Summary
Background
The emergence of SARS-CoV2 (COVID-19) had wide impacts to health and mortality and prompted unprecedented containment efforts. The full impact of the COVID-19 pandemic and resulting responses on mental health and substance abuse related mortality are unknown.
Methods
We obtained records for deaths from suicide, alcohol related liver failure, and overdose from the Michigan Department of Health and Human Services (MDHHS) for 2006 to 2020. We compared mortality within sex, age, marital, racial and urban/rural groups using basic statistical methods. We compared standardized mean daily mortality incidence before and after the onset of the pandemic using t-tests. We used an interrupted time series approach, using generalized additive Poisson regression models with smoothed components for time to assess differences in mortality trends before and after the onset of the pandemic within demographic groups.
Findings
There were 19,365 suicides, 8,790 deaths from alcohol related liver failure, and 21,778 fatal drug overdoses. Compared with 2019, suicides in 2020 declined by 17.6%, overdose mortality declined by 22.5%—while alcohol deaths increased by 12.4%. Crude comparisons suggested that there were significant declines in suicides for white people, people 18 to 65 and increases for rural decedents, overdoses increased for Black people, females and married/widowed people, and alcohol mortality increased for nearly all groups. ITS models, however, suggested increased suicide mortality for rural residents, significantly increased alcohol related mortality for people ≥65 and increased overdose mortality in men.
Interpretation
The onset of the pandemic was associated with mixed patterns of mortality between suicide, alcohol and overdose deaths. Patterns varied within demographic groups, suggesting that impacts varied among different groups, particularly racial and marital groups.
Funding
This work was supported by the United States National Institute of Environmental Health Sciences [K99/R00ES026198] and their Michigan Center on Lifestage Environmental Exposures and Disease [grant number P30ES017885]; and the Institute for Global Biological Change at the University of Michigan.
Keywords: Suicide, Self-harm, Overdose, Alcohol, Substance abuse, Mortality, COVID-19, Time series
Research in context.
Evidence before this study
Before starting this study, we searched PubMed, Web of Science and Scopus for papers published in English using the search terms ((COVID-19) OR (SARS-COV2) OR (coronavirus)) AND ((suicide) OR (overdose) OR (liver failure) OR (substance abuse) OR (self harm) OR (mental health)) AND (time series). After further analysis we resulted in 11 possible studies examining mortality patterns before and after the onset of the COVID-19 pandemic. Most published articles at that time speculated on possible patterns of mortality based on patterns observed in previous crises. Using time series data, only two studies indicated changes in patterns of suicide, overdose and alcohol related liver failure mortality following the onset of the pandemic. These studies were from Japan and Maryland. We were unable to find any studies on mental health and substance abuse mortality patterns in Michigan. However, the authors previously published research showing a decline in emergency admissions for self-harm and suicide attempts following the onset of the pandemic.
Added value of this study
To our knowledge this is the first study to use state mortality records to systematically assess changes in multiple types of mental health and substance abuse mortality after the onset of the COVID-19 pandemic in the United States. The results of this study suggest that patterns of suicide, overdose and alcohol related liver failure all followed different trajectories following the beginning of the pandemic. We have also demonstrated that patterns differed by age groups, race and urban/rural location of residence.
Implications of all the available evidence
The rapid increase in deaths from overdose and alcohol related liver failure, the decline in suicide mortality and the unique patterns of change among demographic groups imply that the COVID-19 pandemic had wide ranging psychiatric impacts that differed from previous economic crises.
Alt-text: Unlabelled box
Introduction
In the United States SARS-CoV2 (COVID-19) had wide ranging impacts on public health that may have affected different groups of people in disparate ways. After the emergence of COVID-19 many states and localities implemented expansive stay at home orders and distancing recommendations. While these measures may have reduced case incidence, hospitalization, and mortality1 there were concerns that disruptions in employment, economic uncertainty, changing household roles, and physical isolation would influence suicide and mental health related mortality. For example, models predicted that pandemic-related economic pressures and isolation would increase the incidence of suicide worldwide.2 Mental health professionals also worried that the pandemic would have an impact on opioid abuse and access to treatment.2, 3, 4, 5 Social distancing measures have been shown to have reduced COVID-19 incidence and mortality in other regions.6 However, the effects of the COVID-19 pandemic on mental health are not yet fully understood—and its effects on the mental health of demographic and racial sub-populations are also unknown.
Studies have shown that societal and economic shocks can impact mental health related mortality. Patterns of suicide mortality increased in 2009 following the Great Recession of 2008.7 County level unemployment and rural economic deprivation have been associated with risks for alcohol related mortality8, 9, 10—internet searches for information on problem drinking rose during the Great Recession.11 Chronic unemployment has also been associated with a higher risk of overdose death.12, 13, 14 Depressed housing prices during the Great Recession have been associated with increased incidence of overdose.15 Suicide and overdose have a common causality—both are thought to be influenced by labor insecurities and shocks similar to those that resulted from COVID-19 pandemic.16
Previous studies have shown racial and demographic disparities in mental health related deaths occurring in the wake of economic and societal disruptions. Typically, rates of suicide and premature death from alcohol related liver failure are lower in Black and Hispanic communities than in White communities in the U.S.17,18 However, the foreclosure crisis of the Great Recession was a substantial risk factor for depression and thoughts of suicide for African Americans.19 In recent years, suicide rates have been rising for Black and Asian American populations—despite declines for other groups.17,18 Similarly, opioid overdoses have been increasing for Black and Hispanic Americans faster than other groups since the Great Recession.20 The impacts of unemployment on suicide differ across age groups.21 Increased alcohol abuse was linked with suicides in men following the Great Recession,22 and suicides and alcohol abuse during that time were found to vary along gender, racial, and socioeconomic lines.23
This study aims to advance our understanding of what impact the COVID- 19 pandemic has had on mental health related mortality using Michigan death records from 2006 through 2020. Time series methods test whether temporal trends in suicide, alcohol related liver failure, and overdoses differed between the times before and after the emergence of the COVID-19 pandemic. This research tests three main hypotheses: (1) that patterns of mortality from mental health related causes would change after the onset of the pandemic, (2) that changes in mental health related mortality would express unique patterns by cause of death, and (3) that outcomes would differ by racial and demographic groups. Identifying disparities in mental health related mortality due to the COVID-19 pandemic and the subsequent response will help inform public health strategies that can proactively target specific groups.
Methods
Mortality data
The Michigan Department of Health and Human Services (MDHHS) records information on all deaths which occur within state borders. Records include information such as sex, age, race/ethnic group, and marital status. MDHHS lists the residential address of the decedent, even for those whose primary residence is outside the state of Michigan. This study focused on three major mental health related causes of death as recorded in Michigan death records: suicide, drug overdoses, and alcohol related liver failure. This study was approved by the Institutional Review Boards of the University of Michigan and the MDHHS.
Statistical methods
The announcement of confirmed COVID-19 cases and the declaration of a State of Emergency by Michigan's governor on March 13, 202024 was considered the onset of the COVID-19 pandemic in Michigan for the purposes of this study. A dichotomous variable was created to separate the data into groups of people who died before and after the announcement of the declaration. We compared demographic indicators including age, gender, race, and marital status before and after the announcement through descriptive and analytic methods.
Since the experience of the stay-at-home orders and the COVID-19 pandemic likely differed between urban and rural areas of the state, we tested for differences in counts before and after the stay-at-home order between urban and rural areas. We used the geolocated address to locate each residence within the Urban/Rural designation from the U.S. Census.25 All urbanized areas and urbanized clusters were considered “urban”, and all other areas were considered “rural” for this research.
For continuous variables, we performed standard t-tests for differences in means. We checked for normality and, where appropriate, standardized continuous variables. We performed Chi-Square tests for categorical variables.
We tested whether temporal trends of causes of death—varied within age, sex, race, or urban rural groups—differed before and after the onset of the pandemic in Michigan. We aggregated the data set to daily counts of suicide deaths to allow us to explore temporal patterns in suicide mortality. To compare mortality from suicide, liver failure, and overdose by year between 2020 and previous years, cumulative yearly counts were plotted against one another. To assess changes in mortality patterns within specific race, sex, age, and urban and rural groups, we compared mean standardized mortality counts (per 100,000 people) before and after COVID-19 through t-tests of means. A Bonferroni correction was applied to all p-values to account for the numerous independent statistical tests being performed.
