Abstract
Background
The COVID-19 pandemic increased reliance on virtual care for patients with persistent asthma.
Objective
This retrospective cohort study assessed changes from in-person to virtual care during the pandemic. In patients with persistent asthma, compared with the same period before the pandemic.
Methods
Kaiser Permanente Colorado members aged 18 to 99 years with persistent asthma were evaluated during two periods (March to October 2019 and March to October 2020). Comparison of asthma exacerbations (hospitalizations, emergency department visits, and courses of oral prednisone) and asthma medication metrics were evaluated between the two periods and by type of care received during the pandemic (no care, virtual care only, in-person care only, or a mix of virtual and in-person care). Population characteristics by type of care received during the pandemic were also evaluated.
Results
Among 7,805 adults with persistent asthma, those who used more virtual care or sought no care during the pandemic were younger and had fewer comorbidities, mental health diagnoses, or financial barriers. Exacerbations decreased (0.264 to 0.214; P <.001) as did courses of prednisone (0.213 to 0.169). Asthma medication adherence (0.53 to 0.54; P <.001) and the asthma medication ratio, a quality-of-care metric (0.755 to 0.762; P = .019), increased slightly. Patients receiving a mix of in-person and virtual care had the highest rate of exacerbations (0.83) and a lower asthma medication ratio (0.74) despite having the highest adherence (.57).
Conclusions
Despite an increase in virtual care, asthma exacerbations decreased except among individuals who received both in-person and virtual care, likely because they had more severe disease.
Key words: Persistent asthma, COVID-19 pandemic, Virtual asthma care, Telemedicine, Asthma exacerbations
Abbreviations used: AMR, Asthma medication ratio; ED, Emergency department; EHR, Electronic health record; KPCO, Kaiser Permanente Colorado; PDC, Proportion of days covered
What is already known about this topic? The COVID-19 pandemic led to a rapid and significant change from in-person care to virtual care. This change in the way care was delivered affected patient populations differently. Patients with asthma had a reduction in exacerbations during the pandemic.
What does this article add to our knowledge? This article highlights how care for patients with asthma was delivered both virtually and in person, as well as where barriers to virtual care existed, and suggests that care could be delivered virtually without an adverse effect on asthma outcomes.
How does this study impact current management guidelines? This article should give clinicians some confidence that asthma care can be delivered virtually, although it will require ongoing work to improve accessibility and acceptance while maintaining quality.
Introduction
The COVID-19 pandemic has had a dramatic impact on the delivery of outpatient care. In an effort to slow the spread of COVID-19, and with the support of regulatory changes in public and private reimbursement for telemedicine services,1 , 2 health care systems curtailed in-person visits and increased the availability of virtual care options. Documenting this change in the first 8 months of the pandemic, a report by the Centers for Medicare and Medicaid Services3 found that between mid-March and mid-October, more than 24.5 million of 63 million eligible patients (nearly 40%) received telemedicine service covered by Medicare. However, virtual care did not fully replace in-person care during the pandemic. For example, in a large national study of over 16 million commercially insured patients,4 a substantial decrease in in-person visits was only partially offset by telemedicine visits.
Given the rapid and unprecedented transition to virtual care, several studies highlighted the difficulties associated with this historic transition.5, 6, 7 The impact of virtual care on the management of chronic diseases, including asthma, has been particular concerning because these conditions require ongoing access to primary and specialty care to maintain quality and prevent adverse events such as hospitalizations. Preliminary studies that assessed the impact of this transition on chronic disease management showed variable outcomes.8, 9, 10, 11 The care of asthma patients during the pandemic was a particular concern because early in the pandemic, the Center for Disease Control and Prevention suggested that patients with moderate to severe asthma could potentially be at higher risk for complications of COVID-19.12
In this study, we describe the transition to virtual care that took place in a large integrated health care system with a population of nearly 8,000 adult patients with asthma during the first 8 months of the pandemic (March 2020 to October 2020). We examined the extent to which patients received care through virtual channels and the effect of this transition on asthma outcomes, compared with the same period in 2019.
Methods
Setting
This retrospective cohort study was conducted at Kaiser Permanente Colorado (KPCO), an integrated health care delivery system composed of direct-pay, employer-sponsored Medicaid, Medicare, and Medicare Advantage insurance plans with more than 545,000 members in the Denver-Boulder metropolitan area. Within KPCO, patients with persistent asthma receive collaborative team care, including primary care and specialty care clinicians, pharmacists, and nurses. Before the COVID-19 pandemic, KPCO members could access care through a call-center telephone line or by e-mail through a secure patient portal (kp.org). To obtain care with a KPCO clinician, patients could schedule an in-person visit, telephone visit, or video visit, and, beginning in late 2016, by synchronous chat, via functionality embedded in the secure patient portal. In 2019, over 85% of all care was done with in-person visits whereas 15% was virtual (9% scheduled telephone, less than 1% video visit, and 5% synchronous chat). The system also provided medical care through automated voice message and website notifications. Beginning on March 13, 2020, when the COVID-19 national emergency was declared, health care systems, including KPCO, rapidly converted to virtual-first care by leveraging existing telehealth infrastructure and by reallocating clinicians and staff to provide virtual care.
Data sources
The primary data source for this analysis was patient-level information from the KPCO electronic health records (EHRs), augmented by administrative and claims databases, which included procedure codes, diagnosis codes, and census-based measures of socioeconomic status, pharmacy dispensing data, as well as all internal hospital and ambulatory encounters and claims for services outside KPCO.
