Abstract
Purpose of Review
The COVID-19 pandemic is associated with increased levels of stress, anxiety and depression in the population. These are associated with unhealthy eating patterns and sedentary behaviour. In turn, this may increase risk of obesity or aggravate it. This narrative review discusses the link between adverse mental health states and weight related behaviours. We present emerging evidence for this phenomenon during the COVID-19 pandemic in individuals with and without pre-existing obesity.
Recent Findings
A sizeable proportion of the population exhibits deterioration in mental health during the pandemic and those affected often report unhealthy weight-related behaviours such as “junk food” consumption and physical inactivity. Women, individuals with obesity, and those with pre-existing mental health conditions seem to be particularly at risk for overeating in response to stress (i.e. emotional eating). A number of psychological interventions including cognitive behavioural therapy and self-compassion may be effective in improving mental health and emotional eating patterns among the general population and particularly in individuals living with obesity.
Summary
There is a need to complement efforts to improve mental health in the general population during the COVID-19 pandemic with targeted action to improve physical activity levels and healthy eating particularly among groups at-risk. This may be achieved by reducing disruptions to specialist and primary healthcare services and facilitating access to psychological interventions that address stress-related eating behaviours. Additional studies that examine such interventions, especially those that are delivered remotely, are urgently needed.
Keywords: Obesity, Weight, COVID-19, Pandemic, Mental health, Stress, Emotional eating
Introduction
The COVID-19 pandemic caused unprecedented changes in people’s lives. Public health measures to control the infection led to widespread closures of education, workplace, commercial and healthcare organizations. Many people transitioned to working from home and children were unable to attend school for extended periods of time. “Stay at home” orders prevented regular social interactions between individuals, extended family and community members. Healthcare systems redeployed resources to support acute hospital care limiting access to primary and specialist care. Remaining healthcare services transitioned to telemedicine thus reducing availability of support [1].
The breakdown of normal daily routine coupled with limited availability of social support contributed to increased levels of depression and anxiety among the public [2]. Individuals who were facing greater adversity such as those who suffered loss of employment, those deemed at high-risk for a severe COVID-19 infection and those with pre-existing mental health conditions often showed higher levels of depression and anxiety compared with the general population [3–5].
Weight-related behaviours including physical activity and a high-quality diet are negatively associated with poor mental health [6, 7]. It is therefore expected that the pandemic will adversely affect health behaviours especially among those who experience high levels of stress, social isolation, health worries, as well as symptoms of depression and anxiety. While it is important to explore changes in weight-related behaviours during the pandemic among the general population, it is of interest to examine the effect on individuals with pre-existing obesity. These individuals have high rates of co-occurring mental health conditions [8•] and are therefore at risk for worsening of both their mental and physical health during these difficult times. While this review focuses on the propensity for weight gain among individuals who experience poor mental health during the pandemic, we acknowledge that additional factors play a contributing role (e.g. medications, genetics). This narrative review aims to (1) discuss the effect of the pandemic and the societal measures to limit its spread on the mental health of the general population and people with obesity; (2) describe the interplay between poor mental health (e.g. depression, anxiety, stress) and weight-related behaviours in the general population and in people with obesity; (3) present evidence on stress eating as a maladaptive coping strategy during the pandemic and (4) suggest strategies to mitigate stress-induced unhealthy behaviours among the population and people with obesity. This knowledge synthesis identifies priority groups in the general population in addition to individuals with obesity that may benefit from psychological support to reduce stress levels at this time which in turn may improve weight-related behaviours and prevent weight gain.
Obesity Under the Spotlight During COVID-19
Early reports during the initial wave of the COVID-19 pandemic indicated that certain patient characteristics were associated with greater morbidity and mortality from the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [9]. Older age, male sex, tobacco use and the presence of chronic medical conditions including diabetes and respiratory conditions were the most prevalent documented risk factors [10]. In addition, obesity (defined as body mass index-BMI ≥ 30 kg/m2) has also been noted as a determinant of adverse COVID-19 outcomes and a meta-analyses of retrospective cohort studies found it to be a risk factor for intensive care unit admission (OR = 1.21, CI: 1.00–1.46), mechanical ventilation (OR = 2.05, CI: 1.16–3.64) and death (OR = 1.37 (CI: 1.06–1.75) [11, 12].
The mechanisms that link obesity with poor COVID-19 outcomes are only partially understood [13]. It has been suggested that both obesity and severe COVID-19 share an exaggerated inflammatory response [14] and also that certain genetic factors predispose to both obesity and a severe course of COVID infection [15]. As such, the US Centers for Disease Control and Prevention included obesity in the list of high-risk criteria for a severe disease [16]. Noteworthy, the risk for a severe COVID-19 infection among individuals with obesity appears to be reversible upon weight loss. In a case control study from the Cleveland Clinic in the USA, post bariatric surgery individuals who exhibited an improved metabolic profile due to weight loss had a lower risk for a severe COVID-19 infection compared with controls matched with individuals’ pre-bariatric weight [17].
