Abstract
Objective
Data regarding the efficacy and safety of bridging thrombolysis (BT) initiated before transfer for evaluation of endovascular therapy is heterogeneous. We, therefore, analyse efficacy and safety of BT in patients treated within a drip-and-ship stroke service.
Methods
Consecutive adult patients suffering from acute ischaemic stroke and large-vessel occlusions (LVO) transferred to our comprehensive stroke centre for evaluation of endovascular therapy in 2017–2020 were identified from a local prospective stroke database and categorised according to BT and no-BT. BT was defined as intravenous thrombolysis initiated before transfer. LVO was assessed before and after transfer. Functional outcome before stroke and at 3 months using the modified Rankin scale (mRS) was determined. Excellent outcome was defined as mRS 0–1 or return to prestroke mRS. For safety analysis, intracranial haemorrhages and mortality at 3 months were analysed. Main analysis was limited to patients with anterior circulation stroke.
Results
Of N=714 patients, n=394 (55.2%) received BT. More patients in the BT group with documented LVO before transfer recanalised without endovascular therapy (n=46, 11.7%) than patients who did not receive BT before transfer (n=4, 1.3%, p<0.001). In multivariate analysis, BT was the strongest independent predictor of early recanalisation (adjusted OR 10.9, 95% CI 3.8 to 31.1, p<0.001). BT tended to be an independent predictor of an excellent outcome at 3 months (adjusted OR 1.38, 95% CI 0.97 to 1.96, p=0.077). There were no differences in safety between the BT and no-BT groups.
Conclusions
BT initiated before transfer was a strong independent predictor of early recanalisation.
Keywords: thrombolysis, thrombectomy, stroke
Introduction
Two out of three randomised clinical trials have recently shown that endovascular therapy alone is not inferior to intravenous thrombolysis plus endovascular therapy with regards to functional outcome after acute ischaemic stroke with large-vessel occlusion (LVO).1–3 However, these results cannot be directly translated into drip-and-ship stroke services as the treatment modalities were randomised at hospitals that are ready to give endovascular treatment.4 Consequently, exposure times to intravenous thrombolysis before starting endovascular therapy were rather short. Furthermore, in light of the neutral results of a first randomised clinical trial investigating prehospital triage for patients with suspected LVO to enable direct transfer to an ‘endovascular-ready hospital’5 and conflicting data from observational studies,6–9 a controversial debate regarding the optimal stroke service structure continues.10 The basic rationale of a drip-and-ship stroke service, that is, admission to the nearest primary stroke centre, is to provide intravenous thrombolysis as early as possible. Early thrombolysis is weighed against delays in initiating endovascular therapy, which is only available at comprehensive stroke centres that, in turn, are fewer in number. Whether intravenous thrombolysis initiated at the primary stroke-ready hospital before immediate shipment to evaluate endovascular therapy in case of suspected or proven LVO (so-called bridging thrombolysis, BT) is indeed efficient and safe enough to support the drip-and-ship concept is unknown. Recently, a meta-analysis included 30 studies reporting outcomes of BT compared with patients who went directly to endovascular therapy11 and reported both better functional outcome and lower mortality at 90 days in the BT group, with no safety issues. Data were in line with reports from previous meta-analyses.12 13 However, interpretation of these data is hampered by the fact that most of the studies including the recent studies14 15 had analysed heterogeneous groups of patients transferred within a stroke service together with patients directly admitted to the endovascular-ready hospitals, and only a minority of studies reported the portion of cases transferred, which ranged from 9% to 57%.16–18
We, therefore, aimed to analyse the efficacy and safety of BT initiated before transfer in a large cohort of patients treated within a drip-and-ship stroke service.
Methods
Study design, setting and patients
We screened our prospective local database, the Heidelberg Recanalization Registry (HeiReKa) for adult patients with (1) acute ischaemic stroke, (2) LVO (internal carotid artery (ICA), carotid T, middle cerebral artery (MCA, segments M1–M3), posterior cerebral artery (PCA), vertebral artery (VA) or basilar artery (BA)) and (3) transfer for evaluation of endovascular therapy from 2017 to 2020. We restricted the main analysis to patients with anterior circulation stroke (here, ICA; carotid T, MCA (M1–M2)) but included patients with distal MCA occlusion (M3) or posterior circulation stroke (PCA, VA, BA) in a supplementary analysis (full cohort analysis, see online supplemental file). Patients with non-cerebral acute ischaemic stroke and/or transfer from non-thrombolysis-ready hospitals were excluded.
svn-2021-001024supp001.pdf (365.3KB, pdf)
Presence of LVO in the anterior or posterior circulation was determined by CT or MRI at the referring hospital, including CT or MR angiography. In two patients, LVO was determined according to a hyperdense artery sign, with occlusion confirmed later at the comprehensive stroke centre. Patients were assigned to the BT group if intravenous thrombolysis was initiated at the referring site prior to transfer. HeiReKa and analyses within are approved by the ethics committee of the Medical Faculty of Heidelberg (S-325/2015).