Study sample
The cohort for this study included adults aged 18 years and older who were continuously enrolled in KPCO during the period before COVID-19 (from March 2019 through October 2019) and during COVID-19 (from March 2020 through October 2020). Matched time periods were used to account for the usual seasonality of asthma exacerbations.13 We included only patients who had persistent asthma for both study periods, based on clinician diagnosis. Patients with diagnoses of chronic obstructive pulmonary disease were excluded. We also required that the clinical diagnosis of persistent asthma, captured in both periods, be confirmed by at least one of the following: a visit (in-person or virtual) with an asthma diagnosis, a fill of controller medication (eg, inhaled corticosteroids, leukotriene receptor antagonist), a fill of reliever medication (eg, short-acting β-agonist), or an asthma exacerbation (prednisone fill, emergency department [ED], hospital, or urgent care visit with an asthma diagnosis).
Measures
The primary outcome was the difference in asthma exacerbations in the period before COVID-19 compared with the period during COVID-19. Asthma exacerbations were defined as oral corticosteroid bursts and asthma-related urgent care visits, ED visits, and hospitalizations, in which there was a corresponding primary or secondary visit diagnostic code for asthma. When oral corticosteroids were prescribed, the exacerbation had to be linked to a diagnosis of asthma to be counted. Emergency department visits, urgent care visits, or hospitalizations were included when asthma was the primary diagnosis or when an asthma exacerbation was listed as a primary or secondary diagnosis.
Secondary outcome measures included adherence to inhaled corticosteroids and the asthma medication ratio (AMR), a National Committee for Quality Assurance metric for asthma. Adherence to inhaled corticosteroids was defined as the proportion of days covered (PDC), a proportion between 0.0 and 1.0.14 The AMR was defined as a ratio of asthma controller canisters dispensed to the sum of asthma controller plus asthma reliever canisters dispensed.15 In addition to comparing patients with persistent asthma before and during COVID-19, we compared the same outcomes, during the COVID-19 period only, according to the type of care patients received. Patients were broadly categorized by the type of care received during COVID-19 as no care of any type, in-person care only, virtual care (video, phone, or chat) only, or a mix of virtual and in-person care. Finally, we conducted a subanalysis looking at patients with at least one exacerbation both before and during COVID-19 to compare rates of in-person, virtual, and total visits for these periods.
Statistical analyses
To assess patient characteristics for the period during COVID-19 (March 2020 through October 2020), we used Kruskal-Wallis tests for continuous variables and χ2 tests for categorical variables. At the start of the COVID-19 period (March 2020), we also reported demographic subgroup distributions across each category of care use by age group, female sex, racial and ethnic group, insurance payer and type of insurance (which were not mutually exclusive and hence have separate P values), number of medical (Elixhauser) comorbidities,16 any mental health comorbidities, number of address changes, and receipt of medical financial assistance, a marker of financial resource strain. Race and ethnicity variables were derived from the EHR, in which medical personnel entered patient self-reported identification. Income and education were derived as proxy socioeconomic variables by linking a patient’s address to the census tract of residence.
For health care outcomes before and during the COVID-19 pandemic, we used Poisson regression models, adjusting for overdispersion and repeated measures to compare total prednisone exacerbations and PDC. For binary outcomes (any hospitalization, any ED visit, and any urgent care), we used log-binomial models with repeated-measure adjustment.17 Because AMR is a ratio of the count of controller medications relative to the count of controller plus reliever medications, we analyzed AMR using a binary logit model with a fractional dependent variable. All outcomes were adjusted for person-years except AMR, which was time-independent.
For outcomes across use groups during COVID-19, we used the same analytical methods except for hospitalizations and the sum of ED and urgent care visits, for which we used Poisson regression models accounting for overdispersion. We did not account for multiple time points because we were using an analysis of covariance framework, but calculated unadjusted models as well as models adjusting for age, sex, race, and the baseline value of the outcome of interest. All rates were adjusted for person-years except AMR.
For patients with exacerbations in both periods, we compared use across periods using Poisson models and nonlinear mixed models to derive confidence intervals for the difference between the two periods. To calculate rate ratios, the differences calculated from the model were exponentiated. All use rates were adjusted for person-years.
We used histograms to show use trends for the asthma cohort in both periods, for counts and relative percentages, for in-person compared with virtual visits. All analyses were performed using SAS Studio software (version 3.8, SAS Institute Inc, Cary, NC). Study protocols and human subjects’ considerations were reviewed and approved by the KPCO Institutional Review Board.
Results
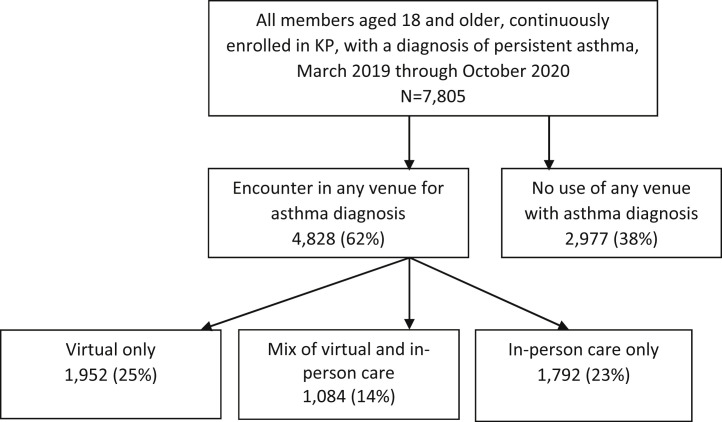
We identified a cohort of 7,805 adult patients (aged 18-99 years) with persistent asthma. During the first 8 months of the COVID-19 pandemic (March 2020 through October 2020), 4,828 patients (62%) received care from a provider for asthma whereas 2,977 received no care for asthma (38%). Of the group receiving clinician care for asthma, 1,952 received virtual care only (25%), 1,792 received in-person care only (23%), and 1,084 received a mix of virtual and in-person care for asthma (14%) (Figure 1 ). During the study period, 129 participants in the study had a diagnosis of COVID-19 disease, but none died during this period.
Figure 1.
