Abstract
Purpose
Given the poor soft-tissue quality in rheumatoid arthritis patients, many believe that rheumatoid arthritis should be treated with reverse total shoulder arthroplasty (rTSA). The purpose of this paper is to systematically assess outcomes of anatomic total shoulder arthroplasty (aTSA) in rheumatoid arthritis to determine if aTSA remains a viable option.
Methods
A comprehensive literature search was conducted identifying articles relevant to aTSA in the setting of rheumatoid arthritis with intact rotator cuff. Outcomes include clinical outcomes and rates of complication and revision.
Results
Ten studies were included with a total of 279 shoulders with mean follow-up of 116 ± 69 months. The mean age was 68 ± 10 years. Survivorship was 97%, 97% and 89% at 5, 10 and 20 years, respectively. The overall complication rate was 9%. Radiolucency was present in 69% of patients, of which 34% were at risk of loosening at 79 months. The overall rate of revision was 8.4%. Studies generally reported clinically significant improvements in range of motion, Constant score and ASES score.
Conclusion
aTSA in the rheumatoid patient results in improvements in range of motion and patient-reported outcomes. Rates of complications and survivorship are generally good in this population. However, it should be noted that there is significant heterogeneity in outcome reporting amongst the literature on this topic and that many studies fail to adequately report complication and revision rates. When compared to rTSA in patients with rheumatoid arthritis, evidence suggests that aTSA is still a viable treatment option despite the shift in utilization to rTSA.
Keywords: Rheumatoid arthritis, total shoulder arthroplasty, total range of motion
Introduction
Rheumatoid arthritis (RA) is the most common inflammatory arthritis, 1 with a majority of diagnoses occurring in patients aged 30 to 50 years. 2 Incidence of RA range from 5 to 50 per 100,000 adults in developed countries.3,4 It is estimated that up to 48% of patients with RA develop erosive changes within the shoulder. 5 Moreover, up to 75% of patients with seropositive RA develop debilitating shoulder symptoms impacting pain and function. 6
Various options exist to surgically treat patients with RA including anatomic total shoulder arthroplasty (aTSA), reverse total shoulder arthroplasty (rTSA) and hemiarthroplasty. Shoulder arthroplasty in the context of RA presents unique challenges due to the loss of bone stock (i.e. glenoid erosion), associated rotator cuff pathology, 7 risk of infection from immunosuppressive medications, 8 risk of fractures due to compromised bone mineral density from corticosteroids, quality of implant fixation 9 and internal rotation deformities.10,11 Moreover, decreased bone stock and quality can result in postoperative component loosening, 8 resulting in concerns regarding long-term survivorship of glenoid components. 8
The utility of rTSA for patients with RA has been widely investigated.9,12,13 A systematic review by Cho et al. 12 identified patients with RA undergoing rTSA had significant improvements in both pain relief and range of motion. However, those without rotator cuff pathology had decreased complication rates compared to those with rotator cuff pathology. Another systematic review by Gee et al. 9 found that patients undergoing rTSA for RA have significant improvements in patient-reported outcomes post-operatively, with relatively low rates of revision and complications. At present, controversy exists surrounding the use of aTSA versus rTSA in the rheumatoid population with rTSA being the treatment of choice for many surgeons given perceived concerns regarding survivorship. 14 As such it is important to determine if aTSA is still a viable treatment option, or if the shift to rTSA is warranted. We hypothesize that complication rates, clinical improvements and survivorship will be similar between procedures.
Methods
This study was conducted in accordance with the methods outlined in the Cochrane Handbook and is reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.
Search strategy and study screening
A comprehensive literature search was performed on PubMed, Medline and Embase for relevant titles from data inception to 3 July 2019 (Appendix Table 1). The research question and criteria for study eligibility were determined a priori. Titles, abstracts and full texts were screened in duplicate by two independent reviewers (A.H, A.S). Disagreements at the title and abstract stages were automatically carried over to the next stage. Disagreements at the full-text stage were resolved by an independent senior arbitrator (N.H). The unweighted kappa was calculated at each stage to address agreement.
Table 1.
