Abstract
Purpose.
Individuals with poor physical and mental health may face elevated risk for suicide, particularly suicide by firearm.
Methods.
This retrospective cohort study used statewide, longitudinally-linked ED patient record and mortality data to examine 12-month incidence of firearm suicide among emergency department (ED) patients presenting with a range of physical health problems. Participants included all residents presenting to a California ED in 2009-2013 with nonfatal visits for somatic diagnoses hypothesized to increase suicide risk, including myocardial infarction, congestive heart failure, cerebrovascular disease, chronic obstructive pulmonary disease, diabetes, cancer, back pain, headache, joint disorder, and injuries. For each patient diagnostic group, we calculated rates of firearm suicide per 100,000 person-years and standardized mortality ratios (SMRs) relative to the demographically matched California population.
Results.
Firearm suicide rates per 100,000 person-years ranged from 9.6 (among patients presenting with unintentional injury) to 55.1 (patients with cancer diagnoses), with SMRs from 1.48 to 7.45 (all p<0.05). SMRs for patients with cardiovascular conditions ranged from 2.45 to 5.10. Males and older individuals had higher firearm suicide rates, and there was substantial between-group variability in the proportion of suicide decedents who used a firearm.
Conclusions.
ED patients presenting with deliberate self-harm injuries, substance use, and cancer were especially at risk for firearm suicide. To avoid missed suicide-prevention opportunities, EDs should implement evidence-based suicide interventions as a best practice for their patients.
Keywords: Suicide, firearm, emergency department
In 2018, 61.5% of all firearm deaths in the United States were suicides, and 50.5% of all suicides involved a firearm (1). Moreover, between 2001 and 2018 firearm suicide rates rose 18% overall, and even more among demographic subgroups (e.g., women) (1). A growing consensus indicates that means restriction strategies, such as legislation regulating access to firearms (e.g., permit-to-purchase laws and extreme risk protection orders), are effective at preventing firearm suicides (2-8). While necessary, these community-based interventions are likely insufficient to address the burden of firearm suicide deaths. Efforts that focus on early identification of and selective prevention among individuals with elevated risk for firearm suicide will also be important (9,10).
Prior research suggests that firearm suicide decedents differ in important ways from suicide decedents who use other means, offering potential insight into subpopulations of high-risk individuals who could be targeted for screening and intervention efforts (11). For example, firearm suicide decedents are more likely than other suicide decedents to be male, older, and of non-Hispanic white or black race/ethnicity (12,13); to have access to firearms (14,15), to lack a documented history of psychiatric problems and/or psychiatric treatment (15-17), and to be suffering from serious physical illness or disability (16,17). Specific to this last association, firearm suicide decedents – particularly males – are more likely than other suicide decedents to have recently experienced or been hospitalized for injury, substance use, cardiovascular disease, cancer, and other chronic illnesses (16,17). Suicide by any means is also associated with decedent history of major physical health conditions, even after accounting for comorbid mental health and substance use problems (18-20).
The associations between physical health conditions and firearm suicide risk suggest that patients seen in healthcare settings may be an important population to target for firearm suicide prevention (21). Indeed, the Zero Suicide campaign (22) – a health care system organizational commitment to safer suicide care – is based on research indicating that suicidal individuals frequently make healthcare visits prior to their deaths (16,23), and that provider-based screening and brief intervention strategies may reduce suicidal behavior (24,25). Although the Zero Suicide campaign calls for broad implementation of screening and intervention, most suicide prevention programs in healthcare settings still target individuals exhibiting overtly suicidal or self-harming behavior. Interventions specific to firearm suicide prevention, however, may have better success if targeted to high-risk individuals who do not exhibit overt suicidality – since suicide attempts involving a firearm are usually the person’s initial attempt (26) and usually fatal (16,17). Identifying subsets of healthcare patients with physical health problems who face elevated risk of firearm suicide would inform the development of clinical practice guidelines, screening instruments, and lethal means counseling strategies (27-29).
Identifying these patients, who may represent “missed opportunities” for suicide prevention, requires a prospective design that follows patients from an index healthcare visit and ascertains their subsequent firearm suicide mortality outcomes. To our knowledge, no such studies exist (30), largely due to the low base rate of firearm suicide and scarcity of databases that link healthcare and mortality records. Most previous research examining individual-level risk factors for firearm suicide relies upon case series or case-control designs (e.g., (13,15-17,31)). The only prior cohort studies focused on firearm ownership (32,33) or risk factors specific to military personnel (34).
Here, we contribute to this sparse literature by examining rates of firearm suicide mortality in selected groups of emergency department (ED) patients. EDs are a promising healthcare setting for reducing population suicide risk (21,35), as ED patients have higher concentrations of suicide risk than outpatients (36-38), comprise a larger proportion and broader spectrum of the population than hospitalized patients (39,40), and are already the site of effective intervention programs (24,41). We focused on patients with somatic illness diagnoses that prior research identified as potentially associated with elevated risk of firearm suicide, including various chronic illnesses, cancer, non-cancerous pain conditions, and injuries (16-20). To contextualize these findings, we also examined patients with substance use or mental health problems known to be strongly associated with suicide risk (42).
METHODS
Data
We obtained discharge data from the California Office of Statewide Health Planning and Development (OSHPD) on all visits between 2009-2013 to all California-licensed EDs by individuals aged ≥5 years with a California residential zip code (n=51,951,260). OSPHD also provided information on all individuals in this ED cohort to the California Department of Public Health Vital Records, which assessed vital status in California death records and provided information on date and underlying cause of death for all matching decedents who died in 2009-2013 (excluding those who died out of state, <1% of the total), the most recent years of mortality data available. Probabilistic linkage matching was implemented based on patient’s social security number (SSN), gender, birthdate, race/ethnicity, and zip code of residence. All data obtained and used by the study team were de-identified. This study was approved by the Institutional Review Boards of the California Health and Human Services Agency and the University of California, Merced.