Fear of falling ill with COVID-19 has affected many in the general population but those who belong to high-risk groups may be particularly worried or anxious. A qualitative study found that individuals with obesity were especially frightened about contracting the virus due to potential unfavourable outcomes and fear of dying [18]. Another study found exaggerated COVID-19 health-related worries among individuals with obesity which was also linked to a hesitancy towards COVID-19 vaccination [19]. Many were concerned because they had co-occurring risk factors for a severe COVID infection such as lung/breathing problems and diabetes which are common in people with obesity [18]. In turn, this led some to completely avoid leaving their home and disengage from social contacts in their neighbourhood, potentially increasing the risk of mental health deterioration, and also of weight gain [18]. Health worries about contracting COVID-19 are only one of many worries and stressors experienced by the public in a response to the pandemic, which may lead to a propensity for weight gain.
The COVID-19 Pandemic as the “Perfect Storm” to Increase Stress in the Population
The pandemic and the resultant societal response to limit the spread of the virus have disrupted all aspects of our lives. Public health orders to socially distance and avoid gatherings led to widespread closures of educational institutions as well as “non-essential” workplaces and businesses such as leisure and entertainment venues, fitness facilities and community organizations. “Stay at home” orders issued locally to reduce the rate of COVID transmission caused people to be confined to their homes for periods of weeks to months at a time. Many experience social isolation and loneliness due to the inability to meet friends or family in social gatherings [20].
The economic impact of the pandemic is far-reaching. These disruptions led to job loss and limited employment opportunities, resulting in significant financial stressors [21]. Those able to work from home may face challenges due to the additional stress of managing work as well as supporting dependent children in home-schooling [22].
Healthcare services redeployed resources to acute hospital care to treat those infected by the virus. Access to routine and preventative health services is reduced and as a result, patients have limited support with potential deleterious effects on physical and mental health. For instance, a study of post-bariatric patients in Spain found that those who did not visit the bariatric clinic during “lock down”, compared to those who did, were more likely to gain weight [23]. Also, abrupt transition from in-person care to telemedicine comes with challenges, especially for complex patients who are accustomed to high intensity face-to-face support [24], leaving many with unmet health needs.
The excess in stressors accompanied by paucity of support may worsen mental health most commonly expressed as an increase in symptoms of depression and anxiety. A number of community-based surveys found that the levels of depression and anxiety have been higher during the pandemic compared with pre-pandemic samples. For example, one survey found that 22% vs. 9% of women and 17% vs. 5% of men reported a moderate to high level of depressive symptoms during as compared to before the pandemic [2] and another found more than a 3-fold increase in the prevalence of depressive symptoms [25]. Looking at individual differences, studies noted that those who identified belonging to a COVID-19 risk group had higher levels of depression and anxiety [4]. Also, individuals who experienced greater disruptions in their day-to-day lives such as loss of employment were also at risk for poor mental health [5]. Lastly, both women and those with pre-existing mental health conditions reported worsening of mental well-being during the pandemic above and beyond that seen in the general population [3].
Mental Well-Being During the Pandemic and Change in Weight-Related Behaviours
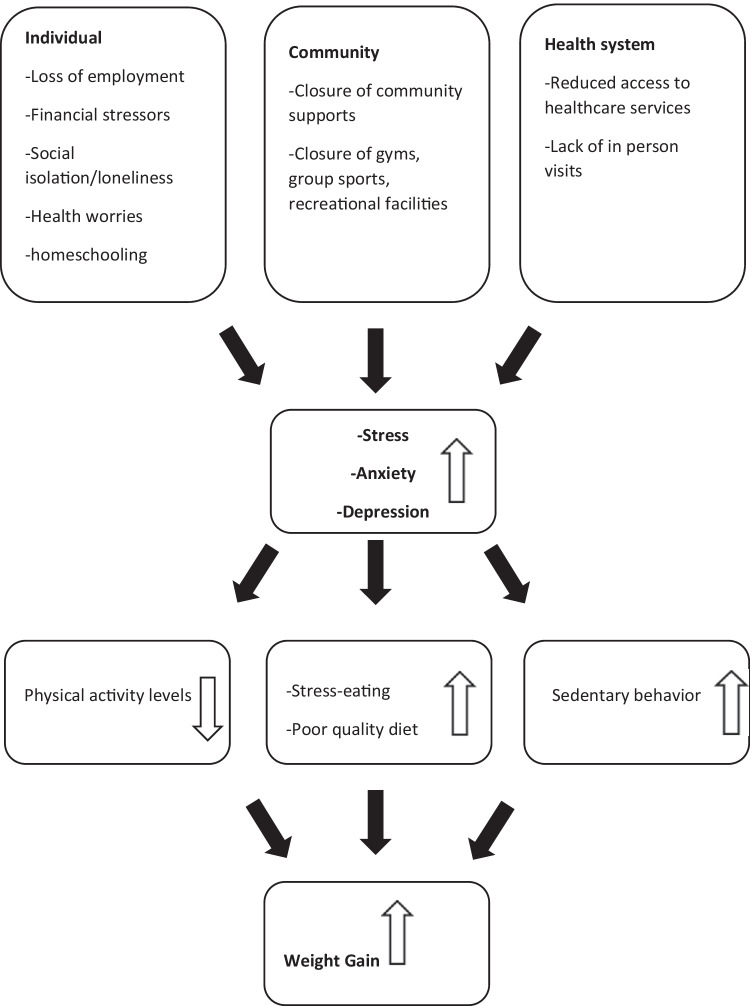
The pandemic and public health measures to limit the spread of COVID-19 are associated with high levels of anxiety and depression as well as stress in the population. Poor mental health and stress are conducive to unhealthy weight-related behaviours [6]. Evidence suggests a positive association between stress and low levels of physical activity [26•]. Particularly, prior studies pointed out to the deleterious effect of social isolation and loneliness on levels of physical activity [7]. Therefore, loneliness, aggravated by the pandemic, is likely to be a barrier for exercise. Similarly, an abundance of evidence supports the link between stress and unhealthy eating habits [27, 28]. The effects of stress on eating behaviour are further exacerbated during pandemic times due to additional “down time” spent at home in the presence of “food stockpiling” which increased opportunities for snacking [22] (Fig. 1). Moreover, stress positively correlates with sleep disturbances [29]. Sleep of low quality is linked with obesity, low levels of physical activity and metabolic dysregulation [30].
