Abstract
Background: Estimating the prevalence of depressive and anxiety symptoms among older adults with different health conditions can inform mental health services for this population during the corona virus disease-2019 (COVID-19) pandemic. Method: A search of 12 scientific databases identified 17 studies with 11,237 Chinese older adults who were infected by COVID-19, were generally healthy, or had chronic illnesses. Meta-analysis was used to estimate the overall prevalence of depressive and anxiety symptoms in these three groups. Assessment criteria, region, and time phase of the pandemic were tested as sources of heterogeneity. Results: With an average risk of bias score of 6.71 (range = 6–8), the majority of included studies employed appropriate statistical methods, used validated measurement tools, and had adequate response rates; however, they might have deficiencies in sample frame, sampling method, and sample size. Within the COVID-19, general, and chronic illness groups, the prevalence of depressive symptoms was 27%, 26%, and 61%, respectively, and the prevalence of anxiety symptoms was 14%, 23%, and 85%, respectively. Among generally healthy older adults, anxiety was more prevalent during the Phase 2 (March–April 2020) of the pandemic compared with other time phases. Conclusions: The results have implications for addressing the mental health problems of Chinese older adults, especially those with chronic illnesses, during the COVID-19 pandemic.
Keywords: COVID-19, depressive symptom, anxiety symptom, older adults, prevalence, China
Introduction
At the end of December 2019, a cluster of unexplained pneumonia cases was reported in Wuhan, China, and soon thereafter cases were also found in other parts of the world.1 On 11 March 2020, the World Health Organization2 (WHO) declared corona virus disease-2019 (COVID-19) to be a pandemic. As of 20 April 2021,3 more than 140 million people had been infected and over three million people had died worldwide. The rapid spread of COVID-19 has threatened both the physical and mental health of the public. Researchers and media vividly predicted that COVID-19 would cause a “tsunami” of mental health problems worldwide4,5 and they called for increased awareness of mental health problems under the pandemic.6,7
The older population (individuals aged 60 and above)8 is one of the most vulnerable groups during the pandemic.9,10 They are more susceptible to the virus and have had higher fatality rates once being infected.11,12 Besides, the effects of long-term confinement following the onset of the COVID-19 pandemic can be more unfavorable for older adults. As older adults generally rely on face-to-face communication and lack skills in using electronic devices,13,14 lockdown may largely cut off their connections with the outside world. In addition, older individuals are suffering from ageism as well as devaluing15,16 during the pandemic and have had more difficulties in coping with the COVID-19 information explosion.12,17 These problems have great potential to cause or increase mental health problems (e.g., depression and anxiety) among older populations. Therefore, many institutions and researchers have appealed for more attention to the mental health of the older populations.18,19
There have been mixed results on studies investigating the mental health of older adults during the pandemic. Longitudinal studies20,21 found that loneliness, depression, anxiety, and insomnia significantly increased among older adults after the outbreak of COVID-19. When compared with juveniles and middle-aged adults, older adults showed higher distress; demonstrated more stress responses including anxiety, depression, and physical symptoms; and showed a greater loss of social functioning.22 However, some studies found the reverse trend. In a Chinese nationwide survey,23 results showed that the prevalence of both depressive and anxiety symptoms were negatively correlated with age. Among Chinese COVID-19 survivors, Cai et al.24 found less depressive and anxiety symptoms among the older survivors compared with survivors under 60. Similar findings were also reported among Dutch older adults and older adults with pre-existing depression.25,26 Thus, although older adults might feel lonely or perceive decreased life quality, no significant increases in the prevalence of depressive or anxiety symptoms were found among these studies. These results suggested that instead of being vulnerable, older adults would possibly become the “important anchors in society during this time of sweeping change.”27 In the current study, we tried to rectify these inconsistent results by estimating the prevalence of depressive and anxious symptoms among older people with COVID-19, older people in the general population, and older people with chronic illness.