Data for the current study initially included all patient ED visit records with a valid SSN at which the patient was discharged alive (n=44,545,676; 85.8%). We retained all patient visits that received a principal International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis included in one of our diagnostic groups of interest (n=17,292,539). We constructed these diagnostic groups based on prior literature (18,43,44). The groups were as clinically specific as possible while maximizing statistical power, given the rare outcome. There were six chronic illness groups (myocardial infarction, congestive heart failure, cerebrovascular disease, chronic obstructive pulmonary disease (COPD), diabetes, and all other chronic illnesses, defined following the Charlson Comorbidity Index (45)); cancer (45); four non-cancerous pain condition groups (back pain, headache, joint disorders, and other pain conditions) (43); three injury groups (unintentional, assault, and deliberate self-harm injuries); mental disorder; and substance use. Specific ICD-9-CM codes used to define each diagnostic group are shown in the Table 1 footnote.
Table 1.
12-month rates of firearm suicide and associated SMRs among California emergency department patients presenting in 2009-2013, according to patient diagnostic group.
| Diagnostic group | Total unique individuals in diagnostic group |
Firearm suicide deaths, n |
Incidence rate per 100,000 person-years |
Standardized mortality ratio | ||
|---|---|---|---|---|---|---|
| Rate | 95% CI | SMRa | 95% CI | |||
| Chronic illnessb | ||||||
| Myocardial infarction | 181,715 | 22 | 13.5 | 8.9, 20.5 | 2.45 | 1.53, 3.71 |
| Congestive heart failure | 238,096 | 60 | 30.2 | 23.4, 38.9 | 5.10 | 3.89, 6.56 |
| Cerebrovascular disease | 331,106 | 53 | 17.9 | 13.7, 23.5 | 3.24 | 2.43, 4.23 |
| COPD | 743,180 | 85 | 11.8 | 9.6, 14.6 | 2.31 | 1.85, 2.86 |
| Diabetes | 189,889 | 22 | 12.0 | 7.9, 18.3 | 2.34 | 1.47, 3.55 |
| Other chronic illness | 168,832 | 31 | 20.8 | 14.7, 29.6 | 3.71 | 2.52, 5.27 |
| Cancerc | 217,082 | 80 | 55.1 | 44.3, 68.7 | 7.45 | 5.91, 9.28 |
| Non-cancerous paind | ||||||
| Back pain | 877,036 | 121 | 14.0 | 11.7, 16.8 | 2.79 | 2.32, 3.33 |
| Headache | 712,109 | 52 | 7.4 | 5.6, 9.7 | 1.48 | 1.10, 1.94 |
| Joint disorders | 507,466 | 45 | 9.0 | 6.7, 12.1 | 1.79 | 1.31, 2.40 |
| Other non-cancerous pain | 320,672 | 43 | 13.8 | 10.2, 18.6 | 2.71 | 1.96, 3.65 |
| Injurye | ||||||
| Unintentional injury | 6,095,058 | 574 | 9.6 | 8.9, 10.4 | 1.90 | 1.75, 2.07 |
| Assault injury | 413,427 | 49 | 11.9 | 9.0, 15.8 | 2.40 | 1.77, 3.17 |
| Deliberate self-harm injury | 136,210 | 119 | 88.7 | 74.1, 106.1 | 17.67 | 14.64, 21.14 |
| Mental disorderf | 654,704 | 262 | 40.6 | 35.9, 45.8 | 8.09 | 7.14, 9.14 |
| Substance useg | 353,736 | 147 | 42.3 | 36.0, 49.8 | 8.40 | 7.10, 9.88 |
Abbreviations: CI, confidence interval; COPD, chronic obstructive pulmonary disease.
Calculated from California data for 2009-2014 from CDC WISQARS (external causes), standardized to match the distribution of gender, age category, and race/ethnicity category of the corresponding group from the ED cohort.
Chronic illness diagnostic groups’ ICD-9-CM codes: Myocardial infarction, 410.x, 412.x; congestive heart failure, 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 425.4-425.9, 428.x; cerebrovascular disease, 362.34, 430.x-438.x; COPD, 416.8, 416.9, 490.x-505.x, 506.4, 508.1, 508.8; diabetes, 250.0-250.3, 250.8, 250.9, 250.4-250.7; other chronic disease, 042.x-044.x, 070.22, 070.23, 070.32, 070.33, 070.44, 070.54, 070.6, 070.9, 093.0, 290.x, 294.1, 331.2, 334.1, 342.x, 343.x, 344.0-344.6, 344.9, 403.01, 403.11, 403.91, 404.02, 404.03, 404.12, 404.13, 404.92, 404.93, 437.3, 440.x, 441.x, 443.1-443.9, 446.5, 447.1, 456.0-456.2, 531.x-534.x, 557.1, 557.9, 570.x, 571.x, 572.2-572.8, 573.3, 573.4, 573.8, 573.9, 582.x, 583.0-583.7, 585.x, 586.x, 588.0, 710.0-710.4, 714.0-714.2, 714.8, 725.x, V42.0, V43.4, V42.7,V45.1, V56.x.
Cancer diagnostic group’s ICD-9-CM codes: 140-239, 258.02-258.03, 511.81, 789.x, 795.x, 796.70-796.76, V10.x, V12.72, V58.x, V66.1-V66.2, V67.1-V67.2.
Non-cancerous pain diagnostic groups’ ICD-9-CM codes: Back pain, 720-724.x; headache, 339.0-339.x, 346.0-346.x, 784.0; joint disorders, 713-716.x, 718-719.x; other non-cancerous pain, 307.89, 307.81, 388.29, 729.1, 780.96, 800.0-804.x, 850.0-854.x, 907.0, V155.2.
Injury diagnostic groups’ ICD-9-CM codes: Unintentional injury, E000-E019.x, E029-E030.x, E800-E806.x, E810-E838.x, E840-E858.x, E860-E888.x, E890-E928.x; assault injury, E960.0-E960.9; deliberate self-harm injury, E950.0-E950.8.
Mental disorder diagnostic group’s ICD-9-CM codes: 293.8x, 295.x, 296.x, 297.x, 298.x, 300.0-300.5x, 300.89, 300.9, 308.0-308.9, 309.x, 311.0-314.x, V62.84.