Waterfall diagram for venues of care received by patients with persistent asthma during COVID-19. KP, Kaiser Permanente.
Care use during COVID-19
Table I compares patient characteristics of the four care classification groups in March 2020 (no care, in-person only, virtual only, and a mix of virtual and in-person care). Older patients received more in-person care (29.3% for those aged 65 years and older compared with 23% for the group as a whole) than virtual (22.8% for those aged 65 years and older vs 25% for the group as a whole), whereas younger patients tended to receive care more often virtually (26.8% for those aged 18-34 years and 26.5% for those aged 35-50 years vs 25% for the group as a whole) or received no care at all (41% for those aged 18-34 years and 40.2% for those aged 35-50 years vs 38% for the group as a whole). The portion of patients receiving virtual care was roughly equal across racial and ethnic groups, although Black patients received a relatively higher proportion of care virtually (29.7% vs 25% for the group as a whole) and were less likely to be in the no-care group (30.9% vs 38%). Those requiring medical financial assistance were less likely to be in the no-care group (31.3% vs 38%) and more likely to have sought in-person care (27% vs 23%) or to have required a mix of virtual and in-person care (22% vs 14%). Those with Medicaid did not seek care differently from those in the larger persistent asthma population (P = .09). Individuals with a prior mental or behavioral health diagnosis (24.5% vs 23%) or those with a higher number of comorbid conditions (2.4 vs 2.0) more often sought in-person care.
Table I.
Patient sociodemographic, clinical, and social health characteristics of use subgroups derived from March 2020 to October 2020 (n = 7,805)
| Characteristic‡ | Characteristic for entire cohort column (%) | Distribution by visit type |
P | |||
|---|---|---|---|---|---|---|
| No asthma care during COVID-19 (row %) (n = 2,977; 38%) | In-person asthma care only (row %) (n = 1,792; 23%) | Mix of in-person and virtual care (row %) (n = 1,084; 14%) | Virtual care only (row %) (n = 1,952; 25%) | |||
| Age group, y (n [%])∗ | <.001 | |||||
| 18-34 | 1,264 (16.2) | 518 (41.0) | 248 (19.6) | 159 (12.6) | 339 (26.8) | |
| 35-50 | 2,064 (26.4) | 829 (40.2) | 405 (19.6) | 283 (13.7) | 547 (26.5) | |
| 51-64 | 2,253 (28.9) | 877 (38.9) | 488 (21.7) | 329 (14.6) | 559 (24.8) | |
| ≥65 | 2,224 (28.5) | 753 (33.9) | 651 (29.3) | 313 (14.1) | 507 (22.8) | |
| Sex, n (%) | <.001 | |||||
| Female∗ | 4,920 (63.0) | 1,730 (35.2) | 1,139 (23.2) | 758 (15.4) | 1,293 (26.3) | |
| Male | 2,885 (37.0) | 1,247 (43.2) | 653 (22.6) | 326 (11.3) | 659 (22.8) | |
| Racial and ethnic subgroups, n (%)∗ | .009 | |||||
| Asian | 172 (2.2) | 70 (40.7) | 36 (20.9) | 22 (12.8) | 44 (25.6) | |
| Black | 417 (5.3) | 129 (30.9) | 91 (21.8) | 73 (17.5) | 124 (29.7) | |
| Other race | 247 (3.2) | 109 (44.1) | 55 (22.3) | 26 (10.5) | 57 (23.1) | |
| Unknown race | 161 (2.1) | 75 (46.6) | 34 (21.1) | 11 (6.8) | 41 (25.5) | |
| White | 5,724 (73.3) | 2,200 (38.4) | 1,325 (23.2 | 788 (13.8) | 1,411 (24.7) | |
| Hispanic ethnicity | 1,084 (13.9) | 394 (36.4) | 251 (23.2) | 164 (15.1) | 275 (25.4) | |
| Insurance coverage, n (%)∗ | ||||||
| Medicaid and subsidized | 517 (6.6) | 170 (32.9) | 128 (24.8) | 80 (15.5) | 139 (26.9) | .087 |
| Health maintenance organization | 4,205 (53.9) | 1,523 (36.2) | 1,088 (25.9) | 614 (14.6) | 980 (23.3) | <.001 |
| Deductible/coinsurance | 3,971 (50.9) | 1,573 (39.6) | 833 (21.0) | 524 (13.2) | 1,041 (26.2) | <.001 |
| Count of medical comorbidities, n (SD)† | 2.0 (1.8) | 1.7 (1.7) | 2.3 (2.0) | 2.4 (1.9) | 1.9 (1.7) | <.001 |
| Any mental health comorbidity, n (%)∗ | 2,226 (28.5) | 718 (32.3) | 545 (24.5) | 371 (16.7) | 592 (26.6) | <.001 |
| Median family income (mean [75th percentile, 25th percentile])†,§ | 98,124 (74,794, 117,083) | 98,966 (75,156, 118,958) | 96,767 (74,000, 116,416) | 96,409 (74,148, 116,750) | 99,039 (76,107, 118,958) | .014 |
| Less than high school education (% [SD])†,§ | 7.9 (0.08) | 7.9 (0.08) | 8.2 (0.09) | 7.9 (0.08) | 7.5 (0.08) | .064 |
| Receipt of medical-financial assistance, n (%)∗ | 300 (3.8) | 94 (31.3) | 81 (27.0) | 66 (22.0) | 59 (19.7) | <.001 |
| Address changes, n (SD)† | 0.10 (0.36) | 0.08 (0.3) | 0.12 (0.38) | 0.13 (0.39) | 0.12 (0.40) | <.001 |
Other race includes Native Hawaiian or other Pacific Islander, American Indian, Native Alaskan, and those that identify as other race without specificity.
Categorical variables are row percentages to allow for comparison of characteristics across use categories in header columns. P values were obtained with χ2 test. Insurance coverage is not mutually exclusive.
