supplementary Information
Additional file 1. Supplemental methods.
Additional file 2. Clinical characteristics of males and females.
Additional file 3. Univariable, and Multivariable and Age cubic Spline adjusted association of Age, Gender, and comorbidity count with in-hospital mortality.
Additional file 4. Mediation analysis with Age ≥ 70 as independent predictor, multi-comorbidity (> 2 comorbidities) as mediator and in-hospital mortality as outcome.
Additional file 5. Age-spline adjusted associations with predicted in-hospital mortality, stratified for: A) sex; B) number of comorbidities; C) hypertension; D) diabetes mellitus; E) dyslipidemia; F) chronic kidney disease; G) chronic obstructive pulmonary disease (COPD); H) cardiac disease.
Additional file 6. Clinical characteristics of patients below and ≥ 60 years of age.
Additional file 7. A) Univariable association of Age 60+ with in-hospital mortality in the total cohort B) Univariable association of sex and comorbidities with in-hospital mortality in patients younger than 60 years.
Acknowledgements
We want to express our gratitude and appreciation to all participating sites and researchers part of the CAPACITY-COVID collaborative consortium. CAPACITY-COVID gratefully acknowledges the following organizations for their assistance in the development of the registry and/or coordination regarding the data registration in the collaborating centres: partners of the Dutch CardioVascular Alliance (DCVA), the Dutch Association of Medical Specialists (FMS), and the British Heart Foundation Centers of Research Excellence. In addition, the consortium is grateful for the endorsement of the CAPACITY-COVID initiative by the European Society of Cardiology (ESC), the European Heart Network (EHN), and the Society for Cardiovascular Magnetic Resonance (SCMR). Furthermore, the consortium appreciates the endorsement of CAPACITY-COVID as a flagship research project within the National Institute for Health Research (NIHR)/British Heart Foundation (BHF) Partnership framework for COVID-19 research. Part of this work is supported by the BigData@Heart Consortium, funded by the Innovative Medicines Initiative-2 joint undertaking under grant agreement no. 116074. This joint undertaking receives support from the EU’s Horizon 2020 research and innovation programme and EFP IA.
CAPACITY-COVID collaborative consortium (listed alphabetically)
Al-Ali AK1, Al-Muhanna FA2, Al-Windy NYY3, Almubarak YA4, Alnafie AN5, Alshahrani M6, Alshehri AM7, Anthonio RL8, Asselbergs FW9,10,11, Aujayeb A12, ten Berg JM13, van Boxem AJM14, Captur G11,15, Caputo M16,17, Charlotte N18, Dark P19, De Sutter J20,21, Delsing CE22, Dorman HGR23, Drost JT24, Emans ME25, Ferreira JB26, Gabriel L27, van Gilst WH28, Groenemeijer BE29, Haerkens-Arends HE30, van der Harst P9, Hedayat B31, van der Heijden DJ32, Hellou E33, Hermanides RS34, Hermans-van Ast JF35, van Hessen MWJ36, Heymans SRB37,38,39, van der Horst ICC40,41, van Ierssel SH42, Jewbali LS43,44, Kearney MT45, van Kesteren HAM46, Kietselaer BLJH47, Koning AMH48, Kopylov PY49, Kuijper AFM50, Kwakkel-van Erp JM51, van der Linden MMJM52, Linschoten M9, Linssen GCM53, Macias Ruiz R54, Magdelijns FJH55, Martens FMAC56, McCann GP57, van der Meer P58, Meijs MFL59, Messiaen P60,61, Monraats PS62, Montagna L63, Moriarty A64, Mosterd A65, Nierop PR66, van Ofwegen-Hanekamp CEE67, Pinto YM68, Poorhosseini H69, Prasad S70,71, Redón J72,73, Reidinga AC74, Ribeiro MIA75, Ripley DP76, Salah R77, Saneei E78, Saxena M79, Schaap J80,81, Schellings DAAM82, Schut A80, Shafiee A83, Shore AC84, Siebelink HJ85, van Smeden M86, Smits PC87, Pisters R88, Tessitore E89, Tieleman RG28,90, Timmermans P Jr91, Tio RA92,93, Tjong FVY68,94,95, den Uil CA43,44,96, Van Craenenbroeck EM97, van Veen HPAA98, Veneman T99, Verschure DO100, de Vries JK101, van de Wal RMA102, van de Watering DJ103, Westendorp ICD104, Westendorp PHM105, Weytjens C106, Wierda E95, Williams B107, Woudstra P108, Wu KW109, Zaal R110, Zaman AG111, van der Zee PM112.