Substance use diagnostic group’s ICD-9-CM codes: 291.x, 292.x, 303.x, 304.x, 305.00-305.03, 305.20-305.93, 357.5, 425.5, 535.3, 571.0-571.3, 648.30-648.34, 655.50-655.53, 760.71-760.73, 760.75, 779.5, 965.00-965.02, 965.09, 980.0, V65.42.
A unique patient could have multiple qualifying visits in a diagnostic group during the study period; only his or her first-occurring visit was retained for analysis (hereafter, the “index visit”). Patients could be members of multiple diagnostic groups. Diagnostic group-specific counts of total visits and total unique patients are shown in Appendix Figure 1. For all index visits resulting in patient discharge or transfer to another facility, the index date was the date of ED presentation. For visits that resulted in a same-hospital admission, the index date was the date of hospital discharge from the associated hospitalization (46).
We extracted age-, gender-, and race-specific counts of firearm suicide deaths in California in 2009-2013, and corresponding population denominators, from the Center for Disease Control’s WONDER compressed mortality files database (47). These files are derived from death certificates collected by the states and are considered complete (48).
Measures
Our primary outcome of interest was death within one year of the index date by firearm suicide. Firearm suicide was defined as any death with ICD-10 codes X72, X73, or X74 as the immediate cause of death. The secondary outcome was death by suicide from any mechanism (ICD-10 codes X60-X84, Y87.0, or U03).
Patient demographic characteristics were examined for purposes of description, heterogeneity analyses, and to calculate standardized mortality ratios. These characteristics included sex (male, female), age group (5-24, 25-44, 45-64, ≥65 years), race/ethnicity (collapsed into non-Hispanic white, non-Hispanic black, Hispanic, Asian/Pacific Islander, other), and insurance status (private, Medicaid, Medicare, self-pay/other).
Analyses
We calculated crude mortality rates per 100,000 person-years of follow-up for firearm suicide death and any suicide death in the year after the index date, for each patient diagnostic group separately. Person-time accrued to a given diagnostic group was calculated as beginning on each patient’s index visit date for that group and ending on the patient’s date of death, 365 days after his or her index visit, or Dec. 31, 2013, whichever was earliest. Individuals who did not link to California mortality records from 365 days after the index date were presumed alive for this period. Decedents were treated as censored on their date of death.
We calculated annualized standardized mortality rate ratios (SMRs) as the ratio of the observed numbers of deaths in each ED patient group to expected deaths in that group. Confidence intervals around SMRs (95% CIs) were calculated using Fisher’s exact method. The numbers of expected deaths in California for 2009-2013 for firearm suicide were calculated using the Centers for Disease Control and Prevention WONDER mortality database, standardized to the distribution of sex, age category, and race/ethnicity category of the respective ED diagnostic groups.
Within each diagnostic group, we further calculated age-, sex-, and race/ethnicity-specific rates of firearm suicide, and used Cox proportional hazards regression models to test for group differences (17,49-51). Younger, female, and Hispanic individuals were used as the reference categories in these analyses, based on research showing reduced suicide risk in these groups (38). Lastly, because there is heterogeneity in the likelihood of using a firearm in the event of a suicide attempt (12,52), we calculated proportion of each patient group’s total suicide deaths that involved a firearm. Statistical analyses were conducted using Stata 14.0 (StataCorp LP).
RESULTS
Cohort characteristics
A total of 8,684,782 ED patients had index visits in at least one diagnostic group. The average follow-up time was 341.3 days. There were 1,254 total firearm suicide deaths observed in the study population, accounting for approximately 17% of all firearm suicide deaths in California during the study period (53). The crude firearm suicide in California during this period was 4.1 per 100,000 (1).
Firearm suicide rates
Firearm suicide rates in the year after index visit within each patient diagnostic group are shown in Table 1. Rates among patients presenting with chronic illnesses were high, ranging from 11.8 per 100,000 (COPD patients) to 30.2 per 100,000 (congestive heart failure patients). The corresponding SMRs indicated that chronic illness patients were 2.3 to 5.1 times more likely than the demographically matched population to die by firearm suicide; all 95% CIs around these SMR estimates excluded the null.
Patients with a cancer diagnosis had a very high 12-month firearm suicide rate of 55.1 per 100,000, more than seven times higher than the demographically matched population (SMR: 7.45, 95% CI: 5.91, 9.28).
Firearm suicide rates among patients in the non-cancerous pain groups were somewhat lower than those in the chronic illness and cancer groups. The lowest rate was among headache patients, at 7.4 per 100,000, and the highest was among back pain patients, at 14.0 per 100,000. These rates were all significantly higher than the demographically matched population, with SMRs ranging from 1.48 (95% CI: 1.10, 1.94) to 2.79 (95% CI: 2.32, 3.33).
Firearm suicide rates among injury patients varied substantially. The highest observed rate was in the deliberate self-harm patient group (88.7 per 100,000), whose firearm suicide rate was nearly 18 times higher than that of the demographically matched California population (SMR: 17.7, 95% CI: 14.6, 21.1). The lowest rate was among unintentional injury patients (9.6 per 100,000), who were approximately two times more likely than the California population to die by firearm suicide (SMR: 1.9, 95% CI: 1.8, 2.1).
ED patients presenting with mental disorder or substance use had high firearm suicide rates (42.3 per 100,000 and 40.6 per 100,000, respectively). Notably, these rates were comparable to or slightly lower that of cancer patients. Compared to the demographically matched California population, firearm suicide rates among patients with mental disorder (SMR: 8.09, 95% CI: 7.14, 9.14) and substance use (SMR: 8.40, 95% CI: 7.10, 9.88) were approximately 8-fold higher.
Heterogeneity in firearm suicide rates by demographic characteristics
Hazard rates of firearm suicide were 3 to 18 times higher among male patients compared to female patients, a significant difference in every diagnostic group (Table 3; Appendix Figure 2). Older patient age was generally associated with higher risk of firearm suicide, although the strength of this pattern varied by patient group (Table 3; Appendix Figure 3). In most diagnostic groups, individuals of non-Hispanic white race had significantly higher firearm suicide rates than Hispanic patients; statistical power was more limited for the other race groups and estimates were imprecise (Table 3; Appendix Figure 4).
