Abstract
Objective
Food allergy (FA) management requires youth to avoid allergens and carry emergency medication which can impact participation in social activities. Previous research indicates that some youth experience FA-related bullying, but many studies are limited by single-item assessment methods and a narrow definition of bullying. This study describes FA-related bullying among a diverse cohort of youth with FA and evaluates parent–child disagreement and bullying assessment methods.
Methods
Youth ages 9–15 years (n = 121) diagnosed with an IgE-mediated FA and their primary caregivers were recruited from pediatric FA clinics to complete surveys about their FA-related bullying experiences. Descriptive statistics were conducted to assess overall FA-related bullying and McNemar tests were utilized to assess disagreement among parent–child report and between multi-item and single-item assessment methods.
Results
Seventeen percent and 31% of youth reported FA-related bullying on single-item and multi-item assessments, respectively. Twelve percent of parents reported their child had experienced FA-related bullying. Youth reported overt physical (51%), overt non-physical (66%), and relational FA-related bullying (20%). FA-related bullying was most common among classmates. Assessment method significantly affected the rates of FA-related bullying reported by youth, and parents and youth only agreed on FA-bullying experiences when assessed via the single-item measure.
Conclusions
A subset of a diverse sample of youth with FA reported FA-related bullying. Clinicians should use multi-item assessment methods and ask both parents and children about their experiences to fully capture the experiences of families managing FA. School policies that facilitate FA safety and social inclusion should be promoted.
Clinical Trial Registration
N/A.
Keywords: adolescents, chronic illness, parent–adolescent communication, parents, social functioning and peers
Introduction
IgE-mediated food allergy (FA) is a time-consuming and potentially life-threatening chronic illness that affects an estimated 8% of children in the United States (Gupta et al., 2018). Stress and anxiety are common in pediatric FA patients, and many children report a negative impact on their quality of life (QoL) (Shaker et al., 2017). Research has shown that managing FA in social situations can be challenging for youth because they have to bring allergen-free foods to social events or eat nothing at all, ask about ingredients at restaurants and social gatherings, and sometimes sit at a separate lunch table at school. Many social activities center around food, and youth with FA may perceive their diagnosis and FA management regimen as isolating and causing unwanted attention or feel that they are treated differently as a result (Johnson & Woodgate, 2017).
Bullying is a common form of peer victimization among children and adolescents that can be delineated into overt victimization (i.e., physical or verbal aggression) and relational victimization (i.e., covert or indirect aggression that damages one’s social status within a peer group) (Casper & Card, 2017). A National Academies of Sciences, Engineering, and Medicine report estimated that the prevalence of bullying victimization among U.S. school-aged children ranged from 17.9% to 30.9% and bullying is related to increased risk of anxiety, depression, and suicidal ideation and suicidal/self-injurious behaviors in healthy children (Flannery et al., 2016). Rates of bullying, teasing, and social exclusion are higher among adolescents with chronic health conditions than the general population (Fong et al., 2017).
Results from initial studies regarding FA-related bullying provide a broad overview of youths’ experiences. FA-related bullying was reported by 23% of youth in a study conducted by Fong et al. (2018), 24% of youth in a study by Muraro et al. (2014), and 32% of youth in a study by Shemesh et al. (2013). In an Italian study, children and adolescents with FA were approximately twice as likely to be bullied as a healthy control group matched for sex and age (Muraro et al., 2014). These studies indicated that FA-related bullying is related to decreased QoL (Annunziato et al., 2014; Shemesh et al., 2013) and increased distress in youth with FA and their parents (Shemesh et al., 2013). Furthermore, FA-related bullying poses a risk of a serious allergic reaction if harassment with the child’s allergen is involved. Thus, it is established that youth with FA should be considered high risk for FA-related bullying victimization and related outcomes such as psychosocial distress and even allergic reactions (Muraro et al., 2014). However, the majority of these studies have only examined FA-related bullying as an overarching experience and not delineated the frequency of overt victimization versus relational victimization, an important distinction given that overt victimization may directly lead to an allergic reaction if there is allergen contact. Further research is needed to understand the ways in which youth are bullied for their FA.
