Abstract
Background
Olecranon fractures in the elderly have an increasing incidence. This retrospective study aims to identify the complications and survivorship of these patients.
Methods
All patients >70 years old treated for an olecranon fracture at our institution were identified between 2007 and 2019. Loss of reduction and/or metalwork loosening was recorded. Also noted were wound healing problems, deep/superficial infections, and any subsequent treatment including return to surgery and/or removal of metalwork.
Results
From a total of 177 cases, 28 presented with concomitant fractures (16%), half of which were hip fractures. The largest treatment group underwent tension band wiring (n = 82, 46%, mean age 80.8 yrs). Twenty-one of these suffered failure of fixation (26%), all requiring return to surgery. The second largest treatment group underwent plating (n = 50 28%, mean age 80.1 yrs). Four of these suffered failure of fixation (8%), all requiring return to surgery. Forty-four patients were treated non-operatively (25%, mean age 83.8 yrs). Two patients suffered other complications (4.5%). Overall 1 year survivorship was 0.82.
Discussion
Olecranon fractures in the elderly have higher than expected 1 year mortality rates. Operative management results in high complication rates, often requiring return to surgery for metalwork problems. Significant consideration of treatment options is required in this cohort.
Keywords: Olecranon fracture, tension band wire, fracture fixation, elderly
Introduction
Olecranon fractures account for approximately 10% of elbow fractures. 1 Generally these fractures have a bimodal distribution: patients in their early twenties secondary to high energy trauma, and in the elderly population. 2 Olecranon fractures in the elderly have an increasing incidence, and often present as fragility fractures secondary to low energy trauma such as a fall from standing height.3–6
The management of these fractures is often based on the degree of displacement and comminution seen on radiological imaging. Undisplaced fractures may be managed non-operatively, while various different surgical procedures for more complex fractures are described. 7 Common techniques include tension band wire (TBW) and fixation with plate and screws (ORIF). TBW is associated with complications such wire migration and loss of compression.8–10 This may occur more frequently in an elderly population. 11 Plate fixation is the preferred method in more comminuted and obliquely configured fractures, but has been associated with increased infection rates and revision surgery.12,13
Surgical decision-making may be simple when treating a young and active cohort, but in the elderly, decisions are complex and must reconcile pre-existing co-morbidities, functional demands, poor bone quality and poor physiological reserve. The associated complication rates can far exceed complication rates in a younger population with the same injury.2,10 Good function and satisfaction after non-operative treatment of displaced olecranon fractures in the elderly has been demonstrated, without the associated complications of surgery and anesthesia.2,12,13
In this study, we have identified a large cohort of consecutive olecranon fractures over the age of 70 presenting to a large UK teaching hospital. This study aims to define the complications of the surgical treatment of elderly patients with olecranon fractures.
Methods
Patients and data sources
We performed a retrospective review of consecutive olecranon fractures from a level 1 trauma centre which provides specialist services for an immediate population of 770,000 and regional specialist care for up to 5.4 million people. Cases occurred between November 2007 and February 2019. Patients were identified using clinical coding records and admission records, as well as the local trauma database. These were then cross-referenced using radiological records and case notes. Cases were followed up in local fracture clinic until discharge where possible. Regional records including death records were checked during data collection on 1 October 2019 to establish if the patient had undergone further intervention, encountered further problems or died. Mean duration of follow-up in clinic was 19 weeks (range 0 to 345 weeks).
The study design was approved by the local institutional review board.
Diagnosis and treatment
Patients with olecranon fractures occurring within the region under the remit of our healthcare trust were initially seen in the Emergency Department (ED) or a Minor Injuries Walk-in Centre (MIU). The diagnosis was made and initial management (usually analgesia and immobilisation) performed. The patient would then be referred to the trauma team. In the majority of cases, management would occur in the outpatient setting, with the patient returning to a fracture clinic in our department within a week of the injury. Patients would be examined and discussed with senior surgeons, where a treatment plan was made. The decision of whether to operate would be made by a consultant surgeon, and would be based upon patient factors (age, co-morbidities, cognitive impairment, frailty, etc.) and fracture factors (open/closed injuries, integrity of surrounding soft tissues, displacement, concomitant injuries). If surgery was required, this would usually involve a ‘day-case’ operative procedure, where the patient would return home that evening, if all was well.
Occasionally patients referred from ED or MIU would require admission to hospital: this would be for the patient’s own safety. This would generally be those in which the fall leading to the olecranon fracture could have a medical cause (e.g. myocardial infarction, stroke, etc.), or if the patient sustained other injuries. Most often, patients admitted to hospital wards would often be those deemed high risk if discharged home with an arm immobilised following olecranon fracture. This is usually those elderly patients living independently alone, with other mobility or cognitive issues. They may require inpatient admission until medical treatment and social care was complete and the patient assessed as safe for discharge.
