Abstract
Breast cancer is the second most reported cancer in women with high mortality causing millions of cancer-related deaths annually. Early detection of breast cancer intensifies the struggle towards discovering, developing, and optimizing diagnostic biomarkers that can improve its prognosis and therapeutic outcomes. Breast cancer-associated biomarkers comprise macromolecules, such as nucleic acid (DNA/RNA), proteins, and intact cells. Advancements in molecular technologies have identified all types of biomarkers that are exclusively studied for diagnostic, prognostic, drug resistance, and therapeutic implications. Identifying biomarkers may solve the problem of drug resistance which is a challenging obstacle in breast cancer treatment. Dysregulation of non-coding RNAs including circular RNAs (circRNAs) and microRNAs (miRNAs) initiates and progresses breast cancer. The circulating multiple miRNA profiles promise better diagnostic and prognostic performance and sensitivity than individual miRNAs. The high stability and existence of circRNAs in body fluids make them a promising new diagnostic biomarker. Many therapeutic-based novels targeting agents have been identified, including ESR1 mutation (DNA mutations), Oligonucleotide analogs and antagonists (miRNA), poly (ADP-ribose) polymerase (PARP) in BRCA mutations, CDK4/6 (cell cycle regulating factor initiates tumor progression), Androgen receptor (a steroid hormone receptor), that have entered clinical validation procedure. In this review, we summarize the role of novel breast cancer diagnostic biomarkers, drug resistance, and therapeutic implications for breast cancer.
Keywords: diagnostic biomarkers, circular RNAs, miRNAs, drug resistance, breast cancer
1 Introduction
Breast cancer is a kind of cancer that affects mostly females and is a primary factor of mortality worldwide (Wu and Chu, 2021). It is a heterogeneous disease with six distinct molecular subtypes: luminal A (progesterone receptors (PR)+, estrogen receptor (ER)+, Human epidermal growth factor receptor 2 (HER2)-, and Ki67), luminal B (ER+, HER+/−, and Ki67+), human epidermal growth receptor 2(HER2)+, basal-like subtype (ER-, PR- and HER2−) normal breast like and claudin low type (where low expression of cellular adhesion genes can be detected) (Perou et al., 2000). Breast cancer initial detection and monitoring are two significant treatments that enhance therapy results and provide patients with a positive prognosis (Pace and Keating, 2014). Mammography is a common approach for identifying breast cancer, although it has several drawbacks, such as a low sensitivity of 25%–59% for cancer detection in younger females with dense breasts. It has also recorded erroneous negative and positive findings, as well as a 1%–10% over detection rates (Bleyer and Welch, 2012; Oeffinger et al., 2015).
Biomarkers that aid in the diagnosis, prognosis, and prediction of breast cancer are essential for timely identification and appropriate control of the disease throughout treatment (Hayes et al., 2001; Weigel and Dowsett, 2010). Moreover, an increasing percentage of patients are demanding personalized or unique treatments, demanding the development of novel biomarkers for diagnostic and prognostic procedures as well as intact cells, are utilized as biomarkers in the diagnosis of cancer. Artificial intelligence technologies like machine learning have the potential to greatly enhance the existing anti-cancer medication development process. Constituents produced by cancer-affected cells or various tissues in reaction to tumors, and also physiological indicators that may be recognized by diagnostics or molecular technology, are all examples of cancer biomarkers (Loke and Lee, 2018; Voith von Voithenberg et al., 2019). Biomarkers may be used to assess the biological condition of a disorder, which can then be used to identify the type of the tumor, its progression, or therapy responses, assisting in the control of breast cancer (Wu and Chu, 2021). Because tumor cells are so heterogeneous, a singular biomarker is insufficiently sensitive or precise to effectively diagnose cancer growth and metastasis, hence a combination of biomarkers is preferred. Significant advances in genetic fingerprints and molecular signaling processes have found a variety of biomarkers in tissues and blood (liquid biopsies) that may be used to predict the likelihood of cancer spread, resurgence, therapy recommendations, prediction, and medication tolerance. Some of these biomarkers have been utilized in clinical trials, however, their sensitivity and selectivity are zero (Nalejska et al., 2014; Wu and Chu, 2021). As a result, novel and more effective biomarkers are required. Moreover, several therapeutic approaches for breast cancer are still in their early phases of development, therefore, it is vital to find precise biomarkers that may be used to help with immunotherapies (Wu and Chu, 2021).
2 Types of Biomarkers
Larger molecules such as nucleic acids, genetic alterations, and protein molecules, as well as intact cells, are utilized as biomarkers in the diagnosis of cancer. They can be observed in blood in the form of circulating tumor cells, DNA, and RNA enabling liquid biopsies a useful clinical technique (Eccles et al., 2013; Berghuis et al., 2017; Voith von Voithenberg et al., 2019). Prognostic and predictive biomarkers are two categories of biomarkers linked to likely clinical results and therapy success in breast cancer subtypes (Fine and Pencina, 2015; Janes et al., 2015; Simon, 2015).
3 Role of Macromolecules in Breast Cancer Diagnosis
3.1 DNA
Alteration in DNA methylation is one of the major significant molecular changes in carcinogenesis. Adenomatous polyposis coli (APC) and retinoic acid receptors-2 (RARb2) methylated promoters were discovered in 93.4% and 95.6% of blood samples from females having breast cancer, respectively, but not in healthy people (Swellam et al., 2015). All methylation variations surpassed the conventional markers CEA and CA 15–3 in detecting early breast cancer, low-grade tumors, and Triple Negative Breast Cancer (NBC). Utilizing a human methylation DNA study BeadChip. Yang et al. revealed that hypomethylation of S100 calcium-binding protein P (S100P) and hyalurono glucosaminidase 2 (HYAL2) in the peripheral blood is linked with breast cancer (Yang et al., 2015; Yang et al., 2017). Both genes with lower methylation have been proven to be possible biomarkers circulating in blood, for the diagnosis of breast cancer, specifically in adolescent girls in the initial stages (Bleyer and Welch, 2012; Fleming and Powers, 2012).
The latest study has found that aberrant DNA methylation is significantly linked to breast cancer, and suggesting that DNA methylation testing can aid in predicting the prognosis of breast cancer patients. MAST1, PRDM14, and ZNF177 irregular DNA methylation variants were found and verified as prospective breast cancer molecular indicators by X Mao et al. X Mao et al. also showed that the DNA methylation range of ADCY4, CPXM1, DNM3, PRDM14, PRKCB, and ZNF177. In essence, these findings point to the development of novel epigenetic prognosis systems that might assist in the detection and prediction of breast cancer therapy (Uehiro et al., 2016). An exceptionally sensitive mobile cell-free DNA (cfDNA) system with epigenetic biomarkers and droplet digital methylation-specific PCR (ddMSP) has been created for the early diagnosis of breast cancer. Ras-specific guanine nucleotide-releasing factor 1 (RASGRF1), carboxypeptidase X (CPXM1), Hox-A10 (HOXA10), and Dachshund homolog 1 (DACH1) were the four methylation markers employed in the efficient screening method (Uehiro et al., 2016). This epigenetic-marker-based technique was able to reliably discriminate women with breast cancer from healthy controls, hinting that it might be utilized for breast cancer screening and therapy (Uehiro et al., 2016).
3.2 Proteins
Circulating protein has been considered as the second choice as a biological marker for the recognition and analysis of Breast cancer (BC). Blood proteomics and mass spectrometry have analyzed the systemic and comprehensive visualization of the blood proteomics pathologically and physiologically, resulting in the finding of numerous protein biomarkers in blood that can be used as effective diagnostic biomarkers in breast cancer detection. A panel of trefoil factor (TFF) 1, TFF2, and TFF3 have been stated as promising biomarkers for BC screening as they can express specific proteins differentially in the serum of BC patients that cannot be produced by healthy cells (Ishibashi et al., 2017). The two well-known groups such as Cks of intermediate filaments and glycoprotein (MUC) family can produce several classical breast cancer biomarkers. The CA 15–3 assay, for example, is currently used for tracking purposes in treatment (Duffy, 2006), while CKs have been proposed as early-stage BC markers, but their efficacy is masked due to poor sensitivity (Levenson, 2007). The serum epithelial membrane antigen/CK1 concentration ratio is recommended as possible diagnostic marker, especially for initial stage breast cancer diagnosis. The diagnostic capability of this new combination was assessed better than CA 15–3 (Attallah et al., 2014).
