Abstract
Recent studies suggest that the COVID-19 pandemic can serve as a unique psychosocial stressor that can negatively impact individuals with chronic pain. Using a large online sample in the U.S., the present study sought to investigate the impact of the pandemic on the trajectories of pain severity and interference, emotional distress (ie, anxiety and depressive symptoms), and opioid misuse behaviors across one year. Potential moderating effects of socio-demographic factors and individual differences in pain catastrophizing, pain acceptance, and sleep disturbance on outcome trajectories were also examined. Adults with chronic pain were surveyed three times across 1 year (April/May 2020 [N = 1,453]; June/July 2020 [N = 878], and May 2021 [N = 813]) via Amazon's Mechanical Turk online crowdsourcing platform. Mixed-effects growth models revealed that pain severity and interference, emotional distress, and opioid misuse behaviors did not significantly deteriorate across one year during the pandemic. None of the socio-demographic factors, pain catastrophizing, or sleep disturbance moderated outcome trajectories. However, individuals with higher pain acceptance reported greater improvement in pain severity (P< .008, 95% CI: -.0002, -.00004) and depressive symptoms (P< .001, 95% CI: -.001, -.0004) over time. Our findings suggest that the negative impact of the pandemic on pain, emotional distress, and opioid misuse behaviors is quite small overall. The outcome trajectories were also stable across different socio-demographic factors, as well as individual differences in pain catastrophizing and sleep disturbance. Nevertheless, interventions that target improvement of pain acceptance may help individuals with chronic pain be resilient during the pandemic.
Perspective
Individuals with chronic pain overall did not experience significant exacerbation of pain, emotional distress, and opioid misuse across one year during the COVID-19 pandemic. Individuals with higher pain acceptance showed greater improvement in pain severity and depressive symptoms over time during the pandemic.
Key Words: COVID-19, chronic pain, depression, anxiety, pain acceptance, pain catastrophizing, Sleep, opioid
Introduction
Chronic pain is a major public health concern that impacts one third of American adults.18 In addition to physiological factors, pain is modulated by various psychosocial stressors.19 The COVID-19 pandemic, which has resulted in more than 4.5 million deaths across the world (as of September 2021) and unprecedented socio-economic consequences (eg, social distancing, stay-at-home orders, financial instability), is considered a novel and on-going psychosocial stressor.25 , 29 A few cross-sectional studies that were conducted in the early phase of the pandemic demonstrated that individuals with chronic pain reported significant elevation of pain experience (ie, pain severity and interference), emotional distress (ie, anxiety and depressive symptoms), and/or opioid use.16 , 25 , 29 The impact of the pandemic on long-term trajectories of pain-related outcomes (ie, pain severity and interference, emotional distress, and opioid misuse), however, is currently unknown.
To identify individuals who may be at risk for experiencing difficulty in coping with pain during the pandemic, it is imperative to examine socio-demographic correlates of pain-related outcome trajectories. Recent studies found that women, racial/ethnic minorities, and individuals with a low socio-economic status (SES) were more likely to report worse pain during the pandemic compared to their counterparts.16 , 29 Some evidence also suggests that women, younger adults, and those who have lost their job due to the pandemic are more likely to experience emotional distress.17 , 44 In terms of opioid use, one study reported that Black individuals were at greater risk of non-fatal opioid overdose during the pandemic.33 Investigating potential socio-demographic disparities of pain-related outcome trajectories may provide important information for our collective effort to eliminate disparities and improve equity in chronic pain care.
It is also critical to examine modifiable individual difference factors to effectively treat or prevent worsening pain, emotional distress, and opioid misuse during the pandemic. Pain acceptance (ie, individuals’ willingness to stay with pain and engage in meaningful activities),27 pain catastrophizing (ie, a dysfunctional cognitive-affective reaction to pain),42 and sleep disturbance have consistently been found to be associated with pain,27 , 30 , 39 emotional distress,12 , 28 , 39 and prescription opioid use.21 , 26 , 30 Additionally, these factors are some of the key targets for first-line evidence-based psychological interventions for chronic pain, such as Acceptance and Commitment Therapy (ACT) and Cognitive Behavioral Therapy (CBT).11 , 43 Investigating whether pain acceptance, pain catastrophizing, and sleep disturbance moderate trajectories of pain-related outcomes will provide insight regarding which factors to target in treatment for those who are adversely impacted by the pandemic.
The present study addressed several aims using a large (N = 1,453) online sample of individuals with chronic pain in the U.S. who were assessed three times across one year. First, we examined the trajectories of pain severity, pain interference, depressive and anxiety symptoms, and prescription opioid misuse. Second, we investigated whether socio-demographic factors moderate these outcome trajectories. Lastly, we examined whether individual differences in pain acceptance, pain catastrophizing, and sleep disturbance moderate the outcome trajectories.
Methods
Participants
Participants were recruited from Amazon Mechanical Turk (MTurk) three times during the study: Time 1 (04/22/2020–05/15/2020), Time 2 (07/29/2020–08/05/2020), and Time 3 (05/07/2021–05/26/2021). Cloud Research, a third-party data collection company, was used to recruit MTurk “workers” for the survey. Note that studies have shown that MTurk responses have overall good validity and reliability.5 Based on a study by Johannes and colleagues,18 we oversampled individuals who identified as women, Black/African American race, and Hispanic ethnicity to achieve a sample representative of the chronic pain population in the U.S. in terms of gender, race, and ethnicity.
Workers who responded affirmatively to an initial screening item that asked whether they had pain more than half of the week over the past 3 months were invited to complete an additional screener to fully determine study eligibility. Inclusion criteria were: (a) age ≥18 years; (b) average past week pain severity of ≥3/10; (c) U.S. residence; (d) English proficiency; and (e) willingness to participate in follow-up assessments. To maximize the quality and reliability of survey responses, we also applied data quality standards. First, only workers with ≥95% approval ratings from other MTurk requesters were invited. Second, we excluded data from participants who failed one or more attention check items (out of three). Third, data were excluded from participants who took substantially greater (>60 minutes) or less than (<16 minutes) the average completion duration of 35 minutes based upon pilot data.