Variables
Patient variables including sex, age, date of admission, fracture classification (Mayo Olecranon Fracture Classification 14 ), treatment method, other injuries and date of death. During follow-up, all radiographs were reviewed and appraised by the authors (by JP, GM, AY, SQ and verified by senior author PC). Complications were defined as being a change in the position of the fracture noted on the intra-operative images in subsequent radiographs (‘loss of reduction’), or the change in the position of metalwork when comparing the intra-operative images with subsequent radiographs (‘metalwork loosening’). Patients may suffer either of these complications, or may of course suffer both complications (‘loss of reduction’ and ‘metalwork loosening’). Any subsequent treatment, including return to surgery and/or removal of metalwork, as well as radiological union was recorded where possible.
Statistics
Normally distributed continuous variables were expressed as means with standard deviations (SDs) and non-normally distributed continuous variables were expressed as median values with interquartile range. Comparisons of continuous variables were performed with Welch’s t-tests, and categorical variables were compared with chi-square tests. Survival was estimated using a Kaplan–Meier method. Cases were censored when patients died prior to end of follow-up. Statistical significance was set at p < 0.05 to reduce the risk of inappropriate false positives.
Results
Patient demographics
One hundred ninety-five cases of olecranon fracture were identified during the study period. Eighteen (9.2%) patients were lost to follow-up and excluded from subsequent analysis. Mean follow-up in clinic for the remaining cohort of 177 patients was 19 weeks (range 0 to 345 weeks). Mean age (SD) of patients was 81.3 (6.1) years and 71.8% of patients were female (Table 1).
Table 1.
Demographics for all patients with olecranon fracture.
| n (%) | |
|---|---|
| Total subjects | 176 |
| Age (mean (SD)) | 81.35 (6.08) |
| Sex (%) | |
| Female | 126 (71.6) |
| Male | 50 (28.4) |
| Other injuries (%) | |
| No | 148 (84.1) |
| Yes | 28 (15.9) |
| Other injury location (%) | |
| Wrist | 6 (3.4) |
| Hip | 14 (8.0) |
| Humeral shaft | 2 (1.1) |
| Proximal humerus | 3 (1.7) |
| Pubic ramus | 0 (0.0) |
| Talus | 2 (1.1) |
SD: standard deviation.
All values represent numbers of cases and proportion in parentheses unless otherwise stated.
Concomitant fractures occurred in 28 patients presenting with an olecranon fracture (16%), of which half were hip fractures.
Fixation failure was noted in 14.2% of cases. This was catagorised into ‘loss of reduction’, occurring in one case (0.6% of total cohort) which was managed non-operatively; and ‘metalwork loosening’, which occurred in 12.5% of all cases, all of which were managed operatively. Two patients were classified as having suffered both a loss of reduction and metalwork loosening (1.1% of the total cohort, with both requiring surgical intervention; Table 2).
Table 2.
Outcomes following olecranon fracture treatment in all study patients.
| n (%) | |
|---|---|
| n | 176 |
| Fixation failure (%) | |
| No | 151 (85.8) |
| Yes | 25 (14.2) |
| Loss of reduction only (%) | |
| No | 175 (99.4) |
| Yes | 1 (0.6) |
| Non-operative management (%) | 1 (0.6) |
| Surgical management (%) | 0 (0.0) |
| Metalwork loosening only (%) | |
| No | 154 (87.5) |
| Yes | 22 (12.5) |
| Non-operative management (%) | 0 (0.0) |
| Surgical management (%) | 22 (12.5) |
| Both loss of reduction and metalwork loosening (%) | |
| No | 174 (98.9) |
| Yes | 2 (1.1) |
| Non-operative management (%) | 0 (0.0) |
| Surgical management (%) | 2 (1.1) |
| Other complication (%) | |
| No | 158 (89.8) |
| Yes | 14 (8.0) |
| Unknown | 4 (2.3) |
| Other complication details (%) | |
| Conversion to ORIF | 1 (0.6) |
| SSI | 3 (1.7) |
| Periprosthetic fracture | 1 (0.6) |
| Wound dehiscence | 1 (0.6) |
| Unknown | 2 (1.1) |
| No | 170 (96.6) |
Comparisons between treatment methods
When the cohort was split into the three treatment groups of non-operative management, open reduction internal fixation (ORIF) and TBW, age differed between treatment groups, with those treated non-operatively being substantially older (mean age 83.8 years, p < 0.05). The distribution of males and females was similar (p = 0.27, Table 3). There was no significant difference in proportion of patients sustaining a concomitant injury between each treatment group.