1. Department of Clinical Biochemistry, King Fahd Hospital of the University, Imam Abdulrahman Bin Faisal University, Alkhobar, Saudi Arabia.
2. Department of Internal Medicine, King Fahd Hospital of the University, Imam Abdulrahman Bin Faisal University, Alkhobar, Saudi Arabia.
3. Department of Cardiology, Gelre Hospital Zutphen, Zutphen, the Netherlands.
4. Department of Critical Care, King Fahd Hospital of the University, Imam Abdulrahman Bin Faisal University, Alkhobar, Saudi Arabia.
5. Department of Pathology, King Fahd Hospital of the University, Imam Abdulrahman Bin Faisal University, Alkhobar, Saudi Arabia.
6. Department of Emergency Medicine, King Fahd Hospital of the University, Imam Abdulrahman Bin Faisal University, Alkhobar, Saudi Arabia.
7. Department of Internal Medicine, Cardiology Section, King Fahd Hospital of the University, Imam Abdulrahman Bin Faisal University, Alkhobar, Saudi Arabia.
8. Department of Cardiology, Treant Zorggroep, Emmen, the Netherlands.
9. Department of Cardiology, Division of Heart and Lungs, University Medical Center Utrecht, Utrecht University, Utrecht, the Netherlands.
10. Health Data Research United Kingdom and Institute of Health Informatics, University College London, London, United Kingdom.
11. Institute of Cardiovascular Science, Faculty of Population Health Sciences, University College London, London, United Kingdom.
12. Department of Respiratory and Acute Medicine, Northumbria Healthcare NHS Foundation Trust, Newcastle, United Kingdom.
13. Department of Cardiology, St. Antonius Hospital, Nieuwegein, the Netherlands.
14. Department of Pulmonology, Bravis Hospital, Roosendaal, the Netherlands.
15. Department of Cardiology, Royal Free London NHS Foundation Trust, London, United Kingdo.
16. Bristol Heart Institute, University Hospitals Bristol and Weston NHS Foundation Trust, Bristol, United Kingdom.
17. Bristol Medical School, University of Bristol, Bristol, United Kingdom.
18. Department of Cardiology, SSR Val Rosay, Saint Didier au Mont d’Or, Franc.
19. Department of Critical Care, Salford Royal NHS Foundation Trust, Salford, United Kingdom.
20. Department of Cardiology, AZ Maria Middelares, Ghent, Belgium.
21. Department of Internal Medicine, Ghent University, Ghent, Belgium.
22. Department of Internal Medicine and Infectious Diseases, Medisch Spectrum Twente, Enschede, the Netherlands.
23. Department of Cardiology, Bravis Hospital, Roosendaal, the Netherlands.
24. Department of Cardiology, Saxenburgh Medical Center, Hardenberg, the Netherlands.
25. Department of Cardiology, Ikazia Hospital, Rotterdam, the Netherlands.
26. Department of Cardiology, Hospital Professor Doutor Fernando Fonseca, Amadora, Portugal.
27. Department of Cardiology, CHU UCL Namur site Godinne, Université Catholique de Louvain, Yvoir, Belgium.
28. Department of Cardiology, University Medical Center Groningen, Groningen, the Netherlands.
29. Department of Cardiology, Gelre Hospital Apeldoorn, Apeldoorn, the Netherlands.
30. Department of Cardiology, Jeroen Bosch Hospital, ‘s-Hertogenbosch, the Netherlands.
31. Department of Cardiology, Tehran Heart Center, Cardiovascular Diseases Research Institute, Tehran University of Medical Sciences, Tehran, Iran.
