Abstract
Depression and anxiety have been associated with cigarette use among young people. Higher impulsivity has also been associated with increased smoking behavior. However, relatively less is known about the associations between depression, anxiety, impulsivity and e-cigarette use and how these associations compare with the associations between depression, anxiety, impulsivity and cigarette smoking. In addition, little is known about how impulsivity influences the relationships between depression, anxiety, cigarette, and e-cigarette use. This study tested the hypothesis that higher depression and anxiety symptoms are associated with higher e-cigarette use and cigarette smoking in a similar way, and that these associations would be stronger among those with higher impulsivity. A sample of 2,622 young adults (18-25 year olds; 54% women) enrolled in 4-year and 2-year colleges in Hawai‘i participated in a cross-sectional survey. Approximately 68% of the sample reported no use of either e-cigarettes or cigarettes, 13% reported only e-cigarette use, 9% reported only cigarette smoking, and 11% reported use of both. The study found that higher depressive and anxiety symptoms and higher impulsivity were significantly associated with current cigarette and e-cigarette use. For example, one unit increases in depression, anxiety, and impulsivity were associated with 34%, 17%, and 38% increased odds of e-cigarette use versus non-use, respectively. Impulsivity was found to significantly moderate the association between higher anxiety and higher cigarette smoking, such that the association was stronger among those with higher impulsivity. Impulsivity was not found to moderate any other association. Results suggest that tobacco product use prevention education should target children and young adults with higher internalizing symptoms, with particular attention to those who show higher impulsivity.
Keywords: Depressive symptoms, Anxiety symptoms, Impulsivity, Cigarettes, E-Cigarettes, Young Adults
Introduction
Electronic or e-cigarettes are becoming more commonly used by United States (US) high and middle school students than combustible cigarettes,1 despite having been marketed widely for only about a decade. The risks of cigarette smoking and second-hand exposure to cigarette smoke have been known for decades.2 However, as e-cigarettes are a relatively new product on the market, little is known regarding their potential risks. E.cigarettes appear to be less harmful than cigarettes; as a result, some people perceive them to be safer or healthier alternatives to combustible cigarettes.3 Unfortunately, however, now many young people are being introduced to nicotine use through e.cigarettes, especially in Hawai‘i.4 In 2017, more Hawai‘i high school students reported themselves as current e-cigarette users (26%) than cigarette smokers (8%).5 Nationally, approximately, 3.6 million youths are current e-cigarette users.6 E-cigarettes are available in many different flavors, which young people tend to find highly attractive.7
Apart from flavors, young people find e-cigarettes attractive because e-cigarette aerosol is easier to inhale, does not smell bad, is considered less harmful, and yet is able to deliver nicotine.8 For some young people, the motive of e-cigarette use is social enhancement, such as an increase in popularity among peers and an enhanced social image.8 Although cigarette smokers commonly use e-cigarettes for help with smoking cessation, some do not find e-cigarettes to be helpful in managing their cigarette smoking behavior.9 Another potential risk of e-cigarettes is that individuals who have never smoked cigarettes, or who are novice smokers, may find e-cigarettes as a more appealing cigarette alternative for nicotine delivery.8,9 Smokers consume cigarettes primarily because of nicotine, which is a psychostimulant and addictive. However, cigarette smoke smells relatively harsh and tastes bitter. These characteristics may deter never or novice smokers from smoking, even though they may like the pleasurable effects of nicotine. E-cigarette aerosol, on the other hand, is less harsh and bitter. Furthermore, because e-cigarette aerosol is usually flavored, it smells and tastes good. Hence, individuals who might have been deterred from smoking cigarettes for nicotine intake may find e-cigarettes as a better alternative for delivery of nicotine.
Cigarettes have been known to cause cancer (especially lung cancer), asthma, diabetes, gum disease, heart disease, and stroke.2 However, the definite harms caused by e-cigarettes are not as well-known. E-cigarettes may cause asthma,10 decreased lung function,11 an increased innate immune response in the lung,12,13 and cardiovascular disease.14 Even though in smaller amounts than cigarettes, e-cigarettes are known to contain dangerous carcinogens such as nitric oxide, which when burned creates formaldehyde.15 Second-hand exposure to e-cigarette aerosol may also be risky, although the level of risks are currently unknown.16 In 2019, the CDC investigated a national outbreak of e-cigarette or vaping product use associated lung injury (EVALI).17,18 As of October 2019, there were 1,604 reported cases of EVALI, and 34 EVALI-related deaths in 24 states.17,18 Therefore, despite popular notions about e-cigarettes being safer than cigarettes, there are still many potential risks that e-cigarettes may pose.