We formally tested temporal patterns using an interrupted time series (ITS) approach. An interrupted time series (ITS) study uses a time series of a particular outcome of interest to establish an underlying trend, which is then ‘interrupted’ by an event or intervention at a known point in time.26 ITS has been applied to a number of health and policy studies.27, 28, 29 For this research we used a generalized additive Poisson regression model including a smoothed (loess) predictor for time and a predictor representing the time periods before and after the announcement of the stay-at-home order. We compared trends before and after the onset of the COVID-19 crisis. To test whether there were differences in mortality from suicide, liver failure, and overdoses within demographic groups before and after the onset of the COVID-19 pandemic, we included variables for race, sex, age category, and urban and rural groups—and included an interaction term with the before/after term for the onset of the pandemic for each. All analyses were conducted using R version 4.1.1.30
Role of the funding source
Data from the MDHHS was purchased using funds from a grant from the United States National Institute of Environmental Health Sciences [K99/R00ES026198]. Salary support for PSL was provided from the Institute for Global Biological Change (IGBC) at the University of Michigan. RSB was supported by the the United States National Institute of Environmental Health Sciences Michigan Center on Lifestage Environmental Exposures and Disease [grant number NIEHS P30ES017885].
Results
Between 2006-01-01 and 2020-12-21 there were 19,365 deaths from suicide, 8,790 deaths from alcohol related liver failure, and 21,778 deaths from drug overdoses—out of 1,399,714 total deaths within the State of Michigan. The gender distribution of mental health related mortality for each cause was heavily skewed towards men. Nearly 80% of suicides were, 70% of alcohol related liver failures deaths, and 65% of overdose deaths were men. The mean age for suicide was 46 years, 55 years for alcohol related deaths, and 42 years for overdose deaths. Suicide was the most common mental health related cause of death in children. The distribution of marital groups was similar between suicide and alcohol deaths, but more than 42% of deaths from overdoses were divorced. The distributions of racial groups within cause of death varied. While Black decedents were 14% of all deaths, roughly reflecting overall demographics in Michigan, only 8% of suicides and only 10% of alcohol related deaths were of Black people. However, more than 18% of deaths from overdoses were in Black decedents. While 25% of decedents had residences in rural areas, 30% of suicide deaths and 18% of overdose deaths were of rural residents (See Table 1). The mean yearly number of deaths was 93,313 people with an overall increasing trend of mortality in Michigan. The yearly average for each was 1,291 deaths from suicide, 586 deaths from alcohol related liver failure and 1,451 overdose deaths.
Table 1.
Sample demographics for all deaths and within each cause of death: suicide, alcohol related liver failure and overdose.
| All deaths | Suicide | Alcohol | Overdose | p | |
|---|---|---|---|---|---|
| N = 1399714 | N = 19365 | N = 8790 | N = 21778 | ||
| Sex: | <0.001 * | ||||
| Male | 700476 (50.0%) | 15390 (79.5%) | 6098 (69.4%) | 14251 (65.4%) | |
| Female | 699198 (50.0%) | 3975 (20.5%) | 2692 (30.6%) | 7527 (34.6%) | |
| Age at death (mean) | 72.9 (18.4) | 46.3 (18.3) | 55.3 (10.9) | 42.9 (13.5) | <0.001 * |
| Age categories: | <0.001 * | ||||
| 0–17 | 25298 (1.81%) | 984 (5.08%) | 1 (0.01%) | 254 (1.17%) | |
| 18–65 | 370906 (26.5%) | 15435 (79.7%) | 7385 (84.0%) | 20596 (94.6%) | |
| Over 65 | 1003478 (71.7%) | 2946 (15.2%) | 1404 (16.0%) | 928 (4.26%) | |
| Marital status: | <0.001 * | ||||
| Never married | 312826 (22.4%) | 6594 (34.2%) | 2287 (26.2%) | 6348 (29.4%) | |
| Married/legally separated | 495523 (35.5%) | 4324 (22.4%) | 1842 (21.1%) | 2681 (12.4%) | |
| Divorced | 195530 (14.0%) | 5784 (30.0%) | 2725 (31.2%) | 9255 (42.9%) | |
| Widowed | 390668 (28.0%) | 2594 (13.4%) | 1885 (21.6%) | 3312 (15.3%) | |
| Racial group: | <0.001 * | ||||
| White | 1175400 (84.0%) | 17219 (88.9%) | 7533 (85.7%) | 17155 (78.8%) | |
| Black or African American | 196023 (14.0%) | 1527 (7.89%) | 909 (10.3%) | 3947 (18.1%) | |
| Other | 17483 (1.25%) | 357 (1.84%) | 195 (2.22%) | 363 (1.67%) | |
| Am. Indian/Alaskan Native | 7826 (0.56%) | 171 (0.88%) | 151 (1.72%) | 296 (1.36%) | |
| Asian | 2982 (0.21%) | 91 (0.47%) | 2 (0.02%) | 17 (0.08%) | |
| Urban/Rural: | <0.001 * | ||||
| Rural | 341598 (25.0%) | 5601 (29.3%) | 2298 (26.9%) | 3872 (18.1%) | |
| Urban | 1026634 (75.0%) | 13502 (70.7%) | 6256 (73.1%) | 17528 (81.9%) |
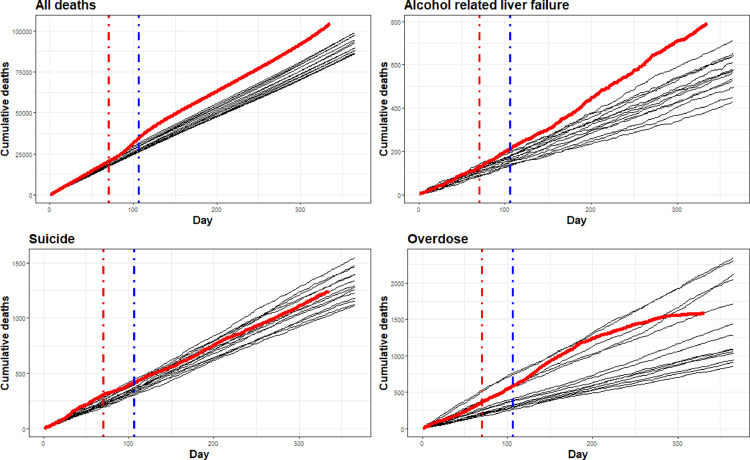
In Figure 1 we present yearly patterns of cumulative mortality (from Jan 1 to Dec 31) for all deaths, suicide, alcohol related liver failure and overdoses. Cumulative patterns can provide insight into how temporal mortality trends in 2020 compared with previous years. Overall deaths rose following the onset of the pandemic, reflecting the sudden rise in mortality during the first wave of the pandemic. The period following the onset of the pandemic had higher levels of mortality than any previous year examined. Cumulative mortality from suicide was high compared to previous years until the onset of the pandemic when it began to decline. Alcohol related deaths started high, but then increased rapidly following the onset of the pandemic; cumulative alcohol related deaths were higher than any year previous. The pattern of overdose related deaths began on a somewhat average trajectory compared the previous years, but then followed an atypical pattern that rose several weeks after the onset of the pandemic and slowed starting in mid-summer.
Figure 1.
Cumulative mortality for all days in all years, 2006–2020. Bold, red line represents cumulative mortality in 2020. Cumulative mortality plots presented for mortality from all causes: suicide, alcohol related liver failure, and drug overdose. Red vertical line represents the date of the announcement of the State of Emergency order (March 13, 2020) and the beginning of the pandemic in Michigan. Blue line represents the date of the first peak of COVID-19 deaths in Michigan (April 16, 2020).
For suicides and deaths from alcohol related liver failure, there was no evidence to suggest that the distribution of genders changed after the onset of the pandemic. As a percentage, however, there were more deaths in males from overdose after the onset of the pandemic than before (After: 69.4% vs. Before: 65.2%, p = 0.003). There was little evidence to suggest that the distribution of age, both as a continuous and a categorized data variable, changed for alcohol related mortality and overdose deaths after the start of the pandemic. However, there was weak evidence to suggest that the mean age of suicide victims rose after the onset of the pandemic compared with before (After: 47.8 years vs. Before: 46.5 years, p = 0.053). The categorized age variable suggested that, for suicides, the share of all age groups made up of people over 65 rose after the start of the pandemic (After: 18.9% vs. Before: 15.4%, p = 0.017).
The distribution of deaths within marital groups changed significantly (at the p ≤ 0.0001 level) for all three causes of death. Specifically, for all three causes of death, the share represented by married persons declined significantly from before to after the onset of the pandemic, from 23.3% to 6.07% for suicides, from 22.1% to 7.1% for alcohol related liver failure, and from 12.9% to 4.34% for overdoses. The share of deaths in divorced people rose for suicides (29.3% to 40.4%) and overdoses (42.1% to 57.1%). The share of deaths among widowers rose for all three causes of death, from 13.3% to 19.6% for suicides, from 20.6% to 34.7% for alcohol related liver failure and from 15% to 21.9% for overdoses.