Table 3.
Associations between patient demographic factors at index visit and firearm suicide rate, according to patient diagnostic group.
| Diagnostic group | Age group (reference: patients 5-24 years) | Male gender (reference: females) HR (95% CI)a |
Race/ethnicity (reference: Hispanic patients) | |||||
|---|---|---|---|---|---|---|---|---|
| 25-44 years HR (95% CI)a |
45-64 years HR (95% CI)a |
≥65 years HR (95% CI)a |
NH White HR (95% CI)a |
NH Black HR (95% CI)a |
Asian/PI HR (95% CI)a |
NH other HR (95% CI)a |
||
| Chronic illnessb | ||||||||
| MI | -- | -- | 3.55 (1.20, 10.50) | [undefined] | [undefined] | [undefined] | [undefined] | [undefined] |
| CHF | -- | -- | 2.42 (1.19, 4.92) | 13.6 (4.9, 37.6) | 3.84 (1.54, 9.59) | 0.33 (0.04, 2.84) | [undefined] | [undefined] |
| CVD | -- | -- | 0.81 (0.47, 1.41) | 6.06 (2.86, 12.85) | 7.6 (1.9, 31.5) | 3.10 (0.52, 18.55) | 2.03 (0.29, 14.41) | 5.3 (0.8, 37.7) |
| COPD | -- | -- | 6.65 (4.20, 10.48) | 9.32 (4.95, 17.55) | 8.68 (3.51, 21.47) | 1.11 (0.27, 4.64) | 0.97 (0.11, 8.30) | 2.33 (0.45, 11.99) |
| Diabetes | -- | -- | 4.41 (1.88, 10.31) | 5.50 (1.63, 18.59) | 4.42 (1.48, 13.23) | 0.62 (0.07, 5.54) | 1.71 (0.19, 15.29) | [undefined] |
| Other | -- | -- | 1.06 (0.51, 2.18) | 5.98 (2.09, 17.08) | 13.7 (1.9, 101.6) | 9.9 (1.1, 88.3) | 3.0 (0.2, 48.6) | 7.2 (0.5, 115.7) |
| Cancer | 0.10 (0.01, 0.85) | 0.88 (0.33, 2.34) | 1.97 (0.79, 4.92) | 12.5 (6.0, 26.0) | 34.9 (4.9, 251.5) | 6.3 (0.7, 60.5) | 9.4 (1.1, 84.1) | 18.3 (1.9, 175.8) |
| Non-cancer pain | ||||||||
| Back pain | 1.63 (1.22, 2.19) | 2.91 (2.22, 3.81) | 3.99 (3.05, 5.21) | 6.85 (5.35, 8.76) | 4.83 (3.61, 6.46) | 1.24 (0.75, 2.06) | 1.40 (0.81, 2.43) | 2.50 (1.57, 3.99) |
| Headache | 1.02 (0.44, 2.35) | 1.77 (0.79, 3.93) | 2.82 (1.17, 6.81) | 18.0 (7.7, 42.1) | 12.4 (3.9, 39.9) | [undefined] | 3.88 (0.65, 23.34) | 4.0 (0.7, 23.9) |
| Joint disorders | 1.30 (0.44, 3.88) | 1.73 (0.64, 4.68) | 2.08 (0.75, 5.78) | 6.10 (2.84, 13.11) | 5.43 (1.94, 15.23) | 0.84 (0.15, 4.60) | [undefined] | 2.51 (0.46, 13.70) |
| Other | 2.06 (0.70, 6.01) | 3.39 (1.23, 9.33) | 3.99 (1.42, 11.20) | 10.3 (3.7, 28.9) | 3.97 (1.55, 10.14) | 1.08 (0.21, 5.56) | 0.94 (0.11, 8.08) | 0.98 (0.12, 8.42) |
| Injury | ||||||||
| Unintentional | 1.63 (1.22, 2.19) | 2.91 (2.22, 3.81) | 3.99 (3.05, 5.21) | 6.85 (5.35, 8.76) | 4.83 (3.61, 6.46) | 1.24 (0.75, 2.06) | 1.40 (0.81, 2.43) | 2.50 (1.57, 3.99) |
| Assault | 1.21 (0.62, 2.39) | 1.72 (0.82, 3.60) | 2.12 (0.48, 9.25) | 8.5 (2.6, 27.3) | 1.65 (0.84, 3.20) | 0.87 (0.35, 2.19) | 0.66 (0.09, 5.00) | 0.82 (0.19, 3.65) |
| DSH | 2.34 (1.33, 4.13) | 3.45 (1.95, 6.10) | 11.50 (6.14, 21.5) | 4.20 (2.78, 6.36) | 3.69 (1.98, 6.89) | 0.72 (0.20, 2.59) | 3.03 (1.12, 8.19) | 1.61 (0.51, 5.07) |
| Mental disorder | 1.40 (0.94, 2.08) | 2.38 (1.63, 3.47) | 3.27 (2.14, 4.98) | 4.98 (3.69, 6.71) | 3.86 (2.64, 5.63) | 1.00 (0.51, 1.95) | 1.72 (0.92, 3.61) | 0.97 (0.41, 2.33) |
| Substance use | 1.96 (1.14, 3.38) | 3.01 (1.79, 5.06) | 3.47 (1.79, 6.73) | 3.45 (2.21, 5.39) | 3.06 (1.83, 5.08) | 0.46 (0.13, 1.56) | 2.29 (0.77, 6.82) | 1.42 (0.53, 3.86) |
Abbreviations: HR, hazard ratio; NH, non-Hispanic; CI, confidence interval; MI, myocardial infarction; CHF, congestive heart failure; CVD, cerebrovascular disease; COPD, chronic obstructive pulmonary disease; DSH, deliberate self-harm.
Where the absolute distance between upper- and lower-bound CIs was very wide (≥20), we report the point estimate and 95% CIs to one decimal place.
Due to small numbers and the relatively low base rate of firearm suicide in chronic illness diagnostic groups, the reference category for age analyses in these diagnostic groups was patients aged 5-64 years.