Data acquisition and definitions
All diagnostic and treatment decisions were left to the discretion of the treating physicians based on detailed local Standard Operating Procedures. Decision to perform intravenous thrombolysis with recombinant tissue plasminogen activator (rtPA) (0.9 mg/kg body weight) was made at the referring sites according to general recommendations and labelling, and most referring centres received advice via teleneurological and teleradiological consultations. The decision to transfer for evaluation of endovascular therapy was made in multidisciplinary emergency consultations involving neurologists and neuroradiologists at our endovascular-ready comprehensive stroke centre. Information about medical history, stroke severity and clinical course and treatment modalities as well as time metrics were extracted from the database. If not stated otherwise, time window was defined as the duration since stroke symptoms were definitely present to first recanalisation therapy. Reasons for not performing BT were added to the database by reviewing the digital hospital archive and the discharge letters. Grade of reperfusion after endovascular therapy according to the modified thrombolysis in cerebral infarction (mTICI) score19 was also available from the database. Early recanalisation was defined as recanalised vessel before endovascular treatment with documented LVO prior to transfer. Vessel recanalisation was documented through repeated CT-angiography/MR-angiography or diagnostic, non-therapeutic digital subtraction angiography (DSA). Migration of thrombi with persisting LVO was not defined as early recanalisation. Functional status before and after stroke was assessed using the modified Rankin scale (mRS). The follow-up outcome at 3 months after stroke was obtained through rehabilitation reports, outpatient assessments or a standardised interview by an unblinded investigator, and the assessment was part of the prospective database. As patients with pre-existing disability were included, excellent functional outcome was defined as mRS 0–1 or return to prestroke mRS. For safety analysis, intracranial haemorrhage in routine follow-up imaging according to the Heidelberg Bleeding Classification,20 mortality due to intracranial haemorrhage and mortality at 3 months were analysed. Transfer distance for ground-based transport was estimated using Google maps, with the referring clinic as the start point, our CSC as the destination and considering the fastest connection.
Statistics
For categorical data, absolute and relative frequencies (count and percentage) are reported, and the distribution of continuous data is described as mean (SD) or median (IQRs). The Kolmogorov–Smirnov test was used to ascertain distribution of data. To compare proportions of demographic and clinical characteristics between the BT and no-BT groups, the χ2 test or Fisher exact test was used, as appropriate. To compare continuous variables, the t-test or the Mann-Whitney test was used, according to the skewness of the data. For exploratory analyses of factors influencing excellent functional outcome or early vessel recanalisation, we performed multivariate binary logistic regression analyses (method: enter). Explanatory variables of the univariate between-group comparison (BT vs no-BT) with a p value <0.1 were included for multivariate analysis with excellent functional outcome as the dependent variable, whereas the variables for potential thrombus composition, age, sex, arterial hypertension, diabetes mellitus, hypercholesterinaemia, atrial fibrillation, previous stroke and occlusion site were included in the multivariate analysis, with early recanalisation as the dependent variable. ORs are described with 95% CIs. All statistical tests were two-sided, and p values of <0.05 were considered statistically significant. Analyses were conducted using IBM SPSS Statistics, V.27 (Armonk, New York). This study was performed according to the Strengthening of the Reporting of Observational Studies in Epidemiology guidelines for observational studies.
Results
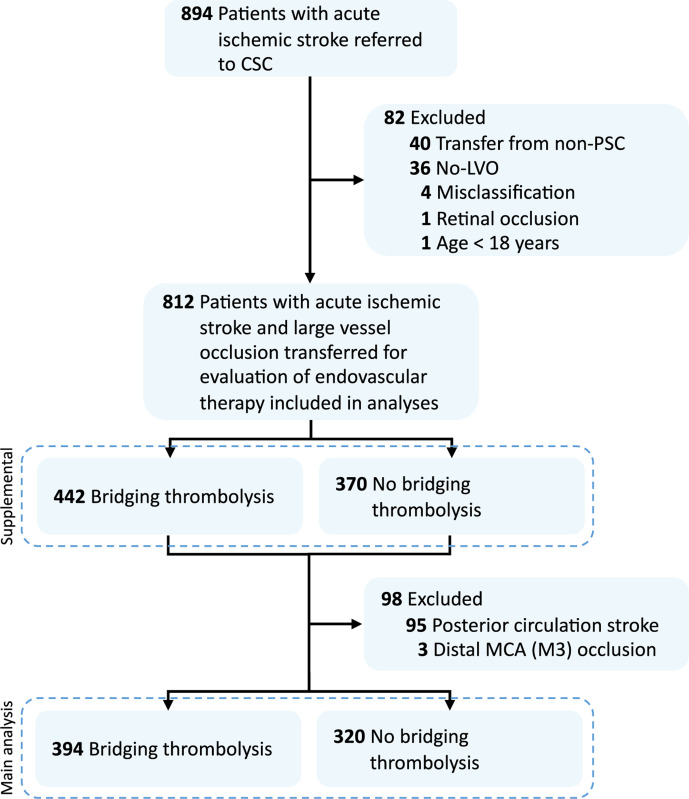
We screened N=894 patients suffering from acute ischaemic stroke and transferred for evaluation of acute endovascular therapy in a drip-and-ship stroke service and included n=714 in main analyses (see figure 1 for inclusions/exclusions). Patients were transferred from 26 different sites, with >30 referrals per site from n=10 sites. Median transfer distance was 55 km (IQR 33–83).
