Abstract
Background
Patient and family engagement (PFE) has been defined as a partnership between patients, families, and health care providers to achieve positive health care outcomes. There is evidence that PFE is critical to improving outcomes. We sought to systematically identify and map the evidence on PFE strategies for adults with chronic conditions and identify areas needing more research.
Methods
We searched PubMed, CINAHL, EMBASE, and Cochrane, January 2015 to September 2021 for systematic reviews on strategies for engaging patients with chronic conditions and their caregivers. From each review, we abstracted search dates, number and type of studies, populations, interventions, and outcomes. PFE strategies were categorized into direct patient care, health system, and community-policy level strategies. We found few systematic reviews on strategies at the health system, and none at the community-policy level. In view of this, we also searched for original studies that focused on PFE strategies at those two levels and reviewed the PFE strategies used and study findings.
Results
We found 131 reviews of direct patient care strategies, 5 reviews of health system strategies, and no reviews of community-policy strategies. Four original studies addressed PFE at the health system or community-policy levels. Most direct patient care reviews focused on self-management support (SMS) (n = 85) and shared decision-making (SDM) (n = 43). Forty-nine reviews reported positive effects, 35 reported potential benefits, 37 reported unclear benefits, and 4 reported no benefits. Health system level strategies mainly involved patients and caregivers serving on advisory councils. PFE strategies with the strongest evidence focused on SMS particularly for patients with diabetes. Many SDM reviews reported potential benefits especially for patients with cancer.
Discussion
Much more evidence exists on the effects of direct patient care strategies on PFE than on the effects of health system or community-policy strategies. Most reviews indicated that direct patient care strategies had positive effects or potential benefits.
A limitation of this evidence map is that due to its focus on reviews, which were plentiful, it did not capture details of individual interventions. Nevertheless, this evidence map should help to focus attention on gaps that require more research in efforts to improve PFE.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13643-021-01873-5.
Keywords: Engagement, Self-management, Shared decision-making, Patient engagement, Family engagement, Self-management support, Evidence map, Chronic disease
Introduction
Health care providers, governmental agencies, patient advocates, and insurers are increasingly focusing on patient and family engagement (PFE) [1–4]. Their reasons vary from considering engagement as a goal and patient right (e.g., patient’s right to take part in all decisions affecting them), to supporting PFE as a means toward improving outcomes and reducing costs [5–7]. Early on, engagement was defined as actions that patients must take to “obtain the greatest benefit from the health care services available to them” [8]. This conceptualization was later expanded to incorporate health care professionals’ and systems’ “actions, interventions, and supports” that promote successful engagement [5, 7–9]. Recently, Carmen et al. further defined PFE as patients, families, and health care providers “working in active partnership at various levels”, including direct care, organizational design and governance, and policy-making to help improve health care outcomes [10]. Carman et al. described a continuum of PFE with activities ranging from basic information sharing (e.g., providers offering information during visits and patients providing feedback on health services) to shared authority and co-leadership of improvement efforts [10]. Increasingly, health care systems are making efforts to engage patients and families to improve patients’ outcomes and experiences [1, 11, 12]. Many hospitals have established patient and family advisory councils [11], and PFE strategies have been incorporated into new primary care models including the Patient Centered Medical Home and the Comprehensive Primary Care Initiative of the Centers for Medicare and Medicaid Services [13, 14].
Studies have demonstrated that engaged patients have better outcomes and lower acute care use [15], and that low levels of engagement are associated with more adverse events [16]. Despite its benefits, not all patients have the capacity to become engaged in their care. Family-caregiver engagement is particularly important to support vulnerable patients including children, the elderly, people at the end of life, and people with disabilities [17, 18].
PFE is particularly relevant for patients with chronic conditions [19]. About 60% of adults in the USA have at least 1 chronic condition, and 4 in 10 adults have two or more [20]. The Chronic Care Model emphasizes the need for an “informed activated patient” to improve outcomes [19, 21]. The increasing complexity of health care places more demands on these patients (e.g., to handle multiple appointments, choose health insurances, make treatment decisions, and self-manage chronic conditions). Supporting patients to meet their goals is consistent with delivering patient-centered care [19]. Engagement strategies that have been studied among people with chronic conditions include self-management support (SMS) interventions, such as programs that enable patients to work with nurses and diabetes educators to advance their glucose monitoring and medication management skills [22–28]; technology-based solutions, such as patient access to the electronic health record and facilitating communication with providers through patient portals [29, 30] and interventions to improve clinicians’ communication skills and shared decision-making (SDM) [31–35].
Health care providers and health systems are particularly invested in identifying and advancing effective PFE strategies to support patients with chronic conditions and improve their health outcomes. However, there are no clear guidelines or summary evidence to inform decision-making by health system leaders on which strategies to deploy to achieve successful engagement and improve outcomes for patients. To help address this gap, the Agency for Healthcare Research and Quality (AHRQ) commissioned a review to create a map of the evidence on PFE strategies used to help patients with chronic conditions and identify areas in need of further research.
Methods
Given the wide range of PFE strategies being researched, we used an evidence mapping approach. Unlike other systematic reviews, evidence maps tackle broad questions and provide a framework to understand key components of the strategies of interest [36–38]. Rather than focusing on describing specific studies, evidence maps use tables and visuals to summarize evidence and enable policy-makers to then refer to specific studies [36–38].
The full-review protocol, methods, and evidence map are described elsewhere [39]. In this paper, we focus on the findings for adults with chronic conditions.
Our review questions were the following:
What engagement strategies have been studied to help patients, families, and caregivers manage their chronic conditions and improve patient health outcomes?
What gaps exist in the current research?
To inform our approach, we conducted meetings with key informants, including patients, caregivers, providers, insurers, and researchers, and sought their perspectives on the protocol.
Conceptual framework
We adapted a PFE framework developed by Carman et al. that categorized PFE strategies according to whether they focused on engaging people at the direct patient care , health system, or community-policy levels (Fig. S1) [5]. While a PFE strategy at direct patient care level helps engage patients in their own care, a health system level strategy engages patients in efforts that have an impact beyond their own health care, such as improving health care quality, and a community-policy level strategy engages patients in developing health care policies [5]. According to this framework, robust engagement at all levels is necessary to improve patient outcomes. Engagement at the health system and community-policy levels contributes to development of more patient-centered health care delivery. In turn, patients, caregivers, and providers are able to work effectively together to address system-level barriers that undermine patient’s ability to follow treatment plans and adopt the recommended health behaviors to improve outcomes. Table 1 provides the definitions we used in this review.
Table 1.
Definitions
| Patient and Family Engagement (PFE) | Patients, families, their representatives, and health professionals working in active partnership at various levels across the health care system—direct care, organizational design and governance, and policymaking—to improve health and health care” [ 5 ]. In addition, we used the term PFE to represent engagement of the patient and family, as well as non-family caregivers, who the patient deems part of his or her care. |
| Chronic diseases | Conditions that last 1 year or more and require ongoing medical attention or limit activities of daily living or both.” |
| PFE levels | Direct patient-care level strategy is a strategy that directly inform the patients’ own treatment decisions, health behaviors, or outcomes; a health system level strategy is one that engages patients in efforts that have an impact beyond their own health care such as improving health care quality; community-policy level strategy is one that engages patients, consumers, or citizens in policymaking or that engages communities in health care policies. |
| Benefits categorization for reported findings | ‘Positive effects’ describe a study where the authors made clear unequivocal statements about an overall positive effect of the reviewed interventions; ‘potential benefits’ reported when the authors mentioned likely benefits; ‘unclear benefits’ when the authors were inconclusive; and ‘harms’ when the authors reported harm from the reviewed interventions. |
We defined the eligibility criteria for studies using the PICOTS (Population, Intervention, Comparison, Outcomes, Timing, and Setting) framework (Table 2) [39].
