Abstract
Background
The ratio of partial pressure of arterial oxygen to inspired oxygen fraction (PaO2/FIO2) during invasive mechanical ventilation (MV) is used as criteria to grade the severity of respiratory failure in acute respiratory distress syndrome (ARDS). During the SARS-CoV2 pandemic, the use of PaO2/FIO2 ratio has been increasingly used in non-invasive respiratory support such as high-flow nasal cannula (HFNC) and non-invasive ventilation (NIV). The grading of hypoxemia in non-invasively ventilated patients is uncertain. The main hypothesis, investigated in this study, was that the PaO2/FIO2 ratio does not change when switching between MV, NIV and HFNC.
Methods
We investigated respiratory function in critically ill patients with COVID-19 included in a single-center prospective observational study of patients admitted to the intensive care unit (ICU) at Uppsala University Hospital in Sweden. In a steady state condition, the PaO2/FIO2 ratio was recorded before and after any change between two of the studied respiratory support techniques (i.e., HFNC, NIV and MV).
Results
A total of 148 patients were included in the present analysis. We find that any change in respiratory support from or to HFNC caused a significant change in PaO2/FIO2 ratio. Changes in respiratory support between NIV and MV did not show consistent change in PaO2/FIO2 ratio. In patients classified as mild to moderate ARDS during MV, the change from HFNC to MV showed a variable increase in PaO2/FIO2 ratio ranging between 52 and 140 mmHg (median of 127 mmHg). This made prediction of ARDS severity during MV from the apparent ARDS grade during HFNC impossible.
Conclusions
HFNC is associated with lower PaO2/FIO2 ratio than either NIV or MV in the same patient, while NIV and MV provided similar PaO2/FIO2 and thus ARDS grade by Berlin definition. The large variation of PaO2/FIO2 ratio indicates that great caution should be used when estimating ARDS grade as a measure of pulmonary damage during HFNC.
Keywords: Acute respiratory distress syndrome, Mechanical ventilation, High-flow oxygen, Non-invasive ventilation
Introduction
The Berlin definition of the acute respiratory distress syndrome (ARDS)[1] is clinically useful as index of both organ dysfunction and severity of hypoxemia [2, 3]. There is growing interest in non-invasive respiratory support for acute hypoxemic respiratory failure [4]. The ongoing Corona Virus Infectious Disease 2019 (COVID-19) pandemic brought an even wider use of high-flow nasal cannula oxygen therapy (HFNC) and non-invasive ventilation (NIV) because of limited availability of mechanical ventilation (MV) [5]. While NIV provides a measurable positive end expiratory pressure (PEEP) that maybe consistent with the Berlin criteria, the level of PEEP generated by HFNC is uncertain [6, 7]. In addition, the inspiratory fraction of oxygen (FIO2) is uncertain because of leakage and variable dead space volume.
This means that the current ARDS criteria for grading hypoxemia are difficult or impossible to apply in non-invasively ventilated patients [8]. However, despite lacking clinical evidence, ARDS criteria have been applied to patients not undergoing invasive mechanical ventilation [9]. Recent reports have indicated some applicability of a low PaO2/FIO2 ratio during HFNC to predict mortality [10]. The main aim of the current study was to allow the accurate stratification of respiratory dysfunction during HFNC and NIV in COVID-19 ARDS patients by providing expected differences in PaO2/FIO2 ratio upon a change in ventilatory strategy.
Materials and methods
PaO2/FIO2 ratios were investigated in critically ill adult patients with COVID-19 admitted to the intensive care unit (ICU) at Uppsala University Hospital in Sweden from March 14, 2020 until January 14, 202 and included in a prospective observational cohort study due to COVID-19. During the most intense part of the pandemic, HFNC was used in regular wards up to 60 L/min of 60% oxygen at our hospital. Reaching this level, patients were transferred to the ICU where increasing oxygen supplementation, prone position or a change of respiratory support would be performed. Actual flow rate was 50 ± 9 L/min at 66 ± 13% oxygen during step-up from HFNC, and 44 ± 10 L/min at 55 ± 13% oxygen during step-down to HFNC. Standard starting PEEP during NIV was between 5 and 10 cmH2O, and during MV 7 to 14 cmH2O (Table 1A and B). During step-down, a PEEP below 10 cmH2O during MV would be matched with a similar PEEP in NIV (Table 1A and B). The corresponding changes in PEEP are reported in Table 1C.