Table 3.
Demographics for all patients with olecranon fracture by treatment group.
| Non-operative | ORIF | TBW | p overall | |
|---|---|---|---|---|
| Total subjects | 44 | 50 | 82 | |
| Age (mean (SD)) | 83.82 (6.49) | 80.14 (5.61) | 80.77 (5.82) | 0.006 |
| Sex (%) | ||||
| Female | 33 (75.0) | 39 (78.0) | 54 (65.9) | 0.274 |
| Male | 11 (25.0) | 11 (22.0) | 28 (34.1) | |
| Other injuries (%) | ||||
| No | 38 (86.4) | 41 (82.0) | 69 (84.1) | 0.846 |
| Yes | 6 (13.6) | 9 (18.0) | 13 (15.9) | |
| Other injury location (%) | ||||
| Wrist | 0 (0.0) | 1 (11.1) | 5 (41.7) | 0.117 |
| Hip | 4 (66.7) | 4 (44.4) | 6 (50.0) | |
| Humeral shaft | 0 (0.0) | 2 (22.2) | 0 (0.0) | |
| Proximal humerus | 2 (33.3) | 1 (11.1) | 0 (0.0) | |
| Talus | 0 (0.0) | 1 (11.1) | 1 (8.3) |
SD: standard deviation; ORIF: open reduction and internal fixation; TBW: tension band wire.
All values represent numbers of cases and proportion in parentheses unless otherwise stated.
Fracture type and treatment method
The most common fracture type was 2a (66 of 176 (37.5%)) followed by 58 (33.0%) 2b fractures, 23 (13.2%) 1a fractures, 13 (7.4%) 3b fractures, 9 (5.1%) 1b fractures and 7 (4.0%) 3a fractures.
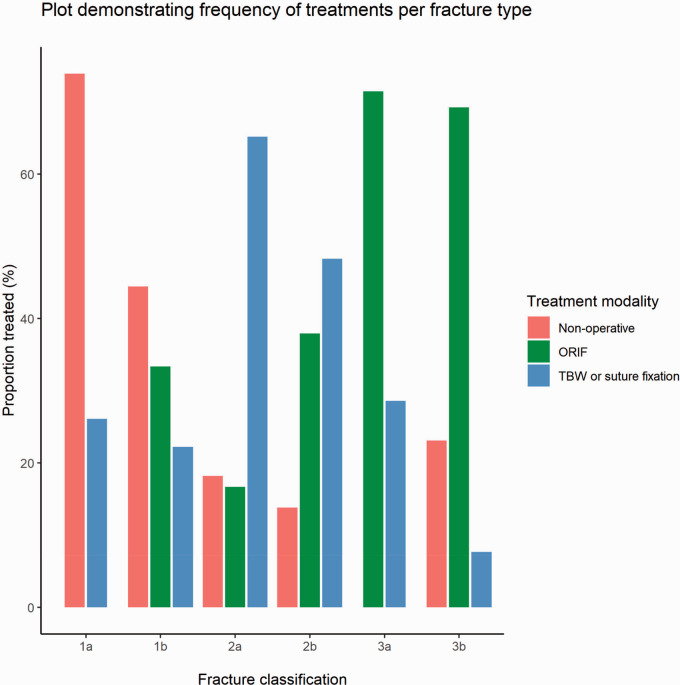
ORIF was most commonly performed in displaced comminuted fractures (2b) and fractures associated with instability (3a and 3b). TBW was most commonly performed in displaced simple fractures (2a). Most undisplaced fractures were treated non-operatively (Figure 1).
Figure 1.
Histogram demonstrating the treatment methods for each fracture type in the whole cohort.
Twenty-eight (48.3%) displaced comminuted (2b) fractures were treated with TBW, 22 (38.0%) were treated with ORIF and 8 (13.8%) were treated non-operatively (Figure 1).
Complications by treatment method
In the groups undergoing surgery (TBW and ORIF combined), 25 (18.9%) patients suffered a failure of fixation of any type, and all 25 (100.0%) required a return to surgery (Table 4). No patients in the ‘non-operative’ group went on to have any further surgical intervention, but one patient in this ‘non-operative’ group subsequently sustained an ipsilateral humeral shaft fracture.
Table 4.