Study characteristics and MINORS score of included studies.
| Author (year of publication) | Study type | Study design | Follow-up (months) | Sample size | Mean age (years) | Sex (% male) | MINORS score |
|---|---|---|---|---|---|---|---|
| Schentzke (2015) | Prospective | Case series | 24 | 5 | 71 (58–86) | N/R | 11 |
| Boardman et al. 17 | Prospective | Case series | 49 | 20 | 65 (31–85) | N/R | 10 |
| Fevang (2012) | N/A | Cross-sectional | 46.8 | 7 | 67 (SD 10) | N/R | 12 |
| Khan (2009) | Prospective | Cohort | N/R | 13 | 78.6 (38–84) | N/R | 13 |
| Burroughs et al. 24 | Prospective | Cohort | 67.2 (26–155) | 3 | 38.7 (SD 7.8) | N/R | 17 |
| Trail and Nuttall 19 | Prospective | Cohort | 68 (SD 22) | 40 | N/R | N/R | 12 |
| Barlow et al. 8 | Prospective | Cohort | 166 | 129 | 56 (17–83) | 27% | 13 |
| Betts et al. 21 | Prospective | Case series | 237 (198–285) | 14 | 48 (21–67) | 8% | 10 |
| Van De Sande and Rozing 20 | Prospective | Case series | 12 | 18 | 62 | N/R | 13 |
| Parsons et al. 25 | Prospective | Case series | 54 (24–111) | 17 | 58 (20–84) | 23% | 11 |
Study eligibility
The inclusion criteria for this review were as follows: (1) aTSA in the setting of RA; (2) outcomes must be presented and (3) papers must be in the English language.
Exclusion criteria were: (1) studies with a sample population which included other aetiologies unless outcomes for those with RA were presented separately; (2) articles in which patients had torn or severely compromised rotator cuffs, unless outcomes for those with intact rotator cuffs are presented separately; (3) outdated prostheses were used (metal-backed glenoids, uncemented glenoids, semi-constrained Stanmore prosthesis, Gristina Prosthesis, first generation Neer prosthesis); (4) review articles, case studies, technique articles and biomechanical studies. In some cases, if a small percentage of patients (<15%) had a minor rotator cuff tear, studies were included in order to increase sample size.
Data abstraction
Data were extracted independently by the two reviewers (A.H., A.S.) using an electronic data abstraction form. Relevant data were abstracted including study characteristics, patient demographics, details regarding operative procedures, rehabilitation protocol, outcome scores and rates of complication and failure.
The primary outcomes abstracted were rates of complications, radiographic findings, rates of revision, and survivorship. Secondary outcomes included clinical outcome measures such as: Range of motion (ROM), Constant score (CS), the Hospital for Special Surgery (HSS) assessment scale, the Shoulder Function Assessment (SFA) scale, the American Shoulder & Elbow Surgeons (ASES) score, the Simple Shoulder Test (SST), the Shoulder Pain and Disability (SPADI) index, as well as measures of pain.
Quality assessment
Methodological quality of all included studies was assessed independently and in duplicate by both reviewers using the Methodological Index for Non-Randomized Studies (MINORS) tool. 15 The MINORS tool is a quality assessment tool which assesses the aim, study sample, study design, outcome measures, bias, follow-up, and power of a study for a total of 16 points for non-comparative studies. 15 Comparative studies are evaluated with four additional criteria for a total of 24 points. Methodological quality was categorized a priori as follows: a score of 0–8 or 0–12 was considered poor quality, 9–12 or 13–18 was considered fair quality and 13–16 or 19–24 was considered excellent quality, for non-comparative and comparative studies, respectively.
Statistical analysis
Descriptive statistics including mean and measures of variance were utilized to report demographic information and outcome scores where applicable. Inter-reviewer agreement for screening was assessed using an unweighted Kappa (κ) statistic at all screening stages. Inter-reviewer agreement for the quality assessment was evaluated using the intraclass correlation coefficient (ICC). Agreement scores were categorized a priori as follows: 0.81 to 0.99 was considered as almost perfect agreement; 0.61 to 0.80 was substantial agreement; 0.41 to 0.60 was moderate agreement; 0.21 to 0.40 was fair agreement and a value of 0.20 or less was considered slight agreement. 16
Results
Study screening
The literature search yielded 2939 articles. Once duplicates were removed, 2238 articles remained for screening, from which 926 were moved forward to abstract screening. Following application of inclusion and exclusion criteria, 10 articles were identified for inclusion in this study. The Kappa scores at the title, abstract and full-text stages were 0.87 (95% CI 0.85–0.89), 0.76 (96% CI 0.70–0.82) and 0.86 (95% CI 0.77–0.96), respectively, indicating substantial agreement at the abstract screen and almost complete agreement at the title and full-text screens (Figure 1).
