Abstract
Prior to the COVID-19 pandemic, transportation barriers prevented millions of Americans from accessing needed medical care. Then the pandemic disrupted medical and transportation systems across the globe. This research explored ways the COVID-19 pandemic changed how people experienced transportation barriers to accessing health care. We conducted in-depth interviews with social workers, nurses, and other care coordinators in North Carolina to identify barriers to traveling for medical care during the pandemic and explore innovative solutions employed to address these barriers. Analyzing these interviews using a flexible coding approach, we found that the pandemic exacerbated existing transportation barriers and created new barriers. Yet, simultaneously, temporary policy responses expanded the utilization of telehealth. The interviews identified specific advantages of expanded telehealth, including increasing access to mental health services in rural areas, reducing COVID-19 exposure for high-risk patients, and offering continuity of care for COVID-19 patients with other health conditions. While telehealth cannot address all medical needs, such as emergency or cancer care, it may be well-suited for preliminary screenings and follow-up visits. The findings provide insights on how post-pandemic telehealth policy changes can benefit individuals facing transportation barriers to accessing health care and support more accommodating and convenient health care for patients and their families.
Keywords: Care Coordination, COVID-19, Health, Interviews, Telehealth, Transportation Barriers
1. Introduction
Accessing routine and emergency medical care is critical to health and well-being. The transportation system facilitates physical access, but approximately 6 million people in the United States in 2017 reported transportation barriers preventing them from seeking needed medical care (Wolfe et al. 2020). Individuals living in rural areas, racial and ethnic minority groups, and older adults face higher rates of transportation barriers to care leading to poorer health outcomes and worsening of chronic conditions (Wallace et al. 2014).
COVID-19 has disrupted transportation and health systems globally. Service on fixed-route and paratransit systems has decreased and, on some routes, been eliminated (Olin 2020). Availability of ridehailing services such as Uber and Lyft declined particularly at the start of the pandemic (Goldstein 2020). Even for transit and ridehailing services in operation, concerns about COVID exposure may make riders reluctant to use the modes (Cochran 2020a). The potential for carpooling has declined as individuals try to maintain social distance. At the same time, vehicle purchases have increased according to media reports (Boudette 2020).
Health systems also made changes that impacted access during the pandemic. Providers reduced appointments for all but essential medical services (Jain et al. 2020). For services that continued, limits on visitors made access more difficult for some (Brown 2020). But the COVID-19 pandemic also induced innovation that has redefined what it means to access health care. Telehealth emerged as a major force during the pandemic as insurers and the government changed reimbursement and other policies to make it easier for patients and providers to use existing virtual solutions (Faget, 2020, Looney and Huffman, 2020). These disruptions to the health and transportation systems are likely to have reshaped access barriers to care today and—if they persist—have the potential to change barriers in the long term.
The aim of this study was to identify the transportation barriers to care that patients encountered during the pandemic, solutions medical systems used to address these access challenges, and differential impacts of these shifts on the groups traditionally most impacted by transportation barriers. We used semi-structured interviews with social workers, nurses, and other professionals involved in care coordination to assess these topics in depth.
Specifically, this study answers the following questions:
-
•
How did the onset of the COVID-19 pandemic change transportation barriers to accessing health care?
-
•
How were technological innovations utilized during the COVID-19 pandemic to help overcome transportation barriers to accessing health care?
2. Background
The role of transportation as a significant barrier to health care access is well-supported by empirical evidence (Syed et al. 2013). Transportation access is one of many social determinants of health, or the non-medical factors that influence health outcomes. Other important social determinants of health pose barriers that may occur apart from or alongside transportation barriers including cultural and socioeconomic constraints, health literacy limitations, and a scarcity of health care services or supporting infrastructure (e.g., broadband internet services) (Douthit et al. 2015). Prior to COVID-19, in 2017, 5.8 million people in the United States delayed medical care due to lack of transportation (Wolfe et al. 2020). Transportation barriers to accessing health care are multi-faceted, including lack of access to a private vehicle or reliable public transportation, distance and time traveled to reach health care providers, costs associated with transportation, and the inability to operate or utilize transportation options due to disability or limited mobility (Johnson et al., 2003, Syed et al., 2013, Yin, 2019).
People experiencing transportation barriers to health care report late arrivals, canceled/rescheduled, or missed appointments (Wallace et al. 2014), and also missed or delayed medication use (Syed et al. 2013). Ultimately, lack of transportation contributes to poorer health outcomes and the worsening of chronic illnesses—which may result in the need for more costly health care, subsequently (Wallace et al. 2014).
Vulnerable populations are more susceptible to experiencing transportation-related obstacles when accessing health care. A systematic review of literature on transportation barriers to health care access concluded “patients with lower socio-economic status had higher rates of transportation barriers to ongoing health care access than those with a higher socio-economic status,” (Syed et al. 2013 pg. 989). Other groups of particular concern include rural residents (Yin 2019), people with disabilities (Iezzoni et al. 2006), pregnant women (Johnson et al., 2003, Maldonado et al., 2020), as well as racial and ethnic minority groups, older adults, and veterans (Syed et al. 2013).
2.1. COVID-19 pandemic precipitated rapid expansion of telehealth
The onset of the COVID-19 pandemic brought sudden and drastic changes to daily life. In March and April of 2020, partial or statewide stay-at-home orders were issued in most states to reduce the spread of coronavirus; orders were re-instituted in some states in the fall of 2020 (Mervosh et al. 2020). Several trends converged that influenced changes in travel behavior including loss of income from widespread layoffs or reductions in work hours (Parker et al. 2020), and reduced transit capacity due to service cuts or boarding restrictions (De La Garza 2020). Health care access was also impacted where staff at overwhelmed hospitals were faced with diverting patients or delaying transfers and implementing restrictive visitation policies to manage loads of COVID and non-COVID patients (Ali 2020). At some hospitals, elective procedures were postponed in anticipation of needing to reallocate staffing, protective equipment, and beds for COVID patients or to reduce the risk of exposure for non-COVID patients (Jain et al. 2020). Additionally, hospitals and clinics changed visitation and guest policies to reduce the number of people that could accompany a patient seeking care (University of Washington Medicine 2020).