Fig. 1.
The relationship between the effects of the pandemic, mental well-being and weight-related behaviours
Change in Weight-Related Behaviours in the General Population
Interestingly, not everyone responded in the same way to COVID-19 public health restrictions. A study of UK adults during “lock down” months conducted to assess its effect on weight-related behaviours found a wide variability in reported behaviours [31]. While approximately 40% of all participants decreased their exercise levels, a further 45% reported increasing it. Similar proportions of participants (18%) reported either a decrease or an increase in eating a balanced diet. A longitudinal study from France also found opposing trends where some individuals reported an improvement in their diet quality (due to eating home-cooked meals) while others reported a decrease in diet quality (due to snacking of palatable foods) [32]. When examining characteristics of the groups who exhibited unfavourable weight-related behaviours, it was more likely to occur among those with lower education levels, greater medical co-morbidities, those with a BMI higher than 35 kg/m2 and among people experiencing poor mental health [31].
A Canadian survey noted variability for “junk food” consumption with 25% vs. 15% of respondents reporting an increase vs. decrease in intake, respectively [33]. Yet, the vast majority of respondents increased time spent in sedentary behaviours with 62% and 66% reporting additional TV watching and internet surfing, respectively. Notably, those who had an increase in unhealthy behaviours were more likely to report having been adversely impacted by the pandemic. These associations were more pronounced among women. A US study found that women experiencing financial stressors such as trouble paying bills were 32% more likely to eat an unhealthful diet and 37% less likely to exercise compared to women without financial stressors [34].
These results are not surprising, as past literature described a link between stressful events, especially those who undermine economic stability, and change in health behaviours including poor diet and low levels of physical activity, which are likely to be mediated through poor mental health [6]. Vulnerability of women to the ill-effects economic instability has also been reported elsewhere [35] and is closely tied to pre-pandemic socioeconomic disparities between men and women.
Similar to change in other weight-related behaviours, authors found that individuals either increased or decreased their sleep duration during the pandemic [36]. In particular, negative mood was associated with poor sleep quality in a UK study, which was conducted during “lock down” [37]. Hence, together with changes in physical activity and healthy eating, sleep is another weight-related behaviour that was adversely affected by changes brought about by the pandemic.
Change in Weight-Related Behaviours in People with Obesity
A link between unhealthy eating habits and unpleasant emotions (e.g. fear, loneliness, sadness) exists in many individuals with obesity and at times predates the onset of obesity [38]. It is one of the reasons for increased rates of obesity in individuals with depression, especially if the depression is untreated [8]. It can be expected therefore that the stressors brought about by the pandemic will elicit “emotional eating” in this group. Indeed, surveys of persons with obesity demonstrated greater percentages of change in weight-promoting behaviours during COVID-19 compared to that seen in the general public. For example, 63% ate in response to stress and 53% increased food stockpiling thus finding it harder to adhere with diet plans [39]. A decrease in physical activity is also known to occur in relation to low mood/stress [40]. Indeed, half of individuals with obesity noted that they reduced their exercise duration compared with only 17% who increased it [39]. The changes noted to eating and exercise behaviours were in the context of heightened mood symptoms in the sample with depression, anxiety and sleep disturbances reported by 81%, 64% and 62%, respectively. An Italian study documented the reasons given by individuals with obesity for change in weight-related behaviours to be boredom/social isolation (36%), mood symptoms (34%) and the continuous availability of foods (19%) [41]. This underscored the psychological as well as social and environmental aspects of weight-related habits and highlights why the conditions created by the COVID pandemic may be particularly challenging for those with pre-existing vulnerabilities.
As described previously, individuals with obesity may exhibit greater health worries during COVID-19 as they belong to a high-risk group. When surveyed, more than two thirds of individuals with obesity feared getting infected with COVID-19 [42]. Those with heightened mood symptoms including fear of infection had unfavourable changes in weight-related behaviours. Half of the respondents reported weight gain during “lock down” and mood symptoms mediated the association between pandemic stress and weight-promoting behaviours [42]. This is in line with prior reports that document the complex relationship between adverse psychosocial conditions (e.g. anxiety, depression, loneliness) and weigh-related behaviours (e.g. physical activity, healthy diet) [6, 7].