Table 2.
Inclusion and exclusion criteria
| PICOTS | Include | Exclude |
|---|---|---|
| Population |
• Patients with chronic medical conditions • Patient and family members of committees/councils aimed at improving care • Subpopulations, including • Ethnic and racial minority • Limited language skills • Low literacy/low health literacy • Cognitive impairment |
None |
| Interventions |
• Direct patient level interventions • Practice, health system, and reimbursement interventions • Models under alternative payment mechanisms • Community-level interventions |
• One-time education-only (e.g., providing a handout) • Without 2-way interaction or ability for patient to ask questions (e.g., providing access to web-based educational program) |
| Comparators | Any comparator (pre/post, concurrent) | No comparison group |
| Outcomes |
• Intermediate outcomes (e.g., behavior change, cost, provider satisfaction, health system level changes) • Patient outcomes (e.g., mortality, quality of life, utilization) |
None |
| Timing |
All timing • Right after implementation strategy (within 3 months) • Longer follow-up |
|
| Setting | All settings where self-management occurs (e.g., home/community/clinic/assisted living) | Non-USA-based studies |
We aimed to include a wide variety of PFE interventions, based on previously reported definitions and the multi-dimensional perspectives of stakeholders on this topic. Study designs with comparator groups were included (e.g., pre/post and concurrent designs). Outcomes of interest included both intermediate outcomes (e.g., behavior change, cost, provider satisfaction, health system level changes) and clinical outcomes (e.g., mortality, quality of life, hospitalizations). We excluded direct patient care interventions that were unidirectional or involved “basic consultation” on the PFE continuum [10]. For example, we excluded interventions involving a one-time education handout, or online informational programs that did not allow patients to ask questions. Also, health system and community-policy level interventions that only included patients and family members as study subjects (e.g., participants in focus groups and surveys) were not considered PFE interventions.
Data sources and searches
Given the large body of evidence, we focused our search on systematic reviews, with supplemental searches for original research articles in areas having a paucity of reviews. We included search terms for patient/family/consumer engagement, participation, involvement, activation, or empowerment, as well as terms describing engagement interventions based on the study’s conceptual framework and prior publications in this area (Table S1—Search strategy). We searched the following databases; PubMed, CINAHL, EMBASE, and Cochrane from January 2015 through September 2021 for systematic reviews. Because the majority of reviews on PFE strategies focused on direct care level, we conducted another search (using the same terms) to identify relevant original studies on health system and community-policy level strategies. We screened the search output (title/ abstract then full text) and included original studies on PFE strategies at the system and community levels.
Study selection
Search results were screened independently by two team members, first at the abstract level and then at the full-text level. Discrepancies were resolved by consensus, or by a third reviewer if consensus could not be achieved. To be included, we required systematic reviews to address the research question, be published after 2015, and provide details of their search strategy. For original research articles we excluded those without comparison groups.
Data extraction and synthesis
The included systematic reviews were reviewed by two team members. Author, publication year, search dates, number and type of included studies, populations, intervention characteristics, quality assessment, measured outcomes, and findings from each eligible review were abstracted. If the two reviewers disagreed, conflicts were resolved by discussion and consensus . PFE strategies were categorized into those at the direct patient care, health system, and community-policy levels, and for each study the reviewers identified whether it reported positive effects, potential benefits, unclear benefits, no benefits, or harms (see Table 1 for definitions). An evidence table was compiled with the characteristics of each included systematic review and its reported findings. Data was then depicted in summary tables that reported on studied chronic conditions, tested interventions, and reported outcomes.
A similar process was followed to abstract information from the included original articles. An evidence map was then constructed to visually represent available evidence. The map along with the summary tables for systematic reviews helped reveal where evidence is most abundant and where it is lacking.
Results
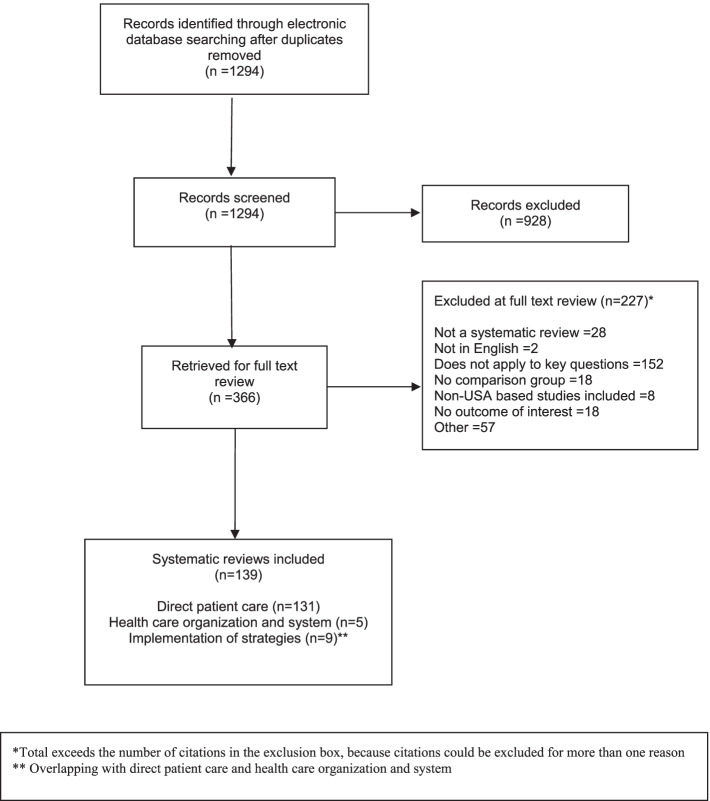
The systematic review search identified 1294 references and 366 references were selected for full-text review. Of those 139 systematic reviews reported PFE strategies among adults with chronic conditions (Fig. 1). The original articles search identified 8192 references and 280 references were selected for full-text review. Of those 3 were original articles of PFE strategies at the health system level and one at the community-policy level (Fig. S2).
Fig. 1.
PRISMA flow diagram
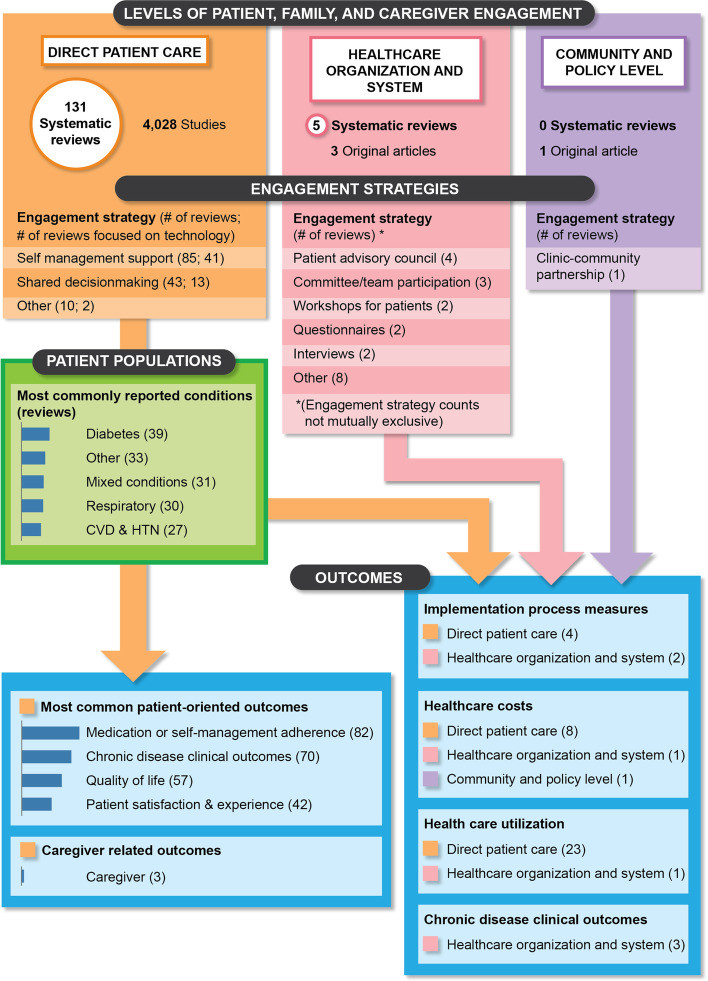
Figure 2 maps the available evidence by level of engagement and displays the numbers of systematic reviews of PFE strategies by engagement type (e.g., SMS, SDM), chronic condition, and measured outcomes. Overall, 131 reviews focused on the direct patient care level of engagement, five on the health system level, and none on the community-policy level.