Depressive and anxiety symptoms are common under states of public health emergency and social isolation.28–30 A meta-analysis30 of 82 studies comparing the prevalence of various psychiatric symptoms during SARS and COVID-19 pandemic found that overall, 23.9% and 23.4% of participants (e.g., health professionals and infected people) demonstrated depressive and anxiety symptoms, respectively, during the COVID-19 pandemic. Other studies showed that these symptoms were common among COVID-19 patients (45% and 47%, respectively),31 front-line medical workers (24.3% and 25.8%, respectively),32 and the general public (34.3% and 38.12%, respectively).33 Specifically, the impact of depressive and anxiety symptoms on older people cannot be ignored. These symptoms are associated with higher frailty (e.g., reduced physiological reserve and increased vulnerability to stressors), more somatization symptoms, decreased functioning, lower well-being, and lower quality of life among older adults,34–39 which may result in higher susceptibility to COVID-19. Despite these possible negative outcomes, the results of recent studies investigating the prevalence of depressive and anxiety symptoms among older adults were inconsistent. In one study,40 around 10% of older adults experienced anxiety symptoms during the pandemic, while in another study41 the prevalence was as high as 57.8%. Similarly, findings on the prevalence of depression ranged widely from 9.1%42 to approximately 40%.21 These mixed findings call for a meta-analysis to synthesize the prevalence data, so as to draw a comprehensive picture of how the COVID-19 pandemic has affected older adults and what factors could contribute to the heterogeneity in these effects.
Particularly, special attention should be given to Chinese older adults. China has the largest older population in the world.19 However, established geriatric mental health services in China seem unable to cope with the challenge posed by COVID-19 pandemic.19,43 In order to provide focalized suggestions to Chinese geriatric mental health services during and after emergencies, it is of significance to target the Chinese older population and understand the impact of the pandemic on their mental health. In sum, this meta-analysis estimated the prevalence of depressive symptoms (depression hereinafter) and anxiety symptoms (anxiety hereinafter) during the COVID-19 pandemic among Chinese older adults with different physical health conditions (i.e., COVID-19 patients, older adults from general public, and those with chronic illnesses), and explored potential sources of between-study heterogeneity through subgroup analysis of screening criteria, regions, and time phase of the pandemic.
Method
The research was conducted and reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist (see Supplementary Materials 1).44 Meta-analyses protocol has been registered on PROSPERO (CRD42021240664).
Search strategy
Two authors (YY and DX) systematically searched for relevant literature in electronic databases, namely, PubMed, Web of Science, Embase, Scopus, Academic Search Premier, PsycINFO, PsycARTICLES, Psychology and Behavioral Sciences Collection, China National Knowledge Infrastructure, Wanfang Standards Database, and CQVIP. Preprint articles published on Medrxiv servers were also included. The search covered the literature up to March 2021. Based on the CoCoPop mnemonic,45 search terms used were: Condition (depression OR depressive OR depressed OR anxiety OR anxious OR “mental health” OR psychological) AND Context (“COVID-19” OR coronavirus OR “2019-ncov” OR “sars-cov-2” OR “cov-19” OR “2019 pandemic”) AND Population (old OR older OR elderly OR geriatric OR geriatrics OR aging OR senior OR seniors) AND Region (China OR Chinese OR mainland OR “Hong Kong” OR Taiwan OR Macao). The full search strategy and an example search can be found in Supplementary Materials 2. In addition, we screened the references of included studies to expedite the identification of eligible research.
Selection procedure and data extraction
The title and abstract of studies identified through the database searches were reviewed to ascertain whether the study potentially met the inclusion criteria; if so, the full text was then examined. Two authors (YY and DX) independently determined if the study should be included in the meta-analysis, and disagreement was resolved by discussion with the research team.
Inclusion criteria were that the study: (a) reported the prevalence of depressive and/or anxiety symptoms, or sufficient information to compute these, and was conducted during the COVID-19 outbreak with an observational design (i.e., quantitative studies that are designed to assess relations among variables rather than intervene experimentally); (b) studied Chinese participants aged 60 and above who were recruited from Mainland China, Hong Kong, Macau, or Taiwan (we also considered studies on the Chinese general public that reported separate data on older participants); (c) utilized standardized and validated scales to measure the mental health status of the participants; and (d) was written in English or Chinese.
Exclusion criteria were that the study: (a) was review article, case report, commentary, book, conference paper, and other document that did not present empirical findings with detailed method illustrations and (b) focused on other specialized groups (e.g., medical workers and Chinese older adults living abroad).