There is also a need to establish best practices for FA-related bullying assessment, including operational definitions of bullying, ways bullying is queried, and who should be asked about FA-related bullying (i.e., child, parent, both). A cohort study of U.S. students in three cities found that general bullying victimization was significantly underreported using a single-item question that directly referenced “bullying” compared to a multiple-item measure focused on specific victimization behaviors with no mention of “bullying” (Jetelina et al., 2019); children may be uncertain about what experiences fall into the “bullying” category and more likely to endorse specific victimization behaviors. Many previous studies about FA-related bullying have assessed victimization using the former method (Brown et al., 2021; Lieberman et al., 2010; Shemesh et al., 2013). In contrast, Muraro et al. (2014) asked about the frequency of multiple victimization behaviors on a Likert scale and reported on the frequency at which participants experienced FA-related bullying at least once. However, they did not compare response rates to a single-item method, so it is unknown if these methods were equivalent. Determining who to ask about FA-related bullying is important as well because there is evidence from studies of general bullying experiences that parents may be unaware when bullying occurs and that adults may underestimate bullying frequency (Blomqvist et al., 2020; Boulton et al., 2017; Demaray et al., 2013; Stives et al., 2019). Most FA-related bullying studies either use all or mostly parent report (Lieberman et al., 2010), or just child report (Muraro et al., 2014). Only one pediatric FA study examined parent–child FA-related bullying agreement and found that parents did not report FA-related bullying reported by their child about 50% of the time (Shemesh et al., 2013). A greater understanding of how to assess FA-related bullying could improve identification of youth who experience such bullying and subsequently increase the likelihood that these individuals receive help addressing the bullying and its impact on their psychosocial functioning.
This study uses self-report and parent-report to examine FA-related bullying experiences among a racially and socioeconomically diverse sample of children and adolescents recruited from FA clinics. This article aims to (1) describe FA-related bullying experiences as reported by youth with FA and their parents; (2) evaluate two self-report FA-related bullying assessment methods, a multi-item bullying inventory versus a single-item, and (3) evaluate child–parent disagreement regarding FA-related bullying. Based on prior estimates of FA-related bullying (Fong et al., 2018; Muraro et al., 2014; Shemesh et al., 2013) and research regarding parent–child agreement regarding general bullying experiences (Blomqvist et al., 2020; Boulton et al., 2017; Demaray et al., 2013; Stives et al., 2019), we hypothesized that one-quarter to one-third of youth would report having experienced FA-related bullying, that a multi-item inventory of FA-related bullying behavior would be more sensitive to FA-related bullying experiences than a single-item, and that youth would report more FA-related bullying than their parents.
Methods
Participants
Study procedures were approved by the Institutional Review Board. All data were collected from May 2016 to December 2019 as part of a broader study about FA-related adjustment and adherence among youth. Participants were recruited from five allergy clinics at two mid-Atlantic pediatric hospitals. Eligible youth were patients ages 8–18 years diagnosed with at least one of the top eight IgE-mediated FAs (peanut, tree nut, cow’s milk, egg, wheat, soy, shellfish, and fish) by an allergist, and a primary caregiver (hereafter called ‘parent’). Youth diagnosed with other allergic conditions (e.g., asthma, atopic dermatitis) commonly comorbid with FA were included. Exclusion criteria included youth diagnosis of a non-atopic medical illness or developmental disorder, non-English fluency, and lack of parental consent.
Procedure
Potential participants were consecutively identified by members of the study research team via review of clinic appointment schedules, or by referral from a member of the allergy team. A study team member then contacted the family by phone or email or met with the family in-person at a routine allergy appointment to assess eligibility and interest in participation. Eligible patients completed informed written consent (parent), and verbal assent (child) or written assent (child ages 12 and up) in person with a study team member at an allergy appointment. Consented participants then had the option to complete questionnaires on paper or online via REDCap (Research Electronic Data CAPture; Harris et al., 2009) either on an iPad in clinic or at home. Youth and primary caregivers completed questionnaires separately. Families were given modest compensation ($50) for questionnaire completion.
Measures
Sociodemographics
Demographic questionnaires collected information on child age, gender, race and ethnicity, parent age, gender, education, employment status, family composition, and household annual income.
Child Medical Information
Child medical information was obtained from the parent, including age of first FA diagnosis, current FA diagnoses, comorbid allergic diagnoses, epinephrine auto-injector prescription status, and past allergic reaction history.
Food Allergy-Related Bullying
Youth completed the EMPOWER Program Survey of Children with Food Allergy (EMPOWER—Child) and parents completed the EMPOWER Program Survey of Parents of a Child with Food Allergy (EMPOWER—Parent) (Shemesh et al., 2013). Both versions of the questionnaire begin with a definition and examples of bullying, instructing respondents to keep the definition in mind while answering questions. The EMPOWER Program Surveys were developed by Shemesh et al. (2013) and have been used previously in pediatric FA populations.