32. Department of Cardiology, Haaglanden Medical Center, the Hague, the Netherlands.
33. Department of Cardiology, E.M.M.S. Hospital, Nazareth, Israel.
34. Department of Cardiology, Isala Hospital, Zwolle, the Netherlands.
35. Durrer Center, Netherlands Heart Institute, Utrecht, the Netherlands.
36. Department of Cardiology, Groene Hart Hospital, Gouda, the Netherlands.
37. Department of Cardiology, Cardiovascular Research Institute Maastricht (CARIM), Maastricht University Medical Center+, Maastricht, the Netherlands.
38. Department of Cardiovascular Sciences, Center for Molecular and Vascular Biology, KU Leuven, Belgium.
39. The Netherlands Heart Institute, Utrecht, the Netherlands.
40. Department of Intensive Care, Maastricht University Medical Center+, Maastricht University, Maastricht, the Netherlands.
41. Cardiovascular Research Institute Maastricht (CARIM), Maastricht University Medical Center, Maastricht, the Netherlands.
42. Department of General Internal Medicine, Infectious Diseases and Tropical Medicine, Antwerp University Hospital, Antwerp, Belgium.
43. Department of Cardiology, Erasmus MC University Medical Center, Rotterdam, the Netherlands.
44. Department of Intensive Care, Erasmus MC University Medical Center, Rotterdam, the Netherlands.
45. Leeds Institute for Cardiovascular and Metabolic Medicine, University of Leeds, Leeds, United Kingdom.
46. Department of Cardiology, Admiraal de Ruyter Hospital, Goes, the Netherlands.
47. Department of Cardiology, Zuyderland Medical Center, Heerlen, the Netherlands.
48. Department of Gynaecology, Amstelland Hospital, Amstelveen, the Netherlands.
49. World-Class Research Center Digital Biodesign and Personalized Healthcare, I.M. Sechenov First Moscow State Medical University, Sechenov University, Moscow, Russia.
50. Department of Cardiology, Spaarne Gasthuis, Haarlem, the Netherlands.
51. Department of Pulmonology, Antwerp University Hospital, University of Antwerp, Edegem, Belgium.
52. Department of Cardiology, Franciscus Vlietland, Schiedam, the Netherlands.
53. Department of Cardiology, Ziekenhuis Groep Twente (ZGT), Almelo, the Netherlands.
54. Arrhythmias Unit, Department of Cardiology, Hospital Universitario Virgen de las Nieves, Granada, Spain.
55. Department of Internal Medicine, Division of General Internal Medicine, Section Geriatric Medicine, Cardiovascular Research Institute Maastricht (CARIM), Maastricht University Medical Center+, Maastricht, the Netherlands.
56. Department of Cardiology, Deventer Hospital, Deventer, the Netherlands.
57. Department of Cardiovascular Sciences, University of Leicester and Cardiovascular Theme, National Institute for Health Research (NIHR) Leicester Biomedical Research Center, Glenfield Hospital, Leicester, United Kingdom.
58. Department of Cardiology, LangeLand Hospital, Zoetermeer, the Netherlands.
59. Department of Cardiology, Thorax Center Twente, Medisch Spectrum Twente, Enschede, the Netherlands.
60. Department of Infectious Diseases & Immunity, Jessa Hospital, Hasselt, Belgium.
61. Faculty of Medicine and Life Sciences, Hasselt University, Hasselt, Belgium.
62. Department of Cardiology, Elizabeth-TweeSteden Hospital, Tilburg, the Netherlands.
63. Department of Cardiology, A.O.U. San Luigi Gonzaga, Orbassano, Turin, Italy.
64. Cardiovascular Research Unit, Craigavon Area Hospital, Southern Health and Social Care Trust, Portadown, Nothern Ireland.
65. Department of Cardiology, Meander Medical Center, Amersfoort, the Netherlands.
66. Department of Cardiology, Franciscus Gasthuis, Rotterdam, the Netherlands.
67. Department of Cardiology, Diakonessenhuis, Utrecht, the Netherlands.
68. Amsterdam University Medical Center, University of Amsterdam, Heart Center; Department of Clinical and Experimental Cardiology, Amsterdam Cardiovascular Sciences, Amsterdam, the Netherlands.
69. Department of Interventional Cardiology, Tehran Heart Center, Cardiovascular Diseases Research Institute, Tehran University of Medical Sciences, Tehran, Iran.
