Abstract
Aims
To identify virtual healthcare services and digital health technologies deployed in South Africa during coronavirus disease 2019 (COVID-19) and the challenges associated with their use.
Methods
To determine the status of digital health utilization during COVID-19 in South Africa, the preferred reporting items for systematic reviews and meta-analyses model was used to perform a systematic and in-depth critical analysis of previously published studies in well-known and trusted online electronic databases using specific search keywords words that are relevant to this study. We selected published peer-reviewed articles available from the onset of COVID-19 to July 2021.
Results
Total of 24 articles were included into this study. This study revealed that South Africa adopted digital technologies such as SMS-based solutions, mobile health applications, telemedicine and telehealth, WhatsApp-based systems, artificial intelligence and chatbots and robotics to provide healthcare services during COVID-19 pandemic. These innovative technologies have been used for various purposes including screening infectious and non-infectious diseases, disease surveillance and monitoring, medication and treatment compliance, creating awareness and communication. The study also revealed that teleconsultation and e-prescription, telelaboratory and telepharmacy, teleeducation and teletraining, teledermatology, teleradiology, telecardiology, teleophthalmology, teleneurology, telerehabilitation, teleoncology and telepsychiatry are among virtual healthcare services delivered through digital health technologies during COVID-19 in South Africa. However, these smart digital health technologies face several impediments such as infrastructural and technological barriers, organization and financial barriers, policy and regulatory barriers as well as cultural barriers.
Conclusion
Although COVID-19 has invigorated the use of digital health technologies, there are still some shortcomings. The outbreak of pandemics like COVID-19 in the future is not inevitable. Therefore, we recommend increasing community networks in rural areas to bridge the digital divide and the modification of mHealth policy to advocate for the effective use of innovative technologies in healthcare and the development of sustainable strategies for resources mobilization through private-public partnerships as well as joining available international initiatives advocating for smart digital health.
Keywords: Digital health technology, Virtual healthcare, Coronavirus disease 2019 (COVID-19), Health systems, South Africa
1. Introduction
The novel coronavirus disease 2019 (COVID-19) continues to decimate populations globally, threatening universal access to healthcare and widening the gap among world economies. The South African government declared a national state of disaster on 15 March 2020 and commenced a state of lockdown from 26 March 2020 to reduce COVID-19 transmission in the country.1 As of 20 July 2021, the country recorded a cumulative of 2.3 million confirmed COVID-19 cases and 67 080 deaths.2 South Africa, like other African countries, partially managed to tackle the catastrophic impact of the first wave by implementing several COVID-19 regulations and travelling restrictions. Based on the recommendations of Africa Centres for Disease Control and Prevention, the World Health Organization (WHO) and the Ministerial Task Team on COVID-19 of South Africa, South Africa implemented measures including blanket national lockdowns, travelling restrictions (inter-provincial) except for workers providing essential services,3 curfews, reduction of face-to-face meetings, wearing of face masks in public,4 banning of large social gatherings, contact tracing,5 intensified screening and testing as well as social distancing among others.6
The deadliest COVID-19 variant, known as the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) B.1.617.2 (Delta) variant,7, 8 has been threatening the progress made towards reducing infections and fatalities.9 The lethal Delta variant, first detected in India, is highly contagious and more transmissible than the original lineage.10 With over 6.2 million COVID-19 cases so far in Africa, South Africa accounts for 37% of them, followed by Morocco and Tunisia with 9% and 8%, respectively.2 Since the emergence of the Delta variant, South Africa has been recording the highest daily infections and deaths since the pandemic. Despite the re-introduction of robust virus containment strategies, the South African healthcare systems face several impediments to tackle the COVID-19, just like other countries in the continent. These challenges include lack of personal protective equipment (PPE),11 weak health systems (COVID-19-related admissions outweigh the available health facilities), scarce resources,12 insufficient COVID-19 vaccines, the resurgence of other communicable and non-communicable diseases (including malaria, HIV/AIDS, cancer, tuberculosis),11 social and spatial inequalities,13 healthcare access disparities, social unrest (which affect contact tracing), informal sectors, and insufficient funding.14 These impediments affect virus containment strategies. For instance, social unrest ultimately leads to violation of social distancing guidelines and affects testing and screening as well as the vaccination process. The surge in infections has laid bare the weaknesses of the public health services, with hospitals overflowing and shortages of oxygen, but above all, insufficient health personnel. However, the country's health system adopted the Pfizer-BioNTech COVID-19 Vaccine and Janssen (Johnson and Johnson) COVID-19 Vaccine after pausing the use of the Oxford/AstraZeneca COVID-19 vaccine.15 Additionally, the vaccination process has been affected by the dearth of vaccines, vaccines’ efficacy to fight emerging variants (low efficacy against the 501Y.V2 SARS-CoV-2 variant) and low vaccination rate faltering vaccination campaign.16
Due to the unprecedented nature of the situation posed by the COVID-19 pandemic, the uncertainties about the disease and the need to effectively deliver healthcare, the integration of emerging smart technologies has taken centre stage in supporting the delivery of virtual healthcare during COVID-19 in South Africa. Emerging digital technologies such as telemedicine, artificial intelligence (AI), 5G technology, smart health applications,17 big data, cloud computing, blockchain, Internet of Things, smart wearable devices and robotics have been playing a tremendous role to alleviate the unprecedented challenges posed by the pandemic.18 Several authors including Guy et al.,19 Mbunge et al.,20 Azam et al.,21 Wang et al. highlighted the importance of incorporating emerging technologies to provide healthcare services remotely.22 Despite South Africa recording the highest COVID-19 cases in the African continent, there is limited comprehensive literature on the utilization of smart digital health technologies in South Africa during COVID-19, making it difficult to organize the current research contributions and identify key challenges, neglected research and key policy areas that need to be addressed in the future. Therefore, this systematic review on the utilization of smart digital health technologies to provide virtual healthcare services delivery in South Africa during COVID-19 provides insights into key strategies, technologies, and their associated uncertainties as well as implementation challenges. Thus, this paper aimed to address the following research objectives: (1) Identify and explain smart digital health technologies that have been utilised to provide virtual healthcare services during COVID-19 in South Africa; (2) Provide comprehensive analysis of virtual healthcare services delivered through smart digital health technologies; (3) Identify challenges and risks associated with the provision of virtual healthcare through smart digital health technologies in South Africa; and (4) Provide recommendations and propose future work based on the findings of the study after synthesising literature.
2. Materials and methods
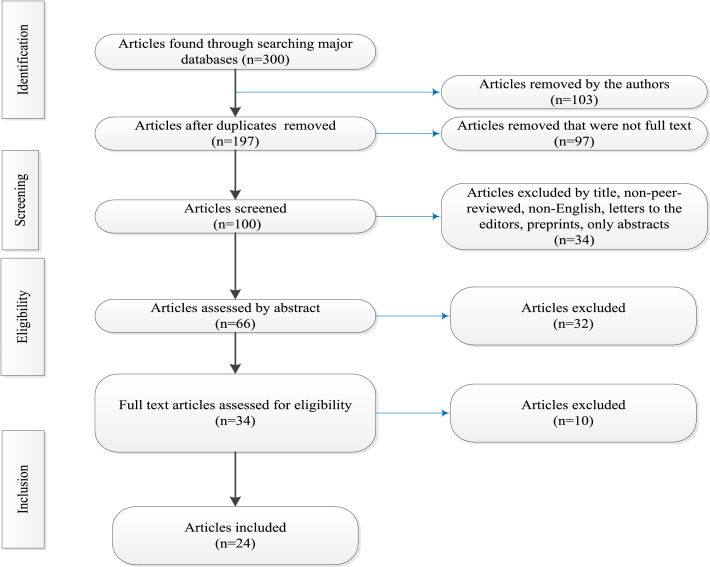
The study adopted the preferred reporting items for systematic reviews and meta-analyses (PRISMA) model.23 The PRISMA model is prominently used to conduct systematic reviews because of its flexibility to guide search and synthesising literature.24 The steps of the PRISMA model guided the literature search in various electronic databases on the utilization of smart digital health technologies to provide virtual healthcare services in South Africa during COVID-19.
2.1. Search strategy
Previously published studies were searched in the following online electronic databases: Google Scholar, PubMed, Science Direct, IEEE Xplore Digital Library, ACM Digital Library, and Springer Link. The literature searching was based on the following search terms: “Digital Technology” OR “Telehealth”OR “emerging technology” OR “Digital health” OR “Telemedicine” AND “COVID-19” OR “coronavirus disease” OR “SARS-CoV-2” OR “severe acute respiratory syndrome coronavirus 2” AND “South Africa” OR “Republic of South Africa”.
2.2. Study selection and eligibility criteria
We selected published peer-reviewed articles available from the onset of COVID-19 up to July 2021. A total of 300 articles were retrieved from electronic databases. The selected articles were screened based on the following: titles, abstracts and full-text. The selection of relevant studies all met the following inclusion criteria: (1) written in English or have English translations; (2) peer-reviewed; (3) published after the outbreak of COVID-19.
2.3. Data extraction
The excluded papers were incomplete, opinion pieces, and non-peer‐reviewed articles, and articles without English translations. To ensure that all relevant articles were included in the study, the authors performed a citations chain for each article retrieved. The authors removed 103 articles including duplicates articles from a pool of articles and were left with 197 articles. The authors further removed 97 incomplete articles, reprints, letters to the editors, non-peer-reviewed articles. We further checked the abstracts and removed 34 unqualified articles. A total of 66 articles were further checked independently by all authors and 32 unqualified articles were excluded. After the selection of relevant articles, authors further assessed articles’ abstracts independently, and 34 articles were considered for review eligibility. We further assessed full-text articles for eligibility and removed 10 articles. Only 24 articles were considered in this study. The study designs included were mainly digital health technologies utilised to provide virtual healthcare services in South Africa during COVID-19. The steps followed to report the number of published articles is presented in the PRISMA flow diagram in Fig.1.