Table 1.
Estimated positive end-expiratory pressure (PEEP) and change of PEEP during a change of ventilatory strategy
| 1st Strategy | 2nd Strategy | ||
|---|---|---|---|
| HFNC | NIV | MV | |
| A: First strategy PEEP (cmH2O) | |||
| HFNC | – | 3 | 3 |
| NIV | 6.3 ± 1.4 | – | 7.1 ± 2.1 |
| MV | 7.7 ± 2.1 | 7.1 ± 1.8 | – |
| B: Second strategy PEEP (cmH2O) | |||
| HFNC | – | 5.8 ± 1.2 | 11.3 ± 4.0 |
| NIV | 3 | – | 13.1 ± 2.9 |
| MV | 3 | 6.5 ± 1.6 | – |
| C: Estimated change in PEEP (cmH2O) | |||
| HFNC | – | 2.8 ± 1.2 | 8.3 ± 4.0 |
| NIV | − 3.3 ± 1.4 | – | 6.0 ± 3.2 |
| MV | − 4.7 ± 2.1 | − 0.5 ± 2.0 | - |
The changes were from the first strategy to the second strategy that were either of high-flow nasal cannula (HFNC), non-invasive ventilation (NIV) or invasive mechanical ventilation (MV). The PEEP during HFNC was estimated to 3 cmH2O. A: PEEP before the change of strategy. B: PEEP after the change of strategy. C: Change in PEEP
We analyzed the PaO2/FIO2 ratio before a change in respiratory strategy compared to 30 to 60 min after a switch in respiratory support. Patients who were not in steady state ventilation, or who did not have a blood gas analysis within a reasonable time were excluded. For each included patient, the first two changes of respiratory support were used, resulting in six comparisons. (1) HFNC-to-NIV; (2) HFNC-to-MV; (3) NIV-to-HFNC; (4) NIV-to-MV; (5) MV-to-HFNC; (6) MV-to-NIV.
Results