While together these transportation and health care issues threatened to exacerbate existing transportation barriers to health care during the pandemic, it prompted a new pivot in the proliferation of telehealth. Rapid expansion of telehealth utilization during the COVID-19 pandemic was enabled by emergency legislation and executive orders that eased restrictions for telehealth practice related to licensure, reimbursement rates, location requirements, and compliance with the Health Insurance Portability and Accountability Act (HIPAA, Faget, 2020, Looney and Huffman, 2020). These provisions allowed for broader utilization of telehealth to minimize person-to-person contact and reallocate demand for health care away from pandemic hotspots where providers were overwhelmed with caring for COVID-positive patients.
Speaking to the Wall Street Journal, a data expert with the Centers for Medicare & Medicaid Services (CMS) at the U.S. Department of Health and Human Services reported that “beneficiaries receiving telehealth visits [had] gone from about 10,000 a week to 300,000 already for the week ending March 28 [2020],” (The Editorial Board 2020). Some authors distinguish between telehealth—receiving non-physician health care services (appointments with a nurse, pharmacist, etc.) virtually—and telemedicine—meeting with physicians specifically (Weinstein et al. 2013). This paper uses the term telehealth broadly, to include telemedicine and non-physician services.
Telehealth is playing a role in this era of new mobility, where technological innovation is transforming how people travel, enabled by smartphones, tablets, computers and other digital devices (Lewis and Steckler 2020). The development of virtual services, like telehealth, eliminate the need to travel at all in some instances, and have the potential to play an important role in health care access—as experienced during the COVID-19 pandemic. In a letter to the editor of the Journal of Rural Health, Physician Jason Nagata (2020) writes, “The rapid scale-up of telehealth during the COVID-19 pandemic may have long-term implications for access to subspecialty care for people living in rural communities. As more providers are now trained and more practices are now equipped with telehealth infrastructure, these services will likely continue to be offered beyond the pandemic,” (pg. 1).
Building upon previous studies on transportation barriers to health care and the role of technological innovation in the delivery of care, our work makes a novel contribution. This study offers unique insights into the early adaptations that occurred in response to COVID-19 to facilitate continuity of health care in light of transportation challenges—from the perspectives of care coordinators who were positioned on the front lines of the pandemic.
3. Methods
3.1. Learning from care coordinators
Care coordination is provided by social workers, nurses and other practitioners who support patients’ health care utilization by addressing health-related social needs, including transportation issues. Care coordination providers often work with individual patients continuously—giving the providers an opportunity to develop a breadth and depth of knowledge about their patients’ lived experiences with transportation issues.
Fields et al. (2020) found that while interactions between social workers and transportation experts (i.e., engineers and planners) are limited, there is a willingness and potential for greater interprofessional collaboration between the two fields. Specifically, “this collaboration provides an opportunity to adequately serve [vulnerable] populations by re-evaluating long-held practices related to data collection and data analysis within the transportation decision-making process, particularly with regard to the understanding of transportation gaps and needs of vulnerable populations,” (Fields et al. 2020 pg. 5). Care coordinators can offer invaluable insights about transportation challenges and needs of vulnerable populations—and existing strategies and services that address these barriers. As essential workers, care coordinators observed first-hand the transportation barriers to health care access during the COVID-19 pandemic and how patients, transportation services, and medical providers were able to manage these obstacles.
3.2. Sampling and data collection
The qualitative data analyzed in this study were drawn from semi-structured, in-depth interviews—conducted during the Coronavirus pandemic in October and November 2020—about care coordinators’ perspectives on transportation barriers and their thoughts on innovative strategies to overcome transportation barriers to health care. Semi-structured interviews offer a standardized method for gathering information from multiple respondents, while allowing the flexibility to pursue interesting threads that may arise in conversations (Singleton and Straits 2005).
The interview protocol included open-ended questions related to three themes: understanding clients’ transportation challenges and barriers, the impact of the Coronavirus pandemic on transportation access to health care, and perspectives on innovative strategies to address transportation barriers. The questions were informed by the literature on transportation barriers to accessing health care in urban, suburban, and rural contexts. Additionally, the protocol was reviewed by a transportation specialist who works with transportation-disadvantaged seniors in a pilot interview (Arksey and Knight 1999), to incorporate practitioner feedback on the topics and language used in the interview protocol. The Institutional Review Board at the University of North Carolina at Chapel Hill reviewed the interview protocol and determined that the study did not constitute human subjects research as defined under federal regulations.
The interview respondents were identified through referral sampling (Singleton and Straits 2005). Members of the research team contacted individuals from their professional networks to identify a list of potential participants. Due to the COVID-19 pandemic, all interviews were conducted virtually via Zoom in October and November of 2020. The interviews ranged in length from 23 to 49 min and were recorded with respondents’ permission. Following the completion of the interview, respondents received a $5 gift card.
While not a representative sample, the study included variation in geography, setting, and health care specialization. The participants worked in the Research Triangle and Albemarle regions of North Carolina, in a professional capacity that supports patient utilization of health care that includes addressing transportation issues.1 The participants were comprised of employees of hospitals—with backgrounds in social work, nursing, etc.—that serve patients in the two regions and around the state, as well as treatment centers and social service agencies. The participants worked with patients seeking a range of health care services including behavioral health, cancer/oncology, and emergency services. Select respondent characteristics are summarized in Table 1 .
Table 1.
Summary Characteristics of Interview Respondents.