An area of research that has been understudied is the use of e-cigarettes by youth and young adults with symptoms of poor mental health. Data from the 2016 National Survey of Children’s Health (NSCH) found that among children aged 3-17 years in the US, 7.1% had been diagnosed with anxiety and 3.2% had been diagnosed with depression.19,20 Thirteen percent of youth aged 12-17 years report having at least one major depressive episode in the past year.21 Research shows that cigarette smoking and dependence are strongly associated with higher depression and anxiety.22,23 Some evidence suggests that use of e-cigarettes is higher among people with psychiatric and substance use disorders.24,25 Individuals with higher levels of depression and anxiety are more likely to smoke cigarettes because of the need to self-medicate, as nicotine is believed to alleviate the symptoms of anxiety and depression.23 People with symptoms of poor mental health may be attracted to use e-cigarettes for similar reasons. In addition, higher impulsivity has also been associated with an increase in risky behaviors and undesirable outcomes. Impulsivity is a strong correlate of cigarette smoking.26-28 This is because higher impulsivity is an indicator of poor self-control.29
Currently, findings from studies examining the associations between anxiety, depression, and e-cigarette use have been mixed. Some studies have found significant positive associations between depressive symptoms and e-cigarette use,30,31 whereas others have not.22 This study tested the associations between depression, anxiety, and e-cigarette use and cigarette smoking among young adults in Hawai‘i. The study also examined impulsivity as a moderator of the association between mental health symptoms and cigarette and e-cigarette use. The hypotheses were: (1) higher depression and anxiety symptoms would be associated with higher cigarette smoking and e-cigarette use, and (2) the associations between depression and anxiety symptoms and cigarette smoking/e-cigarette use would be stronger among those who show higher impulsivity.
Methods
Procedures
This study was conducted in 2018-2020. The study protocol was approved by the University of Hawai.i (UH) Human Studies Program under CFR 46.110 and 21 CFR 56.110, Category (7) (CHS#23645). Students from two, 4-year and four, 2-year (community) colleges under the same university system in Hawai‘i were approached with the opportunity to participate in the study. To be eligible to participate in the study, participants had to be 18-25 years old and enrolled in a 2- or 4-year program within the UH system. E-mail addresses were obtained for all 18-25 year olds enrolled across the college campuses. A link to the screener survey was e-mailed to 7000 randomly selected e-mail addresses, inviting potential participants to participate in the study, which was described in generic terms, as a study on marketing and young adult health behavior. The screener survey included questions on age, sex, tobacco, alcohol, and dietary behaviors. In addition, the survey collected potential participants’ basic contact information such as phone number and university e-mail address. Of 7000 students invited to complete the screener survey, 60% completed the screener survey at baseline.
However, respondents to the e-mail invitation were predominantly women, never cigarette smokers. To increase the proportion of men in the sample and for adequate representation of cigarette smokers and experimenters in the sample (relative to nationally representative samples of 18-25 year olds), classroom-based recruitment was conducted. Participants were approached in the classroom with the assumption that more men and cigarette smokers would complete the screener survey. Since students are a captive audience in the classrooms, they are more likely to pay attention to the invitation to participate in a research study if the opportunity to do so is presented face-to-face by research staff.
For classroom-based recruitment, approximately 40 classes from each participating campus were randomly selected, and instructors of those classes were approached with requests for a classroom visit. On average, 25% of the instructors who were approached (approximately 10 classes per college) either did not respond to the research team’s request or actively denied participation. Hence, the research staff visited about 30 classrooms per college and presented the study and the opportunity to participate in the study to the students. Interested students (total 2700) completed the paper-and-pencil version of the screener survey. Participants provided consent either online or on paper before completing the screener survey.