Complications following non-operative versus surgical management in all study patients.
| Non-operative | Surgical | p overall | |
|---|---|---|---|
| n | 44 | 132 | |
| Fixation failure (%) | |||
| No | 44 (100.0) | 107 (81.1) | 0.004 |
| Yes | 0 (0.0) | 25 (18.9) | |
| Loss of reduction only (%) | |||
| No | 44 (100.0) | 131 (99.2) | 1 |
| Yes | 0 (0.0) | 1 (0.8) | |
| Non-operative management (%) | 0 (0.0) | 0 (0.0) | – |
| Surgical management (%) | 0 (0.0) | 1 (0.8) | 1 |
| Metalwork loosening only (%) | |||
| No | 44 (100.0) | 110 (83.3) | 0.008 |
| Yes | 0 (0.0) | 22 (16.7) | |
| Non-operative management (%) | 0 (0.0) | 0 (0.0) | - |
| Surgical management (%) | 0 (0.0) | 22 (16.7) | 0.008 |
| Both loss of reduction and metal work loosening (%) | |||
| No | 44 (100.0) | 130 (98.5) | 1 |
| Yes | 0 (0.0) | 2 (1.5) | |
| Non-operative management (%) | 0 (0.0) | 0 (0.0) | – |
| Surgical management (%) | 0 (0.0) | 2 (1.5) | 1 |
| Other complication (%) | |||
| No | 39 (88.6) | 119 (90.2) | 0.045 |
| Yes | 2 (4.5) | 12 (9.1) | |
| Unknown | 3 (6.8) | 1 (0.8) | |
| Other complication details (%) | |||
| Conversion to ORIF | 0 (0.0) | 1 (8.3) | 0.082 |
| SSI | 0 (0.0) | 3 (25.0) | |
| Humeral fracture | 1 (50.0) | 0 (0.0) | |
| Malunion | 1 (50.0) | 0 (0.0) | |
| Nonunion | 0 (0.0) | 1 (8.3) | |
| Periprosthetic fracture | 0 (0.0) | 1 (8.3) | |
| Stiffness | 0 (0.0) | 1 (8.3) | |
| Wound dehiscence | 0 (0.0) | 3 (25.0) | |
| In hospital death (%) | |||
| No | 40 (90.9) | 130 (98.5) | 0.055 |
| Yes | 4 (9.1) | 2 (1.5) |
SD: standard deviation; ORIF: open reduction and internal fixation; TBW: tension band wire; SSI: surgical site infection.
– indicates no test performed.
All values represent numbers of cases and proportion in parentheses unless otherwise stated. Fixation failure describes total number of cases where loss of reduction or metal work loosening or both loss of reduction and metal work loosening occur.
A failure of fixation differed by surgical treatment group, occurring in 25.6% of those patients undergoing TBW, and in 8.0% of those undergoing ORIF (p < 0.05, Table 5). Metal work loosening was the most common reason for failure and occurred following 22% of TBW treatments: it also accounted for all fixation failures following ORIF (p = 0.07).
Table 5.
Complications following surgical olecranon fracture treatment in all study patients.
| ORIF | TBW | p overall | |
|---|---|---|---|
| n | 50 | 82 | |
| Fixation failure (%) | |||
| No | 46 (92.0) | 61 (74.4) | 0.023 |
| Yes | 4 (8.0) | 21 (25.6) | |
| Loss of reduction only (%) | |||
| No | 50 (100.0) | 81 (98.8) | 1 |
| Yes | 0 (0.0) | 1 (1.2) | |
| Non-operative management (%) | 0 (0.0) | 0 (0.0) | – |
| Surgical management (%) | 0 (0.0) | 1 (1.2) | 1 |
| Metalwork loosening only (%) | |||
| No | 46 (92.0) | 64 (78.0) | 0.065 |
| Yes | 4 (8.0) | 18 (22.0) | |
| Non-operative management (%) | 0 (0.0) | 0 (0.0) | – |
| Surgical management (%) | 4 (8.0) | 18 (22.0) | 0.065 |
| Both loss of reduction and metal work loosening (%) | |||
| No | 50 (100.0) | 80 (97.6) | 0.705 |
| Yes | 0 (0.0) | 2 (2.4) | |
| Non-operative management (%) | 0 (0.0) | 0 (0.0) | – |
| Surgical management (%) | 0 (0.0) | 2 (2.4) | 0.705 |
| Other complication (%) | |||
| No | 44 (88.0) | 75 (91.5) | 0.416 |
| Yes | 5 (10.0) | 7 (8.5) | |
| Unknown | 1 (2.0) | 0 (0.0) | |
| Other complication details (%) | |||
| Conversion to orif | 0 (0.0) | 1 (14.3) | 0.16 |
| SSI | 0 (0.0) | 3 (42.9) | |
| Periprosthetic fracture | 1 (20.0) | 0 (0.0) | |
| Stiffness | 0 (0.0) | 2 (28.6) | |
| Wound dehiscence | 1 (20.0) | 0 (0.0) | |
| Unknown | 2 (40.0) | 1 (14.3) | |
| In hospital death (%) | |||
| No | 50 (100.0) | 80 (97.6) | 0.705 |
| Yes | 0 (0.0) | 2 (2.4) |
SD: standard deviation; ORIF: open reduction and internal fixation; TBW: tension band wire and SSI is surgical site infection.