| Sample Characteristics | N = 16 | ||||
|---|---|---|---|---|---|
| Region | |||||
| Albemarle | 4 (25.0%) | ||||
| Triangle | 12 (75.0%) | ||||
| Medical Subspecialty | |||||
| Behavioral Health | 2 (12.5%) | ||||
| Prenatal - Age 5 Care | 5 (31.3%) | ||||
| Comprehensive Cancer Support | 1 (6.3%) | ||||
| Emergency Services | 1 (6.3%) | ||||
| Intellectual or Developmental Disabilities | 2 (12.5%) | ||||
| Kidney Dialysis | 1 (6.3%) | ||||
| Mobility Coordination | 2 (12.5%) | ||||
| Patient Discharge and Transition | 2 (12.5%) | ||||
| Employer | |||||
| County Government | 1 (6.3%) | ||||
| Health Center | 1 (6.3%) | ||||
| Hospital | 9 (56.3%) | ||||
| Regional Health Service | 3 (18.8%) | ||||
| Social Service Agency | 1 (6.3%) | ||||
| State Government | 1 (6.3%) | ||||
3.3. Data cleaning and analysis
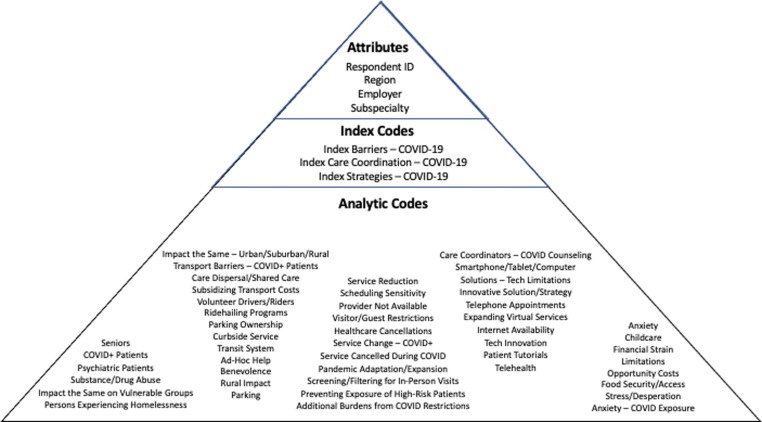
Audio recordings of the interviews were transcribed verbatim and uploaded to Dedoose, a qualitative data analysis (QDA) software. Using the flexible coding method (Deterding and Waters 2018), the text was divided into larger sections with broader structural (i.e., index) codes; these sections were then further parsed using more granular, conceptual and thematic (i.e., analytic) codes. This approach allows for a more focused analysis of subsections of the data, which is particularly effective for a data set that will be used for multiple research endeavors—like the one developed for this study, which included a set of questions related to the pandemic. Responses related to the pandemic were analyzed in this paper. Methods used in this paper closely track those employed by Cochran, 2020a, Cochran, 2020b.
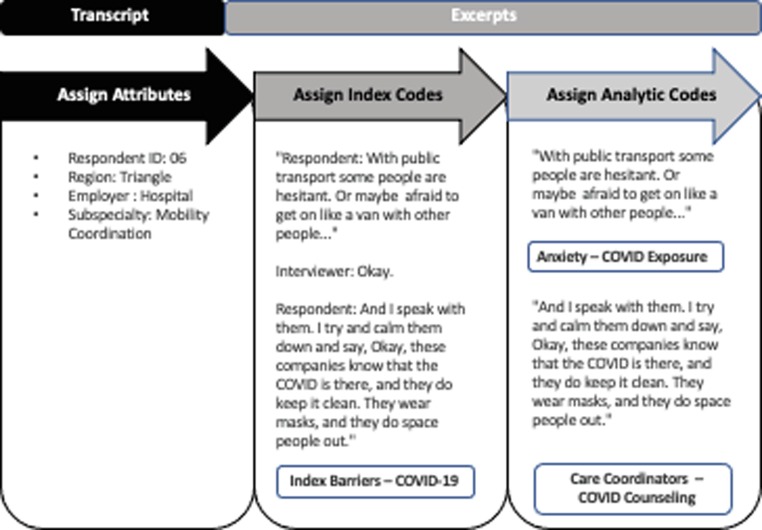
When uploaded to Dedoose, transcripts were ascribed attributes related to the respondent (e.g., region, professional title, health care subspecialty, employment setting, etc.). Next, index codes were applied according to the questions in the interview protocol. Examples of index codes applied include “Index Community Served” and “Index Barriers – COVID-19.” A final set of analytic codes were applied, specific to the topic of this paper: transportation barriers to accessing health care experienced during the COVID-19 pandemic and innovative strategies to address these challenges. The analytic codes comprised of a combination of codes informed by the research questions as well as themes that emerged inductively. Examples of analytic codes applied included: “Anxiety – COVID Exposure” and “Care Coordination – COVID.“ The flexible coding process is illustrated in Fig. 1 . Inter-rater reliability was not a concern in our coding process as this article’s primary author, L. Oluyede, applied all analytic codes.
Fig. 1.
Example of Flexible Coding Process. Figure adapted from Cochran (2020a, Fig. 1) with author’s permission.
This paper focuses on the experience with transportation barriers during the COVID-19 pandemic and the innovative solutions that were utilized to address these challenges. A second paper focused on understanding transportation barriers and solutions under more typical conditions—i.e., not during a pandemic (Oluyede et al., 2022). Accordingly, an analysis of data assigned to the analytic codes identified themes around transportation barriers to accessing health care and the role of telehealth as an innovative strategy during the pandemic.
Fig. 2 displays the coding scheme for this paper. Three index codes were used for this paper, corresponding with the responses to questions 9, 10 and 18 in the interview protocol, respectively (see Appendix A). If information pertaining to the COVID-19 pandemic was provided as part of the response to other questions, the appropriate COVID-19 index code was applied to that excerpt as well. The list of analytic codes includes all thematic codes that were assigned to excerpts associated with any of the three identified index codes.
Fig. 2.
Coding Scheme by Flexible Coding Categories.
4. Findings
Our findings indicate that the COVID-19 pandemic exacerbated existing transportation barriers to accessing health care as well as created new challenges. Yet, the pandemic prompted a new pivot with the proliferation of telehealth. Virtual visits enabled remote access for patients to a broad range of health care services, thereby bypassing the need for transportation during an especially precarious time. Our findings offer insights from care coordinators from their experiences with patients or clients.
4.1. COVID-19 pandemic exacerbated existing transportation barriers
Respondents observed that the pandemic heightened existing transportation barriers. Overall, there were higher levels of stress and financial strain in patients during the COVID-19 pandemic—which affected transportation as well. One care coordinator conveyed, “People have lost jobs, lost household income…The pandemic has just exacerbated everybody's financial challenges.”
The pandemic impacted the realms of health care and transportation—which combined, presented unique challenges for traveling to access health care. For patients who travel via private vehicle to seek health care, gas and parking costs were noted as being prominent issues, particularly for low-income patients already facing additional financial strain during the pandemic. A care coordinator at a hospital mentioned that during the first wave of the pandemic, parking costs were eliminated at the hospital but once hospitalizations began to wane, patients had to pay for parking once again. At this same hospital, all obstetrics clinics closed and when they eventually reopened, some were moved to other locations that offered free parking. However, this decision proved inequitable:.