Fig. 2.
Map of the evidence on patient and family engagement strategies among adults with chronic conditions by level of engagement
PFE at the direct patient-care level
Out of the 131 reviews on direct patient care level engagement strategies, 85 focused on SMS, and 43 focused on SDM or enhanced patient-provider communication. Table S2 depicts characteristics of all included systematic reviews at direct care level by intervention type. Table 3 depicts the chronic medical conditions targeted in the direct patient care reviews, by intervention modalities and reported outcomes.
Table 3.
Chronic medical conditions targeted in systematic reviews, intervention modalities, and reported outcomes by intervention type
| Interventions (no. of reviews)* |
Clinical focus (no. of reviews) |
Outcomes reported (no. of reviews) |
Intervention modality (no. of reviews) |
|---|---|---|---|
| Self-management education and support (85) |
- Multiple conditions** (9) - Mix of conditions included (22) - Diabetes (34) -CVD and hypertension (23) - Respiratory (27) - Cancer or cancer screening (12) - Mental health (12) - Other (23) |
- Chronic disease clinical outcomes (56) - Decisional support outcome (3) - Health care utilization (18) - Medication or self-management adherence (65) - Mortality (2) - Patient satisfaction/experience (20) - Quality of life (38) |
- Community health worker/patient navigator (1) - Education/counseling (11) - Mobile health (15) - Nurse/case managers (24) - Patient portal (8) - Peer/lay support (7) - Team-based care (1) - Telehealth (3) - Multiple modalities (13) - Multiple technologies (12) - Other technology (3) - Other (2) |
| SDM(43) |
- Multiple conditions**(5) - Mix of conditions included (11) - Diabetes (4) - CVD and hypertension (2) - Respiratory (2) - Cancer or cancer screening (13) - Mental health (4) - Other (8) |
- Chronic disease clinical outcomes (13) - Decisional support outcome (36) - Health care utilization (4) - Medication or self-management adherence (18) - Mortality (0) - Patient satisfaction/experience (22) - Quality of life (15) |
- Education/counseling (16) - Mobile health (1) - Nurse/case managers (10) - Patient portal (2) - Telehealth (1) - Multiple modalities (13) - Multiple technologies (2) - Other technology (8) - Other (8) |
| Other (10) |
- Multiple conditions** (1) - Mix of conditions included (2) - Diabetes (2) - CVD and hypertension (2) - Respiratory (2) - Cancer or cancer screening (0) - Mental health (1) - Other (2) |
- Chronic disease clinical outcomes (4) - Decisional support outcome (2) - Health care utilization (3) - Medication or self-management adherence (2) - Mortality (2) - Patient satisfaction/experience (2) - Quality of life (6) |
- Education/counseling (6) - Nurse/case managers (2) - Peer/lay support (2) - Multiple modalities (5) - Other technology (1) - Other (3) |
*Six reviews addressed more than one intervention type; **Multiple conditions refer to reviews of patients who have multimorbidity/comorbidity, CVD = cardiovascular disease
Fifty-seven of the 131 reviews focused on studies using mobile health, electronic health record tools, or web-based programs for PFE. Diabetes mellitus was the most studied chronic condition.
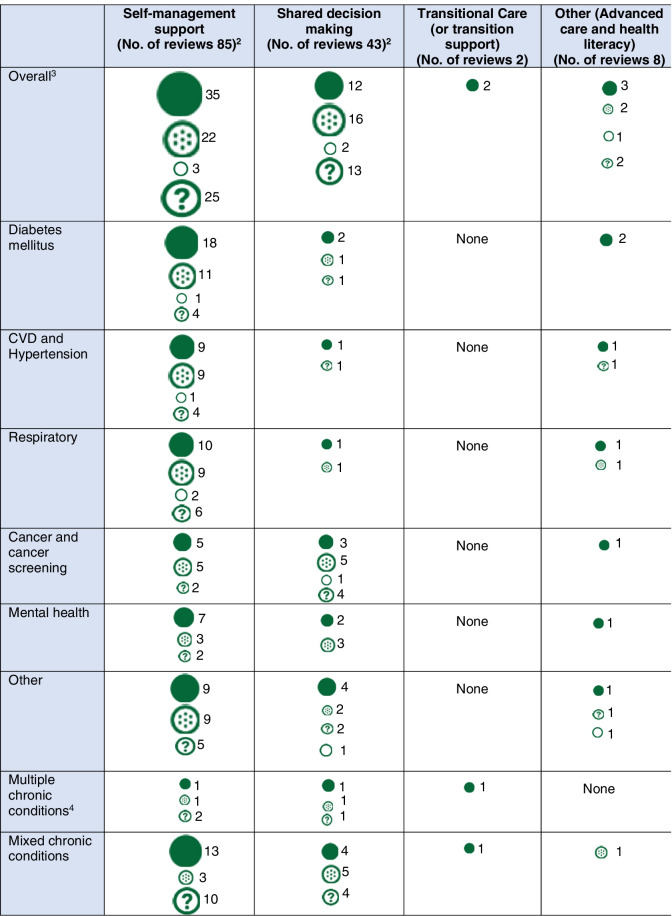
Table 4 depicts findings on the benefits of direct PFE, by intervention type and health condition. The reviews that most frequently reported benefits addressed SMS for diabetes and cardiovascular disease, and reviews of SDM for cancer screening and treatment.
Table 4.
Benefits of patient and family engagement interventions at the direct care level, as reported in systematic reviews, by engagement type and health condition
Interpretation:
 Positive effects
Positive effects
 Potential benefits
Potential benefits
 No benefits
No benefits
 Unclear benefits
Unclear benefits
1 Circle size is based on total number of reviews
2Unclear benefits—in five reviews of self-management and 1 review of shared decision-making, the review question was not about evaluating outcomes (see Table S2 Reviews # 22, 105, 160, 495, 352, 545)
3Total exceeds the number for overall because reviews could be included for more than one condition
4Multiple conditions refer to reviews of patients who have multimorbidity/comorbidity
PFE strategies including Self-management support
We identified 85 reviews evaluating SMS strategies for adults. The number of original studies in the reviews ranged from 2 to 488, with 0 to 105 being randomized controlled trials. The most frequently reviewed chronic conditions were diabetes mellitus (n = 34), respiratory disorders (n = 27), and cardiovascular disease including hypertension (n = 23) (Table 3).
SMS strategies were mostly tested within multi-component interventions. These strategies included (1) education and information sharing on condition and treatment options; (2) helping patients with goal-setting, self-monitoring and symptom management, using action plans, problem-solving, tracking data and feedback; (3) using reminders and alerts, remote monitoring, and decision support to facilitate patient-provider communication and adherence; (4) providing psychosocial support including health care navigation assistance, connection to social services and peers, counseling and cognitive behavioral therapy.