Firearm suicides as a proportion of all suicide deaths
There was considerable heterogeneity across diagnostic groups in the proportion of total suicide deaths accounted for by firearm suicides (Table 2 and Figure 1). The lowest proportion was among deliberate self-harm patients, in whom firearm suicides accounted for just 12.9% of all 924 suicide deaths. The highest proportion was among cancer patients, in whom firearm suicides accounted for a striking 70.2% of 114 suicide deaths. In general, firearm suicides accounted for higher proportions of suicide among cancer patients (70%) and chronic illness patients (ranging from 33% to 67%) than among the other diagnostic groups (13% to 36%).
Table 2.
Contribution of firearm suicides to total suicide deaths among patients seen in the emergency department, according to patient diagnostic group.
| Total suicide deaths | ||||
|---|---|---|---|---|
| Diagnostic group | N | Incidence rate per 100,000 person-years |
95% CI | Percent of all suicide deaths that involved a firearm |
| Chronic illness | ||||
| Myocardial infarction | 36 | 22.1 | (15.9, 30.6) | 61.1% |
| Congestive heart failure | 89 | 44.8 | (36.4, 55.1) | 67.4% |
| Cerebrovascular disease | 109 | 36.8 | (30.5, 44.5) | 48.6% |
| COPD | 207 | 28.8 | (25.1, 33.0) | 41.1% |
| Diabetes | 66 | 36.0 | (28.3, 45.9) | 33.3% |
| Other chronic illness | 63 | 42.4 | (33.1, 54.2) | 49.2% |
| Cancer | 114 | 78.6 | (65.4, 94.4) | 70.2% |
| Non-cancerous pain | ||||
| Back pain | 348 | 40.3 | (36.3, 44.8) | 34.8% |
| Headache | 200 | 28.3 | (24.6, 32.5) | 26.0% |
| Joint disorders | 151 | 30.3 | (25.8, 35.5) | 29.8% |
| Other non-cancerous pain | 119 | 38.2 | (31.9, 45.7) | 36.1% |
| Injuries | ||||
| Unintentional injury | 1,624 | 27.2 | (25.9, 28.6) | 35.4% |
| Assault injury | 235 | 57.1 | (50.3, 64.9) | 20.9% |
| Deliberate self-harm injury | 924 | 688.3 | (645.3, 734.2) | 12.9% |
| Mental disorder | 1,256 | 194.4 | (184.0, 205.5) | 20.9% |
| Substance use | 531 | 152.9 | (140.5, 166.5) | 27.7% |
Total suicide counts and incidence rates include suicide by any means.
Figure 1.
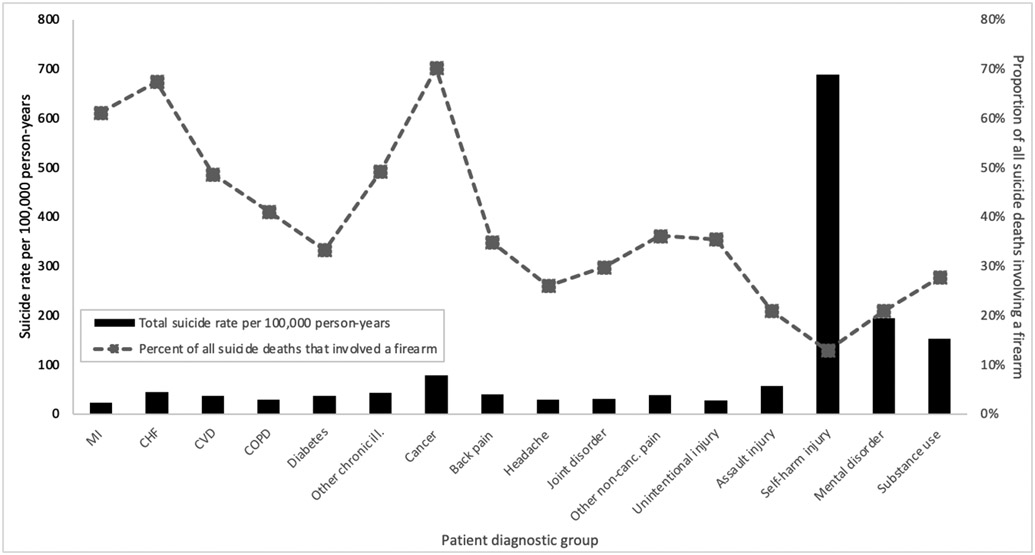
Total suicide rate, and proportion of all suicide deaths that involved a firearm, by patient diagnostic group.
DISCUSSION
This study represents, to the best of our knowledge, the first population-based examination of firearm suicide rates among patients seen in the emergency department in the U.S. We found that patients presenting with cancer, congestive heart failure, cerebrovascular disease, and other chronic diseases had comparatively high rates of firearm suicide (3- to 8-fold higher than the demographically matched population). Some of these rates were as high as those found among patients presenting with mental disorder or substance use diagnoses. Rates among patients presenting with non-cancerous pain conditions and injuries were also elevated (1.5- to 2.8-fold higher than the general population). These findings strongly reinforce the value of the emergency department as a “boundaried setting” in which to implement firearm suicide prevention practices (21), and suggest that subgroups of patients with physical health problems – not only patients with overt suicidality or other behavioral health issues – could be promising targets for interventions such as lethal means and safe storage counseling (54).
Our findings are consistent with U.S. case-control and case series studies showing associations between death by firearm suicide and history of physical and mental illness (16,17), as well as cohort studies documenting excess risk of suicide (by any means) among patients with specific conditions like cancer (38,55). Our study advances this prior work by assessing prospectively-assessed firearm suicide rates among multiple diagnostic groups within a defined patient population, allowing for direct inference about which patient groups might benefit most from firearm-specific suicide prevention efforts.