Fig.1.
Selection and extraction flow diagram.
The included studies were reviewed independently by all authors. The studies were also examined in full text, and data was collected regarding the type of digital health technology, healthcare services offered, study area or province, purpose, challenges and risks.
3. Results analysis and discussion
The selected articles were extracted and synthesized in response to the research objectives. Digital health technologies that have been utilised to provide virtual healthcare services in South Africa during COVID-19 are shown in Table 1 .
Table 1.
Digital technologies utilised to provide virtual healthcare in South Africa.
| No. | Utilization | Digital health technology used | Healthcare services offered | Province | Noted challenges and risks |
|---|---|---|---|---|---|
| 1 | Virtual Learning and health communication25 | Television and Radio | Health promotion | Not specified, generalised to SA | Limited funding to adopt and scale up 4IR, infrastructural challenges, broadband, and the cost of data, difficult to roll out 4IR tools in rural areas due to poor internet connectivity and the general state of infrastructure |
| 2 | Provision of mental health services26 | Telemedicine | Tele-counselling and remote monitoring | Not specified, generalised to SA | Huge mental health backlog of patients seeking mental health consultations and lack of equipment, no guidance on the use of telemedicine for the delivery of mental healthcare. Telehealth requires changes in working practices and curating data. Telehealth may worsen and perpetuate the digital divide, security breaches and lack of trust in digital systems to securely keep patient data27 |
| 3 | Diabetic retinopathy screening28 | Telemedicine | Teleophthalmology | Gauteng | Even though telemedicine can overcome geographical, financial, and socioeconomic barriers, lack of equipment and intermittent internet connectivity can hamper their successful adoption and utilization |
| 4 | Diagnosis, treatment andprevention of neuromusculoskeletal disorders29 | Telemedicine | Provision of chiropractic services | The province is not specified; however, data were collected from chiropractors in SA | Lack of financial incentives, insufficient resources to implement and operate telemedicine technologies, a lack of interoperability between devices and technology as well as concerns in maintaining confidentiality and privacy |
| 5 | Provision of COVID-19-related information30 | COVID-19 Connect- Whatsapp helpline | Health communication on preventative solutions | Western Cape | Poor health literacy due to language and cultural barriers, access to health information in some rural areas. Data-constrained and under-resourced communities will not have been the primary audience of health-related webinars and online briefings |
| 6 | Provision of maternal and child health (antenatal care services), to connect pregnant women to health services31 | Momconnect mobile health application | Health communication and consultations | The programme was rolled out nationally in SA, the province was not specified. | Lack of knowledge about the available m-health that improve health services. Complaints regarding the platforms by health workers, specifically nurses dealing with pregnant and postpartum women32 |
| 7 | Appointment reminders, adherence to maternal and infant health care and bridging existing gaps in access to quality health education33 | MAMA SMS text messages | Teleconsultation and communications | Gauteng | Language barriers, access to mobile phones understaffed facilities and poor services34 |
| 8 | Exposure notification and social distancing35 | COVID-19 Alert SA application | COVID-19 exposure notification | Western Cape | Concerns over the infringement of users’ rights to security and privacy |
| 9 | Tracks individuals who have come into contact with others who have tested positive36 | COVi-ID smartphone contact tracing application | Contact tracing | Not specified, generalised to SA | Lack of access, contributing to low penetration rates and limited application with deepening socio-economic divides especially in rural areas. Ethical and human rights dilemmas |
| 10 | Communicate COVID-19 daily cases (new and recovered) and deaths as well as preventive measures37 | Social media platforms | Health communication | Not specified, generalised to SA | Misinformation, conspiracy theories surrounding the virus creation, ineffective home remedies for treatment, and downplaying of the need for prevention control, such as social distancing and mask use |
| 11 | Home delivery of medication system linked an e-pharmacy was established to reduce the risk of COVID-19 in this vulnerable group of patients38 | E-prescribing and e-delivery | Electronic delivery of prescriptions and home delivery of medication. | Western Cape | Unanswered follow-up phone calls, redirecting of a parcel due to change of physical address which was not easily accommodated by the system, home delivery could lead to inadvertent disclosure of HIV status to family members. The system requires good communication and coordination between role-players and managers |
| 12 | Schedule and engage in virtual healthcare professional consultations39 | Telemedicine- DrConnect | Teleconsulation | Not specified, generalised to SA | The study highlighted that the full adoption of telemedicine might face impediments such as disruption, engagement, integration and trust |
| 13 | Support TB treatment and adherence in children, medication reminders40 | Mobile app-based technology | Remote TB patient monitoring and Education | Gauteng | Limited access to phones and tablets that could support apps, limited funding and relatively high implementation cost |
| 14 | Improve maternal healthcare services41 | Mum & Baby | Health education and communication | Gauteng | Disparities in access to health services, inadequacies of health infrastructure, limited human resources for health, cost to the individual of accessing health services and challenges in health financing |
| 15 | Sensors in smartphones and activity trackers enable users to easily access physical activity programmes and monitor physical activity levels remotely42 | Smartphone physical activity mobile apps | E-physical training | Gauteng | Intermittent internet connection to a GPS and churning of participants |
| 16 | Reporting, monitoring and speeding up malaria notifications during COVID-1943 | Malaria connect- Malaria mobile application | 24-h mobile reporting tool | KwaZulu-Natal, Limpopo and Mpumalanga | Some health workers fail to report malaria cases through MalariaConnect, delays in both data collection and recording.44 Case notification within 24 hours and accurate case classification remain challenges.45 Network challenges delay reporting in some instances |
| 17 | Mobile learning to support and educate parents and caregivers through an SMS46 | ChildConnect South Africa | Health education | Not specified, generalised to SA | Lack of mobile phones and cost of data bundles |
| 18 | Measuring heart-rate pressure, tracking steps taken and distance travelled, daily calories burnt, tracking sleep patterns47 | Smart wearable devices. | Remote health monitoring | Gauteng | The efficacy of the smart wearable technologies was measured using a small sample in Gauteng Province and one generation |
| 19 | Smart devices are used for the self-management of health behaviours of individuals with chronic diseases of lifestyle48 | Smart wearable devices. | Remote health and activity monitoring | Not specified, generalised to SA | The smart devices collected and stored physiological data that could violate participants’ security and privacy through health data leakages |
| 20 | Use infrared thermometers to triage suspected people with COVID-1949 | Infrared thermometers | COVID-19 screening | Western Cape | The study noted that the use of infrared thermometers to triage patients may not have resulted in inaccurate measurements and therefore fever may be under observed |
| 21 | SMS as reminders of follow-up care to mental health care users50 | SMS | Reminders | KwaZulu-Natal | Missed appointments, lack of policy for development and implementation of SMS systems to deliver mental health care services |
| 22 | Digital medical systems are used for early detection, contact tracing and providing non-pharmaceutical health knowledge51 | Digital medical systems | Disease surveillance | KwaZulu-Natal | Privacy and cost would be barriers to use the technology, especially in marginalised rural areas |
| 23 | Collect biometric data and send to medical centres and monitor patients52 | Robotic devices | Disease surveillance | Free State | Robotic devices are expensive and many people may not afford them |
| 24 | Voice call reminders from healthcare providers about clinic visits and also reminders about taking medication53 | Mobile phones | Reminders | Mpumalanga | Lack of financial resources to buy airtime for phone calls and messages, data bundles for internet access. Lack of strategies on how to get information from the web |
4IR: fourth industrial revolution; SMS: short messaging service; TB: tuberculosis; Mum & Baby: an Apps for women, their partners, familiesand maternity staff; COVi-ID: an apps on Google Play; SA: South Africa.
3.1. Identified digital health technologies for providing virtual healthcare in South Africa
Being one of the most COVID-19 affected countries in Southern Africa, the Republic of South Africa has responded to the pandemic in numerous ways, including the deployment of digital technologies. This section presents digital technologies that South Africa has deployed to provide healthcare during COVID-19.
