Abstract
Background
Pectoralis minor syndrome involves pain, paraesthesia and weakness in the arm due to compression of the brachial plexus passing beneath pectoralis minor; this paper reports the results of a single centre’s treatment pathway in affected patients.
Methods
During a four-year period, patients exhibiting symptoms of pectoralis minor syndrome without significant improvement following physiotherapy proceeded to Botulinum injection. Those with good response to injection but subsequent recurrence of symptoms were offered pectoralis minor tenotomy. Oxford shoulder Scores were collected at baseline and after interventions.
Results
Twenty-one patients received Botulinum injection; at six weeks following injection, mean change in Oxford Shoulder Score was +12.4, with only one patient reporting a worsening of symptoms. Of the 17 patients with clinically significant response to injection, 12 have subsequently undergone tenotomy; three months following tenotomy, mean change in Oxford Shoulder Score from baseline was +22.3. Improvement was maintained in all patients at prolonged follow-up (average 20 months post-tenotomy).
Discussion
This pathway has shown to be extremely effective in patients not responding to first-line treatment for pectoralis minor syndrome, with 85% of patients post-injection and 100% of patients post-tenotomy showing significant (greater than published minimal clinically important difference value of six points) improvements in Oxford Shoulder Score, maintained at follow-up.
Keywords: Pectoralis minor syndrome, shoulder surgery, Botulinum injection, tenotomy
Introduction
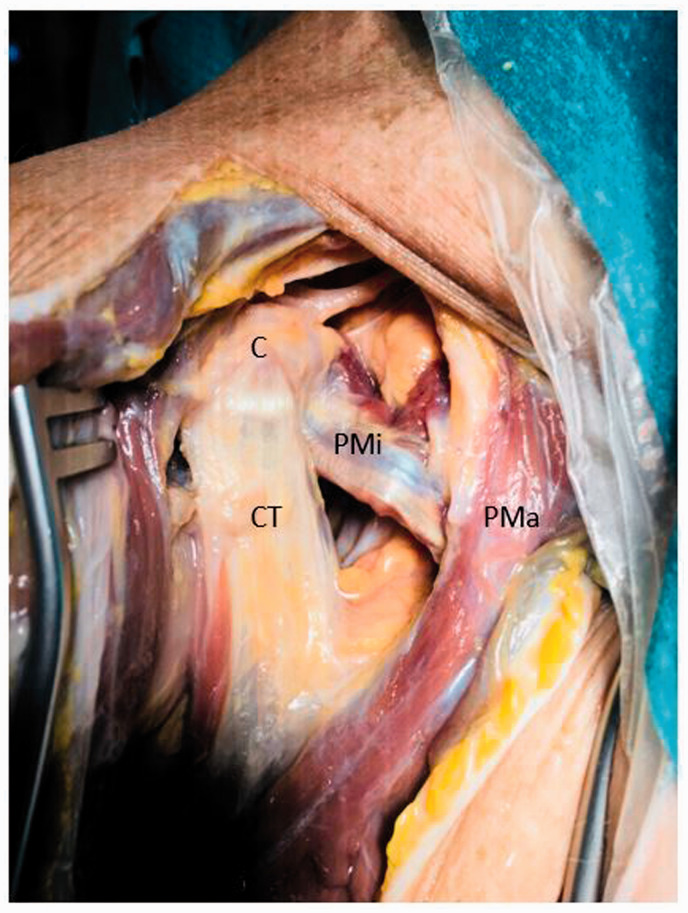
Pectoralis minor syndrome (PMS) consists of a collection of symptoms including pain, paraesthesia and weakness in the affected arm due to compression of the brachial plexus (usually C8-T1) as it passes beneath the pectoralis minor muscle, close to its insertion on to the coracoid process (see Figure 1). 1 Pain is often reported in the shoulder and anterior chest wall, radiating down the arm and hand (usually in a median/ulnar nerve distribution), and is exacerbated by the use of the arm above shoulder height. There is usually tenderness to palpation over the coracoid insertion of pectoralis minor itself. 2 PMS is often regarded as part of the spectrum of neurogenic thoracic outlet syndrome, which includes other potential sites of plexus compression more proximally. 3
Figure 1.