Eating in Response to Pandemic-Related Stress
“Stress eating” is commonly defined as episodic eating of foods with a high caloric content that are rich in fat and sugar in response to stress [43]. The consumption of calorie-dense foods is known to activate brain reward centres yielding a pleasurable feeling that alleviates stress or unpleasant emotions [44]. With repeated exposure of the brain to episodes of stress eating, a sensitization of the reward centre to palatable foods occurs. In turn, the consumption of palatable foods is particularly reinforcing in times of stress. This is manifested by anticipation or craving for high-calorie foods during stressful events which leads to the behaviour of “stress eating” [27]. This is further compounded by the inhibitory effects of acute and chronic stress on the pre-frontal cortex, the brain area responsible for behaviour control [45]. Even though palatable foods can improve negative mood, it can only do so momentarily. Yet, many individuals misattribute the effects of “comfort food” to have a long-lasting effect [46].
Stress-eating has been implicated in both the pathogenesis and aggravation of obesity [47]. It is common in the general population, with an estimated 40% of adults increasing their eating in response to stress [48]. Certain groups are at risk and the literature indicates that women and people who are already have obesity are more likely to manage minor and major stressful events with eating [49••]. It is therefore critical to examine the influence of COVID and its related stressors on stress eating and identify groups who are at risk of harm.
A population-based study conducted in Norway examined the relationship between global psychological distress and pandemic-specific worries with emotional eating during the pandemic [50•]. The study found that those with above vs. below average psychological distress were over 4 times more likely to report emotional-eating episodes. This was followed by financial stressors as a predictor of emotional eating (OR 1.7, CI 1.5–1.9) and health worries (OR 1.3, CI 1.2–1.5). Similar findings were reported in samples from the UK [51] and Italy [52]. The latter study also supported previous research that found those with a high BMI tend to respond to adverse emotional stimuli with overeating [53].
Groups who experience socioeconomic disadvantage are also prone to experience elevation in stress levels during and following the pandemic due to low social capital and limited financial means to endure pandemic-related hardships. A Canadian study found that people who reported that the pandemic impacted them financially were two times more likely to increase their “junk food” consumption compared to those who were not impacted [33]. This could be explained by emotional eating in response to financial stress but also related to tight finances that limit purchase of healthy foods such as fruits and vegetables. Elevated psychological distress has been implicated in contributing to high levels of obesity among disadvantaged groups [54, 55] and the potential for the pandemic to strengthen this link is alarming.
Pandemic-Related Stress: Implications for Obesity Prevention During and Following the Pandemic
Prior to the pandemic, the World Health Organization (WHO) estimated 13% of adults worldwide were affected by obesity and this figure was projected to grow over time [56]. Scholars have sounded the alarm regarding the negative effects of the pandemic on obesity levels among adults [57] and children [58]; hence, obesity prevention remains a public health priority during this time. The role poor mental health and stress play in unhealthy behaviours and emotional eating, both of which lead to or worsen obesity, should be given careful consideration.
Interventions that address the psychological determinants of weight-promoting behaviours are needed to prevent excess weight gain in at-risk populations. Therefore, interventions that support individuals in developing alternative strategies to cope with stress and limit emotional eating are of particular value at this time. While these interventions may benefit the larger community, special attention should be given to those deemed at the highest risk, namely women, people with obesity and those pre-existing mental illness.
Interventions to Improve Weight-Related Behaviours
At best of times, the majority of the public does not meet the recommended weekly physical activity targets and the pandemic has further increased sedentary behaviours among many [59]. Also, it is well established that there are barriers for integrating regular physical activity into one’s routine and even greater barriers for maintaining the behaviour long term [60]. In the context of the pandemic, individuals with vs. without obesity had greater perceived barriers for physical activity which was attributed to the lack of motivation and lack of social support [31]. Research suggests that targeting sedentary behaviour (e.g. time spent sitting or lying down) may be a more attainable goal compared with efforts aimed at increasing physical activity with potential positive effects on mental health [61]. Reducing sedentary behaviour can be integrated with relative ease into the “new normal” life of COVID-19 and includes light intensity activity (e.g. standing up, pacing around, stretching) for 2–5 min every 20–30 min [62]. Emerging evidence proposes that scheduled “mini-breaks” have a beneficial effect on both physical and mental health [63, 64]. Targeting sedentary behaviour during COVID-19 could be especially beneficial to groups who are more likely to isolate/stay home (e.g. those deemed at high risk of infection) and for groups who face structural barriers for physical activity (e.g. low socio-economic neighbourhoods) [64, 65].
Technology-based interventions to promote healthy eating and physical activity have seen success prior to the pandemic and can be delivered via telephone or internet [66]. The pandemic boosted the use of technology in all aspects of our lives but most notably is its expanding role in healthcare. Weight management programs with nimble adoption from in-person to internet-based delivery saw positive results in weight outcomes during the pandemic [67]. This is not surprising as internet delivery holds potential to provide structure, psychological and social support to participants in a comparable manner to in-person care. All of the above are critical components of health behaviour change that were absent for many due to the pandemic.