3.1.1. Short messaging service (SMS)-based solutions
SMS-text messages have a wider reach than mobile applications since they can reach any user with a mobile phone, whether a smart or feature phone. SMS health solutions that provide health information such as health content on COVID-19 has been disseminated via mobile SMSs by different telecommunication companies and healthcare service providers Table 1. shows that SMS-based solutions are used for multipurposes and the health content delivered covers different thematic areas, including disease awareness creation, adherence, reminders and prevention measures. SMS-based solutions used in South Africa include MAMA SMS text messages and ChildConnect.33 , 46 Their uses range from appointment reminders, adherence to maternal and infant health care, bridging existing gaps in access to quality health education and health education of caregivers and parents.46 Also, a cross-sectional study conducted by utilised SMS-based solutions as reminders of follow-up care to mental health care users in South Africa. However, the utilization of SMS-based solutions during COVID-19 is not immune to operational and implementation challenges. These impediments include missed appointments, lack of policy for the development and implementation of SMS systems to deliver mental health care services,50 language barriers, poor access to mobile phones, understaffed facilities and poor services, and lack of money to buy SMS bundles.34 Additionally, patients receiving text messages only without follow-ups are unable to get the necessary medical assistance to actively manage their health conditions at home.33
3.1.2. Mobile health applications
Alhough not everyone owns a smartphone, people are becoming more popular and pervasive, and South Africa is taking advantage of the proliferation of smartphones to improve healthcare. The use of mobile health applications in South Africa go beyond the fight against COVID-19 to include combating malaria and improving child and maternal health during the pandemic. MomConnect is a mobile application used to provide maternal and child care by connecting pregnant women to health services.54 Also, Grobbelaar et al. state that Momconnect mobile health application has been used to improve health communication and consultations as well as providing antenatal care services and to connect pregnant women to health services during the pandemic.31 While much attention and resources were allocated towards virus containment,43 the MalariaConnect mobile application has been utilized to intensify malaria reporting, monitoring and speed up malaria notifications during COVID-19 in Mpumalanga, Limpopo and KwaZulu-Natal provinces in South Africa. To speed up contact tracing activities, the University of Cape Town together with the regulatory authorities developed a mobile-based contact tracing application called COVi-ID.36 The medical fraternity is also using mobile applications such as Vula mobile applications for consultation, medical chats and referrals.55 Another virtual healthcare application used to provide remote healthcare services is called Signapps. This virtual healthcare application provides numerous services including secure messaging, reporting, predictive analytics, mobile forms, secure patient data storage, referrals and referral management, care team coordination and patient engagement.56 However, the utilization of mobile health applications to provide healthcare services faces several challenges which subsequently affect their efficacy. These challenges include internet connection intermittent, network challenges which delay reporting in some instances, security and privacy issues.35 Also, a mobile app-based technology deployed to enhance medication reminders and support tuberculosis (TB) treatment and adherence in children encountered challenges such as limited access to phones and tablets that could support the installation and utilization of the application, limited funding and relatively high implementation cost.40 This study also revealed that some health workers fail to report malaria cases through MalariaConnect, causing delays in both data collection and recording.44 Also, case notification within 24 hours and accurate case classification remain challenges.45 Among other challenges, disparities in access to health services (rural vs. urban areas), inadequacies of health infrastructure, limited human resources, cost of individuals accessing health services via mobile applications and insufficient health financing impact the utilization of mobile health applications.41
3.1.3. Telemedicine and telehealth
Telemedicine is defined as the provision of remote clinical services to patients without an in-person visit through the use of electronic communication (computers, video, phone calls, messaging) in both audio and virtual means.57 It uses information and communication technologies to deliver healthcare services remotely. Telehealth is defined as the use of medical information that could be exchanged from one point to another via electronic communication to promote the health conditions of patients.58 It also uses various technologies and services to provide patient care and enhance healthcare delivery. These technologies assist to reduce the risk of exposure to COVID-19 by providing patient care remotely. For instance, DrConnect is an example of a telemedicine solution offered in South Africa.39 The services offered include teleconsulting and remote monitoring.26 Similar to telemedicine, the popularity of telehealth is increasing as patients and medical practitioners shun physical contact in accessing and delivering healthcare services. Philips hospital telehealth provides services like electronic intensive care unit, remote patient monitoring, telehealth and teleconsultation.59 This study revealed that variants of telemedicine provide virtual healthcare services such as Teleconselling and remote monitoring, teleophthalmology, provision of chiropractic services, teleconsultation, teleeducation, teleradiology, teleneurology, telerehabilitation, teleoncology, and telepsychiatry have been utilized in South Africa to provide healthcare services during COVID-19. However, the utilization of telemedicine during COVID-19 face several impediments such as technological barriers, organisation and financial barriers, policy and regulatory barriers as well as cultural barriers. Technological barriers include poor internet connectivity, insufficient technological infrastructure,60 lack of interoperability and standardization between devices and technology, unavailability of supporting software, digital divide and high cost of telecommunication equipment.61 Organisation and financial barriers include the dearth of clinicians with hybrid expertise in telemedicine software, inadequate training, lack of financial incentives, low motivation to use telemedicine, lack of awareness about telemedicine products, resistance to change, duplication and fragmented implementation of telemedicine projects,39 language barriers, high cost of infrastructure development, implementation and maintenance, insufficient resources to implement and operating telemedicine technologies, high cost of electricity supply, high-cost of telemedicine services and insufficient funding. Policy and regulatory barriers include the need for full governmental support, lack of policy clarity, policy and regulatory framework, privacy and confidentiality in the application of the telemedicine system and limited budgetary support .62 For instance, in South Africa, the mHealth policy that was introduced in 2015 provided no guidance on the use of telemedicine for the delivery of mental healthcare.26 Cultural barriers such as socio-demographic and cultural dynamics as well as religion that discourages people to use telemedicine applications, digital illiteracy and resistance to change.61
3.1.4. WhatsApp-based systems
WhatsApp is increasingly becoming a popular mobile social media application amongst smartphone users in South Africa. With so much misinformation and disinformation happening on social media, South Africa uses HealthAlert, a WhatsApp-based helpline that uses automated response and triage for disseminating accurate and timely COVID-19 related information from the National Department of Health to the public.63 South Africa is currently using the COVi-ID smartphone contact tracing application together with the COVID-19 Alert application to intensify contact tracing, exposure notification and social distancing to contain the COVID-19 pandemic.35
3.1.5. AI and chatbots
South Africa is using AI to provide healthcare services like disease diagnosis and treatment, decision support systems, and chatbots. Examples include EMGuidance, a mobile and web-based application for medicines and treatment meant for medical professionals.64 Moreover, chatbots also fall under this category since they are implemented using AI, e.g., HealthAlert Virtual assistants, also called chatbots, help provide useful health information at any time in an interactive manner. AI-based smart wearable devices such as pedometers, various electrode-based chest straps, accelerometer-based arm straps, fashion bracelets, fitness bands and watches, earphones, and smart clothing have been utilised to monitor heart rate for self-management of health behaviours of individuals with chronic diseases or non-infectious diseases.48
3.1.6. Robotics
Robotics has become helpful in health delivery that minimises human contact. This technology has gained traction in South Africa and provides such services as automated delivery and dispensing of medicines and smart lockers. Right ePhamarcy, a digital technology solution in South Africa, provides various robotics related solutions like smart lockers, automated delivery and dispensing of medicines.65 CapeRay and Lodox also provide robotics solutions through advanced imaging to diagnose COVID-19 X-Ray chest images.66, 67
3.2. Virtual health care services delivered through smart digital technologies
3.2.1. Teleconsultation and e-prescription
COVID-19 has changed conventional methods of seeking medical care due to movement restrictions and, thereof, lack of in-person medical consultations. COVID-19 has led to an increase in telemedicine in Africa because telemedicine allows patient-doctor interactions without physical contact.68 Telemedicine allows for teleconsultation, where patients receive medical assistance from medical professionals from all over the world through virtual interactions. Mobile usage in South Africa is very high.69 Through teleconsultation, patients in South Africa can use SMS texts and voice calling to consult with healthcare providers.70 COVID-19 has led to different disease-specific interventions that are targeted at ensuring that people with pre-existing diseases are not affected adversely by COVID-19.62 Because of teleconsultation, patients can get their medication prescriptions through SMS or email, a phenomenon called e-prescription. E-prescription has been reported to reduce prescription errors and improve medication safety.71
3.2.2. Mobile medical services such as telelaboratory and telepharmacy
Due to COVID-19 movement restrictions, patients can, through telepharmacy, order their medication from their pharmacies and have them delivered straight to their homes. Telepharmacy refers to the provision of pharmacist services using telecommunications to distant patients by qualified pharmacists.72 In South Africa, some individuals have devised mobile applications that connect patients and medication delivery drivers, saving time, reducing COVID-19 transmission, and maintaining patients’ adherence to medication. In addition to their provision of medication, pharmacists in South Africa are, during COVID-19, also involved in patient counselling, drug therapy and other health interventions.73 This is mainly due to insufficient medical personnel consequent to COVID-19 restrictions. The role of pharmacists during COVID-19 in South Africa is very pronounced. The South African Society of Clinical Pharmacy functions as a guide to clinical pharmacists, elucidating their role in the fight against COVID-19.74 COVID-19 has instigated the improvement of medical services in South Africa, such as the introduction of mobile medical services that allow testing of people for COVID-19 in their localities and homes. Mobile testing services do improve not only access of people to testing but also increase the number of people tested.75 Since day 3 of COVID-19 in South Arica, people with COVID-19 symptoms have been referred to mobile testing stations to increase testing among communities.68 In 2020, the government of South Africa, through the National Health Laboratory Service, introduced 60 new COVID-19 mobile testing and sampling units that act as mobile laboratories and allow the undertaking of COVID-19 polymerase chain reaction (PCR) testing.76 The mobile laboratories are not only crucial for COVID-19 testing but can also serve as testing centres for other diseases such as TB and HIV/AIDS. South Africa is using electronic pharmacies to eliminate physical contact in dispensing medicines to patients. These solutions use robotics in automating pharmacies, dispensing drugs using ATM-like dispensers, tele-pharmacy (using telecommunication technologies to deliver medicines to faraway patients), centralised dispensing and collect-and-go smart lockers.65
3.2.3. Tele-education and e-learning
Tele-education has been in existence in South Africa since the 1970s.77 Because of COVID-19 restrictions, tele-education has become very popular. E-learning, a form of tele-education which involves the use of digital platforms for online teaching and learning, emerged in the 1990s in South Africa.78 E-learning is time-efficient, cheap, interactive and very convenient.79 South Africa is one of the countries that has utilized e-learning during the COVID-19 pandemic. During COVID-19 lockdown, 17 out of 21 universities in South Africa converted to e-learning as well as the use of online resources and tools such as Zoom and Blackboard.80 Despite the recommendation of these e-learning tools by most South African universities, a study of first-year university students in South Africa showed that students preferred informal learning platforms such as WhatsApp which are easily accessible and easy to use when compared to formal platforms such as Moodle.81 Although e-learning is a useful strategy, the major disadvantages of its use are lack of infrastructure and stable internet.82 Therefore, e-learning may appear biased because only students from well off backgrounds can fully benefit from it. However, it is encouraging that tele-education appears to be gaining momentum in South Africa. In the KwaZulu-Natal Province, a tele-education service, which has been running since 2001, now offers over 1 400 hours of video conferenced education every year. Such service is even more needed in the current COVID-19 pandemic.