Continuous variable P values were obtained with Kruskal-Wallis test.
Characteristics were derived as of March 2020.
US Census tract using postal code to obtain income and education status estimates.
Courses of prednisone and asthma exacerbations requiring urgent care, ED care, or hospitalization were all more common in those receiving a mix of in-person and virtual care (Table II ). Individuals receiving no care during COVID-19 had the highest AMR (0.78 vs 0.76 for the group as a whole) whereas those receiving a mix of care (the group with the highest rate of exacerbations during COVID-19) had a lower AMR (0.74 vs 0.76 overall) despite having the highest PDC (0.57 vs 0.54) (Table II). We adjusted for age, sex, and race and ethnicity. The baseline value of the outcome did not affect these findings (Table III ).
Table II.
Unadjusted comparison of asthma outcomes between use groups during COVID-19
| Outcome | Overall during COVID-19 (n = 7,805) | No asthma care during COVID-19 (n = 2,977) | In-person asthma care only (n = 1,792) | Mix of in-person and virtual care (n = 1,084) | Virtual care only (n= 1,952) | P |
|---|---|---|---|---|---|---|
| Total exacerbations | 0.214 (0.009) | 0.017 (0.004) | 0.164 (0.014) | 0.827 (0.041) | 0.221 (0.016) | <.001 |
| Prednisone∗ | 0.169 (0.008) | 0.017 (0.004) | 0.099 (0.011) | 0.610 (0.035) | 0.221 (0.016) | <.001 |
| Emergency department or urgent care visits∗ | 0.116 (0.009) | 0 | 0.063 (0.008) | 0.204 (0.019) | 0 | <.001 |
| Hospitalizations∗ | 0.006 (0.002) | 0 | 0.003 (0.002) | 0.012 (0.004) | 0 | .021 |
| Proportion of days covered† | 0.539 (0.004) | 0.563 (0.006) | 0.497 (0.008) | 0.570 (0.010) | 0.525 (0.007) | <.001 |
| Asthma medication ratio‡ | 0.762 (0.002) | 0.784 (0.003) | 0.780 (0.004) | 0.736 (0.004) | 0.732 (0.004) | <.001 |
Data are presented as mean (SE).
Poisson model accounting for overdispersion used to obtain P. Rates are person-year adjusted.
Poisson model accounting for overdispersion used to obtain P. Mean is total number of days covered by total number of days of enrollment in study period.
Logit binomial model with fractional-dependent variable (controller divided by sum of controller and reliever) model used to determine P.
Table III.
Exacerbation rates before and during COVID-19 (n = 7,805)
| Outcome | Rate before COVID-19 (mean [SE])‡ | Rate during COVID-19 (mean [SE])‡ | Ratio of rates before vs during COVID-19 (95% confidence interval) | P |
|---|---|---|---|---|
| All exacerbations∗ | 0.264 (0.009) | 0.214 (0.009) | 0.810 (0.739-0.888) | <.001 |
| Prednisone∗ | 0.213 (0.008) | 0.169 (0.008) | 0.794 (0.718-0.878) | <.001 |
| Any inpatient visit† | 0.004 (0.001) | 0.002 (0.001) | 0.478 (0.238-0.960) | .04 |
| Any emergency department visit† | 0.017 (0.002) | 0.015 (0.002) | 0.874 (0.650-1.175) | .37 |
| Any urgent care visit† | 0.025 (0.002) | 0.023 (0.002) | 0.903 (0.717-1.137) | .39 |
| Portion of days covered∗ | 0.528 (0.004) | 0.539 (0.004) | 1.022 (1.010-1.033) | <.001 |
| Asthma medication ratio§ | 0.755 (0.003) | 0.762 (0.003) | 1.035 (1.006-1.064) | .019 |
Poisson model accounting for repeated measures unadjusted for covariates. The ratio with the confidence interval is the incidence density ratio.
Generalized linear model using log-binomial model accounting for repeated measures unadjusted for covariates. The reported ratio and confidence interval are the relative risk.
Rates are adjusted for person-years except for the asthma medication ratio, which is not dependent on time.
Odds ratio for logit model with fractional-dependent variable accounting for repeated measures.
We also analyzed the number of visits patients had in each mode of care they used. Patients who used only in-person care had a mean of 1.3 visits (SD, 0.9 visits; median, 1 visit; interquartile range [IQR], 1-1 visit). Patients who used only virtual care had a mean of 1.4 visits (SD, 0.8 visit; median, 1 visit; IQR, 1-2 visits) in all virtual care channels. Those who used a combination of in-person and virtual care had a mean of 1.6 in-person visits (SD, 1.26 visits) and 1.9 virtual visits (SD, 1.26 virtual visits), with medians of 1 for both in-person and virtual visits (IQR, 1-2 for both). The many different blends of in-person and virtual care made it difficult to test the association of visit volume with outcomes.
Comparison of time periods
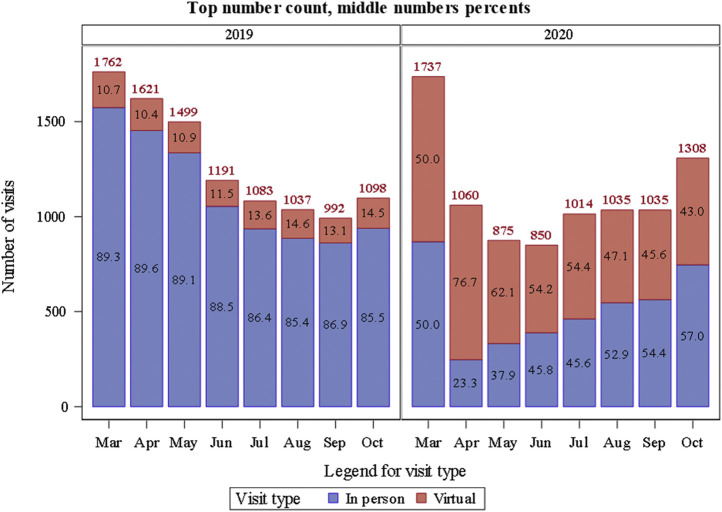
Cohort members received a higher volume of care during the spring months (March to May) of 2019, when seasonal allergies would typically induce more requests for care (Figure 2 ). However, in spring 2020, as the pandemic first developed, the level of care decreased for all modes of care, with a shift from an in-person mode of care (85% of all visits in 2019) to virtual care, ranging from a high of 76.7% of care in April to 43% by October 2020. In October 2020, there was a 19% increase in total care compared with October 2019.