The most frequently reported outcomes were adherence to medication or self-management tasks (reported in 65 reviews), chronic disease control measures (56 reviews), quality of life (38 reviews), patient satisfaction or experience (20 reviews), and health care utilization (18 reviews). Thirty-five reviews reported positive effects, 22 reported potential benefits, 25 reported unclear benefits, and 3 reported no benefits. None reported any harms. Among the 34 reviews focused on SMS in diabetes, 18 reported positive effects and 11 reported potential benefits. These benefits were frequently reported for measures of glycemic control and medication adherence. Cost benefits for SMS interventions were reported in three reviews [40–42].
Two large reviews focused on SMS interventions for low-income, underserved, and minority patients [43, 44]. The first review examined community health center-based interventions for patients with diabetes and reported significant improvement in glucose control when interventions included in-person individual or group education sessions with phone follow-up. SMS interventions that were fully telephone-based showed no significant improvements [43]. The second review focused on community-based health worker interventions among vulnerable populations and reported evidence of cost-effectiveness in self-management of selected health conditions including hypertension and diabetes [44].
Two reviews of studies of patients with multiple chronic conditions reported that SMS had unclear benefits, possibly due to complexity of self-management of multiple chronic conditions and reduced chances for SMS to help these patients [45, 46]. There were three reviews of studies involving caregivers. One of those, included nine RCTs of self-care interventions for patients with various chronic conditions and their caregivers [47], and showed a reduction in rehospitalizations. Another reviewed telehealth interventions involving caregivers and reported better psychological health and reduced burden for caregivers [48]. Seven reviews focused on patient self-management via patient portals and secure messaging systems [49–55]. One of these reviews explored impact on diabetes control (hemoglobin A1c level), and reported that 7 out of 11 included studies demonstrated lower hemoglobin A1c levels with the use of secure messaging [55].
PFE strategies including SDM and patient-provider communication
Forty-three reviews evaluated SDM or patient-provider communication. The number of original studies in reviews ranged from 4 to 488 original studies, with 1 to 105 RCTs. The chronic conditions most studied were cancer screening or treatment (n = 13), multimorbidity (n = 5), and mental health conditions (n = 4). SDM interventions often involved multiple components, including provider training and patient education tools, and the interventions used technology-enabled delivery modes and decision supports (Table 2). Frequently reported outcomes were decisional support outcomes (n = 36) (e.g., decisional conflict measures), and patient satisfaction or experience (n = 22). There were no reports on mortality and few on health care utilization (n = 4). Twelve showed positive effects,16 showed potential benefits, 13 showed unclear benefits, and 2 showed no benefits.
A large Cochrane review (n = 115 studies) broadly assessed decision aids for people with chronic diseases facing treatment or screening decisions [56]. The review reported high- and moderate-quality evidence of improved knowledge, reduced decisional conflict, more engagement in decision-making, and fewer people choosing discretionary surgery [56].
Four reviews evaluated SDM strategies for advanced care planning and reported a shortage of studies in this area [57–60]. One reported beneficial effects on patients or surrogate decision-makers’ knowledge [58]. Two reviews examined the role of the electronic health record’s patient portal or secure messaging system as a PFE strategy to enhance patient-provider communication [54, 61]. Evidence of benefits were inconclusive. One review reported provider perceptions that releasing abnormal or sensitive test results to patients through the electronic health record could cause confusion or excess worry for patients, but there was no systematic measurement of harm in that review [54]. Cancer screening and treatment were the most studied condition for the SDM reviews, with three reviews showing positive effects [62–64] and 5 reporting potential benefits [65–69]. Two recent reviews reported unclear benefits [70, 71]. One review identified 10 studies focused on cancer treatment decision-making specifically for patients from racial and ethnic minority backgrounds, and showed improved patient engagement outcomes (i.e., higher satisfaction, improved communication) [64] (Table S2).
Other direct care PFE strategies
We identified six reviews that focused on engagement around care transitions [72, 73], personalized care planning [74, 75], educational programming for patients undergoing peritoneal dialysis [76], and digital health coaching [77]. One other review examined health literacy and patient activation elements of self-management interventions for patients with COPD [78].
PFE at the health system level
We identified five reviews [79–83] and three original articles [84–86] that focused on PFE at the health system level. Most commonly addressed chronic conditions were mental health [79, 81, 83], cancer [81, 83], diabetes mellitus [79, 81], and neurologic conditions [81, 83]. The most commonly reported strategies to engage patients at the system level included assembling patient and family advisory councils [79, 81–83], and including patients on committees [81–83], and in forums and workshops [80, 81] and involving patients as educators for medical trainees [80]. Report on impact of PFE at system level were limited to changes in the process of care, policies, documents, and tools. Sharma and colleagues conducted a review of the impact of patient advisors [83]. They reported impact on clinics’ priority setting in one cluster RCT and found no studies with robust designs that reported on clinical outcomes or patient satisfaction [83]. Another review of patient and family advisory councils by Oldfield et al also reported a “paucity of RCTs or high-quality observational studies” [79].
PFE at the community-policy level
We did not find any reviews on PFE engagement at the community-policy level. We identified one original article that described community-policy level engagement using community advisory councils at the Indian Health Service [87].
Gaps in evidence
Figure 2 provides an evidence map that highlights the overall findings about the existing evidence. Compared with direct patient care strategies, fewer reviews addressed health system level strategies (n = 5) and even when we augmented the search to identify original studies, very few studies (n = 3) met our inclusion criterion of having a comparison group. No reviews were found on community-policy level engagement. Five reviews focused on PFE strategies for advanced care planning, and reported inconsistent conclusions [57–60, 75]. Only one review focused on interventions that address health literacy elements, and this review was restricted to SMS interventions for patients with COPD [78]. Few direct patient care reviews focused on patients with multiple chronic conditions (n = 15), and vulnerable populations such as urban or rural, minority, low income, or older adults (n = 15). Few reviews reported on caregiver outcomes, health care utilization, or cost.
Discussion
Increasingly, patients and caregivers play key roles not only in managing their own health and health care, but also in contributing to health care system improvement. Given the broad and multi-dimensional scope of PFE, it is not surprising that we found a great deal of heterogeneity among included studies. This is consistent with the recent position paper by the American College of Physicians, “Principles for Patient and Family Partnership in Care,” which highlighted that the meaning of PFE vastly differs by setting, scale, and intended outcomes [1].
This study was conducted to address the information needs of health care leaders on PFE. Given its broad scope, we provided a high-level examination of the evidence on the effects of PFE strategies across a range of chronic diseases and at various levels for engagement. Our findings are consistent with earlier reviews on benefits of PFE strategies at the direct care level on patient outcomes. The evidence map reinforces that there is a need for more high quality evidence on the impact of PFE on health care costs, and the impact of PFE at the health system and policy levels [81, 88, 89].
The evidence map showed that most of the evidence for PFE is at the direct patient care level, with the most studied interventions being on SMS and SDM. The reviews varied in terms of studied chronic diseases (diabetes was the most studied), and clinical settings and modalities for engagement. Strategies with the most frequently reported evidence for effectiveness were SMS interventions, particularly among patients with diabetes. Despite the large number of reviews, we identified inconsistent findings for the benefits of SMS and SDM strategies, sometimes among studies of patients with the same chronic conditions. This is in part due to the heterogeneity of tested interventions, different measures used, and varying quality of the original studies. Most measured anticipated outcomes of engagement including adherence to chronic disease self-management behaviors, clinical outcomes, health care utilization, and patient satisfaction and experience. Measurement of the engagement process and the extent of patient engagement in studied interventions were largely lacking. The latter requires use of validated PFE measures that are specific for patients with various chronic conditions. The need for development of more measures in these areas is increasingly being recognized [89–92]. Although the PFE interventions in principle aim to advance engagement, the lack of assessment of the engagement process makes it impossible to fully assess the merits of various interventions. Furthermore, the extent of engagement likely affects achievement of intended outcomes from studied interventions and may explain the inconsistency in reported findings among studies [9, 93].