Interventions to Improve Emotional Eating
The past decade has seen a plethora of research surrounding the psychological determinants of obesity and the role they play in successful weight loss [68]. Of a number of psychological constructs, such as self-efficacy, restraint, and emotional eating: the tendency to respond to stress by eating, was found to have the strongest correlation with future weight gain [69]. Recently, researchers attempted to reduce emotional eating among individuals with obesity by using Abraham and Michie’s health behaviour change techniques [70] applied to healthy eating and physical activity in an intensive program that lasted for 52 weeks [71]. Results were encouraging with a significantly greater weight loss in the intervention vs. control group (6.5% vs. 2.9%) that was sustained for up to 2 years.
Additional psychological interventions that appear beneficial in the treatment of emotional eating are mindfulness and self-compassion. Mindfulness-based interventions afford participants the skills needed to identify and acknowledge unpleasant emotions rather than try to relieve them by an unhealthy behaviour (e.g. impulsive eating) [72]. Emerging evidence suggests that mindfulness is advantageous in improving emotional eating as well as other forms of pathological eating patterns (e.g. binge eating) [73]. Given the relative ease of understanding the basic skills of mindfulness, a number of mobile applications were developed to promote mindful eating. Theses mobile applications were recently reviewed with high scores assigned to “Am I Hungry?® Mindful Eating Virtual Coach” and “In the Moment” apps [73]. Self-compassion is another psychological intervention that holds promise to improve emotional eating. It is generally defined as being kind and non-judgemental towards oneself (i.e. compassionate) in particular accepting one’s mistakes and weaknesses [74]. It may be especially helpful to circumvent the typical pitfall of feeling depressed or anxious in response to a “slip” of unhealthy eating and helping individuals stay “on track” with their healthy eating plan [75]. This approach has seen success in reducing emotional eating during COVID, when a self-compassion intervention was delivered through a mobile app [76•]. Finally, cognitive behavioural therapy (CBT) has seen success in improving psychological well-being among people with obesity and aiding in weight loss and its maintenance [77]. Evidence exists for both phone [78•] and internet delivery [79] of CBT programs for weight management in specialist care which specifically target emotional eating. As such, additional research is needed to test widescale implementation of these programs into settings within the broader health system.
Conclusion
The burden of the COVID-19 is not equally shared among all population groups. This includes differential morbidity and mortality as well as psychological distress among those whose lives are most affected by the pandemic (e.g. loss of employment) or are at risk of infection (e.g. those with obesity). Pandemic stressors are linked with poor mental health and are conducive to unhealthy behaviours such as physical inactivity and a poor diet. This is further compounded by public health restrictions that limit opportunities for healthy active living and conversely increase opportunities for sedentary behaviours and unhealthy eating patterns. Individuals with pre-existing obesity as well as those with mental health conditions are particularly at risk for exhibiting weight-promoting behaviours at this time. Public health actions to support emotional well-being in the population during COVID-19 should be complemented with efforts to improve healthy behaviours. The use of remote programming (via telephone or internet) to support at-risk groups in changing weight-promoting behaviours holds promise for scalable widespread interventions for obesity prevention.
Declarations
Ethics Approval and Consent to Participate
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
No conflict of interest for all authors.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Psychological Issues
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Patel SY, et al. Trends in outpatient care delivery and telemedicine during the COVID-19 pandemic in the US. JAMA Intern Med. 2021;181(3):388–391. doi: 10.1001/jamainternmed.2020.5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schmitz N, et al. COVID-19 and depressive symptoms: a community-based study in Quebec. Canada. Can J Psychiatry. 2020;65(10):733–735. doi: 10.1177/0706743720943812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021;8(2):141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jia R, et al. Mental health in the UK during the COVID-19 pandemic: cross-sectional analyses from a community cohort study. BMJ Open. 2020;10(9):e040620. [DOI] [PMC free article] [PubMed]
- 5.Sherman AC, et al. Mental health outcomes associated with the COVID-19 pandemic: prevalence and risk factors in a southern US state. Psychiatry Res. 2020;293:113476. [DOI] [PMC free article] [PubMed]