Figure 1.
Flow diagram of screening process. CSC, comprehensive stroke centre; LVO, large-vessel occlusion; MCA, middle cerebral artery, PSC, primary stroke centre.
Baseline characteristics
In a total of 394 patients (55.2%), BT was initiated at the referring hospital (table 1). Reasons for not performing BT are listed in table 2 (see online supplemental table S2 for full cohort analysis). In patients for whom the exact time of stroke onset was known (BT, 87.8% vs no-BT, 49.8%), time to first recanalisation therapy, that is, intravenous thrombolysis in the BT group, was shorter in the BT group (table 1). High-grade stenosis or occlusion was present in all patients before transfer, with isolated M1 or M2 occlusions being the most frequent occlusion sites (44.1% and 22.7%, respectively). Distribution of LVO was similar between patients treated with BT or not (table 1). Thrombus migration was observed more often with BT than without (BT, M1 to M2, n=6, M2 to M3, n=7; no-BT, M1 to M2, n=1, M1 to M3, n=1).
Table 1.
Baseline demographics and clinical characteristics
| Bridging thrombolysis | No bridging thrombolysis | P value | |
| N (%) | 394 (55.2%) | 320 (44.8%) | – |
| Age, mean year (SD) | 74.5 (11.8) | 76.0 (12.0) | 0.097 |
| Women, n (%) | 217 (55.1%) | 181 (56.6) | 0.705 |
| Comorbidities, n (%) | |||
| Arterial hypertension | 310 (78.7%) | 257 (80.3 %) | 0.642 |
| Diabetes mellitus | 84/393 (21.4%) | 88 (27.5%) | 0.065 |
| Hyperlipidaemia | 129/392 (32.9) | 121/318 (38.1%) | 0.156 |
| Ischaemic heart disease | 101/393 (25.7%) | 91/319 (28.5%) | 0.445 |
| Peripheral artery disease | 25/392 (6.4%) | 27/317 (8.5%) | 0.311 |
| Stroke/TIA | 74/392 (18.9%) | 83/319 (26%) | 0.023 |
| Current smoker | 56/383 (14.6%) | 43/315 (13.7%) | 0.745 |
| Atrial fibrillation* | 162/392 (41.3%) | 179/318 (56.3%) | <0.001 |
| Prestroke mRS | |||
| Median (IQR) | 0 (0–2) | 1 (0–3) | <0.001 |
| 0–1 | 274/393 (69.7%) | 175/318 (55.0%) | <0.001 |
| 2–5 | 119/393 (30.3%) | 143/318 (45.0%) | <0.001 |
| NIHSS, median (IQR) | 15 (10–21) | 15 (9–20) | 0.063 |
| ASPECTS, median (IQR) | 9 (7–10) | 9 (8–10) | 0.358 |
| Occlusion site, n (%) | |||
| ICA | 14 (3.6%) | 24 (7.5%) | 0.028 |
| ICA plus MCA | 55 (14.0%) | 44 (13.8%) | >0.99 |
| Carotid T | 64 (16.2%) | 36 (11.3%) | 0.065 |
| MCA, M1 | 169 (42.9%) | 146 (45.6%) | 0.495 |
| MCA, M2 | 92 (23.4%) | 70 (21.9%) | 0.654 |
| Time window†, median (IQR) | 1:45 (1:20–2:45) | 6:38 (4:16–10:49) | <0.001 |
*Known or newly diagnosed.
†In patients in whom exact time of onset is known.
ASPECTS, Alberta Stroke Programme Early Computed Tomography Score; ICA, internal carotid artery; MCA, middle cerebral artery; M1–M2, segments of the MCA; mRS, modified Rankin scale score; NIHSS, National Institutes of Health Stroke Scale.
Table 2.