Anterior view of a right cadaveric shoulder dissection showing the insertion of the CT and PMi onto the C. PMa also visible. C: coracoid; CT: conjoint tendon; PMa: pectoralis major; PMi: pectoralis minor.
Aetiology is thought to consist of hyperactivity of pectoralis minor causing protraction and abduction of the shoulder, with subsequent pressure on the lower brachial plexus. This frequently results from an acquired abnormality in muscle patterning following either acute or chronic injury to the neck or shoulder. 1
Diagnosis of PMS is challenging and consists of thorough history and examination rather than specific radiological or electrophysiological studies. This difficulty means that the syndrome is often overlooked, and patients may suffer for prolonged periods or even undergo unnecessary and unsuccessful surgical procedures such as carpal or cubital tunnel releases as a result of misdiagnosis. It frequently occurs in relatively young and otherwise healthy individuals, meaning there is also a significant potential economic burden associated with the condition due to loss of employment. 2
Injections to either anaesthetise the area or paralyse pectoralis minor muscle in the form of local anaesthetic or Botulinum injection have been reported as methods of diagnosis of the syndrome, and a way of providing temporary relief from symptoms.4–8 A good result from such injections can be used as a positive indicator to proceed with a potential definitive procedure, in the form of pectoralis minor tenotomy.2,4,9,10
This paper reports the results of a single centre’s diagnostic and treatment pathway in patients with clinical features consistent with PMS, using Botulinum injection as a diagnostic tool, and subsequent pectoralis minor tenotomy in patients with a positive response.
Methods
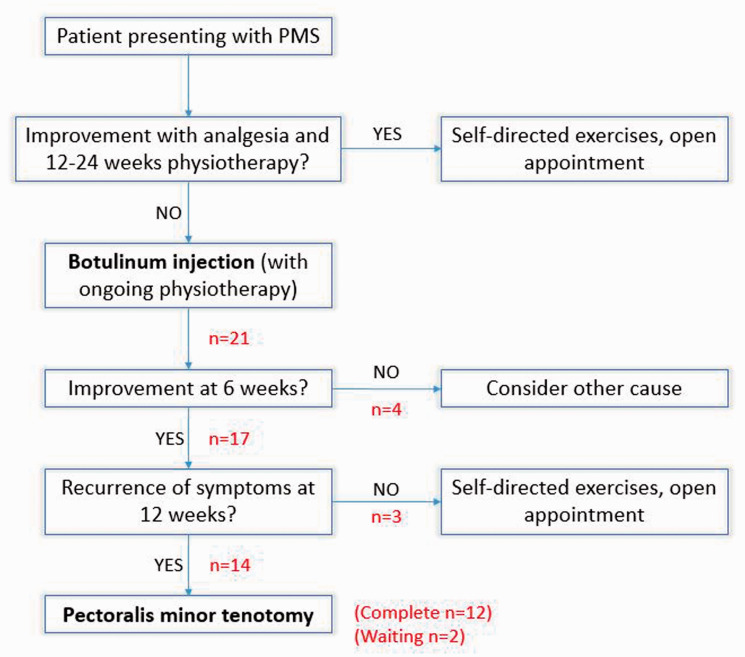
Patients presenting to upper limb elective outpatient clinics at a single centre from January 2016 to December 2019 who were found to have features consistent with PMS (Table 1) were initially treated with a 12- to 24-week course of physiotherapy and analgesia. Unless otherwise indicated, magnetic resonance imaging scans or neurophysiology studies were not routinely requested. Those patients who were still suffering from symptoms following this went on to have Botulinum Toxin A injection (Dysport, 500 iu, split between three and four sites in the pectoralis minor muscle belly) under ultrasound guidance in the radiology department, with further regular physiotherapy following this. Exercises incorporated diaphragmatic breathing, stretches for the anterior chest, functional open and closed kinetic chain whole-body movement patterns, and emphasis on retraction and upward rotation of the scapula during functional activity. Patients were reassessed at six weeks and four months following the injection, and those who had an initial good response (as evidenced by clinical examination, patient feedback, and Oxford Shoulder Score (OSS)) but subsequent recurrence of symptoms were offered pectoralis minor tenotomy (Figure 2).