Figure 2.
Virtual and in-person care in 2019 compared with 2020.
Compared with before COVID-19, there was a decrease in asthma exacerbations during COVID-19 from 0.264 to 0.214 (P < .001) (Table IV ), largely reflected in a significant decrease in the prescription of oral corticosteroids (0.213 to 0.169; P < .001). Decreases in ED, urgent care, and hospitalization rates for asthma exacerbations during COVID-19 were not statistically significant. There was a statistically significant increase when the period before COVID-19 is compared with the same months in the first year of the COVID-19 pandemic, for the whole population for both PDC (0.53 to 0.54; P < .001) and for AMR (0.75 to 0.76; P = .019). However, these changes do not appear to be clinically meaningful.
Table IV.
Adjusted comparison of asthma outcomes among use groups during COVID-19
| Outcome§ | Overall during COVID-19 (n = 7,805) | No asthma care during COVID-19 (n = 2,977) | In-person asthma care only (n = 1,792) | Mix of in-person and virtual care (n = 1,084) | Virtual care only (n = 1,952) | P |
|---|---|---|---|---|---|---|
| Total exacerbations | 0.136 (0.014) | 0.013 (0.003) | 0.127 (0.015) | 0.537 (0.055) | 0.161 (0.018) | <.001 |
| Prednisone∗ | 0.127 (0.013) | 0.015 (0.003) | 0.088 (0.011) | 0.456 (0.045) | 0.183 (0.019) | <.001 |
| Emergency department or urgent care visits∗ | 0.082 (0.018) | 0 | 0.048 (0.012) | 0.137 (0.033) | 0 | <.001 |
| Hospitalizations∗ | <0.001 (0.106) | 0 | <0.001 (0.062) | <0.001 (0.291) | 0 | .034 |
| Proportion of days covered† | 0.477 (0.006) | 0.489 (0.007) | 0.446 (0.008) | 0.497 (0.010) | 0.476 (0.008) | <.001 |
| Asthma medication ratio‡ | 0.760 (0.004) | 0.778 (0.005) | 0.762 (0.006) | 0.745 (0.006) | 0.743 (0.005) | <.001 |
Data are presented as mean (SE).
Poisson model accounting for overdispersion used to obtain P. Rates are person-year adjusted.
Poisson model accounting for overdispersion used to obtain P. Mean is total number of days covered by total number of days of enrollment in study period.
Logit binomial model with fractional-dependent variable (controller divided by sum of controller and reliever) model used to determine P.
Each outcome is adjusted for age, sex, race, and baseline value of outcome.
In comparing patients who had one or more exacerbations in 2019 with those who had one or more exacerbations during 2020, the mean number of total visits was equal. However, the portion of total visits that were virtual for this population increased from 13% of all visits before COVID-19 to 58% of all visits during COVID-19 (Table V ).
Table V.
Mean visits in patients with one or more exacerbations before COVID-19 (2019) vs during COVID-19 (2020) (n = 223)
| Use measure | Before COVID-19∗ | During COVID-19∗ | Difference (mean [95% confidence interval])† | Rate ratio (mean [95% confidence interval])‡ |
|---|---|---|---|---|
| In-person visits | 4.11 (0.23) | 1.98 (0.17) | –2.13 (–2.57 to –1.70) | 0.48 (0.41-0.57) |
| Virtual visits | 0.62 (0.07) | 2.75 (0.19) | 2.13 (1.75-2.52) | 4.46 (3.48-5.70) |
| Total visits (in-person / virtual visits) | 4.73 (0.24) | 4.73 (0.29) | 0.00 (–0.59 to 0.59) | 1.00 (0.88-1.13) |
Means are adjusted for person-years; SEs were derived from Poisson regression.
Confidence intervals were derived from Poisson regression and nonlinear mixed models.
Confidence intervals were derived from Poisson regression.
Discussion
In this retrospective cohort study of patients with persistent asthma, during the transition of care delivery from before to during COVID-19, we found no evidence for an adverse impact on the important clinical outcomes of hospitalizations, ED visits, and courses of prednisone for asthma flares or on asthma medication adherence or AMR. Although there was an expected and widely documented decrease in volumes of care early on in the pandemic, the volume of care recovered quickly and transitioned from in-person to virtual care. To a large extent, virtual care was adopted across age, race, income, and insurance-type groups. At the same time, the use of virtual care tended to be lower among older patients, those with a lower household income, and those with a mental health diagnosis or a higher number of comorbidities. Asthma exacerbations (courses of prednisone, ED visits, and hospitalizations) all decreased during COVID-19 relative to the same period before COVID-19, although only a reduction in the courses of prednisone was statistically significant.