The evidence map identified 46 reviews focused on using technology as part of the engagement strategy. The use of patient portals was influenced by patients’ age, ethnicity, education level, health literacy, health status, provider endorsement, and portal usability [61]. More studies are needed that explore ways by which technology can be leveraged in a manner that addresses barriers to its use by patients.
Few studies reported on caregiver measures, which reflected the overall paucity of studies looking at effects of PFE on caregivers. We also found few reviews on decision-making for older adults, advanced care planning and end of life care, compared to other areas of PFE suggesting the need for more focus on this area. Reports on cost-effectiveness of PFE strategies were sparse. More evidence in this area is essential for health care leaders and policy-makers to make the financial case for funding of programs that advance PFE within health systems.
To our knowledge, this is the first systematic review to address PFE strategies focused on health system and community-policy level strategies, in addition to direct patient care level strategies. Similar to our review, the systematic review by Coulter and colleagues included direct-patient care engagement strategies and identified many studies focused on SMS, as well as clinical decision-making through patient-provider communication strategies [9]. Sharma and colleagues conducted a review of PFE strategies specifically related to patient safety and identified only one review with a health system level engagement strategy [93]. One of the principles of the learning health system is to “promote the inclusion of patients as vital members of the learning team,” making it important to identify best practices and high-quality evidence to select strategies that not only engage patients but also lead to improvements in care quality and value [94]. Despite the enthusiasm about increasing patient engagement at a system level and calls to make it an expectation, our evidence map identified a paucity of rigorous studies about the effectiveness and implementation of PFE strategies at the health system level. Though it is not feasible to implement RCTs to assess effectiveness of system level strategies, it is feasible to use other research designs including cluster randomization, stepped-wedge trial, and pre-post designs with comparison groups.
The evidence map highlighted that among various PFE strategies, SMS interventions, particularly for patients with diabetes, have benefits for patients and should be integrated into clinical settings. To accomplish this, health care systems need to promote and provide SMS services for patients with diabetes and other chronic conditions in an equitable manner, addressing social determinants of health and barriers for vulnerable populations (e.g., attention to the needs of patients with low literacy, addressing transportation barriers). Reimbursement policies that enable provision of these services in an equitable and sustainable manner are needed. Furthermore, the evidence map shows that many reviews of SDM interventions, particularly among patients with cancer, showed potential benefits especially for patient satisfaction. More studies are needed that examine interventions that are likely to be successfully implemented and sustained by health care professionals and patients with cancer and other preference sensitive conditions. Studies on SDM with older adults and people living with dementia are also needed.
Our study has several strengths. First, to our knowledge, this is the first review to address PFE strategies at the levels of direct patient care, health system, and community/policy. Second, given the widespread implementation of electronic health records and the proliferation of mobile phone applications in recent years, an important contribution of our map was the identification of many reviews focused on using technology as part of the engagement strategy. Third, this review took a broad and inclusive approach for reviewing PFE strategies in response to the different needs and perspectives of the multiple stakeholders who are interested in PFE and its advancement in clinical settings.
Our study has several limitations. First, given the broad scope of PFE, we focused on synthesizing findings from systematic reviews, rather than from all original studies. For each of the included systematic reviews we reported on the total count of primary studies, the medical conditions studied, the outcomes measured, the intervention types and modalities and the findings. Given the aim and broad scope of this paper, we did not abstract specific information about the tested interventions, which were often not available from systematic reviews. Thus, our study offers an evidence map that allows for health care leaders to quickly identify areas and populations where benefits from PFE interventions have been consistently reported and to consider how they might implement these strategies into their health systems. Second, we excluded articles and reviews explicitly focused on patient engagement in research studies. Third, we may have missed some exemplars of community-policy level engagement, as few of these articles met inclusion criteria for having a comparison group or including outcomes of interest [95–104].
In conclusion, we identified a large body and diversity of evidence on direct patient care level engagement strategies, most of which indicated positive effects or potential benefits. We also found multiple gaps in evidence that call for more research on strategies to engage patients with chronic conditions and their caregivers, especially at the health system and community levels.
Supplementary Information
Additional file 1: Figure S1. Patient, family, and caregiver engagement conceptual framework. Table S1. PubMed Search Strategy. Figure S2. Search flow diagram for original studies. Table S2. Characteristics of included systematic reviews on PFE strategies at the direct patient care level and their findings.
Acknowledgements
This project was funded under Contract No. HHSA2902015000061 from the Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services. The authors of this report are responsible for its content. Statements in the report should not be construed as endorsement by the Agency for Healthcare Research and Quality or the U.S. Department of Health and Human Services.
Disclaimer
This project was funded under Contract No. HHSA290-2015-00006-I, Task Order. 75Q80119F32015, from the AHRQ of the US Department of Health and Human Services (HHS).
The findings and conclusions in this document are those of the author(s), who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services.
Abbreviations
- PFE
Patient and family engagement
- SMS
Self-management support
- SDM
Shared decision-making
- RCTs
Randomized controlled trials
- AHRQ
Agency for Healthcare Research and Quality
- PICOTS
Population, Intervention, Comparison, Outcomes, Timing, and Setting
Authors’ contributions
HA wrote the manuscript with support from WB, SP, and RS. HA, WB, SP, and EB developed the main conceptual ideas and review approach. All authors participated in data abstraction and/or synthesis, provided critical feedback, helped shape the report on review findings, and contributed to the final manuscript.
Funding
Agency for Healthcare Research and Quality
Availability of data and materials
Not applicable
Declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nickel WK, Weinberger SE, Guze PA. Principles for Patient and Family Partnership in Care: An American College of Physicians Position Paper. Ann Intern Med. 2018;169(11):796–799. doi: 10.7326/M18-0018. [DOI] [PubMed] [Google Scholar]
- 2.Clancy CM. Patient engagement in health care. Health Serv Res. 2011;46(2):389–393. doi: 10.1111/j.1475-6773.2011.01254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patient engagement, patient safety, and quality of care. Health Aff. 2013;32(2):432-5. https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2013.0021. Accessed 8 Jan 2022. [DOI] [PubMed]
- 4.CMS. Person and family engagement. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/Person-and-Family-Engagement. Accessed 8 Jan 2022.
- 5.Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff. 2013;32(2):223–231. doi: 10.1377/hlthaff.2012.1133. [DOI] [PubMed] [Google Scholar]
- 6.Charmel PA, Frampton SB. Building the business case for patient-centered care. Healthc Financ Manage. 2008;62(3):80–85. [PubMed] [Google Scholar]
- 7.“Health policy brief: patient engagement”, Health Affairs. https://www.healthaffairs.org/do/10.1377/hpb20130214.898775/full/. Accessed 8 Jan 2022.
- 8.Gruman J, Rovner MH, French ME, Jeffress D, Sofaer S, Shaller D, et al. From patient education to patient engagement: implications for the field of patient education. Patient Educ Couns. 2010;78(3):350–356. doi: 10.1016/j.pec.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. BMJ. 2007;335(7609):24–27. doi: 10.1136/bmj.39246.581169.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Threnhauser S. OPEN MINDS -from consumer engagement to consumer activation. 2018. [Google Scholar]
- 11.Herrin J, Harris KG, Kenward K, Hines S, Joshi MS, Frosch DL. Patient and family engagement: a survey of US hospital practices. BMJ Qual Saf. 2016;25(3):182–189. doi: 10.1136/bmjqs-2015-004006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Institute of M . The national academies collection: reports funded by national institutes of health. In: Olsen LA, Saunders RS, McGinnis JM, editors. Patients charting the course: citizen engagement and the learning health system: workshop summary. Washington (DC): National Academies Press (US) National Academy of Sciences; 2011. [PubMed] [Google Scholar]
- 13.CMS CPCI. https://innovation.cms.gov/initiatives/comprehensive-primary-care-initiative/. Accessed 8 Jan 2022.