Initially, the only eligibility criterion for participation was age: participants had to be 18-25 years old. However, as recruitment progressed and a higher percentage of females than males enrolled in the study, eligibility criteria was adjusted to ensure a more balanced men to women ratio. Similarly, once the predetermined percentage of non-cigarette smokers was fulfilled in the sample, eligibility criteria were adjusted to exclude further enrollment of nonsmokers going forward, in order to ensure that cigarette smokers were adequately represented in the sample. Of the students who completed the screener survey, either online or in the classroom, 3,664 students were eligible to participate in the study. Research staff explained the follow up survey procedure to the participants in person or by telephone. Participants were first e-mailed a link to the online consent form. After participants indicated their consent to participate in the study by clicking the “I agree to participate” button, they were sent unique links to the survey via e-mail. Of these, informed consent was obtained from 2,884 (79%) potential participants; the remainder could not be reached for consent procedure. A total of 2,622 participants completed the survey. The survey was programmed on Inquisit 4.0 computer software (Millisecond Software, Seattle, WA, 2015). No incentive was provided to complete the screener survey. Participants who completed the main survey received a $40 Amazon gift card.
Measures
Demographic Variables
Demographic variables assessed included age, sex, ethnicity, and annual household income. Age and sex were assessed both in the screener survey and the main study survey. Age, sex, and household income were assessed with single items. To determine ethnicity, participants were asked, “What is your ethnic background?” and were provided with a list of ethnicities common in Hawaii and the US. The question was asked in two different ways. The first question asked participants to refer to the list and “check all that apply.” The second question asked participants to choose the ethnic background that they identify with most. The response to the second question was utilized to assign mixed-ethnicity individuals to a particular racial/ethnic category. These items have been used successfully in past research.8
E-Cigarette and Cigarette Use
Cigarette smoking was assessed in the screener survey and the main survey. E-cigarette use was assessed only in the main survey. As in most national surveys,4,32 current e-cigarette use and cigarette smoking were assessed in terms of past-30-day use. For example, “During the last 30 days (1 month), on how many days did you use an electronic cigarette (e-cigarette) or a similar vaping device?” (8-point scale: “0 days,” “1-2 days,” “3-5 days,” up to “All days”). For logistic regression analyses, the variables were dichotomized to use (1) vs non-use (0). In addition, different patterns of e-cigarette and cigarette use, namely cigarette-only smoking, e-cigarette-only use, dual use of cigarette and e-cigarette, and use of neither product were also compared (see Table 1).
Table 1.
Demographic Characteristics of the Entire Sample and by Smoking and E-cigarette Use Status
| Variables | Entire sample (N = 2,622, 100%) | No smoking/No e-cigarette use (n=1,750, 67.9%) | E-cigarette use only (n=324, 12.6%) | Cigarette smoking only (n=233, 9.0%) | Dual use of e-cigarette and cigarette (n=271, 10.5%) | P value |
|---|---|---|---|---|---|---|
| Age: yrs (SD) | 21.2 + (2.2) | 21.0 + 0.05 | 20.9 + 0.12 | 22.4 + 0.14 | 21.6 + 0.13 | P <.001 |
| Sex | ||||||
| Female | 54.4% | 56.5% | 39.6% | 64.0% | 50.2% | P <.001 |
| Male | 45.6% | 43.5% | 60.4% | 36.1% | 49.8% | |
| Ethnicity | ||||||
| Asian | 26.0% | 27.3% | 23.2% | 18.0% | 26.2% | P <.001 |
| White | 24.3% | 24.1% | 18.2% | 35.6% | 24.4% | |
| NHPI | 21.2% | 19.9% | 24.4% | 22.3% | 24.0% | |
| Filipino | 17.9% | 17.5% | 24.7% | 11.6% | 18.5% | |
| Other | 10.6% | 11.2% | 9.6% | 12.5% | 7.0% | |
| Annual Household Income | ||||||
| Low (<$60K/yr) | 40.1% | 39.6% | 42.9% | 41.9% | 40.3% | P =.126 |
| Medium ($60 000-$99 999) | 29.0% | 29.2% | 29.8% | 21.8% | 31.7% | |
| High (>$100K/yr) | 30.9% | 31.3% | 27.3% | 36.2% | 28.0% | |
| Depressive Symptoms | 38.5% | 37.8% | 41.4% | 57.0% | 58.0% | P <.001 |
| Anxiety Symptoms | 25.5% | 23.2% | 22.7% | 35.6% | 37.2% | P <.001 |
| High Impulsivity | 52.6% | 48.6% | 54.6% | 61.2% | 69.7% | P <.001 |
SD = standard deviation, NHPI = Native Hawaiian or Pacific Islander
Mental Health Symptoms
Depression was assessed using the Center for Epidemiological Studies Depression (CES-D) scale,33 which asks 20 questions about feelings in the past week. Each question was scored from 0 to 3, and the scores were added with a total range from 0 to 60. A previously defined cut-point ≥16 was used for presence of depressive symptoms.34,35 Anxiety symptoms were defined using the Generalized Anxiety Disorder 7-item (GAD-7) scale,36 which asked 7 questions about feelings in the past 2 weeks. Each question was scored from 0 to 3, and the scores were added with a total range from 0 to 21. A previously defined cut-point ≥ 10 was used for presence of anxiety symptoms.36
Impulsivity
Impulsivity was defined using a modified version of the Kendall Wilcox Impulsivity Scale for Children (Self-Control Rating Scale),37 which asked 7 questions about impulsivity, each rated on a 5-point scale (1=never, 2=a little, 3=sometimes, 4=pretty often, 5=usually), for a sum score ranging from 5 to 35. High impulsivity was defined using a cut-point ≥ 10 based on median score.