70. National Heart and Lung Institute, Imperial College, London, United Kingdom.
71. Royal Brompton Hospital, London, United Kingdom.
72. Department of Internal Medicine, Clinic University Hospital, INCLIVA Health Research Institute, Valencia, Spain.
73. Department of Medicine, School of Medicine, University of Valencia, Valencia, Spain.
74. Department of Intensive Care, Martini Hospital, Groningen, the Netherlands.
75. Intensive Care Unit, Hospital do Espírito Santo, Évora, Portugal.
76. Department of Cardiology, Northumbria Healthcare NHS Foundation Trust, Newcastle, United Kingdom.
77. Benha Faculty of Medicine, Benha, Egypt.
78. Department of Nursing, Tehran Heart Center, Cardiovascular Diseases Research Institute, Tehran University of Medical Sciences, Tehran, Iran.
79. Barts National Institute for Health Research (NIHR) Biomedical Research Center, William Harvey Research Institute, Queen Mary University of London, United Kingdom.
80. The Dutch Network for Cardiovascular Research (WCN), Utrecht, the Netherlands.
81. Department of Cardiology, Amphia Hospital, the Netherlands.
82. Department of Cardiology, Slingeland Hospital Doetinchem, the Netherlands.
83. Department of Cardiovascular Research, Tehran Heart Center, Cardiovascular Diseases Research Institute, Tehran University of Medical Sciences, Tehran, Iran.
84. National Institute for Health Research (NIHR) Exeter Clinical Research Facility, Royal Devon and Exeter Hospital and University of Exeter College of Medicine & Health, Exeter, United Kingdom.
85. Department of Cardiology, Leiden University Medical Center, Leiden, the Netherlands.
86. Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht University, Utrecht, the Netherlands.
87. Department of Cardiology, Maasstad Hospital, Rotterdam, the Netherlands.
88. Department of Cardiology, Rijnstate Hospital, Arnhem, the Netherlands.
89. Department of Cardiology, University Hospitals of Geneva, Geneva, Switzerland.
90. Department of Cardiology, Martini Hospital, Groningen, the Netherlands.
91. Department of Cardiology, Heart Center Hasselt, Jessa Hospital, Hasselt, Belgium.
92. Department of Cardiology, Catharina Hospital, Eindhoven, the Netherlands.
93. Department of Educational Development and Research in the Faculty of Health, Medicine and Life Sciences, Catharina Hospital, Eindhoven, the Netherlands.
94. Department of Cardiology, Vrije Universiteit Amsterdam, Amsterdam Cardiovascular Sciences, Amsterdam, the Netherlands.
95. Department of Cardiology, Dijklander Hospital, Hoorn, the Netherlands.
96. Department of Intensive Care Medicine, Maasstad Hospital, Rotterdam, the Netherlands.
97. Cardiovascular Research, Antwerp University and Cardiology, Antwerp University Hospital, Antwerp, Belgium.
98. Department of Pulmonology, Medisch Spectrum Twente, Enschede, the Netherlands.
99. Department of Intensive Care, Ziekenhuis Groep Twente (ZGT), Almelo, the Netherlands.
100. Department of Cardiology, Zaans Medical Center, Zaandam, the Netherlands.
101. Department of Internal Medicine, Antonius Hospital, Sneek, the Netherlands.
102. Department of Cardiology, Bernhoven Hospital, Uden, the Netherlands.
103. Department of Cardiology, Albert Schweitzer Hospital, Dordrecht, the Netherlands.
104. Department of Cardiology, Rode Kruis Hospital, Beverwijk, the Netherlands.
105. Department of Cardiology, Beatrix Hospital, Gorinchem, the Netherlands.
106. Department of Cardiology, CHVZ, University Hospital Brussels, Jette, Belgium.
107. National Institute for Health Research Biomedical Research Center, University College London Hospitals, London, United Kingdom.
108. Department of Cardiology, Medical Center Leeuwarden (MCL), Leeuwarden, the Netherlands.
109. Department of Cardiology, van Weel-Bethesda Hospital, Dirksland, the Netherlands.
110. Department of Pulmonology, Ziekenhuis Groep Twente (ZGT), Almelo, the Netherlands.
111. Freeman Hospital, Newcastle Upon Tyne NHS Hospitals Foundation Trust and Newcastle University, Newcastle Upon Tyne, NE7 7DN, United Kingdom.