“Ironically, though, the main obstetrics clinic (located at the main hospital, which does not have free parking) that's been reopened does have a large number of people who have Medicaid or self-pay as their insurance source. So, some of the low-income patients were being penalized by having to pay for parking at the hospital, when there are many people not having to pay parking depending on the alternate location of their prenatal care.”
4.2. COVID-19 created new transportation barriers
New transportation barriers emerged during the pandemic as well. Respondents noted disruptions to visitation and guest policies—including closed waiting rooms and/or restrictions on the number of people who could accompany or visit patients in hospitals, clinics and other facilities—which created logistical challenges. Specifically, a few care coordinators noted the need to arrange for—and potentially transport—children to attend childcare because they were not allowed to be with family members seeking health care. Lobby closures created additional inconveniences, requiring that any accompanying guests waited outside during an appointment. A care coordinator recalled a scenario with the parents of an infant in a neonatal intensive care unit where the parents commented, “We’re not going to drive two or three hours to the hospital, when only one of us can come into the hospital…And the other is just going to sit in the car in the garage.”
The pandemic created new barriers to accessing health care for some patients without access to a private vehicle. One care coordinator said:
“I think at the beginning, when this first started, there was just a lot of uncertainty on all parts but particularly on the part of patients. What was this going to mean? Were they going to be able to continue riding public transportation? Were they going to be safe riding public transportation?”
The extent of service disruption differed in the two regions that were the focus of this study. A respondent in the Triangle region said, “I haven’t seen any major disruptions in transportation.” Meanwhile, a respondent in Albemarle, referring to local transit that carries trips to medical appointments, remarked, “the transportation was totally shut down at one point.” Where transit service was stopped, reduced, or enforced limited ridership, it was more difficult for patients to arrive to appointments on time. Respondents identified other transportation services that stopped operating altogether (at least temporarily), including a volunteer driver program. As a result, some patients resorted to seeking rides with a family member—a task made even more cumbersome during the pandemic. Family members residing outside of a patient’s household might have been reluctant to provide a ride out of concern about the risk of exposure to the virus. Similarly, patients may have been hesitant to ask friends or family members for help, fearing their risk of exposure would be elevated or that asking would be too burdensome. This aligns with other literature indicating concerns about getting needed assistance with transportation during the pandemic can be both personal and relational (Cochran 2020a).
Additionally, one care coordinator mentioned, with work schedules deeply impacted by the pandemic, working family members could be more hesitant to take time off or request schedule modifications to oblige requests for rides. For instance, when scheduling appointments for COVID-19 testing prior to labor induction or a Caesarean delivery, patients were asked “what day is best for them?” The care coordinator explained:
“I try to be very sensitive to the fact that there are some patients that depend on their significant other or a sister or a friend to bring them for their appointments. And it needs to be done around the time that the other person would not be needing to work because they’ve been out of work quite a bit.”
Transportation options were even more limited for COVID-positive patients without access to a private vehicle. A care coordinator explained the dilemma:
“When COVID patients get discharged and they have no means of transportation, we can’t put them in a Lyft, of course Lyft won’t take a COVID-positive rider…And there are times where families don’t want to take the COVID-positive patient home…It’s another barrier to getting people discharged from the hospital.”
In some instances, accommodations for patients testing positive for COVID-19 impacted health care routines. For example, a care coordinator at a dialysis clinic explained that patients confirmed or suspected of having COVID-19 were diverted to another location for treatment. This alternate location was not as accessible using local transit services, and thus contracting COVID-19 caused a change in patients’ usual care routine that was less viable for individuals without access to a private vehicle and dependent on public transportation for travel.
In addition to transportation barriers related to the availability of transportation options, the pandemic also presented an emotional barrier. Consistent with other literature examining transportation barriers during the pandemic (see Cochran 2020a), patients were anxious about their exposure to COVID while traveling—especially when using a service that required interaction with strangers, including public transportation, van transport, and ridehailing. Describing the experience with patients’ anxiety, one care coordinator said:
“I have some patients who are anxious, very anxious about getting into a vehicle. I basically just talk them through it and just let them know that the van service or the Lyft service is fairly safe; they follow their protocols. Lyft is not a small company, so they have protocols set in place. The drivers wear masks, nobody is allowed in the front seat, and they keep their cars clean. And I speak with them, I try and calm them down and say, ‘Okay, these companies know that COVID is out there….’”
4.3. Rapid expansion of telehealth during pandemic
The COVID-19 pandemic saw a proliferation of telehealth—both the expansion of existing services and the creation of new ones. Several respondents noted a precipitous increase in the utilization of telehealth as cities and states began to implement stay-at-home orders. One care coordinator noted that “the push for telehealth really came to the forefront.” Another remarked, “I went from having very few checkups, to more people using telehealth now. Now, quite a few actually.” Prior to the pandemic, the adoption of telehealth for mental health services was limited, attributed in part to low reimbursement rates from insurers (Wilson et al. 2017). However, a care coordinator noted that among patients, “mental health services were extremely limited to begin with, and now the majority of those are doing telehealth.”
In addition to the expansion of existing telehealth services, new virtual services were established during the pandemic. A hospital neonatal intensive care unit piloted the use virtual rounding. The staff repurposed the telehealth platform used in outpatient clinics to allow families to participate in the daily meetings of the full care team to discuss the patient’s status and treatment plan. According to the care coordinator, initial feedback on the virtual rounding was positive:
“We really encourage parents to be present so that they can be up to date on their infant’s status…It’s hard for people to get to the hospital for daily rounding because the parents of a lot of these babies are back at work. I think we’re going to start trying to roll [virtual rounding] out more, we’ve gotten great feedback.”
Another example of new virtual services established during the pandemic is a hospital maternity ward that made its programming available online, including a virtual tour of the maternity ward and online childbirth classes to reduce patient visits. Also, a care coordinator observed that some Alcoholics Anonymous (AA) meetings had become virtual during the pandemic, given that restrictions on gathering size and social distancing limited the number of attendees at in-person meetings.
These findings indicate the expansion of virtual services during the pandemic beyond telehealth, to a broader range of health-related support programming like facility tours and behavioral support groups. According to one care coordinator, the increased availability of telehealth “really alleviated the transportation stressor” and another observed that telehealth appointments allowed patients to avoid riding the bus to access health care during the pandemic. Thus, telehealth addressed both general transportation-related barriers, including distance, cost, and vehicle or transit availability—which were exacerbated in the pandemic—as well as the pandemic-related barriers such as the avoidance of public transit to reduce exposure to the coronavirus.