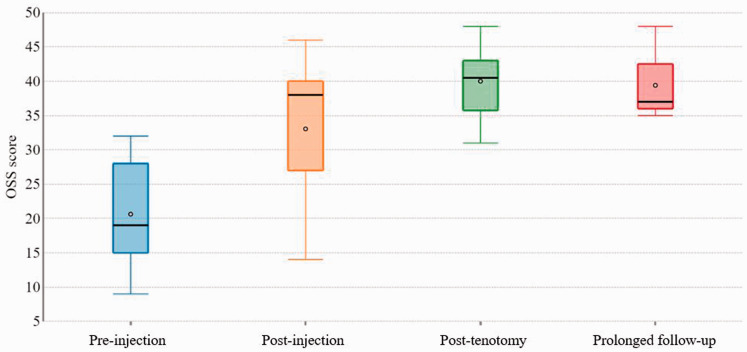
Figure 3.
Box plot of change in OSS throughout treatment pathway. OSS: Oxford Shoulder Score.
Table 1.
Signs and symptoms associated with pectoralis minor syndrome.
| – Pain/numbness/paraesthesia in neck/arm/hand |
| – Symptoms exacerbated by elevation of arm |
| – Scapular protraction at rest |
| – Tenderness to palpation over coracoid insertion of pectoralis minor |
Figure 2.
Diagnostic and treatment pathway for PMS. PMS: pectoralis minor syndrome.
Tenotomy was performed as an open procedure using a deltopectoral approach under general anaesthetic in the beach chair position. Prophylactic antibiotics and tranexamic acid were not required. The coracoid was identified and pectoralis minor isolated and then incised from its insertion with scissors while protecting the underlying structures. Patients were placed in a sling postoperatively which they were instructed to remove as comfort dictated, with early mobilisation encouraged (though no heavy lifting or repetitive overhead activity for the first two weeks). Prior to surgery patients had been educated regarding the vital role of rehabilitation in postoperative recovery and shown self-directed exercises to perform from the first day following surgery, incorporating neural glide stretches to reduce the chance of adhesion formation. An early face-to-face physiotherapy appointment was provided within the first week, and postoperative exercises were continued and progressed for a minimum of three months to gain longer term improvements. As pain settled, more attention was focused on increasing strength in trapezius and serratus anterior muscles using a graded approach.
Patient-reported outcome measures (PROMs) in the form of OSSs were recorded at each stage in the pathway. The OSS is a validated PROM consisting of 12 questions assessing shoulder pain and function, providing a score ranging from 0 (worst) to 48 (best). Values for the minimal clinically important difference (MCID) of the OSS vary in the literature, but there is a general consensus around a value of 6.11,12 Therefore, for this study, an improvement in scores of at least six points between stages was seen as significant.
However, any change in OSS was used in conjunction with clinical examination and patient feedback to determine patient progression to the next stage in the treatment pathway, rather than relying on OSS alone.
Results
Twenty-one patients (mean age 39 (range 23–58), M:F ratio of 1:10.5, 10 left:11 right sided, nil bilateral) displaying symptoms of PMS for at least six months with no improvement following an initial course of physiotherapy received an ultrasound guided Botulinum injection; mean baseline OSS prior to injection was 20.7 (range 9–32).
Six weeks following injection, mean OSS was 33.0 (range 14–46); mean change in OSS was +12.4 (range −18 to +30), with only one patient reporting a worsening of symptoms. Of the improvements, 17 (85%) patients reported a difference of greater than the MCID of six points and were therefore potentially clinically significant. Despite a clinically significant OSS improvement, 1 of these 17 patients was subsequently deemed to be suffering from alternative pathology on clinical examination and did not subjectively feel that their symptoms had significantly improved, so was removed from the pathway. One of the patients who saw an improvement of OSS <6 nonetheless reported subjective improvement and had a supportive clinical examination, so proceeded to the next stage. The remainder of the improvements <6 did not feel they had subjectively improved so were removed.