A total of 30,096 workers responded to the initial one-item screening question. Among these workers, 10,308 (34.3%) indicated the presence of chronic pain. Of these, 2,153 met the inclusion criteria, and 1,809 (84.0%) initiated the survey. A total of 1,484 (82%) people passed the data quality standards. Of these, we identified 31 duplicate cases. As a result, the final Time one sample size was 1,453. These participants were invited to participate in Time two and three follow-up assessments. Among 1,453 participants, 878 (60%) were retained in Time 2 and 813 were retained in Time 3 (56%). The retention rates were overall slightly higher than those of other longitudinal MTurk studies.41
Procedures
MTurk workers who met study eligibility received a link to the main survey, which included self-report questionnaires. Participants were compensated $5 for their participation for each time point. All study procedures were approved by the Johns Hopkins School of Medicine (JHSOM) Institutional Review Board. In accordance with the JHSOM IRB policy for exempt applications, whereby the identity of human subjects cannot be readily ascertained, each participant was provided with an overview of the study, the contact information of the principle investigator, and the JHSOM IRB number prior to agreeing to participate.
Measures
Socio-Demographics
Participants provided information about their age, gender, race, ethnicity, education, income, marital status, impact on their employment status due to the pandemic, and duration of chronic pain. Note that the present study focused on the gender binary (ie, male and female) for a group comparison, as a very small proportion (.5%) of individuals indicated the non-binary/genderqueer category.
Pain Severity and Interference
The Brief Pain Inventory–Short Form7 was used to assess pain severity and pain interference. For pain severity, participants rated their current pain, as well as least, worst, and average pain in the prior 24 hours based upon a scale ranging from 0 (no pain) to 10 (pain as bad as you can imagine). For pain interference, participants were asked to indicate the extent to which pain interfered with general activity, mood, walking ability, work, relations with others, sleep, and enjoyment of life based up on a scale ranging from 0 (does not interfere) to 10 (complete interferes). We computed mean scores for pain severity and interference. Cronbach's alphas across Time one and three ranged from .71 to .92 for pain severity, and .91 to .93. for pain interference.
Emotional Distress
The 4-item PROMIS Emotional Distress-Depression/Anxiety scales22 assessed participants’ past 7-day severity of emotional distress. Each of the items were rated on a scale ranging from 1 (never) to 5 (always). Total scores were transformed into T-scores with a score of 50 reflecting the average for the general U.S. population. These scales have demonstrated good internal reliability and convergent validity among individuals with chronic pain. Cronbach's alphas ranged from .89 to .93 across the three time points.
Prescription Opioid Misuse
The well-validated 7-item PROMIS Prescription Pain Medication Misuse scale35 measured prescription opioid misuse behaviors during the past 7 days. Total scores were converted to T-scores, with higher scores indicating more misuse problems. Cronbach's alphas ranged from .90 to .93 across the three time points.
Pain Catastrophizing
The 13-item Pain Catastrophizing Scale (PCS)42 assessed the extent to which people feel helpless, ruminate about, and magnify their pain experience. Each item is rated on a scale ranging from 0 (not at all) to 4 (all the time). A total sum score was computed, with higher scores indicating greater pain catastrophizing. Cronbach's alpha was .95 for all time points.
Pain Acceptance
The psychometrically well-validated 8-item Chronic Pain Acceptance Questionnaire (CPAQ-8) 13 assessed the extent which individuals are willing to engage in meaningful daily activities while experiencing pain and trying not to control or avoid their pain. Items were rated on a scale ranging from 0 (never) to 6 (always true). Higher sum scores indicate greater pain acceptance. Cronbach's alphas for CPAQ-8 ranged from .82 to .85 across the time points.
Sleep Disturbance
The Insomnia Severity Index (ISI)3 assessed perceived severity of sleep disturbance. Each of the seven items is rated on a scale ranging from 0 (not at all) to 4 (very much). Cronbach's alphas ranged from .89 to .90 across the time points.
Power Analysis
We computed the sensitivity to detect an interaction effect in a mixed-effects model based upon the Time 1 sample size. A sample of 1,453 with three assessment points and an alpha level of .05 (two-tailed) can produce a power of .80 to detect small effects (Cohen's f = .04). Note that Cohen's f values of .10, .25, and .40 indicate small, medium, and large effect sizes, respectively.
Data Analytic Strategy
Mixed-effects growth modeling was conducted to assess the outcome trajectories. First, we conducted a series of unconditional growth models including only a time variable to evaluate the average trajectories of the study outcomes. For each outcome, we started with adding a fixed slope of time. Then, we tested a fixed slope of quadratic term to incorporate a non-linear trajectory of the outcome by using the likelihood ratio test (LRT). Lastly, LRT was also used to test whether adding a random slope of time is necessary in the model. When adding a random slope resulted in a model convergence issue, we only included fixed slope of time.
Next, we included a set of socio-demographic variables and their interactions with the time variable. We then tested whether trajectories of outcomes are moderated by person-means of pain catastrophizing, pain acceptance, and sleep disturbance measured across three time points. Note that this model adjusts for socio-demographic variables that were significantly associated with outcomes. For all analyses, we used the ‘lme4’ package from R. For measuring effect sizes in mixed-effects models, the proportion of the variance reduction (ie, pseudo R2) was computed for each outcome. Missing data were handled by the maximum likelihood estimation based upon the missing at random (MAR) assumption. As we were testing five different outcome variables, we set the alpha level to .01 (two-tailed) based upon a Bonferroni adjustment.
Results
Sample Characteristics
Table 1 presents a summary of the participant characteristics at Time one. The mean age of participants was 41.7 years, and the majority of them were women (65.2%), White (81.9%), had at least some college education (87.8%), were working part- or full-time (62.2%), and were married (45.7%). The median income category range was $50,000-$74,999. Close to half (42.7%) of the sample reported experiencing an impact in their employment due to the pandemic at Time 1. In terms of the clinical characteristics, participants reported on average 10.9 years of experiencing chronic pain. They reported an overall moderate level of pain severity (M = 4.2), pain interference (M = 4.9), and depressive (M = 58.0) and anxiety (M = 59.3) symptoms. A total of 467 (32.1% of the sample) participants reported using prescription opioids. Among them, the level of opioid misuse behaviors was overall low (M = 44.2). In terms of self-reported positive COVID-19 cases, there were nine and 48 positive cases at Time one and three, respectively.
Table 1.