After exploratory analyses, we decided to keep only Black and White decedents in the data set. Asians, American Indian/Alaskan Native people and “Other” comprised less than 4% of mental health related deaths over the study period in Michigan and the numbers of deaths following the on-set of the pandemic were too small to allow reliable statistical comparisons. Using only the two racial groups, we found that the percentage of suicide and overdose decedents who were Black rose after the onset of the pandemic. Black decedents made up 8.05% of suicide deaths before and 10.1% of suicide deaths after the onset of the pandemic (p = 0.036). For overdose, Black decedents made up 18.3% before and 25.2% of suicide deaths after the onset of the pandemic (p ≤ 0.001). The distribution of racial groups for alcohol related liver failure was unchanged (10.7% to 11.1% (p = 0.791)). For urban and rural decedents, we only found significant changes for suicide mortality. The share of deaths made up by rural residents rose from 29.4% to 32.8% (p = 0.034). See Table 2 for full results.
Table 2.
Comparison of the distribution of sex, age, marital status, race and urban/rural groups before and after the onset of the COVID-19 pandemic. p values for categorical variables are based on Chi-square tests. p values for the single continuous variable of age are based on a Student's T-test of means.
| Suicide |
Alcoholic |
Overdose |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Before | After | p | Before | After | p | Before | After | p | |
| N = 18458 | N = 907 | N = 8117 | N = 673 | N = 20561 | N = 1217 | ||||
| Sex: | 0.160 | 0.753 | 0.003 ** | ||||||
| Male | 14652 (79.4%) | 738 (81.4%) | 5627 (69.3%) | 471 (70.0%) | 13406 (65.2%) | 845 (69.4%) | |||
| Female | 3806 (20.6%) | 169 (18.6%) | 2490 (30.7%) | 202 (30.0%) | 7155 (34.8%) | 372 (30.6%) | |||
| Age at death (mean) | 46.5 (18.3) | 47.8 (19.4) | 0.053 | 55.3 (10.8) | 55.5 (12.3) | 0.774 | 43.0 (13.6) | 43.5 (13.5) | 0.191 |
| Age categories: | 0.017 * | 0.076 | 0.073 | ||||||
| 0–17 | 884 (4.94%) | 36 (4.17%) | 1 (0.01%) | 0 (0.00%) | 237 (1.19%) | 6 (0.51%) | |||
| 18–65 | 14244 (79.7%) | 664 (76.9%) | 6561 (84.1%) | 516 (80.6%) | 18842 (94.5%) | 1103 (94.6%) | |||
| Over 65 | 2755 (15.4%) | 163 (18.9%) | 1240 (15.9%) | 124 (19.4%) | 857 (4.30%) | 57 (4.89%) | |||
| Marital status: | <0.001 *** | <0.001 *** | <0.001 *** | ||||||
| Never married | 6087 (34.1%) | 291 (34.0%) | 2012 (25.9%) | 183 (28.9%) | 5936 (30.0%) | 192 (16.7%) | |||
| Married or legally separated | 4147 (23.3%) | 52 (6.07%) | 1714 (22.1%) | 45 (7.10%) | 2548 (12.9%) | 50 (4.34%) | |||
| Divorced | 5225 (29.3%) | 346 (40.4%) | 2436 (31.4%) | 186 (29.3%) | 8331 (42.1%) | 658 (57.1%) | |||
| Widowed | 2370 (13.3%) | 168 (19.6%) | 1600 (20.6%) | 220 (34.7%) | 2958 (15.0%) | 253 (21.9%) | |||
| Racial group: | 0.036 * | 0.791 | <0.001 *** | ||||||
| White | 16443 (91.9%) | 776 (89.9%) | 6964 (89.3%) | 569 (88.9%) | 16283 (81.7%) | 872 (74.8%) | |||
| Black/African American | 1440 (8.05%) | 87 (10.1%) | 838 (10.7%) | 71 (11.1%) | 3653 (18.3%) | 294 (25.2%) | |||
| Urban/Rural: | 0.034 * | 0.552 | 0.139 | ||||||
| Rural | 5177 (29.4%) | 282 (32.8%) | 2015 (26.6%) | 177 (27.8%) | 3544 (18.1%) | 187 (16.3%) | |||
| Urban | 12460 (70.6%) | 578 (67.2%) | 5556 (73.4%) | 460 (72.2%) | 16046 (81.9%) | 959 (83.7%) | |||
Mean standardized daily mortality pre and post COVID-19
We compared the mean number of daily events per 100,000 for all three outcomes within each group of interest. This provides insight into whether the number of daily events increased or decreased following the onset of the pandemic within each group independent of all other groups. Daily suicide deaths declined for both males (-20.64% (p = 0.04)) and females (-9.32% (p = 0.01)). Daily suicide mortality incidence for White people declined significantly, falling from 0.043 deaths per 100,000 to 0.038 deaths per 100,000, a decline of 15% (p ≤ 0.001). For Black people there was a non-significant increase of 10%. Suicides among married people increased, from 0.109/100,000 deaths per day to 0.124/100,00 deaths per days, an increase of 14%. There was no change in the rural suicides, but a significant decrease in urban suicides of 14.21% (p ≤ 0.001).
Deaths from alcohol related liver failure significantly increased within nearly all groups. Deaths among men increased by 36% (p ≤ 0.001) and by 50% among women (p ≤ 0.001). Deaths among White people increased by 43% (p ≤ 0.001) and by 56% among Black people (p ≤ 0.001). Increases of 40% (p ≤ 0.001) and 78% (p ≤ 0.001) were seen in 18–65 year-olds and over 65 s, respectively. Rural deaths from alcohol related liver failure increased by 85% while urban deaths increased by 47% (p ≤ 0.001). The only decrease in the number of alcohol related deaths was in people who had never married (-38%; p ≤ 0.001). Married people, divorcees and widowed people all rose by 48% (p ≤ 0.001), 52% (p ≤ 0.001), and 96% (p ≤ 0.001), respectively. The standardized mean daily incidence of alcohol related deaths for widowed people rose from 0.073 per 100,000 to 0.143 per 100,000 people, a change of 96.1% (p ≤ 0.001).
For overdose, significant changes were only seen in race and marital groups. The mean daily incidence of overdose mortality for White people dropped 11.86%, from 0.046/100,000 before the pandemic to 0.041/100,000 after. Similarly, while deaths from overdose fell 36% (p ≤ 0.001) for never married and by 45% (p = 0.02) for divorced people, deaths rose by 19% for married (p ≤ 0.001). The change (19%) in widowed people was non-significant (p = 0.09). See Table 3 for full results.
Table 3.
Comparison of standardized mean daily incidence per 100,000 people (95% confidence intervals) of suicide, alcohol related liver failure, and overdose by race (black vs. white), sex, age groups, and urban vs. rural residence pre-COVID-19 (January 2006 – March 2020) and from the onset of the pandemic.