Besides, some other proteinaceous biological markers with promising diagnostic capability have been revealed by ELISA. Among these proteins, a single diagnostic marker model of pleiotrophin (PTN) (Ma et al., 2017a), and double diagnostic marker models such as integration of microRNA (miRNA) miR-127-3p with human epididymis secretory protein 4 (HE4) (Lu et al., 2017), human anterior gradient (AGR) 2 with AGR3 (Garczyk et al., 2015) and vascular endothelial growth factor (VEGF) with CA 15–3 (Ławicki et al., 2016). Serum apolipoprotein C-I (apoC-I) has demonstrated promise results in prognosis and diagnosis of triple-negative Breast cancer (TNBC), as it could distinguish TNBC from non-TNBC cases by greater ApoC-I mRNA and protein expression in the former when compared to both non-TNBC affected individuals and controls (Song et al., 2016).
3.3 Autoantibodies
Autoantibodies are reported as another approach used as diagnostic biomarkers with the potential of multiple targets, short time-frames, and minimalist hardware (Soler et al., 2016). The associated antigens of these antibodies are synthesized by the body’s cells; in healthy cells, it is expressed at a modest level, while it is overexpressed in malignant cells. The immune system determines this expression, using toll-like receptors (TLRs) for the innate response, thus reverting tumor growth. MUC1, an integral membrane protein, is overexpressed in 90% of adenocarcinomas and has been linked to tumor aggressiveness (Zaenker et al., 2016). Antibodies that target oncogenic and tumor suppressor proteins are considered as the significant diagnostic biomarkers for the efficient detection of breast cancer. The presence of autoantibodies before the medical diagnosis of the disorder in paraneoplastic syndrome and systemic autoimmune diseases has raised the prospect that the medical diagnosis of BC could also be carried out through detection of auto-immunoglobulins (Fernández Madrid, 2005). As a result, extensive research has revealed the detection of tumor-associated antigens by autoantibodies that were detected in the patient blood sample. The integration of modern proteomics, advanced genomics, high-throughput technology, and traditional immunological approaches has significantly aided advancement in this area (Fernández Madrid, 2005).
3.4 miRNA
miRNAs are single-stranded, non-coding, small (20–25 nucleotide) RNAs that suppress the post-transcriptional expression of specifically selected genes via mRNA breakdown or mRNA expression. The detection and persistence of miRNAs in the bloodstream and their role in diagnostic and therapeutic approaches have been studied thoroughly (Schwarzenbach et al., 2011). Since miRNAs are soluble and observable in cancer cells (Shen et al., 2013), blood, plasma, and patients’ saliva, they can be used as biological markers for non-invasive early diagnosis, detection, and treatment of breast cancer (Mitchell et al., 2008; Schwarzenbach et al., 2014). miRNAs are released into the bloodstream by apoptotic cells (Schwarzenbach et al., 2011). miRNAs can travel through the bloodstream in two forms: cell-free (Ago2-related) or embedded in membrane vesicles, microvesicles, or exosomes (Simpson et al., 2009). miRNAs profiling studies can classify dysregulated miRNAs and categorize patients of breast cancer for therapies, highlighting their potential to be used as a predictive and therapeutic biomarker (McGuire et al., 2015). Furthermore, like oncogenes (oncomiRNAs) and tumor suppressors, unregulated miRNA is responsible for tumor growth, development, cell death, invasion, and cell proliferation. Recently, numerous suspected candidates, for example, miR-221, miR-21, and miR-145, have appeared in the blood serum or plasma of BC-affected individuals. Blood-based identities containing miR-221 and/or miR-21 have been shown to have higher diagnostic susceptibility than CEA and CA 15–3 for all stages of cancer, distinguishing BC subjects from patients with benign tumors and healthy people and doing better in distinguishing the TNBC subtype from healthy subjects (Gao et al., 2013; Motawi et al., 2016; Thakur et al., 2016). Exosomal miR-21 expression has also been shown to be elevated in Breast cancer patients’ plasma-derived exosomes. The exosomal miR-21 and miR-1246 form modest diagnostic (Hannafon et al., 2016).
In terms of diagnosis, Iorio et al. (2005) discovered a 13-miRNA hallmark that could differentiate affected Breast cancer from healthy breast tissues with 100% precision. Blenkiron et al. (2007) discovered 133 miRNAs with abnormal expression patterns in breast tumor tissues irrespective of normal breast tissues. Despite the discovery of miRNAs with abnormal expression in BC tissues, there are still inconsistencies between the variously identified miRNA signatures. Roth et al. introduced single circulating miRNAs as diagnostic and prognostic instruments after discovering miR-155 in the serum of Breast cancer affected individuals but not in stable controls, and Heneghan et al. identified elevated miR-195 activity in the bloodstream of only affected subjects with BC (Heneghan et al., 2010; Roth et al., 2010). Some miRNAs, such as miR-21and miR-29a or 4-miRNA signature, have been found in the plasma of BC patients (miR-222, miR-16, miR-25, and miR-324-3p) (Wu et al., 2011; Hu et al., 2012).
A vast number of other miRNAs have been reported that overexpress in Breast cancer a few examples are miR-29a, miR-146a, miR-373, miR589, miR-221/222 cluster, miR-9, miR10b, miR-96, miR-181, miR-375, and miR-520c. These miRNAs are linked with treatment, diagnosis, and prognosis of Breast cancer (Polytarchou et al., 2012; Khoshnaw et al., 2013; Sandhu et al., 2014).
3.5 CircRNAs as Diagnostic/Prognostic Markers
Circular RNAs (circRNAs) are recently identified non-coding RNAs that are classified as tiny endogenous RNAs with a broad distribution, various forms, and several regulatory applications (Ashwal-Fluss et al., 2014). Sanger et al. (1976) were the first to find cricRNA in the viroids. Up till now, a large number of circRNAs have been found in various cell lines and organisms (Bleyer and Welch, 2012; Pace and Keating, 2014; Oeffinger et al., 2015), namely protozoa, fungi, worms, plants, fish, mice, insects, and humans (Wang et al., 2014; Westholm et al., 2014). CircRNAs are present in large numbers, about 1/8th of the human genome’s transcriptome can generate observable circRNAs, and their expression levels are much more than tenfold higher than that of the comparable linear mRNAs (Salzman et al., 2012; Jeck et al., 2013). Furthermore, as a result of their covalent closed-loop configuration and absence of free terminal ends, circRNAs are much more stable unlike linear RNAs, conferring susceptibility to deterioration by endonuclease R (RNase R) (Chen and Yang, 2015). CircRNAs can also be used to distinguish and recognize various tumor types due to their ability to express particular cell types, tissues, and developmental stages, as well as the fact that different subtypes of circRNAs can be generated (Salzman et al., 2013; Smid et al., 2019). Given the above, we conclude that circRNAs have growing research potential. Various biochemical roles of circRNAs have been discovered as science has progressed. CircRNAs may serve as “sponges” for microRNAs (miRNAs), influencing the role of miRNA target genes (Hansen et al., 2013). Furthermore, circRNAs can be attached to various RNA binding proteins (RBPs), influencing the role of the parental genes (Zeng et al., 2017; Kristensen et al., 2019). Surprisingly, provided evidence suggests that circRNAs may express proteins/peptides playing a role in tumor development and progression (Legnini et al., 2017; Zheng et al., 2019). CircRNAs’ special properties and biological roles show the role of circRNAs in tumor growth, replication, metastasis, invasion, and drug tolerance, implying that circRNAs can be used as biological markers and tumor therapeutic goals (Liu et al., 2018a; Kun-Peng et al., 2018). Circular RNAs can avoid exonuclease-induced degradation and are more soluble in blood or plasma than linear RNAs because of their closed continuous loop structure (Alhasan et al., 2016). It has been shown that ncRNAs, such as miRNAs and non-coding RNAs, can serve as reliable biological markers for hepatocellular carcinoma (Li et al., 2015). CircRNAs are regaining attention among researchers as high-throughput sequencing and bioinformatics technology improves. Due to their stability and tissue specificity, circRNAs have been established as suitable biological markers for the diagnosis of gastric cancer (Simon, 2015), hepatocellular carcinoma, and other cancers (Qin et al., 2016). Evidence have revealed that circRNAs can cause tumorigenesis, providing a new approach for identifying diagnostic biomarkers (Kulcheski et al., 2016; Zhu et al., 2017).