Characteristics of the Study Sample at Time 1
| Variables | M (SD) or N (%) |
|---|---|
| Age (years) | 41.7 (13.1) |
| Gender | |
| Female | 968 (65.2%) |
| Male | 498 (34.3%) |
| Other (Non-binary/genderqueer) | 7 (0.5%) |
| Race | |
| White | 1189 (81.9%) |
| Black/African American | 99 (6.8%) |
| Asian/Asian American | 50 (3.4%) |
| American Indian/Alaska Native | 13 (0.9%) |
| Native Hawaiian/Pacific Islander | 0 (0%) |
| Mixed Race | 67 (4.6%) |
| Other Race | 28 (1.9%) |
| Prefer not to answer | 5 (0.3%) |
| Don't know | 1 (0.1%) |
| Ethnicity | |
| Hispanic | 144 (9.9%) |
| Non-Hispanic | 1297 (89.4%) |
| Prefer not to answer | 7 (0.5%) |
| Don't know | 3 (0.2%) |
| Education | |
| Less than high school diploma | 9 (0.6%) |
| GED or high school diploma | 168 (11.6%) |
| Some college, no degree | 402 (27.7%) |
| Associate's degree (2-year degree) | 224 (15.4%) |
| Bachelor's degree/college degree | 399 (27.5%) |
| Beyond college education | 250 (17.2%) |
| Prefer not to answer | 1 (0.1%) |
| Employment Status | |
| Working full-time | 694 (47.8%) |
| Working part-time | 209 (14.4%) |
| Unemployed or laid off | 176 (12.1%) |
| Looking for work | 49 (3.4%) |
| Keeping house or raising children full-time | 110 (7.6%) |
| Retired | 103 (7.1%) |
| Other | 112 (7.7%) |
| Income | |
| Less than $5,000 | 45 (3.1%) |
| $5,000-$11,999 | 67 (4.6%) |
| $12,000-$15,999 | 54 (3.7%) |
| $16,000-$24,999 | 148 (10.2%) |
| $25,000-$34,999 | 211 (14.5%) |
| $35,000-$$49,999 | 224 (15.4%) |
| $50,000-$74,999 | 310 (21.3%) |
| $75,000-$99,999 | 177 (12.2%) |
| $100,000 and greater | 201 (13.8%) |
| Prefer not to answer | 8 (0.5%) |
| Don't know | 7 (0.5%) |
| Marital Status | |
| Married | 663 (45.7%) |
| Divorced | 198 (13.6%) |
| Separated | 29 (2.0%) |
| Widowed | 32 (2.2%) |
| Single | 517 (35.6%) |
| Prefer not to answer | 13 (0.9%) |
| Changes in employment status due to COVID-19 | |
| Yes | 620 (42.7%) |
| Chronic Pain Duration (years) | 10.9 (9.1) |
| Pain Severity (0-10 NRS) | 4.2 (1.6) |
| Pain Interference (0-10 NRS) | 4.9 (2.4) |
| Depressive Symptoms (T-score) | 58.0 (10.1) |
| Anxiety Symptoms (T-score) | 59.3 (9.7) |
| Prescribed Opioids | |
| Yes | 467 (32.1%) |
| Prescription Opioid Misuse Behaviors (T-score) | 44.2 (8.4) |
Attrition Analyses
We conducted a series of attrition analyses (ie, t-tests for continuous variables and chi-square tests for categorical variables). Results showed that participants of a younger age (P< .001), men (P< .001), those who identified as Hispanic (P< .001), had a lower education level (P< .01), experienced a negative job impact (P= .01), exhibited greater depressive (P= .01) and anxiety (P= .04) symptoms, as well as greater opioid misuse behaviors (P= .01) were more likely to drop out at one-year follow-up. These results provide further support that the missingness in the present study may meet the MAR assumption, which indicates that there is a systematic association between the missingness and some observed data.
Trajectories of Pain Severity and Interference, Emotional Distress, and Opioid Misuse
Table 2 provides the detailed parameter estimates of all unconditional growth models.
Table 2.
Unconditional Mixed-Effects Growth Models of Study Outcomes
| Pain Severity |
Pain Interference |
Depressive Symptoms |
Anxiety Symptoms |
Opioid Misuse Behaviors |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictors | B | 95% CI | p | B | 95% CI | p | B | 95% CI | p | B | 95% CI | p | B | 95% CI | p |
| Intercept | 4.18 | 4.09 – 4.27 | < .001 | 4.90 | 4.77 – 5.02 | < .001 | 58.05 | 57.52 – 58.57 | < .001 | 59.34 | 58.85 – 59.83 | < .001 | 43.63 | 42.97 – 43.30 | < .001 |
| Linear Time | −.15 | −.19 – −.11 | < .001 | −.11 | −.17 – −.06 | < .001 | −.37 | −.57 – −.17 | < .001 | −.12 | −.17 – −.08 | < .001 | −.03 | −.10 – .03 | .310 |
| Curvature Time | .01 | .01 – .01 | < .001 | .01 | .00 – .01 | .003 | .02 | .01 – .04 | .008 | — | — | — | — | — | — |
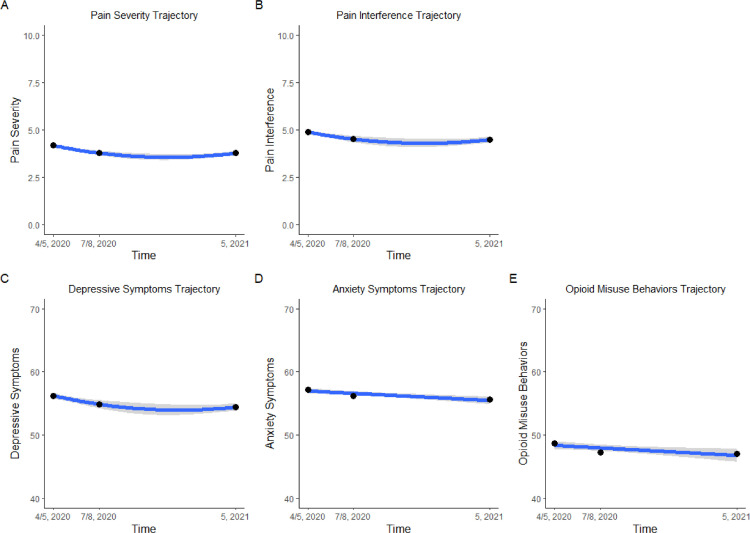
Pain severity and interference trajectories. Change in pain severity across time is best captured by a quadratic model (Fig 1 A). The model is characterized by an initial decrease in pain severity followed by a slight incline. Pain interference change is also best captured by a quadratic model (Fig 1B). Inclusion of time predictors reduced within-person level variances by 4.9% and 1.8%, respectively, from null models that do not include any predictors.
Figure 1.