Others have documented that the extent and duration of the virtual care transition during COVID-19 varied by disease,8, 9, 10, 11 , 18, 19, 20, 21, 22, 23, 24, 25 socioeconomic status,5 , 6 ethnicity,6 , 18 and practice type.26 , 27 For instance, there was a rapid and nearly complete transition to virtual visits in mental health care,27, 28, 29 suggesting an easier transition for health conditions that were not as dependent on in-person testing and examinations. However, other studies showed that people with lower socioeconomic status had more difficulty making connections for virtual care.14 , 18 Our finding of the lower use of virtual care among more economically vulnerable populations is consistent with this finding. Similar to our study findings, a study conducted in the Department of Veterans Affairs health care system documented an increase in virtual care among those who were younger (aged less than 45 years), but in contrast found that those with a lower income, higher disability, and more chronic conditions were more likely to receive virtual care during the pandemic.30 Findings from an urban academic medical center were similar to those of our own study, showing that virtual visits were less likely in men and in elderly patients. However, in contrast to our study, they found fewer virtual visits among people with Medicaid-sponsored insurance.31
Although several studies looked at the rapid implementation of virtual care for chronic disease and patient satisfaction with this change in mode of care,8 , 19, 20, 21, 22 , 30 , 31 few looked at outcomes for these chronic diseases.24 , 25 A few studies examined the transition to virtual care specifically in allergy practices and asthma populations but did not include clinical outcomes.8 , 23 One study of children with asthma presenting to a large inner-city tertiary hospital found that courses of prednisone, outpatient visits, and hospitalizations all decreased during the first few months of the pandemic, whereas video visits and prescriptions for asthma medications increased.32 Despite the change in how outpatient care was delivered to the current KPCO adult patient population with asthma, adverse outcomes decreased. Even patients with at least one asthma exacerbation before COVID-19 received the same volume of care during COVID-19, which suggests that this higher-need population of asthma patients was able to access the care that it needed either virtually or in person. The existence of virtual care options within KPCO before the onset of the pandemic may have led to greater awareness and comfort with virtual care once COVID-19 arrived.
Multiple studies documented that patients with asthma had improved outcomes during the pandemic.33 Several factors may have led to improved outcomes in patients with persistent asthma during this time. These include improved adherence32 , 34 and decreased exposure to traditional viral triggers as well as to the COVID-19 virus.34 , 35 Eosinophilic inflammation, which is characteristic of allergic asthma, may also have been protective against the COVID-19 virus.36 Other mitigating factors may have included decreased exposure to air pollution, fire smoke, tobacco smoke, and indoor allergens in the workplace or social settings; social distancing; mask wearing; and improved personal hygiene. For all of these reasons, the impact of the rapid conversion to virtual care cannot be distinguished from clinical and social changes resulting from the COVID-19 pandemic itself. Also, fewer adverse outcomes may have occurred in the no-care and virtual-only care groups because they tended to be younger and to have fewer comorbidities.
We found that adherence improved overall for the current patient population during the COVID-19 pandemic, but this statistically significant improvement was not likely clinically meaningful, because changes in adherence need to be substantial to affect asthma outcomes.37 The no-care group had the highest AMR, which suggests that asthma remained more stable or was more mild. It is also possible that those individuals managed the exacerbations at home rather than attending an in-person visit, although those exacerbations likely would have been mild. All persistent asthma patients recieved automated reminders if they are due to refill controller medications, which has been shown to improve adherence.37 Those receiving virtual care had the lowest AMR, which suggests less well-controlled but perhaps milder asthma, which, with a little reassurance via virtual care, they were able to manage at home. Those receiving a mix of care had the highest rate of exacerbations and a lower AMR despite having a higher PDC. Driving down the AMR, despite the higher PDC, was a higher use of albuterol. Thus, this group using more care and more albuterol likely had more severe asthma. This is consistent with previous studies that found the Healthcare Effectiveness Data and Information Set AMR, and in particular albuterol use, to be a stronger correlate for adverse asthma outcomes.38, 39, 40
Our study had several limitations. It was conducted in an integrated health care system whose clinicians shared an EHR and for which modes of virtual care had already been developed, although those care channels were infrequently used (15% of patient encounters, with less than 1% conducted through video visits) before the pandemic. Thus, it may not be generalizable to other health care delivery systems or populations. We chose to use a clinician diagnosis of persistent asthma but no other criteria such as AMR, frequent use of β-agonists, frequency of asthma flares, or other criteria to define this population. An asthma exacerbation was used as an inclusion criterion, which may have blunted differences in outcomes among populations. Nevertheless, we found a difference in important outcomes both for the population as a whole between the two periods and within the subpopulations (divided by mode of care) during COVID-19. Finally, our research was restricted to an analysis of EHR data, which does not include patients’ perceptions regarding perceived or actual challenges to accessing care, their perceptions of the quality of care during COVID-19, and motivational factors that may have influenced their decisions regarding whether or how to access care.
Given the persistence of the COVID-19 pandemic, it is hard to predict how the expanded use of virtual care will be maintained. For patients with asthma, some amount of in-person care will be needed to assess the patient objectively by examination and spirometry testing. The amount and mix of virtual and in-person care will depend on both patient and clinician comfort with virtual visits, but also patient and clinician resources to conduct virtual visits efficiently and effectively. Before the pandemic, one study, which looked at children with asthma living in rural locations, who were managed by a tertiary care allergy clinic, demonstrated noninferior outcomes with those managed virtually versus in person.41 A 2015 Cochrane systematic review examining the impact of telehealth involving remote monitoring or video conferencing compared with in-person or telephone visits for chronic conditions, including diabetes and congestive heart failure, found similar health outcomes for patients with those conditions.42 Future research will need to continue to examine outcomes and ensure maintenance of care quality. In addition, there will be a need for research that surveys or interviews patients to facilitate the development of interventions to address systems-level and patient-level barriers to access in health care systems. Compensation for virtual visits will also likely influence the outcome, as will the potential cost savings in both personal and office space derived from conducting fewer in-person visits.
Our study suggests that access to services for this large population of patients with persistent asthma was maintained during the COVID-19 pandemic despite the change from in-person to virtual care. Although it was likely the result of other mitigating factors imposed by the pandemic itself, this sudden transition to virtual care did not lead to worse outcomes. Our study and others have highlighted a number of issues regarding the ongoing delivery of virtual care that will require thoughtful research in the future, particularly when the pandemic has subsided.