- 14.PCMH standards and guidelines. 2017. https://fdocuments.in/document/pcmh-standards-and-pcmh-standards-and-pcmh-standards-and-guidelines-2017.html. Accessed 8 Jan 2022.
- 15.Remmers C, Hibbard J, Mosen DM, Wagenfield M, Hoye RE, Jones C. Is patient activation associated with future health outcomes and healthcare utilization among patients with diabetes? J Ambul Care Manage. 2009;32(4):320–327. doi: 10.1097/JAC.0b013e3181ba6e77. [DOI] [PubMed] [Google Scholar]
- 16.Weingart SN, Zhu J, Chiappetta L, Stuver SO, Schneider EC, Epstein AM, et al. Hospitalized patients’ participation and its impact on quality of care and patient safety. Int J Qual Health Care. 2011;23(3):269–277. doi: 10.1093/intqhc/mzr002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patient- and family-centered care and the pediatrician’s role. Pediatrics 2012;129(2):394-404. [DOI] [PubMed]
- 18.Conway JB, Edgman-Levitan S, Schlucter J, Ford D, Sodomka P, Simmons L. Partnering with patients and families to design a patient- and family-centered health care system: a roadmap for the future, a work in progress. Bethesda; 2006. https://www.ipfcc.org/resources/Roadmap.pdf. Accessed 8 Jan 2022.
- 19.Wagner EH, Bennett SM, Austin BT, Greene SM, Schaefer JK, Vonkorff M. Finding common ground: patient-centeredness and evidence-based chronic illness care. J Altern Complement Med. 2005;11(Suppl 1):S7–15. doi: 10.1089/acm.2005.11.s-7. [DOI] [PubMed] [Google Scholar]
- 20.Chronic Diseases in America. Centers for disease control and prevention, https://www.cdc.gov/chronicdisease/resources/infographic/chronic-diseases.htm. Published October 23, 2019. Accessed 19 May 2020.
- 21.Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. Ann Intern Med. 1997;127(12):1097–1102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- 22.Rost K, Nutting P, Smith JL, Elliott CE, Dickinson M. Managing depression as a chronic disease: a randomised trial of ongoing treatment in primary care. BMJ. 2002;325(7370):934. doi: 10.1136/bmj.325.7370.934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lorig KR, Sobel DS, Stewart AL, Brown BW, Jr, Bandura A, Ritter P, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999;37(1):5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Greenfield S, Kaplan SH, Ware JE, Jr, Yano EM, Frank HJ. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3(5):448–457. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 25.Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National standards for diabetes self-management education. Diabetes Care. 2012;35(Suppl 1):S101–S108. doi: 10.2337/dc12-s101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fitzpatrick SL, Schumann KP, Hill-Briggs F. Problem solving interventions for diabetes self-management and control: a systematic review of the literature. Diabetes Res Clin Pract. 2013;100(2):145–161. doi: 10.1016/j.diabres.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Effing T, Monninkhof EM, van der Valk PD, van der Palen J, van Herwaarden CL, Partidge MR, Walters EH, Zielhuis GA. Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2007;(4):CD002990. 10.1002/14651858.CD002990.pub2. Update in: Cochrane Database Syst Rev. 2014;3:CD002990. [DOI] [PubMed]
- 28.Bayliss EA, Ellis JL, Steiner JF. Barriers to self-management and quality-of-life outcomes in seniors with multimorbidities. Ann Fam Med. 2007;5(5):395–402. doi: 10.1370/afm.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vo V, Auroy L, Sarradon-Eck A. Patients’ perceptions of mhealth apps: meta-ethnographic review of qualitative studies. JMIR mHealth uHealth. 2019;7(7):e13817. doi: 10.2196/13817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Broderick A, Haque F. Mobile health and patient engagement in the safety net: a survey of community health centers and clinics. Issue Brief (Commonw Fund). 2015;9:1-9. [PubMed]
- 31.Entwistle VA, McCaughan D, Watt IS, Birks Y, Hall J, Peat M, et al. Speaking up about safety concerns: multi-setting qualitative study of patients’ views and experiences. Qual Saf Health Care. 2010;19(6):e33. doi: 10.1136/qshc.2009.039743. [DOI] [PubMed] [Google Scholar]
- 32.Griffin SJ, Kinmonth AL, Veltman MW, Gillard S, Grant J, Stewart M. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trials. Ann Fam Med. 2004;2(6):595–608. doi: 10.1370/afm.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):S110–S127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 34.Peat M, Entwistle V, Hall J, Birks Y, Golder S. Scoping review and approach to appraisal of interventions intended to involve patients in patient safety. J Health Serv Res Policy. 2010;15(Suppl 1):17–25. doi: 10.1258/jhsrp.2009.009040. [DOI] [PubMed] [Google Scholar]
- 35.Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163(1):83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 36.Snilstveit B, Vojtkova M, Bhavsar A, Stevenson J, Gaarder M. Evidence & gap maps: a tool for promoting evidence informed policy and strategic research agendas. J Clin Epidemiol. 2016;79:120–129. doi: 10.1016/j.jclinepi.2016.05.015. [DOI] [PubMed] [Google Scholar]
- 37.Polisena J, Garritty C, Kamel C, Stevens A, Abou-Setta AM. Rapid review programs to support health care and policy decision making: a descriptive analysis of processes and methods. Syst Rev. 2015;4:26. doi: 10.1186/s13643-015-0022-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parkhill AF, Clavisi O, Pattuwage L, Chau M, Turner T, Bragge P, et al. Searches for evidence mapping: effective, shorter, cheaper. J Med Libr Assoc. 2011;99(2):157–160. doi: 10.3163/1536-5050.99.2.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bennett WL, Pitts S, Aboumatar H, et al. Strategies for patient, family and caregiver engagement. Technical Brief. (Prepared by the Johns Hopkins University Evidence-based Practice Center under Contract No. HHSA290201500006I.) AHRQ Publication No. XX-EHCXXX-EF. Rockville, MD: Agency for Healthcare Research and Quality. UNDER REVIEW.