| Pre COVID-19 | COVID-19 | p | sig | direction | ||
|---|---|---|---|---|---|---|
| Suicide | ||||||
| 1 | Female | 0.016 (0.015, 0.017) | 0.012 (0.01, 0.014) | 0.01 | *** | ↓ (-9.32%) |
| 2 | Male | 0.06 (0.059, 0.061) | 0.055 (0.051, 0.059) | 0.04 | * | ↓ (-20.64%) |
| 3 | Age group 0–17 | 0.009 (0.008, 0.01) | 0.007 (0.005, 0.009) | 0.43 | ↓ (-21.92%) | |
| 4 | Age group 18–65 | 0.049 (0.048, 0.05) | 0.042 (0.039, 0.045) | 0.00 | *** | ↓ (-13.65%) |
| 5 | Age group Over 65 | 0.033 (0.032, 0.034) | 0.034 (0.029, 0.039) | 0.99 | ↑ (2.85%) | |
| 6 | Never married | 0.014 (0.013, 0.015) | 0.004 (0.003, 0.005) | 0.02 | *** | ↓ (-15.1%) |
| 7 | Married or legally separated | 0.109 (0.105, 0.113) | 0.124 (0.111, 0.137) | 0.00 | *** | ↑ (14.33%) |
| 8 | Divorced | 0.043 (0.042, 0.044) | 0.037 (0.033, 0.041) | 0.12 | ↓ (-69.84%) | |
| 9 | Widowed | 0.102 (0.097, 0.107) | 0.108 (0.093, 0.123) | 0.99 | ↑ (5.85%) | |
| 10 | White | 0.042 (0.041, 0.043) | 0.036 (0.033, 0.039) | 0.00 | *** | ↓ (-15.32%) |
| 11 | Black | 0.021 (0.02, 0.022) | 0.023 (0.018, 0.028) | 0.99 | ↑ (10.3%) | |
| 12 | Rural | 0.06 (0.058, 0.062) | 0.06 (0.053, 0.067) | 0.99 | ↓ (-0.05%) | |
| 13 | Urban | 0.032 (0.031, 0.033) | 0.027 (0.025, 0.029) | 0.00 | *** | ↓ (-14.21%) |
| Alcohol related liver failure | ||||||
| 1 | Female | 0.011 (0.011, 0.011) | 0.015 (0.013, 0.017) | 0.00 | *** | ↑ (50.67%) |
| 2 | Male | 0.023 (0.022, 0.024) | 0.035 (0.032, 0.038) | 0.00 | *** | ↑ (36.54%) |
| 3 | Age group 18–65 | 0.023 (0.022, 0.024) | 0.033 (0.03, 0.036) | 0.00 | *** | ↑ (40.71%) |
| 4 | Age group Over 65 | 0.015 (0.014, 0.016) | 0.027 (0.022, 0.032) | 0.00 | *** | ↑ (78.39%) |
| 5 | Never married | 0.006 (0.006, 0.006) | 0.004 (0.003, 0.005) | 0.00 | *** | ↓ (-38.22%) |
| 6 | Married or legally separated | 0.043 (0.041, 0.045) | 0.066 (0.057, 0.075) | 0.00 | *** | ↑ (48.51%) |
| 7 | Divorced | 0.016 (0.015, 0.017) | 0.023 (0.02, 0.026) | 0.00 | *** | ↑ (52.24%) |
| 8 | Widowed | 0.073 (0.069, 0.077) | 0.143 (0.124, 0.162) | 0.00 | *** | ↑ (96.51%) |
| 9 | White | 0.018 (0.017, 0.019) | 0.026 (0.024, 0.028) | 0.00 | *** | ↑ (43.47%) |
| 10 | Black | 0.012 (0.011, 0.013) | 0.019 (0.015, 0.023) | 0.00 | *** | ↑ (56.44%) |
| 11 | Rural | 0.024 (0.023, 0.025) | 0.038 (0.033, 0.043) | 0.00 | *** | ↑ (55.68%) |
| 12 | Urban | 0.014 (0.014, 0.014) | 0.022 (0.02, 0.024) | 0.00 | *** | ↑ (50.66%) |
| Overdose | ||||||
| 1 | Female | 0.028 (0.025, 0.031) | 0.032 (0.031, 0.033) | 0.11 | ↑ (2.58%) | |
| 2 | Male | 0.064 (0.058, 0.07) | 0.062 (0.061, 0.063) | 0.99 | ↓ (-12.43%) | |
| 3 | Age group 0–17 | 0.002 (0.002, 0.002) | 0.002 (0.001, 0.003) | 0.99 | ↑ (0.91%) | |
| 4 | Age group 18–65 | 0.073 (0.072, 0.074) | 0.07 (0.064, 0.076) | 0.99 | ↓ (-3.48%) | |
| 5 | Age group Over 65 | 0.012 (0.011, 0.013) | 0.013 (0.01, 0.016) | 0.99 | ↑ (11.03%) | |
| 6 | Never married | 0.01 (0.009, 0.011) | 0.005 (0.004, 0.006) | 0.00 | *** | ↓ (-35.97%) |
| 7 | Married or legally separated | 0.194 (0.188, 0.2) | 0.232 (0.209, 0.255) | 0.00 | *** | ↑ (19.41%) |
| 8 | Divorced | 0.041 (0.04, 0.042) | 0.026 (0.022, 0.03) | 0.02 | ** | ↓ (-45.56%) |
| 9 | Widowed | 0.142 (0.136, 0.148) | 0.169 (0.149, 0.189) | 0.09 | ↑ (19.44%) | |
| 10 | White | 0.046 (0.045, 0.047) | 0.041 (0.037, 0.045) | 0.04 | * | ↓ (-11.86%) |
| 11 | Black | 0.061 (0.058, 0.064) | 0.08 (0.069, 0.091) | 0.02 | ** | ↑ (30.47%) |
| 12 | Rural | 0.044 (0.042, 0.046) | 0.043 (0.037, 0.049) | 1.00 | ↓ (-0.62%) | |
| 13 | Urban | 0.046 (0.045, 0.047) | 0.045 (0.041, 0.049) | 1.00 | ↓ (-2.11%) | |
Interrupted time series models
We used generalized additive models including smoothed terms for time before and after the onset of the pandemic, creating models for each demographic group of three levels or less. For suicide, we found that the pandemic was associated with an overall decline in the daily number of suicides. We also found, however, that there were significant changes in the daily patterns of mortality for specific groups. Due to the relatively small numbers of child suicides in our data set, we used 18–65 years old decedents as a reference group. The log counts of daily suicide deaths in elderly people was significantly elevated after the onset of the pandemic compared with other groups. However, when accounting for the baseline decrease in the log counts of suicide, there was still a net decrease (log counts -0.37 + 0.18 = -0.19). However, when comparing urban and rural suicides, there is a significant and additional decrease in the log counts of suicide after the onset of the pandemic compared with before (-0.21; p = 0.43). No significant differences in the log counts of suicide between before and after the pandemic were found for Black vs. white, or among sex groups. See Table 4.
Table 4.
Results of generalized additive models of standardized daily counts (per 100,000) of suicide deaths by age group, race, sex, and urban/rural residence. Parameter estimates are given in differences in log counts.
| Sex | ||||||
| A. parametric coefficients | Estimate | Std. Error | t-value | p | sig. | |
| (Intercept) | -4.1496 | 0.0194 | -213.7685 | < 0.0001 | *** | |
| COVID-19 | -0.4247 | 0.5947 | -0.7142 | 0.4751 | ||
| Male | 1.3547 | 0.0216 | 62.5917 | < 0.0001 | *** | |
| COVID-19:Male | 0.1080 | 0.0829 | 1.3018 | 0.1930 | ||
| B. smooth terms | edf | Ref.df | F-value | p-value | sig. | |
| s(Date of death):Pre-COVID-19 | 2.9851 | 4.0000 | 15.6288 | < 0.0001 | *** | |
| s(Date of death):COVID-19 | 0.4242 | 4.0000 | 0.1842 | 0.1876 | ||
| Age group | ||||||
| A. parametric coefficients | Estimate | Std. Error | t-value | p | sig. | |
| (Intercept) | -3.0045 | 0.0157 | -191.0820 | < 0.0001 | *** | |
| COVID-19 | -0.7755 | 1.1872 | -0.6532 | 0.513 | ||
| Age over 0–17 | -1.6399 | 0.0385 | -42.6512 | < 0.0001 | *** | |
| Age over 65 | -0.3796 | 0.0243 | -15.6126 | < 0.0001 | *** | |
| COVID-19:Age over 0–17 | -0.1880 | 0.1563 | -1.2028 | 0.230 | ||
| COVID-19:Age over 65 | 0.1852 | 0.0871 | 2.1251 | 0.034 | ** | |
| B. smooth terms | edf | Ref.df | F-value | p-value | sig. | |
| s(Date of death):Pre-COVID-19 | 3.0282 | 4.0000 | 16.7425 | < 0.0001 | *** | |
| s(Date of death):COVID-19 | 0.6659 | 4.0000 | 0.4984 | 0.0836 | ||
| Black vs. white | ||||||
| A. parametric coefficients | Estimate | Std. Error | t-value | p | sig. | |
| (Intercept) | -3.1550 | 0.0836 | -37.7467 | < 0.0001 | *** | |
| COVID-19 | -0.1241 | 0.3167 | -0.3920 | 0.695 | ||
| Black (vs. white) | -0.7047 | 0.1453 | -4.8483 | < 0.0001 | *** | |
| COVID-19:Black (vs. white) | 0.2475 | 0.5171 | 0.4788 | 0.6321 | ||
| B. smooth terms | edf | Ref.df | F-value | p-value | sig. | |
| s(Date of death):Pre-COVID-19 | 0.0000 | 4.0000 | 0.0000 | 0.4313 | ||
| s(Date of death):COVID-19 | 0.0000 | 4.0000 | 0.0000 | 0.6884 | ||
| Urban vs. rural residence | ||||||
| A. parametric coefficients | Estimate | Std. Error | t-value | p | sig. | |
| (Intercept) | -3.0057 | 0.0194 | -155.1202 | < 0.0001 | *** | |
| COVID-19 | -0.5629 | 1.3045 | -0.4315 | 0.6661 | ||
| Urban | -0.3218 | 0.0295 | -10.9115 | < 0.0001 | *** | |
| COVID-19:Urban | -0.123147 | 0.1064 | -2.0176 | 0.0437 | * | |
| B. smooth terms | edf | Ref.df | F-value | p | sig. | |
| s(Date of death):Pre-COVID-19 | 2.5583 | 4.0000 | 6.7215 | < 0.0001 | *** | |
| s(Date of death):COVID-19 | 0.6025 | 4.0000 | 0.3787 | 0.1128 | ||
We removed children from the analysis as there was only a single death from liver failure in the data set in a person under 18 years of age. The interaction term for demographic variables and the onset of the pandemic was only significant for people over the age of 65 compared with people 18–65. There was a significant increase in the log counts of suicide incidence following the onset of the pandemic (0.23; p = 0.018) compared with people 18–65. Weak evidence (at the p = 0.10 level) suggests that log counts of urban suicide incidence declined for urban residents compared with rural residents (log counts -0.23 p = 0.075). See Table 5.