Reasons for not performing thrombolysis at the referring hospital
| Reason | N (%) |
| Unknown time window | 98 (30.6) |
| Anticoagulation | 94 (29.4) |
| Time window ≥4.5 hour | 57 (17.8) |
| Contraindication to intravenous thrombolysis | 45 (14.1) |
| Multiple reasons | 18 (5.6) |
| Unknown reason | 5 (1.6) |
| Other | 3 (0.9) |
Patients who received BT had a better prestroke functional status, suffered less frequently from previous stroke and less frequently presented known or newly diagnosed atrial fibrillation. Stroke severity at admission was similar in the two groups with a median National Institutes of Health Stroke Scale of 15.
Treatment modalities
Of 394 patients treated with BT, 329 (83.5%) underwent DSA. Of these, 32 (8.1%) did not need any extracranial or intracranial endovascular therapy. In those 320 patients, in whom BT was not initiated at the referring hospital, 6 patients received intravenous thrombolysis at our comprehensive stroke centre (n=2 intravenous thrombolysis only, 0.6%) and in 318, DSA was performed (99.4%), there ultimately being no need for endovascular therapy in 5/318 patients (1.6%).
Efficacy
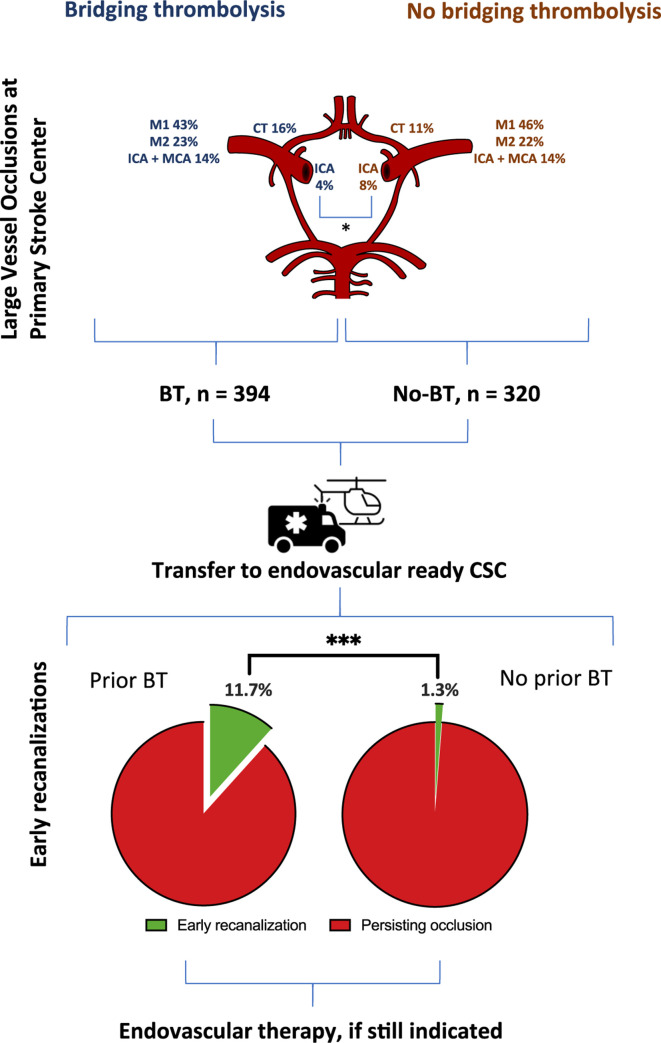
More patients in the BT group with documented LVO before transfer were recanalised without endovascular therapy (46/394, 11.7%) than patients who did not receive BT before transfer (4/320, 1.3%; p<0.0001) (figure 2) (see online supplemental figure SF2 for visualisation of occlusion sites and rates of early recanalisation of the full cohort). BT remained the strongest independent predictor of early recanalisation in a multivariate analysis (adjusted OR 10.9, 95% CI 3.8 to 31.1, p<0.001; table 3). In a sensitivity analysis including additional n=95 patients with posterior circulation and n=3 with distal MCA (M3) occlusion (see online supplemental table S1 for patient details), results were consistent (adjusted OR 14.55, 95% CI 5.2 to 41.1, p<0.001, online supplemental table S3). Time window was excluded from the main model because it constituted a major reason for withholding BT while it otherwise showed a strong correlation with initiation of BT. However, BT remained the strongest independent predictor of early recanalisation (adjusted OR 9.99, 95% CI 1.32 to 75.89, p=0.026) in a sensitivity analysis including only patients for whom the exact time window for stroke onset was known <4.5 hour (n=403).
Figure 2.
Visualisation of occlusion sites and rates of early recanalisation according to treatment with bridging thrombolysis (BT) or no-BT. BT, bridging thrombolysis; CSC, comprehensive stroke centre; ICA, internal carotid artery; MCA, middle cerebral artery; M1–M2, segments of the MCA.
Table 3.