- 6.Chwastiak LA, Rosenheck RA, Kazis LE. Association of psychiatric illness and obesity, physical inactivity, and smoking among a national sample of veterans. Psychosomatics. 2011;52(3):230–6. doi: 10.1016/j.psym.2010.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: cross-sectional & longitudinal analyses. Health Psychol. 2009;28(3):354–63. doi: 10.1037/a0014400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.• Avila C. et al. An overview of links between obesity and mental health. Curr Obes Rep. 2015;4(3):303–10. This review details the evidence regarding the link between common and severe mental disorders and obesity. It provides information on clinical and biological factors that account for the increased prevalence of co-existing obesity among people with mental disorders. [DOI] [PubMed]
- 9.Guan W-J, et al. Clinical characteristics of coronavirus disease 2019 in China. New England journal of medicine. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehra MR, et al. Cardiovascular disease, drug therapy, and mortality in Covid-19. N Engl J Med. 2020;382(25):e102. [DOI] [PMC free article] [PubMed] [Retracted]
- 11.Foldi M, et al. Obesity is a risk factor for developing critical condition in COVID-19 patients: a systematic review and meta-analysis. Obes Rev. 2020;21(10):e13095. [DOI] [PMC free article] [PubMed]
- 12.Huang Y, et al. Obesity in patients with COVID-19: a systematic review and meta-analysis. Metabolism. 2020;113: 154378. [DOI] [PMC free article] [PubMed]
- 13.Sattar N, McInnes IB, McMurray JJV. Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation. 2020;142(1):4–6. doi: 10.1161/CIRCULATIONAHA.120.047659. [DOI] [PubMed] [Google Scholar]
- 14.McNeill JN, et al. The role of obesity in inflammatory markers in COVID-19 patients. Obes Res Clin Pract. 2020. [DOI] [PMC free article] [PubMed]
- 15.Aung N, et al. Causal inference for genetic obesity, cardiometabolic profile and COVID-19 susceptibility: a mendelian randomization study. Front Genet. 2020;11:586308. [DOI] [PMC free article] [PubMed]
- 16.Centers for disease control and prevention (CDC) underlying medical conditions associated with high risk for severe COVID-19. Accessed on April 23, 2021. 2021; Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html. [PubMed]
- 17.Aminian A, et al. Association of prior metabolic and bariatric surgery with severity of coronavirus disease 2019 (COVID-19) in patients with obesity. Surg Obes Relat Dis. 2021;17(1):208–214. doi: 10.1016/j.soard.2020.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grannell A, le Roux CW, McGillicuddy D. I am terrified of something happening to me the lived experience of people with obesity during the COVID-19 pandemic. Clin Obes. 2020;10(6):e12406. [DOI] [PubMed]
- 19.Vallis M, Glazer S. Protecting individuals living with overweight and obesity: attitudes and concerns towards COVID-19 vaccination in Canada. Obesity (Silver Spring). 2021. [DOI] [PMC free article] [PubMed]
- 20.Creese B. Loneliness, physical activity and mental health during Covid-19: a longitudinal analysis of depression and anxiety in adults over 50 between, et al 2015 and 2020 Int Psychogeriatr. 2020;1:21. [DOI] [PMC free article] [PubMed]
- 21.Zajacova A, et al. Mental health and economic concerns from March to May during the COVID-19 pandemic in Canada: insights from an analysis of repeated cross-sectional surveys. SSM Popul Health. 2020;12:100704. [DOI] [PMC free article] [PubMed]
- 22.Carroll N, et al. The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients. 2020;12(8). [DOI] [PMC free article] [PubMed]
- 23.de Luis Roman DA, et al. Effect of lockdown for COVID-19 on self-reported body weight gain in a sample of obese patients. Nutr Hosp. 2020;37(6):1232–1237. doi: 10.20960/nh.03307. [DOI] [PubMed] [Google Scholar]
- 24.Eberly LA, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(12):e2031640. [DOI] [PMC free article] [PubMed]
- 25.Ettman CK, et al. Low assets and financial stressors associated with higher depression during COVID-19 in a nationally representative sample of US adults. J Epidemiol Community Health. 2020. [DOI] [PMC free article] [PubMed]
- 26.• Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med. 2014;44(1):81-121. This systematic review examined the influence of stress on physical activity. Analysis of 55 prospective studies found that in the majority of cases psychological stress predicts lower levels of physical activity. [DOI] [PMC free article] [PubMed]
- 27.Adam TC, Epel ES. Stress, eating and the reward system. Physiol Behav. 2007;91(4):449–458. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 28.Yau YH, Potenza MN. Stress and eating behaviors. Minerva Endocrinol. 2013;38(3):255–67. [PMC free article] [PubMed] [Google Scholar]
- 29.Kim EJ, Dimsdale JE. The effect of psychosocial stress on sleep: a review of polysomnographic evidence. Behav Sleep Med. 2007;5(4):256–78. doi: 10.1080/15402000701557383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hargens TA, et al. Association between sleep disorders, obesity, and exercise: a review. Nat Sci Sleep. 2013;5:27–35. doi: 10.2147/NSS.S34838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robinson E, et al. Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite. 2021;156:104853. [DOI] [PMC free article] [PubMed]