Table 5.
Results of generalized additive models of standardized daily counts (per 100,000) of deaths from alcohol related liver failure by age group, race, sex, and urban/rural residence. Parameter estimates are given in differences in log counts.
| Sex | |||||
| A. parametric coefficients | Estimate | Std. Error | t-value | p | sig. |
| (Intercept) | -4.5343 | 0.0238 | -190.9029 | < 0.0001 | *** |
| COVID-19 | 0.2613 | 0.2784 | 0.9384 | 0.348 | |
| Male | 0.7762 | 0.0285 | 27.2179 | < 0.0001 | *** |
| COVID-19:Male | 0.0984 | 0.0888 | 1.1079 | 0.2679 | |
| B. smooth terms | edf | Ref.df | F-value | p | sig. |
| s(Date of death):Pre-COVID-19 | 2.6422 | 4.0000 | 8.3709 | < 0.0001 | *** |
| s(Date of death):COVID-19 | 0.0724 | 4.0000 | 0.0195 | 0.299 | |
| Age group | |||||
| A. parametric coefficients | Estimate | Std. Error | t-value | p | sig. |
| (Intercept) | -3.7563 | 0.0218 | -172.2304 | < 0.0001 | *** |
| COVID-19 | 0.0651 | 0.7656 | 0.0850 | 0.932 | |
| Age Over 65 | -0.4108 | 0.0341 | -12.0565 | < 0.0001 | *** |
| COVID-19:Age Over 65 | 0.2379 | 0.1005 | 2.3682 | 0.018 | ** |
| B. smooth terms | edf | Ref.df | F-value | p | sig. |
| s(Date of death):Pre-COVID-19 | 2.9502 | 4.0000 | 13.2861 | < 0.0001 | *** |
| s(Date of death):COVID-19 | 0.3118 | 4.0000 | 0.1132 | 0.228 | |
| Black vs. white | |||||
| A. parametric coefficients | Estimate | Std. Error | t-value | p | sig. |
| (Intercept) | -4.0009 | 0.1276 | -31.3582 | < 0.0001 | *** |
| COVID-19 | 0.3610 | 0.3943 | 0.9156 | 0.360 | |
| Black (vs. white) | -0.3971 | 0.2013 | -1.9731 | 0.048 | * |
| COVID-19:Black (vs. white) | 0.0865 | 0.6147 | 0.1408 | 0.888 | |
| B. smooth terms | edf | Ref.df | F-value | p | sig. |
| s(Date of death):Pre-COVID-19 | 0.0000 | 4.0000 | 0.0000 | 0.522 | |
| s(Date of death):COVID-19 | 0.0000 | 4.0000 | 0.0000 | 0.745 | |
| Urban vs. rural residence | |||||
| A. parametric coefficients | Estimate | Std. Error | t-value | p | sig. |
| (Intercept) | -3.9056 | 0.0301 | -129.7212 | < 0.0001 | *** |
| COVID-19 | 0.6166 | 0.0834 | 7.3940 | < 0.0001 | *** |
| Urban | -0.2484 | 0.0447 | -5.5598 | < 0.0001 | *** |
| COVID-19:Urban | -0.2331 | 0.1311 | -1.7780 | 0.075 | |
| B. smooth terms | edf | Ref.df | F-value | p | sig. |
| s(Date of death):Pre-COVID-19 | 3.3870 | 4.0000 | 16.1938 | < 0.0001 | *** |
| s(Date of death):COVID-19 | 0.104001 | 4.0000 | 0.0000 | 0.628 |
Models did not indicate a significant change in standardized daily counts of overdose mortality following the onset of the pandemic in Michigan for age groups, race, or for urban and rural residence. However, there was evidence to suggest that incidence in males grew more after the beginning of COVID-19 than in females (log counts 0.17, p < 0.001). See Table 6.
Table 6.
Results of generalized additive models of standardized daily counts (per 100,000) of overdose deaths by age group, race, sex, and urban/rural residence. Parameter estimates are given in differences in log counts.
| Sex | |||||
| A. parametric coefficients | Estimate | Std. error | t-value | p-value | sig. |
| (Intercept) | -3,474 | 0,0145 | -240,035 | <0.0001 | *** |
| COVID-19 | -297,129 | 753,5728 | -0,3943 | 0.693 | |
| Male | 0,6638 | 0,0174 | 38,1814 | <0.0001 | *** |
| COVID-19:Male | 0,1769 | 0,0669 | 2,6463 | 0.008 | * |
| B. smooth terms | edf | Ref.df | F-value | p-value | sig. |
| Date of death::Pre-COVID-19 | 3,935 | 4 | 278,5958 | <0.0001 | *** |
| Date of death: Covid-19 | 2,1426 | 4 | 67,7791 | <0.0001 | *** |
| Age group | |||||
| A. parametric coefficients | Estimate | Std. error | t-value | p-value | sig. |
| (Intercept) | -2,6489 | 0,0142 | -186,535 | <0.0001 | *** |
| COVID-19 | -510,81 | 492,283 | -1,0376 | 0.299 | |
| Age 0–17 | -3,5346 | 0,0802 | -44,0817 | <0.0001 | *** |
| Age Over 65 | -1,8033 | 0,0358 | -50,4246 | <0.0001 | *** |
| COVID-19:Age 0–17 | -0,0964 | 0,3222 | -0,2991 | 0.764 | |
| COVID-19:Age Over 65 | 0,0803 | 0,1308 | 0,6137 | 0.539 | |
| B. smooth terms | edf | Ref.df | F-value | p-value | sig. |
| Date of death::Pre-COVID-19 | 3,8528 | 4 | 131,5889 | <0.0001 | *** |
| Date of death: Covid-19 | 2,02 | 4 | 28,3441 | <0.0001 | *** |
| Black vs. white | |||||
| A. parametric coefficients | Estimate | Std. error | t-value | p-value | sig. |
| (Intercept) | -3,1008 | 0,0819 | -37,8434 | <0.0001 | *** |
| COVID-19 | 4,476 | 7,6101 | 0,5882 | 0.556 | |
| Black (vs. white) | 0,2759 | 0,1062 | 2,5991 | 0.009 | ** |
| COVID-19:Black (vs. white) | 0,3827 | 0,3872 | 0,9885 | 0.322 | |
| B. smooth terms | edf | Ref.df | F-value | p-value | sig. |
| Date of death::Pre-COVID-19 | 2,8497 | 4 | 41,6431 | <0.0001 | *** |
| Date of death: Covid-19 | 0,8068 | 4 | 4,1652 | 0.023 | ** |
| Urban vs. Rural residence | |||||
| A. parametric coefficients | Estimate | Std. error | t-value | p-value | sig. |
| (Intercept) | -3,5283 | 0,0255 | -138,62 | <0.0001 | *** |
| COVID-19 | 3,4816 | 7,784 | 0,4473 | 0.654 | |
| Urban | 0,4513 | 0,0318 | 14,1886 | <0.0001 | *** |
| COVID-19:Urban | -0,1127 | 0,1166 | -0,9667 | 0.333 | |
| B. smooth terms | edf | Ref.df | F-value | p-value | sig. |
| Date of death::Pre-COVID-19 | 3,7682 | 4 | 65,3174 | <0.0001 | *** |
| Date of death: COVID-19 | 0,9829 | 4 | 10,5962 | <0.0001 | *** |
Discussion
Using 15 years of mortality data from the State of Michigan, this study specified the impact of the COVID-19 pandemic on temporal trends of mental health associated mortality including suicide, alcohol related liver failure, and drug overdoses. We found significant support for our first hypothesis—that patterns of mortality from mental health related causes would change after the onset of the pandemic. Suicide rates changed and —despite predictions to the contrary— began to decline soon after the onset of the pandemic in Michigan and remained low throughout the year. Alcohol-related liver failure and drug overdose deaths increased, although their temporal patterns were distinct. We found significant differences between age groups, race groups, and sex groups as well as between urban and rural residents for the three types of mental health-related mortality. For example, crude analyses suggested increases in suicide mortality for married people and rural residents—but significant declines for White decedents, among both sexes, people 18–65 years of age, and never married people. Standardized mortality incidence from alcohol related causes for all groups was significantly higher for all groups. Finally, overdose mortality was significantly higher for Black people, females, married and widowed people—but it was significantly lower for White people and unmarried people.