3.2.4. Teledermatology
Dermatology is a branch of medicine that deals with skin disease. Teledermatology, therefore, is the practice of dermatology using telecommunications without patient-doctor interaction.83 Teledermatology is a tool that can improve the delivery of speciality medical care in South Africa. In Africa, it has been reported that most people visit dermatologists for infectious diseases and eczema.84 Because it is very visual, dermatology is very suited for modern telemedicine techniques. However, dermatology has been identified as one of the vectors responsible for the transmission of COVID-19.85 In South Africa, a teledermatology scale-up framework and its implementation roadmap model were initiated in a bid to develop a national teledermatology program.86 This model emphasises the need for stakeholder-government-community engagement in the implementation of teledermatology in South Africa. However, legal frameworks must be considered during the initiation of teledermatology programs in South Africa.
3.2.5. Teleradiology
During the COVID-19 pandemic, teleradiology has allowed the transmission of radiological images of patients from one geographical location to another. This has allowed patients to receive radiological medical services without patient-doctor interaction. Teleradiology, therefore, allows the provision of radiological services to healthcare institutes in rural areas in the absence of radiologists. Because COVID-19 affects the lungs, radiology has played a central role during the pandemic through the computed tomography of the lungs.87 In a survey study that investigated the response of radiologists to COVID-19, it was reported that there are disparities in radiology research and infrastructure in South Africa.88 In the North West Province in South Africa, a recent study found that radiographers are working beyond their designated roles that are stipulated in the service-level agreement primarily because of insufficient infrastructure.89 For teleradiology to be optimally effective in South Africa, training of radiologists, especially in rural areas, should be improved such that they can meet the expectations of their roles beyond their designated duties. Another study in Tshwane, a city in South Africa, reported that some doctors in the city use free global searches to scan chest radiographs without adequate training on image interpretation.90 The use of these free global searches may present challenges in the use of teleradiology amid the COVID-19 pandemic due to the unsystematic nature of these searches. There are possibilities of misidentification or non-identification of abnormalities in the radiographs. It is therefore recommended that as many as possible doctors undergo training on the correct interpretation of chest radiograph images.
3.2.6. Telecardiology
Telecardiology allows the monitoring and adherence of patients with cardiovascular diseases to their medication. It involves a vast array of activities such as the monitoring of implantable monitoring devices, sending of ECGs by telephone and the provision of patient education and support.77 The COVID-19 pandemic has increased the promotion and awareness of telecardiology in South Africa. Due to the seriousness and prevalence of heart diseases, telecardiology allows speedy diagnosis of heart diseases and subsequently speedy provision of medication. There are, however, issues of cost in telecardiology.91 Additionally, there are issues of legislation and ethics that have to be addressed, not only in telecardiology but in telehealth at large.
3.2.7. Teleophthalmology
Diabetic retinopathy is the most common cause of incidental blindness.92 Teleophthalmology is a great tool in the fight against diabetic retinopathy which in South Africa has been mainly reported in people from poor economic and social backgrounds.92 In a recent study, it was reported that teleophthalmology programs in South Africa were cost-effective, based on economic evaluations.28 Teleophthalmology can be as simple as using mobile camera transport to capture images of patients which are then taken to an ophthalmologist in a different location for interpretation or the transmission of retinal images to a reading facility where they are graded by an eye specialist. Teleophthalmology may also involve motor vehicles that carry ophthalmic units that capture images and send them to experts via satellite or the uploading of retinal images into a server for their documentation and grading by retinal experts.93 Teleophthalmology does not only reduce medical costs but also reduce the costs associated with the transportation of people to seek medical assistance. In this devastating era of COVID-19 in South Africa, teleophthalmology can improve the screening of eye defects thereby reducing blindness that is caused by conditions that are otherwise curable if detected early.
3.2.8. Teleneurology
Teleneurology involves the provision of information and care to patients suffering from neurological disorders such as stroke especially in rural areas where health facilities and personnel are lacking.94 The number of neurologists who use teleneurology has increased during the COVID-19 pandemic.95 Most neurological disorders are found in low-and-middle-income countries.96 These include many countries in sub-Saharan Africa. Teleneurology provides a convenient platform for dealing with these neurological disorders. However, there is a need for more research to be conducted on the cost, efficacy, and feasibility of teleneurology. In South Africa, teleneurology, like any other type of telemedicine, does not only reduce cost in monetary terms but also reduce cost in terms of PPE purchasing. Because of the limited number of neurologists in Africa, intracontinental collaborations would make teleneurology more feasible in the African continent. However, because the effective use of digital technologies requires specific skills, there is a need for neurologists in South Africa to undergo regular training. Additionally, around 60% of people in rural areas of South Africa have no access to electricity.94 This cast in doubt the ability of people in the rural areas of South Africa to afford the necessary infrastructure that is requisite for teleneurology. However, nowadays, most people have access to the internet through their mobile phones. In fact, by early 2019, South Africa had attained mobile phone penetration of over 100% owing to the ability of its people to own multiple subscriber identification module cards from multiple mobile network providers.
3.2.9. Telerehabilitation
Telerehabilitation involves follow-ups on patients who have undergone physiotherapy, speech therapy, occupational therapy and another form of therapy that require post-therapeutic rehabilitation. These follow-ups can come in the form of telephonic calls, emails, or fax messages.77 Although the COVID-19 pandemic has increased the practice of telerehabilitation on a global scale, it remains relatively unexplored in South Africa.97 Telerehabilitation involves real-time interactions through platforms such as Zoom and Skype and recorded content that patients can access at their own time such as recorded sessions, the use of applications, webinars, and pre-recorded lectures. WhatsApp is an example of a platform that can be used to transmit recorded content.97 Because many South Africans have access to mobile phones,69 the use of mobile applications such as WhatsApp would be very effective in driving telerehabilitation in South Africa in the era of COVID-19. Telerehabilitation can also be used as a training tool for both students and health workers through seminars and recorded lectures.98 The few educators and service providers in South Africa who have started the practice of telerehabilitation due to COVID-19 restrictions have reported positive outcomes.26 For telerehabilitation to be mainstream in South Africa, the raising of its awareness among physiotherapists and other professionals is very imperative. Introducing rehabilitation in higher education curricula in South Africa may also promote its visibility as a viable healthcare service delivery model. Equally importantly, the introduction of telerehabilitation in education curricula will equip students with requisite healthcare skills.
3.2.10. Teleoncology
The advent of COVID-19 has negatively impacted the medical care of people with terminal illnesses such as cancer in Africa. This was observed in the form of limited availability of resources, limited provision of healthcare services and other factors.99 Resource limitation, which was brought about by rationing of medication and hospital facilities to accommodate COVID-19 patients, can have devastating effects on patients with terminal illnesses, worse of which is increased fatalities. This is further exacerbated by the fact that approximately 85% of South Africans are dependent on the public health system, 99 therefore, cannot afford private health care even in a COVID-19-free South Africa. COVID-19 has also led to a depletion of medical and pharmaceutical staff. Teleoncology can be an answer to the devastation brought by COVID-19 in cancer care. Hypofractionated radiation therapy has been reported to maintain cancer care during the COVID-19 pandemic.100 This type of radiation can reduce cancer care costs and promote the convenience of patients. Because of COVID-19 restrictions, online clinical oncology learning is reported to have increased in South Africa, reducing cancer patient visits to hospitals. 99 Teleoncology provides solutions to issues of insufficient funding in cancer care as well as insufficient cancer specialists.
3.2.11. Telepsychiatry
Telepsychiatry refers to the provision of mental health services without patient-doctor interaction.70 COVID-19 restrictions have resulted in spikes in cases of gender-based violence (GBV) and mental health problems. South Africa is no exception to this harsh reality. The increase in GBV and mental problems has increased the demand for telepsychiatry and counselling. Ten years ago, a study reported that most hospitals in the KwaZulu-Natal Province were not ready for e-health, a component of which is telepsychiatry.101 Although telepsychiatry holds great potential in alleviating mental health problems in South Africa, there is a need for psychiatry awareness initiatives in the country before they can be uniformly implemented.
3.3. Utilization of Smart digital health technologies in health care
Digital smart health technologies have been used for various purposes including screening infectious diseases and non-infectious diseases, disease surveillance, medication and treatment compliance, appointment reminders, communication between healthcare providers and patients, maternal and child health and disease diagnosis.
3.3.1. Screening infectious and non-infectious diseases
Smart digital devices such as infrared thermometers, smart wearable devices, PCR, HIV self-test kits have been adopted and significantly improve screening of infectious and non-infectious diseases. For instance, non-contact infrared digital thermometers have been used in the strategic entry and exit points to measure body temperature for COVID-19 screening. The infrared thermometers are fast, relatively affordable and convenient as early COVID-19 screening tools. A descriptive observational study conducted by Mash et Al. showed that infrared thermometers were used in district hospitals in the Western Cape province,102 South Africa for COVID-19 screening. However, an infrared thermometer is susceptible to false readings. Also, a cross-sectional study conducted by Wesson et Al. utilized smart devices to remotely monitor the activities, behaviour and health of people with chronic disease such as lung disease, diabetes, cardiovascular diseases and cancer.48 However, some developed countries utilise non-wearable passive multiparametric sensors embedded in under-mattress pads to monitor heart rate, respiratory rate and other sleep parameters useful to identify early physiological decompensation.103 Such technology might not be feasible in developing countries due to cost implications.