Of the 17 patients with an overall positive response to the injection, 14 then were listed for pectoralis minor tenotomy following recurrence of symptoms at four-month follow-up (the remaining 3 patients did not relapse and therefore did not require further intervention). At the time of writing, 12 patients from this group had undergone the procedure. Three months following tenotomy, mean OSS was 38.8 (range 31–48); mean change in OSS from baseline was +21.6 (range +10 to +38). Of these improvements, all 12 (100%) reported a difference of greater than six points and were therefore deemed clinically significant.
There were no surgical complications reported intra-operatively or noted subsequently during follow-up. At tenotomy, pectoralis minor was consistently found to be flaccid with no evidence of contracture, supporting the theory that this was a dynamic problem.
Prolonged follow-up scores reveal that the improvement following tenotomy appears to be sustained (Figure 3); all patients reported that symptoms remained improved long after the operation, with mean OSS of 39.7 at average prolonged follow-up time of 20 months (range 5–45 months).
Although further qualitative data were not formally collected, verbal and written patient feedback at prolonged follow-up was universally positive, with one patient reporting that the treatment pathway had ‘changed my world’.
Discussion
PMS is an underdiagnosed condition that can be extremely debilitating for patients. It is not often considered as a presentation to a shoulder clinic, as most thoracic outlet syndrome patients are seen by vascular surgeons (with most studies on the subject published in vascular literature); increased awareness and understanding of the condition within the orthopaedic community is therefore extremely important. Previous studies have demonstrated good temporary symptomatic response to Botulinum injection,4-7 with others demonstrating that subsequent pectoralis minor tenotomy can provide good long-term symptom relief; Sanders and Rao reported 92% success rates at 1- to 3-year follow-up post-tenotomy, 4 while Vemuri et al. reported 75% success at a shorter 3-month follow-up. 2 The diagnosis and treatment pathway described here builds on previous research and has shown good levels of sustained success for those patients who have not responded to simple first-line treatment in the form of analgesia and physiotherapy. Botulinum injection is a relatively painless procedure performed as an outpatient in the radiology department, which is well tolerated by patients. Although proceeding to pectoralis minor tenotomy is obviously significantly more invasive and involves a general anaesthetic, the procedure is a simple one, performed as a day-case, and with low risk of complications.
Although not specifically validated for PMS, the OSS is a widely used PROM for patients undergoing shoulder surgery 12 and was felt to be the most appropriate tool to use to assess change in symptoms – though crucially also taking into account clinical examination and general patient feedback at each stage. There are other PROMs validated specifically for neuropathic pain, such as the Neuropathic Pain Scale, 13 which may be helpful to include in future studies.
A preponderance of female patients is reflected in other studies of PMS, though the percentage seen here (90%) is high, albeit with a relatively small study population. To our knowledge, there does not seem to be an explained cause of this imbalance.
There were patients in this study who, despite seeing an improvement in OSS after Botulinum, did not subjectively feel their symptoms had significantly improved and did not have a clinical exam to support this at their six-week follow-up post-injection. It is therefore important for clinicians to remain open to the consideration of alternative pathologies at all points along the treatment pathway. The most likely differential for these patients was thought to be compression of the plexus more proximally, at the level of the scalene muscles – meaning that pectoralis minor tenotomy would not be indicated. One patient experienced concurrent paralysis of pectoralis major following injection; the dose of Botulinum injection for subsequent patients in the pathway has now been reduced to 300 iu.
Interestingly, three patients who saw a positive response following Botulinum injection did not experience a recurrence in their symptoms after the effects of Botulinum had ceased and so did not proceed to tenotomy. There was no apparent difference in demographics or presentation symptoms for this sub-group (mean age 37, all female, presenting with radicular pain). It is likely that the ongoing physiotherapy during this time, aided by the effect of the Botulinum, allowed effective treatment of the condition without having to resort to a more invasive procedure. Success in treating these patients relies on a multidisciplinary approach at each stage between surgeons, radiologists, and physiotherapists.
