Highlights
-
•
Self-advocacy and building rapport with providers facilitated decision-making for RRS-DO-focused previvors.
-
•
Avoiding menopause through RRS was a key motivator for RRS-DO-focused previvors.
-
•
RRS-DO-focused previvors viewed RRS as a stepwise approach to risk reduction.
-
•
Understanding previvor priorities and experiences can help optimize shared decision-making.
Keywords: BRCA, Lynch syndrome, Risk-reducing salpingectomy with delayed oophorectomy, Ovarian cancer risk reduction, Qualitative research
Abstract
Objective
Previvors are becoming more aware of the option of risk-reducing salpingectomy with delayed oophorectomy (RRS-DO) to mitigate their risk of ovarian cancer. In this qualitative study, we explored the clinical and non-clinical factors that impacted previvors’ decision-making to pursue RRS-DO as a risk reduction strategy.
Methods
Semi-structured telephone interviews were conducted with previvors and transcribed verbatim. Using ATLAS.ti® software, two primary investigators interpreted data through thematic analysis. After coding four interviews, the investigators discussed discrepancies between codes with a moderator and resolved and refined code. The investigators applied the universal codebook to all interviews and revised the codebook using an iterative approach. Examining codes within and across interviews allowed for major themes and patterns to emerge.
Results
Interviews were conducted with seventeen previvors (ages 31–46). 6 (25%) previvors had a BRCA1 mutation, 7 (41%), a BRCA2 mutation, 3 (13%), a Lynch-related mutation, and 1 (6%), other (MUTYH mutation). At the time of interview, 12 previvors (71%) were planning (6) or had undergone (6) RRS-DO, 4 (23%) were planning (1) or had undergone (3) risk reducing salpingo-oophorectomy (RRSO), and 1 (6%) was undecided. Three major themes emerged: motivating factors for selecting surgical risk reduction option, barriers complicating surgical decision-making, and facilitating factors for surgical decision-making. RRS-DO-focused previvors prioritized avoiding menopause, and they also emphasized that self-advocacy and building rapport with providers facilitated their decision-making.
Conclusion
By understanding previvors’ priorities and experiences, physicians can better partner with previvors as they navigate their ovarian cancer risk reduction journey. This will ultimately optimize shared decision-making.
1. Introduction
People with hereditary breast and ovarian cancer syndrome (HBOC) have an elevated risk for developing breast and ovarian cancer (Lancaster et al., 2007, Chen and Parmigiani, 2007, Antoniou et al., 2003). By age 70, people with a mutation in the BRCA1 gene have a 39–46% risk for developing ovarian cancer, and people with a mutation in the BRCA2 gene have a 10–27% risk (King et al., 2003). In comparison, the general population has a lifetime risk of 1.2% (SEER, 2021).
Screening with CA-125 and transvaginal ultrasound (TVUS) has little utility in reducing ovarian cancer mortality (Pinsky et al., 2017, Fishman et al., 2005, Menon et al., 2009). Consequently, the National Comprehensive Cancer Network (NCCN) recommends risk-reducing salpingo-oophorectomy (RRSO) to mitigate risk for people with HBOC (Daly et al., 2021). Studies have evaluated outcomes after RRSO, demonstrating a decrease in ovarian cancer risk and an overall survival benefit (Kauff et al., 2002, Rebbeck et al., 2002, Kauff et al., 2008, Finch et al., 2006, Grann et al., 2002). The NCCN recommends that people with a BRCA1 mutation undergo RRSO at ages 35–40 and people with a BRCA2 mutation undergo RRSO at ages 40–45 (Daly et al., 2021).
Despite recommendations, many with HBOC are reluctant to undergo RRSO at the recommended age (Holman et al., 2014). In light of accumulating evidence that BRCA1/2-associated ovarian tumors originate in the fallopian tube (Crum et al., 2007, Callahan et al., 2007, Leeper et al., 2002, Medeiros et al., 2006, Powell et al., 2005, Lu et al., 2000, Colgan et al., 2001, Yates et al., 2011, Jarboe et al., 2008, Kurman and Shih, 2010), some providers are now offering risk reducing salpingectomy with delayed oophorectomy (RRS-DO) as an alternative for these high-risk individuals (Swanson and Bakkum-Gamez, 2016). While RRS-DO is not currently accepted as standard of care, the WISP (NCT02760849), TUBA (NCT02321228), PROTECTOR (ISRCTN25173360), and SOROCk (NCT04251052) trials are prospective, multicenter trials investigating the outcomes associated with RRS-DO (M.D. Anderson Cancer Center, 2019, Harmsen et al., 2015, Gaba et al., 2021, NRG Oncology, 2021).
While previvors, people with HBOC, are increasingly aware of the option of RRS-DO to manage their genetic cancer risk, there are few studies assessing why previvors might choose RRS-DO over RRSO. In this study, we aimed to better understand the factors, both clinical and non-clinical, that contributed to previvors’ decisions to select RRS-DO as a risk reduction strategy.
2. Methods
This study was determined exempt by The Human Research Protection Program at the Icahn School of Medicine at Mount Sinai (ISMMS). Research methods were designed in consultation with a qualitative research expert.
2.1. Participants
Participants were referred by physicians at the Mount Sinai Hospital Campus and the Blavatnik Family Chelsea Medical Center at Mount Sinai. Participants were eligible if they were considering or had considered RRS-DO and if they had a documented deleterious mutation in one of the following genes associated with ovarian cancer: BRCA1, BRCA2, BRIP1, PALB2, RAD51C, RAD51D, BARD1, MUTYH, or Lynch-associated genes. All patients who met this eligibility criteria and presented to participating providers between June through September 2020 were invited to participate. Previvors who were planning RRSO or who had already completed RRSO were included as well to allow for further exploration of the tension arising in the surgical decision-making process.