- 40.van Eeden M, van Heugten CM, van Mastrigt GA, Evers SM. Economic evaluation studies of self-management interventions in chronic diseases: a systematic review. Int J Technol Assess Health Care. 2016;32(1-2):16–28. doi: 10.1017/S0266462316000027. [DOI] [PubMed] [Google Scholar]
- 41.Teljeur C, Moran PS, Walshe S, Smith SM, Cianci F, Murphy L, et al. Economic evaluation of chronic disease self-management for people with diabetes: a systematic review. Diabet Med. 2017;34(8):1040–1049. doi: 10.1111/dme.13281. [DOI] [PubMed] [Google Scholar]
- 42.Smalley KR, Aufegger L, Flott K, Mayer EK, Darzi A. Can self-management programmes change healthcare utilisation in COPD?: A systematic review and framework analysis. Patient Educ Couns. 2020;104(1):50–63. doi: 10.1016/j.pec.2020.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Han HR, McKenna S, Nkimbeng M, Wilson P, Rives S, Ajomagberin O, Alkawaldeh M, Grunstra K, Maruthur N, Sharps P. A Systematic Review of Community Health Center Based Interventions for People with Diabetes. J Community Health. 2019;44(6):1253-80. 10.1007/s10900-019-00693-y. Epub 2019 Jul 6. [DOI] [PubMed]
- 44.Kim K, Choi JS, Choi E, Nieman CL, Joo JH, Lin FR, et al. Effects of community-based health worker interventions to improve chronic disease management and care among vulnerable populations: a systematic review. Am J Public Health. 2016;106(4):e3–e28. doi: 10.2105/AJPH.2015.302987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ko D, Bratzke LC, Roberts T. Self-management assessment in multiple chronic conditions: A narrative review of literature. Int J Nurs Stud. 2018;83:83–90. doi: 10.1016/j.ijnurstu.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 46.Smith SM, Wallace E, O'Dowd T. Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2016;3:Cd006560. doi: 10.1002/14651858.CD006560.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Deek H, Hamilton S, Brown N, Inglis SC, Digiacomo M, Newton PJ, et al. Family-centred approaches to healthcare interventions in chronic diseases in adults: a quantitative systematic review. J Adv Nurs. 2016;72(5):968–979. doi: 10.1111/jan.12885. [DOI] [PubMed] [Google Scholar]
- 48.Chi NC, Demiris G. A systematic review of telehealth tools and interventions to support family caregivers. J Telemed Telecare. 2015;21(1):37–44. doi: 10.1177/1357633X14562734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Price M, Bellwood P, Kitson N, Davies I, Weber J, Lau F. Conditions potentially sensitive to a personal health record (PHR) intervention, a systematic review. BMC Med Inform Decis Mak. 2015;15:32. doi: 10.1186/s12911-015-0159-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res. 2015;17(2):e44. doi: 10.2196/jmir.3171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ammenwerth E, Hoerbst A, Lannig S, Mueller G, Siebert U, Schnell-Inderst P. Effects of adult patient portals on patient empowerment and health-related outcomes: a systematic review. Stud Health Technol Inform. 2019;264:1106–1110. doi: 10.3233/SHTI190397. [DOI] [PubMed] [Google Scholar]
- 52.Dendere R, Slade C, Burton-Jones A, Sullivan C, Staib A, Janda M. Patient portals facilitating engagement with inpatient electronic medical records: a systematic review. J Med Internet Res. 2019;21(4):e12779. doi: 10.2196/12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Risling T, Martinez J, Young J, Thorp-Froslie N. Evaluating patient empowerment in association with ehealth technology: scoping review. J Med Internet Res. 2017;19(9):e329. doi: 10.2196/jmir.7809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kelly MM, Coller RJ, Hoonakker PL. Inpatient portals for hospitalized patients and caregivers: a systematic review. J Hosp Med. 2018;13(6):405–412. doi: 10.12788/jhm.2894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kuo A, Dang S. Secure messaging in electronic health records and its impact on diabetes clinical outcomes: a systematic review. Telemed J E Health. 2016;22(9):769–777. doi: 10.1089/tmj.2015.0207. [DOI] [PubMed] [Google Scholar]
- 56.Stacey D, Legare F, Lewis K, Barry MJ, Bennett CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;4:Cd001431. doi: 10.1002/14651858.CD001431.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Baik D, Cho H, Masterson Creber RM. Examining interventions designed to support shared decision making and subsequent patient outcomes in palliative care: a systematic review of the literature. Am J Hosp Palliat Care. 2019;36(1):76–88. doi: 10.1177/1049909118783688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cardona-Morrell M, Benfatti-Olivato G, Jansen J, Turner RM, Fajardo-Pulido D, Hillman K. A systematic review of effectiveness of decision aids to assist older patients at the end of life. Patient Educ Couns. 2017;100(3):425–435. doi: 10.1016/j.pec.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 59.Geddis-Regan A, Errington L, Abley C, Wassall R, Exley C, Thomson R. Enhancing shared and surrogate decision making for people living with dementia: A systematic review of the effectiveness of interventions. Health Expect. 2020;24(1):19–32. doi: 10.1111/hex.13167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vermunt N, Harmsen M, Westert GP, Olde Rikkert MGM, Faber MJ. Collaborative goal setting with elderly patients with chronic disease or multimorbidity: a systematic review. BMC Geriatr. 2017;17(1):167. doi: 10.1186/s12877-017-0534-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Irizarry T, DeVito DA, Curran CR. Patient portals and patient engagement: a state of the science review. J Med Internet Res. 2015;17(6):e148. doi: 10.2196/jmir.4255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nathan AG, Marshall IM, Cooper JM, Huang ES. Use of decision aids with minority patients: a systematic review. J Gen Intern Med. 2016;31(6):663–676. doi: 10.1007/s11606-016-3609-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.ElKefi S, Asan O. How technology impacts communication between cancer patients and their health care providers: a systematic literature review. Int J Med Inform. 2021;149:104430. doi: 10.1016/j.ijmedinf.2021.104430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.DeRosa AP, Grell Y, Razon D, Komsany A, Pinheiro LC, Martinez J, Phillips E. Decision-making support among racial and ethnic minorities diagnosed with breast or prostate cancer: A systematic review of the literature. Patient Educ Couns. 2021:S0738-3991(21)00621-2. 10.1016/j.pec.2021.09.012. Epub ahead of print. [DOI] [PubMed]
- 65.Kashaf MS, McGill E. Does shared decision making in cancer treatment improve quality of life? A systematic literature review. Med Decis Making. 2015;35(8):1037–1048. doi: 10.1177/0272989X15598529. [DOI] [PubMed] [Google Scholar]
- 66.Spronk I, Burgers JS, Schellevis FG, van Vliet LM, Korevaar JC. The availability and effectiveness of tools supporting shared decision making in metastatic breast cancer care: a review. BMC Palliat Care. 2018;17(1):74. doi: 10.1186/s12904-018-0330-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Martinez-Alonso M, Carles-Lavila M, Perez-Lacasta MJ, Pons-Rodriguez A, Garcia M, Rue M. Assessment of the effects of decision aids about breast cancer screening: a systematic review and meta-analysis. BMJ Open. 2017;7(10):e016894. doi: 10.1136/bmjopen-2017-016894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.McIntyre R, Craig A. A literature review of patient education: is it time to move forward? J Med Imaging Radiat Sci. 2015;46(3s):S75–s85. doi: 10.1016/j.jmir.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 69.Baptista S, Teles Sampaio E, Heleno B, Azevedo LF, Martins C. Web-based versus usual care and other formats of decision aids to support prostate cancer screening decisions: systematic review and meta-analysis. J Med Internet Res. 2018;20(6):e228. doi: 10.2196/jmir.9070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Keinki C, Momberg A, Clauß K, Bozkurt G, Hertel E, Freuding M, et al. Effect of question prompt lists for cancer patients on communication and mental health outcomes-a systematic review. Patient Educ Couns. 2021;104(6):1335–1346. doi: 10.1016/j.pec.2021.01.012. [DOI] [PubMed] [Google Scholar]
- 71.Negarandeh R, Yazdani Z, Ramtin S, Janani L. Impact of using question prompt list on shared decision-making in the cancer patient: a systematic review. Nurs Pract Today. 2021;8(3):179–193. [Google Scholar]
- 72.Le Berre M, Maimon G, Sourial N, Gueriton M, Vedel I. Impact of transitional care services for chronically ill older patients: a systematic evidence review. J Am Geriatr Soc. 2017;65(7):1597–1608. doi: 10.1111/jgs.14828. [DOI] [PubMed] [Google Scholar]