In our study we found evidence to suggest that trends of some types of mental health mortality were influenced by the COVID-19 pandemic. The pattern of suicides did not increase compared to previous years—but the incidence of alcohol related mortality rose to its highest level in 15 years. Trends of overdose mortality followed an atypical trend. These results suggest that the impacts of the pandemic were very different from those of typical economic shocks such as the Great Recession.31 These unique patterns deserve special attention.
The mixed results of mortality among demographic groups might reflect varied economic experiences of the pandemic. Service industries—often staffed by ethnic minorities in the US—were some of the first and hardest hit occupations during the COVID-19 crisis due to social distancing guidelines and a decreased capacity for remote or virtual alternatives.32 Wage laborers often had to stop work entirely, and the most serious economic impacts might have been buffered by unemployment insurance such as during the Great Recession.33 In the case of “essential workers”—such as those in agricultural and meat processing occupations—migrants or minorities might have been forced to work under conditions that put them at risk without access to sufficient worker protections.34 Future research might examine how COVID-19 risks to essential workers influenced mental health and substance abuse risks during the pandemic.
The temporal patterns in suicide were consistent with results from other state, national, and international studies and reports which suggested that there was no increase in suicide incidence following the onset of the pandemic.35, 36, 37, 38, 39 Supporting our third hypothesis about mental health outcomes differing among racial groups, crude analyses in our study suggested a decline in suicides among White people, which was consistent with results from Maryland and Illinois.35,36 The decline in suicides, however, could be temporary; one study from Japan found that the trend in suicides rebounded to pre-pandemic levels within months.38
A number of factors may have contributed to lower rates of suicide during the COVID-19 pandemic. First, actions taken on behalf of governmental and local agencies may have attenuated the impacts of economic hardship. For example, Federal stimulus payments which targeted households impacted by the economic effects of the pandemic might have helped provide a cushion for some of the most disastrous economic impacts of the pandemic. Prior work indicates that exposure to traumatic community-wide disasters alone do not always increase the risk of suicide.40 In response to catastrophic events or economic shocks, a robust public response might play an important role in managing potential impacts on suicide,41 particularly those targeted to at risk groups.33 Future work might examine the role that unemployment insurance and worker support programs mitigated psychiatric impacts of the pandemic on financially unstable people and low-income households.
During the early stages of the pandemic nearly 30% of Americans reported some kind of mental health stressor—with Hispanic/Latinx people reporting the highest number.42 18% of people surveyed indicated that their mental health was worse after the onset of the pandemic.43 However—despite these reports of declining mental health—emergency psychiatric visits declined in Italy after the onset of the COVID-19 crisis.44 Our results for suicide agreed with previous research from our group showing that patterns of emergency room visits found for suicide attempts and self-harm in a hospital in Michigan did not increase.45 While self-harm attempts and suicide mortality might reflect the general mental health and wellbeing of a population, it has been shown that depression itself is not a perfect predictor of suicide attempt.46 Thus, the suicide patterns shown might be poorer indicators of mental health risks than patterns of mortality from substance abuse.
We found some support for our first hypothesis as it related to changes in alcohol consumption after the pandemic began. At the beginning of the pandemic in 2020 some researchers expressed concern over increases in incidence of liver failure and mortality because of increased alcohol consumption and decreased access to clinical care for people with alcohol use disorder (AUD), alcohol-associated liver disorder (ALD), and possible hepatic injury from COVID-19 infections.47 Alcohol sales rose for nearly all months of 2020 compared with three year monthly averages,48 confirming the possibility of overall increased consumption of alcohol. Inactivity and boredom have been associated with increased alcohol consumption among several demographic groups including older individuals,49 refugees,50 young people,51 and university students.52 These studies suggest that the lack of stimulating activities during the pandemic might have increased alcohol consumption and thus increased risks for liver related health problems, explaining the patterns found in our results. We note that while we found that incidence of mortality from alcohol related liver failure increased for all groups in the crude analyses, ITS analyses indicated that deaths only significantly increased for those over 65.
Consistent with our hypothesis, we observed an increase in substance use related deaths due to alcohol related liver disease and drug overdoses during the earlier phase of the pandemic in Michigan. In our data, the increase in drug overdoses began soon after the onset of the COVID-19 pandemic and peaked in mid-summer. The pattern of increase agrees with studies of overdose mortality in other regions.53,54 There are distinct pathways by which the pandemic may influence substance use-related mortality, despite the lack of increase in suicide deaths. Unlike suicide, substance use can also serve as a coping mechanism for psychosocial stressors.55 Joblessness among low wage earners is suspected to play a role in higher rates of opioid overdoses during the pandemic.53,56 In the past, economic downturns were also associated with increased numbers of opioid overdose deaths— particularly in white men under the age of 45—and macro-economic conditions drive opioid related deaths.15 Long-term unemployment is also a risk factor for overdose-related deaths.56 The inability to reach patients struggling from addiction and substance abuse disorders has also been noted as a possible pathway that might increase overdose deaths.57 More work should be done to disentangle the complex factors that determine overdose risk and mortality during sudden and unforeseen events like the COVID-19 pandemic.
While the patterns of mortality incidence in this study could be attributed to exogenous societal and economic factors, it is possible that endogenous factors of COVID-19 infection also played a role. SARS-CoV-2 can cross the blood brain barrier and increase the risk of neurological and psychiatric outcomes,58 especially among those with more severe forms of COVID-19 (e.g., hospitalization, intubation).59 Patterns within demographic groups might represent disparate levels of infection. For example, Black and American Indian and Alaska Native (AIAN) communities have experienced higher COVID-19 infection and mortality rates than predominantly White communities.60 While we did not have enough AIAN decedents to test the association of AIAN with mental health related mortality before and after the onset of the pandemic, some of the increase in substance-abuse related mortality in Black decedents might be explained by high levels of infection. Further research should test whether “long covid” or lingering cognitive and psychiatric impacts of acute COVID-19 infection influence mental health mortality risk. This hypothesis could not be tested within our data since we did not have information on COVID-19 infection status, but it is worthy of further study.
This study has limitations—namely that misclassification and recording errors on death certificates are common problems in mortality studies.61,62 Incomplete death certificates,63 attributing suicide deaths to other causes,64, 65, 66, 67 and racial biases in death reporting,67, 68, 69, 70 including suicide and self-inflicted injury,71,72 is well established and could be exasperated during the pandemic. Another limitation is the inability to validate whether decedents who died because of alcohol related liver failure or overdose suffered from a substance abuse disorder. Studies of mortality could benefit from more detailed patient histories. In the case of death records, information on past substance abuse or psychiatric problems are unavailable. Moreover, there could be misclassification of overdose death; some overdoses may have actually been intentional poisonings. Other research has found evidence for ambiguous intent or misreporting in overdose deaths.73,74 Finally, there is the general limitation the variables examined are not sufficient to capture all of the factors that might influence mortality risk given a sudden shock like the COVID-19 pandemic. While we believe that examining temporal patterns of mortality among, for example, racial groups, information on household income or employment status might provide more detailed insights.
This research suggests that sudden crises such as the COVID-19 pandemic present unique risks for mental health related mortality. Future work should explore how sudden uncertainty due to a confluence of health; economic, and societal factors impact individual mental health. Research should focus on developing methods to support those most likely to be impacted by crises like the COVID-19 pandemic to minimize mental health related mortality. For example, this research found that while being married was protective against all forms of mortality, being widowed or divorced significantly raised the risk for alcohol related liver failure and overdose. Programs might be designed to provide mental health and substance use support those who have lost a partner in a context of stay-at-home orders and pauses in regular work schedules. Work might be also be done to target prescribing physicians, who need to be aware of the risks of overdose among patients within specific groups in the context of similar and sudden crises. Further, research should use newly found insights—along with wide community engagement—to create new models and modelling strategies of mortality risk which account for the unique nature of pandemic crises.
Contributors
PSL and RSB contributed equally to all aspects of this research.
Declaration of interests
The authors declare no conflicts of interest.
Acknowledgments
We thank Dr. Jon Zelner and Dr. Ryan Malosh for their assistance in this research.
Funding
Data from the MDHHS was purchased using funds from a grant from the United States National Institute of Environmental Health Sciences [K99/R00ES026198]. Salary support for PSL was provided from the Institute for Global Biological Change (IGBC) at the University of Michigan. RSB was supported by the the United States National Institute of Environmental Health Sciences Michigan Center on Lifestage Environmental Exposures and Disease [grant number NIEHS P30ES017885].