Using the circRNA microarray method, Lu et al. determined the circRNA expression pattern in breast cancer and normal tissues and discovered that hsa circ 103110, hsa circ 104689, and hsa circ 104821 levels were upregulated in breast cancer cells with area under the curve (AUC) value of 0.63 (0.52–0.74), 0.61 (0.50–0.73), and 0.60 (0.49–0.71) respectively, while hsa circ 006054, hsa circ 100219, and hsa circ 406697 were downregulated with the area under the curve (AUC) value of 0.71 (0.61–0.81), 0.78 (0.69–0.88) and 0.64 (0.52–0.75) respectively. As a result, mixing hsa circ 006054, hsa circ 100219, and hsa circ 406697 yielded successful diagnostic results as mentioned in table 1 (Lü et al., 2017). Similarly, Yin et al. found that in the plasma of breast cancer patients, 19 circRNAs were upregulated and 22 were downregulated as opposed to stable controls (Maselli et al., 2019). Further investigation found that the plasma hsa circ 0001785 had a higher diagnostic accuracy than CEA and CA15-3. Furthermore, hsa circ 0001785 plasma levels were correlated with histological grade (p = 0.013), TNM stage (p = 0.008), and remote metastasis (p = 0.016), indicating a possible biomarker for breast cancer diagnosis. The expression levels of hsa circ 0001785 were shown to be lower in post-operative BC patients’ plasma samples relative to pre-operative patients (Sarkar and Diermeier, 2021).
TABLE 1.
Regulation pattern of different circRNAs in cancer lesions.
| Regulation pattern | Types of CircRNAs | Value of area under the curve (AUC) |
|---|---|---|
| Upregulation in cancer lesions | hsa circ 103110 | 0.63 (0.52–0.74) |
| hsa circ 104689 | 0.61 (0.50–0.73) | |
| hsa circ 104821 | 0.60 (0.49–0.71) | |
| Downregulation in cancer lesions | hsa circ 006054 | 0.71 (0.61–0.81) |
| hsa circ 100219 | 0.78 (0.69–0.88) | |
| hsa circ 406697 | 0.64 (0.52–0.75) |
3.5.1 Limitations of Circulating miRNA as a Diagnostic Biomarker
The development of a precise and effective biomarker for breast cancer diagnostic approaches is challenging at every step ranging from sample collection to data processing (Witwer, 2015). For example, the low abundance of circulating miRNAs as diagnostic biomarker hinders their detection using microarray-based miRNA profiling techniques. Modified strategies can be adopted to reduce the limitations; such as miRNA isolation before expression profiling (Hamam et al., 2016). Another issue is sample collection which can be resolved by serum selection to avoid limitations of excluding a large number of samples. Because recent studies reported a high level of circulating miRNA in serum than in plasma (Wang, 2012). A recent study identified the fluctuations in circulating miRNA levels in response to chemotherapy. This drawback can be eliminated by collecting blood samples before chemotherapy (Diener et al., 2015).
3.6 Exosome
Exosomes are extracellular membrane-bound vesicles that are nano-sized (30–100 nm) and actively released by cancer cells and neighboring cells present in the tumor microenvironment (TME) (Taylor and Gercel-Taylor, 2013; Gajos-Michniewicz et al., 2014). They are surrounded by a lipid bilayer composed up of phosphoglycerides, ceramides, sphingolipids, and cholesterols (Vlassov et al., 2012) and comprise a diverse array of molecules such as DNA, sugars, proteins, peptides, lipids, mRNAs, miRNAs, as well as other types of ncRNAs (Moreno-Gonzalo et al., 2014). Exosomes like miRNAs, are present in a variety of human bodily fluids, including blood, sweat, urine, and breastfeeding (Vlassov et al., 2012; Raposo and Stoorvogel, 2013).
Exosomes can facilitate tumor development, angiogenesis, immunosuppression, and metastasis by promoting intermodulation between tumor cells and healthy or cancer-affected stromal cells (Alderton, 2012; Moon et al., 2016a). The surface proteins present on circulating extracellular vesicle (EVs), developmental endothelial locus-1 protein (Del-1) (Moon et al., 2016a), and fibronectin (Moon et al., 2016b), are promising materials for cancer detection. Fibronectin, a matrix protein present extracellularly, binds to several integrins and activates a variety of signaling proteins, including FAK, Src, and Akt (Moon et al., 2016b). Fibronectin levels rose dramatically (p < 0.0001) throughout all phases of breast cancer and went back to normal after the tumors were removed. The clinical diagnostic efficacy for fibronectin recognition outside the cellular vesicles was better than that in plasma (Moon et al., 2016b). This underscores the significance of extracellular matrix proteins in breast cancer. The high amount of Del-1 in patients’ circulating exosomes (p 0.0001) resulted in excellent diagnostic success in distinguishing patients with early-stage breast cancer from the control system (Moon et al., 2016a).
4 Role of Biomarkers in Drug Resistance
Chemotherapy treatment has a significant role in the prevention of breast cancer recurrence and spreading (Liu et al., 2018b). But the main problem of this method is Chemo-therapeutic resistance, hsa-circ 0006528 is upregulated in breast cancer cells resistant to Adriamycin resistant breast cancer (ADM), presumably by the circ. pathway. Axis of RNA/miR-7-5p/Raf1 (Guo et al., 2020). Low concentrations of miR-7 expression have long been associated with resistance to breast cancer chemotherapy. Another research of ADM-resistant breast cancer discovered that circKDM4C downregulation inhibited tumor proliferation and alleviated ADM resistance by controlling the miR-548p/PBLD axis (Ma et al., 2019; Yang et al., 2020).
Furthermore, the level of expression of circMTO1 (hsa circ 007874) in monastrol-resistant breast cancer cell lines is substantially lower than in monastrol-sensitive breast cancer cell lines, and uncontrolled expression of circMTO1 will reverse monastrol resistance through the circRNA/TNF receptor-associated factor 4 (TRAF4)/Eg5 pathway. Furthermore, Ma et al. discovered that circMOTL1, which could play an important role in breast cancer cell PTX resistance by controlling the AKT pathway, encouraging anti-apoptotic protein expression, and impeding pro-apoptotic protein synthesis, is found to be elevated in breast cancer (Greene et al., 2019). Yang et al. reported that in Breast cancer cells, the expression of circ-ABCB10 is increased. Through the let-7a-5p/DUSP7 axis, Circ-ABCB10 regulates PTX resistance, apoptosis, invasion, and autophagy in breast cancer cells (Wu et al., 2019).
The impact of Erα36 on the oncogenesis of breast and drug resistance was assessed by Pangano et al. (Yin et al., 2018). Tamoxifen, reported as anti-estrogen, has been shown to act as an agonist of ER36 to proliferate, invade, and metastasize breast cancer cells (Yin et al., 2018), which explains why many breast cancer patients develop drug resistance to anti-estrogens that block the signaling pathways mediated by ER36. A serum autoantibody was recently discovered that functions against ERα in a wide proportion of patients affected by breast cancer and was shown to cause ER36, leading to tamoxifen tolerance (Maselli et al., 2016; Maselli et al., 2019).
