The COVID-19 pandemic has brought about a public health crisis of substantial scale. As of January 2022, there had been over 281 million confirmed cases of COVID-19 worldwide and over 5.4 million deaths reported to the World Health Organization.1 In response to the pandemic, global lockdowns, social distancing, and quarantine procedures were imposed. Because of the high risk of transmission of COVID-19 due to aerosols and other occupational exposures, many countries suspended elective oral health care during the pandemic.
According to the American Cancer Society,2 oral cancer is a cancer within the oral cavity including the buccal mucosa, the teeth, the gums, the front two-thirds of the tongue, the floor of the mouth below the tongue, the bony roof of the mouth and the retromolar trigone. Oral cancer is a major health concern in both high- and low-income countries. The American Cancer Society’s estimates for oral cancer in the United States in 2021 included about 54,010 new cases of oral cavity or oropharyngeal cancer, with an overall 5-year survival rate of approximately 60%.3 , 4
Regular dental visits are integral to maintaining oral health and minimizing risks associated with a delayed and more severe diagnosis. The pandemic, in addition to interrupting continuity of care and preventative health care visits, has led to a dramatic increase in certain risk factors for oral carcinogenesis, including increased use of tobacco and alcohol, poor diet, and increased rates of obesity and poor oral hygiene. It is critical to understand the impact of the practice restrictions on oral health care and oral cancer diagnosis and progression. The postlockdown continuation of these trends raises substantial concern for health care providers. Health care providers need to be vigilant in identifying changes in patient lifestyle behaviors.
Background
Oral cancer remains the sixth most common cancer in the world.5 In most ethnic groups, the prevalence of oral cancer is 3 times higher in men than in women.6 According to the World Health Organization,7 there are an estimated 657,000 new cases of cancers of the oral cavity and pharynx each year and more than 330,000 deaths. From 2014 through 2018, oral cavity and pharynx cancer showed an increase in mortality for men and a decrease in mortality for women.
Patients undergoing kidney, bone marrow, heart, or liver transplant and patients with HIV infection are all at increased risk of developing oral malignancies,8 which may be related to the underlying immunosuppressed state or immunosuppressive treatment regimens for patients with these conditions. In addition, oral cancer is associated with a depression of the cell-mediated immune response.9 The Centers for Disease Control and Prevention considers immunosuppressed patients to be at high risk of developing serious illness from COVID-19. This is particularly concerning for patients with long-standing use of systemic corticosteroids or other immunosuppressive agents related to cancer treatment, including patients with oral cancer.10
Lee and colleagues11 reported in 2021 that compared with participants without cancer, those living with cancer had a 60% increased risk of a positive COVID-19 test. Chemotherapeutic treatment also was associated with a 2.2-fold increased risk of testing positive for COVID-19, with the association between cancer and COVID-19 infection most pronounced among participants who were 65 years and older and male. Although it is unsurprising that the most severe outcomes of a respiratory illness like COVID-19 have been associated with patients diagnosed with lung cancer, the association of the immunosuppressed state with carcinogenesis and chemotherapy puts patients managing a cancer diagnosis at an increased risk.12 , 13
Risk Factors For Oral Cancer: Changing Trends During The COVID-19 Pandemic
The development of oral cancer has been linked to tobacco and alcohol use, poor diet and nutrition, excess body weight, human papillomavirus (HPV) infection, poor oral hygiene, and male sex.14
Emerging research indicates that tobacco use, alcohol consumption, and obesity rates have risen significantly during the COVID-19 pandemic.15, 16, 17, 18, 19 These risk factors, in addition, are implicated in an increased risk of experiencing COVID-19–related mortality. If postpandemic trends in tobacco use, alcohol use, diet, and obesity continue, we postulate increases in global oral cancer rates and a necessity for more aggressive screening practices.