Multivariate analyses
| Predictors of excellent functional outcome | |||
| OR | 95% CI | P value | |
| Bridging thrombolysis | 1.38 | 0.97 to 1.96 | 0.077 |
| Age | 0.98 | 0.96 to 0.99 | 0.001 |
| Atrial fibrillation | 0.91 | 0.62 to 1.33 | 0.612 |
| Diabetes mellitus | 0.66 | 0.42 to 1.01 | 0.056 |
| Previous stroke | 1.05 | 0.69 to 1.6 | 0.818 |
| Occlusion site | |||
| Most distal occlusion (M2) | Ref. | ||
| ICA | 0.52 | 0.22 to 1.26 | 0.150 |
| ICA plus MCA | 0.48 | 0.26 to 0.86 | 0.014 |
| Carotid T | 0.37 | 0.19 to 0.69 | 0.002 |
| MCA, M1 | 0.71 | 0.47 to 1.08 | 0.106 |
| Predictors of early recanalisation | |||
| Bridging thrombolysis | 10.9 | 3.8 to 31.1 | <0.001 |
| Age | 1.04 | 1.01 to 1.07 | 0.013 |
| Sex (female) | 0.86 | 0.45 to 1.64 | 0.643 |
| Arterial hypertension | 0.51 | 0.25 to 1.07 | 0.074 |
| Atrial fibrillation | 0.75 | 0.39 to 1.45 | 0.386 |
| Diabetes mellitus | 0.47 | 0.19 to 1.17 | 0.103 |
| Hypercholesterinaemia | 1.26 | 0.65 to 2.45 | 0.503 |
| Previous stroke | 1.12 | 0.53 to 2.37 | 0.777 |
| Occlusion site | |||
| Most distal occlusion (M2) | Ref. | ||
| ICA | Did not converge | ||
| ICA plus MCA | 0.17 | 0.04 to 0.78 | 0.023 |
| Carotid T | 0.21 | 0.06 to 0.74 | 0.016 |
| MCA, M1 | 0.90 | 0.46 to 1.78 | 0.767 |
ICA, internal carotid artery; MCA, middle cerebral artery; M1–M2, segments of the MCA.;
In patients in whom diagnostic or therapeutic DSA was performed, reperfusion grades were similar between patients pretreated with BT and those who were not (excellent reperfusion (mTICI 2c–3), 208/329, 63.2% vs 184/318, 57.9%, p=0.172; good reperfusion (mTICI 2b) 79/329, 24.0% vs 79/318, 24.8%, p=0.855), but no reperfusion was observed more often in non-BT patients ((mTICI 0), BT 20/329, 6.1% vs non-BT 36/318, 11.3%, p=0.025).
In univariate analysis, patients treated with BT had a better functional outcome at 3 months (BT, median mRS 3 (IQR 2–5) vs no-BT, 4,2–5 p=0.048), and more patients had an excellent favourable outcome (mRS 0–1, 23.1% vs 14.4%, p=0.004). In binary logistic regression analysis adjusting for confounders, there was trend for BT as an independent predictor for an excellent favourable outcome (mRS 0–1) or return to prestroke mRS at 3 months (adjusted OR 1.38, 95% CI 0.97 to 1.96, p=0.077; table 3). In an analysis of all N=812 patients including those with posterior circulation stroke or distal MCA occlusion, BT became an independent predictor (adjusted OR 1.42, 95 % CI 1.02 to 1.98, p=0.04; online supplemental table S3).
Safety
Bleeding complications did not differ between patients who received BT and those who did not (table 4 for Heidelberg Bleeding Classification; see online supplemental table S4 for Heidelberg Bleeding Classification of the full cohort analysis). Fatal intracranial haemorrhage developed in 7/394 (1.8%) patients in the BT group and 4/320 (1.3%) in the non-BT group (p=0.565). There was no difference in overall mortality (25.4% vs 26.1%, p=0.858).
Table 4.
Intracranial haemorrhages according to the Heidelberg bleeding classification
| Class | Type | Bridging thrombolysis | No bridging thrombolysis |
| 0 | None | 284 (72.6%) | 225 (71.0%) |
| 1a | HI1 | 37 (9.5%) | 42 (13.2%) |
| 1b | HI2 | 10 (2.6%) | 16 (5.0%) |
| 1c | PH1 | 16 (4.1%) | 9 (2.8%) |
| 2 | PH2 | 18 (4.6%) | 7 (2.2%) |
| 3a | Remote PH | 5 (1.3) | 1 (0.3%) |
| 3b | IVH | 1 (0.3%) | 0 (0%) |
| 3c | SAH | 20 (5.1%) | 16 (5.0%) |
| 3d | SDH | 0 (0%) | 0 (0%) |
| Other | Non-classified | 0 (0%) | 1 (0.3%) |
Missing data in n=3 patients in each group.
HI, haemorrhagic infarction; IVH, intraventricular haemorrhage; PH, parenchymal haemorrhage; SAH, subarachnoid haemorrhage; SDH, subdural haematoma.