Data were extracted independently by the two authors of this paper (YY and DX), and coding discrepancies were resolved by discussion among all authors. Each primary study was coded based on the following characteristics: (a) identification of the study (title, first author’s name, publication year, and date of data collection); (b) methodological characteristics (study design, sampling method, sample size, and response rate for questionnaire); (c) sample characteristics (region and physical health conditions); and (d) assessment criteria and outcome (scales for depression and/or anxiety, cut-offs, and prevalence of depression and/or anxiety). In case of insufficient information (e.g., cut-offs for scales and sample sizes for each cut-off group) on the published article, data were obtained via email contact with authors.
Risk of bias assessment
Risk of bias for each included study was assessed using the Joanna Briggs Institute (JBI) Critical Appraisal Instrument for prevalence studies (see Supplementary Materials 3).45 This instrument consists of nine items, each yielding a score of 0 or 1, with the total score ranging from 0 to 9. Each study was rated independently by two authors (YY and DX) and discrepancies were resolved via discussion between the two evaluators. The Spearman correlation coefficient of 0.744 (p < 0.001) indicated high inter-rater reliability.46 All disagreements were resolved through discussion between the two raters until consensus was reached.
Statistical analysis
We used R software Version 4.0.4 (http://www.R-project.org), RStudio software version 1.4.1106 (https://rstudio.com/products/rstudio), and the “meta” package version 4.18-0 (https://CRAN.R-project.org/package=meta) to perform statistical analyses. Our main outcomes were the pooled prevalence of depressive symptoms and anxiety symptoms with their 95% confidence intervals (CIs). A one-step approach in generalized linear mixed models (GLMMs)47 with logit link was used for synthesizing proportions. Using GLMMs in proportional meta-analysis can account for within-study uncertainties and does not require corrections for zero counts.48,49 This method thus leads to smaller biases and mean squared errors, and higher coverage probabilities, than traditional two-step methods such as log and Freeman–Tukey double-arcsine transformations.
The studies included in this meta-analysis were conducted in diverse populations and regions, and there were different assessment methods across studies. Therefore, random-effect models were used to estimate the pooled prevalence of depressive and anxiety symptoms among Chinese older adults with different health conditions. Cochran’s Q and Tau2 were used as tests of heterogeneity, with a p value of <0.05 considered an indication of substantial heterogeneity. We also reported the I2 statistic, with I2 > 50% indicating significant heterogeneity. When there was significant heterogeneity, subgroup analyses were conducted on assessment criteria, regions, and time phase (revealed by date of data collection), to explore the potential sources. Publication bias was determined through visual inspection of the asymmetry of the funnel plot, and the asymmetry was tested empirically using Egger’s regression test.50 Bias was considered significant when the p value was <0.05.
Results
Study characteristics
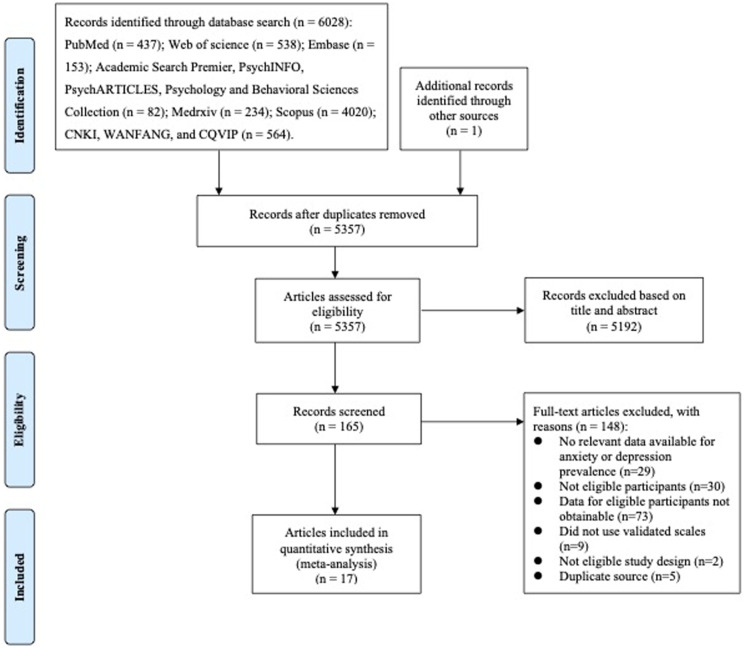
A total of 17 studies with 11,237 older adult participants were included in the meta-analysis. Among them, 11 reported the prevalence of both depressive symptoms and anxiety symptoms,21,24,41,42,51–57 three reported only the prevalence of depressive symptoms58–60 and three reported only the prevalence of anxiety symptoms.61–63 The flow diagram of the study is depicted in Figure 1. Details for each study are shown in Table 1.