The EMPOWER—Child assesses FA-related bullying experiences across the child’s lifetime using youth self-report. The questionnaire first assesses the frequency of six FA-related bullying behaviors (being called mean names due to FA, being teased about FA, being made fun of due to FA, being hit, kicked, shoved, or pushed around, and being threatened with allergen exposure, having lies told about their FA to make others dislike them) using a 5-option scale ranging from “This has never happened to me” to “Several times a week.” The questionnaire then asks a separate question about FA-related bullying: “Were you ever bullied, teased, or harassed about your food allergy?” Descriptive questions about FA-related bullying are then completed pertaining to the setting(s), perpetrator(s), and reason(s) for being bullied. Respondents who endorsed FA-related bullying are asked to check off any locations where FA-related bullying occurred (inside at school, outside at school, at work, at a mall, at a restaurant, at home, and at someone else’s house), any individuals who engaged in FA-related bullying (classmates, teachers/school staff, other students, siblings, relatives, coworkers, and significant other), and any reasons they believed they were bullied (due to FA, due to wearing/carrying medications, due to special FA treatment, and due to not being able to be with the group). Respondents are then asked to check off any specific FA-related overt physical, overt verbal, and relational victimization they experienced (see Figure 1 for a list) and any impact from the FA-related bullying (see Figure 2 for a list). Finally, respondents indicate if they ever told anyone about their victimization or if they ever worry about being bullied.
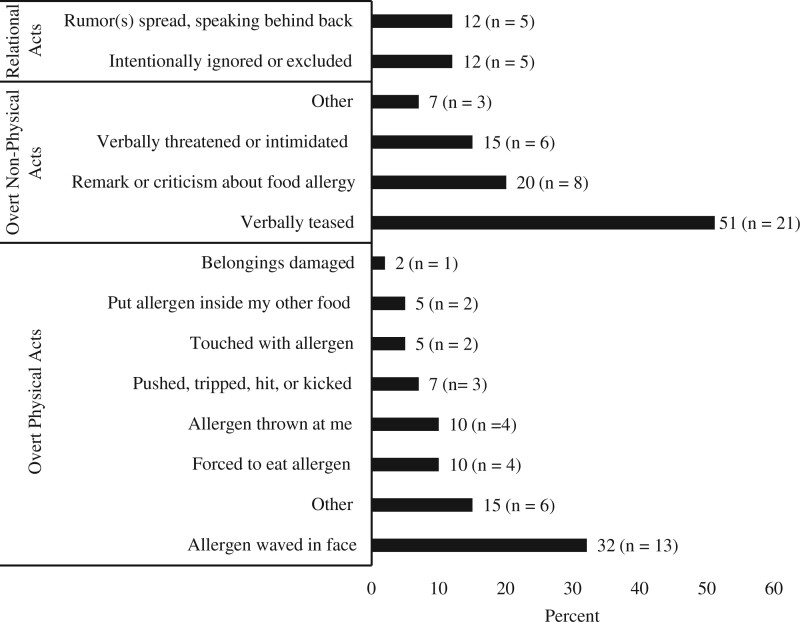
Figure 1.
Frequency of food allergy-related bullying victimization involving overt physical, overt non-physical, and relational acts (n = 41).
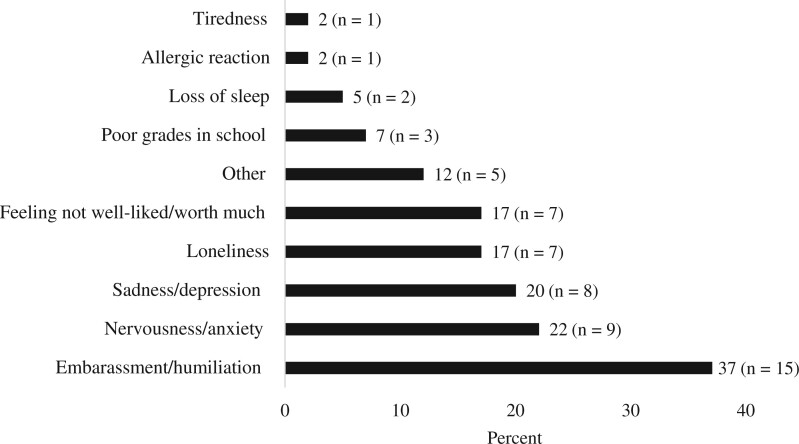
Figure 2.
Food allergy-related bullying outcomes (n = 41).
The EMPOWER—Parent assesses the parent’s perception of their child’s experience of FA-related bullying across the child’s lifetime and their own FA-related bullying experiences. The measure first assesses the child’s FA-related bullying by asking: “Was your child ever bullied because of food allergy?” It subsequently asks parents to indicate if their child ever told them they were bullied due to FA, if they needed to do anything to stop the FA-related bullying, and if what they did was helpful. Parents are then asked if they as a parent have ever been made fun of or teased in a hurtful way due to their concerns about their child’s FA. Parents who endorse that they have experienced FA-related bullying as a parent then check off the perpetrators (e.g., spouse, friend).