Data Analysis
Data were analyzed using SAS software, version 9.2 (SAS Institute Inc., Cary, NC).38 General Linear Models (GLM) and chi-square tests were used to compare means and proportions of variables across the 4 smoking/e-cigarette use categories: “no use,” “cigarette-only use,” “e-cigarette-only use,” and “dual use.” GLMs were also used to examine the associations between 4 smoking categories and depressive symptoms, anxiety symptoms and impulsivity after adjusting for demographic variables such as age, sex, ethnicity, and family/household income. Logistic regression was used to test the associations between depression, anxiety, impulsivity and cigarette and e-cigarette use. The logistic regression models adjusted for demographic covariates (age, sex, ethnicity, and family/household income) and cigarette smoking or e-cigarette use, depending on the outcome (ie, cigarette smoking for e-cigarette use outcome and vice-versa). Interaction effects of impulsivity on the associations between the mental health symptoms and cigarette and e-cigarette use were tested using GLMs as well. All continuous variables used in the regression analysis were standardized, centering the mean at zero. After standardization, Depression X Impulsivity and Anxiety X Impulsivity interaction terms were created. Next, the interaction terms were entered as independent variables along with depression/anxiety, impulsivity, and demographic covariates, with cigarette/e-cigarette use as the dependent variable.
Results
Participants
Table 1 shows participants’ (N = 2622) characteristics. The mean age of the participants was 21.2 (SD = 2.2). There were 1423 females and 1194 males who completed the survey. Ethnically, participants included 26% Asians, 24% Whites, 21% Native Hawaiian and Pacific Islanders (NHPI), 18% Filipinos and 11% Other ethnicities. Overall, women were slightly more represented than men (55% vs 45%). Forty-three percent of the students were enrolled in 2-year or community colleges. Almost half of the participants were Asian or Pacific Islanders.
Table 1 shows differences between demographic and mental health variables across the following groups: no use, cigarette-only use, e-cigarette-only use, and dual use. No use of either e-cigarettes or cigarettes was reported in 68% of the sample, while 13% reported use of e-cigarette only, 9% reported use of cigarette only, and 11% reported use of both. Cigarette-only smokers were slightly older than other groups (P <.001). E.cigarette-only users were more likely to be men and cigarette-only smokers were more likely to be women, compared to other groups (P <.001). Household income was significantly different across the 4 categories.
After adjusting for age, sex, ethnicity and annual household income, multivariable analyses found significant stepwise associations between the 4 smoking categories and depressive symptoms (P <.001), anxiety symptoms (P <.001) and high impulsivity (P <.001) (see Figure 1). After stratifying into low and high impulsivity groups, the associations between depressive and anxiety symptoms and the 4 categories were stronger in the high impulsivity group (see Figure 2).
Figure 1.
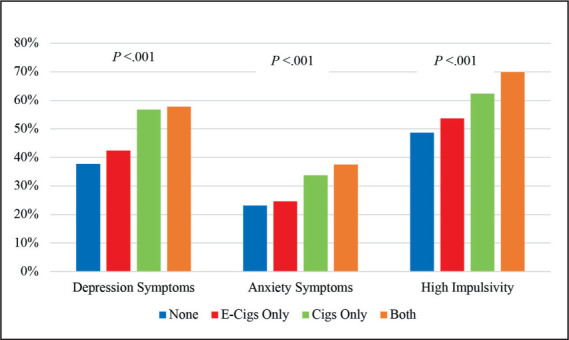
Adjusted Depression, Anxiety, and High Impulsivity by Tobacco Product Usea
a Adjusted for age, sex, ethnicity, and annual household income.