112. Department of Cardiology, St. Jansdal Hospital, Harderwijk, the Netherlands.
Abbreviations
- ADE
Average direct effect
- ACME
Average causal mediation effect
- CKD
Chronic kidney disease
- COPD
Chronic obstructive pulmonary disease
- SARS-CoV-19
severe acute respiratory syndrome coronavirus 2
- DM
Diabetes mellitus
- ICU
Intensive care unit
Authors’ contributions
MH, AR and ML were in the lead for data collection. MH, AR and JV were in the lead for the conception and design of the study, the analysis and interpretation of the data. MvS and PW helped with the analysis and interpretation of data. MH and AR were also in the lead for drafting the article. JV, ML, MvS, BvH, RT, MJ, RtB, MHazebroek, IvdH, FA, FM and SH provided additive contribution to the conception, design and interpretation of the data and critically revised the draft. All authors fulfil all three of the ICMJE guidelines for authorship: 1) substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; 2) drafting the article or revising it critically for important intellectual content; and 3) final approval of the version to be published.
Funding
The CAPACITY-COVID registry is supported by the Dutch Heart Foundation (2020B006 CAPACITY), the EuroQol Research Foundation, Novartis Global, Sanofi Genzyme Europe, Novo Nordisk Nederland, Servier Nederland, and Daiichi Sankyo Nederland. The Dutch Network for Cardiovascular Research (WCN), a partner within the CAPACITY-COVID consortium, received funding from the Dutch Heart Foundation (2020B006 CAPACITY) for site management and logistic support in the Netherlands. Marijke Linschoten is supported by the Alexandre Suerman Stipend of the University Medical Center Utrecht. Folkert W. Asselbergs is supported by CardioVasculair Onderzoek Nederland 2015–12 eDETECT and by the National Institute of Health Research (NIHR) University College London Hospitals Biomedical Research Centre.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was performed according to the Helsinki declaration and local ethics approval was obtained in all participating hospitals (Medisch Ethische ToetsingsCommissie Maastricht for MUMC). Informed consent (when required by local ethical committees) was obtained by either opt-in or opt-out approaches, following local regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
M. T. H. M. Henkens and A. G. Raafs contributed equally to this work.
F. W. Asselbergs and F. J. H. Magdelijns contributed equally to this work.
Contributor Information
M. T. H. M. Henkens, Email: michiel.henkens@mumc.nl
on behalf of the CAPACITY-COVID collaborative consortium:
A. K. Al-Ali, F. A. Al-Muhanna, N. Y. Y. Al-Windy, Y. A. Almubarak, A. N. Alnafie, M. Alshahrani, A. M. Alshehri, R. L. Anthonio, F. W. Asselbergs, A. Aujayeb, J. M. ten Berg, A. J. M. van Boxem, G. Captur, M. Caputo, N. Charlotte, P. Dark, J. De Sutter, C. E. Delsing, H. G. R. Dorman, J. T. Drost, M. E. Emans, J. B. Ferreira, L. Gabriel, W. H. van Gilst, B. E. Groenemeijer, H. E. Haerkens-Arends, P. van der Harst, B. Hedayat, D. J. van der Heijden, E. Hellou, R. S. Hermanides, J. F. Hermans-van Ast, M. W. J. van Hessen, S. R. B. Heymans, I. C. C. van der Horst, S. H. van Ierssel, L. S. Jewbali, M. T. Kearney, H. A. M. van Kesteren, B. L. J. H. Kietselaer, A. M. H. Koning, P. Y. Kopylov, A. F. M. Kuijper, J. M. Kwakkel-van Erp, M. M. J. M. van der Linden, M. Linschoten, G. C. M. Linssen, R. Macias Ruiz, F. J. H. Magdelijns, F. M. A. C. Martens, G. P. McCann, P. van der Meer, M. F. L. Meijs, P. Messiaen, P. S. Monraats, L. Montagna, A. Moriarty, A. Mosterd, P. R. Nierop, C. E. E. van Ofwegen-Hanekamp, Y. M. Pinto, H. Poorhosseini, S. Prasad, J. Redón, A. C. Reidinga, M. I. A. Ribeiro, D. P. Ripley, R. Salah, E. Saneei, M. Saxena, J. Schaap, D. A. A. M. Schellings, A. Schut, A. Shafiee, A. C. Shore, H. J. Siebelink, M. van Smeden, P. C. Smits, R. Pisters, E. Tessitore, R. G. Tieleman, P. Timmermans, Jr, R. A. Tio, F. V. Y. Tjong, C. A. den Uil, E. M. Van Craenenbroeck, H. P. A. A. van Veen, T. Veneman, D. O. Verschure, J. K. de Vries, R. M. A. van de Wal, D. J. van de Watering, I. C. D. Westendorp, P. H. M. Westendorp, C. Weytjens, E. Wierda, B. Williams, P. Woudstra, K. W. Wu, R. Zaal, A. G. Zaman, and P. M. van der Zee
References
- 1.WHO COVID-19 Dashboard. Geneva: World Health Organization, 2020. Available online: https://covid19.who.int/ (last cited: 16-07-2021).