Footnotes
This research was funded by an internal Kaiser Permanente Colorado grant and National Institutes of Health, National Heart, Lung, and Blood Institute Grant R01HL126125.
Conflicts of interest: The authors declare that they have no relevant conflicts of interest.
References
- 1.Chao G.F., Li K.Y., Zhu Z., McCullough J., Thompson M., Claflin J., et al. Use of telehealth by surgical specialties during the COVID-19 pandemic. JAMA Surg. 2021;156:620–626. doi: 10.1001/jamasurg.2021.0979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel S.Y., Mehrotra A., Huskamp H.A., Uscher-Pines L., Ganguli I., Barnett M.L. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Intern Med. 2021;181:388–391. doi: 10.1001/jamainternmed.2020.5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Medicare & Medicaid Services. Trump administration finalizes permanent expansion of Medicare telehealth services and improved payment for time doctors spend with patients [press release]. December 1, 2020. Accessed July 22, 2021. https://www.cms.gov/newsroom/press-releases/trump-administration-finalizes-permanent-expansion-medicare-telehealth-services-and-improved-payment
- 4.Patel S.Y., Mehrotra A., Huskamp H.A., Uscher-Pines L., Ganguli I., Barnett M.L. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Intern Med. 2021;181:388–391. doi: 10.1001/jamainternmed.2020.5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cantor J.H., McBain R.K., Pera M.F., Bravata D.M., Whaley C.M. Who is (and is not) receiving telemedicine care during the COVID-19 pandemic. Am J Prev Med. 2021;61:434–438. doi: 10.1016/j.amepre.2021.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chunara R., Zhao Y., Chen J., Lawrence K., Testa P.A., Nov O., et al. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J Am Med Inform Assoc. 2021;28:33–41. doi: 10.1093/jamia/ocaa217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi N.G., DiNitto D.M., Marti C.N., Choi B.Y. Telehealth use among older adults during COVID-19: associations with sociodemographic and health characteristics, technology device ownership, and technology learning. J Appl Gerontol. 2022;41:600–609. doi: 10.1177/07334648211047347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tsao L.R., Villanueva S.A., Pines D.A., Pham M.N., Choo E.M., Tang M.C., et al. Impact of rapid transition to telemedicine-based delivery on allergy/immunology care during COVID-19. J Allergy Clin Immunol Pract. 2021;9:2672–2679.e2. doi: 10.1016/j.jaip.2021.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Banks J., Corrigan D., Grogan R., El-Naggar H., White M., Doran E., et al. LoVE in a time of CoVID: clinician and patient experience using telemedicine for chronic epilepsy management. Epilepsy Behav. 2021;115:107675. doi: 10.1016/j.yebeh.2020.107675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perisetti A., Goyal H. Successful distancing: telemedicine in gastroenterology and hepatology during the COVID-19 pandemic. Dig Dis Sci. 2021;66:945–953. doi: 10.1007/s10620-021-06874-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bitar H., Alismail S. The role of eHealth, telehealth, and telemedicine for chronic disease patients during COVID-19 pandemic: a rapid systematic review. Digit Health. 2021;7 doi: 10.1177/20552076211009396. 20552076211009396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.CDC COVID-19 Response Team Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 - United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnston N., Sears M. Asthma exacerbations . 1: epidemiology. Thorax. 2006;61:722–728. doi: 10.1136/thx.2005.045161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raebel M.A., Schmittdiel J., Karter A.J., Konieczny J.L., Steiner J.F. Standardizing terminology and definitions of medication adherence and persistence in research employing electronic databases. Med Care. 2013;51(8 suppl 3):S11–S21. doi: 10.1097/MLR.0b013e31829b1d2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schatz M., Zeiger R.S., Vollmer W.M., Mosen D., Mendoza G., Apter A.J., et al. The controller-to-total asthma medication ratio is associated with patient-centered as well as utilization outcomes. Chest. 2006;130:43–50. doi: 10.1378/chest.130.1.43. [DOI] [PubMed] [Google Scholar]
- 16.Agency for Healthcare Research and Quality Elixhauser comorbidity software refined for ICD-10-CM. https://www.hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/comorbidity_icd10.jsp
- 17.McCullagh P., Nelder J. 2nd ed. Chapman & Hall/CRC; London, UK: 1989. Generalized Linear Models. [Google Scholar]
- 18.Yuan N., Pevnick J.M., Botting P.G., Elad Y., Miller S.J., Cheng S., et al. Patient use and clinical practice patterns of remote cardiology clinic visits in the era of COVID-19. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.4157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grossman S.N., Han S.C., Balcer L.J., Kurzweil A., Weinberg H., Galetta S.L., et al. Rapid implementation of virtual neurology in response to the COVID-19 pandemic. Neurology. 2020;94:1077–1087. doi: 10.1212/WNL.0000000000009677. [DOI] [PubMed] [Google Scholar]
- 20.Roberts A., Johnston G.H.F., Landells C. COVID-19: pivoting from in-person to virtual orthopedic surgical evaluation. Can J Surg. 2021;64:E101–E102. doi: 10.1503/cjs.022520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Itamura K., Tang D.M., Higgins T.S., Rimell F.L., Illing E.A., Ting J.Y., et al. Comparison of patient satisfaction between virtual visits during the COVID-19 pandemic and in-person visits pre-pandemic. Ann Otol Rhinol Laryngol. 2021;130:810–817. doi: 10.1177/0003489420977766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fung A., Irvine M., Ayub A., Ziabakhsh S., Amed S., Hursh B.E. Evaluation of telephone and virtual visits for routine pediatric diabetes care during the COVID-19 pandemic. J Clin Transl Endocrinol. 2020;22:100238. doi: 10.1016/j.jcte.2020.100238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sabina Sousa C., Trigueiro Barbosa M., Aguiar R., Benito-Garcia F., Morais-Almeida M. What do asthmatic patients think about telemedicine visits? Eur Ann Allergy Clin Immunol. 2021;53:138–142. doi: 10.23822/EurAnnACI.1764-1489.182. [DOI] [PubMed] [Google Scholar]