Tobacco
The relationship between tobacco use and oral cancer pathogenesis has been established firmly.20, 21, 22 Research suggests that the risk of developing oral cancer is 3 times higher in smokers than in nonsmokers.23 However, pandemic-related anxiety, boredom, and irregular routines have driven substantial increases in tobacco use during the COVID-19 pandemic.16 Even more concerning, smoking cessation rates also have declined during the pandemic. Calls to cessation support programs in 2020 were at the lowest since 2007, further demonstrating the substantial negative impact the COVID-19 pandemic had on smoking rates compared with rates during the previous period of over a decade.24 Studies have found no sex differences with increased smoking rates or reduced smoking cessation, suggesting that these trends are holding true for all smokers.25 A 2020 study found a global increase in electronic cigarette consumption as well as nicotine products used to cope with pandemic-related stress and anxiety.26
Personal hygiene and HPV
The COVID-19 pandemic has interrupted routine preventative dental services severely, owing to dental office closures amid lockdowns. Poor oral hygiene and oral health care and chronic ulceration due to improper dentures have all been implicated in an increase in oral cancer rates, especially in combination with other risk factors.27 With the use of masks, toothbrushing frequency also has been shown to have decreased significantly, as people have been less concerned about oral hygiene and reported halitosis.28 In addition, poor oral hygiene also can be secondary to self-neglect in people with depression, which has been exacerbated because of the pandemic.29 , 30
In addition, poor oral hygiene has been shown to be an independent risk factor for HPV infection.31 , 32 HPV disrupts the cell cycle, destroying tumor suppressor proteins and leading to dysplasia in the mouth and throat. Moreover, early in the pandemic, HPV vaccination rates among adolescents fell 75% owing to a decrease in wellness visits, and throughout the pandemic, child and teen HPV vaccination rates declined approximately 20%.33 , 34 We posit that these changing trends in oral hygiene and vaccination rates will lead to higher incidence of oral cancer in the future.
Alcohol
Many patients who receive a diagnosis of oral cancer are heavy drinkers, and alcohol use remains high in countries with increasing oral cancer rates.27 , 35 , 36 In a cross-sectional study of US adults during the pandemic, approximately two-thirds of participants reported increased alcohol consumption compared with before the pandemic.15 Study participants reported consuming an average of 26.8 alcohol drinks on 12.2 of the past 30 days. A total of 34.1% of participants reported engaging in binge drinking, and 7% reported engaging in extreme binge drinking during this time.15 Across Europe and Asia, alcohol sales and consumption have increased similarly.37
The top reported reasons for increased alcohol use were higher levels of stress, greater alcohol availability, and general boredom.15 People with pandemic-related depression were 64% more likely to increase their alcohol intake, and those with pandemic-related anxiety were 41% more likely to do so.38 A study found that the relationship between emotional distress and increased alcohol consumption was more significant for men than women, with 12.7% of men indicating that they began drinking more during the pandemic compared with 11.6% of women.39 These studies indicate that extreme stress during the pandemic was correlated with more significant increases in alcohol consumption.
Diet, nutrition, and obesity
Poor diet and nutrition and obesity have been linked to oral carcinogenesis.27 , 40 Obesity has been found to be associated with a 5-fold increase in risk of experiencing death from early-stage squamous cell carcinoma of the tongue.41 In addition, obesity has been linked with worse outcomes once a patient has been diagnosed with oral cancer, possibly putting the patient in an even more immunocompromised state.42, 43, 44 Hyperadiposity, dysregulated energy metabolism, increased levels of proinflammatory mediators, and altered adipolin levels all have been postulated as carcinogenic mechanisms.41
Throughout the COVID-19 pandemic, prolonged lockdowns, work from home policies, and gym closures all have contributed to worse dietary habits and increased body weight. Studies examining adolescent food intake during the COVID-19 pandemic recorded increased consumption of fried and sweet food and red meat and increasing caloric intake of foods with lesser nutritional value.17, 18, 19 According to the American Psychological Association, weight gain has been particularly challenging for parents of children 18 years and younger, with 55% of fathers reporting unintentional weight changes.45 Rises in weight gain during the pandemic also can be attributed to a general loss of routine and structure involving sleep dysregulation, reduced physical activity, disrupted family time, increased access to unhealthy snacks, and less consistent access to appropriately proportional meals.46
A cross-sectional study among US adults after mandatory quarantines were lifted still found increased consumption of sweet and salty snacks that was adopted during the pandemic.47 If habits adopted during the COVID-19 pandemic continue, practitioners must take additional considerations to assess risk stratification for patients with oral cancer who are at high risk and continue to ask patients about lifestyle changes at regular intervals.