4.4. Telehealth expanded during pandemic, but was not a panacea
Respondents noted that telehealth services are particularly effective for preliminary screenings and follow-up care. Telehealth is being used for screening appointments to determine whether an in-person visit is necessary. One care coordinator remarked, “[Telehealth] gives a provider the opportunity to be more thoughtful about who actually has to come in. The virtual visit is an intermediate step.”
Telehealth is also being used for follow-up appointments, in instances where patients only need to see the provider, but labs or treatments are not required. Respondents from multiple medical subspecialties expressed additional benefits of using telehealth, including: to avoid taking high-risk premature infants in public, provide mental health services to patients in rural areas who cannot access the nearest provider, and increase the chances of compliance for patients receiving addiction or psychiatric care who “are a bit more ambivalent, their motivation is not quite as high,” to commit to ongoing care.
However, telehealth has not been a perfect substitute for in-person care during the pandemic; there are limitations. Telehealth is not suitable for appointments where lab work, scans, procedures, or treatment is involved, for example emergency care or many types of cancer treatment. Perspectives on the effectiveness of telehealth for substance abuse or addiction care diverged. Despite expanding access for patients, a respondent remarked that substance abuse or addiction appointments are difficult to manage via telehealth, specifically that some patients “found that they wanted a little bit more personal connection and felt like the telehealth visit wasn’t enough for them.”
Technology presented several issues for telehealth utilization, including internet availability or reliability, access to a mobile device or computer, and patients’ technological savviness. In some regions in North Carolina, such as the rural northeastern part of the state, internet connectivity is limited. Without solid internet service, patients may experience difficulty accessing the telehealth platform or be unable to participate in the virtual appointment due to diminished visual or audio quality. One care coordinator noted, “[Internet service] is typically reliable, but every now and then there are some glitches.”
Access to an internet-enabled mobile device (e.g., smartphone or tablet) or computer is also required for patients to utilize telehealth services. The care coordinators expressed that most patients they encounter have access to a smartphone. However, certain populations experience reduced smartphone access, including the elderly, and Medicaid-eligible patients with low incomes. A care coordinator who works with children at high risk for poor health, reported that some low-income families are not able to keep up with cell phone plan payments. This results in multiple phone number changes, making it difficult for the care coordinator to keep in contact: “I’ve got clients right now I’ve been trying to find for two or three months.”
Lastly, technological literacy poses an obstacle for patients using telehealth, and the literacy levels primarily vary by age. A care coordinator who interfaces with a range of clinical services remarked on ease of telehealth use among patients:
“It varies among age of the patients. The younger patients are very tech savvy. It's easy for them to be able to do a telehealth visit at home. We’ve done that for behavioral health, primary care, family planning, all of those kinds of things. It doesn't work as well for some of the older patients that we see. As they don't have the technology skills, or maybe not even have a cell phone or something they can access the telehealth platform with.”
Given the need for quick adoption during the pandemic, some patients faced a steep learning curve when using the telehealth platforms. One care coordinator commented, “one of the hardest things is just teaching patients on a virtual platform how to use a virtual platform.” When a web-enabled telehealth appointment is not possible, a provider may resort to a telephone appointment without a virtual component.
4.5. “Telehealth is here to stay”: Pandemic telehealth use reveals future opportunities
“Telehealth is here to stay,” proclaimed one respondent, a transportation specialist who works with the elderly. Multiple respondents held the opinion that telehealth and other virtual services will continue to play a more significant role in the delivery of health care as cities and states reopen:
“I can see in the future telehealth will probably continue. It'll be the best for the patients. This will just be the new rule for how we'll do things in the future.”
“Telehealth has been great, and I think should be more frequently utilized, especially for rural residents who might not be able to get to the nearest mental health provider…COVID or non-COVID, or whatever.”
“They should have been doing virtual rounding before; the pandemic forced a really good change.”
These interviews with care coordinators illuminated some specific advantages of expanded telehealth offerings:
-
•
Increasing access in rural a reas to mental health services – In rural areas with a dearth of providers, patients may face multiple transportation barriers to accessing health care. Telehealth and other virtual services offer a viable workaround. One care coordinator said about the role of telehealth in expanding access to mental health services, “Telehealth has been great, and I think should be more frequently utilized, especially for people living in rural areas who might not be able to get to the nearest mental health provider.” This insight aligns with Nagata's (2020) assertion that the rapid expansion of telehealth will have long-term benefits for rural areas, particularly related to access to mental health services.
-
•
Reducing COVID-19 exposure for high-risk patients – During the pandemic, it has been critical to reduce COVID-19 exposure for immunocompromised patients, including seniors and infants born prematurely. A care coordinator with a neonatal intensive care unit remarked, “Telehealth visits are beneficial…Just the fact that you’re not always having to take the infant in public to see a provider, they’re a high-risk population anyway.”
-
•
Offering care continuity for COVID patients – Care coordinators observed instances where COVID-19 exposure or diagnosis impacted other ongoing care. Telehealth has helped to reduce this disruption. One care coordinator commented, “A lot of our patients struggle with addiction or psychiatric issues, and so they require extensive follow-up. But there’s no facility or program that will take a COVID-19-positive person struggling with addiction, if they require any kind of inpatient treatment—that’s not an option…So, that’s why telehealth has been great because there are intensive outpatient programs that are available via telehealth.”
One respondent raised another important consideration for the future of telehealth, specifically that it has the potential to support patients with varying levels of illness. Traditionally, research on transportation barriers has focused on external factors—distance, cost, and the availability of transportation—but has rarely acknowledged the simple notion of whether patients are well enough to travel. Preventive care aside, patients seeking health care are likely experiencing disease or chronic illnesses that affect their physical or mental well-being. When patients are not well, utilizing transportation can be a barrier to accessing health care regardless of distance, cost, or availability. A social worker who supports cancer patients, explained this dilemma:
“If a patient has a vehicle but they are not well enough to drive, or they don’t have someone to drive them, it's a problem because a lot of them are too sick to ride the bus. Riding the bus, standing, doing transfers…walking three blocks from one bus to another, it's just not realistic even if the bus system is decent. And so, they're going to have the same transportation problems as a patient without a vehicle.”