(A-E). Overall trajectories of study outcomes
Note. “4/5, 2020” = April/May 2020; “7/8, 2020” = July/August 2020; “5, 2021” = May 2021. Grey bands indicate 95% confidence intervals.
Emotional distress trajectories. While depressive symptom trajectory is best captured by a quadratic model (Fig 1C), anxiety symptom trajectory is best captured by a linear model (Fig 1D) with a slight decrease in anxiety symptoms over time. Inclusion of time predictor(s) reduced within-person level variances by 1.7% and 13.2%, respectively, from null models.
Prescription opioid misuse trajectory. The prescription opioid misuse trajectory (Fig 1E) showed overall no significant changes across one year. Inclusion of the time predictor did not reduce within-person level variance from a null model.
Moderating Effects of Socio-Demographic Cactors
Detailed fixed effect parameter estimates are displayed in Table 3 . None of the socio-demographic factors significantly moderated any outcome trajectories. In terms of main effects, older age was associated with overall lower emotional distress and opioid misuse behaviors during the pandemic. Women reported overall greater pain severity and interference, greater anxiety symptoms, but lower opioid misuse behaviors. Although there were no significant racial differences in outcomes, those of Hispanic ethnicity reported an overall greater level of pain interference and opioid misuse behaviors compared to those who identified as non-Hispanic. Lower income level was associated with overall higher pain severity and interference, and depressive symptoms. Lower education level was associated with greater pain severity. Negative job impact due to the pandemic was not significantly associated with any outcomes. Inclusion of socio-demographic predictors reduced between-person level variances by 1.5% (pain severity), 4.1% (pain interference), 12.9% (depressive symptoms), 12.0% (anxiety symptoms), and 12.6% (opioid misuse) from the unconditional growth models that only included time predictor(s).
Table 3.
Mixed-Effects Growth Models With Socio-Demographic Moderators
| Pain Severity |
Pain Interference |
Depressive Symptoms |
Anxiety Symptoms |
Opioid Misuse Behaviors |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictors | B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | B | 95% CI | P | B | 95% CI | P |
| Intercept | 3.78 | 3.30 – 4.27 | < .001 | 4.53 | 3.85 – 5.21 | <.001 | 63.07 | 60.26 – 65.89 | <.001 | 63.06 | 60.36 – 65.75 | <.001 | 49.45 | 46.01 – 52.88 | <.001 |
| Linear Time | −.09 | −.13 – −.05 | < .001 | −.10 | −.16 – −.03 | .002 | −.28 | −.49 – −.07 | .009 | .04 | −.21 – .28 | .777 | .36 | .01 – .72 | .046 |
| Curvature Time | .003 | −.00 – .01 | .209 | −.00 | −.01 – .01 | .744 | .02 | −.01 – .04 | .231 | — | — | — | — | — | — |
| Age | .01 | −.00 – .01 | .087 | .00 | −.01 – .01 | .661 | −.19 | −.23 – −.15 | <.001 | −.17 | −.20 – −.13 | <.001 | −.09 | −.14 – −.04 | .001 |
| Women | .34 | .15 – .53 | < .001 | .37 | .10 – .64 | .006 | 1.22 | .12 – 2.33 | .030 | 2.62 | 1.56 – 3.67 | <.001 | −2.79 | −4.26 – −1.32 | <.001 |
| White (vs Black) | −.35 | −.71 – .01 | .054 | −.38 | −.88 – .13 | .146 | .50 | −1.63 – 5.37 | .643 | .53 | −1.48 – 2.54 | .604 | −.49 | −2.85 – 1.87 | .686 |
| Asian (vs Black) | −.14 | −.74 – .46 | .649 | .06 | −.79 – .90 | .898 | 1.87 | −2.39 – 3.73 | .295 | .72 | −2.62 – 4.07 | .671 | 4.99 | 1.09 – 8.90 | .012 |
| Other (vs Black) | −.35 | −.87 – .18 | .198 | −.42 | −1.16 – .32 | .268 | .67 | −1.60 – 2.59 | .668 | −1.09 | −4.01 – 1.84 | .467 | −2.50 | −6.25 – 1.24 | .190 |
| Hispanic | .14 | −.18 – .46 | .398 | .63 | .18 – 1.09 | .006 | .86 | −1.03 – 2.74 | .372 | 2.25 | .46 – 4.05 | .014 | 3.53 | 1.34 – 5.73 | .002 |
| Income | .30 | .08 – .51 | .008 | .66 | .36 – .97 | <.001 | 3.22 | 1.95 – 4.49 | <.001 | 1.54 | .33 – 2.76 | .013 | −.41 | −2.05 – 1.23 | .625 |
| Education | .39 | .12 – .66 | .005 | .34 | −.04 – .72 | .079 | 1.69 | .12 – 3.26 | .035 | .70 | −.80 – 2.20 | .361 | −1.29 | −3.49 – .92 | .254 |
| Job Impact | .04 | −.14 – .23 | .630 | .21 | −.05 – .46 | .111 | 1.13 | .07 – 2.18 | .036 | 1.31 | .30 – 2.32 | .011 | .28 | −1.10 – 1.65 | .692 |
| Time x Age | .000 | −.000 – .000 | .440 | .000 | −.000 – .000 | .213 | −.000 | −.000 – .000 | .840 | −.003 | −.01 – .00 | .066 | −.01 | −.01 – −.00 | .021 |
| Time x Women | .001 | −.001 – .002 | .313 | .002 | −.000 – .004 | .059 | −.000 | −.01 – .01 | .975 | −.04 | −.14 – .05 | .383 | −.03 | −.18 – .12 | .680 |
| Time x White | −.001 | −.003 – .002 | .634 | .002 | −.002 – .006 | .296 | −.000 | −.01 – .01 | .945 | .001 | −.18 – .18 | .988 | −.06 | −.30 – .17 | .594 |
| Time x Asian | .003 | −.002 – .008 | .265 | −.001 | −.008 – .006 | .801 | −.009 | −.03 – .02 | .474 | .04 | −.28 – .37 | .786 | −.25 | −.72 – .22 | .294 |
| Time x Other | .000 | −.004 – .004 | .893 | .004 | −.002 – .01 | .158 | .007 | −.01 – .03 | .452 | .06 | −.20 – .32 | .665 | −.02 | −.37 – .33 | .914 |
| Time x Hispanic | .002 | −.001 – .002 | .202 | .001 | −.003 – .004 | .793 | .003 | −.01 – .02 | .679 | −.07 | −.25 – .11 | .452 | .14 | −.12 – .39 | .296 |
| Time x Income | .001 | −.001 – .002 | .252 | .000 | −.002 – .002 | .831 | .001 | −.01 – .01 | .723 | −.002 | −.11 – .10 | .970 | .07 | −.09 – .23 | .384 |
| Time x Education | .001 | −.001 – .003 | .217 | .001 | −.001 – .004 | .298 | .003 | −.01 – .01 | .514 | .06 | −.07 – .19 | .339 | −0.01 | −.22 – .20 | .934 |
| Time x Job Impact | .001 | −.000 – .003 | .080 | .002 | −.000 – .004 | .076 | .000 | −.01 – .01 | .978 | .02 | −.07 – .11 | .610 | −0.05 | −.19 – .09 | .442 |
Note. ‘Time’ indicates either linear or curvature time depending on each outcome. ‘—’ indicates that the predictor was not included in the model.