Data Analytic Plan
Demographic and medical variable frequencies and EMPOWER survey response frequencies were assessed using SPSS. Three variables were used for the series of McNemar tests: (1) ‘FA Child Inventory’: a dichotomous variable that was created by collapsing the six FA-related bullying frequency questions on the EMPOWER—Child (‘yes’ assigned if they endorsed experiencing at least one of the six FA-related bullying behaviors at any frequency, ‘no’ assigned if they did not endorse experiencing any of the bullying behaviors), (2) ‘FA Child Dichotomous’: the yes/no question that children answered regarding whether or not they had experienced FA-related bullying, and (3) ‘FA Parent Proxy Dichotomous’: a dichotomous parent proxy question created using ‘yes’ and ‘no’ answers about whether or not their child had experienced FA-related bullying. McNemar tests were conducted to assess child disagreement regarding the two child FA-related bullying assessment methods (FA Child Inventory vs. FA Child Dichotomous) and to assess child–parent disagreement regarding FA-related bullying experiences (FA Child Dichotomous vs. FA Parent Proxy Dichotomous). Three youths had one or more missing items on the questions that comprised the FA Child Inventory, but none were missing answers on all six questions. In the recode, missing items were considered as not endorsing any frequency of the victimization behavior. There were no missing data for FA Child Dichotomous or FA Parent Proxy Dichotomous.
Results
Participant Demographics
One hundred seventy-two participants consented to be in the study. Of these, 121 youth (Mage = 11.8 years, SD = 1.37, Range = 9–15) and 121 primary caregivers (Mage = 43.6 years, SD = 7.11, 90% mothers) completed questionnaires. Youth were 60% male (n = 72) and 37% Black, 30% White, 12% Multiracial, 6% American Indian or Alaskan Native, 1% Native Hawaiian or Pacific Islander, and 6% an “Other” race. Twelve percent (n = 14) of youth were Latinx or Hispanic. Primary caregivers were 90% female (n = 104). Sixty-one percent (n = 71) of primary caregivers had a 2-year college education or more and 41% (n = 46) had an annual household income of $100,000 or more. According to the United States Census Bureau (2019), these educational and household income estimates are comparable to the region’s median education and income census data. The racial/ethnic breakdown estimates are also comparable to our clinic populations (42% female, 41% Black 25% White, and 12% Hispanic). See Table I for additional sociodemographic details.
Table I.
Participant Demographic Information (n = 121)
| Child/family demographics | Percentage | M | SD | Range |
|---|---|---|---|---|
| Child age (years) | 11.83 | 1.37 | 9.00–15.00 | |
| Child sex (% female) | 40.0 | |||
| Child race | ||||
| Black | 37.0 | |||
| White | 30.0 | |||
| Asian | 0.0 | |||
| American Indian or Alaskan Native | 6.0 | |||
| Native Hawaiian or Pacific Islander | 1.0 | |||
| Multiracial | 12.0 | |||
| Other | 6.0 | |||
| Child ethnicity (% Hispanic) | 12.0 | |||
| Parent age (years) | 43.6 | 7.11 | ||
| Parent sex (% female) | 90.0 | |||
| Parent education | ||||
| Some high school or less | 6.0 | |||
| Occupational/vocation certificate | 3.0 | |||
| High school diploma or GED | 18.0 | |||
| Some college | 12.0 | |||
| Bachelor’s or Associate’s degree | 29.0 | |||
| Graduate degree | 32.0 | |||
| Household annual income | ||||
| <$20,000 | 5.0 | |||
| $20,000–50,000 | 23.0 | |||
| $50,000–100,000 | 9.0 | |||
| >$100,000 | 41.0 | |||
| No income from the sources mentioned | 2.0 | |||
| Prefer not to answer | 15.0 | |||
| Don’t know/unsure | 5.0 |
Medical Information
Total number of currently diagnosed FAs ranged from 1 to 10 allergens (MtotalFA = 2.75, SD = 1.77), and all top eight most common food allergens were represented, as well as other allergens (e.g., sesame, chickpea, sunflower seed). Tree nuts (77%, n = 93) and peanut (67%, n = 81) were the most common FA diagnoses. The average age of first FA diagnosis was 3.14 years (SD = 2.69, Range = 0.04–14 years). All youth had prescriptions for epinephrine auto-injectors. Fifty-three youth (44%) had experienced an allergic reaction within the past year. Comorbid conditions included eczema (n = 87, 72%), asthma (n = 69, 57%), and environmental allergies (n = 78, 65%). See Table II for additional medical information.
Table II.