We also report, for the first time, substantial heterogeneity across patient groups in the likelihood of using a firearm vs. other means, given death by suicide. For example, 70% of suicides among cancer patients involved a firearm, as compared with 41% among COPD patients and just 20% among assault injury patients. Surprisingly, the likelihood of using a firearm was comparatively low among patients with mental disorder (21%) and substance use problems (28%). Explanations for this heterogeneity are not clear, but may involve differential access to or familiarity with guns, as well as socio-cultural norms around the appropriateness of using firearms in suicidal crises (13,17,49,50,56,57). Prior work has documented sociodemographic variation in rates of suicide using a firearm vs. other means, but basing prevention efforts on sociodemographic risk indicators alone is challenging (52,57). Our study provides actionable evidence that means safety/restriction approaches specifically addressing firearms (e.g., screening for firearm access, promoting safe firearm storage practices (58)) may be most useful for preventing suicide death in ED patients presenting with cancer, cardiovascular disease, and chronic illnesses, who often suffer severe distress and depression (59,60). This may be particularly appropriate for patients who are also male, older, and/or non-Hispanic white.
There is broad public acceptance around health professionals initiating gun safety conversations when these conversations involve a patient with known elevated risk for firearm-related harm (61). Nevertheless, barriers remain: ED physicians often report believing that most of their patients would not benefit from a discussion of firearm safety (62), or express concern about “physician gag laws” that ostensibly prohibit practitioners from inquiring whether patients own firearms or from delivering gun-safety messages (63) (although such statutes do not apply when the information is relevant to the health of the patient or others) (30). Future research should examine whether access to information about which patients face excess risk of firearm suicide alters clinicians’ and policymakers’ attitudes towards offering respectful and effective patient counsel around firearm safety. In addition, future work could leverage public health survey data or longitudinal patient records to further probe the role of physical health problems in suicide risk, and utilize machine learning predictive modeling methods to compute individualized firearm suicide risk (64,65).
Strengths and limitations
Our study had several important advantages, including a large population-based cohort with over eight million individual ED patients, from the largest and most diverse U.S. state; comprehensive coding of external cause of injury, which is not available in all states; and inclusion of suicide mortality outcomes from validated high-quality registers, which are also not available in all states.
Several limitations should be considered when interpreting the results. Because the sociodemographic characteristics of California differ from those of other states and because California has a relatively low state suicide rate, the results may not generalize to the entire US (1). Mortality data for ED patients who died outside of California were not available for this study, and there was some truncation bias among patients whose index visits occurred in 2013; we expect these artefacts resulted in a slight downward bias on both the absolute suicide rates in our ED groups. Diagnoses made in ED contexts are prone to error and misclassification, and the assignment of patients to diagnostic groups could thus be subject to misclassification. Furthermore, the administrative dataset lacked other important information, such as patient clinical severity and socio-environmental risk factors for suicide. Death determinations that classify whether a given death was a suicide are also subject to misclassification for reasons related to stigma avoidance, legal/religious pressure, and under-resourcing of death investigation systems; the typical result is under-counting of suicides (66). In patients without a psychiatric diagnosis or history of mental health treatment, coroners may be less likely to rule their deaths as suicide, so misclassification could be differential based on patient group (67).
Conclusion
The high risk of firearm suicide following emergency department visits for specific physical and behavioral health problems highlights the potential value of targeting these patients for suicide prevention efforts – including targeted screening (68), safety planning interventions (69), access to lethal means counseling, and caring postcards sent by hospital staff after patient discharge (54) – if future research demonstrates that such interventions are effective and cost-effective in these patient populations. Increasing clinical attention to the psychological distress experienced by patients suffering from chronic illnesses, cancer, and pain conditions may help address the public health burden of firearm suicide in the US.
Supplementary Material
Acknowledgments
This project was funded through the University of California Firearm Violence Research Center and through National Institute of Mental Health grant R15 MH113108-01. The sponsors had no role in the study design; collection, analysis, or interpretation of data; writing of the report, or decision to submit the article for publication.
The authors would like to thank the two anonymous reviewers for their helpful suggestions when revising the manuscript.
Contributor Information
Sidra Goldman-Mellor, Department of Public Health; School of Social Sciences, Humanities, and Arts; University of California, Merced; Merced CA 95343, USA..
Carlisha Hall, Department of Public Health; School of Social Sciences, Humanities, and Arts; University of California, Merced; Merced CA 95343, USA..
Magdalena Cerdá, Department of Population Health at NYU Grossman School of Medicine; New York, NY 10016, USA.
Harish Bhat, Department of Applied Mathematics, School of Natural Sciences; University of California, Merced; Merced CA 95343.
References
- 1.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) Fatal Injury Reports: National, regional, and state (restricted), 1999-2017. Retrieved from https://webappa.cdc.gov/sasweb/ncipc/mortrate.html on February 20, 2019.