Figure 1.
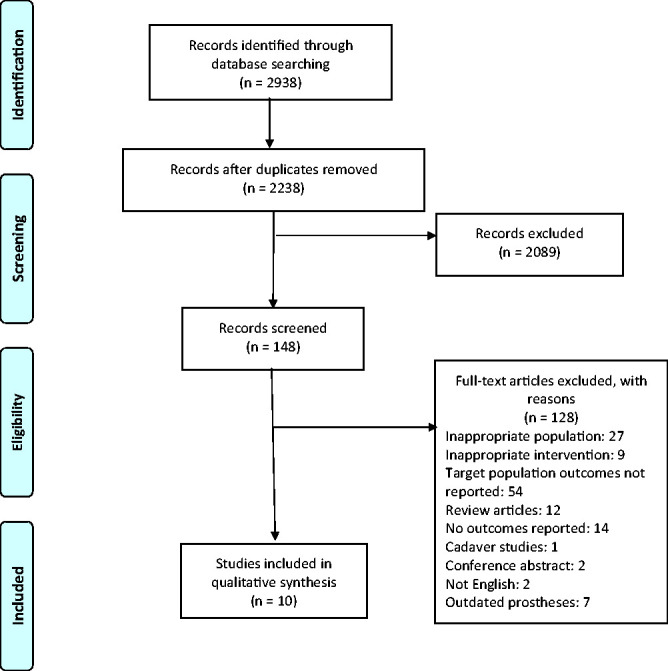
PRISMA flow diagram.
Study characteristics
Of the 10 included studies, of which nine were prospective and one was cross-sectional. This included three cohort studies and six case series.
Included studies were of fair quality overall with mean MINORS scores of 11.3 ± 1.2 and 13.0 ± 1.2 for non-comparative and comparative studies, respectively. Inter-reviewer agreement was almost perfect with ICC = 0.97 (95% CI 0.95–0.99). Methodological quality and study characteristics are presented in Table 1.
Patient demographics
There were a total of 279 shoulders included in this study. The mean age of patients in included studies was 68 ± 10 years. Sex was rarely reported for the target population. The mean follow-up of studies included in this review was 116 ± 69 months. Dominance/handedness of the injured arm was rarely reported for the target population. Demographic information is presented in Table 1.
By design, studies included in this review only commented on patients with intact rotator cuffs or presented the outcomes of those with intact rotator cuffs separately from those with rotator cuff tears (Appendix Table 2).
Table 2.
Complications.
| Study | Findings |
|---|---|
| Betts et al. 21 | Complications: 2 intraoperative humeral fractures; 1 deep infection; 1 painful aseptic loosening of both glenoid and humeral components; |
| Radiographic Findings: 11 components showed radiographic signs of loosening; continuous radiolucent lines in 12; incomplete radiolucency in 2; superior subluxation in all 14; | |
| Trail and Nuttall 19 | No loosening noted; |
| Radiographic findings: Not reported for target population. | |
| Boardman et al. 17 | Complications: Subscapular disruption in 1. |
| Radiographic findings: not reported. | |
| Van de Sande and Rozing 20 | Complications: 1 post-operative wound infection; 1 case of proximal humeral migration making acromioplasty necessary; 1 case had a traumatic fracture of greater tubercle and rupture of supraspinatus and infraspinatus muscles; |
| Radiographic findings: glenoid radiolucency in 8; humeral radiolucency in 1; none at risk of loosening. |
Outcomes
Complications and radiographic findings
The rate of complications was reported by 4 studies with a total of 92 shoulders. The overall rate of complication was 9%. The most common complications were humeral fractures (2%) and wound infections (2%). Regarding radiologic findings, only two included studies with 32 patients reported on radiographic findings for the target population. Among these patients, glenoid radiolucency was present at least to some degree in 69% of cases, of which 34% were determined to be at risk of loosening at mean follow-up of 79 months. Data on complication rates and radiographic findings are reported in Table 2.