– indicates no test performed.
All values represent numbers of cases and proportion in parentheses unless otherwise stated. Fixation failure describes total number of cases where loss of reduction or metal work loosening or both loss of reduction and metal work loosening occur.
Other complications were more frequent following ORIF than TBW, but the difference did not reach statistical significance (10.0% versus 8.5% respectively, p = 0.16).
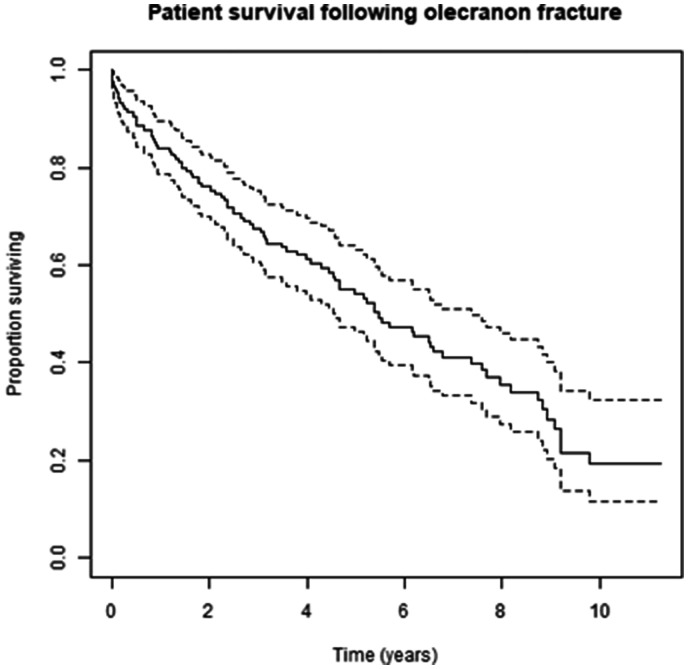
Patient survival
Patient survival following olecranon fracture was estimated to be 0.96 (95% CI 0.93 to 0.99) at 30 days and 0.84 (95% CI 0.79 to 0.90) at one year (Table 6 and Figure 2).
Table 6.
Kaplan–Meier estimates of patient survival following olecranon fracture.
| Time (days) | Number at risk | Deaths | Proportion surviving | Lower 95% CI | Upper 95% CI |
|---|---|---|---|---|---|
| 30 | 170 | 7 | 0.96 | 0.93 | 0.99 |
| 90 | 164 | 7 | 0.92 | 0.88 | 0.96 |
| 120 | 162 | 1 | 0.92 | 0.88 | 0.96 |
| 365 | 142 | 13 | 0.84 | 0.79 | 0.9 |
CI: confidence interval estimate; ORIF: open reduction and internal fixation; TBW: tension band wire.
Figure 2.
Kaplan–Meier survivorship following olecranon fracture.
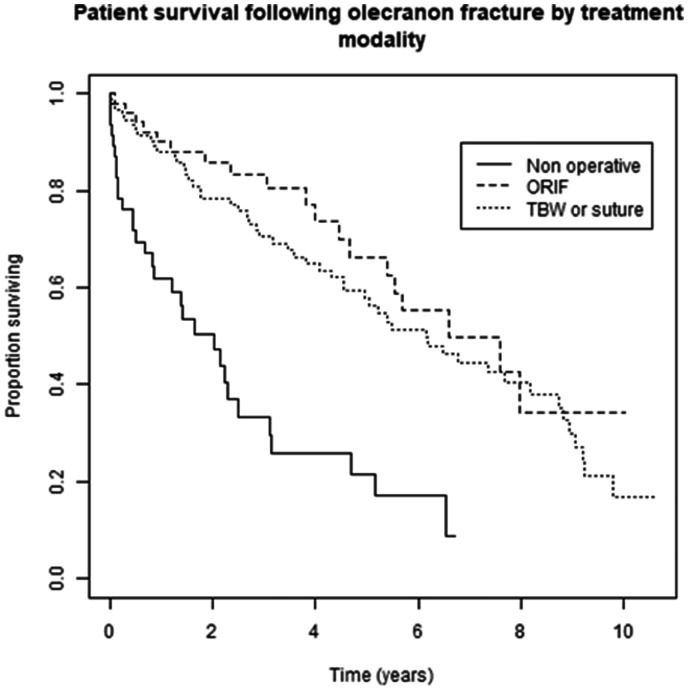
Overall survival of patients undergoing non-operative treatment was significantly worse than both ORIF (p < 0.01) and TBW (p < 0.01). Survival between patients treated with ORIF and TBW did not differ (p = 0.3; Table 7 and Figure 3).