Discussion
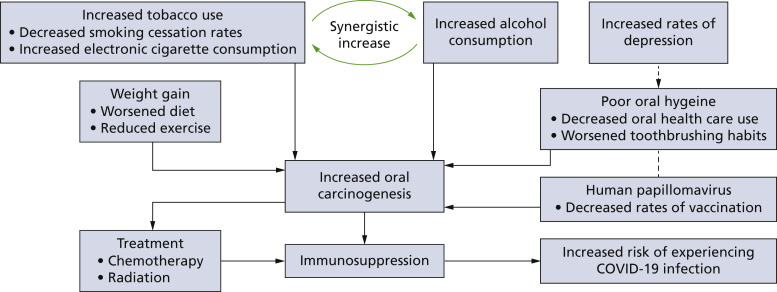
The COVID-19 pandemic has brought about many lifestyle and behavioral changes that can greatly affect oral cancer incidence, detection, and treatment. Worsening rates of tobacco and alcohol use, poor diet, weight gain, and oral hygiene, all of which are postulated to contribute to the acceleration of oral cancer development (Figure), have been documented globally in the past year. These statistics provide reason to believe that the incidence of oral cancer can rise as more patients return to dental care providers, especially as lockdown trends continue. Increasingly severe presentations of oral cancer at the time of diagnosis because of treatment delays intended to minimize COVID-19 transmission are also of concern. Given that over 6 million adults have lost their dental insurance owing to the pandemic and more than 1 in 10 people in the United States have delayed oral health care owing to cost, lack of insurance, and fear of exposure to severe acute respiratory syndrome coronavirus 2,48 health care providers must screen vigilantly for these risk factors and lifestyle changes in the context of oral cancer.
Figure.
Pathway of rising oral cancer risk factors and incidence in the context of the COVID-19 pandemic. The flowchart depicts how screening and intervention can disrupt the cycle of immunosuppressant and increased infection rate. Figure created with BioRender.com.
As of January 2022, nearly 507 million COVID-19 vaccine doses had been administered in the United States,49 and more than 8.6 billion COVID-19 vaccine doses had been administered worldwide.1 However, both domestically and globally, many more doses must be administered for a return to normalcy in daily living and clinical care. With unreliable sources of information on the internet and social media, it is a dentist’s responsibility to serve as a knowledgeable guide to navigating the intricacies of living through a pandemic. Providers must investigate how informed a patient is about avoiding risk factors, discuss vaccination and the importance it holds as a prevention tool, and provide a nonjudgmental space for learning.
Oral health care providers also must educate their patients about the oral systemic risks associated with increased alcohol and tobacco consumption, poor diet and nutrition, and worsening oral hygiene. Dental care practitioners must be vigilant about rises in oral cancer risk factors and must increase screening measures for all demographics, with particular attention to weight and nutritional changes in adolescents and fathers and increases in alcohol use among men. We recommend that oral health care providers increase collaboration with their medical counterparts to increase HPV vaccination rates and encourage medical wellness visits throughout the pandemic. Given pandemic-related trends, dentists must continue to examine for oral manifestations of HPV and improve in-office screening metrics.
Although the true effect of the COVID-19 pandemic on oral cancer risk factors remains unclear, dental care practitioners must remain vigilant. Increasing COVID-19 rates may increase patient high-risk behaviors and reduce the frequency of patient visits to their dental homes, further necessitating more comprehensive screening practices. Educating patients about how to conduct their own at-home oral cancer screenings also can be beneficial to mitigating oral cancer spread.
Conclusions
Medical and dental health care providers must be conscious of the lasting impact the COVID-19 pandemic may have on oral cancer outcomes for decades, owing to altered lifestyle habits that have formed since March 2020. The recent uprise in cases and widespread dissemination of the Delta variant indicate that our struggle with severe acute respiratory syndrome coronavirus 2 is far from over. Thus, to minimize the degree of spread, it is important that providers maintain proper public health measures.
Biographies
Ms. Nath is a predoctoral student, Harvard School of Dental Medicine, Boston, MA.