- 32.Deschasaux-Tanguy M, et al. Diet and physical activity during the coronavirus disease 2019 (COVID-19) lockdown (March-May 2020): results from the French NutriNet-Sante cohort study. Am J Clin Nutr. 2021;113(4):924–938. doi: 10.1093/ajcn/nqaa336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zajacova A, et al. Changes in health behaviours during early COVID-19 and socio-demographic disparities: a cross-sectional analysis. Can J Public Health. 2020;111(6):953–962. doi: 10.17269/s41997-020-00434-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sampson L, et al. Financial hardship and health risk behavior during COVID-19 in a large US national sample of women. SSM Popul Health. 2021;13:100734. [DOI] [PMC free article] [PubMed]
- 35.Hauksdottir A, et al. Increased stress among women following an economic collapse–a prospective cohort study. Am J Epidemiol. 2013;177(9):979–88. doi: 10.1093/aje/kws347. [DOI] [PubMed] [Google Scholar]
- 36.Park JH, et al. What happened pre- and during COVID-19 in South Korea? Comparing physical activity, sleep time, and body weight status. Int J Environ Res Public Health. 2021;18(11). [DOI] [PMC free article] [PubMed]
- 37.Ingram J, Maciejewski G, Hand CJ. Changes in diet, sleep, and physical activity are associated with differences in negative mood during COVID-19 lockdown. Front Psychol. 2020;11:588604. [DOI] [PMC free article] [PubMed]
- 38.Konttinen H. Emotional eating and obesity in adults: the role of depression, sleep and genes. Proc Nutr Soc. 2020;79(3):283–289. doi: 10.1017/S0029665120000166. [DOI] [PubMed] [Google Scholar]
- 39.Almandoz JP, et al. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin Obes. 2020;10(5):e12386. [DOI] [PMC free article] [PubMed]
- 40.Fornaro M, et al. The burden of mood-disorder/cerebrovascular disease comorbidity: essential neurobiology, psychopharmacology, and physical activity interventions. Int Rev Psychiatry. 2017;29(5):425–435. doi: 10.1080/09540261.2017.1299695. [DOI] [PubMed] [Google Scholar]
- 41.Pellegrini M, et al. Changes in weight and nutritional habits in adults with obesity during the lockdown period caused by the COVID-19 virus emergency. Nutrients. 2020;12(7). [DOI] [PMC free article] [PubMed]
- 42.Jimenez A, et al. Psychosocial, lifestyle, and body weight impact of COVID-19-related lockdown in a sample of participants with current or past history of obesity in Spain. Obes Surg. 2021;31(5):2115–2124. doi: 10.1007/s11695-021-05225-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Klatzkin RR, et al. Negative affect is associated with increased stress-eating for women with high perceived life stress. Physiol Behav. 2019;210:112639. [DOI] [PMC free article] [PubMed]
- 44.Volkow ND, et al. Obesity and addiction: neurobiological overlaps. Obes Rev. 2013;14(1):2–18. doi: 10.1111/j.1467-789X.2012.01031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kekic M, et al. Bad things come to those who do not wait: temporal discounting is associated with compulsive overeating, eating disorder psychopathology and food addiction. Front Psychiatry. 2019;10:978. doi: 10.3389/fpsyt.2019.00978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wagner HS, et al. The myth of comfort food. Health Psychol. 2014;33(12):1552–7. doi: 10.1037/hea0000068. [DOI] [PubMed] [Google Scholar]
- 47.Sominsky L, Spencer SJ. Eating behavior and stress: a pathway to obesity. Front Psychol. 2014;5:434. doi: 10.3389/fpsyg.2014.00434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Block JP, et al. Psychosocial stress and change in weight among US adults. Am J Epidemiol. 2009;170(2):181–92. doi: 10.1093/aje/kwp104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.•• Cotter EW, Kelly NR. Stress-related eating, mindfulness, and obesity. Health Psychol. 2018;37(6):516–25. Using US cross-sectional data, authors found that experiences of stress were linked with a higher BMI. Further analyses revealed that the relationship was mediated by stress-eating and moderated by female gender and obesity (stronger association). [DOI] [PMC free article] [PubMed]
- 50.• Bemanian M, et al. Emotional eating in relation to worries and psychological distress amid the COVID-19 pandemic: a population-based survey on adults in Norway. Int J Environ Res Public Health. 2020;18(1). A Norwegian survey found emotional-eating in over half the population during lock down. Female gender and having psychological distress predicted higher rates of emotional-eating. [DOI] [PMC free article] [PubMed]
- 51.McAtamney K, et al. Emotional eating during COVID-19 in the United Kingdom: exploring the roles of alexithymia and emotion dysregulation. Appetite. 2021;161:105120. [DOI] [PMC free article] [PubMed]
- 52.Cecchetto C, et al. Increased emotional eating during COVID-19 associated with lockdown, psychological and social distress. Appetite. 2021;160:105122. [DOI] [PMC free article] [PubMed]
- 53.Finch LE, Cummings JR, Tomiyama AJ. Cookie or clementine? Psychophysiological stress reactivity and recovery after eating healthy and unhealthy comfort foods. Psychoneuroendocrinology. 2019;107:26–36. doi: 10.1016/j.psyneuen.2019.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lopez-Cepero A, et al. Association between food insecurity and emotional eating in Latinos and the mediating role of perceived stress. Public Health Nutr. 2020;23(4):642–648. doi: 10.1017/S1368980019002878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Spinosa J, et al. From socioeconomic disadvantage to obesity: the mediating role of psychological distress and emotional eating. Obesity (Silver Spring) 2019;27(4):559–564. doi: 10.1002/oby.22402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.World Health Organization (WHO). Accessed on 2021 Apr 23. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- 57.Mattioli AV, et al. Obesity risk during collective quarantine for the COVID-19 epidemic. Obes Med. 2020;20:100263. [DOI] [PMC free article] [PubMed]