Table 7.
Kaplan–Meier estimates of patient survival following olecranon fracture by treatment group.
| Time (days) | Number at risk | Deaths | Proportion surviving | Lower 95% CI | Upper 95% CI |
|---|---|---|---|---|---|
| Non-operative | |||||
| 30 | 41 | 5 | 0.89 | 0.81 | 0.99 |
| 90 | 36 | 6 | 0.76 | 0.65 | 0.90 |
| 120 | 35 | 0 | 0.76 | 0.65 | 0.90 |
| 365 | 23 | 6 | 0.62 | 0.49 | 0.78 |
| ORIF | |||||
| 30 | 52 | 1 | 0.98 | 0.94 | 1.00 |
| 90 | 51 | 0 | 0.98 | 0.94 | 1.00 |
| 120 | 49 | 1 | 0.96 | 0.91 | 1.00 |
| 365 | 44 | 3 | 0.90 | 0.82 | 0.99 |
| TBW or suture | |||||
| 30 | 91 | 3 | 0.97 | 0.93 | 1.00 |
| 90 | 88 | 1 | 0.96 | 0.92 | 1.00 |
| 120 | 87 | 1 | 0.95 | 0.90 | 0.99 |
| 365 | 80 | 6 | 0.88 | 0.82 | 0.95 |
CI: confidence interval estimate; ORIF: open reduction and internal fixation; TBW; tension band wire.
Figure 3.
Kaplan–Meier plot demonstrating the survival of patients in each treatment group following admission.
Discussion
This study demonstrates high complications rates in patients >70 years old undergoing surgery for an olecranon fracture, with 18.9% suffering a failure of fixation, and of these all required a return to surgery. Most complications were related to fixation failure, metal work problems and non-union: wound healing problems and SSI were low.
To our knowledge, this study represents the largest cohort of olecranon fractures in the elderly. Previous studies have also demonstrated high rates of fixation failure in older patients with olecranon fractures.5,11,15 Fixation failure in this age group may be related to the biomechanics of olecranon fractures, reduced adherence to any movement restriction in rehabilitation and poor bone quality. Biomechanically, fractures in proximity to the centre of rotation of the elbow joint undergo distraction during elbow flexion, which is not conducive to healing. Compliance with any restriction of movement in post-operative rehabilitation may also be a challenge in older patients. Finally, in this older population, poor bone quality provides significant challenge for surgical fixation, both at the time of fixation and until union. This coupled with the possibility of poor surgical technique or incorrect decision-making in the method of fixation creates an environment where, without due care and attention, surgical failure could frequently occur. Further analysis is required to determine the surgical factors that may relate to fixation failure.
Our analysis of concomitant injuries with olecranon fracture presentation demonstrated that over 15% of patients presented with another fracture at the same time injury, with 50% of those being a hip fracture. To our knowledge, this is the first study to comment on simultaneous injuries. These multiply injured patients can have significant challenges in rehabilitation, especially with a simultaneous lower limb injury. They may find difficulty with rehabilitation, which may also in part explain treatment failure.
To our knowledge, this is the first study to examine mortality rates following olecranon fracture, finding a 4% 30 day mortality, and a 16% mortality rate at 1 year. In 2018, the Office for National Statistics’ period mortality rates for the UK population were estimated to be between 1.1% and 9% for patients aged over 70 years old using a similar age spread to the current study, and found that people aged 65 years in the UK in 2018 can expect to live on average a further 19.9 years for males and 22.0 years for females. 16 In comparison to hip fracture, the 2019 UK National Hip Fracture Database annual report found a 30-day mortality rate of 6.1%, 17 and a 1 year mortality rate following hip fracture of 33%.17,18 One previous study attempted to calculate ‘excess mortality’ following specific fractures in the Danish population aged >50 years: they found that excess mortality was observed following all proximal and lower leg fractures, with hip fractures predictably the highest excess mortality of 33% in men, and 20% in women. 19 The authors did not record rates specifically for olecranon fractures, but for humerus fractures they found 5–10% excess rate, and for forearm fractures 2%. Though the cause of mortality cannot be accurately attributed and is unlikely to result directly from an olecranon fracture, these fractures are likely to be a surrogate for pronounced general frailty and other underlying medical co-morbidities.