Survivorship and revision
The rate of revision was reported by 3 studies with 173 patients. The overall rate of revision was found to be 13% (range 3%–36%). Kaplan–Meyer survivorship was reported by Barlow et al. 8 to be 97%, 97% and 89% and 5, 10 and 20 years, respectively (Appendix Table 3).
Table 3.
Range of motion.
| Study: Author (year of publication) | Mean forward elevation (degrees) | Mean external rotation | Mean internal rotation | Mean abduction |
|---|---|---|---|---|
| Boardman et al. 17 | Pre-op: 82 | Pre-op: 28 | Pre-op: L3 | N/R |
| Post-op: 135 | Post-op: 57 | Post-op: T12 (median) | ||
| Khan (2009) | Pre-op: 61 | Pre-op: 8 (−25–30) | Pre-op: thigh/buttock | Pre-op: 33 (10–50) |
| Post-op: 84.6 (20–160) | Post-op: 41.2 (10–70) | Post-op: buttock | Post-op: 43 (10–70) | |
| 10-year follow up: | 10-year follow-up: | 10-year follow-up: | 10-year follow-up: | |
| Intact rotator cuff: 93 (30–160) | Intact rotator cuff: 38 (10–60) | Intact rotator cuff: T12 | Intact rotator cuff: 60 (40–70) | |
| Torn rotator cuff: 85 (20–100) | Torn rotator cuff: 43 (20–70) | Torn rotator cuff: Thigh | Torn rotator cuff: 34 (0–50) | |
| Trail and Nuttall 19 | Post-op: 89 | N/R | N/R | Post-op: 79 |
| Barlow et al. 8 | Improvement: 45 degrees (SD 53 degrees) | Improvement: 21 degrees (SD 38) | Improvement: 1 spinal level (SD 3.8) | N/R |
| Betts et al. 21 | N/R | Pre-op: 5 | Pre-op: buttock | Pre-op: 45 |
| Post-op: 40 (24 mo.); 40 (114 mo.); 25 (132 mo.); | Post-op: L4 (24 mo.); Buttock to T7 (114 mo.); Buttock (132 mo.); | Post-op: 75 (24 mo.); 75 (114 mo.); 60 (132 mo.); | ||
| Van de Sande and Rozing 20 | Pre-op: 58 | Pre-op: 10 | N/R | Pre-op: 50 |
| Post-op: 91 | Post-op: 17 | Post-op 86 |
Range of motion
ROM was reported in six studies. Five studies with 220 patients reported forward elevation,8,17–20 5 studies with 194 patients reported external rotation.8,17,18,20,21 4 studies with 176 patients reported internal rotation8,17,18,21 and 4 studies with 65 patients reported abduction.18–21 Internal rotation was measured as the highest vertebral level patients could reach behind their back with their thumb. Studies which reported improvements in range of motion in degrees were pooled. Mean improvements in forward elevation, external rotation, internal rotation and abduction were 44° (range 33–53), 22° (range 7–35), 1 spinal level (range 0–5) and 27° (range 10–36), respectively.
None of the studies commented on the statistical significance of these improvements. However, substantial improvements were reported in forward elevation by four studies,8,17,18,20 external rotation by four studies,8,17,18,21 internal rotation by two studies17,21 and abduction by two studies20,21 (Table 3).
Pain
Pain scores were reported as an outcome in six studies. Four studies reported VAS scores,18–21 one study reported pain on a numerical scale from 1 to 15, 22 and one study reported pain on a numerical scale from 1 to 5. 8
None of the studies commented on the statistical significance of improvements in pain outcomes. However, substantial improvements were demonstrated in all studies which reported improvements in pain outcomes. Two of these studies measured the VAS score,18,20 and one utilized a scale from 1 to 5. 8 The remaining studies only reported post-operative values, making it impossible to determine the degree of improvement. Pain outcomes are summarized in Table 4.
Table 4.