- 2.Miller M, Barber C, White RA, et al. Firearms and suicide in the United States: Is risk independent of underlying suicidal behavior? Am. J. Epidemiol 2013;178(6):946–955. [DOI] [PubMed] [Google Scholar]
- 3.Crifasi CK, Meyers JS, Vernick JS, et al. Effects of changes in permit-to-purchase handgun laws in Connecticut and Missouri on suicide rates. Prev. Med 2015;79:43–49. [DOI] [PubMed] [Google Scholar]
- 4.Reisch T, Steffen T, Habenstein A, et al. Change in suicide rates in Switzerland before and after firearm restriction resulting from the 2003 “Army XXI” reform. Am. J. Psychiatry 2013;170:977–984. [DOI] [PubMed] [Google Scholar]
- 5.Miller M, Azrael D, Barber C. Suicide mortality in the United States: The importance of attending to method in understanding population-level disparities in the burden of suicide. Annu. Rev. Public Health 2012;33(1):393–408. [DOI] [PubMed] [Google Scholar]
- 6.Rodríguez Andrés A, Hempstead K. Gun control and suicide: The impact of state firearm regulations in the United States, 1995-2004. Health Policy. 2011;101(1):95–103. [DOI] [PubMed] [Google Scholar]
- 7.Kivisto AJ, Phalen PL. Effects of risk-based firearm seizure laws in Connecticut and Indiana on suicide rates, 1981-2015. Psychiatr. Serv 2018;69(8):855–862. [DOI] [PubMed] [Google Scholar]
- 8.Swanson JW, Norko MA, Lin HJ, et al. Implementation and effectiveness of Connecticut’s risk-based gun removal law: Does it prevent suicides? Law Contemp. Probl 2017;80(2):179–208. [Google Scholar]
- 9.Mann JJ, Michel CA. Prevention of firearm suicide in the United States: What works and what is possible. Am. J. Psychiatry 2016;173(10):969–979. [DOI] [PubMed] [Google Scholar]
- 10.Sumner SA, Maenner MJ, Socias CM, et al. Sentinel events preceding youth firearm violence: An investigation of administrative data in Delaware. Am. J. Prev. Med 2016;51(5):647–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ranney ML, Fletcher J, Alter H, et al. A consensus-driven agenda for emergency medicine firearm injury prevention research. Ann. Emerg. Med 2017;69(2):227–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu RT, Kraines MA, Puzia ME, et al. Sociodemographic predictors of suicide means in a population-based surveillance system: Findings from the National Violent Death Reporting System. J. Affect. Disord 2013;151(2):449–454. [DOI] [PubMed] [Google Scholar]
- 13.Joe S, Marcus SC, Kaplan MS. Racial differences in the characteristics of firearm suicide decedents in the United STates. Am J Orthopsychiatry. 2007;77(1):124–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Opoliner A, Azrael D, Barber C, et al. Explaining geographic patterns of suicide in the US: the role of firearms and antidepressants. Inj. Epidemiol 2014;1(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anestis MD, Khazem LR, Anestis JC. Differentiating suicide decedents who died using firearms from those who died using other methods. Psychiatry Res. 2017;252:23–28. [DOI] [PubMed] [Google Scholar]
- 16.Hempstead K, Nguyen T, David-Rus R, et al. Health problems and male firearm suicide. Suicide Life-Threatening Behav. 2013;43(1):1–16. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan MS, McFarland BH, Huguet N. Characteristics of adult male and female firearm suicide decedents: findings from the National Violent Death Reporting System. Inj. Prev 2009;15(5):322 LP – 327. [DOI] [PubMed] [Google Scholar]
- 18.Ahmedani BK, Peterson EL, Hu Y, et al. Major physical health conditions and risk of suicide. Am. J. Prev. Med 2017;53(3):308–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Webb RT, Kontopantelis E, Doran T, et al. Suicide risk in primary care patients with major physical diseases: A case-control study. Arch. Gen. Psychiatry 2012;69(3):256–264. [DOI] [PubMed] [Google Scholar]
- 20.Juurlink DN, Herrmann N, Szalai JP, et al. Medical illness and the risk of suicide in the elderly. Arch. Intern. Med 2004;164(11):1179–1184. [DOI] [PubMed] [Google Scholar]
- 21.U.S. Department of Health and Human Services (HHS) Office of the Surgeon General, National Action Alliance for Suicide Prevention. 2012 National Strategy for Suicide Prevention: Goals and Objectives for Action. 2012. [PubMed]
- 22.Suicide Prevention Resource Center. Zero Suicide in Health and Behavioral Health Care: Toolkit. Retrieved from zerosuicide.edc.org/toolkit on August 8, 2020.
- 23.Ahmedani BK, Simon GE, Stewart C, et al. Health care contacts in the year before suicide death. J. Gen. Intern. Med 2014;29(6):870–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miller IW, Camargo CA, Arias SA, et al. Suicide prevention in an emergency department population: The ED-SAFE study. JAMA Psychiatry. 2017;74(6):563–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hampton T Depression care effort brings dramatic drop in large HMO population’s suicide rate. JAMA. 2010;303(19):1903–1905. [DOI] [PubMed] [Google Scholar]
- 26.Spicer RS, Miller TR. Suicide acts in 8 states: Incidence and case fatality rates by demographics and method. Am. J. Public Health 2000;90(12):1885–1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The Joint Commission. Detecting and treating suicide ideation in all settings. Sentin. Event Alert 2016;(56):1–7. [PubMed] [Google Scholar]
- 28.Petrik ML, Betz ME, Olson-Madden JH, et al. Identification, assessment, and management of suicide risk in emergency departments: Significant updates in research and practice. Curr. Emerg. Hosp. Med. Rep 2017;5(2):94–102. [Google Scholar]
- 29.Pallin R, Spitzer SA, Ranney ML, et al. Preventing firearm-related death and injury. Ann. Intern. Med 2019;170(11):ITC81. [DOI] [PubMed] [Google Scholar]
- 30.Wintemute GJ, Betz ME, Ranney ML. Yes, you can: Physicians, patients, and firearms. Ann. Intern. Med 2016;165(3):205–213. [DOI] [PubMed] [Google Scholar]
- 31.Kaufman EJ, Morrison CN, Branas CC, et al. State firearm laws and interstate firearm deaths from homicide and suicide in the United States: A cross-sectional analysis of data by county. JAMA Intern. Med 2018;178(5):692–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wintemute GJ, Parham CA, Beaumont JJ, et al. Mortality among recent purchasers of handguns. N. Engl. J. Med 1999;341:1583–9. [DOI] [PubMed] [Google Scholar]
- 33.Studdert DM, Zhang Y, Swanson SA, et al. Handgun ownership and suicide in California. N. Engl. J. Med 2020;382(23):2220–2229. [DOI] [PubMed] [Google Scholar]
- 34.Anglemyer A, Miller ML, Buttrey S, et al. Suicide rates and methods in active duty military personnel, 2005 to 2011: a cohort study. Ann. Intern. Med 2016;165(3):167–174. [DOI] [PubMed] [Google Scholar]
- 35.Larkin GL, Beautrais AL. Emergency departments are underutilized sites for suicide prevention. Crisis. 2010;31(1):1–6. [DOI] [PubMed] [Google Scholar]
- 36.Colpe LJ, Pringle BA. Data for building a national suicide prevention strategy. Am. J. Prev. Med 2014;47(3):S130–S136. [DOI] [PubMed] [Google Scholar]
- 37.Claassen CA, Larkin GL. Occult suicidality in an emergency department population. Br. J. Psychiatry 2005;186(APR):352–353. [DOI] [PubMed] [Google Scholar]
- 38.Goldman-Mellor SJ, Olfson M, Lidon-Moyano C, et al. Association of suicide and other mortality with emergency department presentation. JAMA Netw. Open 2019;2(12):e1917571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Olfson M, Gameroff MJ, Marcus SC, et al. Emergency treatment of young people following deliberate self-harm. Arch. Gen. Psychiatry 2005;62(10):1122–1128. [DOI] [PubMed] [Google Scholar]
- 40.Olfson M, Marcus SC, Bridge JA. Emergency treatment of deliberate self-harm. Arch. Gen. Psychiatry 2012;69(1):80–88. [DOI] [PubMed] [Google Scholar]
- 41.Fleischmann A Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries. Bull. World Health Organ 2008;86(9):703–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Franklin JC, Ribeiro JD, Fox KR, et al. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol. Bull 2017;143(2):187–232. [DOI] [PubMed] [Google Scholar]
- 43.Ilgen MA, Kleinberg F, Ignacio RV., et al. Noncancer pain conditions and risk of suicide. JAMA Psychiatry. 2013;70(7):692–697. [DOI] [PubMed] [Google Scholar]
- 44.Crandall C, Fullerton-Gleason L, Aguero R, et al. Subsequent suicide mortality among emergency department patients seen for suicidal behavior. Acad. Emerg. Med 2006;13:435–442. [DOI] [PubMed] [Google Scholar]
- 45.Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. J. Clin. Epidemiol 1994;47(11):1245–1251. [DOI] [PubMed] [Google Scholar]
- 46.Olfson M, Wall M, Wang S, et al. Suicide following deliberate self-harm. Am. J. Psychiatry 2017;174(8):765–774. [DOI] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention (National Center for Health Statistics). Compressed Mortality File 1999-2016 on CDC WONDER Online Database. 2017. Accessed from https://wonder.cdc.gov/cmf-icd10.html on September 20, 2002.