We demonstrated a greater mortality in patients undergoing non-operative management over the follow-up period. This shows that our decision-making regarding surgical intervention often reasonably predicted those more frail patients. In such instances, patients may be managed non-operatively as the risks of surgery outweigh the potential benefits of no-surgery, with previous studies demonstrating reasonable functional outcomes without the risks of surgical intervention.2,3,5,12–15,20 The observation demonstrates the underlying mortality of patients which are not fit or suitable for surgery.
This demonstrates that decision-making, as well as technical skill, is also necessary for successful surgical intervention. With that in mind, we were surprised to find that just under half (48.3%) of displaced comminuted fractures (2b classification) in our cohort were treated with TBW. Historically, if comminution is noted with an olecranon fracture, convention has been to avoid TBW and perform ORIF, as advocated by the AO group, 21 since compression across a comminuted fracture site using TBW will lead to malalignment, specifically important if the olecranon fossa articular surface is involved.
Limitations
A limitation of our series is the retrospective nature of the data collection, leading to issues with loss of follow-up and access to medical information in a small proportion of patients. As a retrospective study, causality of complications or survivorship cannot be determined.
It is not possible to ascertain from this study whether patients with a simultaneous hip fracture who underwent operative fixation of their olecranon fracture were able to mobilise sooner. Future research should seek to address whether fixation of olecranon fractures in those with a requirement for mobility aids is of any benefit versus non-operative management. It is possible that complications requiring repeated operative intervention are associated with an increased risk of complication and mortality in this frail cohort. Unfortunately, this study was not able to draw useful conclusions to this question but the question warrants further dedicated clinical study.
We did not analyse functional outcomes. Previous studies have demonstrated asymptomatic non-union may not lead to a functional deficit.12–15,20 Likewise, though we have measured the complications of fracture displacement and metalwork problems, it may be that these too do not affect function. The follow-up in this study is representative of normal practice in our hospital and as a result we were unable to quantify rates of union or long-term functional outcome.
The definition of ‘elderly’ varies greatly in the literature. In the UK, the National Institute for Health and Care Excellence provides guidelines of falls in ‘older people’, quantifying this at 65 years or older. 22 In UK orthopaedic practice, the ‘Fragility Hip Fracture Best Practice Tariff’ requires a patient to be aged 60 years or older to qualify. 23 However, previous publications on olecranon fractures in the elderly have used 70 years 2,11,24 and 75 years. 5,15 We chose 70 years as our ‘cut off’ as this is the age a patient admitted to our institution with an orthopaedic injury would also receive specialist orthogeriatric input. However, it has been previously acknowledged that such a ‘cut-off’ is a crude marker of biological age. 5
Conclusions
Olecranon fractures in the elderly have high mortality rates at a year following injury, and carry high rates of complications when operatively managed. Significant thought should be given to the management options of a patient presenting with this injury, with non-operative management providing fewer complications than surgery.
Acknowledgements
The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: PC has a contract for research with the Leeds Biomedical Research Centre (BRC).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This article presents independent research supported by the National Institute for Health Research (NIHR) Leeds Biomedical Research Centre (BRC).
Ethical approval: This retrospective trial was approved by the Trauma and Orthopaedic Departmental Audit and Quality Improvement committee.
Informed Consent: No consent was required for this retrospective.
Guarantor: PC.
Contributorship: PC, RW and JL conceived the study. JP and PC researched the literature. PC, RL and JL identified the patients. RL, SQ, GM, AY and PC reviewed medical records and performed analysis of radiographs. PC, RW and JL organised and performed the statistical analysis of the data collected. JP, SQ, JL and PC wrote the first draft manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript. PC, JP, GM and JL provided the further analysis and response to the reviewers following initial review by the journal.