Pain outcome measures.
| Study: Author (year of publication) | Findings |
|---|---|
| Schnetzke et al. 22 | Pain measure on a scale of 0–15 |
| Post-op: 9.8 (SD 3.6) | |
| Khan (2009) | VAS |
| Pre-op: 7.7 (range 5–10) | |
| Post-op: 1.2 (range 0–9) | |
| Trail and Nuttall 19 | VAS |
| Post-op: 1.8 | |
| Barlow et al. 8 | Scale of 1–5 |
| Improvement: 2.7 Points (SD 1.4) | |
| Betts et al. 21 | VAS |
| Post-op: 1.84 | |
| Van de Sande and Rozing 20 | VAS |
| Pre-op: 5.6 (rest); 8.3 (activity) | |
| Post-op: 2.3 (rest); 3.6 (activity) |
Other outcomes measures
Various other outcome measures were used by included studies (Appendix Table 4). Oxford Shoulder Score (OSS) was reported by two studies,18,23 the Constant score was reported by three studies18,19,22 and ASES was reported by three studies.18,19,24 SST, 25 HSS, 20 SPADI 24 and SFA 20 were each reported on by only one study. Statistically significant improvements were found in HSS, 20 and in SFA, 20 each by one study. The remaining studies did not comment on statistical significance. Substantial improvements were reported in SST, 25 OSS, 18 Constant Score 18 and ASES, 18 each by one study. All studies which reported pre-operative and post-operative values, or improvements in outcome measures demonstrated substantial improvements. The remaining studies only reported post-operative values. Van De Sande et al. 20 reported that 87% of patients satisfied with the procedure at follow-up. 20
Discussion
The present study systematically reviewed the literature for outcomes and failure rates following aTSA in patients with RA. The primary findings of this review suggest that patients with RA can expect significant improvements in range of motion and patient-reported outcomes after aTSA. A particularly interesting finding of this review was the relatively good survivorship of aTSA in the RA population.
Overall, studies reported improvements in ROM and patient-reported outcomes. Almost all improvements in ASES and Constant Score clinically significant 26 and mean improvements in forward elevation, external rotation and abduction were all found to be clinically significant, 27 though statistical significance was not often reported. When compared to populations without RA, there were varying findings. When compared to patients with osteoarthritis, RA patients were found to have significantly higher levels of pain post-operatively (9.8 vs. 14.2, p < 0.0001). 22 Furthermore, they were found to have lower Constant Scores and range of motion, but there was no comment on statistical significance. 22 Additionally, Boardman et al. 17 found that 84% of osteoarthritis patients were able to maintain range of motion post-operatively, while only 65% of RA patients were able to. This was attributed to poor cuff quality in the RA population. Compared to other diagnoses, Parsons et al. 25 found significantly superior SST scores in the RA population as compared to degenerative joint disease and capsulorrhaphy arthropathy (p = 0.02), while Burroughs et al. 24 found superior SPADI scores as compared to post-traumatic patients, though statistical analysis was not performed.
The overall rate of complication was 9%, and the rate of revision was 13% (range 3.0–36.0%) with a mean follow-up of 80 ± 43 months. The most common complications were intra-operative fractures, wound complications and nerve-related complications. Two systematic reviews assessing rTSA in the RA population found revision rates to be 5.0% and 7.3%, and rates of complication to be 22.0% and 19.0%.9,12 These rates of complication are much higher than those reported in this review, but the rates of revision are lower. However, almost all patients included in these studies had damaged rotator cuffs making comparison difficult. Furthermore, these studies were unable to report on long-term survivorship. While there is a trend towards rTSA in this population due to high rates of rotator cuff tear, long-term survivorship of aTSA was found to be excellent in the absence of rotator cuff pathology. As such, in the presence of an intact rotator cuff, aTSA may be an appropriate alternative to rTSA. Surgeons may benefit from determining rotator cuff status preoperatively via MRI or by direct observation at the time of surgery in order to make an appropriate decision. However, in order to better draw conclusions, more high-quality studies are necessary assessing the impact of rotator cuff tears on survivorship in this population.
There are some key strengths of this study that are worth mentioning. Notably – to the best of our knowledge – this study is the first of its kind assessing outcomes of aTSA in the rheumatoid population. Second, the select sample of this study including only patients with intact rotator cuff tears and studies which utilized modern prostheses makes the findings of this review highly applicable to the target population. Additionally, a rigorous screening approach was performed in duplicate in order to minimize reviewer bias. Moreover, agreement among both reviewers at all screening stages was excellent.