Figure 1.
PRISMA flow diagram.
Table 1.
Characteristic table for included studies.
| Author (year) | Region | Sampling method | Date of data collection (time phase of the pandemic) | Sample size | Population | Assessment | Cut-off | Outcome | Quality score | |
|---|---|---|---|---|---|---|---|---|---|---|
| Depression %(n) | Anxiety %(n) | |||||||||
| Cai et al.24 | Mainland China | — | Feb 20–Mar 15 (2) | 26 | COVID-19 patients | SDS | ≥53 | 46.15% (12) | 11.53% (3) | 6 |
| SAS | ≥50 | |||||||||
| Chen et al.61 | Mainland China | Convenience sampling | Jan 31–Feb 2 (1) | 58 | General public | GAD-7 | ≥10 | — | 18.96% (11) | 6 |
| Chen et al.62 | Mainland China | Judgment sampling | Aug 20–Aug 23 (3) | 49 | COVID-19 patients (34); general public (15) | STAI | S ≥ 53 | — | 8.00% (4) | 7 |
| Choi et al.51 | Hong Kong China | Random sampling | Apr 24–May 3 (2) | 136 | General public | PHQ-9 | ≥5 | 47.06% (64) | 44.85% (61) | 8 |
| GAD-7 | ≥10 | |||||||||
| Dai et al.52 | Mainland China | Convenience sampling | Feb 23–Feb 26 (1) | 32 | COVID-19 patients | SDS | ≥53 | 9.38% (3) | 12.50% (4) | 7 |
| SAS | ≥50 | |||||||||
| Fong et al.58 | Hong Kong China | Convenience sampling | Apr 24–May 13 (3) | 42 | COVID-19 patients | PHQ-9 | ≥5 | 28.57% (12) | — | 6 |
| Li et al.53 | Mainland China | Convenience sampling | Feb 18–Mar 18 (2) | 26 | COVID-19 patients | HADS | D ≥ 8 | 53.80% (14) | 23.1% (6) | 6 |
| A ≥ 8 | ||||||||||
| Li et al.54 | Mainland China | Snowball sampling | Mar 1 to 31 (2) | 48 | General public | PHQ-2 | ≥2 | 31.3% (15) | 45.8% (22) | 6 |
| GAD-7 | ≥5 | |||||||||
| Liang et al.59 | Mainland China | Snowball sampling | Jun 15–Jul 10 (3) | 516 | General public | CESD-10 | ≥10 | 31% (159) | — | 7 |
| Liu et al.60 | Mainland China | Snowball sampling | Jan 30–Feb 3 (1) | 5 | General public | SDS | ≥53 | 0% (0) | — | 6 |
| Ren et al.55 | Mainland China | Convenience sampling | — | 92 | General public | GDS-15 | ≥8 | 19.57% (18) | 28.26% (26) | 6 |
| GAD-7 | ≥5 | |||||||||
Note. SDS: Self-Rating Depression Scale; SAS: Self-Rating Anxiety Scale; GAD-7: Generalized Anxiety Disorder-7; STAI: State-Trait Anxiety Inventory; PHQ-9: Patient Health Questionnaire-9; PHQ-2: Patient Health Questionnaire-2; GAD-2: Generalized Anxiety Disorder-7; HADS: Hospital Anxiety and Depression Scale; CESD-10: Center for Epidemiological Studies Depression Scale-10; GDS-15: Geriatric Depression Scale-15.
Prevalence of depressive and anxiety symptoms during the COVID-19 pandemic
Due to the unneglectable heterogeneity among older adults with different health conditions, we identified three sub-populations: older adults infected by COVID-19, older adults from the public that are generally healthy, and older adults with chronic disease. The results were presented separately for each group.