ORCID iDs
G Mohrir https://orcid.org/0000-0002-9653-2575
P Cowling https://orcid.org/0000-0003-3656-8549
References
- 1.Veillette CJH, Steinmann SP. Olecranon fractures. Orthop Clin North Am 2008; 39: 229–236. [DOI] [PubMed] [Google Scholar]
- 2.Gallucci GL, Piuzzi NS, Slullitel PA, et al. Non-surgical functional treatment for displaced olecranon fractures in the elderly. Bone Joint J 2014; 96-B: 530–534. [DOI] [PubMed] [Google Scholar]
- 3.Duckworth AD, Clement ND, Aitken SA, et al. The epidemiology of fractures of the proximal ulna. Injury 2012; 43: 343–346. [DOI] [PubMed] [Google Scholar]
- 4.Flinterman HJA, Doornberg JN, Guitton TG, et al. Long-term outcome of displaced, transverse, noncomminuted olecranon fractures. Clin Orthop Relat Res 2014; 472: 1955–1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duckworth AD, Clement ND, McEachan JE, et al. Prospective randomized trial of non-operative versus operative management of olecranon fractures in the elderly. Bone Joint J 2017; 99-B: 964–972. [DOI] [PubMed] [Google Scholar]
- 6.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury 2006; 37: 691–697. [DOI] [PubMed] [Google Scholar]
- 7.Newman SDS, Mauffrey C, Krikler S. Olecranon fractures. Injury 2009; 40: 575–581. [DOI] [PubMed] [Google Scholar]
- 8.Saeed ZM, Trickett RW, Yewlett AD, et al. Factors influencing k-wire migration in tension-band wiring of olecranon fractures. J Shoulder Elbow Surg 2014; 23: 1181–1186. [DOI] [PubMed] [Google Scholar]
- 9.Van der Linden SC, van Kampen A, Jaarsma RL. K-wire position in tension-band wiring technique affects stability of wires and long-term outcome in surgical treatment of olecranon fractures. J Shoulder Elbow Surg 2012; 21: 405–411. [DOI] [PubMed] [Google Scholar]
- 10.Romero J, Miran A, Jensen CH. Complications and re-operation after tension band wiring of olecranon fractures. J Orthop Sci 2000; 5: 318–320. [DOI] [PubMed] [Google Scholar]
- 11.Umer S, Vioreanu M, Baker J, et al. Olecranon fractures in the elderly: is tension band wiring the right treatment? Injury Extra 2011; 42: 122–122. [Google Scholar]
- 12.Parker MJ, Richmond PW, Andrew TA, et al. A review of displaced olecranon fractures treated conservatively. J R Coll Surg Edinb 1990; 35: 392–394. [PubMed] [Google Scholar]
- 13.Bruinsma W, Lindenhovius AL, McKee MD, et al. Non-union of non- operatively treated displaced olecranon fractures. Shoulder Elbow 2012; 4: 273–276. [Google Scholar]
- 14.Morrey BF and Adams RA. Fractures of the proximal ulna and olecranon. In: The elbow and its disorders. Philadelphia, PA: WB Saunders, 1993, pp.405–428.
- 15.Marot V, Bayle-Iniguez X, Cavaignac E, et al. Results of non-operative treatment of olecranon fracture in over 75-year olds. Orthop Traumatol Surg Res 2018; 104: 79–82. [DOI] [PubMed] [Google Scholar]
- 16.The Office for National Statistics. Past and projected period and cohort life tables. 2018-based, UK: 1981 to 2068, https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/lifeexpectancies/bulletins/pastandprojecteddatafromtheperiodandcohortlifetables/latest (2019, accessed 14 August 2020).
- 17.Royal College of Physicians. National Hip Fracture Database annual report 2019. London: RCP, 2019.
- 18.Roche JJW, Wenn RT, Sahota O, et al. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 2005; 331: 1374–1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tran T, Bliuc D, Hansen L, et al. Persistence of excessive mortality following individual non-hip fractures: a relative survival analysis. J Clin Endocrinol Metab 2018; 103: 3205–3214. [DOI] [PubMed] [Google Scholar]
- 20.Duckworth AD, Bugler KE, Clement ND, et al. Nonoperative management of displaced olecranon fractures in low-demand elderly patients. J Bone Joint Surg Am 2014; 96: 67–72. [DOI] [PubMed] [Google Scholar]
- 21.AO Surgical Reference, https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/proximal-forearm/ulna-articular-olecranon (accessed 12 August 2020).
- 22.Falls in older people: assessing risk and prevention. NICE Clinical guideline [CG161], National Institute for Health and Care Excellence, 2013. [PubMed]
- 23.2019/20 National Tariff Payment System: Best Practice Tariff (BPT) for Fragility Hip Fracture. National hip fracture database, https://www.nhfd.co.uk/20/hipfractureR.nsf/0/9b0c5ea2e986ff56802577af0046b1df/$FILE/Best%20Practice%20Tariff%20User%20Guide.pdf (accessed 4 July 2020).
- 24.Veras Del Monte L, Sirera Vercher M, Busquets, Net R, et al. Conservative treatment of displaced fractures of the olecranon in the elderly. Injury 1999; 30: 105–110. [DOI] [PubMed] [Google Scholar]