- 73.Sendall M, McCosker L, Crossley K, Bonner A. A structured review of chronic care model components supporting transition between healthcare service delivery types for older people with multiple chronic diseases. Health Inf Manag. 2017;46(2):58–68. doi: 10.1177/1833358316681687. [DOI] [PubMed] [Google Scholar]
- 74.Coulter A, Entwistle VA, Eccles A, Ryan S, Shepperd S, Perera R. Personalised care planning for adults with chronic or long-term health conditions. Cochrane Database Syst Rev. 2015;2015(3):CD010523. 10.1002/14651858.CD010523.pub2. [DOI] [PMC free article] [PubMed]
- 75.Nishikawa Y, Hiroyama N, Fukahori H, Ota E, Mizuno A, Miyashita M, et al. Advance care planning for adults with heart failure. Cochrane Database Syst Rev. 2020;2(2):Cd013022. doi: 10.1002/14651858.CD013022.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Schaepe C, Bergjan M. Educational interventions in peritoneal dialysis: a narrative review of the literature. Int J Nurs Stud. 2015;52(4):882–898. doi: 10.1016/j.ijnurstu.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 77.Hillert CJ, Gershkowitz B, Crotty BH. Digital coaching strategies to facilitate behavioral change in type ii diabetes: A systematic review. J Gen Intern Med. 2020;35(SUPPL 1):S645–S6S6. doi: 10.1210/clinem/dgaa850. [DOI] [PubMed] [Google Scholar]
- 78.Yadav UN, Lloyd J, Hosseinzadeh H, Baral KP, Harris MF. Do Chronic Obstructive Pulmonary Diseases (COPD) Self-Management Interventions Consider Health Literacy and Patient Activation? A Systematic Review. J Clin Med. 2020;9(3):646. 10.3390/jcm9030646. [DOI] [PMC free article] [PubMed]
- 79.Oldfield BJ, Harrison MA, Genao I, Greene AT, Pappas ME, Glover JG, et al. Patient, Family, and Community Advisory Councils in Health Care and Research: a Systematic Review. J Gen Intern Med. 2019;34(7):1292–1303. doi: 10.1007/s11606-018-4565-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.McCarron TL, Moffat K, Wilkinson G, Zelinsky S, Boyd JM, White D, et al. Understanding patient engagement in health system decision-making: a co-designed scoping review. Syst Rev. 2019;8(1):97. doi: 10.1186/s13643-019-0994-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bombard Y, Baker GR, Orlando E, Fancott C, Bhatia P, Casalino S, et al. Engaging patients to improve quality of care: a systematic review. Implementation Sci. 2018;13(1):98. doi: 10.1186/s13012-018-0784-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Liang L, Cako A, Urquhart R, Straus SE, Wodchis WP, Baker GR, et al. Patient engagement in hospital health service planning and improvement: a scoping review. BMJ Open. 2018;8(1):e018263. doi: 10.1136/bmjopen-2017-018263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sharma AE, Knox M, Mleczko VL, Olayiwola JN. The impact of patient advisors on healthcare outcomes: a systematic review. BMC Health Serv Res. 2017;17(1):693. doi: 10.1186/s12913-017-2630-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kleinpell R, Zimmerman J, Vermoch KL, Harmon LA, Vondracek H, Hamilton R, et al. Promoting family engagement in the ICU: experience from a national collaborative of 63 ICUs. Crit Care Med. 2019;47(12):1692–1698. doi: 10.1097/CCM.0000000000004009. [DOI] [PubMed] [Google Scholar]
- 85.Iezzoni LI, Chang Y, Matulewicz H, Heaphy D, Warsett KS, Donelan K. Health plan enrollees with disability informing primary care practices and providers about their quality of care: a randomized trial. Disabil Health J. 2018;11(4):537–544. doi: 10.1016/j.dhjo.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 86.Unaka N, Statile A, Jerardi K, Dahale D, Morris J, Liberio B, et al. Improving the readability of pediatric hospital medicine discharge instructions. J Hosp Med. 2017;12(7):551–557. doi: 10.12788/jhm.2770. [DOI] [PubMed] [Google Scholar]
- 87.King C, Goldman A, Gampa V, Smith C, Muskett O, Brown C, et al. Strengthening the role of community health representatives in the Navajo Nation. BMC Public Health. 2017;17(1):348. doi: 10.1186/s12889-017-4263-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.“Patient Engagement”, Health Affairs Health Policy Brief. https://www.healthaffairs.org/do/10.1377/hpb20130214.898775/full/. Accessed 8 Jan 2022.
- 89.Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff. 2013;32(2):207–214. doi: 10.1377/hlthaff.2012.1061. [DOI] [PubMed] [Google Scholar]
- 90.Patient Engagement Action Team . Engaging patients in patient safety – a Canadian Guide. Canadian Patient Safety Institute. 2017. [Google Scholar]
- 91.Graffigna G, Barello S, Bonanomi A, Lozza E. Measuring patient engagement: development and psychometric properties of the Patient Health Engagement (PHE) Scale. Front Psychol. 2015;6:274. doi: 10.3389/fpsyg.2015.00274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Thomas BJ, Ganesan S. Scale construction: valid measurement instrument for diabetes patient engagement. Int J Mark Res. 2019;62(4):468–482. [Google Scholar]
- 93.Sharma AE, Rivadeneira NA, Barr-Walker J, Stern RJ, Johnson AK, Sarkar U. Patient engagement in health care safety: an overview of mixed-quality evidence. Health Aff. 2018;37(11):1813–1820. doi: 10.1377/hlthaff.2018.0716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.About Learning Health Systems . Content last reviewed May 2019. Agency for Healthcare Research and Quality, Rockville, MD. 2019. [Google Scholar]
- 95.Zittleman L, Emsermann C, Dickinson M, Norman N, Winkelman K, Linn G, et al. Increasing colon cancer testing in rural Colorado: evaluation of the exposure to a community-based awareness campaign. BMC Public Health. 2009;9:288. doi: 10.1186/1471-2458-9-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bender BG, Dickinson P, Rankin A, Wamboldt FS, Zittleman L, Westfall JM. The Colorado Asthma Toolkit Program: a practice coaching intervention from the High Plains Research Network. J Am Board Fam Med. 2011;24(3):240–248. doi: 10.3122/jabfm.2011.03.100171. [DOI] [PubMed] [Google Scholar]
- 97.Norman N, Bennett C, Cowart S, Felzien M, Flores M, Flores R, et al. Boot camp translation: a method for building a community of solution. J Am Board Fam Med. 2013;26(3):254–263. doi: 10.3122/jabfm.2013.03.120253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Westfall JM, Zittleman L, Sutter C, Emsermann CB, Staton EW, Van Vorst R, et al. Testing to prevent colon cancer: results from a rural community intervention. Ann Fam Med. 2013;11(6):500–507. doi: 10.1370/afm.1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kiran T, Davie S, MacLeod P. Citizen engagement in primary care. Ann Fam Med. 2018;16(2):175. doi: 10.1370/afm.2185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Roland KB, Milliken EL, Rohan EA, DeGroff A, White S, Melillo S, et al. Use of community health workers and patient navigators to improve cancer outcomes among patients served by federally qualified health centers: a systematic literature review. Health Equity. 2017;1(1):61–76. doi: 10.1089/heq.2017.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Radhakrishnan K, Xie B, Berkley A, Kim M. Barriers and facilitators for sustainability of tele-homecare programs: a systematic review. Health Serv Res. 2016;51(1):48–75. doi: 10.1111/1475-6773.12327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dogba MJ, Dossa AR, Breton E, Gandonou-Migan R. Using information and communication technologies to involve patients and the public in health education in rural and remote areas: a scoping review. BMC Health Serv Res. 2019;19(1):128. doi: 10.1186/s12913-019-3906-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Young A, Menon D, Street J, Al-Hertani W, Stafinski T. Exploring patient and family involvement in the lifecycle of an orphan drug: a scoping review. Orphanet J Rare Dis. 2017;12(1):188. doi: 10.1186/s13023-017-0738-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Menon D, Stafinski T, Dunn A, Short H. Involving patients in reducing decision uncertainties around orphan and ultra-orphan drugs: a rare opportunity? Patient. 2015;8(1):29–39. doi: 10.1007/s40271-014-0106-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1. Patient, family, and caregiver engagement conceptual framework. Table S1. PubMed Search Strategy. Figure S2. Search flow diagram for original studies. Table S2. Characteristics of included systematic reviews on PFE strategies at the direct patient care level and their findings.
Data Availability Statement
Not applicable