Two-hundred fifty-two changes of respiratory support in 148 patients were recorded. Median age was 66 (IQR = 55–73) years, 25% were women. Body mass index was 29 (25–33), and 26% of the included patients had a previous diagnosis of chronic pulmonary disease. Patients were admitted after 10 (8–12) days of symptoms with a simplified acute physiology score 3 (SAPS3) of 53 (47–59) and PaO2 /FIO2 ratio of 114 (101–148) mmHg.
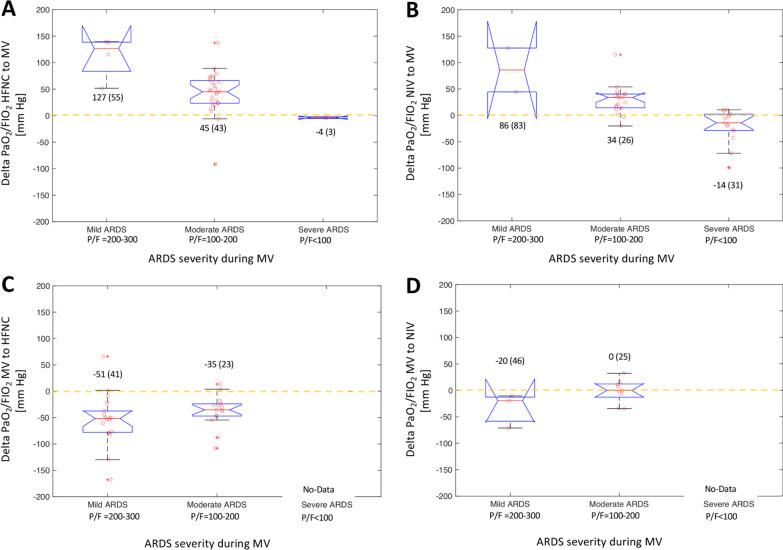
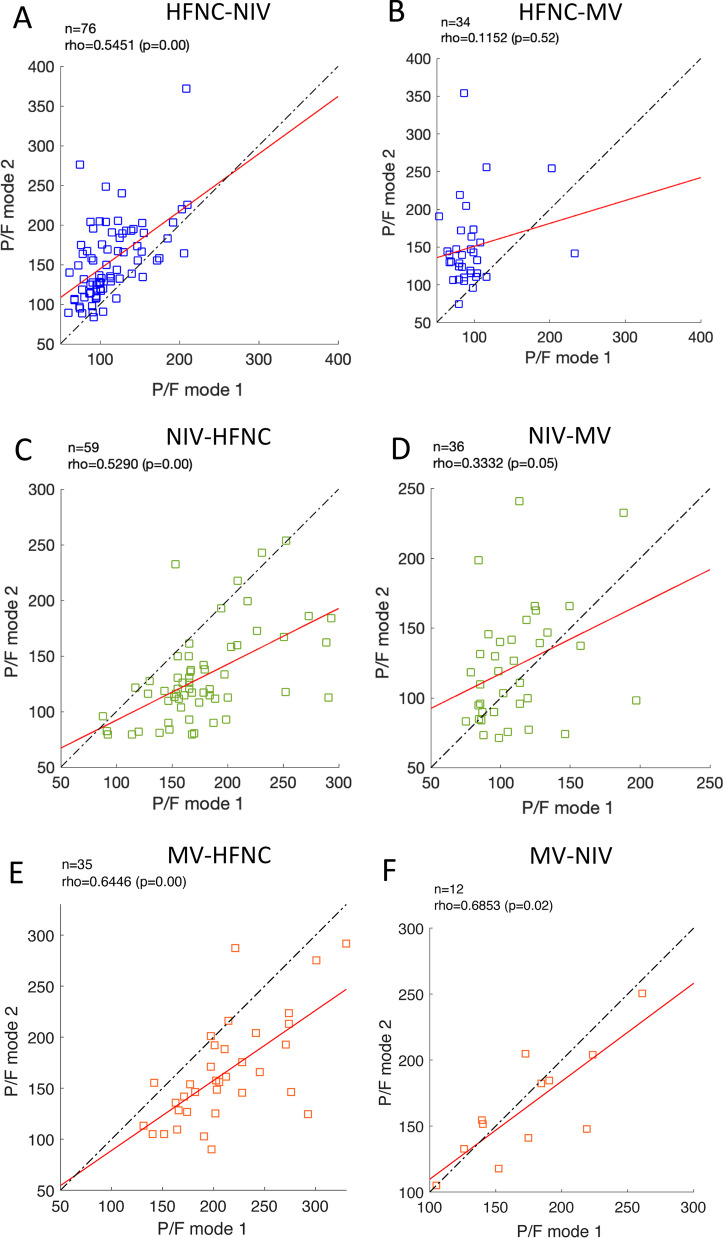
Changes to or from HFNC were biased to lower PaO2 /FIO2-ratio during HFNC, NIV-HFNC: -29(-15 to -60) mmHg, and HFNC-NIV: 41(21–65) mmHg, and more pronounced in HFNC-MV -45(-26 to -28) mmHg, and HFNC-MV 48(23–73) mmHg (Figs. 1A and C, 2A, B, C and E). On the other hand, changes between NIV and MV did not cause consistent differences in PaO2/FIO2 ratio NIV-MV: 11(− 7.5–38) mmHg and MV-NIV: − 4 (− 23—8) mmHg (Figs. 1B and D, 2D and F). All comparisons showed positive correlations between the strategies (Fig. 2 A, C, D, E and F), except HFNC-MV (R2 = 0.12, P = 0.52, Fig. 2B). The correlations improved during step-down from MV to NIV, or MV and NIV to HFNC (Fig. 2C, E and F).
Fig. 1.
Change in PO2/FIO2 after a change in respiratory support in 148 critically ill COVID-19 patients grouped by ARDS severity during mechanical ventilation (MV) based on the Berlin definition. A HFNC to MV. B NIV to MV. C MV to HFNC. D MV to NIV
Fig. 2.