P < .01 (Bonferroni adjustment of 5 outcomes) are indicated as bold.
Moderating Effects of Pain Acceptance, Pain Catastrophizing, and Sleep Disturbance
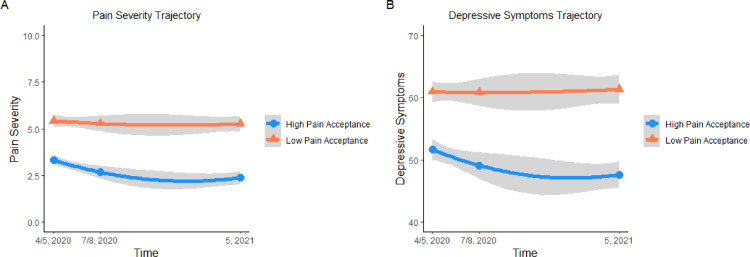
Detailed fixed effect parameter estimates are displayed in Table 4 . Pain catastrophizing and sleep disturbance did not significantly moderate any of the outcome trajectories. However, pain acceptance significantly moderated trajectories of pain severity and depressive symptoms. As shown in Fig 2 A and B, individuals with higher pain acceptance levels during the pandemic reported greater reduction in pain severity and depressive symptoms over time. In terms of main effects, both pain catastrophizing and sleep disturbance were associated with overall higher pain severity and interference, and emotional distress. Higher pain catastrophizing was associated with overall greater opioid misuse behaviors. Inclusion of pain acceptance, pain catastrophizing, and sleep disturbance, in addition to socio-demographic covariates further reduced between-person level variances by 30.7% (pain severity), 63.9% (pain interference), 50.2% (depressive symptoms), 50.0% (anxiety symptoms), and 8.7% (opioid misuse) from the models that included both time and socio-demographic predictors.
Table 4.
Mixed-Effects Growth Models With Pain Acceptance, Pain Catastrophizing, and Sleep Disturbance as Moderators
| Pain Severity |
Pain Interference |
Depressive Symptoms |
Anxiety Symptoms |
Opioid Misuse Behaviors |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictors | B | 95% CI | p | B | 95% CI | p | B | 95% CI | p | B | 95% CI | p | B | 95% CI | p |
| Intercept | 4.26 | 3.79 – 4.73 | <.001 | 5.77 | 5.22 – 6.32 | <.001 | 49.25 | 46.35 – 52.15 | <.001 | 48.62 | 45.81 – 51.44 | <.001 | 45.37 | 40.41 – 50.33 | <.001 |
| Linear Time | -.14 | -.18 – -.10 | <.001 | -.10 | -.16 – -.05 | <.001 | -.28 | -.48 – -.07 | .007 | -.06 | -.30 – .18 | .601 | -.06 | -.43 – .31 | .754 |
| Curvature Time | .01 | .01 – .02 | <.001 | .01 | .00 – .01 | .032 | .03 | .01 – .06 | .008 | — | — | — | — | — | — |
| Pain Acceptance | -.05 | -.06 – -.04 | <.001 | -.12 | -.13 – -.10 | <.001 | -.02 | -.08 – .05 | .603 | .04 | -.02 – .10 | .202 | -.03 | -.14 – .07 | .53 |
| Pain Catastro | .02 | .02 – .03 | <.001 | .04 | .03 – .05 | <.001 | .37 | .32 – .41 | <.001 | .37 | .32 – .41 | <.001 | .11 | .03 – .19 | .006 |
| Sleep Disturbance | .03 | .02 – .05 | <.001 | .08 | .06 – .09 | <.001 | .42 | .35 – .49 | <.001 | .38 | .31 – .46 | <.001 | .14 | .01 – .27 | .031 |
| Time x Pain Acceptance | -.0001 | -.0002 – -.00004 | .008 | -.0008 | -.0002 – .0001 | .284 | -.0008 | -.001 – -.0004 | .001 | -.01 | -.01 – -.0004 | .036 | .002 | -.01 – .01 | .755 |
| Time x Pain Catastro | .0000 | -.00007 – .00008 | .913 | 0.000 | -.00002 – .0001 | .932 | .00004 | -.0003 – .0004 | .854 | .003 | -.002 – .01 | .172 | .003 | -.005 – .01 | .468 |
| Time x Sleep Disturbance | .0001 | -.00002 – .0002 | .11 | .0001 | -.0002 – .0002 | .945 | .0002 | -.0004 – .0008 | .498 | .004 | -.003 – .01 | .288 | -.004 | -.02 – .01 | .493 |
| Age | — | — | — | .40 | .12 – .68 | .005 | -.11 | -.14 – -.08 | <.001 | -.10 | -.13 – -.07 | <.001 | -.08 | -.13 – -.03 | .001 |
| Women | .22 | .07 – .37 | .004 | .26 | .08 – .43 | .004 | — | — | — | 1.29 | .53 – 2.06 | .001 | -3.54 | -4.86 – -2.23 | <.001 |
| Hispanic | — | — | — | — | — | — | — | — | — | — | — | — | 2.64 | .72 – 4.55 | .007 |
| Income | .04 | -.13 – .22 | .628 | .08 | -.12 – .28 | .419 | 1.95 | 1.03 – 2.87 | <.001 | — | — | — | — | — | — |
| Education | .22 | .00 – .44 | .047 | — | — | — | — | — | — | — | — | — | — | — | — |
Note. ‘Pain Catastro’ = Pain Catastrophizing. ‘Time’ indicates either linear or curvature time depending on each outcome. ‘—’ indicates that the predictor was not included in the model. p < .01 (Bonferroni adjustment of 5 outcomes) are indicated as bold.
Figure 2.