Participant Medical Information (n = 121)
| Percentage | M | SD | Range | |
|---|---|---|---|---|
| Total number of food allergies | 2.75 | 1.77 | 1–10 | |
| Specific food allergens | ||||
| Peanut | 66.9 | |||
| Tree nut | 76.9 | |||
| Cow’s milk | 11.6 | |||
| Egg | 19.0 | |||
| Wheat | 5.8 | |||
| Soy | 7.4 | |||
| Fish | 22.3 | |||
| Shellfish | 28.9 | |||
| Sesame | 14.0 | |||
| Other | 14.9 | |||
| Food allergy experiences | ||||
| Age of food allergy diagnosis | 3.14 | 2.69 | 0.04–14 | |
| Child has epinephrine prescription | 100 | |||
| Experienced an allergic reaction in the past year | 43.8 | |||
| Other medical diagnoses | ||||
| Eczema | 72.0 | |||
| Asthma | 57.0 | |||
| Environmental allergies | 65.0 | |||
| Oral allergy syndrome | 10.7 | |||
| Eosinophilic esophagitis | 7.4 |
Youth Self-Report of Food Allergy-Related Bullying Experiences
Using FA Child Dichotomous, 17% of youth (n = 20) disclosed that they had been bullied, teased, or harassed about their FA, while 31% of youth (n = 37) reported that they had experienced FA-related bullying using the FA Child Inventory (endorsing at least one of the six victimization behaviors at any frequency). Twenty-one youths endorsed FA-related bullying using FA Child Inventory but not using FA Child Dichotomous. Conversely, four youths endorsed FA-related bullying using FA Child Dichotomous but not using FA Child Inventory. A McNemar test was conducted comparing youth disagreement regarding FA-related bullying. Results indicated there was significant disagreement between the two assessment strategies, p = .001 (two sided). Chi-square analyses indicated that the proportion of participants who reported FA-related bullying using FA Child Dichotomous did not differ by age (X2 [6, N = 121] = 3.4, p = .76), gender (X2 [1, N = 121] = .9, p = .34), race (X2 [8, N = 121] = 5.4, p = .72), or ethnicity (X2 [3, N = 117] = 6.3, p = .10). Similar chi-square analysis results were found for FA Child Inventory regarding age (X2 [6, N = 118] = 3.8, p = .71), gender (X2 [1, N = 118] = .4, p = .51), race (X2 [8, N = 118] = 13.3, p = .10), and ethnicity (X2 [3, N = 115] = 6.3, p = .10).
Youth who experienced FA-related bullying endorsed both overt and relational victimization experiences. Of the 41 youth who reported FA-related bullying experiences, 51% (n = 21) reported experiencing overt physical acts such as an allergen being waved in their face (32%, n = 13), thrown at them (10%, n = 4), or intentionally put in their food (5%, n = 2). Some participants were forced to eat an allergen (10%, n = 4), and others were purposefully touched with their allergen (5%, n = 2); see Figure 1. One participant reported they experienced an allergic reaction as a direct result of FA-related bullying; see Figure 2 for report of all FA-related bullying outcomes. Twenty-seven youth (66%) endorsed non-physical overt victimization acts including verbal teasing (51%, n = 21), remarks or criticisms about their allergy (20%, n = 8), and verbal threats or intimidation (15%, n = 6); see Figure 1. Eight participants (20%) reported relational FA-related bullying, such as rumors spread or people speaking behind their back (12%, n = 5) and being intentionally ignored or excluded due to their FA (12%, n = 5); see Figure 1.
Of the 41 participants reporting FA-related bullying, 73% were bullied by classmates (n = 30) and 24% by other students (n = 10). FA-related bullying occurred inside the school (71%, n = 29) and outside at school (24%, n = 10). Children who reported FA-related bullying attributed it to a variety of reasons: 46% perceived that it was simply due to having a FA (n = 19), 20% because they were receiving special treatment (i.e., sitting in a different place in the lunchroom, n = 8), 17% because they were not able to be with the group (n = 7), and 2% because they wore or carried FA medications (n = 1). Fifty-six percent of youth reporting FA-related bullying (n = 23) told someone about the bullying behavior, such as a parent, teacher, or friend. Sixty-six percent (n = 27) reported a psychosocial impact of the FA-related bullying: youth reported that the emotional impact of FA-related bullying included embarrassment/humiliation (37%, n = 15), nervousness/anxiety (22%, n = 9), sadness/depression (20%, n = 8), loneliness (17%, n = 7), and feeling that they were not well-liked or worth much (17%, n = 7).
Parent Proxy Report of Youths’ Food Allergy-Related Bullying Experiences
Twelve percent (n = 15) of parents reported that their child had been bullied because of FA, 70% (n = 85) reported their child had not been bullied because of FA, and 17% (n = 21) were not sure. Of the 15 parents that endorsed that their child had been bullied due to FA, 12 (93%) said their child told them about the bullying, and 1 was unsure if their child told them. Nine parents (60%) reported they had to do something to stop the bullying, and of these parents 33% (n = 3) said their intervention helped to stop the bullying from reoccurring.