Correlation of PaO2/FIO2 ratio before and after a change in ventilatory support in 148 critically ill COVID-19 patients. The six tested groups were: A HFNC-to-NIV; B HFNC-to-MV; C NIV-to-HFNC; D NIV-to-MV; E MV-to-HFNC; F MV-to-NIV. Rho and P-value calculated using Spearman rank correlation
The effective delivery of PEEP is considered to be one of the most important differences between HFNC, NIV and MV, which is also an important determinant of the amount of open lung and thereby the PaO2 /FIO2 ratio. Therefore, we analyzed the correlation between the change in PaO2 /FIO2 and the change in PEEP for all individual strategy changes (Fig. 3). It is noteworthy that the correlation is good, but there is a large residual variation.
Fig. 3.
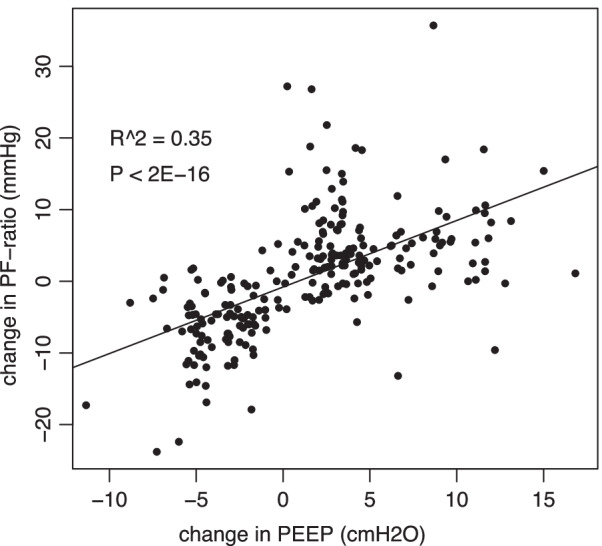
Correlation between the change in PO2/FIO2 ratio caused by a change of ventilatory strategy to the estimated change in positive end-expiratory pressure (PEEP) that accompanied that change. The changes were between high-flow nasal cannula (HFNC), non-invasive ventilation (NIV) and invasive mechanical ventilation (MV). The PEEP for HFNC was estimated at 3 cmH2O, while measured PEEP was used for NIV and MV. PEEP-values are jittered to avoid overlapping points in the graph. Pearson’s correlation was calculated using actual data
This resulted in reassignments between ARDS grades, showing general improvements in oxygenation during step-up from HFNC to NIV or MV. Mostly improvement during step-up from NIV to MV, although several patients showed worsened ARDS grade in this setting (Table 2A). Finally, worsened oxygenation, and increased ARDS grade was seen during step-down to HFNC from either MV or NIV, while step-down from MV to NIV only resulted in the reassignment of one patient in either direction (Table 2B).
Table 2.
The number of patients who are reassigned to a new grade of acute respiratory distress syndrome (ARDS, Mild: 200–300 mmHg, Moderate: 100–200 mmHg, and Severe: < 100 mmHg) during a change in ventilatory strategy
| 1st Strategy | 2nd Strategy | ||
|---|---|---|---|
| HFNC | NIV | MV | |
| A: Decreased ARDS grade | |||
| HFNC | – | 42 (55%) | 25 (74%) |
| NIV | 1 (2%) | – | 10 (28%) |
| MV | 1 (3%) | 1 (8%) | – |
| B: Increased ARDS grade | |||
| HFNC | – | 1 (1%) | 1 (3%) |
| NIV | 20 (34%) | – | 5 (14%) |
| MV | 14 (40%) | 1 (8%) | – |
The changes were from the first strategy to the second strategy that were either of high-flow nasal cannula (HFNC), non-invasive ventilation (NIV) or invasive mechanical ventilation (MV). Patients who decrease their ARDS grade, that improve in oxygenation are reported in A, and those who increase ARDS grade, or show worse oxygenation in B
Discussion
The primary finding of this study is the high variability in the effect on PaO2/FIO2 ratio after changing ventilation strategy. Considering ARDS grade under MV as gold standard, PaO2/FIO2 ratio during HFNC could not reliably predict ARDS severity. The present findings may provide a rationale for using PaO2/FIO2 as ARDS criteria during NIV for decisions related to intubation or for prognosis but suggest great caution for its use during HFNC.