(A,B). Trajectories of pain severity and depressive symptoms with different pain acceptance levels
Note. Median split was used to create ‘high’ and ‘low’ pain acceptance levels. “4/5, 2020” = April/May 2020; “7/8, 2020” = July/August 2020; “5, 2021” = May 2021. Grey bands indicate 95% confidence intervals.
Discussion
To our knowledge, this is the first study to investigate one-year trajectories and their individual differences in pain severity and interference, emotional distress, and opioid misuse behaviors during the COVID-19 pandemic. On average, these pain-related outcomes did not significantly increase during the pandemic. None of the socio-demographic factors moderated the outcome trajectories. However, pain acceptance significantly moderated pain severity and depressive symptom trajectories, such that individuals who reported greater pain acceptance during the pandemic showed greater reduction in pain severity and depressive symptoms over time.
Contrary to some cross-sectional studies reporting an adverse impact of the pandemic on pain-related outcomes,16 , 25 individuals with chronic pain during the pandemic overall did not show significant exacerbation of these outcomes across one year. These findings are largely in line with those from a study by Lassen and colleagues who found that there were no significant changes in pain experience, depression, anxiety, and stress before and during the early phase (May-July 2020) of the pandemic,23 as well as from a study by Reed and colleagues that also revealed that pain-related disability slightly improved among individuals with chronic pain during the early phase (May 2020) of the pandemic when compared to pre-pandemic (January 2020).37 Our previous study, based upon Time one data, also demonstrated that the majority (> 60%) of individuals with chronic pain did not perceive any changes in their pain severity and pain interference during the early phase (April/May 2020) of the pandemic.29 These findings are consistent with the broader literature suggesting that catastrophic events or disasters do not necessarily cause exacerbation of pain or related health outcomes. For instance, a previous study indicated that residents of New York City and New Jersey with fibromyalgia-like pain symptoms reported no significant changes in their pain symptoms after the 9 of 11 terrorist attacks.36 Similarly, Lerman and colleagues24 found that patients with chronic pain who were exposed to 3-week missile attacks in the Southern region of Israel did not show significant changes in affective pain, depression, and anxiety levels. As suggested previously,6 , 10 we speculate that daily hassles that directly interfere with one's psychosocial functioning may be more likely to deteriorate health outcomes than a catastrophic event that can impact individuals on a less personal level. We would also like to note that there has been some speculation on the potential benefits of societal restrictions (eg, stay-at-home orders, social distancing, and remote working) on lifestyle and activity pacing,29 , 37 successful adjustment to a new normal,37 and hope for COVID-19 vaccines1, as potential explanations for the neutral or paradoxical effects of the pandemic on pain-related outcomes.
The present findings did not demonstrate that certain socio-demographic subgroups are more likely to experience worse pain-related outcomes as the pandemic persists. However, consistent with the extant literature,2 , 34 , 40 we found that older age serves as a protective factor for emotional distress and opioid misuse, whereas women in general reported greater pain severity and interference, and anxiety symptoms, but lower opioid misuse behaviors. In line with previous studies,9 we also found significant SES disparities in pain severity and interference, and depressive symptoms, alerting that it is a societal priority to address structural inequality, such as limited access to resources, which significantly hinders individuals’ effective management of chronic pain. Contrary to previous studies suggesting that individuals of Hispanic origin report overall lower levels of pain interference15 and problematic opioid use,38 we found that this demographic group reported greater pain interference and opioid misuse during the pandemic than those who are non-Hispanic. These differences may stem from disparate COVID-19 financial impact on the Hispanic group in particular,14 which may have adversely affected their access to resources for managing pain.
Notably, individuals with higher pain acceptance showed greater improvement in pain severity and depressive symptoms over time. These findings are quite consistent with those from a recent study showing that pain acceptance significantly buffered the effects of COVID-19 fear and avoidance on pain-related disability and depressive symptoms.46 Pain acceptance is an important resilience resource that can help individuals with chronic pain continuously engage in important daily activities and goals in the face of pain, which facilitates better adjustment to persistent pain.28 Evidence-based interventions, such as ACT, that directly strives to augment pain acceptance may serve as a particularly useful chronic pain self-management approach in the context of the COVID-19 pandemic.
As with literature both prior to and during the pandemic indicating that pain catastrophizing and sleep disturbance are important risk factors for maladaptive pain coping,12 , 16 , 29 , 39 higher pain catastrophizing and sleep disturbance were associated with overall greater pain severity and interference, and emotional distress over and above the effects of socio-demographic factors. Higher pain catastrophizing was also associated with greater opioid misuse behaviors. It is also noteworthy that these factors quite largely explained each outcome's variance. Highly accessible, affordable, and scalable interventions, such as a single-session treatment for pain catastrophizing and the Brief Behavioral Treatment for Insomnia, are showing promising results in targeting pain catastrophizing and sleep disturbance.4 , 8 Future studies that investigate whether these brief, targeted interventions can effectively help individuals with chronic pain improve their experience of pain and emotional distress and prevent opioid misuse behaviors are warranted.
The present study had several strengths including a large sample size, a 1-year follow-up assessment, and comprehensive chronic pain outcome assessments. However, there were also a number of limitations. First, as participants were recruited post-pandemic, we could not measure outcomes at baseline. Hence, our data does not allow for comparing changes in outcomes before and during the pandemic. Second, participants’ geographical location data was not collected. It is possible that those residing in certain areas in the U.S. may be more negatively influenced by the pandemic. Third, we did not measure the extent to which individuals felt lonely or socially isolated during the pandemic, which could have provided us with further insight as to who may have been at risk for experiencing worsening pain-related outcomes over time. Indeed, emerging evidence suggests that a significant elevation of loneliness and social isolation is due to the pandemic,31, 32 and such elevation is associated with greater pain severity,45 pain interference,15 and chronic inflammation20 cross-sectionally. Future studies that longitudinally examine the effect of increased loneliness and social isolation on pain-related outcomes during the pandemic are strongly warranted. Fourth, although we had an overall better retention rate than other longitudinal MTurk studies, a substantial proportion of the sample was missing at follow-up assessments. Lastly, we only had three measurement timepoints across one year. More frequent assessment of outcomes could have allowed us to evaluate more nuanced outcome trajectory patterns.