Figure 2.
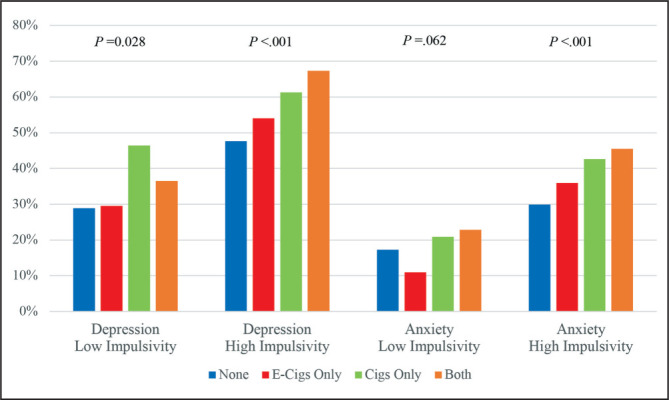
Adjusted Depression and Anxiety Symptoms by Tobacco Product Use Categories, Stratified by Impulsivitya
a Adjusted for age, sex, ethnicity, and annual household income.
Table 2 shows the results of the logistic regression analysis. There were statistically significant associations found between depression, anxiety, impulsivity and cigarette and e-cigarette use, after adjusting for demographic covariates. The associations of depression, anxiety, and impulsivity with cigarette use were stronger than with e-cigarette use. For example, a unit increase in depressive symptoms increased the odds of past-30-day cigarette smoking by 2.29 times compared with 1.34 times for past-30-day for e-cigarette use.
Table 2.
Associations Between Depression, Anxiety, Impulsivity and Current Cigarette and E-cigarette Use (N = 2622)
| Cigarette smoking | E-cigarette use | |
|---|---|---|
| Adjusted Odds Ratio [95% Confidence Interval] | ||
| Depressive Symptoms | 2.29 (1.92-2.72) | 1.34 (1.14-1.56) |
| Anxiety Symptoms | 1.57 (1.39-1.78) | 1.17 (1.05-1.31) |
| Impulsivity | 1.51 (1.35-1.70) | 1.38 (1.25-1.53) |
Note. The regression models adjusted for age, sex, ethnicity, annual household income, and cigarette smoking or e-cigarette use (depending on the outcome variable).
Table 3 shows the results of the interaction analysis. No statistically significant interaction effects of impulsivity on the associations between depression, anxiety, and past-30-day e.cigarette use were found. In addition, impulsivity was not found to moderate the effects of depression on past-30-day cigarette use. However, impulsivity was found to moderate the effects of anxiety on past-30-day cigarette smoking, such that the association between anxiety and cigarette smoking was stronger for those with higher impulsivity.
Table 3.
Interaction Effects of Impulsivity in the Association Between Depression, Anxiety, and Current Cigarette and E-cigarette Use (N = 2622)
| Cigarette | E-cigarette | ||
|---|---|---|---|
| B (SE) | |||
| Model 1 | |||
| Depression | 0.23 (0.04)*** | 0.08 (0.04)* | |
| Impulsivity | 0.15 (0.03)*** | 0.13(0.04)*** | |
| Depression X Impulsivity | 0.04 (0.03) | 0.05 (0.03) | |
| Model 2 | |||
| Anxiety | 0.16 (0.04)*** | 0.04 (0.04) | |
| Impulsivity | 0.17 (0.03)*** | 0.15 (0.04)*** | |
| Anxiety X Impulsivity | 0.06 (0.03)* | 0.04 (0.03) | |
Note.
P = .05
P < .01
P <.001
The regression models adjusted for age, sex, ethnicity, annual household income, and cigarette smoking or e-cigarette use (depending on the outcome variable).