4.1 Role of miRNA
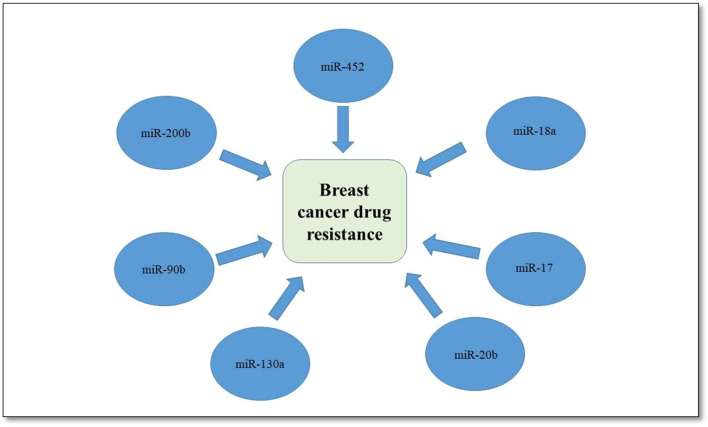
There are several miRNAs whose expressions were downregulated in drug resistance BC. In BC-affected tissues and cells resistant to taxol, the increased expression of nuclear receptor co-activator 3 (NCOA3) results in decreased expression of miR-17 and miR-20b. This shows that these three NCOA3, miR-17, and miR-20b may function as active biological markers and therapeutic targets in breast cancer resistance to taxol (Ao et al., 2016).
Another study reported the overexpression of miR-18a in TNBC cells patients who had received neoadjuvant paclitaxel, thus inhibiting dicer expression and increasing paclitaxel resistance in TNBC cells (Sha et al., 2016). There are four miRNAs; miR-90b, 130a, 200b, and 452 that can regulate drug-related cellular pathways, thus leading to chemoresistance as shown in Figure 1 (Jayaraj et al., 2019).
FIGURE 1.
Role of different miRNA in drug resistance.
4.2 Role of circRNAs
In adriamycin-resistant cell lines and tissues sensitive to Adriamycin, a high-level expression of hsa_circ_00006528 was discovered by Gao et al. (Ma et al., 2017b) by using circRNA microarray expression profiles. The hsa_circ_00006528-miR-7–5p-Raf1 axis has a regulatory effect on breast cancer resistance to adriamycin. This highlights the possibility of the use of hsa_circ_00006528 in controlling the factor of drug resistance. This concludes that for breast cancer treatment, circRNAs come up with novel and reliable therapeutic strategies (Ma et al., 2017b).
has-circ_00006428, a circular RNA, can be used as a promising therapeutic candidate due to its role in reducing drug resistance. This statement can be supported by its overexpression in Adriamycin-resistant cells while expression in Adriamycin-sensitive cells. Besides, the regulatory role of hsa_circ_00006528-miR-7-5p-Rafl axis in Adriamycin resistant breast cancer was revealed (Ma et al., 2017b).
5 Therapeutic Implications
5.1 CircRNAs as Therapeutic Targets in Breast Cancer
New progress in RNA-based therapies plus aberrant expression of circRNAs in breast cancer makes them more potential therapeutic sites (Lei et al., 2019). One solution may be to create synthetic circRNAs with several binding sites for certain oncogenic proteins or miRNAs that could be inserted exogenously to restore the natural regulatory network in the cell and reduce cancer development (Tay et al., 2015; Liu et al., 2018c). On the other hand, endogenous circRNAs can be useful for the treatment of cancer (Dragomir and Calin, 2018). Any of the tumor-suppressor circRNAs discussed above are prime candidates for further development as therapeutic instruments. CircFOXO3, circCCNB1, circKDM4C, circFBXW, and circTADA2A were all shown to be downregulated in patient samples, related to a bad diagnosis and treatment, and biologically linked to cancer etiology (Meganck et al., 2018). CircRNA overexpression constructs transferred by adeno-associated virus (AAV) vectors, which do not incorporate into the genome and are presently used in clinical studies, are recently used as a therapeutic solution. On another side, tumorigenic circRNAs, such as the TNBC-specific circAGFG1 and circANKS1B, may be used as new therapeutic targets for TNBC, which currently have few treatment choices and a weak prognosis (Bianchini et al., 2016). To target overexpressed circRNA expression therapeutically, effective approaches have been designed, including degradation mediated by siRNA, shRNA, or altered antisense oligonucleotides (ASOs) complementary to the back-splice junction (Cortés-López and Miura, 2016; Santer et al., 2019). More steady knockout methods, such as CRISPR/Cas genome editing, have also been evaluated. The CRISPR/Cas13 system is a new addition that achieves circRNA silencing by attacking Cas13 to the circRNA’s back-splice junction via a specific guide RNA that can differentiatedifferentiate between linear transcripts and circRNAs (Li et al., 2021). Cas13d, a small version of Cas13 (Konermann et al., 2018), in particular, may be packaged into an AAV vector for transmission into primary cells and rodents (Konermann et al., 2018; Zhang, 2021). However, since the side effects of Cas13 expression are currently uncertain, the drawbacks of this system in a clinical sense are not known (Li et al., 2021).
6 Homologous Recombination Deficiency in Breast Cancer Genes
Genomic mutations and instability are the attributions of human cancers that occur due to defective DNA repair mechanisms. One such DNA repair process is homologous recombination (HR), which facilitates the repair of double-strand breaks and interstrand cross-links (Li and Heyer, 2008). Mutations in BRCA1 and BRCA2 genes are centrally involved in homologous recombination (HR), DNA damage repair, and cell cycle checkpoint regulation (Joosse, 2012). About 5%–10% of breast cancers are associated with inherited mutations in BRCA1 and BRCA2 genes (Institute, 2013). A recent study reported the significance of germline mutations of BRCA1 and BRCA2 by determining their sensitivity to platinum-based chemotherapy and PARP inhibitors (Von Minckwitz, 2014). HRD-mutational signatures are clinically associated with platinum-based chemotherapy in the advanced–stage of breast cancer (Davies et al., 2017).
7 Conclusion
Breast cancer is the second mostly reported cancer in women showing a high mortality rate worldwide annually. Early diagnosis and prognosis can control its fatality rate up to some extent. No single biomarker is involved in its diagnosis but a group of multiple diagnostic biomarkers plays a key role in its detection, prognosis, and treatments. Several macromolecules are reported as the significant diagnostic biomarkers including circular RNA, miRNA, DNA, protein, exosomes, and antibodies. Identification of these macromolecules can help in the detection of cancer. DNA methylation and miRNA profiling are the prominent approaches through which breast cancer can be identified.