The main physiological reason for these findings is probably the efficiency of PEEP in counteracting alveolar collapse and concomitant shunt, as indicated by the excellent correlation between the change in estimated PEEP and the change in PaO2/FIO2 ratio. However, with a remaining variation of around 65% even the change in PEEP cannot reliably predict the result of a change in ventilatory strategy. Interestingly, PaO2/FIO2 ratio during step-down was markedly better, which probably indicates a well-recruited lung but also the fact that step-down happens when the lung has recovered to some degree. An additional factor which is well-known to affect PaO2/FIO2 ratio is inspired oxygen, which we have not controlled for [11]. This means that some of the difference in PaO2/FIO2 ratio is probably caused by changes in ventilation/perfusion mismatch caused by the change of respiratory strategy. While this could be controlled using a FIO2 of 1.0, this, in turn, would tend to increase absorption atelectasis and therefore the true shunt fraction especially in HFNC [12]. Further, not only the respiratory strategies used, but also the respiratory settings are known to affect PaO2/FIO2 ratio [13]. This means that the mandatory change from spontaneous ventilation to controlled ventilation at intubation will affect the results as well. The relationship between PaO2/FIO2 and FIO2 is influenced by multiple factors, such as the intrapulmonary shunt, arterio-venous difference of oxygen, partial pressure of arterial carbon dioxide, respiratory quotient and hemoglobin as well as the onset of absorption atelectasis [14]. The recognition of these physiological mechanisms as well as our results should prompt the development of more standardized procedures for grading hypoxemia and ARDS severity.
The current study had some limitations. The study focused exclusively on PaO2/FIO2 ratio as a measure of respiratory function, not taking into account the complexity and the multifactorial nature of hypoxic acute respiratory failure and of its management as, for instance, the use of prone positioning, the level of sedation, muscle relaxation or other pharmaceutical interventions. However, when referring to the PaO2/FIO2 ratio in our clinical practice as well as in the Berlin definition of ARDS [1], the PaO2/FIO2 ratio is used as an independent variable, not contextualized to, for instance, patients’ position, hemodynamic, muscle relaxation, sedation. Further, as a single center study, local clinical routines may influence the generalizability of the results.
In conclusion, PaO2/FIO2 ratio, in itself, is not sufficient to grade hypoxemia in ARDS patients during HFNC. PaO2/FIO2 ratio during NIV is a reasonable estimate for actual ARDS grade during MV. There are large individual variations in the effect of changes in ventilatory modality that suggests future ARDS definitions should treat respiratory support strategies separately. Importantly, our findings indicate that clinical trials investigating non-invasive respiratory support in ARDS patients can lead to misinterpretation of these patients’ outcomes. Additional prospective studies of PaO2/FIO2 ratio during HFNO will be needed to fully understand the relation of PaO2/FIO2 ratio to outcomes in patients with and without COVID-19.
Acknowledgements
The authors thank research nurses Joanna Wessbergh and Elin Söderman for their expertise in compiling patient data.
Authors' contributions
All authors participated in project design and planning. MH, OH, RF, ML and MP collected data. MP and MH wrote the first draft. All authors revised the paper and approved the final version for publication.
Funding
Open access funding provided by Uppsala University. The study was funded by the SciLifeLab/Knut and Alice Wallenberg national COVID-19 research program (M.H.: KAW 2020.0182, KAW 2020.0241), the Swedish Heart–Lung Foundation (M.H.: 20210089, 20190639, 20190637, and G.P.: 20200877 and 20200825), the Swedish Research Council (R.F.: 2014-02569, 2014-07606 and G.P.: 2018-02438). The Swedish Society for Medical Research (M.P. 463402221) and the Swedish Society of Medicine (M.P. SLS-959793) and Alvar Gullstrand research grant (G.P.: ALF-938050). Funding bodies had no role in the design of the study, collection and interpretation of data or in the writing of the manuscript.