Discussion
The current findings are somewhat consistent with the existing literature. For example, a study among high school students found psychiatric co-morbidities among both cigarette-only and e-cigarette-only users.39 Similarly, the French Constances cohort study found that depressive symptoms were associated with e-cigarette use in both cross-sectional and longitudinal analyses with a dose-dependent relationship.31 A large study of 2460 adolescents (mean age at baseline 14.1 years), who had never previously used cigarettes or e-cigarettes found a bi-directional association between depressive symptoms and e.cigarette use. Those with higher depressive symptoms at baseline were more likely to start using cigarettes, e-cigarettes or both a year later. In addition, increase in depressive symptoms was associated with sustained use of e-cigarettes over 12 months’ time.40 However, another study of 5445 college students in Texas found that depressive symptoms predicted subsequent e-cigarette use, but e-cigarette use did not predict later increased depressive symptoms.30 There are potential mechanisms to explain our findings. Nicotine use is believed to help cope with symptoms of depression and anxiety, and people with mental health conditions may choose to use nicotine for this reason. Higher impulsivity is an indicator of poor self-control and is associated with nicotine use behavior.29
The current study has many strengths. It was a large study and included use of both e-cigarettes and cigarettes among college students. The study included several ethnic groups that were representative of Hawai‘i. Validated scales were used to measure depressive symptoms, anxiety symptoms, and impulsivity. Limitations of the current study are that the study is cross-sectional in design, so causal conclusions cannot be formed based on the statistically significant associations detected in the current data. Second, smoking behavior may be misclassified, because it was only documented over the past 30 days. Third, the study did not have access to longitudinal data about the negative effects on health of e-cigarette use or cigarette smoking. Finally, data were self-reported and were not verified against objective measures.
Future directions include a longitudinal replication of the current findings. Also needed are prospective studies on the negative outcomes of e-cigarette and cigarette use, especially among those with mental health symptoms. Currently, not much has been done in terms of e-cigarette use prevention. There is a need for e-cigarette use prevention programs and such programs need to address poor mental health symptoms. School-based smoking prevention programs have played a key role in reducing cigarette smoking prevalence among young people in the US over the past several decades.41 The current data suggest that any school-based prevention program designed to address e-cigarette use may need to also address poor mental health symptoms. Our study suggests that smoking prevention education should target children and young adults, particularly those with high impulsivity scores.

Kelly Masaki
Acknowledgments
The first author (KM) would like to acknowledge the encouragement and help of Mr. Jay Hamura, science teacher at St. Andrew’s Priory School, and her mentor Dr. Pokhrel and all the staff at the University of Hawai‘i Cancer Center, that culminated in the completion of the current project. The current study was supported by funds from the National Cancer Institute (R01202277; R01228905).
Biography
Kelly Masaki is a 2020 graduate of St. Andrew’s Priory School. She did this project during her Summer Internship in 2019 at the University of Hawai‘i Cancer Center under the mentorship of Dr. Pallav Pokhrel. She is now a student at Santa Clara University’s School of Engineering studying Computer Science and Engineering.
Conflict of Interest
None of the authors identify a conflict of interest.
References
- 1.Park-Lee E, Ren C, Sawdey MD, et al. Notes from the field: e-cigarette use among middle and high school students - National Youth Tobacco Survey, United States, 2021. MMWR Morb Mortal Wkly Rep. 2021;70((39)):1387–1389. doi: 10.15585/mmwr.mm7039a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services The health consequences of smoking—50 years of progress. Centers for Disease Control and Prevention (CDC) Accessed October 17, 2020. https://www.cdc.gov/tobacco/data_statistics/sgr/50th-anniversary/index.htm.
- 3.Hartmann-Boyce J, McRobbie H, Lindson N, et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2020;10((10)):Cd010216. doi: 10.1002/14651858.CD010216.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Hawaii Behavioral Risk Factor Surveillance System (BRFSS) 2020. Accessed May 6, 2021. https://health.hawaii.gov/brfss/
- 5.Tobacco use in Hawaii 2018 Truth Initiative website. Accessed July 27, 2019. https://truthinitiative.org/research-resources/smoking-region/tobacco-use-hawaii-2018.
- 6.Wang TW, Neff LJ, Park-Lee E, Ren C, Cullen KA, King BA. E-cigarette Use Among Middle and High School Students - United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69((37)):1310–1312. doi: 10.15585/mmwr.mm6937e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smoking and Tobacco Use: Youth and Tobacco Use Centers for Disease Control and Prevention (CDC) website. Accessed July 27, 2019. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/youth_data/tobacco_use/index.htm.