Comments from a social worker who provides outpatient behavioral health services underscored this point:
“Someone who is very depressed might be in a terrible mood and doesn’t have the wherewithal that day to get up and put themselves together and get out of a building, but they are capable of talking on the phone or maybe seeing the provider for telehealth. So, there’s been an increase in what we call our ‘show rate,’ people that show up for their appointments…I forgot what the percentage was, but in the first month that we did telehealth, my numbers skyrocketed. There were a couple of contributing factors, but I would see an average of 70 people a month and once we started doing telephone and telehealth appointments, my number went up to 105.”
Therefore, offering telehealth potentially offers convenience for a range of patients seeking care from a myriad of subspecialties, but also holds potential for patients who are not well enough to travel.
5. Conclusion and policy implications
5.1. Strengths and limitations
The interviews were conducted via Zoom, a cloud-based videoconferencing platform. Zoom is a viable method for qualitative data collection: its visual element supports rapport during interviews; it offers greater flexibility for scheduling; it allows participant recruitment from remote areas; and the platform is relatively easy to use (Archibald et al. 2019). In addition to these advantages, using Zoom for this study was critical to protecting the safety of the researchers and respondents by eliminating the risk of exposure to COVID-19. Using Zoom also allowed the study to extend the scope of the project to the Albemarle region, not limiting the study to the Triangle region where the researchers were located.
This study was not designed to produce a representative sample of any larger population of care coordinators. While the research design used a nonprobabilistic referral sampling method, it was guided by a purposive approach that sought to reflect important sources of variation in the sample (Singleton and Straits 2005). The sources of variation included: medical subspecialty, region, and care coordination setting (e.g., hospital, social service agency, etc.). Additional participants were not recruited due to time constraints. Though this may have limited the study sample—due to a condensed window of time to recruit and conduct interviews—the timeframe allowed for the researchers to capture respondents’ perspectives amid the COVID-19 pandemic, thereby minimizing recall bias.
5.2. Policy implications
“It seems unlikely that the health care industry will ever return to a world where telehealth is the exception.” - Kyle Faget, Health Care Regulatory Attorney (2020).
While many of the policy changes to expand telehealth during the onset of the COVID-19 pandemic were executed through temporary orders and waivers, there have been efforts to permanently codify these telehealth advances. For example, the proposed 2021 Physician Fee Schedule for Medicare coverage includes new telehealth services to be covered, including Group Psychotherapy and Neurobehavioral Status Exam. Faget (2020) believes that the proposed schedule “may be a bellwether for which telehealth adjustments made during the height of the COVID-19 pandemic will become permanent,” but that not all changes will see permanence, stating: “At some point it will likely make sense to transition back to use of HIPAA compliant platforms for delivery of health care via telehealth.”.
Given the insights from care coordinators in this study, permanent policy changes that remove geographic and location requirements, widen the range of services eligible for telehealth appointments, and allow for telephone use will help make telehealth a more viable solution for individuals facing transportation barriers to accessing health care. Such changes would eliminate the transportation stressor for certain types of appointments. Additionally, these changes could help expand health care access for specific populations, including residents in rural areas who may face a dearth of providers and transportation options, and the elderly or low-income residents who may not have access or the expertise to use video-enabled platforms. Furthermore, as demonstrated in this study, the expansion of the use of telehealth platforms to incorporate other services (e.g., virtual rounding) can support more accommodating and convenient health care for patients and their families. Future efforts to support the permanent expansion of telehealth can help address transportation barriers to accessing health care as well as build resilience by equipping communities to be better prepared for future pandemics or other widespread public health emergencies.
CRediT authorship contribution statement
Lindsay Oluyede: Methodology, Investigation, Project administration, Formal analysis, Writing – original draft. Abigail L. Cochran: Investigation, Conceptualization, Writing – review & editing. Mary Wolfe: Conceptualization, Methodology, Writing – review & editing. Lauren Prunkl: Investigation, Data curation, Visualization. Noreen McDonald: Supervision, Conceptualization, Funding acquisition, Methodology, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
We are extremely grateful to all study respondents for sharing their time and valuable insights, especially while serving as essential workers on the frontline of the COVID-19 pandemic. We also thank three anonymous reviewers of this article for their helpful comments.
Financial Disclosure
This work was supported by the U.S. Department of Transportation through the Southeastern Transportation Research, Innovation, Development, and Education (STRIDE) Center. This funding body had no role in study design; data collection, analysis, and interpretation; nor in the writing of the manuscript.
Acknowledgments
Acknowledgements
Financial Disclosure
Footnotes
The Triangle region is home to Raleigh, Durham, and Chapel Hill. The Albemarle region is located in northeastern North Carolina, and includes Bertie, Camden, Chowan, Currituck, Gates, Hertford, Pasquotank, and Perquimans counties.
Appendix A: Interview protocol
Social service providers’ perspectives on transportation barriers and innovative strategies in accessing health care
Understanding Clients’ transportation challenges and barriers
-
1.
To begin, please describe the responsibilities of a [the position held by the respondent] (e.g., social worker, case manager, hospital intake/discharge coordinator, etc.)].
-
2.How would you describe the community that you serve in this position?
-
a.Does it have urban, suburban, and rural areas? Or all?
-
a.
-
3.In broad terms, which vulnerable groups are represented among your clients? For example, persons with disabilities or chronic illnesses, persons with low-income, communities of color, seniors, non-English speakers, etc.?
-
a.Are there any other vulnerable groups that come to mind that are included among your clients, aside from the more traditional categories?
-
a.
-
4.
Overall, is transportation a challenge for your clients? How often do you hear about transportation issues from clients or colleagues (speaking about their own clients)?
-
5.From your experience, what types of transportation challenges and barriers are your clients dealing with? What are common complaints from your clients or colleagues?
-
a.Issues with access—Securing/maintaining private vehicles, public transit availability, etc.?
-
b.Issues with connectivity—Are there particular destinations that they have trouble traveling to, such as jobs, schools, childcare, grocery stores, etc.?
-
c.What about health care specifically (e.g., clinics, hospitals, etc.)?
-
d.Complications with traveling across geographic boundaries?
-
e.Issues with trip planning—How well do they understand the transportation options available to them? Do they take into account planning to get to and from their destination?
-
f.Issues with transportation costs—Are clients able to afford the transportation options available?
-
g.Issues with emotional barriers—Do some of your clients express discomfort or reluctance about using the services available? For example, public transit.