2.2. Procedures
The research team designed a semi-structured interview guide involving open-ended questions. This interview guide explored patient genetic mutation history, physical and psychological effects of surgical menopause, sources of information, role of physicians, personal life, and perceptions after surgery (Supplementary material 1). One member of the research team conducted interviews over the phone between June-September 2020 until reaching data saturation. All participants received a research information sheet outlining possible risks involved in participation, and participants provided verbal consent to recorded interviews. All interviews were audio recorded and transcribed verbatim by a member of the research team. Identifying information was removed during the transcription process to preserve confidentiality.
2.3. Analysis
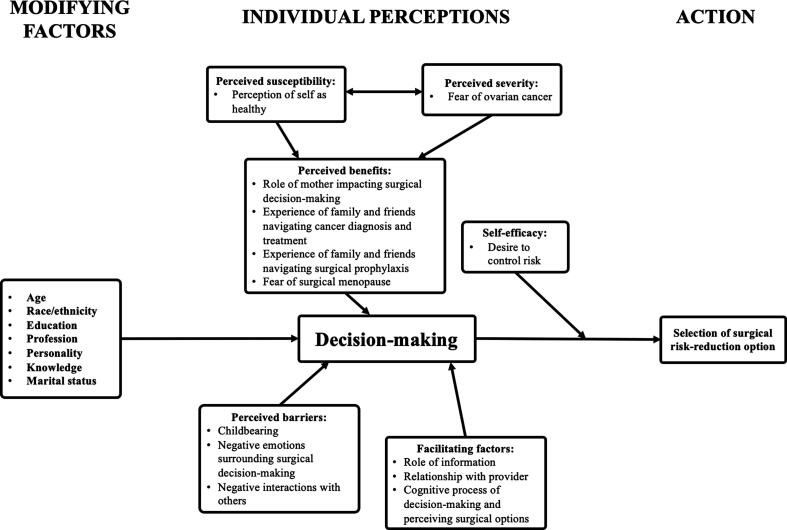
The Health Belief Model (HBM) was used as a theoretical framework to underpin thematic analysis of previvor narratives. First developed in the 1950s, the HBM is still widely applied to understand health behavior and is based on five cognitive constructs: perceived susceptibility, perceived severity, perceived barriers, perceived benefits, and self-efficacy (Green et al., 2020).
Two primary investigators, both clinicians, first read through all interviews (n = 17) using an immersion/crystallization approach, which involved reading, summarizing, and rereading data (Borkan et al., 1999). The two investigators then analyzed interviews (n = 4) through open coding techniques using ATLAS.ti® version 9.0.1, a software program for qualitative analysis. Based on the analytic process described by Boyatzis (Boyatzis, 1998), thematic analysis allowed for themes and patterns to emerge inductively through cataloguing direct quotes from interview narratives.
The two primary investigators then met with a moderator, a clinician trained in qualitative methods, who was blind to the study hypothesis and interview content. The investigators and moderator explored discrepancies between codes, and they resolved and refined codes. The investigators were randomly assigned the remaining interview transcripts, and they individually applied this universal codebook to all transcripts. The investigators continued to revise the codebook throughout the coding process through an iterative approach as themes emerged. Codes were then explored within and across transcripts to identify patterns and connections between interviews.
3. Results
Twenty-two patients were invited to participate, and 17 (age range 31–46) completed interviews with an acceptance rate of 77% (Table 1). The final codebook was comprised of 31 codes derived inductively from illustrative quotes. Codes were further categorized into ten sub-themes and three major themes: motivating factors for selecting surgical risk reduction options (Supplementary material 2, Table 1), barriers complicating surgical decision-making (Supplementary material, Table 2), and facilitating factors for surgical decision-making (Table 2). The relationship between these codes and sub-themes within the context of the HBM is depicted in Fig. 1. For the following sub-themes, the term “most” denotes at least thirteen previvors (76%), “many” denotes at least eight previvors (47%), “several” denotes at least four previvors (24%), and “a few” denotes three or fewer previvors.
Table 1.
Descriptive characteristics of interview participants.
| Characteristic | Previvors (N = 17) |
|---|---|
| Age, years | 38 (31–46) |
| Age at Diagnosis with Genetic Mutation, years | 30 (22–45) |
| Ethnicity | |
| Hispanic | 1 (5.9) |
| Non-Hispanic or Latinx | 16 (94) |
| Race | |
| White | 17 (100) |
| Genetic Mutation | |
| BRCA1 | 6 (35) |
| BRCA2 | 7 (41) |
| Lynch | 3 (18) |
| Other (MUTYH) | 1 (5.9) |
| Stage of Surgical Intervention | |
| Planning RRS | 6 (35) |
| Completed RRS | 5 (29) |
| Completed RRS-DO | 1 (5.9) |
| Planning RRSO | 1 (5.9) |
| Completed RRSO | 3 (18) |
| Undecided | 1 (5.9) |
| Prior Mastectomy | |
| Yes | 7 (41) |
| No | 10 (59) |
| Prior Cancer Diagnosis | |
| Breast cancer | 1 (5.9) |
| Endometrial cancer | 2 (12) |
| None | 14 (82) |
| Marital Status | |
| Married | 12 (71) |
| Single | 5 (29) |
| Children | |
| Yes | 11 (65) |
| No | 6 (35) |
Data are median (range) or n (%).
Table 2.