There are some limitations of this study which should be considered in the interpretation of findings. First, as the population was limited to those with intact rotator cuff tears, the sample size of this review is quite small. Additionally, studies with different indications for surgery included in their sample population often failed to stratify outcomes based off the different indications. Third, while the population was very select, there were a small proportion of patients included in this review with rotator cuff tears or older, metal-backed glenoid components which may not be applicable to aTSA in a modern context. The overall complication and revision rates found in this study must be interpreted with caution as many of the studies failed to adequately report these variables. The same is true for many outcome measures used as some are only reported by a few studies. There was significant heterogeneity in outcome reporting between studies and there was a lack of common comparison groups between studies, thus precluding a meta-analysis. Finally, the quality of included studies overall was relatively poor limiting the applicability and interpretation of these findings. Further high-quality studies are necessary to better understand outcomes of aTSA in the rheumatoid population.
Conclusion
aTSA in the rheumatoid patient results in improvements in range of motion and patient-reported outcomes. Rates of complications and survivorship are generally good in this population. However, it should be noted that there is significant heterogeneity in outcome reporting amongst the literature on this topic and that many studies fail to adequately report complication and revision rates. When compared to rTSA in patients with RA, evidence suggests that aTSA is still a viable treatment option despite the shift in utilization to rTSA.
Supplemental Material
Supplemental material, sj-pdf-1-sel-10.1177_1758573220954157 for Anatomic total shoulder arthroplasty in rheumatoid arthritis: A systematic review by Ahmed Haleem, Ajaykumar Shanmugaraj, Nolan S. Horner, Timothy Leroux, Moin Khan and Bashar Alolabi in Shoulder & Elbow
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Moin Khan https://orcid.org/0000-0002-8237-8095
Bashar Alolabi https://orcid.org/0000-0002-8393-0953
Supplemental Material: Supplemental material is available for this article online.
References
- 1.Firestein GS and Kelley WN. Etiology and pathogenesis of rheumatoid arthritis. In: Firestein GS, Budd RC, McInnes IB, et al. (eds) Kelley and Firestein’s textbook of rheumatology. 8th ed. Philadelphia: Saunder/Elsevier, 2009, pp.1035–1086.
- 2.Klippel JH, Stone JH, Crofford LJ, et al. Rheumatoid arthritis clinical and laboratory manifestations, 13th ed. New York, NY: Springer-Verlag, 2001, pp. 114–121. [Google Scholar]
- 3.Carbonell J, Cobo T, Balsa A, et al. The incidence of rheumatoid arthritis in Spain: results from a nationwide primary care registry. Rheumatology 2008; 47: 1088–1092. [DOI] [PubMed] [Google Scholar]
- 4.Pedersen JK, Kjaer NK, Svendsen AJ, et al. Incidence of rheumatoid arthritis from 1995 to 2001: impact of ascertainment from multiple sources. Rheumatol Int 2009; 29: 411–415. [DOI] [PubMed] [Google Scholar]
- 5.Lehtinen JT, Kaarela K, Belt EA, et al. Incidence of glenohumeral joint involvement in seropositive rheumatoid arthritis. A 15 year endpoint study. J Rheumatol 2000; 27: 347–350. [PubMed] [Google Scholar]
- 6.Rittmeister M, Kerschbaumer F. Grammont reverse total shoulder arthroplasty in patients with rheumatoid arthritis and nonreconstructible rotator cuff lesions. J Shoulder Elbow Surg 2001; 10: 17–22. [DOI] [PubMed] [Google Scholar]
- 7.Barrett WP, Thornhill TS, Thomas WH, et al. Nonconstrained total shoulder arthroplasty in patients with polyarticular rheumatoid arthritis. J Arthroplasty 1984; 4: 91–96. [DOI] [PubMed] [Google Scholar]
- 8.Barlow JD, Yuan BJ, Schleck CD, et al. Shoulder arthroplasty for rheumatoid arthritis: 303 consecutive cases with minimum. J Shoulder Elbow Surg 2014; 23: 791–799. [DOI] [PubMed] [Google Scholar]