-
h.In your experience, how big of an issue is the qualification process for various services? For example, ADA paratransit requires specific approval processes. Can you talk about this and other approval processes that either expedite, or hinder, access for your clients? Is the turnaround time for the application process an issue?
-
i.Are there other issues that you’ve seen, related to transportation challenges and barriers, that we haven’t yet discussed?
-
a.
-
6.
[Ask if service area has an urban/suburban/rural mix.] Of the various transportation challenges and barriers you just mentioned, are some more prevalent in the urban, suburban or rural areas?
-
7.
Again, of the various transportation challenges and barriers you mentioned, are there certain challenges that pertain to one vulnerable population versus another?
-
8.
How does a ____________ [position identified in question #1] support clients to help them address transportation challenges or barriers?
Impact of the Coronavirus pandemic
-
9.In what ways have your clients’ transportation challenges or barriers changed during the Coronavirus pandemic?
-
a.How has the impact of the pandemic varied across urban, suburban or rural areas?
-
b.How has the impact of the pandemic differed across various vulnerable populations?
-
a.
-
10.
During this pandemic, how has the role of a ____________ [position identified in question #1] changed related to helping clients address transportation challenges or barriers?
Perspectives on innovative strategies to address transportation barriers
-
11.What are new programs or initiatives in your area to help address transportation barriers?
-
a.This may include innovations like on-demand transit (requesting rides on transit vehicles with no fixed route or timetable), telehealth or telemedicine (meeting with medical providers remotely through videoconferencing), volunteer driving program, software platforms that allow for scheduling medical appointments and transportation at the same time, etc.
-
a.
-
12.
[Ask if there are not any new programs and initiatives, then skip to question 19.] What obstacles prevent these types of innovative programs and initiatives from being implemented in your area?
-
13.
[Ask if service area has an urban/suburban/rural mix.] Which of these programs or initiatives serve urban areas? Suburban areas? Rural areas?
-
14.
What feedback, both good and bad, have you received from your clients or from colleagues about each of these programs or initiatives?
-
15.In your opinion, how has the introduction of these programs or initiatives impacted your clients?
-
a.Particularly, has there been an impact on how they access health care services?
-
b.Of the vulnerable groups we talked about earlier, are some more likely than others to utilize these programs or initiatives, from your experience? Why is that?
-
a.
-
16.What role does technology play in using these programs or initiatives and how does this affect your clients?
-
a.Is a smartphone, tablet, or computer with Internet required?
-
a.
-
17.Are there any barriers to your clients utilizing these new programs and initiatives?
-
a.In your opinion, are there any changes that could be made to better serve your clients and vulnerable populations, in general?
-
a.
-
18.
In what ways have these programs or initiatives been impacted by the Coronavirus pandemic?
-
19.
Do you have other thoughts or comments that you’d like to share about anything we’ve talked about today?
References
- Ali, S. S. 2020. “Diversion and Transfer Delays Plague Hospitals Overwhelmed by COVID-19 Cases.” NBC News. Retrieved November 19, 2020, from https://www.nbcnews.com/news/us-news/diversions-transfer-delays-plague-hospitals-overwhelmed-covid-19-cases-n1248014.
- Archibald, M. M., Ambagtsheer, R. C., Casey, M. G., and Lawless, M., 2019. “Using Zoom Videoconferencing for Qualitative Data Collection: Perceptions and Experiences of Researchers and Participants.” International Journal of Qualitative Methods (18): 1-8. https://journals-sagepub-com.libproxy.lib.unc.edu/doi/pdf/10.1177/1609406919874596.
- Arksey, H., & Knight, P. T. 1999. “Interviewing for Social Scientists.” London: SAGE Publications. https://dx.doi.org/10.4135/9781849209335.
- Boudette, N. E. 2020. “Looking to Buy a Used Car in the Pandemic? So Is EveryoneElse” New York Times. Retrieved December 15, 2020, from https://www.nytimes.com/2020/09/07/business/used-cars-pandemic.html.
- Brown, T. 2020. “Families say they can’t see children with disabilities as hospitals battle coronavirus.” The News & Observer. Retrieved December 15, 2020, from https://www.newsobserver.com/news/coronavirus/article242367531.html.
- Cochran A.L. Impacts of COVID-19 on Access to Transportation for People with Disabilities. Transportation Research Interdisciplinary Perspectives. 2020;8(November) doi: 10.1016/j.trip.2020.100263. [DOI] [Google Scholar]
- Cochran A.L. Understanding the Role of Transportation-Related Social Interaction in Travel Behavior and Health: A Qualitative Study of Adults with Disabilities. Journal of Transport & Health. 2020;19(December) doi: 10.1016/j.jth.2020.100948. [DOI] [Google Scholar]
- De La Garza, A. 2020. “COVID-19 Has Been 'Apocalyptic' for Public Transit. Will Congress Offer More Help?” Time. Retrieved November 19, 2020, from https://time.com/5869375/public-transit-coronavirus-covid/.
- Deterding N.M., Waters M.C. Flexible Coding of In-Depth Interviews: A Twenty-First-Century Approach. Sociological Methods and Research. 2021;50(2):708–739. [Google Scholar]
- Douthit N., Kiv S., Dwolatzky T., Biswas S. Exposing Some Important Barriers to Health Care Access in the Rural USA. Public Health. 2015;129(6):611–620. doi: 10.1016/j.puhe.2015.04.001. [DOI] [PubMed] [Google Scholar]
- Faget, K. Y. 2020. “Telehealth Today and in a Post-COVID-19 World.” Foley & Lardner LLP. Retrieved December 13, 2020, from https://www.foley.com/en/insights/publications/2020/09/telehealth-today-and-in-a-post-covid19-world).
- Fields N.L., Miller V.J., Cronley C., Hyun K.(., Mattingly S.P., Khademi S., Nargesi S.R.R., Williams J. Interprofessional collaboration to promote transportation equity for environmental justice populations: A mixed methods study of civil engineers, transportation planners, and social workers' perspectives. Transportation Research Interdisciplinary Perspectives. 2020;5:100110. [Google Scholar]
- Goldstein, M. 2020. “What Is The Future For Uber And Lyft After The Pandemic?” Forbes. Retrieved December 15, 2020, from https://www.forbes.com/sites/michaelgoldstein/2020/07/27/what-is-the-future-for-uber-and-lyft--after-the-pandemic/?sh=6067aa5f3bc8.