- 2.Sun P, Lu X, Xu C, Sun W, Pan B. Understanding of COVID-19 based on current evidence. J Med Virol. 2020;92(6):548–551. doi: 10.1002/jmv.25722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu C, Chen X, Cai Y, Ja X, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA. Intern Med. 2020;180(7):934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, Bellani G, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020;180(10):1345–1355. doi: 10.1001/jamainternmed.2020.3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NHS Digital . Coronavirus (COVID-19): shielded patients list. 2020. [Google Scholar]
- 6.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rijksinstituut voor volksgezondheid (RIVM): Mortality rates, Coronadashboard, https://coronadashboard.rijksoverheid.nl/landelijk/sterfte (last cited: 16-7-2021). 2021.
- 8.Ariës MJH, van den Bergh JP, Beudel M, Boersma W, Dormans T, Douma RA, et al. Clinical course of COVID-19 in the Netherlands: an overview of 2607 patients in hospital during the first wave. Ned Tijdschr Geneeskd. 2021;165:1-5. [PubMed]
- 9.Posso M, Comas M, Román M, Domingo L, Louro J, González C, et al. Comorbidities and mortality in patients with COVID-19 aged 60 years and older in a University Hospital in Spain. Arch Bronconeumol. 2020;56(11):756–758. doi: 10.1016/j.arbres.2020.06.012. [DOI] [PubMed] [Google Scholar]
- 10.Zuccaro V, Celsa C, Sambo M, Battaglia S, Sacchi P, Biscarini S, et al. Competing-risk analysis of coronavirus disease 2019 in-hospital mortality in a northern Italian Centre from SMAtteo COvid19 REgistry (SMACORE) Sci Rep. 2021;11(1):1137. doi: 10.1038/s41598-020-80679-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study. Bmj. 2020;369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Atkins JL, Masoli JAH, Delgado J, Pilling LC, Kuo C-L, Kuchel GA, et al. Preexisting comorbidities predicting COVID-19 and mortality in the UK biobank community cohort. J Gerontol Ser A. 2020;75(11):2224–2230. doi: 10.1093/gerona/glaa183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Linschoten M, Asselbergs FW. CAPACITY-COVID: a European registry to determine the role of cardiovascular disease in the COVID-19 pandemic. Eur Heart J. 2020;41(19):1795–1796. doi: 10.1093/eurheartj/ehaa280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CAPACITY-COVID Collaborative Consortium and LEOSS Study Group. Clinical presentation, disease course, and outcome of COVID-19 in hospitalized patients with and without pre-existing cardiac disease: a cohort study across 18 countries. Eur Heart J. 2021:ehab656. 10.1093/eurheartj/ehab656. Epub ahead of print. PMID: 34734634. [DOI] [PubMed]
- 16.Wang Y, Kang H, Liu X, Tong Z. Combination of RT-qPCR testing and clinical features for diagnosis of COVID-19 facilitates management of SARS-CoV-2 outbreak. J Med Virol. 2020;92(6):538–539. doi: 10.1002/jmv.25721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harrell FE., Jr . Rms: regression modeling strategies. R package version 6.2-0. 2021. [Google Scholar]
- 18.Tingley D, Yamamoto T, Hirose K, Keele L, Imai K. Mediation: R package for causal mediation analysis. J Stat Softw. 2014;59(5):1–38. doi: 10.18637/jss.v059.i05. [DOI] [Google Scholar]
- 19.R Core Team . R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2021. [Google Scholar]
- 20.Max Gordon and Thomas Lumley . Forestplot: advanced Forest plot using 'grid' graphics. R package version 1.10.1. 2020. [Google Scholar]
- 21.Wickham H. ggplot2: elegant graphics for data analysis. New York: Springer-Verlag; 2016. [Google Scholar]