Author Contributions
SA conceived the idea of study. MH, SU, and HA wrote the manuscript. FT helped in data collection. MK and SA proofread the article. All authors approved the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Alderton G. K. (2012). Exosomes Drive Premetastatic Niche Formation. Nat. Rev. Cancer 12 (7), 447. 10.1038/nrc3304 [DOI] [PubMed] [Google Scholar]
- Alhasan A. A., Izuogu O. G., Al-Balool H. H., Steyn J. S., Evans A., Colzani M., et al. (2016). Circular RNA Enrichment in Platelets Is a Signature of Transcriptome Degradation. Blood J. Am. Soc. Hematol. 127 (9), e1–e11. 10.1182/blood-2015-06-649434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ao X., Nie P., Wu B., Xu W., Zhang T., Wang S., et al. (2016). Decreased Expression of microRNA-17 and microRNA-20b Promotes Breast Cancer Resistance to Taxol Therapy by Upregulation of NCOA3. Cell Death Dis 7 (11), e2463. 10.1038/cddis.2016.367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashwal-Fluss R., Meyer M., Pamudurti N. R., Ivanov A., Bartok O., Hanan M., et al. (2014). circRNA Biogenesis Competes with Pre-mRNA Splicing. Mol. Cel. 56 (1), 55–66. 10.1016/j.molcel.2014.08.019 [DOI] [PubMed] [Google Scholar]
- Attallah A. M., El-Far M., Omran M. M., Abdallah S. O., El-desouky M. A., El-Dosoky I., et al. (2014). Circulating Levels and Clinical Implications of Epithelial Membrane Antigen and Cytokeratin-1 in Women with Breast Cancer: Can Their Ratio Improve the Results. Tumor Biol. 35 (11), 10737–10745. 10.1007/s13277-014-2375-1 [DOI] [PubMed] [Google Scholar]
- Berghuis A., Koffijberg H., Prakash J., Terstappen L., IJzerman M. (2017). Detecting Blood-Based Biomarkers in Metastatic Breast Cancer: a Systematic Review of Their Current Status and Clinical Utility. Ijms 18 (2), 363. 10.3390/ijms18020363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bianchini G., Balko J. M., Mayer I. A., Sanders M. E., Gianni L. (2016). Triple-negative Breast Cancer: Challenges and Opportunities of a Heterogeneous Disease. Nat. Rev. Clin. Oncol. 13 (11), 674–690. 10.1038/nrclinonc.2016.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blenkiron C., Goldstein L. D., Thorne N. P., Spiteri I., Chin S. F., Dunning M. J., et al. (2007). MicroRNA Expression Profiling of Human Breast Cancer Identifies New Markers of Tumor Subtype. Genome Biol. 8 (10), R214–R216. 10.1186/gb-2007-8-10-r214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleyer A., Welch H. G. (2012). Effect of Three Decades of Screening Mammography on Breast-Cancer Incidence. N. Engl. J. Med. 367 (21), 1998–2005. 10.1056/nejmoa1206809 [DOI] [PubMed] [Google Scholar]
- Chen L.-L., Yang L. (2015). Regulation of circRNA Biogenesis. RNA Biol. 12 (4), 381–388. 10.1080/15476286.2015.1020271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortés-López M., Miura P. (2016). Focus: Epigenetics: Emerging Functions of Circular RNAs. Yale J. Biol. Med. 89 (4), 527. [PMC free article] [PubMed] [Google Scholar]
- Davies H., Glodzik D., Morganella S., Yates L. R., Staaf J., Zou X., et al. (2017). HRDetect Is a Predictor of BRCA1 and BRCA2 Deficiency Based on Mutational Signatures. Nat. Med. 23 (4), 517–525. 10.1038/nm.4292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener Y., Walenda T., Jost E., Brümmendorf T. H., Bosio A., Wagner W., et al. (2015). MicroRNA Expression Profiles of Serum from Patients before and after Chemotherapy. Genomics data 6, 125–127. 10.1016/j.gdata.2015.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragomir M., Calin G. A. (2018). Circular RNAs in Cancer - Lessons Learned from microRNAs. Front. Oncol. 8, 179. 10.3389/fonc.2018.00179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy M. J. (2006). Serum Tumor Markers in Breast Cancer: Are They of Clinical Value. Clin. Chem. 52 (3), 345–351. 10.1373/clinchem.2005.059832 [DOI] [PubMed] [Google Scholar]
- Eccles S. A., Aboagye E. O., Ali S., Anderson A. S., Armes J., Berditchevski F., et al. (2013). Critical Research Gaps and Translational Priorities for the Successful Prevention and Treatment of Breast Cancer. Breast Cancer Res. 15 (5), R92–R37. 10.1186/bcr3493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández Madrid F. (2005). Autoantibodies in Breast Cancer Sera: Candidate Biomarkers and Reporters of Tumorigenesis. Cancer Lett. 230 (2), 187–198. [DOI] [PubMed] [Google Scholar]
- Fine J. P., Pencina M. (2015). On the Quantitative Assessment of Predictive Biomarkers. J. Natl. Cancer Inst. 107 (8). 10.1093/jnci/djv187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming T. R., Powers J. H. (2012). Biomarkers and Surrogate Endpoints in Clinical Trials. Statist. Med. 31 (25), 2973–2984. 10.1002/sim.5403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gajos-Michniewicz A., Duechler M., Czyz M. (2014). MiRNA in Melanoma-Derived Exosomes. Cancer Lett. 347 (1), 29–37. 10.1016/j.canlet.2014.02.004 [DOI] [PubMed] [Google Scholar]
- Gao J., Zhang Q., Xu J., Guo L., Li X. (2013). Clinical Significance of Serum miR-21 in Breast Cancer Compared with CA153 and CEA. Chin. J. Cancer Res. 25 (6), 743–748. 10.3978/j.issn.1000-9604.2013.12.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garczyk S., von Stillfried S., Antonopoulos W., Hartmann A., Schrauder M. G., Fasching P. A., et al. (2015). AGR3 in Breast Cancer: Prognostic Impact and Suitable Serum-Based Biomarker for Early Cancer Detection. PLoS One 10 (4), e0122106. 10.1371/journal.pone.0122106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene J., Baird A. M., Casey O., Brady L., Blackshields G., Lim M., et al. (2019). Circular RNAs Are Differentially Expressed in Prostate Cancer and Are Potentially Associated with Resistance to Enzalutamide. Sci. Rep. 9 (1), 10739–10811. 10.1038/s41598-019-47189-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo X., Zhou Q., Su D., Luo Y., Fu Z., Huang L., et al. (2020). Circular RNA circBFAR Promotes the Progression of Pancreatic Ductal Adenocarcinoma via the miR-34b-5p/MET/Akt axis. Mol. Cancer 19 (1), 83–18. 10.1186/s12943-020-01196-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamam R., Ali A. M., Alsaleh K. A., Kassem M., Alfayez M., Aldahmash A., et al. (2016). microRNA Expression Profiling on Individual Breast Cancer Patients Identifies Novel Panel of Circulating microRNA for Early Detection. Sci. Rep. 6 (1), 25997–25998. 10.1038/srep25997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannafon B. N., Trigoso Y. D., Calloway C. L., Zhao Y. D., Lum D. H., Welm A. L., et al. (2016). Plasma Exosome microRNAs Are Indicative of Breast Cancer. Breast Cancer Res. 18 (1), 90–14. 10.1186/s13058-016-0753-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen T. B., Jensen T. I., Clausen B. H., Bramsen J. B., Finsen B., Damgaard C. K., et al. (2013). Natural RNA Circles Function as Efficient microRNA Sponges. Nature 495 (7441), 384–388. 10.1038/nature11993 [DOI] [PubMed] [Google Scholar]
- Hayes D. F., Isaacs C., Stearns V. (2001). Prognostic Factors in Breast Cancer: Current and New Predictors of Metastasis. J. Mammary gland Biol. Neoplasia 6 (4), 375–392. 10.1023/a:1014778713034 [DOI] [PubMed] [Google Scholar]
- Heneghan H. M., Miller N., Lowery A. J., Sweeney K. J., Newell J., Kerin M. J. (2010). Circulating microRNAs as Novel Minimally Invasive Biomarkers for Breast Cancer. Ann. Surg. 251 (3), 499–505. 10.1097/sla.0b013e3181cc939f [DOI] [PubMed] [Google Scholar]