In conclusion, our study suggests that individuals with chronic pain overall did not experience a significant exacerbation of pain, emotional distress, or opioid misuse across one year during the pandemic. There was also no specific socio-demographic subgroup of individuals that was more negatively impacted. Greater pain acceptance, however, facilitated improvement of pain and depressive symptoms over time. Interventions that target pain acceptance (eg, ACT) may be particularly helpful for individuals effectively self-manage chronic pain during the present pandemic. More longitudinal studies are needed to better understand the multi-faceted impact of the pandemic and COVID-19 infection on development, maintenance, and exacerbation of chronic pain.
Footnotes
Funding for this research was provided by National Institutes of Health grants: F32DA049393 (C.J.M.), R01MD009063 (C.M.C) and T32HD007414 (for L.S.M.’s postdoctoral training).
The authors have no conflicts of interest to disclose.
References
- 1.Amelot A, Jacquot A, Terrier L-M, Aggad M, Planty-Bonjour A, Fouquet B, Cook A-R, Zemmoura I, Velut S, Destrieux C. Chronic low back pain during COVID-19 lockdown: is there a paradox effect? Eur Spine J. 2021;31:1–9. doi: 10.1007/s00586-021-07049-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bartley EJ, Fillingim RB. Sex differences in pain: A brief review of clinical and experimental findings. Br J Anaesth. 2013;111:52–58. doi: 10.1093/bja/aet127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 4.Bramoweth AD, Lederer LG, Youk AO, Germain A, Chinman MJ. Brief behavioral treatment for insomnia versus cognitive behavioral therapy for insomnia: results of a randomized noninferiority clinical trial among veterans. Behav Ther. 2020;51:535–547. doi: 10.1016/j.beth.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buhrmester M, Kwang T, Gosling SD: Amazon's mechanical turk: A new source of inexpensive, yet high-quality data? In: Kazdin AE, editor. Methodol issues Strateg Clin Res American Psychological Association; page 133–1392016. [DOI] [PubMed]
- 6.Clauw DJ, Häuser W, Cohen SP, Fitzcharles M-A. Considering the potential for an increase in chronic pain after the COVID-19 pandemic. Pain. 2020;161:1694–1697. doi: 10.1097/j.pain.0000000000001950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore Annals. 1994;23:129–138. [PubMed] [Google Scholar]
- 8.Darnall BD, Sturgeon JA, Kao M-C, Hah JM, Mackey SC. From catastrophizing to recovery: a pilot study of a single-session treatment for pain catastrophizing. J Pain Res. 2014;7:219–226. doi: 10.2147/JPR.S62329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Day MA, Thorn BE. The relationship of demographic and psychosocial variables to pain-related outcomes in a rural chronic pain population. PAIN®. 2010;151:467–474. doi: 10.1016/j.pain.2010.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeLongis A, Coyne JC, Dakof G, Folkman S, Lazarus RS. Relationship of daily hassles, uplifts, and major life events to health status. Heal Psychol; 1982;1:119. [Google Scholar]
- 11.Ehde DM, Dillworth TM, Turner JA. Cognitive-behavioral therapy for individuals with chronic pain: Efficacy, innovations, and directions for research. Am Psychol. 2014;69:153–166. doi: 10.1037/a0035747. [DOI] [PubMed] [Google Scholar]
- 12.Finan PH, Goodin BR, Smith MT. The association of sleep and pain: an update and a path forward. J Pain. 2013;14:1539–1552. doi: 10.1016/j.jpain.2013.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fish RA, McGuire B, Hogan M, Morrison TG, Stewart I. Validation of the Chronic Pain Acceptance Questionnaire (CPAQ) in an Internet sample and development and preliminary validation of the CPAQ-8. Pain. 2010;149:435–443. doi: 10.1016/j.pain.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 14.Gonzalez D, Karpman M, Kenney GM, Zuckerman S. Urban Inst; Washington, DC: 2020. Hispanic Adults in Families With Noncitizens Disproportionately Feel the Economic Fallout from COVID-19. [Google Scholar]
- 15.Hollingshead NA, Ashburn-Nardo L, Stewart JC, Hirsh AT. The pain experience of Hispanic Americans: a critical literature review and conceptual model. J Pain. 2016;17:513–528. doi: 10.1016/j.jpain.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hruschak V, Flowers KM, Azizoddin DR, Jamison RN, Edwards RR, Schreiber KL. Cross-sectional study of psychosocial and pain-related variables among patients with chronic pain during a time of social distancing imposed by the coronavirus disease 2019 pandemic. Pain. 2021;162:619–629. doi: 10.1097/j.pain.0000000000002128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jewell JS, Farewell C V, Welton-Mitchell C, Lee-Winn A, Walls J, Leiferman JA. Mental health during the COVID-19 pandemic in the United States: online survey. JMIR Form Res. 2020;4:e22043. doi: 10.2196/22043. ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an internet-based survey. J Pain [Internet] 2010;11:1230–1239. doi: 10.1016/j.jpain.2010.07.002. https://www.sciencedirect.com/science/article/pii/S1526590010006012 [cited 2018 Aug 14]. Available from: [DOI] [PubMed] [Google Scholar]
- 19.Karayannis N V, Baumann I, Sturgeon JA, Melloh M, Mackey SC. The impact of social isolation on pain interference: a longitudinal study. Ann Behav Med. 2019;53:65–74. doi: 10.1093/abm/kay017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koyama Y, Nawa N, Yamaoka Y, Nishimura H, Sonoda S, Kuramochi J, Miyazaki Y, Fujiwara T. Interplay between social isolation and loneliness and chronic systemic inflammation during the COVID-19 pandemic in Japan: Results from U-CORONA study. Brain Behav Immun. 2021;94:51–59. doi: 10.1016/j.bbi.2021.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kratz AL, Murphy III J, Kalpakjian CZ, Chen P. Medicate or meditate? Greater pain acceptance is related to lower pain medication use in persons with chronic pain and spinal cord injury. Clin J Pain. 2018;34:357. doi: 10.1097/AJP.0000000000000550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kroenke K, Yu Z, Wu J, Kean J, Monahan PO. Operating characteristics of PROMIS four-item depression and anxiety scales in primary care patients with chronic pain. Pain Med. 2014;15:1892–1901. doi: 10.1111/pme.12537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lassen CL, Siam L, Degenhart A, Klier TW, Bundscherer A, Lindenberg N. Short-term impact of the COVID-19 pandemic on patients with a chronic pain disorder. Medicine (Baltimore) 2021;100:e25153. doi: 10.1097/MD.0000000000025153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lerman SF, Rudich Z, Shahar G. Does war hurt? Effects of media exposure after missile attacks on chronic pain. J Clin Psychol Med Settings. 2013;20:56–63. doi: 10.1007/s10880-012-9313-4. [DOI] [PubMed] [Google Scholar]