- 22.Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Inf Secur. 2020;81(2):e16–e25. doi: 10.1016/j.jinf.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mendes A, Serratrice C, Herrmann FR, Genton L, Périvier S, Scheffler M, et al. Predictors of in-hospital mortality in older patients with COVID-19: the COVIDAge study. J Am Med Dir Assoc. 2020;21(11):1546–54.e3. doi: 10.1016/j.jamda.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gebhard C, Regitz-Zagrosek V, Neuhauser HK, Morgan R, Klein SL. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ. 2020;11(1):29. doi: 10.1186/s13293-020-00304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mohamed MO, Gale CP, Kontopantelis E, Doran T, de Belder M, Asaria M, et al. Sex differences in mortality rates and underlying conditions for COVID-19 deaths in England and Wales. Mayo Clin Proc. 2020;95(10):2110–2124. doi: 10.1016/j.mayocp.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ottenhoff MC, Ramos LA, Potters W, Janssen MLF, Hubers D, Hu S, et al. Predicting mortality of individual patients with COVID-19: a multicentre Dutch cohort. BMJ Open. 2021;11(7):e047347. doi: 10.1136/bmjopen-2020-047347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peckham H, de Gruijter NM, Raine C, Radziszewska A, Ciurtin C, Wedderburn LR, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat Commun. 2020;11(1):6317. doi: 10.1038/s41467-020-19741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schiffer VMMM, Janssen EBNJ, van Bussel BCT, Jorissen LLM, Tas J, Sels J-WEM, et al. The "sex gap" in COVID-19 trials: a scoping review. EClinicalMedicine. 2020;29:100652. [DOI] [PMC free article] [PubMed]
- 29.Linschoten M, Peters S, van Smeden M, Jewbali LS, Schaap J, Siebelink HM, et al. Cardiac complications in patients hospitalised with COVID-19. Eur Heart J Acute Cardiovasc Care. 2020;9(8):817–823. doi: 10.1177/2048872620974605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Linschoten M, Nab L, van der Horst ICC, Tieleman R, Asselbergs FW. Response to "early hydroxychloroquine but not chloroquine use reduces ICU admission in COVID-19 patients". Int J Infect Dis. 2021;103:560–561. doi: 10.1016/j.ijid.2020.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rijksinstituut voor volksgezondheid (RIVM): Mortality rates, Coronadashboard. https://www.coronadashboardrijksoverheidnl/landelijk/sterfte. 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplemental methods.
Additional file 2. Clinical characteristics of males and females.
Additional file 3. Univariable, and Multivariable and Age cubic Spline adjusted association of Age, Gender, and comorbidity count with in-hospital mortality.
Additional file 4. Mediation analysis with Age ≥ 70 as independent predictor, multi-comorbidity (> 2 comorbidities) as mediator and in-hospital mortality as outcome.
Additional file 5. Age-spline adjusted associations with predicted in-hospital mortality, stratified for: A) sex; B) number of comorbidities; C) hypertension; D) diabetes mellitus; E) dyslipidemia; F) chronic kidney disease; G) chronic obstructive pulmonary disease (COPD); H) cardiac disease.
Additional file 6. Clinical characteristics of patients below and ≥ 60 years of age.
Additional file 7. A) Univariable association of Age 60+ with in-hospital mortality in the total cohort B) Univariable association of sex and comorbidities with in-hospital mortality in patients younger than 60 years.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.