Organization of sub-themes and codes with illustrative quotes from RRS-DO-focused previvors for theme ‘Facilitating factors for surgical decision-making’.
| Theme | Sub-theme | Code | Quote |
|---|---|---|---|
| Facilitating factors for surgical decision-making | Role of information | Active data seeking and importance of information | “And every single time I see him, it’s yearly, my question is, what is the research? Tell me the research.“ |
| Sources of information regarding genetic diagnosis and risk reduction options | “I think these kinds of things you could just go down a rabbit hole and with the amount of content available with stuff like this. And I just didn’t -- I felt like I had enough information to make the decision.“ | ||
| Learning about RRS-DO as an option | “I had a baby and when I was by my OB he said 'you know, even if you’re not ready to get your ovaries out, you know they’ve shown that as a like, stopgap kind of thing, you can do this now and then do that a little bit later.' | ||
| Relationships with provider | Trust of provider expertise | “I feel like the best perspective you can get is from someone like [my doctor] who sees so many patients who go through it and sees how it ends up or like someone who’s had it done themselves. The articles are only so useful.“ | |
| Importance of rapport with provider | “So we had a very friendly conversation where I knew she wanted me to take them out. She told me why. She discussed the, you know, the statistics and whatnot… And I would really kind of characterize it as more of like a friendly banter of her saying, ‘you know you gotta get this done,’ and I would say yeah, but let’s wait till here, let’s wait till then.“ | ||
| Self-advocacy when navigating risk reduction options | “I could be proven wrong. But I’m personally comfortable with the risk benefit of keeping my ovaries until 50 at this moment in time….… and I’m going to try to get those five years.“ | ||
| Cognitive process of decision-making and perceiving surgical options | Stepwise approach | “In my head it’s extremely minor and possibly just because I fielded all the work, I met all the surgeons, I met everybody. And the breast surgery was just -- it sounds like a fuckin’ nightmare, and this sounds like, ‘ah, this is easy. This is an easy thing to check off the list.’ So I think that plays into it a lot.” | |
| Inevitability of risk reduction | “To me, like it’s not really that much of a decision. You do it ‘cause you gotta do it. Yeah, there are downsides to it. But you also wanna live.” | ||
| Positive emotions surrounding surgical-decision making | Acceptance of risk reduction option | “Then it’s something that you’ve bought into and accepted as opposed to just being sold on, you know. As opposed to just being convinced of, like, I guess, I didn’t want to be convinced that my situation was dire, drastic, and, you know, and horrible.“ | |
| Reassurance and confidence in surgical decision | “I asked her, hey, my old doctor told me about this thing, and she was like, “yeah, I recommend it.” And I was like there ya go, two doctors! That’s what I need to hear, from two doctors.“ |
Fig. 1.
Schematic representation mapping sub-themes and codes onto an adapted Health Belief Model, based on (Sripad et al., 2019) and (Champion and Skinner, 2008, Sripad et al., 2019, Champion and Skinner, 2008).
3.1. Motivating factors for selecting surgical risk reduction option
3.1.1. Perceptions of ovarian cancer risk
Almost all participants expressed a fear of ovarian cancer as the impetus for pursuing risk reduction. One previvor explained, “I think the ovarian one is so hard because the silent killer concept is very hard for me to grasp. And it’s kind of that one feels more out of control than the other ones.” Previvors who were reluctant to undergo RRSO still viewed salpingectomy as a risk-reducing measure. One previvor who underwent RRS-DO stated, “I think for my sanity I needed to just do what I could do to help myself, and prevent cancer from coming rather than just wait around and see if it happened.”
Still, despite this risk, several previvors weighed the likelihood of an ovarian cancer diagnosis in their decision to undergo RRS-DO. One previvor reflected, “If it didn’t have any adverse effects, I would take it all out… But the other risks of my quality of my life, like so impacted, that I don’t know if it’s worth the risk for me. So with my thirty percent of ovarian cancer and my zero family history of it, I’m not willing to take out every female organ I own.”
3.1.2. Relationships with family
All previvors with children referenced motherhood as the most important factor in their decision to undergo surgical risk reduction. One previvor explained, “Once I found out I was positive, the main factors was just like, ok, I have small children. I want to be around for them. I wanted to do everything that I could. Almost like a panic. Like oh my gosh, nothing can happen to me right now, they’re so little, they need me.”
Several previvors also explained how watching their loved ones navigate cancer motivated them to pursue surgical risk reduction. One previvor recounted her mother’s battle with ovarian cancer: “This is now kind of chronic disease for her, and chronic abdominal pain, and unless there’s some insane tragedy that we’re not anticipating, this is what’s gonna kill her. And we all know it… so it’s always kind of like this afterthought that like, oh yeah, this could be my future unless I do something to prevent it.”
3.1.3. Fear of surgical menopause
Physical and psychological outcomes associated with surgical menopause drove many previvors to select RRS-DO. As one previvor explained, “I was reading everything I could get my hands on. Which basically made my eyes pop out of my head because it wasn’t just vanity things like gaining weight and whatever else. It was also, like, dementia, Alzheimer’s, heart disease. Really crazy, you know, serious stuff.” Almost all previvors also voiced concerns about vaginal dryness, libido, emotional wellbeing, weight gain, hot flashes, and/or aging.
When discussing hormone replacement therapy (HRT), several previvors who chose RRS-DO felt that the research was “inconclusive” or “too ambiguous for my taste.” Conversely, previvors who chose RRSO viewed menopause symptoms as “better than the alternative” and were more receptive to HRT to mitigate side effects.
Previvors who selected RRSO were more likely to cite the need to undergo two surgeries as a factor in decision making. One of these previvors stated, “My thoughts were I’d rather go through as little surgery as possible, so I’d rather take care of something all at the same time.” On the other hand, one previvor who preferred RRS-DO explained how “it’s a laparoscopic surgery. I can handle it. It’s not that bad and it’ll be like five years apart.”