Mr. Ferreira is a predoctoral student, Harvard School of Dental Medicine, Boston, MA.
Ms. McVicar is a predoctoral student, Harvard School of Dental Medicine, Boston, MA.
Ms. Oshilaja is a predoctoral student, Harvard School of Dental Medicine, Boston, MA.
Dr. Swann is an assistant professor of Oral Health Policy and Epidemiology, the interim dean for Diversity, Inclusion, and Belonging, Department of Oral Health Policy and Epidemiology, Harvard School of Dental Medicine, 188 Longwood Ave, Boston, MA 02115.
Footnotes
Disclosures. None of the authors reported any disclosures.
Commentaries represent the opinions of the authors and not necessarily those of the American Dental Association.
References
- 1.Coronavirus disease (COVID-19) pandemic World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019?gclid=CjwKCAiAs92MBhAXEiwAXTi25w2aUxy6vnxho_6pqdhxsQ4jP-zQerbZqbKYqRxICrEHP66tFg1-RxoC5WMQAvD_BwE
- 2.What are oral cavity and oropharyngeal cancers? American Cancer Society. https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/about/what-is-oral-cavity-cancer.html#:∼:text=Oral%20cavity%20cancer%20starts%20in,to%20grow%20out%20of%20control
- 3.Oral cancer 5-year survival rates by race, gender, and stage of diagnosis. National Institute of Dental and Craniofacial Research, National Institutes of Health. https://www.nidcr.nih.gov/research/data-statistics/oral-cancer/survival-rates
- 4.Key statistics for oral cavity and oropharyngeal cancers. https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/about/key-statistics.html
- 5.Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009;45(4-5):309–316. doi: 10.1016/j.oraloncology.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Rivera C. Essentials of oral cancer. Int J Clin Exp Pathol. 2015;8(9):11884–11894. [PMC free article] [PubMed] [Google Scholar]
- 7.Annual report to the nation 2021: national trends in cancer death rates infographic. Surveillance, Epidemiology, and End Results Program, National Institutes of Health. https://seer.cancer.gov/report_to_nation/infographics/trends_mortality.html
- 8.Vial T., Descotes J. Immunosuppressive drugs and cancer. Toxicology. 2003;185(3):229–240. doi: 10.1016/s0300-483x(02)00612-1. [DOI] [PubMed] [Google Scholar]
- 9.Sathiyasekar A.C., Chandrasekar P., Pakash A., Kumar K.U.G., Jaishlal M.S. Overview of immunology of oral squamous cell carcinoma. J Pharm Bioallied Sci. 2016;8(suppl 1):S8–S12. doi: 10.4103/0975-7406.191974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shanti R.M., Stoopler E.T., Weinstein G.S., et al. Considerations in the evaluation and management of oral potentially malignant disorders during the COVID-19 pandemic. Head Neck. 2020;42(7):1497–1502. doi: 10.1002/hed.26258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee K.A., Ma W., Sikavi D.R., et al. COPE consortium Cancer and risk of COVID-19 through a general community survey. Oncologist. 2021;26(1):e182–e185. doi: 10.1634/theoncologist.2020-0572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Addeo A., Friedlaender A. Cancer and COVID-19: unmasking their ties. Cancer Treat Rev. 2020;88:102041. doi: 10.1016/j.ctrv.2020.102041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang L., Chai P., Yu J., Fan X. Effects of cancer on patients with COVID-19: a systematic review and meta-analysis of 63,019 participants. Cancer Biol Med. 2021;18(1):298–307. doi: 10.20892/j.issn.2095-3941.2020.0559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Risk factors for oral cavity and oropharyngeal cancers American Cancer Society. https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/causes-risks-prevention/risk-factors.html