3.3.2. Disease surveillance and monitoring
Smart digital health technologies have been used to collect, analyse and interpret data from different patients so that health practitioners can be able to come up with different measures to prevent and control their diseases. According to Chigona et al. wireless medical devices can be used to transmit data obtained from body sensors in order to monitor patients’ health.35 Robotic devices can be used to monitor patients with diseases like heart failure and diabetes using digital systems. With well-structured digital health systems like contact tracing applications and telemedicine, it is easy to detect COVID-19 early, trace the close-contacts, and make some interventions to the people who need medical attention especially in rural areas of KwaZulu-Natal province, South Africa.51
3.3.3. Medication and treatment compliance
Digital technologies such as SMS-based solutions and mobile health applications have been utilised in South Africa to improve medication and treatment compliance. This study revealed that SMS reminders have been utilised for antiretroviral therapy adherence support,104 malaria treatment adherence, follow-up on antenatal care services,34 compliance with treatment procedures for tuberculosis patients, and in making sure that hypertensive patients adhere to medication procedures. For instance, a cross-sectional study conducted by Siedner et al. shows that SMS reminders of follow-up care to mental healthcare users tremendously improved treatment adherence.51 Such technology has been used to address forgetfulness, improve communication between patients and healthcare professionals, improve medication and treatment adherence, appointments reminders and providing health information as well as creating awareness. A retrospective cohort study conducted by Dietrich et al. highlighted that treatment adherence remains a significant challenge for many which contribute to an increased rate of TB and HIV/AIDS relapse.105 However, the use of SMS text messaging is regarded as the most feasible technology to improve treatment adherence in rural areas.106 Mobile phones have enormous reach in resource-limited settings, providing real potential for low-cost adoption to support engagement in healthcare.
3.3.4. Awareness and communication
Bi-directional SMSs, radios, television, phone calls, social media messaging platforms and chatbots have been used to create COVID-19 awareness and intensifying communication between healthcare professionals and patients in South African health systems. These technologies will allow them not to have physical contact with the patients especially with highly infectious diseases like COVID 19. Table 1 shows that patients receive messages from healthcare providers and make some appointments using SMS, phone calls, chatbots, social media messaging platforms for various purposes such as health promotion, education and communication. Also, the healthcare providers disseminate information to the community such as awareness of certain diseases through radio, television, digital billboards and printed media such as brochures and flyers. A study conducted by Mhlanga et al. posits that television and radio have been utilised to intensify health promotion,25 communication and creating awareness during COVID-19 in South Africa. However, such technologies face infrastructural challenges, poor broadband and network coverage, language and cultural barriers.104
3.4. Identified challenges and limitations of providing virtual healthcare services through digital health technologies in South Africa
3.4.1. Limited funding
Digitization of healthcare requires funding to purchase the required devices and software, adopt and scale-up digital technologies and other necessary operations to roll out the technologies. However, limited funding is a challenge in digitizing healthcare in South Africa, affecting the roll-out of the fourth industrial revolution (4IR) tools in rural areas.25 Funding affects the availability of and access to the internet, the availability of state-of-the-art infrastructure and access to phones and tablets that could support health applications.40
3.4.2. Perpetuation of the digital divide
The access to digital devices and infrastructure in South Africa is not the same across the country, Mhlanga et al. noted that lack of funding affects the potential introduction of 4IR tools in rural South Africa.25 Telehealth may worsen the already existing digital divide in South Africa,26 presenting unequal access opportunities to healthcare, especially in rural areas.36
3.4.3. Lack of guidance on telemedicine use for mental healthcare
Despite the increasing popularity of digital health, there is a lack of guidance on the use of telemedicine to deliver mental healthcare during the pandemic. Moreover, there is a considerable backlog of mental health patients seeking consultations.26 With the use of telemedicine, access to mental health consultation services may be improved.
3.4.4. Security breaches and lack of trust
Privacy and confidentiality are critical issues in digital health which often hamper the adoption and use of digital health tools. Some patients and healthcare professionals lack trust in digital systems to securely keep patient data.27 There is a risk that some digital health tools may fail to ensure, maintain and guarantee the confidentiality and privacy of patient data.29 , 35 Some patients have concerns over the potential infringement of their privacy and confidentiality by digital health tools.35
3.4.5. Lack of digital equipment
Digital health requires equipment and internet access to enable remote healthcare provision and consultations through such technologies as telemedicine. However, there is a lack of equipment and intermittent internet connectivity in some parts of South Africa,42 hindering the utilization of digital health.26 , 28 The lack of equipment is attributed to limited funding.25 , 40
3.4.6. Lack of interoperability of digital tools
One of the promises of digital health is sharing of health data between and among healthcare institutions to improve the overall experience and health delivery to patients. This is possible if the developed digital health tools can interoperate. However, a lack of interoperability between devices and technology is a challenge.29 This lack of interoperability reveals the fact that there are missing standards for developing digital health tools.107
3.4.7. Poor health literacy
There is language barrier and a lack of knowledge about the available tools against COVID-19 in South Africa. Most of the digital health tools in South Africa are not translated to people's vernacular languages based on location, leading to poor health literacy due to language and cultural barriers,33, 34 affecting access to health information in some rural areas.30 Some South Africans lack knowledge about the available m-health tools that improve health services.31 Language barriers affect the utilization of digital health tools.34
3.4.8. Misinformation and conspiracy theories
With the growing popularity of social media, healthcare authorities are using social media platforms to debunk misinformation and conspiracy theories. One of the challenges of social media is misinformation, such as conspiracies surrounding the COVID-19, vaccines, sharing of ineffective home remedies for COVID-19 treatment, and downplaying the need for prevention and control measures such as social distancing and the wearing of masks.37
3.4.9. Rigid systems, risk of disclosure and unanswered follow-ups
South Africa has had several COVID-19-induced national lockdowns, which have affected people's movements. Electronic prescription and electronic delivery have become crucial during these lockdown periods. However, the challenges of unanswered follow-up phone calls and redirecting of parcels due to the change of physical address of patients negatively impact the utilization of digital healthcare in South Africa.38 Some of the e-prescription and e-delivery systems are rigid and cannot easily accommodate the redirection of parcels after a patient's address change. Moreover, home delivery of medication could lead to inadvertent disclosure of a patient's HIV status to family members.38
3.4.10. Cost to individuals to access the digital health tools
Usually, when digital health tools are deployed, patients are not given the required devices and infrastructure, such as internet access, to be able to access and use those tools. Some patients do not have access to mobile phones capable of accessing digital health tools,40 creating disparities in access to health services. Thus, the cost to individuals of accessing digital health services and challenges in health financing impact the utilization of digital health in South Africa.41
3.5. Potential use of digital health technologies in health service supply in rural communities beyond COVID-19
Due to the advent of COVID-19, telehealth has intensified not only in South Africa but around the world. It is crucial that digital health technologies are not only resourceful in the current COVID-19 pandemic but even beyond in rural communities. This is notwithstanding the fact that resources are very scarce within these rural communities. Lack of health resources and medical personnel often causes people in rural areas to walk hours to their nearest health facilities.48 Therefore, digital health technologies should be able to bridge the widening gap between health service supply in urbanised and health service supply in rural areas. The fact that rural areas are very remote and usually have low populations should not disadvantage people in these areas from receiving health care. It is very common to find very few medical personnel in rural areas of African countries such as South Africa. Sometimes a small population of people in a rural dwelling will have only one nurse without even a doctor present. Because telehealth allows the sharing of information between health professionals in different locations, it can circumvent the issue of limited medical personnel and medical infrastructure in rural areas. This is because a health professional situated in a rural area can electronically share medical information with colleagues in urbanised areas leading to speedy medical diagnoses. Telemedicine allows medical professionals in rural areas to seek guidance from their counterparts in urbanised areas during medical emergencies, something that can save the lives of people who live in remote areas. In this way, digital health technologies can provide benefits to many South Africans even beyond the COVID-19 pandemic.53 In this era of COVID-19, the government of South Africa has invested heavily in health infrastructure such as mobile testing and sampling units for use as telelaboratories.73 These infrastructures are deployed across the country to help fight the disease. They are however heavily concentrated in urban areas due to high populations of people in these areas. After COVID-19 has been defeated, such infrastructures will be deemed redundant in urban areas as there are plenty of health facilities there. These facilities will therefore be utilised in the rural areas where health facilities are scarce. In this way, most of the digital health technologies that are utilised during COVID-19 will mostly be relegated to the rural areas and will be of great benefit to the rural dwellers.38 Unlike most urban dwellers, most rural dwellers do not own sophisticated smartphones and therefore do not have access to emails or recorded voice notes. They usually own simple mobile phones that enable voice calling and texting only. Teleconsultation allows patients to contact healthcare providers and seek medical intervention through a simple text message.67 This is another facility that will benefit people in rural villages way beyond the current COVID-19 pandemic. Despite the simplicity of the lifestyles of people in rural communities due to very limited technological advancements, people in these areas will still benefit from digital health technologies even beyond the era of COVID-19.