3.2. Barriers complicating surgical decision-making
3.2.1. Childbearing
Several previvors voiced that they deferred considering risk reduction altogether until after completing childbearing, and a few described psychological distress regarding the loss of fertility accompanying risk reduction. One previvor elucidated, “I feel bad because it’s like this decision is taken away from me because I have to have this surgery done.” Still, although several previvors incorporated surgical risk reduction into their timeline for conceiving or undergoing fertility treatments, maintaining fertility ultimately did not play a role in whether previvors chose to undergo RRS-DO versus RRSO.
3.2.2. Negative emotions surrounding surgical decision-making
Many previvors described their decision-making process as one wrought by confusion and anxiety. Before deciding to undergo RRS-DO, a previvor explained, “I felt like I spent all this time gathering data and I felt very anxious and very nervous and very uneasy.” A few previvors who preferred RRS-DO also voiced concern about insufficient risk reduction. One previvor said, “I don’t know if I’m gonna feel any relief after getting the fallopian tubes out ‘cause right now I don’t know how much of the risk I’m mitigating doing that. But it’s the right path.”
Most previvors also voiced frustration regarding the need for more definitive data and research behind surgical options and ovarian cancer risk, and previvors who were not BRCA1/2 mutation carriers vocalized that a lack of data precluded them from making an informed decision. For example, one previvor stated, “We were sort of desperately looking for more information on the EPCAM mutation and sort of like, more research saying our risks might be a little lower… Every time I’ve asked the doctor it’s been like every research article or any evidence that I’ve found, like ‘there’s just not enough of you to have been researched and we just don’t know yet.’”
3.2.3. Negative interactions with others
Several previvors felt alienated by their providers as they navigated the risk reduction process. As one previvor reflected, her providers failed to provide her with adequate counseling while she weighed her risk reduction options. This previvor felt that “it was ‘ovaries, ovaries, ovaries, now, now, now.’ And also no real discussion about what the rest of my life would look like, as far as going into menopause so early and abruptly.”
3.3. Facilitating factors for surgical decision-making
3.3.1. Role of information
Most previvors actively sought out information and data, which played a central role in their decision to undergo RRS-DO or RRSO. One previvor who underwent RRS-DO stressed her independence in this process: “In terms of the studies, that was extremely important to me. Particularly larger ones and longer ones, ‘cause, you know, that’s where the proof is essentially. And for me as a lawyer I’m very proof and fact driven.” RRS-DO-focused previvors were also more likely to utilize a variety of resources to collect information, from scholarly articles to websites to family and friends. Still, while several previvors found it helpful to explore information on their own, others felt that “there’s just so much clutter” and “it’s just so easy to put out information that’s manipulative.”
3.3.2. Relationships with provider
RRS-DO-focused previvors expressed that shared decision-making with their physicians empowered them to select their preferred risk reduction strategy. One previvor explained how having rapport with her physician encouraged her to pursue RRS-DO: “I’ve also built a relationship with [my doctor] at this point over many, many years. And so I feel very comfortable with her, I like her a lot, I trust her implicitly, and I thought it was a good, you know, compromise.”
Previvors also valued their providers’ expertise in risk reduction. For one previvor, learning about other previvors’ experiences through her gynecologic oncologist helped her settle on RRS-DO: “She gave me a little bit of insight into sentiments of other people who’ve made this decision… Typically I’m pretty fact and data driven, but in this case I actually think that it was helpful to hear other people’s thought process and it was similar, or other processes that I maybe didn’t even think of.”
Self-advocacy with physicians was a crucial component of the risk reduction process for RRS-DO-focused previvors. One previvor who underwent RRS described such conversations: “So about two and a half years ago I had a whole discussion with [my doctor] and we took out the other fallopian tube, but we negotiated. Because she, at the time, wanted me to do my ovaries. And I really wanted to buy myself some more time, so there was a discussion… I’m a tough negotiator.” RRSO-focused previvors, however, were more likely to rely solely on their provider’s recommendation. One previvor simply said, “If I pick a doctor who I trust I really just follow their recommendations.”
3.3.3. Cognitive process of decision-making and perceiving surgical options
Both RRS-DO and RRSO- focused previvors asserted that their choice seemed obvious and inevitable. Once they discussed options with their physician, the RRS-DO-focused previvors described this preference as a “brilliant idea” and “a no-brainer.” RRSO previvors used similar terminology, as their decision was “clear cut” and “pretty easy.”
For several, first pursuing RRS enabled previvors to delay decision-making surrounding surgical menopause. One previvor explained, “I’m just kinda hanging on to that ‘I don’t have to think about it’ feeling, ‘cause I can just deal with the fallopian tubes first… and then I can do my research and make decisions later.” Other previvors viewed RRS as a pragmatic, intermediary step as they anticipated more data regarding RRS-DO outcomes. As one previvor asserted, “Science moves quickly. And I’m just trying to wait it out.”
3.3.4. Positive emotions surrounding surgical decision-making
For both RRSO and RRS-DO focused previvors, positive reinforcement from others helped previvors feel reassured in their decision. For example, as one previvor recounted, “I feel like I finally, after all these years, having this surgery scheduled three times, like I got off the phone with [my doctor] and felt confident in what I was doing. And I really haven’t looked back since then.” Acceptance also permitted previvors to move forward with surgical prophylaxis, and one previvor painted this experience almost as transcendent: “I was in complete alignment in what’s right for me. And I think when you are in that state, when you get to that place where you are at peace with your decision and you know that this is the right thing for you, then there is no place for fear and doubt and any of that.”
4. Discussion
In this study, using the HBM as a theoretical framework shed light on the barriers, motivating factors, and facilitating factors impacting previvors’ selection of RRS-DO as a risk reduction strategy. RRS-DO-focused previvors differed from RRSO-focused previvors in several distinct ways, as they rationalized their ovarian cancer risk, prioritized the delay of surgical menopause, advocated for themselves and partnered with providers, and viewed RRS as a stepwise approach to risk reduction.