- Iezzoni, Lisa I., Mary B. Killeen, and Bonnie L. O’Day. 2006. “Rural Residents with Disabilities Confront Substantial Barriers to Obtaining Primary Care.” Health Services Research 41 (4p1): 1258–75. 10.1111/j.1475-6773.2006.00534.x. [DOI] [PMC free article] [PubMed]
- Jain, A., Dai, T., Bibee, K., and Myers, C. 2020 “Covid-19 Created an Elective Surgery Backlog. How Can Hospitals Get Back on Track?” Harvard Business Review. Retrieved December 15, 2020, from https://hbr.org/2020/08/covid-19-created-an-elective-surgery-backlog-how-can-hospitals-get-back-on-track.
- Johnson A.A., El-Khorazaty M.N., Hatcher B.J., Wingrove B.K., Milligan R., Harris C., Richards L. Determinants of Late Prenatal Care Initiation by African American Women in Washington, DC. Maternal and Child Health Journal. 2003;7(2):103–114. doi: 10.1023/A:1023816927045. [DOI] [PubMed] [Google Scholar]
- Lewis, R., and Steckler, R. 2020. “Emerging Technologies and Cities: Assessing the Impacts of New Mobility on Cities.” National Institute for Transportation and Communities. https://nitc.trec.pdx.edu/research/project/1249/Emerging_Technologies_and_Cities:_Assessing_the_Impacts_of_New_Mobility_on_Cities.
- Looney, K. H. and Huffman, M. A. 2020. “That Was Then and This Is Now—How the COVID-19 Crisis Changed Telehealth Services: Are the Changes Here to Stay?” American Health Law Association. Retrieved December 13, 2020, from https://www.americanhealthlaw.org/content-library/connections-magazine/article/55a5ad47-302e-41f4-8e83-c1c1813c48a4/that-was-then-and-this-is-now-how-the-covid-19-cri.
- Maldonado L.Y., Fryer K.E., Tucker C.M., Stuebe A.M. The Association between Travel Time and Prenatal Care Attendance. American Journal of Perinatology. 2020;37(11):1146–1154. doi: 10.1055/s-0039-1692455. [DOI] [PubMed] [Google Scholar]
- Mervosh, S., Lu, D., and Swales, V. 2020. “See Which States and Cities Have Told Residents to Stay at Home.” New York Times. Retrieved November 19, 2020, from https://www.nytimes.com/interactive/2020/us/coronavirus-stay-at-home-order.html.
- Nagata, J.M., MD, MSc. 2020. Rapid scale‐up of telehealth during the COVID‐19 pandemic and implications for subspecialty care in rural areas. The Journal of Early Health / Early View. https://onlinelibrary.wiley.com/doi/full/10.1111/jrh.12433. [DOI] [PubMed]
- Olin, A. 2020. “Public transit has lost its momentum during the pandemic. Can it be regained?” Rice Kinder Institute for Urban Research. Retrieved December 15, 2020, from https://kinder.rice.edu/urbanedge/2020/08/05/coronavirus-pandemic-houston-metro-public-transit-ridership.
- Oluyede Lindsay, Cochran Abigail L., Prunkl Lauren, Wang Jueyu, Wolfe Mary, McDonald Noreen. Transportation Research Interdisciplinary Perspectives. 2022;13(100565) doi: 10.1016/j.trip.2022.100565. [DOI] [Google Scholar]
- Parker, K., Minkin, R. And Bennett, J. 2020. “Economic Fallout from COVID-19 Continues to Hit Lower-Income Americans the Hardest.” Pew Research Center: Social and Demographic Trends. Retrieved December 15, 2020, from https://www.pewsocialtrends.org/2020/09/24/economic-fallout-from-covid-19-continues-to-hit-lower-income-americans-the-hardest/.
- Singleton R.A., Straits B.C. 4th ed. Oxford University Press; New York, NY: 2005. Approaches to Social Research. [Google Scholar]
- Syed S.T., Gerber B.S., Sharp L.K. Traveling towards Disease: Transportation Barriers to Health Care Access. Journal of Community Health. 2013;38(5):976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Editorial Board. 2020. “The Doctor will Zoom You Now: The pandemic lockdown is proof of concept for mass telemedicine.” Wall Street Journal. Retrieved December 14, 2020, from https://www.wsj.com/articles/the-doctor-will-zoom-you-now-11587935588.
- University of Washington Medicine. 2020. “COVID-19 Visitor Policy.” Retrieved December 15, 2020, from https://www.uwmedicine.org/coronavirus/visitor-policy.
- U.S. Department of Health and Human Services. 2020. “The HIPAA Privacy Rule.” Retrieved December 13, 2020, from https://www.hhs.gov/hipaa/for-professionals/privacy/index.html.
- Wallace R., Hughes-Cromwick P., Mull H., Khasnabis S., Wallace R., Hughes-Cromwick P., Mull H. Access to Health Care and Nonemergency Medical Transportation Two Missing Links. Transportation Research Record: Journal of the Transportation Research Board. 2005 doi: 10.1177/0361198105192400110. [DOI] [Google Scholar]
- Weinstein R.S., Lopez A.M., Joseph B.A., Erps K.A., Holcomb M., Barker G.P., Krupinski E.A. Telemedicine, Telehealth, and Mobile Health Applications That Work: Opportunities and Barriers. American Journal of Medicine. 2014 doi: 10.1016/j.amjmed.2013.09.032. [DOI] [PubMed] [Google Scholar]
- Wilson F.A., Rampa S., Trout K.E., Stimpson J.P. Telehealth Delivery of Mental Health Services: An Analysis of Private Insurance Claims Data in the United States. Psychiatric Services. 2017;68(12):1303–1306. doi: 10.1176/appi.ps.201700017. https://doi-org.libproxy.lib.unc.edu/10.1176/appi.ps.201700017 [DOI] [PubMed] [Google Scholar]
- Wolfe M.K., McDonald N.C., Holmes G.M. Transportation Barriers to Health Care in The United States: Findings From the National Health Interview Survey, 1997–2017. American Journal of Public Health. 2020;110(6):815–822. doi: 10.2105/AJPH.2020.305579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin Ping. Urban–Rural Inequalities in Spatial Accessibility to Prenatal Care: A GIS Analysis of Georgia, USA, 2000–2010. GeoJournal. 2019;84(3):671–683. doi: 10.1007/s10708-018-9884-1. [DOI] [Google Scholar]