4. Recommendations and future work
South Africa had managed to flatten the COVID-19 curve. However, the outbreak of the Delta variant overwhelmed the health systems which subsequently led to the sudden increase in daily infections and death rate. Despite these challenges, the country successfully secured COVID-19 vaccines and now attention has gradually shifted towards vaccination of populations while prioritising high-risk groups such as healthcare professionals and the ageing populations among others.16 Nevertheless, this study revealed several impediments such as social unrest, lack of adherence to contact tracing and challenges in creating vaccination awareness. To improve healthcare service delivery and healthcare access amidst the COVID-19 pandemic, there is a need to integrate smart digital health technologies in South African health systems to intensify remote health care. Our study identified barriers and challenges faced by integrating smart digital health technologies; these barriers can be addressed through modification of policy and the development of sustainable strategies for the mobilisation of resources. Notably, some of these barriers can be addressed through private-public partnerships and joining available international initiatives advocating for smart digital health. Also, there is a need to increase the number of community networks in rural areas to bridge the digital divide considering that there is a significant increase in Wi-Fi hotspots in urban centres. Additionally, financial and political commitment is required to modify mHealth policy to incorporate the use of smart digital technologies to provide virtual health care. Also, there is a need for increased budgetary allocation for setting up digital health technologies such as telemedicine, telehealth among others and funding for research and development. Our study revealed that there is also a need to train healthcare professionals and create awareness about the available digital health technologies that could be utilised to access remote health care, especially during the pandemic to reduce COVID-19 infections. These recommendations will probably have an impact on health policies and practices.
5. Conclusion
The COVID-19 pandemic has drastically changed how health systems operate globally. This prompted the use of smart digital technologies to support virtual health care. These technologies have been utilised to monitor diseases, create awareness, make appointment reminders, promote adherence to maternal and infant health care and to bridge the existing gaps in access to quality health education and communication. They can also be used to assist post-treatment monitoring of convalescing COVID-19 patients to reduce the increasing number of front liners getting infected and some succumbing to the pandemic. Our study noted that the use of telemedicine and telecare in rural areas is poor. However, remote rural areas of South Africa provide opportunities and capabilities to improve healthcare access and delivery through SMS-based solutions. This can be intensified since mobile phones have enormous reach in resource-limited settings, providing real potential for low-cost adoption to support engagement in healthcare. However, this approach lacks regulation regarding data privacy and security.50 Nevertheless, SMS technology continues to fill up the gaps in healthcare access disparities and inequality, which would otherwise remain unfilled.
CRediT author statement
Elliot Mbunge: Conceptualization, Methodology, Writing—Original draft, Writing—Reviewing & Editing. John Batani: Conceptualization, Methodology, Results analysis, Writing—Reviewing & Editing. Goabaone Gaobotse: Writing—Original draft, Writing—Reviewing & Editing. Benhildah Muchemwa: Writing—Original draft, Writing—Reviewing & Editing.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Reddy T., Shkedy Z., van Rensburg C.J., et al. Short-term real-time prediction of total number of reported COVID-19 cases and deaths in South Africa: a data driven approach. BMC Med Res Methodol. 2021;21(1):15. doi: 10.1186/s12874-020-01165-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The National Institute for Communicable Diseases of South Africa. LATEST CONFIRMED CASES OF COVID-19 IN SOUTH AFRICA (18 JULY 2021). https://www.nicd.ac.za/latest-confirmed-cases-of-covid-19-in-south-africa-18-july-2021/. Accessed 20 July 2021.
- 3.Mbunge E. Effects of COVID-19 in South African health system and society: An explanatory study. Diabetes Metab Syndr. 2020;14(6):1809–1814. doi: 10.1016/j.dsx.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mbunge E., Millham R.C., Sibiya M.N., et al. Framework for ethical and acceptable use of social distancing tools and smart devices during COVID-19 pandemic in Zimbabwe. Sustain Oper Comput. 2021;2:190–199. [Google Scholar]
- 5.Mbunge E., Fashoto S.G., Akinnuwesi B., Metfula A., Simelane S., Ndumiso N. Ethics for integrating emerging technologies to contain COVID-19 in Zimbabwe. Hum Behav Emerg Technol. 2021;3(5):876–890. doi: 10.1002/hbe2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arndt C., Davies R., Gabriel S., et al. Covid-19 lockdowns, income distribution, and food security: an analysis for South Africa. Glob Food Sec. 2020;26:100410. doi: 10.1016/j.gfs.2020.100410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Banerjee I., Robinson J., Sathian B., van Teijlingen ER. South Africa and its COVID-19 prohibition predilection. Nepal J Epidemiol. 2020;10(3):874–877. doi: 10.3126/nje.v10i3.31543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duong D. Alpha, Beta, Delta, Gamma: What's important to know about SARS-CoV-2 variants of concern? CMAJ. 2021;193(27):E1059–E1060. doi: 10.1503/cmaj.1095949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davis C., Logan N., Tyson G., et al. Reduced neutralisation of the Delta (B.1.617.2) SARS-CoV-2 variant of concern following vaccination. PLoS Pathog. 2021;17(12):e1010022. doi: 10.1371/journal.ppat.1010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang W., Shaman J. COVID-19 pandemic dynamics in India and impact of the SARS-CoV-2 Delta (B.1.617.2) variant. medRxiv. 2021:21259268. doi: 10.1098/rsif.2021.0900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jassat W., Mudara C., Ozougwu L., et al. Difference in mortality among individuals admitted to hospital with COVID-19 during the first and second waves in South Africa: a cohort study. Lancet Glob Health. 2021;9(9):e1216–e1225. doi: 10.1016/S2214-109X(21)00289-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moodley K., Rossouw T. What could fair allocation of an efficacious COVID-19 vaccine look like in South Africa? Lancet Glob Health. 2021;9(2):e106–e107. doi: 10.1016/S2214-109X(20)30474-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Visagie J., Turok I. Rural–urban inequalities amplified by COVID-19: evidence from South Africa. Area Dev Policy. 2021;6(1):50–62. [Google Scholar]
- 14.Stiegler N., Bouchard JP. South Africa: Challenges and successes of the COVID-19 lockdown. Ann Med Psychol (Paris) 2020;178(7):695–698. doi: 10.1016/j.amp.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahase E. Covid-19: South Africa pauses use of Oxford vaccine after study casts doubt on efficacy against variant. BMJ. 2021;372:n372. doi: 10.1136/bmj.n372. [DOI] [PubMed] [Google Scholar]
- 16.Dzinamarira T., Nachipo B., Phiri B., Musuka G. COVID-19 Vaccine Roll-Out in South Africa and Zimbabwe: Urgent Need to Address Community Preparedness, Fears and Hesitancy. Vaccines (Basel) 2021;9(3):250. doi: 10.3390/vaccines9030250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mbunge E. Integrating emerging technologies into COVID-19 contact tracing: Opportunities, challenges and pitfalls. Diabetes Metab Syndr. 2020;14(6):1631–1636. doi: 10.1016/j.dsx.2020.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chitungo I., Mhango M., Mbunge E., Dzobo M., Dzinamarira T. Digital technologies and COVID-19: reconsidering lockdown exit strategies for Africa. Pan Afr Med J. 2021;39:93. doi: 10.11604/pamj.2021.39.93.29773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fagherazzi G., Goetzinger C., Rashid M.A., Aguayo G.A., Huiart L. Digital Health Strategies to Fight COVID-19 Worldwide: Challenges, Recommendations, and a Call for Papers. J Med Internet Res. 2020;22(6):e19284. doi: 10.2196/19284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mbunge E., Akinnuwesi B., Fashoto S.G., Metfula A.S., Mashwama P. A critical review of emerging technologies for tackling COVID-19 pandemic. Hum Behav Emerg Technol. 2021;3(1):25–39. doi: 10.1002/hbe2.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Azam I., Usman M. In: Emerging Technologies During the Era of COVID-19 Pandemic. Studies in Systems, Decision and Control, vol 348. Arpaci I, Al-Emran MA, Al-Sharafi M, Marques G, editors. Springer; Cham: 2021. Application of Modern Technologies on Fighting COVID-19: A Systematic and Bibliometric Analysis. [Google Scholar]
- 22.Wang Q., Su M., Zhang M., Li R.R. Integrating Digital Technologies and Public Health to Fight Covid-19 Pandemic: Key Technologies, Applications, Challenges and Outlook of Digital Healthcare. Int J Environ Res Public Health. 2021;18(11):6053. doi: 10.3390/ijerph18116053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moher D., Liberati A., Tetzlaff J., Altman D.G., . PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O'Dea R.E., Lagisz M., Jennions M.D., et al. Preferred reporting items for systematic reviews and meta-analyses in ecology and evolutionary biology: a PRISMA extension. Biol Rev Camb Philos Soc. 2021;96(5):1695–1722. doi: 10.1111/brv.12721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mhlanga D., Moloi T. COVID-19 and the Digital Transformation of Education: What Are We Learning on 4IR in South Africa? Educ Sci. 2020;10(7):180. [Google Scholar]
- 26.Adepoju P. Africa turns to telemedicine to close mental health gap. Lancet Digit Health. 2020;2(11):E571–E572. doi: 10.1016/S2589-7500(20)30252-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blandford A., Wesson J., Amalberti R., AlHazme R., Allwihan R. Opportunities and challenges for telehealth within, and beyond, a pandemic. Lancet Glob Health. 2020;8(11):e1364–e1365. doi: 10.1016/S2214-109X(20)30362-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Avidor D., Loewenstein A., Waisbourd M., Nutman A. Cost-effectiveness of diabetic retinopathy screening programs using telemedicine: a systematic review. Cost Eff Resour Alloc. 2020;18:16. doi: 10.1186/s12962-020-00211-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Knowledge, understanding and perceptions of telemedicine amongst Chiropractors in South Africa in response to COVID-19. ProQuest website. https://www.proquest.com/openview/320203a5a7c805da1e8810d7912afc1b/1?pq-origsite=gscholar&cbl=2026366&diss=y. Accessed 9 July 2021.