- 58.Ribeiro K, et al. COVID-19 and nutrition: the need for initiatives to promote healthy eating and prevent obesity in childhood. Child Obes. 2020;16(4):235–237. doi: 10.1089/chi.2020.0121. [DOI] [PubMed] [Google Scholar]
- 59.Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health. 2020;20(1):1351. [DOI] [PMC free article] [PubMed]
- 60.Middleton KR, Anton SD, Perri MG. Long-term adherence to health behavior change. Am J Lifestyle Med. 2013;7(6):395–404. doi: 10.1177/1559827613488867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zieff G, et al. Targeting sedentary behavior as a feasible health strategy during COVID-19. Transl Behav Med. 2021;11(3):826–831. doi: 10.1093/tbm/ibaa101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Paterson C, et al. The effects of acute exposure to prolonged sitting, with and without interruption, on vascular function among adults: a meta-analysis. Sports Med. 2020;50(11):1929–1942. doi: 10.1007/s40279-020-01325-5. [DOI] [PubMed] [Google Scholar]
- 63.Hallgren M, et al. Associations of interruptions to leisure-time sedentary behaviour with symptoms of depression and anxiety. Transl Psychiatry. 2020;10(1):128. doi: 10.1038/s41398-020-0810-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Grant D, et al. The effects of displacing sedentary behavior with two distinct patterns of light activity on health outcomes in older adults (implications for COVID-19 quarantine). Front Physiol. 2020;11:574595. [DOI] [PMC free article] [PubMed]
- 65.Dubay LC, Lebrun LA. Health, behavior, and health care disparities: disentangling the effects of income and race in the United States. Int J Health Serv. 2012;42(4):607–25. doi: 10.2190/HS.42.4.c. [DOI] [PubMed] [Google Scholar]
- 66.Beleigoli AM, et al. Web-based digital health interventions for weight loss and lifestyle habit changes in overweight and obese adults: systematic review and meta-analysis. J Med Internet Res. 2019;21(1):e298. [DOI] [PMC free article] [PubMed]
- 67.Fraticelli F, Nicola MD, Vitacolonna E. A nutritional web-based approach in obesity and diabetes before and during COVID-19 lockdown. J Telemed Telecare. 2020;1357633X20966933. [DOI] [PMC free article] [PubMed]
- 68.Teixeira PJ, et al. Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Med. 2015;13:84. doi: 10.1186/s12916-015-0323-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Koenders PG, van Strien T. Emotional eating, rather than lifestyle behavior, drives weight gain in a prospective study in 1562 employees. J Occup Environ Med. 2011;53(11):1287–93. doi: 10.1097/JOM.0b013e31823078a2. [DOI] [PubMed] [Google Scholar]
- 70.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27(3):379–87. doi: 10.1037/0278-6133.27.3.379. [DOI] [PubMed] [Google Scholar]
- 71.Annesi JJ. Psychosocial correlates of emotional eating and their interrelations: implications for obesity treatment research and development. J Prim Prev. 2020;41(2):105–125. doi: 10.1007/s10935-020-00580-6. [DOI] [PubMed] [Google Scholar]
- 72.Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clinical psychology: Science and practice. 2003;10(2):144–156. [Google Scholar]
- 73.Katterman SN, et al. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eat Behav. 2014;15(2):197–204. doi: 10.1016/j.eatbeh.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 74.Neff K. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and identity. 2003;2(2):85–101. doi: 10.1080/15298860309032. [DOI] [Google Scholar]
- 75.Rahimi-Ardabili H, et al. A systematic review of the efficacy of interventions that aim to increase self-compassion on nutrition habits, eating behaviours, body weight and body image. Mindfulness. 2018;9(2):388–400. doi: 10.1007/s12671-017-0804-0. [DOI] [Google Scholar]
- 76.• Schnepper R, Reichenberger J, Blechert J. Being my own companion in times of social isolation - a 14-day mobile self-compassion intervention improves stress levels and eating behavior. Front Psychol. 2020;11:595806. Trial of a mobile app to increase self-compassion as a way of improving eating behaviour among individuals seeking weight management. Intervention decreased stress, increased self-compassion and eating in response to stress. [DOI] [PMC free article] [PubMed]
- 77.Castelnuovo G, et al. Cognitive behavioral therapy to aid weight loss in obese patients: current perspectives. Psychol Res Behav Manag. 2017;10:165–173. doi: 10.2147/PRBM.S113278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.• Sockalingam S, et al. Telephone-based cognitive behavioural therapy for female patients 1-year post-bariatric surgery: a pilot study. Obes Res Clin Pract. 2019;13(5):499–504. This study found that phone delivery of six sessions of CBT for post-bariatric patients helped reduce emotional eating as well as depression and anxiety symptoms. [DOI] [PubMed]
- 79.Tham M, Chong TW. Evaluation of an online cognitive behavioural therapy weight loss programme as an adjunct to anti-obesity medications and lifestyle interventions. Australas Psychiatry. 2020;28(2):140–147. doi: 10.1177/1039856219871882. [DOI] [PubMed] [Google Scholar]