Other qualitative studies involving people with BRCA1/2 mutations have similarly assessed factors impacting risk reduction choices. Studies in the Netherlands and England identified maintaining ovarian function as the major facilitator and priority, respectively, for previvors selecting RRS-DO (Arts-de Jong et al., 2015, Gaba et al., 2021). Concerns about undergoing surgery and ambivalence about HRT have also been described as deterrents to surgical prophylaxis, and anxiety regarding personal cancer risk has been a motivator behind why some previvors pursue RRSO (Segerer et al., 2020, Bhavnani and Clarke, 2003, Brotto et al., 2012, Kenen et al., 2007, Hurley et al., 2001, Segerer et al., 2020, Herrmann et al., 2018). Our study built upon these prior studies, as we interviewed people with a variety of deleterious mutations and further delved into the dynamics of the patient-provider relationship. As such, our findings offered another window into the risk reduction process, and they suggested that addressing previvor concerns through improved communication and patient education may enhance decision-making.
It is important to note that although RRS-DO is gaining popularity among previvors, this strategy is not currently accepted as standard of care. According to the Society of Gynecologic Oncology (SGO), RRS-DO should be offered only to previvors who would otherwise defer or decline risk reduction entirely (SGO Clinical Practice Statement, 2021). In our findings, unlike in a prior study, uncertainty in the effectiveness of RRS-DO did not compel previvors to select RRSO (Arts-de Jong et al., 2015). These previvors remained optimistic that RRS would enable them to await more information from ongoing trials prior to considering oophorectomy. The currently accruing SOROCk trial will eventually answer these questions for BRCA1 mutation carriers, but with 20 years of follow up, the results will likely not be timely enough for those currently pursuing surgical risk reduction.
The results of this current study have important implications for clinical practice, as developing a relationship with a physician based on trust and mutual respect was central to previvor decision-making. Previvors voiced that learning about other previvors’ experiences with risk reduction through the perspective of the gynecologic oncologist enhanced informed decision-making, which was consistent with prior studies demonstrating the impact of experiential knowledge rather than statistics alone (Siyam et al., 2018, Kenen et al., 2007, Herrmann et al., 2018).
This study has several strengths. To our knowledge, this study is the first in the United States to apply the HBM to ovarian cancer risk reduction and use in-depth interviews to understand why previvors might select RRS-DO over RRSO. Additionally, this comprehensive qualitative approach fully characterized the values and experiences that individually and collectively impacted previvor decision-making. A semi-structured interview format focused on questions that typically arise in patient discussions about surgical prophylaxis while simultaneously allowing for participants to explore ideas that arose organically.
This study also had several limitations. All previvors were recruited from one gynecologic oncology practice at a major academic medical center in New York City and were primarily non-Hispanic white people. As such, findings cannot be generalized to the population of people with HBOC as a whole. Historically, providers have initiated fewer discussions regarding genetic testing with Black and Spanish-speaking Hispanic women, and Black people with BRCA1/2 mutations have had significantly lower rates of RRSO (Cragun et al., 2017, Armstrong et al., 2005, Forman and Hall, 2009). These disparities, evidence of longstanding systemic racism, may explain the lack of ethnic and racial diversity among this study’s participants, although there is irrefutably an unmet need to improve patient education and access to care for people of color who would benefit from risk reduction. Next, findings did not fully capture the way in which breast cancer shaped attitudes towards ovarian cancer risk reduction. The median age of previvors in this study was 38 years, and seven previvors had mastectomies by the time of interview, which together may account for, in part, the low incidence of breast cancer in this particular group.
Ultimately, insights from these previvor narratives can help physicians better understand how each individual patient approaches decision-making and enable physicians to partner with previvors more effectively throughout the risk reduction journey. Improving patient education regarding surgical menopause and prioritizing communication and shared decision-making may build previvor confidence and satisfaction with surgical prophylaxis, allowing each previvor to pursue a risk reduction strategy that best fits individual goals and values. Future studies should employ qualitative methods to better understand factors impacting the ovarian cancer risk-reduction process for people of color and non-English speaking people and to assess the role of expanded health information for these populations. Future studies should also address how previvor and provider opinions shift with forthcoming data from the WISP, TUBA, PROTECTOR, and SOROCk trials.
Funding Sources
None.
Financial Disclosures
None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this abstract.