Two McNemar tests were conducted to examine child–parent disagreement: one comparing FA Child Dichotomous with FA Parent Proxy Dichotomous and a second comparing FA Child Inventory with FA Parent Proxy Dichotomous. Results indicated that there was not significant disagreement between youth and parent report for FA Child Dichotomous (17% vs. 12%, respectively), p = .79, but there was significant disagreement between youth and parent report for FA Child Inventory (31% vs. 12%, respectively), p < .001.
Parent Self-Report of Their Own Food Allergy-Related Bullying Experiences
Seventeen parents (14%) reported they had been made fun of or teased in a hurtful way because of concerns about their child’s FA. Parents who had experienced FA-related bullying reported that friends (41%, n = 7), parents of another child (41%, n = 7), another family member (41%, n = 7), and teachers or principal at the child’s school (29%, n = 5) were the perpetrator(s).
Discussion
This study described the FA-related bullying experiences of children and adolescents, evaluated two FA-related bullying assessment methods, and evaluated child–parent disagreement regarding FA-related bullying. In total, 41 youth (34%) reported FA-related bullying either on the FA Child Inventory variable, the FA Child Dichotomous variable, or both. Fifty-one percent of these youth reported overt physical FA-related bullying, 66% reported overt non-physical FA-related bullying, and 20% reported relational FA-related bullying. FA-related bullying was perpetrated by a variety of individuals across several settings. We found that assessment method significantly affected the rates of FA-related bullying reported by children with FA: 17% of youth endorsed FA-related bullying using the FA Child Dichotomous variable and 31% of youth endorsed FA-related bullying using the FA Child Inventory variable. Twelve percent of parents reported that their child experienced FA-related bullying. The rate of FA-related bullying reported by this racially and socioeconomically diverse sample via FA Child Inventory supports our hypothesis regarding the rate of FA-related bullying and is comparable to or slightly higher than other studies of FA-related bullying (Fong et al., 2018; Muraro et al., 2014) and a general child population (Flannery et al., 2016). However, the rate of FA-related bullying self-reported using the FA Child Dichotomous variable (17%) was lower than other studies.
FA-related bullying may have a profound impact on youth and parent psychosocial functioning and may even endanger patients with FA. A concerning finding of this study was FA-related bullying via dangerous overt physical acts. Multiple youth disclosed being forced to eat something to which they are allergic, which directly put them at risk of a life-threatening allergic reaction. Occurrences of perpetrators waving an allergen in peers’ faces, throwing an allergen at them, or purposefully touching them with an allergen also exposed the participant to risk of allergic reaction, as allergen contact with skin or a nearby surface can result in cross-contact if not properly cleaned (Perry et al., 2004). Indeed, one participant experienced an allergic reaction because of FA-related bullying.
Overt non-physical FA-related bullying acts endanger youths with FA as well. FA management is challenging (Jones et al., 2015), and bullying that punishes youth for FA disclosure or appropriate FA self-management behaviors may further place them at risk for not reading labels, not disclosing an allergic reaction when it occurs, or not having a trusted person who knows how to provide treatment if needed. Furthermore, there is an emotional impact that some youth with FA may experience knowing that someone could harm them with food. Participants reported threats from peers about exposing them to an allergen using the FA Child Inventory variable, and the possibility of being touched by an allergen or having it hidden in their food could impart a constant sense of being unsafe. Being threatened or teased about being exposed to their allergen could interfere with school experiences, their ability to pay attention, and social relationships due to an elevated sense of unsafety or hypervigilance. The current study did not assess the impact of FA-related bullying on youth, or the relation to other factors such as sociodemographic characteristics, and additional work is needed on this subject.
Youth who experience FA-related bullying should be provided with adult support to address the bullying, so identifying accurate assessment methods is critical. This study supports that a multi-item inventory (i.e., FA Child Inventory) identifies twice as much FA-related bullying experiences as a dichotomous response option. The reason for this discrepancy was not investigated, and future studies should investigate the importance of youths’ understanding of what qualifies as bullying and/or comfort with bullying disclosure on FA-related bullying reports. Regardless, the intra-rater disagreement noted in this study indicates that medical and mental health professionals who wish to assess peer experiences among pediatric FA populations should use more comprehensive FA-related bullying assessment methods.