- 9.Gee ECA, Hanson EK, Saithna A. Reverse shoulder arthroplasty in rheumatoid arthritis: a systematic review. Open Orthop J 2015; 9: 237–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rozing PM, Brand R. Rotator cuff repair during shoulder arthroplasty in rheumatoid arthritis. J Arthroplasty 1998; 13: 311–319. [DOI] [PubMed] [Google Scholar]
- 11.Thabe H, Schill S, Dinges H. Die endoprothetische Versorgung des rheumatischen Schultergelenkes. Akt Rhematol 1994; 19: 155–160. [Google Scholar]
- 12.Cho C-H, Kim D-H, Song K-S. Reverse shoulder arthroplasty in patients with rheumatoid arthritis: a systematic review. Clin Orthop Surg 2017; 9: 325–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zumstein MA, Pinedo M, Old J, et al. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg 2011; 20: 146–157. [DOI] [PubMed] [Google Scholar]
- 14.Leroux T, Basques B, Saltzman B, et al. Shoulder arthroplasty in patients with rheumatoid arthritis: a population-based study examining utilization, adverse events, length of stay, and cost. Am J Orthop 2018; 47: 1--13–1--13. [DOI] [PubMed] [Google Scholar]
- 15.Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 2003; 73: 712–716. [DOI] [PubMed] [Google Scholar]
- 16.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–174. [PubMed] [Google Scholar]
- 17.Boardman ND, Cofield RH, Bengtson KA, et al. Rehabilitation after total shoulder arthroplasty. J Arthroplasty 2001; 16: 483–486. [DOI] [PubMed] [Google Scholar]
- 18.Khan A, Bunker TD, Kitson JB. Clinical and radiological follow-up of the Aequalis third-generation cemented total shoulder replacement. J Bone Joint Surg Br 1998; 91: 1594–1600. [DOI] [PubMed] [Google Scholar]
- 19.Trail IA, Nuttall D. The results of shoulder arthroplasty in patients with rheumatoid arthritis. J Bone 2002; 84: 1121–1125. [DOI] [PubMed] [Google Scholar]
- 20.van de Sande MA, Rozing PM. Modular total shoulder system with short stem. A prospective clinical and radiological analysis. Int Orthop 2004; 28: 115–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Betts HM, Abu-Rajab R, Nunn R, et al. Total shoulder replacement in rheumatoid disease: a 16 to 23- year follow-up. J Bone Joint Surg Br 2009; 91: 1197–1200. [DOI] [PubMed] [Google Scholar]
- 22.Schnetzke M, Coda S, Walch G, et al. Clinical and radiological results of a cementless short stem shoulder prosthesis at minimum follow-up of two years. Int Orthop 2015; 39: 1351–1357. [DOI] [PubMed] [Google Scholar]
- 23.Fevang B-tS, Lygre SHL, Bertelsen G, et al. Pain and function in eight hundred and fifty nine patients comparing shoulder hemiprostheses, resurfacing prostheses, reversed total and conventional total prostheses. Int Orthop 2013; 37: 59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burroughs PL, Gearen PF, Petty WR, et al. Shoulder arthroplasty in the young patient. J Arthroplasty 2003; 18: 792–798. [DOI] [PubMed] [Google Scholar]
- 25.Parsons II, Campbell B, Titelman RM, et al. Characterizing the effect of diagnosis on presenting deficits and outcomes after total shoulder arthroplasty. J Shoulder Elbow Surg 2005; 14: 575–584. [DOI] [PubMed] [Google Scholar]
- 26.Hao Q, Devji T, Zeraatkar D, et al. Minimal important differences for improvement in shoulder condition patient-reported outcomes: a systematic review to inform a BMJ Rapid Recommendation. BMJ Open 2019; 9: 1--10–1--10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Muir SW, Corea CL, Beaupre L. Evaluating change in clinical status: reliability and measures of agreement for the assessment of glenohumeral range of motion. N Am J Sports Phys Ther 2010; 5: 98–110. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-sel-10.1177_1758573220954157 for Anatomic total shoulder arthroplasty in rheumatoid arthritis: A systematic review by Ahmed Haleem, Ajaykumar Shanmugaraj, Nolan S. Horner, Timothy Leroux, Moin Khan and Bashar Alolabi in Shoulder & Elbow