CRediT authorship contribution statement
Caroline Gellman: Validation, Formal analysis, Investigation, Visualization, Writing – original draft, Writing – review & editing. Charlotte Ezratty: Formal analysis, Investigation. Julia Schwarz: Conceptualization, Methodology, Validation. Valentin Kolev: Resources, Supervision. Stephanie V. Blank: Conceptualization, Methodology, Validation, Resources, Visualization, Writing – review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We thank all of the previvors who participated in interviews for sharing their stories with us.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.gore.2022.100948.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- Antoniou A., Pharoah P.D.P., Narod S., Risch H.A., Eyfjord J.E., Hopper J.L., Loman N., Olsson H., Johannsson O., Borg Å., Pasini B., Radice P., Manoukian S., Eccles D.M., Tang N., Olah E., Anton-Culver H., Warner E., Lubinski J., Gronwald J., Gorski B., Tulinius H., Thorlacius S., Eerola H., Nevanlinna H., Syrjäkoski K., Kallioniemi O.-P., Thompson D., Evans C., Peto J., Lalloo F., Evans D.G., Easton D.F. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am. J. Hum. Genet. 2003;72(5):1117–1130. doi: 10.1086/375033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong K., Micco E., Carney A., Stopfer J., Putt M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA. 2005;293(14):1729–1736. doi: 10.1001/jama.293.14.1729. [DOI] [PubMed] [Google Scholar]
- Arts-de Jong M., Harmsen M.G., Hoogerbrugge N., Massuger L.F., Hermens R.P., de Hullu J.A. Risk-reducing salpingectomy with delayed oophorectomy in BRCA1/2 mutation carriers: patients’ and professionals’ perspectives. Gynecol. Oncol. 2015;136(2):305–310. doi: 10.1016/j.ygyno.2014.12.031. [DOI] [PubMed] [Google Scholar]
- Bhavnani V., Clarke A. Women awaiting hysterectomy: a qualitative study of issues involved in decisions about oophorectomy. BJOG. 2003;110(2):168–174. [PubMed] [Google Scholar]
- Borkan J. In: Doing Qualitative Research. Crabtree B., Miller W., editors. Sage Publications; 1999. Immersion/Crystallization; pp. 179–194. [Google Scholar]
- Boyatzis R.E. Sage Publications; 1998. Transforming Qualitative Information: Thematic Analysis and Code Development. [Google Scholar]
- Brotto L.A., Branco N., Dunkley C., McCullum M., McAlpine J.N. Risk-reducing bilateral salpingo-oophorectomy and sexual health: a qualitative study. J. Obstet. Gynaecol. Can. 2012;34(2):172–178. doi: 10.1016/S1701-2163(16)35160-X. [DOI] [PubMed] [Google Scholar]
- Callahan M.J., Crum C.P., Medeiros F., Kindelberger D.W., Elvin J.A., Garber J.E., Feltmate C.M., Berkowitz R.S., Muto M.G. Primary fallopian tube malignancies in BRCA-positive women undergoing surgery for ovarian cancer risk reduction. J. Clin. Oncol. 2007;25(25):3985–3990. doi: 10.1200/JCO.2007.12.2622. [DOI] [PubMed] [Google Scholar]
- Champion V.L., Skinner C. Health Behavior and Health Education: Theory, Research, and Practice. 4th ed. Jossey-Bass; 2008. The Health Belief Model; pp. 45–65. [Google Scholar]
- Chen S., Parmigiani G. Meta-analysis of BRCA1 and BRCA2 penetrance. J. Clin. Oncol. 2007;25(11):1329–1333. doi: 10.1200/JCO.2006.09.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colgan T.J., Murphy J., Cole D.E., Narod S., Rosen B. Occult carcinoma in prophylactic oophorectomy specimens: prevalence and association with BRCA germline mutation status. Am. J. Surg. Pathol. 2001;25(10):1283–1289. doi: 10.1097/00000478-200110000-00009. [DOI] [PubMed] [Google Scholar]
- Cragun D., Weidner A., Lewis C., Bonner D., Kim J., Vadaparampil S.T., Pal T. Racial disparities in BRCA testing and cancer risk management across a population-based sample of young breast cancer survivors. Cancer. 2017;123(13):2497–2505. doi: 10.1002/cncr.30621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crum C.P., Drapkin R., Miron A., Ince T.A., Muto M., Kindelberger, et al. The distal fallopian tube: a new model for pelvic serous carcinogenesis. Curr. Opin. Obstet. Gynecol. 2007;19(1):3–9. doi: 10.1097/GCO.0b013e328011a21f. [DOI] [PubMed] [Google Scholar]
- Daly M.B., Pal T., Berry M.P., Buys S.S., Dickson P., Domchek S.M., Elkhanany A., Friedman S., Goggins M., Hutton M.L., Karlan B.Y., Khan S., Klein C., Kohlmann W., Kurian A.W., Laronga C., Litton J.K., Mak J.S., Menendez C.S., Merajver S.D., Norquist B.S., Offit K., Pederson H.J., Reiser G., Senter-Jamieson L., Shannon K.M., Shatsky R., Visvanathan K., Weitzel J.N., Wick M.J., Wisinski K.B., Yurgelun M.B., Darlow S.D., Dwyer M.A. Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 2021;19(1):77–102. doi: 10.6004/jnccn.2021.0001. [DOI] [PubMed] [Google Scholar]
- Finch A., Beiner M., Lubinski J., Lynch H.T., Moller P., Rosen B., et al. Salpingo-oophorectomy and the risk of ovarian, fallopian tube, and peritoneal cancers in women with a BRCA1 or BRCA2 Mutation. JAMA. 2006;296(2):185–192. doi: 10.1001/jama.296.2.185. [DOI] [PubMed] [Google Scholar]
- Fishman D.A., Cohen L., Blank S.V., Shulman L., Singh D., Bozorgi K., Tamura R., Timor-Tritsch I., Schwartz P.E. The role of ultrasound evaluation in the detection of early-stage epithelial ovarian cancer. Am. J. Obstet. Gynecol. 2005;192(4):1214–1221. doi: 10.1016/j.ajog.2005.01.041. [DOI] [PubMed] [Google Scholar]
- Forman A.D., Hall M.J. Influence of race/ethnicity on genetic counseling and testing for hereditary breast and ovarian cancer. Breast J. 2009;15(Suppl 1):S56–S62. doi: 10.1111/j.1524-4741.2009.00798.x. [DOI] [PubMed] [Google Scholar]
- Gaba F., Robbani S., Singh N., McCluggage W.G., Wilkinson N., Ganesan R., Bryson G., Rowlands G., Tyson C., Arora R., Saridogan E., Hanson H., Burnell M., Legood R., Evans D.G., Menon U., Manchanda R. Preventing Ovarian Cancer through early Excision of Tubes and late Ovarian Removal (PROTECTOR): protocol for a prospective non-randomised multi-center trial. Int J Gynecol Cancer. 2021;31(2):286–291. doi: 10.1136/ijgc-2020-001541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaba F., Goyal S., Marks D., Chandrasekaran D., Evans O., Robbani S., et al. Surgical decision making in premenopausal BRCA carriers considering risk-reducing early salpingectomy or salpingo-oophorectomy: a qualitative study. J. Med. Genet. 2021 doi: 10.1136/jmedgenet-2020-107501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grann V.R., Jacobson J.S., Thomason D., Hershman D., Heitjan D.F., Neugut A.I. Effect of prevention strategies on survival and quality-adjusted survival of women with BRCA1/2 mutations: an updated decision analysis. J. Clin. Oncol. 2002;20(10):2520–2529. doi: 10.1200/JCO.2002.10.101. [DOI] [PubMed] [Google Scholar]
- Green, E.C., Murphy, E.M., Gryboski, K., 2020. The Health Belief Model. In: Sweeny, K., Robbins, M., Cohen, L. (Eds.), The Wiley Encyclopedia of Health Psychology, pp. 211–214.