- 24.Mirsky J.B., Thorndike A.N. Virtual group visits: hope for improving chronic disease management in primary care during and after the COVID-19 pandemic. Am J Health Promot. 2021;35:904–907. doi: 10.1177/08901171211012543. [DOI] [PubMed] [Google Scholar]
- 25.Wittmeier K.D.M., Protudjer J.L.P., Wicklow B.A. Reflections on virtual care for chronic conditions during the COVID-19 pandemic. Can J Diabetes. 2021;45:1–2. doi: 10.1016/j.jcjd.2020.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chang J.E., Lai A.Y., Gupta A., Nguyen A.M., Berry C.A., Shelley D.R. Rapid transition to telehealth and the digital divide: implications for primary care access and equity in a post-COVID era. Milbank Q. 2021;99:340–368. doi: 10.1111/1468-0009.12509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yellowlees P., Nakagawa K., Pakyurek M., Hanson A., Elder J., Kales H.C. Rapid conversion of an outpatient psychiatric clinic to a 100% virtual telepsychiatry clinic in response to COVID-19. Psychiatr Serv. 2020;71:749–752. doi: 10.1176/appi.ps.202000230. [DOI] [PubMed] [Google Scholar]
- 28.Uscher-Pines L., Sousa J., Jones M., Whaley C., Perrone C., McCullough C., et al. Telehealth use among safety-net organizations in California during the COVID-19 pandemic. JAMA. 2021;325:1106–1107. doi: 10.1001/jama.2021.0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heyworth L, Kirsh S, Zulman D, Ferguson JM, Kizer KW. Expanding access through virtual care: the VA’s early experience with Covid-19. NEJM Catal Innov Care Deliv. Published online July 1, 2020. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0327.
- 30.Ferguson J.M., Jacobs J., Yefimova M., Greene L., Heyworth L., Zulman D.M. Virtual care expansion in the Veterans Health Administration during the COVID-19 pandemic: clinical services and patient characteristics associated with utilization. J Am Med Inform Assoc. 2021;28:453–462. doi: 10.1093/jamia/ocaa284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gilson S.F., Umscheid C.A., Laiteerapong N., Ossey G., Nunes K.J., Shah S.D. Growth of ambulatory virtual visits and differential use by patient sociodemographics at one urban academic medical center during the COVID-19 pandemic: retrospective analysis. JMIR Med Inform. 2020;8 doi: 10.2196/24544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaye L., Theye B., Smeenk I., Gondalia R., Barrett M.A., Stempel D.A. Changes in medication adherence among patients with asthma and COPD during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8:2384–2385. doi: 10.1016/j.jaip.2020.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lovinsky-Desir S., Deshpande D.R., De A., Murray L., Stingone J.A., Chan A., et al. Asthma among hospitalized patients with COVID-19 and related outcomes. J Allergy Clin Immunol. 2020;146:1027–1034.e4. doi: 10.1016/j.jaci.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Taquechel K., Diwadkar A.R., Sayed S., Dudley J.W., Grundmeier R.W., Kenyon C.C., et al. Pediatric asthma health care utilization, viral testing, and air pollution changes during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8:3378–3387.e11. doi: 10.1016/j.jaip.2020.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kıymet E., Böncüoğlu E., Şahinkaya Ş., Cem E., Çelebi M.Y., Düzgöl M., et al. Distribution of spreading viruses during COVID-19 pandemic: effect of mitigation strategies. Am J Infect Control. 2021;49:1142–1145. doi: 10.1016/j.ajic.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eid R., Borish L. Eosinophils in antiviral immunity and (perhaps) a benefit of having asthma during the SARS-CoV2 pandemic. Ann Allergy Asthma Immunol. 2021;127:3–4. doi: 10.1016/j.anai.2021.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Williams L.K., Pladevall M., Xi H., Peterson E.L., Joseph C., Lafata J.E., et al. Relationship between adherence to inhaled corticosteroids and poor outcomes among adults with asthma. J Allergy Clin Immunol. 2004;114:1288–1293. doi: 10.1016/j.jaci.2004.09.028. [DOI] [PubMed] [Google Scholar]
- 38.Schatz M., Zeiger R.S. Improving asthma outcomes in large populations. J Allergy Clin Immunol. 2011;128:273–277. doi: 10.1016/j.jaci.2011.03.027. [DOI] [PubMed] [Google Scholar]
- 39.Stanford R.H., Shah M.B., D'Souza A.O., Dhamane A.D., Schatz M. Short-acting β-agonist use and its ability to predict future asthma-related outcomes. Ann Allergy Asthma Immunol. 2012;109:403–407. doi: 10.1016/j.anai.2012.08.014. [DOI] [PubMed] [Google Scholar]
- 40.Cvietusa P.J., Goodrich G.K., Shoup J.A., Steffen D.A., Tacinas C., Wagner N.M., et al. Implementing health care technology research into practice to improve adult asthma management. J Allergy Clin Immunol Pract. 2019;7:908–914. doi: 10.1016/j.jaip.2018.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Portnoy J.M., Waller M., De Lurgio S., Dinakar C. Telemedicine is as effective as in-person visits for patients with asthma. Ann Allergy Asthma Immunol. 2016;117:241–245. doi: 10.1016/j.anai.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 42.Flodgren G., Rachas A., Farmer A.J., Inzitari M., Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015;2015:CD002098. doi: 10.1002/14651858.CD002098.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]