Availability of data and material
Data are available from the corresponding author on reasonable request (https://doi.org/10.17044/scilifelab.14229410).
Declarations
Ethics approval and consent to participate
The National Ethical Review Agency approved the study (EPM; No. 2020-01623). The Declaration of HELSINKI and its subsequent revisions were followed. Written informed consent was obtained from the patients when possible. Otherwise, informed consent was firstly asked to next to kin and later confirmed by patients if feasible.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Force ADT, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 2.Martin-Rodriguez F, Lopez-Izquierdo R, Del Pozo VC, Delgado-Benito JF, Ortega GJ, Castro Villamor MA, Sanz-Garcia A. Association of prehospital oxygen saturation to inspired oxygen ratio with 1-, 2-, and 7-day mortality. JAMA Netw Open. 2021;4(4):e215700. doi: 10.1001/jamanetworkopen.2021.5700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, Gattinoni L, van Haren F, Larsson A, McAuley DF, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 4.Hill NS, Ruthazer R. Predicting outcomes of high-flow nasal cannula for acute respiratory distress syndrome. An index that ROX. Am J Respir Crit Care Med. 2019;199(11):1300–1302. doi: 10.1164/rccm.201901-0079ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferguson ND, Pham T, Gong MN. How severe COVID-19 infection is changing ARDS management. Intensive Care Med. 2020;46(12):2184–2186. doi: 10.1007/s00134-020-06245-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chertoff J. High-flow oxygen, positive end-expiratory pressure, and the Berlin definition of acute respiratory distress syndrome: are they mutually exclusive? Am J Respir Crit Care Med. 2017;196(3):396–397. doi: 10.1164/rccm.201701-0005LE. [DOI] [PubMed] [Google Scholar]
- 7.Spoletini G, Alotaibi M, Blasi F, Hill NS. Heated humidified high-flow nasal oxygen in adults: mechanisms of action and clinical implications. Chest. 2015;148(1):253–261. doi: 10.1378/chest.14-2871. [DOI] [PubMed] [Google Scholar]
- 8.Bellani G, Pham T, Laffey JG. Missed or delayed diagnosis of ARDS: a common and serious problem. Intensive Care Med. 2020;46(6):1180–1183. doi: 10.1007/s00134-020-06035-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S, Paolo Navalesi Members Of The Steering Committee. Antonelli M, Brozek J, Conti G, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50(2):1602426. doi: 10.1183/13993003.02426-2016. [DOI] [PubMed] [Google Scholar]
- 10.Ranieri VM, Tonetti T, Navalesi P, Nava S, Antonelli M, Pesenti A, Grasselli G, Grieco DL, Menga LS, Pisani L, et al. High flow nasal oxygen for severe hypoxemia: oxygenation response and outcome in COVID-19 patients. Am J Respir Crit Care Med. 2021;205(4):431–439. doi: 10.1164/rccm.202109-2163OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aboab J, Louis B, Jonson B, Brochard L. Relation between PaO2/FIO2 ratio and FIO2: a mathematical description. Intensive Care Med. 2006;32(10):1494–1497. doi: 10.1007/s00134-006-0337-9. [DOI] [PubMed] [Google Scholar]
- 12.Shapiro BA, Cane RD, Harrison RA, Steiner MC. Changes in intrapulmonary shunting with administration of 100 percent oxygen. Chest. 1980;77(2):138–141. doi: 10.1378/chest.77.2.138. [DOI] [PubMed] [Google Scholar]
- 13.Ferguson ND, Kacmarek RM, Chiche JD, Singh JM, Hallett DC, Mehta S, Stewart TE. Screening of ARDS patients using standardized ventilator settings: influence on enrollment in a clinical trial. Intensive Care Med. 2004;30(6):1111–1116. doi: 10.1007/s00134-004-2163-2. [DOI] [PubMed] [Google Scholar]
- 14.Gowda MS, Klocke RA. Variability of indices of hypoxemia in adult respiratory distress syndrome. Crit Care Med. 1997;25(1):41–45. doi: 10.1097/00003246-199701000-00010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the corresponding author on reasonable request (https://doi.org/10.17044/scilifelab.14229410).