Current nationwide limitations imposed on elective operating mean that there is no clear timescale for the remaining patients awaiting tenotomy in this study to undergo surgery, meaning that repeated Botulinum injections to help symptom control and facilitate further physiotherapy are an option to be considered.
Obvious limitations of the study are its retrospective nature and the small number of patients from a single centre. Prolonged and ongoing follow-up will be helpful to determine whether there is a recurrence of symptoms at a later date. Further prospective studies with larger numbers are required to help definitively quantify the positive effect of this treatment pathway.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: MH.
Contributorship: All authors were involved in conception and design, data collection and analysis and writing of this study.
ORCID iD: Matthew Howard https://orcid.org/0000-0002-7472-9289
Ethical Review and Patient Consent
The study was discussed with the local Trust Research and Development department; as this was an anonymised case series reporting results of current departmental practice, formal ethical approval was not required. Written informed consent was obtained from the patients for their anonymised information to be published in this article.
References
- 1.Boezaart AP, Haller A, Laduzenski S, et al. Neurogenic thoracic outlet syndrome: a case report and review of the literature. Int J Shoulder Surg 2010; 4: 27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vemuri C, Wittenberg AM, Caputo FJ, et al. Early effectiveness of isolated pectoralis minor tenotomy in selected patients with neurogenic thoracic outlet syndrome. J Vasc Surg 2013; 57: 1345–1352. [DOI] [PubMed] [Google Scholar]
- 3.Sanders RJ, Annest SJ. Thoracic outlet and pectoralis minor syndromes. Semin Vasc Surg 2014; 27: 86–117. [DOI] [PubMed] [Google Scholar]
- 4.Sanders RJ, Rao NM. The forgotten pectoralis minor syndrome: 100 operations for pectoralis minor syndrome alone or accompanied by neurogenic thoracic outlet syndrome. Ann Vasc Surg 2010; 24: 701–708. [DOI] [PubMed] [Google Scholar]
- 5.Torriani M, Gupta R, Donahue DM. Botulinum toxin injection in neurogenic thoracic outlet syndrome: results and experience using a ultrasound-guided approach. Skeletal Radiol 2010; 39: 973–980. [DOI] [PubMed] [Google Scholar]
- 6.Finlayson HC, O’Connor RJ, Brasher PMA, et al. Botulinum toxin injection for management of thoracic outlet syndrome: a double-blind, randomized, controlled trial. Pain 2011; 152: 2023–2028. [DOI] [PubMed] [Google Scholar]
- 7.Foley J, Finlayson H, Travlos A. A review of thoracic outlet syndrome and the possible role of botulinum toxin in the treatment of this syndrome. Toxins 2012; 4: 1223–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bottros MM, AuBuchon JD, McLaughlin LN, et al. Exercise-enhanced, ultrasound-guided anterior scalene muscle/pectoralis minor muscle blocks can facilitate the diagnosis of neurogenic thoracic outlet syndrome in the high-performance overhead athlete. Am J Sports Med 2017; 45: 189–194. [DOI] [PubMed] [Google Scholar]
- 9.Sanders RJ. Recurrent neurogenic thoracic outlet syndrome stressing the importance of pectoralis minor syndrome. Vasc Endovascular Surg 2011; 45: 33–38. [DOI] [PubMed] [Google Scholar]
- 10.Ambrad-Chalela E, Thomas GI, Johansen KH. Recurrent neurogenic thoracic outlet syndrome. Am J Surg 2004; 187: 505–510. [DOI] [PubMed] [Google Scholar]
- 11.van Kampen DA, Willems W, van Beers LWAH, et al. Determination and comparison of the smallest detectable change (SDC) and the minimal important change (MIC) of four-shoulder patient-reported outcome measures (PROMs). J Orthop Surg Res 2013; 8: 40–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dawson J, Rogers K, Fitzpatrick R, et al. The Oxford shoulder score revisited. Arch Orthop Trauma Surg 2009; 129: 119–123. [DOI] [PubMed] [Google Scholar]
- 13.May S, Serpell M. Diagnosis and assessment of neuropathic pain. F1000 Med Rep 2009; 1: 76–76. [DOI] [PMC free article] [PubMed] [Google Scholar]