Discussion
According to our analysis, early recanalised LVO was 10-fold higher in patients in whom BT was initiated prior to transfer in a large drip-and-ship stroke service, with consequently fewer endovascular therapies being needed. BT tended to be an independent predictor of an excellent functional outcome. Safety of BT was good, with no difference in the rate and type of intracranial haemorrhages between patients who did or did not receive BT.
Recent and ongoing clinical trials (DIRECT-SAFE, NCT03494920, MR CLEAN-NO IV, ISRCTN80619088 and SWIFT-DIRECT, NCT03192332) are attempting to challenge the currently recommended standard of intravenous thrombolysis administered before or in parallel to endovascular therapy,1–3 and two out of three published trials have shown that these approaches are not inferior to current recommendations with regards to functional outcome after acute ischaemic stroke with LVO in the anterior circulation.1 3 4 Indeed, these data are fueling the current debate regarding the optimal admission strategy for patients with suspected acute LVO. If intravenous thrombolysis is considered unnecessary for these patients, the main rationale for primary admission at stroke centres not capable of performing endovascular therapy would disappear. However, in our interpretation of the available data, translation of the results to current drip-and-ship stroke services is difficult due to the fact that BT was administered only at endovascular-ready hospitals.1–3
The average time from start of intravenous thrombolysis with rtPA to the beginning of endovascular therapy was short in all trials, ranging from 8 min to 40 min.1–3 Therefore, the duration of intravenous thrombolysis might simply have been too low for clot lysis, especially for larger-size clots. Transcranial continuous Doppler determined that recanalisation occurred in 75% of patients within 60 min after start of rtPA in a previous study, with an additional 25% who were recanalised after 60 min.21 In our study, the median transfer distance was 55 km, translating into procedural times that, in the majority of cases, would allow for sufficient exposure of intravenous thrombolysis before (re-)considering endovascular therapy. Early administration of intravenous thrombolysis might be particularly efficient in patients with smaller size clots,22 such as in the MCA M2 segment (20% of our cohort compared with 1.7% to 13% in the randomised trials1–3). While in our main analysis limited to patients with anterior circulation stroke, BT only tended to be an independent predictor for excellent functional outcome, the adjusted OR became significant after extending our analysis to patients with posterior circulation stroke as well as with more distal MCA segments who were evaluated for thrombectomy. This finding could reflect the higher efficacy of BT in these vessels, although efficacy was not as high as to rule out transfer for evaluation of thrombectomy per se.
Furthermore, intravenous thrombolysis is thought to be beneficial by enabling rapid dissolution of distal thrombi that develop during endovascular procedures. While in our study, patients who received BT recanalised more often without endovascular therapy than did patients in whom BT was not initiated at the referring hospital (11.7% vs 1.3%), excellent or good reperfusion grades in those who entered DSA did not differ between the groups. No reperfusion was observed more often in patients not treated with BT. These data suggest that the longer term effects of intravenous thrombolysis were greater than very short effects during the endovascular procedure.
Less patients treated with BT than those without underwent DSA. In patients shipped from external hospitals, we very briefly check the present neurological status. In case, the neurological status is unchanged, or deteriorated, immediate DSA (including the possibility to perform a Dyna-CT) or rapid CT evaluation before DSA is performed, while in patients with significant improvement of the status (as observed in patients with early recanalisation), additional CT-A is performed in the majority of cases in order to rule out the presence of a persisting LVO.
The major reasons for not performing BT at the referring hospitals were unknown or were related to extended time window and anticoagulation. Oral anticoagulation still poses a significant barrier to performing thrombolysis, especially due to the unavailability of rapid coagulation tests for non-vitamin K antagonists that could enable thrombolysis in patients with very low drug concentrations.23 Thrombolysis in unknown or extended time windows ≥4.5 hour would require more advanced neuroimaging,24 25 which is not available at the majority of primary stroke centres yet. As time window strongly correlated with performance of BT, we did not enter time window as an independent variable in our multivariate model. Although unlikely, we cannot rule out that at least part of the better early recanalisation rate observed in the BT group was simply due to the earlier time window in which the patients were diagnosed and treated. Both time window and anticoagulation status could become parameters that are established during the first emergency service dispatch, in order to avoid futile admission to primary stroke centres not able to provide BT in these patients. On the other hand, improving the broad availability of multimodal imaging to facilitate selecting candidates for BT could restrengthen the role of primary stroke centres.