- 48.Centers for Disease Control and Prevention. CDC WONDER Compressed Mortality File help files. Accessed from https://wonder.cdc.gov/wonder/help/cmf.html on August 19, 2020.
- 49.Ajdacic-Gross V, Weiss MG, Ring M, et al. Methods of suicide: International suicide patterns derived from the WHO mortality database. Bull. World Health Organ 2008;86(9):726–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Canetto SS, Sakinofsky I. The gender paradox in suicide. Suicide Life. Threat. Behav 1998;28(1):1–23. [PubMed] [Google Scholar]
- 51.Siegel M, Rothman EF. Firearm ownership and suicide rates among US men and women, 1981-2013. Am. J. Public Health 2016;106(7):1316–1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Matthay EC, Galin J, Ahern J. Changing patterns in rates and means of suicide in California, 2005 to 2013. Am. J. Public Health 2017;107(3):427–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.California Department of Public Health. EPICenter: California Injury Data Online. 2015. Accessed from http://epicenter.cdph.ca.gov/Default.aspx on March 7, 2020.
- 54.Betz ME, Wintersteen M, Boudreaux ED, et al. Reducing suicide risk: Challenges and opportunities in the emergency department. Ann. Emerg. Med 2016;68(6):758–765. [DOI] [PubMed] [Google Scholar]
- 55.Henson KE, Brock R, Charnock J, et al. Risk of suicide after cancer diagnosis in England. JAMA Psychiatry. 2019;76(1):51–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ilgen MA, Zivin K, McCammon RJ, et al. Mental illness, previous suicidality, and access to guns in the United States. Psychiatr. Serv 2008;59(2):198–200. [DOI] [PubMed] [Google Scholar]
- 57.Kaplan MS, Geling O. Sociodemographic and geographic patterns of firearm suicide in the United States, 1989-1993. Heal. Place 1999;5(2):179–185. [DOI] [PubMed] [Google Scholar]
- 58.Betz ME, Wintemute GJ. Physician counseling on firearm safety: A new kind of cultural competence. JAMA. 2015;314(5):449–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Walters TE, Wick K, Tan G, et al. Psychological distress and suicidal ideation in patients with atrial fibrillation: Prevalence and response to management strategy. J. Am. Heart Assoc 2018;7(18):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Walker J, Waters RA, Murray G, et al. Better off dead: Suicidal thoughts in cancer patients. J. Clin. Oncol 2008;26(29):4725–4730. [DOI] [PubMed] [Google Scholar]
- 61.Pallin R, Charbonneau A, Wintemute GJ, et al. California public opinion on health professionals talking with patients about firearms. Health Aff. 2019;10(10):1744–1751. [DOI] [PubMed] [Google Scholar]
- 62.Price JH, Thompson A, Khubchandani J, et al. Perceived roles of emergency department physicians regarding anticipatory guidance on firearm safety. J. Emerg. Med 2013;44(5):1007–1016. [DOI] [PubMed] [Google Scholar]
- 63.Weinberger SE, Lawrence HC, Henley DE, et al. Legislative interference with the patient-physician relationship. N. Engl. J. Med 2012;367(16):1557–1559. [DOI] [PubMed] [Google Scholar]
- 64.Simon GE, Johnson E, Lawrence JM, et al. Predicting suicide attempts and suicide deaths following outpatient visits using electronic health records. Am. J. Psychiatry 2018;175:951–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gradus JL, Rosellini AJ, Horváth-Puhó E, et al. Prediction of sex-specific suicide risk using machine learning and single-payer health care registry data from Denmark. JAMA Psychiatry. 2019;02118:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rockett IRH, Hobbs G, De Leo D, et al. Suicide and unintentional poisoning mortality trends in the United States, 1987-2006: two unrelated phenomena? BMC Public Health. 2010;10(1):705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gray D, Coon H, McGlade E, et al. Comparative analysis of suicide, accidental, and undetermined cause of death classification. 2014;2(74):304–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Boudreaux ED, Camargo CA, Arias SA, et al. Improving suicide risk screening and detection in the emergency department. Am. J. Prev. Med 2016;50(4):445–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stanley B, Brown GK, Brenner LA, et al. Comparison of the Safety Planning Intervention with follow-up vs usual care of suicidal patients treated in the emergency department. JAMA Psychiatry. 2018;75(9):894–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