Differences in parent and child reports of FA-related bullying were not significant when comparing the FA Child Dichotomous and FA Parent Proxy Dichotomous variables but were significant when comparing the FA Child Inventory and FA Parent Proxy Dichotomous variables. It is possible that parents may also be narrowly defining FA-related bullying and typically ask their child about bullying as a close-ended question. Alternatively, parents may be unaware that bullying is occurring because youth are reluctant to disclose their experiences due to peer disapproval, feeling weak, or concerns that adults will ignore it or not believe it is occurring (Blomqvist et al., 2020; Boulton et al., 2017; Stives et al., 2019). It is also possible that disagreement in this study is due to the limited assessment tools utilized. The findings are comparable with one prior study that documented the original use of the EMPOWER measure and demonstrated moderate agreement for FA-related bullying (Shemesh et al., 2013) and other studies of healthy children that indicate adults underestimate bullying (Demaray et al., 2013). Both the intra- and inter-rater results indicate that asking children more specific questions about FA-related bullying leads to more sensitive and comprehensive answers. Supporting this idea, Shemesh et al. (2013) found that when parents knew about FA-related bullying, their child’s QoL was significantly better than those children who experienced FA-related bullying and their parents did not know. Furthermore, some gender differences have been identified regarding different types of victimization.
Among youth who reported FA-related bullying, classmates and other students were the most common perpetrators. However, youth also reported teachers and other school staff being perpetrators of FA-related bullying. Thus, school policies could have an important impact on FA-related bullying and a first direction for intervention could be improving teachers’ awareness of FA-related bullying. Educating teachers on FA-related bullying could play a dual role in reducing the occurrence of teachers and school staff as perpetrators and increasing teachers’ ability to identify and intervene in FA-related bullying when students are perpetrators. A second direction for intervention could be developing a school-based anti-bullying program for FA-related bullying, such as social skills training or whole-school initiatives. These programs have been effective in mitigating bullying in general student populations (Silva et al., 2017), but adaptations for FA-related bullying remain unexplored. In the present study, youth who had experienced FA-related bullying frequently attributed the experience to needing special treatment or being separated and not part of the group, all of which happen at school due to school policies. School policies could be improved to include youth with FAs in meals in a safe manner, so they are not excluded from social interactions.
This study was limited by its inclusion of only English-fluent children and parents. Children and parents whose primary language is not English may experience additional social challenges if in primarily English-fluent settings, but this study did not explore those differences. Other limitations of the study were the lack of a healthy control group, and the cross-sectional design for data collection. Strengths of this study include that it utilized a diverse sample representative of the FA clinic population. The household income level and educational level of the sample were comparable to District of Columbia census data (United States Census Bureau, 2019). Shemesh et al. (2013) found that Hispanic participants with FA were more likely to report FA-related bullying, suggesting that broader racial and ethnic representation in research is important to accurately assess the frequency of victimization. Another study strength was the use of a robust assessment tool. Examining youth and parent reports with the inclusion of thorough descriptive data allowed the researchers to clearly illustrate the prevalence of FA-related bullying and the many contexts in which it occurs.
Conclusion
Assessment of FA-related bullying should routinely be conducted in youth with FA given the consistent prevalence rates demonstrated in this and other studies and the significant safety and psychosocial impacts of FA-related bullying. In order to elicit greater disclosure, youth should be asked directly about their FA-bullying experiences using a multi-item inventory to assess overt and covert bullying behaviors that they may have encountered. Adults who become aware that youth have experienced FA-related bullying should assist youth in addressing the bullying to ensure safety, prevent recurrence, and provide support for the psychosocial impact caused by these experiences. Systemically, this study also demonstrates a need for greater FA education and awareness of FA-related bullying among communities and schools where FA-related bullying is most likely to occur.
Funding
This project was funded by the National Institute of Allergy and Infectious Diseases (NIAID) (5K23AI30184-02) and DC-Baltimore Research Center on Child Health Disparities Award (AWD00001887) awarded to L.H.
Conflicts of interest: None declared.