Our study has limitations. Due to the retrospective study design, we were not able to prove the efficacy of thrombolysis in patients transferred within our stroke service. Although we tried to adjust for potential confounders influencing our findings, unmeasured confounders are likely present. We analysed a mixed cohort of patients including patients with more distal occlusions as well as patients with tandem occlusions, which are all known to be differently susceptible to intravenous thrombolysis. As a strength of our study, we focused on patients in whom intravenous thrombolysis was started before transfer in cases of suspected or proven LVO, excluding patients from the BT group in whom thrombolysis was only initiated at our endovascular-ready stroke centre. Thus, similarly long exposure times to intravenous thrombolysis were guaranteed, as were potential influences due to the transfer procedure itself (such as vibrations, shown to enhance the efficacy of thrombolysis under certain circumstances in a stroke model26).
In conclusion, BT initiated before transfer of patients with acute ischaemic stroke and LVO was a strong independent predictor of early recanalisation. Excellent poststroke functional status tended to be more likely in patients who received BT, but time window as a potential confounding factor could not be fully ruled out. Given the long exposure time to intravenous thrombolysis, which does facilitate early recanalisation in patients transferred for endovascular therapy, intravenous thrombolysis should not be withheld in eligible patients with LVO.
Acknowledgments
We thank Thomas Bruckner (Institute of Medical Biometry and Informatics Heidelberg) for his statistical advice. We also thank all referring sites for their continued trust in our services. We further acknowledge financial support by the Open Access Publishing Fund of Ruprecht-Karls-Universität Heidelberg.
Footnotes
Contributors: Study concept and design: JCP, PAR. Acquisition of data PAR, JCP, MH. Analysis or interpretation of data: all authors. JCP wrote the first draft of the manuscript. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: JCP.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: JCP has received consultation fees and travel expenses from Akcea, Bayer, Boehringer Ingelheim, Daiichi Sankyo and Pfizer. MM reports grants/grants pending from Balt, Medtronic, MicroVention, Stryker (money paid to the institution). PAR received travel support and lecture fees from Boeheringer Ingelheim, Daiichi Sankyo, Pfizer, and Bayer. SN has received consulting fees from Brainomix and Boehringer Ingelheim and lecture fees and travel expenses from Medtronic and Pfizer. CG is speaker of the commission telemedicine service of the German Stroke Society.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request from the corresponding author.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
HeiReKa and analyses within are approved by the ethics committee of the Medical Faculty of Heidelberg (S-325/2015). Participants gave informed consent before inclusion in HeiReKa.
References
- 1. Yang P, Zhang Y, Zhang L, et al. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med 2020;382:1981–93. 10.1056/NEJMoa2001123 [DOI] [PubMed] [Google Scholar]
- 2. Suzuki K, Matsumaru Y, Takeuchi M, et al. Effect of mechanical thrombectomy without vs with intravenous thrombolysis on functional outcome among patients with acute ischemic stroke: the SKIP randomized clinical trial. JAMA 2021;325:244–53. 10.1001/jama.2020.23522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zi W, Qiu Z, Li F, et al. Effect of endovascular treatment alone vs intravenous alteplase plus endovascular treatment on functional independence in patients with acute ischemic stroke: the DEVT randomized clinical trial. JAMA 2021;325:234–43. 10.1001/jama.2020.23523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Xiong Y, Pan Y, Nogueira RG, et al. Treating acute large vessel occlusion stroke: to bridge or not to bridge? Stroke Vasc Neurol 2021. 10.1136/svn-2021-000952. [Epub ahead of print: 26 Apr 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pérez de la Ossa N, Abilleira S, Jiménez X, eds. Transfer to the Local Stroke Center versus Direct Transfer to Endovascular Center of Acute Stroke Patients with Suspected Large Vessel Occlusion in the Cataln Territory (RACECAT). European Stroke Organisation Conference, 2020. [DOI] [PubMed] [Google Scholar]
- 6. Ismail M, Armoiry X, Tau N, et al. Mothership versus drip and SHIP for thrombectomy in patients who had an acute stroke: a systematic review and meta-analysis. J Neurointerv Surg 2019;11:14–19. 10.1136/neurintsurg-2018-014249 [DOI] [PubMed] [Google Scholar]
- 7. Ciccone A, Berge E, Fischer U. Systematic review of organizational models for intra-arterial treatment of acute ischemic stroke. Int J Stroke 2019;14:12–22. 10.1177/1747493018806157 [DOI] [PubMed] [Google Scholar]