- 25.Lynch ME, Williamson OD, Banfield JC: COVID-19 impact and response by Canadian pain clinics: A national survey of adult pain clinics. Can J Pain [Internet]; 4:204–9, 2020. Available from: 10.1080/24740527.2020.1783218 [DOI] [PMC free article] [PubMed]
- 26.Martel MO, Wasan AD, Jamison RN, Edwards RR. Catastrophic thinking and increased risk for prescription opioid misuse in patients with chronic pain. Drug Alcohol Depend [Internet] 2013;132:335–341. doi: 10.1016/j.drugalcdep.2013.02.034. http://www.ncbi.nlm.nih.gov/pubmed/23618767 [cited 2018 Aug 19]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCracken LM, Vowles KE. A prospective analysis of acceptance of pain and values-based action in patients with chronic pain. Heal Psychol; 2008;27:215–220. doi: 10.1037/0278-6133.27.2.215. [DOI] [PubMed] [Google Scholar]
- 28.McCracken LM, Vowles KE, Eccleston C. Acceptance of chronic pain: component analysis and a revised assessment method. Pain. 2004;107:159–166. doi: 10.1016/j.pain.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 29.Mun CJ, Campbell CM, McGill LS, Aaron R V. Vol. 22. 2021. The early impact of COVID-19 on chronic pain: a cross-sectional investigation of a large online sample of individuals with chronic pain in the United States, April to May, 2020; pp. 470–480. (Pain Med). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mun CJ, Finan PH, Smith MT, Carroll CP, Smyth JM, Lanzkron SM, Haythornthwaite JA, Campbell CM. A Preliminary Investigation of the underlying mechanism associating daily sleep continuity disturbance and prescription opioid use among individuals with sickle cell disease. Ann Behav Med. 2021;55:580–591. doi: 10.1093/abm/kaaa099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murayama H, Okubo R, Tabuchi T. Increase in social isolation during the COVID-19 pandemic and its association with mental health: Findings from the JACSIS 2020 study. Int J Environ Res Public Health Multidisciplinary. 2021;18:8238. doi: 10.3390/ijerph18168238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'sullivan R, Burns A, Leavey G, Leroi I, Burholt V, Lubben J, Holt-Lunstad J, Victor C, Lawlor B. Vilar-Compte M: Impact of the COVID-19 Pandemic on Loneliness and Social Isolation: A Multi-Country Study. Int J Environ Res Public Health Multidisciplinary. 2021;18:9982. doi: 10.3390/ijerph18199982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ochalek TA, Cumpston KL, Wills BK, Gal TS, Moeller FG. Nonfatal opioid overdoses at an urban emergency department during the COVID-19 pandemic. JAMA. 2020;324:1673–1674. doi: 10.1001/jama.2020.17477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Papaleontiou M, Henderson Charles R J, Turner BJ, Moore AA, Olkhovskaya Y, Amanfo L, Reid MC. Outcomes associated with opioid use in the treatment of chronic noncancer pain in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2010;58:1353–1369. doi: 10.1111/j.1532-5415.2010.02920.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pilkonis PA, Yu L, Dodds NE, Johnston KL, Lawrence SM, Hilton TF, Daley DC, Patkar AA, McCarty D. Vol. 18. 2017. An item bank for abuse of prescription pain medication from the Patient-Reported Outcomes Measurement Information System (PROMIS®) pp. 1516–1527. (Pain Med). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Raphael KG, Natelson BH, Janal MN, Nayak S. A community-based survey of fibromyalgia-like pain complaints following the World Trade Center terrorist attacks. Pain. 2002;100:131–139. doi: 10.1016/s0304-3959(02)00273-7. [DOI] [PubMed] [Google Scholar]
- 37.Reed DE, Cobos B, Lehinger EA, Nabity PS, Vail KE III, and McGeary DD, Pain-related disability, PTSD symptoms, and mood among a comorbid chronic pain and PTSD sample prior to and during the COVID-19 pandemic. J Health Psychol. In press. [DOI] [PubMed]
- 38.Schuler MS, Schell TL, Wong EC. Racial/ethnic differences in prescription opioid misuse and heroin use among a national sample, 1999–2018. Drug Alcohol Depend. 2021;221 doi: 10.1016/j.drugalcdep.2021.108588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Severeijns R, Vlaeyen JWS, van den Hout MA, Weber WEJ, Vlaeyven J, van den Hout MA, Weber WEJ. Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. Clin J Pain; 2001;17:165–172. doi: 10.1097/00002508-200106000-00009. [DOI] [PubMed] [Google Scholar]
- 40.Silver ER, Hur C. Gender differences in prescription opioid use and misuse: implications for men's health and the opioid epidemic. Prev Med (Baltim) 2020;131 doi: 10.1016/j.ypmed.2019.105946. [DOI] [PubMed] [Google Scholar]
- 41.Strickland JC, Stoops WW. The use of crowdsourcing in addiction science research: Amazon Mechanical Turk. Exp Clin Psychopharmacol Ame Psychol Assoc. 2019;27:1–18. doi: 10.1037/pha0000235. [DOI] [PubMed] [Google Scholar]
- 42.Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess [Internet] 1995;7:524–532. http://doi.apa.org/getdoi.cfm?doi=10.1037/1040-3590.7.4.524 Available from: [Google Scholar]
- 43.Veehof MM, Trompetter HR, Bohlmeijer ET, Schreurs KMG. Acceptance-and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cogn Behav Ther. 2016;45:5–31. doi: 10.1080/16506073.2015.1098724. [DOI] [PubMed] [Google Scholar]
- 44.Verma S, Mishra A. Depression, anxiety, and stress and socio-demographic correlates among general Indian public during COVID-19. Int J Soc Psychiatry. 2020;66:756–762. doi: 10.1177/0020764020934508. [DOI] [PubMed] [Google Scholar]
- 45.Yamada K, Wakaizumi K, Kubota Y, Murayama H, Tabuchi T. Loneliness, social isolation, and pain following the COVID-19 outbreak: data from a nationwide internet survey in Japan. Sci Rep. 2021;11:18643. doi: 10.1038/s41598-021-97136-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yu L, Kioskli K, McCracken LM. The psychological functioning in the COVID-19 pandemic and its association with psychological flexibility and broader functioning in people with chronic pain. J Pain. 2021;22:926–939. doi: 10.1016/j.jpain.2021.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]