- Hu Z., Dong J., Wang L.-E., Ma H., Liu J., Zhao Y., et al. (2012). Serum microRNA Profiling and Breast Cancer Risk: the Use of miR-484/191 as Endogenous Controls. Carcinogenesis 33 (4), 828–834. 10.1093/carcin/bgs030 [DOI] [PubMed] [Google Scholar]
- Institute N. C. (2013). BRCA1 and BRCA2: Cancer Risk and Genetic Testing. Cancer Therapy Advisor. [Google Scholar]
- Iorio M. V., Ferracin M., Liu C.-G., Veronese A., Spizzo R., Sabbioni S., et al. (2005). MicroRNA Gene Expression Deregulation in Human Breast Cancer. Cancer Res. 65 (16), 7065–7070. 10.1158/0008-5472.can-05-1783 [DOI] [PubMed] [Google Scholar]
- Ishibashi Y., Ohtsu H., Ikemura M., Kikuchi Y., Niwa T., Nishioka K., et al. (2017). Serum TFF1 and TFF3 but Not TFF2 Are Higher in Women with Breast Cancer Than in Women without Breast Cancer. Sci. Rep. 7 (1), 4846–4910. 10.1038/s41598-017-05129-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janes H., Pepe M. S., McShane L. M., Sargent D. J., Heagerty P. J. (2015). The Fundamental Difficulty with Evaluating the Accuracy of Biomarkers for Guiding Treatment. JNCI.J 107 (8), djv157. 10.1093/jnci/djv157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayaraj R., Nayagam G. N., Kar A., Sathyakumar S., Mohammed H., Smiti S., et al. (2019). Clinical Theragnostic Relationship between Drug-Resistance Specific miRNA Expressions, Chemotherapeutic Resistance, and Sensitivity in Breast Cancer: a Systematic Review and Meta-Analysis. Cells 8 (10), 1250. 10.3390/cells8101250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeck W. R., Sorrentino J. A., Wang K., Slevin M. K., Burd C. E., Liu J., et al. (2013). Circular RNAs Are Abundant, Conserved, and Associated with ALU Repeats. Rna 19 (2), 141–157. 10.1261/rna.035667.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joosse S. A. (2012). BRCA1 and BRCA2: a Common Pathway of Genome protection but Different Breast Cancer Subtypes. Nat. Rev. Cancer 12 (5), 372. 10.1038/nrc3181-c2 [DOI] [PubMed] [Google Scholar]
- Khoshnaw S. M., Rakha E. A., Abdel-Fatah T., Nolan C. C., Hodi Z., Macmillan R. D., et al. (2013). The microRNA Maturation Regulator Drosha Is an Independent Predictor of Outcome in Breast Cancer Patients. Breast Cancer Res. Treat. 137 (1), 139–153. 10.1007/s10549-012-2358-0 [DOI] [PubMed] [Google Scholar]
- Konermann S., Lotfy P., Brideau N. J., Oki J., Shokhirev M. N., Hsu P. D. (2018). Transcriptome Engineering with RNA-Targeting Type VI-D CRISPR Effectors. Cell 173 (3), 665–676. 10.1016/j.cell.2018.02.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristensen L. S., Andersen M. S., Stagsted L. V. W., Ebbesen K. K., Hansen T. B., Kjems J. (2019). The Biogenesis, Biology and Characterization of Circular RNAs. Nat. Rev. Genet. 20 (11), 675–691. 10.1038/s41576-019-0158-7 [DOI] [PubMed] [Google Scholar]
- Kulcheski F. R., Christoff A. P., Margis R. (2016). Circular RNAs Are miRNA Sponges and Can Be Used as a New Class of Biomarker. J. Biotechnol. 238, 42–51. 10.1016/j.jbiotec.2016.09.011 [DOI] [PubMed] [Google Scholar]
- Kun-Peng Z., Xiao-Long M., Chun-Lin Z. (2018). Overexpressed circPVT1, a Potential New Circular RNA Biomarker, Contributes to Doxorubicin and Cisplatin Resistance of Osteosarcoma Cells by Regulating ABCB1. Int. J. Biol. Sci. 14 (3), 321–330. 10.7150/ijbs.24360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ławicki S., Zajkowska M., Głażewska E. K., Będkowska G. E., Szmitkowski M. (2016). Plasma Levels and Diagnostic Utility of VEGF, MMP-9, and TIMP-1 in the Diagnosis of Patients with Breast Cancer. Onco Targets Ther. 9, 911–919. 10.2147/OTT.S99959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legnini I., Di Timoteo G., Rossi F., Morlando M., Briganti F., Sthandier O., et al. (2017). Circ-ZNF609 Is a Circular RNA that Can Be Translated and Functions in Myogenesis. Mol. Cel. 66 (1), 22–37. 10.1016/j.molcel.2017.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei B., Tian Z., Fan W., Ni B. (2019). Circular RNA: a Novel Biomarker and Therapeutic Target for Human Cancers. Int. J. Med. Sci. 16 (2), 292–301. 10.7150/ijms.28047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levenson V. (2007). Biomarkers for Early Detection of Breast Cancer: what, when, and where. Biochim. Biophys. Acta (Bba) - Gen. Subjects 1770 (6), 847–856. 10.1016/j.bbagen.2007.01.017 [DOI] [PubMed] [Google Scholar]
- Li C., Chen J., Zhang K., Feng B., Wang R., Chen L. (2015). Progress and Prospects of Long Noncoding RNAs (lncRNAs) in Hepatocellular Carcinoma. Cell Physiol Biochem 36 (2), 423–434. 10.1159/000430109 [DOI] [PubMed] [Google Scholar]
- Li S., Li X., Xue W., Zhang L., Yang L.-Z., Cao S.-M., et al. (2021). Screening for Functional Circular RNAs Using the CRISPR-Cas13 System. Nat. Methods 18 (1), 51–59. 10.1038/s41592-020-01011-4 [DOI] [PubMed] [Google Scholar]
- Li X., Heyer W.-D. (2008). Homologous Recombination in DNA Repair and DNA Damage Tolerance. Cell Res 18 (1), 99–113. 10.1038/cr.2008.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu F., Zhang J., Qin L., Yang Z., Xiong J., Zhang Y., et al. (2018). Circular RNA EIF6 (Hsa_circ_0060060) Sponges miR-144-3p to Promote the Cisplatin-Resistance of Human Thyroid Carcinoma Cells by Autophagy Regulation. Aging 10 (12), 3806–3820. 10.18632/aging.101674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Abraham J. M., Cheng Y., Wang Z., Wang Z., Zhang G., et al. (2018). Synthetic Circular RNA Functions as a miR-21 Sponge to Suppress Gastric Carcinoma Cell Proliferation. Mol. Ther. - Nucleic Acids 13, 312–321. 10.1016/j.omtn.2018.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Dong Y., Zhao L., Su L., Luo J. (2018). Circular RNA-MTO1 S-uppresses B-reast C-ancer C-ell V-iability and R-everses M-onastrol R-esistance through R-egulating the TRAF4/Eg5 axis. Int. J. Oncol. 53 (4), 1752–1762. 10.3892/ijo.2018.4485 [DOI] [PubMed] [Google Scholar]
- Loke S. Y., Lee A. S. G. (2018). The Future of Blood-Based Biomarkers for the Early Detection of Breast Cancer. Eur. J. Cancer 92, 54–68. 10.1016/j.ejca.2017.12.025 [DOI] [PubMed] [Google Scholar]
- Lü L., Sun J., Shi P., Kong W., Xu K., He B., et al. (2017). Identification of Circular RNAs as a Promising New Class of Diagnostic Biomarkers for Human Breast Cancer. Oncotarget 8 (27), 44096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu M., Ju S., Shen X., Wang X., Jing R., Yang C., et al. (2017). Combined Detection of Plasma miR-127-3p and HE4 Improves the Diagnostic Efficacy of Breast Cancer. Cbm 18 (2), 143–148. 10.3233/cbm-160024 [DOI] [PubMed] [Google Scholar]
- Ma C. X., Gao F., Luo J., Northfelt D. W., Goetz M., Forero A., et al. (2017). NeoPalAna: Neoadjuvant Palbociclib, a Cyclin-dependent Kinase 4/6 Inhibitor, and Anastrozole for Clinical Stage 2 or 3 Estrogen Receptor-Positive Breast Cancer. Clin. Cancer Res. 23 (15), 4055–4065. 10.1158/1078-0432.ccr-16-3206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J., Fang L., Yang Q., Hibberd S., Du W. W., Wu N., et al. (2019). Posttranscriptional Regulation of AKT by Circular RNA Angiomotin- like 1 Mediates Chemoresistance against Paclitaxel in Breast Cancer Cells. Aging 11 (23), 11369–11381. 10.18632/aging.102535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J., Kong Y., Nan H., Qu S., Fu X., Jiang L., et al. (2017). Pleiotrophin as a Potential Biomarker in Breast Cancer Patients. Clinica Chim. Acta 466, 6–12. 10.1016/j.cca.2016.12.030 [DOI] [PubMed] [Google Scholar]