References
- 1.Wellenius G.A., Vispute S., Espinosa V., et al. Impacts of social distancing policies on mobility and COVID-19 case growth in the us. Nat Commun. 2021;12(1) doi: 10.1038/s41467-021-23404-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown S., Schuman D.L. Suicide in the time of COVID-19: a perfect storm. J Rural Health. 2021;37(1):211–214. doi: 10.1111/jrh.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nordt C., Warnke I., Seifritz E., Kawohl W. Modelling suicide and unemployment: a longitudinal analysis covering 63 countries, 2000–11. Lancet Psychiatry. 2015;2(3):239–245. doi: 10.1016/s2215-0366(14)00118-7. [DOI] [PubMed] [Google Scholar]
- 4.Kawohl W., Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020;7(5):389–390. doi: 10.1016/S2215-0366(20)30141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Serafini G., Parmigiani B., Amerio A., Aguglia A., Sher L., Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM Int J Med. 2020;113(8):531–537. doi: 10.1093/qjmed/hcaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saki M., Ghanbari M.K., Behzadifar M., et al. The impact of the social distancing policy on COVID-19 incidence cases and deaths in Iran from February 2020 to January 2021: insights from an interrupted time series analysis. Yale J Biol Med. 2021;94(1):13–21. https://pubmed.ncbi.nlm.nih.gov/33795979 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7995950/ [PMC free article] [PubMed] [Google Scholar]
- 7.Chang S.S., Stuckler D., Yip P., Gunnell D. Impact of 2008 global economic crisis on suicide: time trend study in 54 countries. BMJ. 2013;347(sep17 1):f5239. doi: 10.1136/bmj.f5239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Herbig B., Dragano N., Angerer P. Health in the long-term unemployed. Dtsch Arzteblatt Int. 2013;110(23–24):413–U17. doi: 10.3238/arztebl.2013.0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mossakowski K.N. Is the duration of poverty and unemployment a risk factor for heavy drinking? Soc Sci Med. 2008;67(6):947–955. doi: 10.1016/j.socscimed.2008.05.019. (1982) [DOI] [PubMed] [Google Scholar]
- 10.Junna L., Moustgaard H., Martikainen P. Unemployment from stable, downsized and closed workplaces and alcohol-related mortality. Addiction. 2021;116(1):74–82. doi: 10.1111/add.15106. (Abingdon, England) [DOI] [PubMed] [Google Scholar]
- 11.Frijters P., Johnston D.W., Lordan G., Shields M.A. Exploring the relationship between macroeconomic conditions and problem drinking as captured by google searches in the us. Soc Sci Med. 2013;84:61–68. doi: 10.1016/j.socscimed.2013.01.028. (1982) [DOI] [PubMed] [Google Scholar]
- 12.Hollingsworth C.J.R, Simon K. Macroeconomic conditions and opioid abuse. J Health Econ. 2017;56:222–233. doi: 10.1016/j.jhealeco.2017.07.009. [DOI] [PubMed] [Google Scholar]
- 13.Frankenfeld L., Leslie T.F. County-level socioeconomic factors and residential racial, hispanic, poverty, and unemployment segregation associated with drug overdose deaths in the united states, 2013–2017. Ann Epidemiol. 2019;35:12–19. doi: 10.1016/j.annepidem.2019.04.009. [DOI] [PubMed] [Google Scholar]
- 14.Pear V.A., Ponicki W.R., Gaidus A., et al. Urban-rural variation in the socioeconomic determinants of opioid overdose. Drug Alcohol Depend. 2019;195:66–73. doi: 10.1016/j.drugalcdep.2018.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown E., Wehby G.L. Economic conditions and drug and opioid overdose deaths. Med Care Res Rev. 2019;76(4):462–477. doi: 10.1177/1077558717722592. [DOI] [PubMed] [Google Scholar]
- 16.Taylor R., Page A., Wodak A., Dudley M., Munot S., Morrell S. Confluence of suicide and drug overdose epidemics in young Australian males: common causality? BMC Public Health. 2018;18(1):965. doi: 10.1186/s12889-018-5875-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ramchand R., Gordon J.A., Pearson J.L. Trends in suicide rates by race and ethnicity in the united states. JAMA Netw Open. 2021;4(5) doi: 10.1001/jamanetworkopen.2021.11563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoon Y.H., Chen C.M., Slater M.E., Jung M.K., White A.M. Trends in premature deaths from alcoholic liver disease in the U.S., 1999–2018. Am J Prev Med. 2020;59(4):469–480. doi: 10.1016/j.amepre.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keene D.E., Cowan S.K., Baker A.C. “when you're in a crisis like that, you don't want people to know”: mortgage strain, stigma, and mental health. Am J Public Health. 2015;105(5):1008–1012. doi: 10.2105/AJPH.2014.302400. (1971) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoopsick R.A., Homish G.G., Leonard K.E. Differences in opioid overdose mortality rates among middle-aged adults by race/ethnicity and sex, 1999-2018. Public Health Rep. 2021;136(2):192–200. doi: 10.1177/0033354920968806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Phillips J.A., Nugent C.N. Suicide and the great recession of 2007–2009: the role of economic factors in the 50 U.S. states. Soc Sci Med. 2014;116:22–31. doi: 10.1016/j.socscimed.2014.06.015. (1982) [DOI] [PubMed] [Google Scholar]
- 22.Kaplan M.S., Huguet N., Caetano R., Giesbrecht N., Kerr W.C., Mcfarland B.H. Heavy alcohol use among suicide decedents relative to a nonsuicide comparison group: gender-specific effects of economic contraction. Alcohol Clin Exp Res. 2016;40(7):1501–1506. doi: 10.1111/acer.13100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Margerison-Zilko C., Goldman-Mellor S., Falconi A., Downing J. Health impacts of the great recession: a critical review. Curr Epidemiol Rep. 2016;3(1):81–91. doi: 10.1007/s40471-016-0068-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.G. Whitmer, Declaration of state of emergency 2020-4 (2020). http://www.legislature.mi.gov/documents/2019-2020/executiveorder/pdf/2020-EO-04.pdf
- 25.United States Census Bureau, 2010 census urban and rural classification and urban area criteria. URL https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural/2010-urban-rural.html
- 26.Bernal J.L, Cummins S., Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2016:dyw098. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fukuma S., Ikenoue T., Yamada Y., et al. Changes in drug utilization after publication of clinical trials and drug-related scandals in japan: an interrupted time series analysis, 2005–2017. J Epidemiol. 2021;31(7):410–416. doi: 10.2188/jea.je20200181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fournier P., Dumont A., Tourigny C., Philibert A., Coulibaly A., Traore M. The free caesareans policy in low-income settings: an interrupted time series analysis in Mali (2003–2012) PLoS One. 2014;9(8) doi: 10.1371/journal.pone.0105130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hategeka C., Ruton H., Karamouzian M., Lynd L.D., Law M.R. Use of interrupted time series methods in the evaluation of health system quality improvement interventions: a methodological systematic review. BMJ Glob Health. 2020;5(10) doi: 10.1136/bmjgh-2020-003567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.R Core Team, R: a language and environment for statistical computing (2017). https://www.R-project.org/
- 31.Harper S., Bruckner T.A. Did the great recession increase suicides in the usa? evidence from an interrupted time-series analysis. Ann Epidemiol. 2017;27(7):409–414. doi: 10.1016/j.annepidem.2017.05.017. e6. [DOI] [PubMed] [Google Scholar]
- 32.Gong B., Zhang S., Yuan L., Chen K.Z. A balance act: minimizing economic loss while controlling novel coronavirus pneumonia. J Chin Gov. 2020;5(2):249–268. doi: 10.1080/23812346.2020.1741940. [DOI] [Google Scholar]
- 33.Kaufman J.A., Livingston M.D., Komro K.A. Unemployment insurance program accessibility and suicide rates in the united states. Prev Med. 2020;141 doi: 10.1016/j.ypmed.2020.106318. https://www.sciencedirect.com/science/article/pii/S009174352030342X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reid E.R.P, Schenker M.B. Migrant workers, essential work, and COVID-19. Am J Ind Med. 2021;64(2):73–77. doi: 10.1002/ajim.23209. [DOI] [PubMed] [Google Scholar]
- 35.Bray M.J.C., Daneshvari N.O., Radhakrishnan I., et al. Racial differences in statewide suicide mortality trends in Maryland during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2020.3938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chavis L. Chicago Sun Times; 2021. More Suicides by Black Cook County Residents in 2020 Than in any Year in Over a Decade.https://chicago.suntimes.com/2021/2/19/22290148/suicide-black-cook-county-residents-rise-mental-health-covid-coronavirus [Google Scholar]
- 37.Leske S., Ko~lves K., Crompton D., Arensman E., De Leo D. Realtime suicide mortality data from police reports in Queensland, Australia, during the COVID-19 pandemic: an interrupted time-series analysis. Lancet Psychiatry. 2021;8(1):58–63. doi: 10.1016/s2215-0366(20)30435-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tanaka T., Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in japan. Nat Hum Behav. 2021 doi: 10.1038/s41562-020-01042-z. [DOI] [PubMed] [Google Scholar]
- 39.Pirkis J., John A., Shin S., et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8(7):579–588. doi: 10.1016/s2215-0366(21)00091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mezuk B., Larkin G.L., Prescott M.R., et al. The influence of a major disaster on suicide risk in the population. J Trauma Stress. 2009;22(6):481–488. doi: 10.1002/jts.20473. [DOI] [PubMed] [Google Scholar]
- 41.Norstrom T., Gronqvist H. The great recession, unemployment and suicide. J Epidemiol Commun Health. 2015;69(2):110–116. doi: 10.1136/jech-2014-204602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mcknight-Eily L.R., Okoro C.A., Strine T.W., et al. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic — United States, April and May 2020. MMWR Morb Mortal Wkly Rep. 2021;70(5):162–166. doi: 10.15585/mmwr.mm7005a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gerlach L.B., Solway E., Maust D.T., et al. The COVID-19 pandemic and mental health symptoms among us adults. J Gen Intern Med. 2021 doi: 10.1007/s11606-021-07046-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stein H., Giordano B., Del Giudice R., Basi C., Gambini O., D'Agostino A. Pre/post comparison study of emergency mental health visits during the Covid -19 lockdown in lombardy, italy. Psychiatry Clin Neurosci. 2020;74(11):605–607. doi: 10.1111/pcn.13126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bergmans R., Larson P.S. Suicide attempt and intentional self-harm during the earlier phase of the COVID-19 pandemic in Washtenaw county, Michigan. J Epidemiol Commun Health. 2021 doi: 10.1136/jech-2020-215333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Handley T., Rich J., Davies K., Lewin T., Kelly B. The challenges of predicting suicidal thoughts and behaviours in a sample of rural australians with depression. Int J Environ Res Public Health. 2018;15(5):928. doi: 10.3390/ijerph15050928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Da B.L., Im G.Y., Schiano T.D. Coronavirus disease 2019 hangover: a rising tide of alcohol use disorder and alcohol-associated liver disease. Hepatology. 2020;72(3):1102–1108. doi: 10.1002/hep.31307. [DOI] [PubMed] [Google Scholar]
- 48.Alcohol sales during the COVID-19 pandemic, surveillance report COVID-19 (2021).