- 15.Grossman E.R., Benjamin-Neelon S.E., Sonnenschein S. Alcohol consumption during the COVID-19 pandemic: a cross-sectional survey of US adults. Int J Environ Res Public Health. 2020;17(24):9189. doi: 10.3390/ijerph17249189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giovenco D.P., Spillane T.E., Maggi R.M., Lee E.Y., Philbin M.M. Multi-level drivers of tobacco use and purchasing behaviors during COVID-19 “lockdown”: a qualitative study in the United States. Int J Drug Policy. 2021;94:103175. doi: 10.1016/j.drugpo.2021.103175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruiz-Roso M.B., Padilha P.D.C., Mantilla-Escalante D.C., et al. Covid-19 confinement and changes of adolescent’s dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients. 2020;12(6):1807. doi: 10.3390/nu12061807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pietrobelli A., Pecoraro L., Ferruzzi A., et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity (Silver Spring) 2020;28(8):1382–1385. doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robinson E., Boyland E., Chisholm A., et al. Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite. 2021;156:104853. doi: 10.1016/j.appet.2020.104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Risk factors. Oral Cancer Foundation. https://oralcancerfoundation.org/cdc/risk-factors/
- 21.Lee J., Taneja V., Vassallo R. Cigarette smoking and inflammation: cellular and molecular mechanisms. J Dent Res. 2012;91(2):142–149. doi: 10.1177/0022034511421200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Selya A.S., Rose J.S., Dierker L., Hedeker D., Mermelstein R.J. Evaluating the mutual pathways among electronic cigarette use, conventional smoking and nicotine dependence. Addiction. 2018;113(2):325–333. doi: 10.1111/add.14013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gandini S., Botteri E., Iodice S., et al. Tobacco smoking and cancer: a meta-analysis. Int J Cancer. 2008;122(1):155–164. doi: 10.1002/ijc.23033. [DOI] [PubMed] [Google Scholar]
- 24.Report on the impact of the COVID-19 pandemic on smoking cessation. North American Quitline Consortium. https://cdn.ymaws.com/www.naquitline.org/resource/resmgr/reports-naqc/report_impact__of_covid-19_p.pdf
- 25.Mihaltan F.D., Rajnoveanu A.-G., Rajnoveanu R.-M. Impact of smoking on women during the Covid-19 pandemic. Front Med (Lusanne) 2021;8:584061. doi: 10.3389/fmed.2021.584061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yach D. Tobacco use patterns in five countries during the COVID-19 lockdown. Nicotine Tob Res. 2020;22(9):1671–1672. doi: 10.1093/ntr/ntaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kumar M., Nanavati R., Modi T., Dobariya C. Oral cancer: etiology and risk factors: a review. J Cancer Res Ther. 2016;12(2):458–463. doi: 10.4103/0973-1482.186696. [DOI] [PubMed] [Google Scholar]
- 28.Pinzan-Vercelino C.R.M., Freitas K.M.S., Girão V.M.P., Silva D.O., Peloso R.M., Pinzan A. Does the use of face masks during the COVID-19 pandemic impact on oral hygiene habits, oral conditions, reasons to seek dental care and esthetic concerns? J Clin Exp Dent. 2021;13(4):e369–e375. doi: 10.4317/jced.57798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kunzler A.M., Röthke N., Günthner L., et al. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Global Health. 2021;17(1):34. doi: 10.1186/s12992-021-00670-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kisely S. No mental health without oral health. Can J Psychiatry. 2016;61(5):277–282. doi: 10.1177/0706743716632523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bui T.C., Markham C.M., Ross M.W., Mullen P.D. Examining the association between oral health and oral HPV infection. Cancer Prev Res. 2013;6(9):917. doi: 10.1158/1940-6207.CAPR-13-0081. [DOI] [PubMed] [Google Scholar]
- 32.Dalla Torre D., Burtscher D., Sölder E., Rasse M., Puelacher W. The correlation between the quality of oral hygiene and oral HPV infection in adults: a prospective cross-sectional study. Clin Oral Investig. 2019;23(1):179–185. doi: 10.1007/s00784-018-2425-y. [DOI] [PubMed] [Google Scholar]
- 33.Daniels V., Saxena K., Roberts C., et al. Impact of reduced human papillomavirus vaccination coverage rates due to COVID-19 in the United States: a model based analysis. Vaccine. 2021;39(20):2731–2735. doi: 10.1016/j.vaccine.2021.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nation’s cancer centers urge action to get HPV vaccinations back on track. UC Davis Health Comprehensive Cancer Center. https://health.ucdavis.edu/cancer/news/headlines/nations-cancer-centers-urge-action-to-get-hpv-vaccinations-back-on-track/2021/05