- 8.Pokhrel P, Lam TH, Pagano I, Kawamoto CT, Herzog TA. Young adult e-cigarette use outcome expectancies: Validity of a revised scale and a short scale. Addict Behav. 2018;78:193–199. doi: 10.1016/j.addbeh.2017.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pokhrel P, Herzog TA, Muranaka N, Fagan P. Young adult e-cigarette users’ reasons for liking and not liking e-cigarettes: A qualitative study. Psychol Health. 2015;30((12)):1450–69. doi: 10.1080/08870446.2015.1061129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schweitzer RJ, Wills TA, Tam E, Pagano I, Choi K. E-cigarette use and asthma in a multiethnic sample of adolescents. Prev Med. 2017;105:226–231. doi: 10.1016/j.ypmed.2017.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rowell TR, Tarran R. Will chronic e-cigarette use cause lung disease? Am J Physiol Lung Cell Mol Physiol. 2015;309((12)):L1398–L1409. doi: 10.1152/ajplung.00272.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen IL, Todd I, Fairclough LC. Immunological and pathological effects of electronic cigarettes. Basic Clin Pharmacol Toxicol. 2019;125((3)):237–252. doi: 10.1111/bcpt.13225. [DOI] [PubMed] [Google Scholar]
- 13.Reidel B, Radicioni G, Clapp PW, et al. E-Cigarette Use Causes a Unique Immune Response in the Lung, Involving Increased Neutrophilic Activation and Altered Mucin Secretion. Am J Respir Crit Care Med. 2018;197((4)):492–501. doi: 10.1164/rccm.201708-1590OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang G, Wang Z, Zhang K, et al. Safety Assessment of Electronic Cigarettes and Their Relationship with Cardiovascular Disease. Int J Environ Res Public Health. 2018;15((1)):75. doi: 10.3390/ijerph15010075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meo SA, Ansary MA, Barayan FR, et al. Electronic Cigarettes: Impact on Lung Function and Fractional Exhaled Nitric Oxide Among Healthy Adults. Am J Mens Health. 2019;13((1)) doi: 10.1177/1557988318806073. 1557988318806073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Avino P, Scungio M, Stabile L, Cortellessa G, Buonanno G, Manigrasso M. Second-hand aerosol from tobacco and electronic cigarettes: Evaluation of the smoker emission rates and doses and lung cancer risk of passive smokers and vapers. Sci Total Environ. 2018;642:137–147. doi: 10.1016/j.scitotenv.2018.06.059. [DOI] [PubMed] [Google Scholar]
- 17.Moritz ED, Zapata LB,, Lekiachvili A, et al. Update: Characteristics of Patients in a National Outbreak of E-cigarette, or Vaping, Product Use-Associated Lung Injuries - United States, October 2019. MMWR Morb Mortal Wkly Rep. 2019;68((43)):985–989. doi: 10.15585/mmwr.mm6843e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siegel DA, Jatlaoui TC, Koumans EH, et al. Update: Interim Guidance for Health Care Providers Evaluating and Caring for Patients with Suspected E-cigarette, or Vaping, Product Use Associated Lung Injury - United States, October 2019. MMWR Morb Mortal Wkly Rep. 2019;68((41)):919–927. doi: 10.15585/mmwr.mm6841e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Children’s Mental Health – Anxiety and depression in children: Get the facts Centers for Disease Control and Prevention (CDC) website. Accessed October 17, 2020. https://www.cdc.gov/childrensmentalhealth/features/anxiety-depression-children.htmlhttps://www.cdc.gov/childrensmentalhealth/features/anxiety-depression-children.html.
- 20.Ghandour RM, Sherman LJ, Vladutiu CJ, et al. Prevalence and Treatment of Depression, Anxiety, and Conduct Problems in U.S. Children. J Pediatr. 2019;206:256–67. doi: 10.1016/j.jpeds.2018.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.2020 Mental Health in America – Youth Data MHA: Mental Health America website. Accessed October 17, 2020. https://mhanational.org/issues/2020/mental-health-america-youth-data#twohttps://mhanational.org/issues/2020/mental-health-america-youth-data#two.