- 49.Kuerbis A, Padovano HT, Shao S, Houser J, Muench FJ, Morgenstern J. Comparing daily drivers of problem drinking among older and younger adults: an electronic daily diary study using smartphones, Drug Alcohol Depend 183 240–246. 10.1016/j.drugalcdep.2017.11.012. [DOI] [PMC free article] [PubMed]
- 50.Horyniak D., Higgs P., Cogger S., Dietze P., Bofu T. Heavy alcohol consumption among marginalised African refugee young people in Melbourne, Australia: motivations for drinking, experiences of alcohol- related problems and strategies for managing drinking. Ethn Health. 2016;21(3):284–299. doi: 10.1080/13557858.2015.1061105. [DOI] [PubMed] [Google Scholar]
- 51.Nothing to do, the relationship between leisure boredom and alcohol and drug addiction, is there a link to youth suicide in rural Australia, Youth Stud Aust. 18(2):24–29.
- 52.Disinhibited characteristics and binge drinking among university student drinkers, Addict Behav.35(3):242–251. 10.1016/j.addbeh.2009.10.020. [DOI] [PubMed]
- 53.Macmadu S.B, Correia Gabel A.M., Rosenberg M., et al. Comparison of characteristics of deaths from drug overdose before vs during the COVID-19 pandemic in Rhode island. JAMA Netw Open. 2021;4(9) doi: 10.1001/jamanetworkopen.2021.25538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shreffler J., Shoff H., Thomas J.J., Huecker M. Brief report: the impact of COVID-19 on emergency department overdose diagnoses and county overdose deaths. Am J Addict. 2021;30(4):330–333. doi: 10.1111/ajad.13148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Colder C.R. Life stress, physiological and subjective indexes of negative emotionality, and coping reasons for drinking is there evidence for a selfmedication model of alcohol use? Psychol Addict Behav. 2001;15(3):237–245. doi: 10.1037/0893-164X.15.3.237. [DOI] [PubMed] [Google Scholar]
- 56.Arnold C. The US Covid pandemic has a sinister shadow—drug overdoses. BMJ. 2020:m4751. doi: 10.1136/bmj.m4751. [DOI] [PubMed] [Google Scholar]
- 57.Rudolph K.E., Kinnard E.N., Aguirre A.R., et al. he relative economy and drug overdose deaths. Epidemiology. 2020;31(4):551–558. doi: 10.1097/EDE.0000000000001199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xie Q., Liu X.B., Xu Y.M., Zhong B.L. Understanding the psychiatric symptoms of COVID-19: a meta-analysis of studies assessing psychiatric symptoms in chinese patients with and survivors of COVID-19 and SARS by using the symptom checklist-90-revised. Transl Psychiatry. 2021;11(1) doi: 10.1038/s41398-021-01416-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Taquet M., Geddes J.R., Husain M., Luciano S., Harrison P.J. 6-month neurological and psychiatric outcomes in 236379 survivors of Covid- 19 a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8(5):416–427. doi: 10.1016/S2215-0366(21)00084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.H. Silverman, K. Toropin, S. Sidner, L. Perrot, Navajo nation surpasses New York State for the highest COVID-19 infection rate in the US, CNN wire service (2020).
- 61.Mcgivern L., Shulman L., Carney J.K., Shapiro S., Bundock E. Death certification errors and the effect on mortality statistics. Public Health Rep. 2017;132(6):669–675. doi: 10.1177/0033354917736514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.The accuracy of death certificate completion in a suburban community, Am J Forensic Med Pathol. 31(3):232–235. 10.1097/PAF.0b013e3181e5e0e2. [DOI] [PubMed]
- 63.Gill J.R., Dejoseph M.E. The importance of proper death certification during the COVID-19 pandemic. JAMA. 2020;324(1):27. doi: 10.1001/jama.2020.9536. [DOI] [PubMed] [Google Scholar]
- 64.Carr J.R., Hoge C.W., Gardner J., Potter R. Suicide surveillance in the U.S. military-reporting and classification biases in rate calculations. Suicide Life Threat Behav. 2004;34(3):233–241. doi: 10.1521/suli.34.3.233.42785. [DOI] [PubMed] [Google Scholar]
- 65.Donaldson E., Larsen G.Y., Fullerton-Gleason L., Olson L.M. Classifying undetermined poisoning deaths. Inj Prev. 2006;12(5):338–343. doi: 10.1136/ip.2005.011171. https://injuryprevention.bmj.com/content/12/5/338.full.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ohberg J.L. Suicides hidden among undetermined deaths. Acta Psychiatr Scand. 1998;98(3):214–218. doi: 10.1111/j.1600-0447.1998.tb10069.x. [DOI] [PubMed] [Google Scholar]
- 67.Rockett R., Wang S., Stack S., et al. Race/ethnicity and potential suicide misclassification: window on a minority suicide paradox? BMC Psychiatry. 2010;10(1):35. doi: 10.1186/1471-244x-10-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jim M.A., Arias E., Seneca D.S., et al. Racial misclassification of American Indians and Alaska natives by Indian health service contract health service delivery area. Am J Public Health. 2014;104(S3):S295–S302. doi: 10.2105/ajph.2014.301933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Noymer A.M.P, Saperstein A. Cause of death affects racial classification on death certificates. PLoS One. 2011;6(1):e15812. doi: 10.1371/journal.pone.0015812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Arias E., Schauman W.S., Eschbach K., Sorlie P.D., Backlund E. The validity of race and Hispanic origin reporting on death certificates in the united states, Vital and health statistics, Series 2. Data Eval Methods Res. 2008;148:1–23. [PubMed] [Google Scholar]
- 71.Rockett R.H., Caine E.D., Connery H.S., et al. Unrecognised self-injury mortality (SIM) trends among racial ethnic minorities and women in the USA. Inj Prev. 2020;26(5):439–447. doi: 10.1136/injuryprev-2019-043371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ali I.R.H.R, Miller T.R., Leonardo J.B. Racial/ethnic differences in preceding circumstances of suicide and potential suicide misclassification among us adolescents. J Racial Ethn Health Disparities. 2021 doi: 10.1007/s40615-020-00957-7. [DOI] [PubMed] [Google Scholar]
- 73.Shiels M.S., Tatalovich Z., Chen Y., et al. Trends in mortality from drug poisonings, suicide, and alcohol- induced deaths in the united states from 2000 to 2017. JAMA Netw Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.16217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bohnert S.B., McCarthy J.F., Ignacio R.V., Ilgen M.A., Eisenberg A., Blow F.C. Misclassification of suicide deaths: examining the psychiatric history of overdose decedents. Inj Prev. 2013;19(5):326–330. doi: 10.1136/injuryprev-2012-040631. https://injuryprevention.bmj.com/content/19/5/326.full.pdf [DOI] [PubMed] [Google Scholar]