- 8. Romoli M, Paciaroni M, Tsivgoulis G, et al. Mothership versus Drip-and-Ship model for mechanical thrombectomy in acute stroke: a systematic review and meta-analysis for clinical and radiological outcomes. J Stroke 2020;22:317–23. 10.5853/jos.2020.01767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sarraj A, Grotta J, Albers GW, et al. Clinical and neuroimaging outcomes of direct thrombectomy vs bridging therapy in large vessel occlusion: analysis of the select cohort study. Neurology 2021;96:e2839-e2853. 10.1212/WNL.0000000000012063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Katsanos AH, Tsivgoulis G. Is intravenous thrombolysis still necessary in patients who undergo mechanical thrombectomy? Curr Opin Neurol 2019;32:3–12. 10.1097/WCO.0000000000000633 [DOI] [PubMed] [Google Scholar]
- 11. Wang Y, Wu X, Zhu C, et al. Bridging thrombolysis achieved better outcomes than direct thrombectomy after large vessel occlusion: an updated meta-analysis. Stroke 2021;52:356–65. 10.1161/STROKEAHA.120.031477 [DOI] [PubMed] [Google Scholar]
- 12. Mistry EA, Mistry AM, Nakawah MO, et al. Mechanical thrombectomy outcomes with and without intravenous thrombolysis in stroke patients: a meta-analysis. Stroke 2017;48:2450–6. 10.1161/STROKEAHA.117.017320 [DOI] [PubMed] [Google Scholar]
- 13. Tsivgoulis G, Katsanos AH, Mavridis D, et al. Endovascular thrombectomy with or without systemic thrombolysis? Ther Adv Neurol Disord 2017;10:151–60. 10.1177/1756285616680549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kaesmacher J, Meinel TR, Nannoni S, et al. Bridging may increase the risk of symptomatic intracranial hemorrhage in thrombectomy patients with low Alberta stroke program early computed tomography score. Stroke 2021;52:1098–104. 10.1161/STROKEAHA.120.030508 [DOI] [PubMed] [Google Scholar]
- 15. Seker F, Bonekamp S, Rode S, et al. Impact of bridging thrombolysis on clinical outcome in stroke patients undergoing endovascular thrombectomy: a retrospective analysis of a regional stroke Registry. Neuroradiology 2021;63:935–41. 10.1007/s00234-020-02619-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Di Maria F, Mazighi M, Kyheng M, et al. Intravenous thrombolysis prior to mechanical thrombectomy in acute ischemic stroke: silver bullet or useless bystander? J Stroke 2018;20:385–93. 10.5853/jos.2018.01543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Casetta I, Pracucci G, Saletti A, et al. Combined intravenous and endovascular treatment versus primary mechanical thrombectomy. The Italian registry of endovascular treatment in acute stroke. Int J Stroke 2019;14:898–907. 10.1177/1747493019851279 [DOI] [PubMed] [Google Scholar]
- 18. Chalos V, LeCouffe NE, Uyttenboogaart M, et al. Endovascular treatment with or without prior intravenous alteplase for acute ischemic stroke. J Am Heart Assoc 2019;8:e011592. 10.1161/JAHA.118.011592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tomsick T, Broderick J, Carrozella J, et al. Revascularization results in the interventional management of stroke II trial. AJNR Am J Neuroradiol 2008;29:582–7. 10.3174/ajnr.A0843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. von Kummer R, Broderick JP, Campbell BCV, et al. The Heidelberg bleeding classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke 2015;46:2981–6. 10.1161/STROKEAHA.115.010049 [DOI] [PubMed] [Google Scholar]
- 21. Christou I, Alexandrov AV, Burgin WS, et al. Timing of recanalization after tissue plasminogen activator therapy determined by transcranial Doppler correlates with clinical recovery from ischemic stroke. Stroke 2000;31:1812–6. 10.1161/01.STR.31.8.1812 [DOI] [PubMed] [Google Scholar]
- 22. Riedel CH, Zimmermann P, Jensen-Kondering U, et al. The importance of size: successful recanalization by intravenous thrombolysis in acute anterior stroke depends on thrombus length. Stroke 2011;42:1775–7. 10.1161/STROKEAHA.110.609693 [DOI] [PubMed] [Google Scholar]
- 23. Seiffge DJ, Meinel T, Purrucker JC, et al. Recanalisation therapies for acute ischaemic stroke in patients on direct oral anticoagulants. J Neurol Neurosurg Psychiatry 2021;92:534–41. 10.1136/jnnp-2020-325456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Campbell BCV, Ma H, Ringleb PA, et al. Extending thrombolysis to 4·5-9 H and wake-up stroke using perfusion imaging: a systematic review and meta-analysis of individual patient data. Lancet 2019;394:139–47. 10.1016/S0140-6736(19)31053-0 [DOI] [PubMed] [Google Scholar]
- 25. Thomalla G, Boutitie F, Ma H, et al. Intravenous alteplase for stroke with unknown time of onset guided by advanced imaging: systematic review and meta-analysis of individual patient data. Lancet 2020;396:1574–84. 10.1016/S0140-6736(20)32163-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dhanesha N, Schnell T, Rahmatalla S, et al. Low-Frequency vibrations enhance thrombolytic therapy and improve stroke outcomes. Stroke 2020;51:1855–61. 10.1161/STROKEAHA.120.029405 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
svn-2021-001024supp001.pdf (365.3KB, pdf)
Data Availability Statement
Data are available upon reasonable request from the corresponding author.