- 30.Farao J. Digital health communication in South Africa during COVID-19. Glob Health Innov. 2020;3(1):1–3. [Google Scholar]
- 31.Grobbelaar S.S., Uriona-Maldonado M. Using technology to improve access to healthcare: The case of the MomConnect programme in South Africa. Local Economy. 2019;34(8):838–852. [Google Scholar]
- 32.Barron P., Pillay Y., Fernandes A., Sebidi J., Allen R. The MomConnect mHealth initiative in South Africa: Early impact on the supply side of MCH services. J Public Health Policy. 2016;37(Suppl 2):201–212. doi: 10.1057/s41271-016-0015-2. [DOI] [PubMed] [Google Scholar]
- 33.Coleman J., Eriksen J., Black V., Thorson A., Hatcher A. The Mobile Alliance for Maternal Action Text Message–Based mHealth Intervention for Maternal Care in South Africa: Qualitative User Study. JMIR Hum Factors. 2020;7(2):e14078. doi: 10.2196/14078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coleman J., Black V., Thorson A.E., Eriksen J. Evaluating the effect of maternal mHealth text messages on uptake of maternal and child health care services in South Africa: a multicentre cohort intervention study. Reprod Health. 2020;17:160. doi: 10.1186/s12978-020-01017-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Critical Discourse Analysis on Media Coverage of COVID-19 Contract Tracing Applications: Case of South Africa. ACM Digital Library website. https://dl.acm.org/doi/10.1145/3461564.3461580. Accessed 9 July 2021.
- 36.Lim W. Assessing the implications of digital contact tracing for COVID-19 for human rights and the rule of law in South Africa. Afr Hum Rights Law J. 2020;20(2):540–557. [Google Scholar]
- 37.Fischer A.E., van Tonder T., Gumede S.B., ST L.alla-E.dward. Changes in Perceptions and Use of Mobile Technology and Health Communication in South Africa During the COVID-19 Lockdown: Cross-sectional Survey Study. JMIR Form Res. 2021;5(5):e25273. doi: 10.2196/25273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brey Z., Mash R., Goliath C., Roman D. Home delivery of medication during Coronavirus disease 2019, Cape Town, South Africa: Short report. Afr J Prim Health Care Fam Med. 2020;12(1):e1–e4. doi: 10.4102/phcfm.v12i1.2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moore A.F., Hawarden V. Discovery Digital Health strategy: COVID-19 accelerates online health care in South Africa. Emerald Emerg Markets Case Stud. 2020;10(3):1–18. [Google Scholar]
- 40.Morse R.M., Myburgh H., Reubi D., et al. Opportunities for Mobile App–Based Adherence Support for Children With Tuberculosis in South Africa. JMIR Mhealth Uhealth. 2020;8(11):e19154. doi: 10.2196/19154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Assessing the impact of mobile technological innovation on maternal healthcare in South Africa. WIReDSpace website. http://wiredspace.wits.ac.za/handle/10539/30299. Accessed 9 July 2021.
- 42.Torres G., Neophytou N., Fourie P., Buntting X., Constantinou D., Gradidge P.J.L. 'I'm doing it for myself: Using a smartphone-based exercise service during the COVID-19 lockdown in the Faculty of Health Sciences, University of the Witwatersrand, South Africa. South Afr J Sports Med. 2021;33(1):1–6. doi: 10.17159/2078-516X/2021/v33i1a9053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moonasar D.M., Davies C., Balawanth R., et al. Progress, challenges and priorities for malaria elimination in South Africa. Trans R Soc South Afi. 2021;76(2):105–116. [Google Scholar]
- 44.Baloyi R.E., Shandukani M.B., Graffy R., et al. Evaluating a 24-h mobile reporting system for malaria notifications in comparison with a paper-based system in South Africa, 2015. Malar J. 2018;17(1):308. doi: 10.1186/s12936-018-2451-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brooke B.D., Raman J., Frean J., et al. Implementing malaria control in South Africa, Eswatini and southern Mozambique during the COVID-19 pandemic. S Afr Med J. 2020;110(11):1072–1076. [PubMed] [Google Scholar]
- 46.Mostert I., Roberts N., Plaatjies LA. In: Internet of Things, Infrastructures and Mobile Applications. IMCL 2019. Advances in Intelligent Systems and Computing, vol 1192. Auer M.E., Tsiatsos T., editors. Springer; Cham: 2021. Measuring Uptake and Engagement in an m-Learning Intervention: The Case of ChildConnect South Africa. [Google Scholar]
- 47.Muller C. Wearable activity-tracking device feature preference amongst South African generation Y students. Int J eBus eGovernment Stud. 2020;12(1):1–16. [Google Scholar]
- 48.Wesson J., Mujuru G., Cowley L. In: Intelligent Human Systems Integration 2021. IHSI 2021. Advances in Intelligent Systems and Computing, vol 1322. Russo D, Ahram T, Karwowski W, Di Bucchianico G, Taiar R, editors. Springer; Cham: 2021. Health and Activity Monitoring Using Smart Devices to Support the Self-management of Health Behavior. [Google Scholar]
- 49.Mash R.J., Presence-Vollenhoven M., Adeniji A., et al. Evaluation of patient characteristics, management and outcomes for COVID-19 at district hospitals in the Western Cape, South Africa: descriptive observational study. BMJ Open. 2021;11(1):e047016. doi: 10.1136/bmjopen-2020-047016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sibiya M.N., Ramlucken L. Willingness and feasibility of utilising short messaging services (SMS) as reminders of follow-up care to mental health care users in the uMgungundlovu District, KwaZulu-Natal. Int J Afr Nurs Sci. 2021;14:100294. [Google Scholar]
- 51.Siedner M.J., Harling G., Derache A., et al. Protocol: Leveraging a demographic and health surveillance system for Covid-19 Surveillance in rural KwaZulu-Natal. Wellcome Open Res. 2020;5:109. doi: 10.12688/wellcomeopenres.15949.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sehume O.L., Markus ED. A Critical Analysis of Medical Robotic Assistive Systems for Early Diagnosis of Common Ailments in South Africa. Int J Mech Eng Robot Res. 2020;9(10):1451–1456. [Google Scholar]
- 53.Watkins J.O.T.A., Goudge J., Gómez-Olivé F.X., Griffiths F. Mobile phone use among patients and health workers to enhance primary healthcare: A qualitative study in rural South Africa. Soc Sci Med. 2018;198:139–147. doi: 10.1016/j.socscimed.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 54.Pillay Y., Motsoaledi PA. Digital health in South Africa: innovating to improve health. BMJ Glob Health. 2018;3(Suppl 2):e000722. doi: 10.1136/bmjgh-2018-000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vula Mobile, the APP which puts members of the health services of rural isolated and under-medicalised areas in contact with specialists. Fondation Pierre Fabre website. https://www.odess.io/files/documents/enquetes/CR_ODESS2017-Vula%20Mobile_English.pdf. Accessed 18 July 2021.
- 56.SignappsTM Care is a suite of modular products that includes. SignappsTM website. https://www.getsignapps.com/products. Accessed 18 July 2021.
- 57.Hollander J.E., Carr BG. Virtually Perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 58.Osei E., Mashamba-Thompson T.P. Mobile health applications for disease screening and treatment support in low-and middle-income countries: a narrative review. Heliyon. 2021;7(3):e06639. doi: 10.1016/j.heliyon.2021.e06639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Southern Africa hoped it was through the worst of Covid-19. Then the Delta variant arrived. CNN website. https://edition.cnn.com/2021/07/09/africa/southern-africa-covid-delta-intl-cmd/index.html. Accessed 18 July 2021.
- 60.Chitungo I., Mhango M., Dzobo M., et al. Towards virtual doctor consultations: A call for the scale-up of telemedicine in sub-Saharan Africa during COVID-19 lockdowns and beyond. Smart Health. 2021;21:100207. doi: 10.1016/j.smhl.2021.100207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dodoo J.E., Al-Samarraie H., Alzahrani AI. Telemedicine use in Sub-Saharan Africa: Barriers and policy recommendations for Covid-19 and beyond. Int J Med Inform. 2021;151:104467. doi: 10.1016/j.ijmedinf.2021.104467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.David N.J., Brey Z., Ismail M. Telemedicine in the Western Cape Department of Health during the first peak of the COVID-19 pandemic: Leveraging data to save lives by activating a telemedicine response. Afr J Prim Health Care Fam Med. 2021;13(1):e1–e4. doi: 10.4102/phcfm.v13i1.2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Digital Health Centre of Excellence for COVID-19 Pandemic Response. ICT Works website. https://www.ictworks.org/covid-19-digital-health-centre-excellence/#. Accessed 18 July 2021.
- 64.Digital Engagement Solutions in Healthcare. EMGuidance website. https://emguidance.com/pharma. Accessed 18 July 2021.
- 65.Our Solutions. Right ePharmacy website. https://rightepharmacy.co.za/solutions/. Accessed 18 July 2021.
- 66.Power of Dual-Modality Imaging. CapeRay website. https://www.caperay.com/power-of-dual-modality/. Accessed 18 July 2021.
- 67.Lodox - Saving Lives through Innovative Solutions. Lodox Systems website. https://lodox.com/trauma/. Accessed 18 July 2021.