- Maselli A., Parlato S., Puglisi R., Raggi C., Spada M., Macchia D., et al. (2019). Autoantibodies Specific to ERα Are Involved in Tamoxifen Resistance in Hormone Receptor Positive Breast Cancer. Cells 8 (7). 10.3390/cells8070750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maselli A., Capoccia S., Pugliese P., Raggi C., Cirulli F., Fabi A., et al. (2016). Autoantibodies Specific to Estrogen Receptor Alpha Act as Estrogen Agonists and Their Levels Correlate with Breast Cancer Cell Proliferation. Oncoimmunology 5 (2), e1074375. 10.1080/2162402x.2015.1074375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire A., Brown J. A. L., Kerin M. J. (2015). Metastatic Breast Cancer: the Potential of miRNA for Diagnosis and Treatment Monitoring. Cancer Metastasis Rev. 34 (1), 145–155. 10.1007/s10555-015-9551-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meganck R. M., Borchardt E. K., Castellanos Rivera R. M., Scalabrino M. L., Wilusz J. E., Marzluff W. F., et al. (2018). Tissue-dependent Expression and Translation of Circular RNAs with Recombinant AAV Vectors In Vivo . Mol. Ther. - Nucleic Acids 13, 89–98. 10.1016/j.omtn.2018.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell P. S., Parkin R. K., Kroh E. M., Fritz B. R., Wyman S. K., Pogosova-Agadjanyan E. L., et al. (2008). Circulating microRNAs as Stable Blood-Based Markers for Cancer Detection. Proc. Natl. Acad. Sci. 105 (30), 10513–10518. 10.1073/pnas.0804549105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon P.-G., Lee J.-E., Cho Y.-E., Lee S. J., Chae Y. S., Jung J. H., et al. (2016). Fibronectin on Circulating Extracellular Vesicles as a Liquid Biopsy to Detect Breast Cancer. Oncotarget 7 (26), 40189–40199. 10.18632/oncotarget.9561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon P.-G., Lee J.-E., Cho Y.-E., Lee S. J., Jung J. H., Chae Y. S., et al. (2016). Identification of Developmental Endothelial Locus-1 on Circulating Extracellular Vesicles as a Novel Biomarker for Early Breast Cancer Detection. Clin. Cancer Res. 22 (7), 1757–1766. 10.1158/1078-0432.ccr-15-0654 [DOI] [PubMed] [Google Scholar]
- Moreno-Gonzalo O., Villarroya-Beltri C., Sã¡nchez-Madrid F. (2014). Post-translational Modifications of Exosomal Proteins. Front. Immunol. 5, 383. 10.3389/fimmu.2014.00383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motawi T. M. K., Sadik N. A. H., Shaker O. G., El Masry M. R., Mohareb F. (2016). Study of microRNAs-21/221 as Potential Breast Cancer Biomarkers in Egyptian Women. Gene 590 (2), 210–219. 10.1016/j.gene.2016.01.042 [DOI] [PubMed] [Google Scholar]
- Nalejska E., Mączyńska E., Lewandowska M. A. (2014). Prognostic and Predictive Biomarkers: Tools in Personalized Oncology. Mol. Diagn. Ther. 18 (3), 273–284. 10.1007/s40291-013-0077-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oeffinger K. C., Fontham E. T. H., Etzioni R., Herzig A., Michaelson J. S., Shih Y.-C. T., et al. (2015). Breast Cancer Screening for Women at Average Risk. Jama 314 (15), 1599–1614. 10.1001/jama.2015.12783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace L. E., Keating N. L. (2014). A Systematic Assessment of Benefits and Risks to Guide Breast Cancer Screening Decisions. Jama 311 (13), 1327–1335. 10.1001/jama.2014.1398 [DOI] [PubMed] [Google Scholar]
- Perou C. M., Sørlie T., Eisen M. B., van de Rijn M., Jeffrey S. S., Rees C. A., et al. (2000). Molecular Portraits of Human Breast Tumours. nature 406 (6797), 747–752. 10.1038/35021093 [DOI] [PubMed] [Google Scholar]
- Polytarchou C., Iliopoulos D., Struhl K. (2012). An Integrated Transcriptional Regulatory Circuit that Reinforces the Breast Cancer Stem Cell State. Proc. Natl. Acad. Sci. 109 (36), 14470–14475. 10.1073/pnas.1212811109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin M., Liu G., Huo X., Tao X., Sun X., Ge Z., et al. (2016). Hsa_circ_0001649: a Circular RNA and Potential Novel Biomarker for Hepatocellular Carcinoma. Cbm 16 (1), 161–169. 10.3233/cbm-150552 [DOI] [PubMed] [Google Scholar]
- Raposo G., Stoorvogel W. (2013). Extracellular Vesicles: Exosomes, Microvesicles, and Friends. J. Cel Biol. 200 (4), 373–383. 10.1083/jcb.201211138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth C., Rack B., Müller V., Janni W., Pantel K., Schwarzenbach H. (2010). Circulating microRNAs as Blood-Based Markers for Patients with Primary and Metastatic Breast Cancer. Breast Cancer Res. 12 (6), R90–R98. 10.1186/bcr2766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salzman J., Chen R. E., Olsen M. N., Wang P. L., Brown P. O. (2013). Cell-type Specific Features of Circular RNA Expression. Plos Genet. 9 (9), e1003777. 10.1371/journal.pgen.1003777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salzman J., Gawad C., Wang P. L., Lacayo N., Brown P. O. (2012). Circular RNAs Are the Predominant Transcript Isoform from Hundreds of Human Genes in Diverse Cell Types. PloS one 7 (2), e30733. 10.1371/journal.pone.0030733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandhu R., Rein J., D’Arcy M., Herschkowitz J. I., Hoadley K. A., Troester M. A. (2014). Overexpression of miR-146a in Basal-like Breast Cancer Cells Confers Enhanced Tumorigenic Potential in Association with Altered P53 Status. Carcinogenesis 35 (11), 2567–2575. 10.1093/carcin/bgu175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanger H. L., Klotz G., Riesner D., Gross H. J., Kleinschmidt A. K. (1976). Viroids Are Single-Stranded Covalently Closed Circular RNA Molecules Existing as Highly Base-Paired Rod-like Structures. Proc. Natl. Acad. Sci. 73 (11), 3852–3856. 10.1073/pnas.73.11.3852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santer L., Bär C., Thum T. (2019). Circular RNAs: a Novel Class of Functional RNA Molecules with a Therapeutic Perspective. Mol. Ther. 27 (8), 1350–1363. 10.1016/j.ymthe.2019.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar D., Diermeier S. D. (2021). Circular RNAs: Potential Applications as Therapeutic Targets and Biomarkers in Breast Cancer. ncRNA 7 (1), 2. 10.3390/ncrna7010002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzenbach H., Hoon D. S. B., Pantel K. (2011). Cell-free Nucleic Acids as Biomarkers in Cancer Patients. Nat. Rev. Cancer 11 (6), 426–437. 10.1038/nrc3066 [DOI] [PubMed] [Google Scholar]
- Schwarzenbach H., Nishida N., Calin G. A., Pantel K. (2014). Clinical Relevance of Circulating Cell-free microRNAs in Cancer. Nat. Rev. Clin. Oncol. 11 (3), 145–156. 10.1038/nrclinonc.2014.5 [DOI] [PubMed] [Google Scholar]
- Sha L. Y., Zhang Y., Wang W., Sui X., Liu S. K., Wang T., et al. (2016). MiR-18a Upregulation Decreases Dicer Expression and Confers Paclitaxel Resistance in Triple Negative Breast Cancer. Eur. Rev. Med. Pharmacol. Sci. 20 (11), 2201–2208. [PubMed] [Google Scholar]
- Shen J., Stass S. A., Jiang F. (2013). MicroRNAs as Potential Biomarkers in Human Solid Tumors. Cancer Lett. 329 (2), 125–136. 10.1016/j.canlet.2012.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon R. (2015). Sensitivity, Specificity, PPV, and NPV for Predictive Biomarkers. J. Natl. Cancer Inst. 107 (8). 10.1093/jnci/djv153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson R. J., Lim J. W., Moritz R. L., Mathivanan S. (2009). Exosomes: Proteomic Insights and Diagnostic Potential. Expert Rev. Proteomics 6 (3), 267–283. 10.1586/epr.09.17 [DOI] [PubMed] [Google Scholar]