- 22.Bierhoff J, Haardörfer R, Windle M, Berg CJ. Psychological Risk Factors for Alcohol, Cannabis, and Various Tobacco Use among Young Adults: A Longitudinal Analysis. Subst Use Misuse. 2019;54((8)):1365–1375. doi: 10.1080/10826084.2019.1581220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tidey JW, Miller ME. Smoking cessation and reduction in people with chronic mental illness. BMJ. 2015;351:h4065. doi: 10.1136/bmj.h4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hefner KR, Sollazzo A, Mullaney S, Coker KL, Sofuoglu M. E-cigarettes, alcohol use, and mental health: Use and perceptions of e-cigarettes among college students, by alcohol use and mental health status. Addict Behav. 2019;91:12–20. doi: 10.1016/j.addbeh.2018.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cummins SE, Zhu SH, Tedeschi GJ, Gamst AC, Myers MG. Use of e-cigarettes by individuals with mental health conditions. Tob Control. 2014;23((Suppl 3)):iii48–53. doi: 10.1136/tobaccocontrol-2013-051511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bourque J, Mendrek A, Dinh-Williams L, Potvin S. Neural circuitry of impulsivity in a cigarette craving paradigm. Front Psychiatry. 2013;4:67. doi: 10.3389/fpsyt.2013.00067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grant JE, Lust K, Fridberg DJ, King AC, Chamberlain SR. E-Cigarette Use (Vaping) is Associated with Illicit Drug Use, Mental Health Problems, and Impulsivity in University Students. Ann Clin Psychiatry. 2019;31((1)):27–35. [PMC free article] [PubMed] [Google Scholar]
- 28.Soneji S, Barrington-Trimis JL, Wills TA, et al. Association Between Initial Use of e-Cigarettes and Subsequent Cigarette Smoking Among Adolescents and Young Adults: A Systematic Review and Meta-analysis. JAMA Pediatr. 2017;171((8)):788–797. doi: 10.1001/jamapediatrics.2017.1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wills TA, Walker C, Mendoza D, Ainette MG. Behavioral and emotional self-control: relations to substance use in samples of middle and high school students. Psychol Addict Behav. 2006;20((3)):265–78. doi: 10.1037/0893-164X.20.3.265. [DOI] [PubMed] [Google Scholar]
- 30.Bandiera FC, Loukas A, Li X, Wilkinson AV, Perry CL. Depressive Symptoms Predict Current E-Cigarette Use Among College Students in Texas. Nicotine Tob Res. 2017;19((9)):1102–1106. doi: 10.1093/ntr/ntx014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wiernik E, Airagnes G, Lequy E, et al. Electronic cigarette use is associated with depressive symptoms among smokers and former smokers: Cross-sectional and longitudinal findings from the Constances cohort. Addict Behav. 2019;90:85–91. doi: 10.1016/j.addbeh.2018.10.021. [DOI] [PubMed] [Google Scholar]
- 32.The Centers for Disease Control and Prevention (CDC) Youth Risk Behavior Surveillance System (YRBSS) Accessed May 6, 2021. https://www.cdc.gov/healthyyouth/data/yrbs/index.htm.
- 33.Radloff LS. The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurements. 1977;(1)(1):385–401. [Google Scholar]
- 34.Vilagut G, Forero CG, Barbaglia G, Alonso J. Screening for Depression in the General Population with the Center for Epidemiologic Studies Depression (CES-D): A Systematic Review with Meta-Analysis. PLoS One. 2016;11((5)):e0155431. doi: 10.1371/journal.pone.0155431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106((3)):203–14. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- 36.pitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166((10)):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 37.Kendall PC, Wilcox LE. Self-control in children: Development of a rating scale. Journal of Consulting and Clinical Psychology. 1979;47((6)):1020–1029. doi: 10.1037//0022-006x.47.6.1020. [DOI] [PubMed] [Google Scholar]
- 38.SAS software . Cary, NC, USA: SAS Institute Inc; Version 9.4, of the SAS system for Windows. [Google Scholar]
- 39.Leventhal AM, Strong DR, Sussman S, et al. Psychiatric comorbidity in Adolescent Electronic and Conventional Cigarette Use. J Psychiatr Res. 2016;73:71–78. doi: 10.1016/j.jpsychires.2015.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lechner WV, Janssen T, Kahler CW, Audrain-McGovern J, Leventhal AM. Bi-directional associations of electronic and combustible cigarette use onset patterns with depressive symptoms in adolescents. Prev Med. 2017;96:73–78. doi: 10.1016/j.ypmed.2016.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lantz PM, Jacobson PD, Warner KE, et al. Investing in youth tobacco control: a review of smoking prevention and control strategies. Tob Control. 2000;9((1)):47–63. doi: 10.1136/tc.9.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]