References
- Annunziato R. A., Rubes M., Ambrose M. A., Mullarkey C., Shemesh E., Sicherer S. H. (2014). Longitudinal evaluation of food allergy-related bullying. The Journal of Allergy and Clinical Immunology. In Practice, 2, 639–641. [DOI] [PubMed] [Google Scholar]
- Blomqvist K., Saarento-Zaprudin S., Salmivalli C. (2020). Telling adults about one's plight as a victim of bullying: tudent- and context-related factors predicting disclosure. Scandinavian Journal of Psychology, 61(1), 151–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulton M. J., Boulton L., Down J., Sanders J., Craddock H. (2017). Perceived barriers that prevent high school students seeking help from teachers for bullying and their effects on disclosure intentions. Journal of Adolescence, 56, 40–51. [DOI] [PubMed] [Google Scholar]
- Brown D., Negris O., Gupta R., Herbert L., Lombard L., Bozen A., Assa'ad A., Chura A., Andy-Nweye A. B., Fox S., Mahdavinia M., Tobin M., Robinson A., Sharma H., Coleman A., Jiang J., Bilaver L., Fierstein J. L., Galic I., Warren C. (2021). Food allergy-related bullying and associated peer dynamics among Black and White children in the FORWARD study. Annals of Allergy. Annals of Allergy, Asthma & Immunology, 126, 255–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casper D. M., Card N. A. (2017). Overt and relational victimization: A meta-analytic review of their overlap and associations with social-psychological adjustment. Child Development, 88, 466–483. [DOI] [PubMed] [Google Scholar]
- Demaray M. K., Malecki C. K., Secord S. M., Lyell K. M. (2013). Agreement among students’, teachers’, and parents’ perceptions of victimization by bullying. Children and Youth Services Review, 35, 2091–2100. [Google Scholar]
- Flannery D. J., Todres J., Bradshaw C. P., Amar A. F., Graham S., Hatzenbuehler M., Masiello M., Moreno M., Sullivan R., Vaillancourt T., Le Menestrel S. M., Rivara F. (2016). Bullying prevention: A summary of the report of the National Academies of Sciences, Engineering, and Medicine. Prevention Science, 17, 1044–1053. [DOI] [PubMed] [Google Scholar]
- Fong A. T., Katelaris C. H., Wainstein B. (2017). Bullying and quality of life in children and adolescents with food allergy. Journal of Paediatrics and Child Health, 53, 630–635. [DOI] [PubMed] [Google Scholar]
- Fong A. T., Katelaris C. H., Wainstein B. K. (2018). Bullying in Australian children and adolescents with food allergies. Pediatric Allergy and Immunology, 29, 740–746. [DOI] [PubMed] [Google Scholar]
- Gupta R. S., Warren C. M., Smith B. M., Blumenstock J. A., Jiang J., Davis M. M., Nadeau K. C. (2018). The public health impact of parent-reported childhood food allergies in the United States. Pediatrics, 142, e20181235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P. A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J. G. (2009). Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42, 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jetelina K. K., Reingle Gonzalez J. M., Cuccaro P. M., Peskin M. F., Pompeii L., Atem F., Elliott M. N., Earnshaw V. A., Davies S. L., Schuster M. A. (2019). Self-reporting discrepancies of bullying victimization and perpetration measures. Annals of Epidemiology, 32, 58–63. [DOI] [PubMed] [Google Scholar]
- Johnson S. F., Woodgate R. L. (2017). Qualitative research in teen experiences living with food-induced anaphylaxis: A meta-aggregation. Journal of Advanced Nursing, 73, 2534–2546. [DOI] [PubMed] [Google Scholar]
- Jones C. J., Llewellyn C. D., Frew A. J., Du Toit G., Mukhopadhyay S., Smith H. (2015). Factors associated with good adherence to self-care behaviours amongst adolescents with food allergy. Pediatric Allergy and Immunology, 26, 111–118. [DOI] [PubMed] [Google Scholar]
- Lieberman J. A., Weiss C., Furlong T. J., Sicherer M., Sicherer S. H. (2010). Bullying among pediatric patients with food allergy. Annals of Allergy, Asthma & Immunology, 105, 282–286. doi:10.1016/j.anai.2010.07.011 [DOI] [PubMed] [Google Scholar]
- Muraro A., Polloni L., Lazzarotto F., Toniolo A., Baldi I., Bonaguro R., Gini G., Masiello M. (2014). Comparison of bullying of food-allergic versus healthy schoolchildren in Italy. The Journal of Allergy and Clinical Immunology, 134, 749–751. [DOI] [PubMed] [Google Scholar]
- Perry T. T., Conover-Walker M. K., Pomes A., Chapman M. D., Wood R. A. (2004). Distribution of peanut allergen in the environment. The Journal of Allergy and Clinical Immunology, 113, 973–976. [DOI] [PubMed] [Google Scholar]
- Shaker M. S., Schwartz J., Ferguson M. (2017). An update on the impact of food allergy on anxiety and quality of life. Current Opinion in Pediatrics, 29, 497–502. [DOI] [PubMed] [Google Scholar]
- Shemesh E., Annunziato R. A., Ambrose M. A., Ravid N. L., Mullarkey C., Rubes M., Chuang K., Sicherer M., Sicherer S. H. (2013). Child and parental reports of bullying in a consecutive sample of children with food allergy. PEDIATRICS, 131(1), e10–e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva J., Oliveira W. A., Mello F., Andrade L. S., Bazon M. R., Silva M. (2017). Anti-bullying interventions in schools: a systematic literature review. Ciencia & Saude Coletiva, 22, 2329–2340. 10.1590/1413-81232017227.16242015 [DOI] [PubMed] [Google Scholar]
- Stives K. L., May D. C., Pilkinton M., Bethel C. L., Eakin D. K. (2019). Strategies to combat bullying: Parental responses to bullies, bystanders, and victims. Youth & Society, 51, 358–376. [Google Scholar]
- United States Census Bureau. (2019). U.S. Census Bureau QuickFacts: District of Columbia, United States. https://www.census.gov/quickfacts/fact/table/DC,US/PST045219. Retrieved 18 July 2021.