- Smid M., Wilting S. M., Uhr K., Rodríguez-González F. G., de Weerd V., Prager-Van der Smissen W. J. C., et al. (2019). The Circular RNome of Primary Breast Cancer. Genome Res. 29 (3), 356–366. 10.1101/gr.238121.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soler M., Estevez M.-C., Villar-Vazquez R., Casal J. I., Lechuga L. M. (2016). Label-free Nanoplasmonic Sensing of Tumor-Associate Autoantibodies for Early Diagnosis of Colorectal Cancer. Analytica Chim. Acta 930, 31–38. 10.1016/j.aca.2016.04.059 [DOI] [PubMed] [Google Scholar]
- Song D., Yue L., Zhang J., Ma S., Zhao W., Guo F., et al. (2016). Diagnostic and Prognostic Significance of Serum Apolipoprotein C-I in Triple-Negative Breast Cancer Based on Mass Spectrometry. Cancer Biol. Ther. 17 (6), 635–647. 10.1080/15384047.2016.1156262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swellam M., Abdelmaksoud M. D. E., Sayed Mahmoud M., Ramadan A., Abdel-Moneem W., Hefny M. M. (2015). Aberrant Methylation ofAPCandRARβ2genes in Breast Cancer Patients. Iubmb Life 67 (1), 61–68. 10.1002/iub.1346 [DOI] [PubMed] [Google Scholar]
- Tay F. C., Lim J. K., Zhu H., Hin L. C., Wang S. (2015). Using Artificial microRNA Sponges to Achieve microRNA Loss-Of-Function in Cancer Cells. Adv. Drug Deliv. Rev. 81, 117–127. 10.1016/j.addr.2014.05.010 [DOI] [PubMed] [Google Scholar]
- Taylor D. D., Gercel-Taylor C. (2013). The Origin, Function, and Diagnostic Potential of RNA within Extracellular Vesicles Present in Human Biological Fluids. Front. Genet. 4, 142. 10.3389/fgene.2013.00142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakur S., Grover R. K., Gupta S., Yadav A. K., Das B. C. (2016). Identification of Specific miRNA Signature in Paired Sera and Tissue Samples of Indian Women with Triple Negative Breast Cancer. PloS one 11 (7), e0158946. 10.1371/journal.pone.0158946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uehiro N., Sato F., Pu F., Tanaka S., Kawashima M., Kawaguchi K., et al. (2016). Circulating Cell-free DNA-Based Epigenetic Assay Can Detect Early Breast Cancer. Breast Cancer Res. 18 (1), 129–214. 10.1186/s13058-016-0788-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlassov A. V., Magdaleno S., Setterquist R., Conrad R. (2012). Exosomes: Current Knowledge of Their Composition, Biological Functions, and Diagnostic and Therapeutic Potentials. Biochim. Biophys. Acta (Bba) - Gen. Subjects 1820 (7), 940–948. 10.1016/j.bbagen.2012.03.017 [DOI] [PubMed] [Google Scholar]
- Voith von Voithenberg L., Crocetti E., Martos C., Dimitrova N., Giusti F., Randi G., et al. (2019). Cancer Registries - Guardians of Breast Cancer Biomarker Information: A Systematic Review. Int. J. Biol. Markers 34 (2), 194–199. 10.1177/1724600819836097 [DOI] [PubMed] [Google Scholar]
- Von Minckwitz G. (2014). Pathological Complete Response (pCR) Rates after Carboplatin-Containing Neoadjuvant Chemotherapy in Patients with Germline BRCA (G BRCA) Mutation and Triple-Negative Breast Cancer (TNBC): Results from GeparSixto. American Society of Clinical Oncology. [Google Scholar]
- Wang K. (2012). Comparing the MicroRNA Spectrum between Serum and Plasma. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang P. L., Bao Y., Yee M.-C., Barrett S. P., Hogan G. J., Olsen M. N., et al. (2014). Circular RNA Is Expressed across the Eukaryotic Tree of Life. PloS one 9 (3), e90859. 10.1371/journal.pone.0090859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weigel M. T., Dowsett M. (2010). Current and Emerging Biomarkers in Breast Cancer: Prognosis and Prediction. Endocrine-related cancer 17 (4), R245–R262. 10.1677/erc-10-0136 [DOI] [PubMed] [Google Scholar]
- Westholm J. O., Miura P., Olson S., Shenker S., Joseph B., Sanfilippo P., et al. (2014). Genome-wide Analysis of drosophila Circular RNAs Reveals Their Structural and Sequence Properties and Age-dependent Neural Accumulation. Cel Rep. 9 (5), 1966–1980. 10.1016/j.celrep.2014.10.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witwer K. W. (2015). Circulating microRNA Biomarker Studies: Pitfalls and Potential Solutions. Clin. Chem. 61 (1), 56–63. 10.1373/clinchem.2014.221341 [DOI] [PubMed] [Google Scholar]
- Wu G., Sun Y., Xiang Z., Wang K., Liu B., Xiao G., et al. (2019). Preclinical Study Using Circular RNA 17 and Micro RNA 181c-5p to Suppress the Enzalutamide-Resistant Prostate Cancer Progression. Cel Death Dis 10 (2), 37–14. 10.1038/s41419-018-1048-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu H.-J., Chu P.-Y. (2021). Recent Discoveries of Macromolecule- and Cell-Based Biomarkers and Therapeutic Implications in Breast Cancer. Ijms 22 (2), 636. 10.3390/ijms22020636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Q., Lu Z., Li H., Lu J., Guo L., Ge Q. (2011). Next-generation Sequencing of microRNAs for Breast Cancer Detection. J. Biomed. Biotechnol. 2011, 597145. 10.1155/2011/597145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang R., Pfütze K., Zucknick M., Sutter C., Wappenschmidt B., Marme F., et al. (2015). DNA Methylation Array Analyses Identified Breast Cancer-associatedHYAL2methylation in Peripheral Blood. Int. J. Cancer 136 (8), 1845–1855. 10.1002/ijc.29205 [DOI] [PubMed] [Google Scholar]
- Yang R., Stöcker S., Schott S., Heil J., Marme F., Cuk K., et al. (2017). The Association between Breast Cancer and S100P Methylation in Peripheral Blood by Multicenter Case-Control Studies. Carcinogenesis 38 (3), 312–320. 10.1093/carcin/bgx004 [DOI] [PubMed] [Google Scholar]
- Yang W., Gong P., Yang Y., Yang C., Yang B., Ren L. (2020). Circ-ABCB10 Contributes to Paclitaxel Resistance in Breast Cancer through Let-7a-5p/DUSP7 axis. Cmar Vol. 12, 2327–2337. 10.2147/cmar.s238513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin W.-B., Yan M.-G., Fang X., Guo J.-J., Xiong W., Zhang R.-P. (2018). Circulating Circular RNA Hsa_circ_0001785 Acts as a Diagnostic Biomarker for Breast Cancer Detection. Clinica Chim. Acta 487, 363–368. 10.1016/j.cca.2017.10.011 [DOI] [PubMed] [Google Scholar]
- Zaenker P., Gray E. S., Ziman M. R. (2016). Autoantibody Production in Cancer-The Humoral Immune Response toward Autologous Antigens in Cancer Patients. Autoimmun. Rev. 15 (5), 477–483. 10.1016/j.autrev.2016.01.017 [DOI] [PubMed] [Google Scholar]
- Zeng Y., Du W. W., Wu Y., Yang Z., Awan F. M., Li X., et al. (2017). A Circular RNA Binds to and Activates AKT Phosphorylation and Nuclear Localization Reducing Apoptosis and Enhancing Cardiac Repair. Theranostics 7 (16), 3842–3855. 10.7150/thno.19764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y. (2021). Optimized RNA-Targeting CRISPR/Cas13d Technology Outperforms shRNA in Identifying Functional circRNAs. Genome Biol. 22 (1), 1–22. 10.1186/s13059-021-02263-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng X., Chen L., Zhou Y., Wang Q., Zheng Z., Xu B., et al. (2019). A Novel Protein Encoded by a Circular RNA circPPP1R12A Promotes Tumor Pathogenesis and Metastasis of colon Cancer via Hippo-YAP Signaling. Mol. Cancer 18 (1), 47–13. 10.1186/s12943-019-1010-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J., Ye J., Zhang L., Xia L., Hu H., Jiang H., et al. (2017). Differential Expression of Circular RNAs in Glioblastoma Multiforme and its Correlation with Prognosis. Translational Oncol. 10 (2), 271–279. 10.1016/j.tranon.2016.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]