- 35.Ogden G.R. Alcohol and oral cancer. Alcohol. 2005;35(3):169–173. doi: 10.1016/j.alcohol.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 36.Mello F.W., Melo G., Pasetto J.J., Silva C.A.B., Warnakulasuriya S., Rivero E.R.C. The synergistic effect of tobacco and alcohol consumption on oral squamous cell carcinoma: a systematic review and meta-analysis. Clin Oral Investig. 2019;23(7):2849–2859. doi: 10.1007/s00784-019-02958-1. [DOI] [PubMed] [Google Scholar]
- 37.Ramalho R., Adiukwu F., Gashi Bytyçi D., et al. Alcohol and tobacco use during the COVID-19 pandemic: a call for local actions for global impact. Front Psychiatry. 2021;12:634254. doi: 10.3389/fpsyt.2021.634254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Capasso A., Jones A.M., Ali S.H., Foreman J., Tozan Y., DiClemente R.J. Increased alcohol use during the COVID-19 pandemic: the effect of mental health and age in a cross-sectional sample of social media users in the U.S. Prev Med. 2021;145:106422. doi: 10.1016/j.ypmed.2021.106422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thompson K., Dutton D.J., MacNabb K., Liu T., Blades S., Asbridge M. Changes in alcohol consumption during the COVID-19 pandemic: exploring gender differences and the role of emotional distress. Health Promot Chronic Dis Prev Can. 2021;41(9):254–263. doi: 10.24095/hpcdp.41.9.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bernzweig E., Payne J.B., Reinhardt R.A., Dyer J.K., Patil K.D. Nicotine and smokeless tobacco effects on gingival and peripheral blood mononuclear cells. J Clin Periodontol. 1998;25(3):246–252. doi: 10.1111/j.1600-051x.1998.tb02435.x. [DOI] [PubMed] [Google Scholar]
- 41.Iyengar N.M., Kochhar A., Morris P.G., et al. Impact of obesity on the survival of patients with early-stage squamous cell carcinoma of the oral tongue. Cancer. 2014;120(7):983–991. doi: 10.1002/cncr.28532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grossberg A.J., Chamchod S., Fuller C.D., et al. Association of body composition with survival and locoregional control of radiotherapy-treated head and neck squamous cell carcinoma. JAMA Oncology. 2016;2(6):782–789. doi: 10.1001/jamaoncol.2015.6339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang K., Yu X.H., Tang Y.J., Tang Y.L., Liang X.H. Obesity: an emerging driver of head and neck cancer. Life Sci. 2019;233:116687. doi: 10.1016/j.lfs.2019.116687. [DOI] [PubMed] [Google Scholar]
- 44.Iyengar N.M., Ghossein R.A., Morris L.G., et al. White adipose tissue inflammation and cancer-specific survival in patients with squamous cell carcinoma of the oral tongue. Cancer. 2016;122(24):3794–3802. doi: 10.1002/cncr.30251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.One year on: unhealthy weight gains, increased drinking reported by Americans coping with pandemic stress. American Psychological Association. http://www.apa.org/news/press/releases/2021/03/one-year-pandemic-stress
- 46.Jenssen B.P., Kelly M.K., Powell M., Bouchelle Z., Mayne S.L., Fiks A.G. COVID-19 and changes in child obesity. Pediatrics. 2021;147(5) doi: 10.1542/peds.2021-050123. [DOI] [PubMed] [Google Scholar]
- 47.Bin Zarah A., Enriquez-Marulanda J., Andrade J.M. Relationship between dietary habits, food attitudes and food security status among adults living within the United States three months post-mandated quarantine: a cross-sectional study. Nutrients. 2020;12(11):3468. doi: 10.3390/nu12113468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tranby E.P., Jacob M., Kelly A., Frantsve-Hawley J. State of oral health equity in America 2021 research report 1: a coming surge in oral health treatment needs. CareQuest Institute for Oral Health Advancement. https://www.carequest.org/system/files/CareQuest-Institute-Coming-Surge-Oral-Health-Treatment-Needs-Report-1.pdf
- 49.COVID-19 vaccine data Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/index.html