- Harmsen M.G., Arts-de Jong M., Hoogerbrugge N., Maas A.H.E.M., Prins J.B., Bulten J., Teerenstra S., Adang E.M.M., Piek J.M.J., van Doorn H.C., van Beurden M., Mourits M.J.E., Zweemer R.P., Gaarenstroom K.N., Slangen B.F.M., Vos M.C., van Lonkhuijzen L.R.C.W., Massuger L.F.A.G., Hermens R.P.M.G., de Hullu J.A. Early salpingectomy (TUbectomy) with delayed oophorectomy to improve quality of life as alternative for risk-reducing salpingo-oophorectomy in BRCA1/2 mutation carriers (TUBA study): a prospective non-randomised multicentre study. BMC Cancer. 2015;15(1) doi: 10.1186/s12885-015-1597-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann A., Hall A., Proietto A. Using the Health Belief Model to explore why women decide for or against the removal of their ovaries to reduce their risk of developing cancer. BMC Women’s Health. 2018;18(1):184. doi: 10.1186/s12905-018-0673-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman L.L., Friedman S., Daniels M.S., Sun C.C., Lu K.H. Acceptability of prophylactic salpingectomy with delayed oophorectomy as risk-reducing surgery among BRCA mutation carriers. Gynecol. Oncol. 2014;133(2):283–286. doi: 10.1016/j.ygyno.2014.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley K.E., Miller S.M., Costalas J.W., Gillespie D., Daly M.B. Anxiety/uncertainty reduction as a motivation for interest in prophylactic oophorectomy in women with a family history of ovarian cancer. J. Womens Health Gend. Based. Med. 2001;10(2):189–199. doi: 10.1089/152460901300039566. [DOI] [PubMed] [Google Scholar]
- Jarboe, E.A., Folkins, A., Callahan, M.J., (Eds.), 2008. Pathology of BRCA-Associated Ovarian Cancers, Including Occult Cancers. In: Hereditary Gynecologic Cancer: Risk, Prevention, and Management. Informa Healthcare, pp. 29-43.
- Kauff N.D., Satagopan J.M., Robson M.E., Scheuer L., Hensley M., Hudis C.A., Ellis N.A., Boyd J., Borgen P.I., Barakat R.R., Norton L., Castiel M., Nafa K., Offit K. Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N. Engl. J. Med. 2002;346(21):1609–1615. doi: 10.1056/NEJMoa020119. [DOI] [PubMed] [Google Scholar]
- Kauff N.D., Domchek S.M., Friebel T.M., Robson M.E., Lee J., Garber J.E., Isaacs C., Evans D.G., Lynch H., Eeles R.A., Neuhausen S.L., Daly M.B., Matloff E., Blum J.L., Sabbatini P., Barakat R.R., Hudis C., Norton L., Offit K., Rebbeck T.R. Risk-reducing salpingo-oophorectomy for the prevention of BRCA1- and BRCA2-associated breast and gynecologic cancer: a multicenter, prospective study. J. Clin. Oncol. 2008;26(8):1331–1337. doi: 10.1200/JCO.2007.13.9626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenen R.H., Shapiro P.J., Friedman S., Coyne J.C. Peer-support in coping with medical uncertainty: discussion of oophorectomy and hormone replacement therapy on a web-based message board. Psychooncology. 2007;16(8):763–771. doi: 10.1002/pon.1152. [DOI] [PubMed] [Google Scholar]
- King M.-C., Marks J.H., Mandell J.B. Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science. 2003;302(5645):643–646. doi: 10.1126/science.1088759. [DOI] [PubMed] [Google Scholar]
- Kurman R.J., Shih I.-M. The origin and pathogenesis of epithelial ovarian cancer: a proposed unifying theory. Am. J. Surg. Pathol. 2010;34(3):433–443. doi: 10.1097/PAS.0b013e3181cf3d79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancaster J., Bethanpowell C., Kauff N., Cass I., Chen L., Lu K., Mutch D., Berchuck A., Karlan B., Herzog T. Society of Gynecologic Oncologists Education Committee Statement on Risk Assessment for Inherited Gynecologic Cancer Predispositions. Gynecol. Oncol. 2007;107(2):159–162. doi: 10.1016/j.ygyno.2007.09.031. [DOI] [PubMed] [Google Scholar]
- Leeper K., Garcia R., Swisher E., Goff B., Greer B., Paley P. Pathologic findings in prophylactic oophorectomy specimens in high-risk women. Gynecol. Oncol. 2002;87(1):52–56. doi: 10.1006/gyno.2002.6779. [DOI] [PubMed] [Google Scholar]
- Lu K.H., Garber J.E., Cramer D.W., Welch W.R., Niloff J., Schrag D., Berkowitz R.S., Muto M.G. Occult ovarian tumors in women with BRCA1 or BRCA2 mutations undergoing prophylactic oophorectomy. J. Clin. Oncol. 2000;18(14):2728–2732. doi: 10.1200/JCO.2000.18.14.2728. [DOI] [PubMed] [Google Scholar]
- M.D. Anderson Cancer Center. WISP (Women Choosing Surgical Prevention). clinicaltrials.gov; 2019. Accessed January 28, 2021. https://clinicaltrials.gov/ct2/show/NCT02760849.