- 68.Karim S.S.A. The South African Response to the Pandemic. N Engl J Med. 2020;382(24):e95. doi: 10.1056/NEJMc2014960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Adebayo P.B., Oluwole O.J., Taiwo F.T. COVID-19 and Teleneurology in Sub-Saharan Africa: Leveraging the Current Exigency. Front Public Health. 2021;8:574505. doi: 10.3389/fpubh.2020.574505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kamulegeya L.H., Bwanika J.M., Musinguzi D., Bakibinga P. Continuity of health service delivery during the COVID-19 pandemic: the role of digital health technologies in Uganda. Pan Afr Med J. 2020;35(Suppl 2):43. doi: 10.11604/pamj.supp.2020.35.2.23115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kaushal R., Kern L.M., Barrón Y., Quaresimo J., Abramson E.L. Electronic Prescribing Improves Medication Safety in Community-Based Office Practices. J Gen Intern Med. 2010;25(6):530–536. doi: 10.1007/s11606-009-1238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Telepharmacy Win .A.Z. Time to pick up the line. Res Social Adm Pharm. 2017;13(4):882–883. doi: 10.1016/j.sapharm.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 73.Sridhar S.B., Rabbani S.A. Pharmaceutical care services provided by pharmacists during COVID-19 pandemic: perspectives from around the World. J Pharm Health Serv Res. 2021;12(3):463–468. [Google Scholar]
- 74.Goff D.A., Ashiru-Oredope D., Cairns K.A., et al. Global contributions of pharmacists during the COVID-19 pandemic. J Am Coll Clin Pharm. 2020;3(8):1480–1492. doi: 10.1002/jac5.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rapid Deployment of a Community-Centered Mobile Covid 19 Testing Unit to Improve Health Equity. NEJM Catalyst website. https://catalyst.nejm.org/doi/pdf/10.1056/CAT.20.0522. Accessed 18 July 2021.
- 76.Zhou S., van Staden Q., Toska E. Resource reprioritisation amid competing health risks for TB and COVID-19. Int J Tuberc Lung Dis. 2020;24(11):1215–1216. doi: 10.5588/ijtld.20.0566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mars M. Tele-Education in South Africa. Front Public Health. 2014;2:173. doi: 10.3389/fpubh.2014.00173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bagarukayo E., Kalema B. Evaluation of elearning usage in South African universities: A critical review. Int J Educ Dev Using Inf Commun Technol. 2015;11(2):168–183. [Google Scholar]
- 79.Schleicher A. The Impct of COVID-19 on Education: Insights from Education at a Glance 2020. OECD; Paris: 2020. [Google Scholar]
- 80.Higher education institutions and the use of online instruction and online tools and resources during the COVID-19 outbreak - An online review of selected U.S. and SA’s universities. Research Square website. https://www.researchsquare.com/article/rs-61482/v1. Accessed 18 July 2021.
- 81.Mpungose C.B. Is Moodle or WhatsApp the preferred e-learning platform at a South African university? First-year students’ experiences. Educ Inf Technol. 2020;25(2):927–941. [Google Scholar]
- 82.Oyediran W.O., Omoare A.M., Owoyemi M.A., Adejobi A.O., Fasasi R.B. Prospects and limitations of e-learning application in private tertiary institutions amidst COVID-19 lockdown in Nigeria. Heliyon. 2020;6(11):e05457. doi: 10.1016/j.heliyon.2020.e05457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Colven R., Shim M.H.M., Brock D., Todd G. Dermatological Diagnostic Acumen Improves with Use of a Simple Telemedicine System for Underserved Areas of South Africa. Telemed eHealth. 2011;17(5):363–369. doi: 10.1089/tmj.2010.0163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Faye O., Bagayoko C.O., Dicko A., et al. A Teledermatology Pilot Programme for the Management of Skin Diseases in Primary Health Care Centres: Experiences from a Resource-Limited Country (Mali, West Africa) Trop Med Infect Dis. 2018;3(3):88. doi: 10.3390/tropicalmed3030088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kwatra S.G., Sweren R.J., Grossberg A.L. Dermatology practices as vectors for COVID-19 transmission: a call for immediate cessation of nonemergent dermatology visits. J Am Acad Dermatol. 2020;82(5):e179–e180. doi: 10.1016/j.jaad.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Marolana L.E.M., Scott R.E., Mars M. A Teledermatology Scale-Up Framework and Roadmap for Sustainable Scaling: Evidence-Based Development. J Med Internet Res. 2018;20(6):e9940. doi: 10.2196/jmir.9940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Boufarasse Y.B., Ettahir A., Bekkali D., Bennani J. Teleradiology and AI as Solution to Overcome the COVID-19 PandemicImpact during the Lockdowns in Africa. Health Sci J. 2020;14(6):771. [Google Scholar]
- 88.Rehani B., Rodriguez J.A., Nguyen J.K., et al. COVID-19 Radiology Preparedness, Challenges & Opportunities: Responses From 18 Countries. Curr Probl Diagn Radiol. 2022;51(2):196–203. doi: 10.1067/j.cpradiol.2021.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Essop H., Kekana M. The experiences of teleradiology end users regarding role extension in a rural district of the North West province: A qualitative analysis. Afr J Prim Health Care Fam Med. 2020;12(1):1–8. doi: 10.4102/phcfm.v12i1.2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sethole K.M., Rudman E., Hazell L.J. Methods Used by General Practitioners to Interpret Chest Radiographs at District Hospitals in the City of Tshwane, South Africa. J Med Imaging Radiat Sci. 2020;51(2):271–279. doi: 10.1016/j.jmir.2019.12.010. [DOI] [PubMed] [Google Scholar]
- 91.Ferenczi G.L., Mahmood A.N., Bergmann R.K. Telemedicine Pre and Post Covid-19: Lessons for Commercialisation Based on Previous Use Cases. J Int Soc Telemed eHealth. 2020;8(65):e8. [Google Scholar]
- 92.Khan T., Bertram M.Y., Jina R., Mash B., Levitt N., Hofman K. Preventing diabetes blindness: Cost effectiveness of a screening programme using digital non-mydriatic fundus photography for diabetic retinopathy in a primary health care setting in South Africa. Diabetes Res Clin Pract. 2013;101(2):170–176. doi: 10.1016/j.diabres.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 93.Rachapelle S., Legood R., Alavi Y., et al. The Cost–Utility of Telemedicine to Screen for Diabetic Retinopathy in India. Ophthalmology. 2013;120(3):566–573. doi: 10.1016/j.ophtha.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 94.Nyika G.T. Use of ICTS for socio-economic development of marginalised communities in rural areas: Proposals for establishment of sectoral Rural Entrepreneurial Networks. J Dev Commun Stud. 2020;7(1-2):126–147. [Google Scholar]
- 95.Patterson V. Neurological telemedicine in the COVID-19 era. Nat Rev Neurol. 2020;17(2):73–74. doi: 10.1038/s41582-020-00438-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sarfo F.S., Adamu S., Awuah D., Ovbiagele B. Tele-neurology in sub-Saharan Africa: A systematic review of the literature. J Neurol Sci. 2017;380:196–199. doi: 10.1016/j.jns.2017.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.de Wit M., Gaskin A., Coetzee M., Louw Q.A., Plastow N.A. Navigating Telerehabilitation for student training: Sharing experiences. South Afr J Occup Ther. 2021;51(1):454. [Google Scholar]
- 98.Kn G.H., Fong K.N. Effects of telerehabilitation in occupational therapy practice: A systematic review. Hong Kong J Occup Ther. 2019;32(1):3–21. doi: 10.1177/1569186119849119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Grossheim L., Ruff P., Ngoma T., et al. Cancer and COVID-19 Experiences at African Cancer Centers: The Silver Lining. JCO Glob Oncol. 2021;7:410–415. doi: 10.1200/GO.20.00564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Irabor O.C., Swanson W., Shaukat F., et al. Can the Adoption of Hypofractionation Guidelines Expand Global Radiotherapy Access? An Analysis for Breast and Prostate Radiotherapy. JCO Glob Oncol. 2020;6:667–678. doi: 10.1200/JGO.19.00261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chipps J., Mars M. Readiness of health-care institutions in KwaZulu-Natal to implement telepsychiatry. J Telemed Telecare. 2012;18(3):133–137. doi: 10.1258/jtt.2012.SFT103. [DOI] [PubMed] [Google Scholar]
- 102.Mash R.J., Presence-Vollenhoven M., Adeniji A., et al. Evaluation of patient characteristics, management and outcomes for COVID-19 at district hospitals in the Western Cape, South Africa: descriptive observational study. BMJ Open. 2021;11(1):e047016. doi: 10.1136/bmjopen-2020-047016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Radin J.M., Quer G., Jalili M., Hamideh D., Steinhubl S.R. The hopes and hazards of using personal health technologies in the diagnosis and prognosis of infections. Lancet Digit Health. 2021;3(7):E455–E461. doi: 10.1016/S2589-7500(21)00064-9. [DOI] [PubMed] [Google Scholar]
- 104.Dietrich J.J., Hornschuh S., Khunwane M., et al. A mixed methods investigation of implementation barriers and facilitators to a daily mobile phone sexual risk assessment for young women in Soweto, South Africa. PLoS One. 2020;15(4):e0231086. doi: 10.1371/journal.pone.0231086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Georgette N., Siedner M.J., Petty C.R., Zanoni B.C., Carpenter S., Haberer JE. Impact of a clinical program using weekly Short Message Service (SMS) on antiretroviral therapy adherence support in South Africa: a retrospective cohort study. BMC Med Inform Decis Mak. 2017;17(1):18. doi: 10.1186/s12911-017-0413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Maraba N., Orrell C., Chetty-Makkan C.M., et al. Evaluation of adherence monitoring system using evriMED with a differentiated response compared to standard of care among drug-sensitive TB patients in three provinces in South Africa: a protocol for a cluster randomised control trial. Trials. 2021;22(1):389. doi: 10.1186/s13063-021-05337-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ben Fekih R., Lahami M. Application of Blockchain Technology in Healthcare: A Comprehensive Study. Impact Dig Technol Public Health Dev Dev Countr. 2020;12157:268–276. [Google Scholar]