- Medeiros F., Muto M.G., Lee Y., Elvin J.A., Callahan M.J., Feltmate C., Garber J.E., Cramer D.W., Crum C.P. The tubal fimbria is a preferred site for early adenocarcinoma in women with familial ovarian cancer syndrome. Am. J. Surg. Pathol. 2006;30(2):230–236. doi: 10.1097/01.pas.0000180854.28831.77. [DOI] [PubMed] [Google Scholar]
- Menon U., Gentry-Maharaj A., Hallett R., Ryan A., Burnell M., Sharma A., Lewis S., Davies S., Philpott S., Lopes A., Godfrey K., Oram D., Herod J., Williamson K., Seif M.W., Scott I., Mould T., Woolas R., Murdoch J., Dobbs S., Amso N.N., Leeson S., Cruickshank D., Mcguire A., Campbell S., Fallowfield L., Singh N., Dawnay A., Skates S.J., Parmar M., Jacobs I. Sensitivity and specificity of multimodal and ultrasound screening for ovarian cancer, and stage distribution of detected cancers: results of the prevalence screen of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) Lancet Oncol. 2009;10(4):327–340. doi: 10.1016/S1470-2045(09)70026-9. [DOI] [PubMed] [Google Scholar]
- NRG Oncology. A Non-Randomized Prospective Clinical Trial Comparing the Non-Inferiority of Salpingectomy to Salpingo-Oophorectomy to Reduce the Risk of Ovarian Cancer Among BRCA1 Carriers [SOROCk]. clinicaltrials.gov; 2021. Accessed December 21, 2020. https://clinicaltrials.gov/ct2/show/NCT04251052.
- Pinsky P.F., Prorok P.C., Yu K., Kramer B.S., Black A., Gohagan J.K., Crawford E.D., Grubb R.L., Andriole G.L. Extended mortality results for prostate cancer screening in the PLCO trial with median follow-up of 15 years. Cancer. 2017;123(4):592–599. doi: 10.1002/cncr.30474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell C.B., Kenley E., Chen L.-M., Crawford B., McLennan J., Zaloudek C., Komaromy M., Beattie M., Ziegler J. Risk-reducing salpingo-oophorectomy in BRCA mutation carriers: role of serial sectioning in the detection of occult malignancy. J. Clin. Oncol. 2005;23(1):127–132. doi: 10.1200/JCO.2005.04.109. [DOI] [PubMed] [Google Scholar]
- Rebbeck T.R., Lynch H.T., Neuhausen S.L., Narod S.A., van't Veer L., Garber J.E., Evans G., Isaacs C., Daly M.B., Matloff E., Olopade O.I., Weber B.L. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N. Engl. J. Med. 2002;346(21):1616–1622. doi: 10.1056/NEJMoa012158. [DOI] [PubMed] [Google Scholar]
- SEER. Cancer of the Ovary - Cancer Stat Facts. Accessed March 10, 2021. https://seer.cancer.gov/statfacts/html/ovary.html.
- Segerer R., Peschel C., Kämmerer U., Häussler S., Wöckel A., Segerer S. Factors Impacting on Decision-Making towards Prophylactic Surgeries in BRCA Mutation Carriers and Women with Familial Predisposition. Breast Care (Basel). 2020;15(3):253–259. doi: 10.1159/000503370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SGO Clinical Practice Statement. Salpingectomy for Ovarian Cancer Prevention. Accessed January 27, 2021. https://www.sgo.org/resources/sgo-clinical-practice-statement-salpingectomy-for-ovarian-cancer-prevention/#:~:text=SGO%20Clinical%20Practice%20Statement%3A%20Salpingectomy,Prevention%20(SGO%2C%20November%202013)&text=Salpingectomy%20may%20be%20appropriate%20and,may%20be%20the%20fallopian%20tube.
- Siyam T., Ross S., Shandro T., Hagen S., Battochio L., Yuksel N. Perspectives and decision-making about menopausal therapies in women who had bilateral oophorectomy. Menopause. 2018;25(7):795–802. doi: 10.1097/GME.0000000000001069. [DOI] [PubMed] [Google Scholar]
- Sripad P., Kirk K., Adoyi G., Dempsey A., Ishaku S., Warren C.E. Exploring survivor perceptions of pre-eclampsia and eclampsia in Nigeria through the health belief model. BMC Pregnancy Childbirth. 2019;19(1):431. doi: 10.1186/s12884-019-2582-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson C.L., Bakkum-Gamez J.N. Options in Prophylactic Surgery to Prevent Ovarian Cancer in High-Risk Women: How New Hypotheses of Fallopian Tube Origin Influence Recommendations. Curr. Treat. Options Oncol. 2016;17(5):20. doi: 10.1007/s11864-016-0396-2. [DOI] [PubMed] [Google Scholar]
- Yates M.S., Meyer L.A., Deavers M.T., Daniels M.S., Keeler E.R., Mok S.C., Gershenson D.M., Lu K.H. Microscopic and early-stage ovarian cancers in BRCA1/2 mutation carriers: building a model for early BRCA-associated tumorigenesis. Cancer Prev Res. 2011;4(3):463–470. doi: 10.1158/1940-6207.CAPR-10-0266. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.