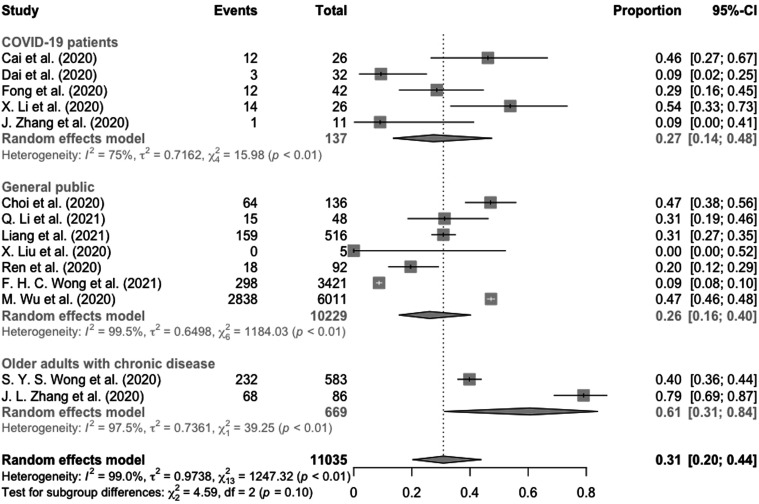
Of the 17 included studies, 14 reported the prevalence of depression. Five studies24,42,52,53,58 were conducted on older COVID-19 patients. In this group, the pooled prevalence of depression was 27% (95% CI: 14%–48%, I2 = 75%). Seven studies41,51,54,55,57,59,60 were conducted on older adults from the general public, and the pooled prevalence of depression was 26% (95% CI: 16%–40%, I2 = 99.5%). Older adults in the remaining two studies21,56 were those with chronic disease, and the pooled prevalence of depression was 61% (95% CI: 31%–84%, I2 = 97.5%). Details about the pooled prevalence of depression for each older adult group were presented in Figure 2.
Figure 2.
Prevalence of depression among Chinese older adults with different health conditions.
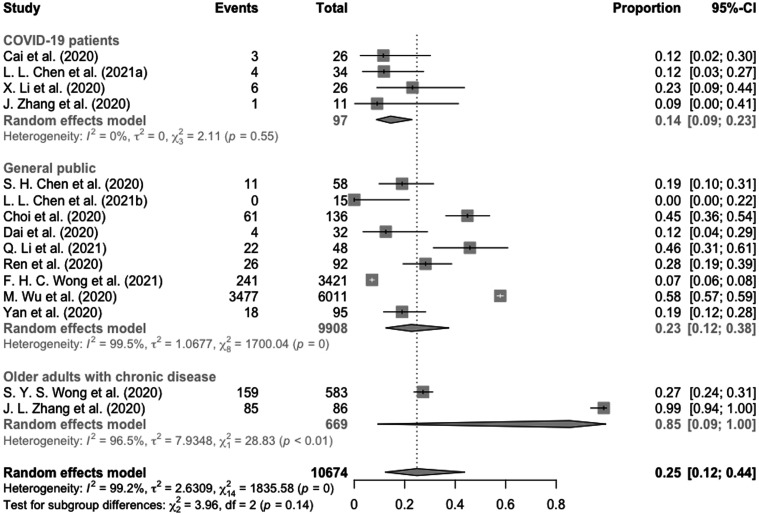
Of the 17 included studies, 14 studies reported the prevalence of anxiety. One study62 reported separate results for older adults with COVID-19 and older adults from the general public; therefore, 15 samples were used to estimate the prevalence of anxiety. Four studies24,42,53,62 were conducted in a sample of older COVID-19 patients and the pooled prevalence of anxiety was 14% (95% CI: 9%–23%, I2 = 0%); nine studies41,51,52,54,55,57,61–63 were conducted on older adults from the general public, with a pooled prevalence of anxiety of 23% (95% CI: 12%–38%, I2 = 99.5%); older adults in the remaining two studies21,56 were those with chronic disease, and the pooled prevalence of anxiety in the two samples was 85% (95% CI: 9%–100%, I2 = 96.5%). Details of the pooled prevalence of anxiety for each group of older adults were presented in Figure 3.
Figure 3.
Prevalence of anxiety among Chinese older adults with different health conditions.
Subgroup analyses in prevalence of depressive symptoms during the COVID-19 pandemic
When a set of studies showed significant heterogeneity, we conducted subgroup analysis to determine the source of the heterogeneity. First, we tested whether different prevalence estimates were obtained based on the measure and cut-offs used to identify symptoms. Second, we compared prevalence estimates from Mainland China and Hong Kong China. Third, we compared prevalence estimates based on time of data collection. According to Allan et al.64 and the epidemiological characteristics of COVID-19 in China,65 we set three phases, that is, Phase 1 (January–February 2020), Phase 2 (March–April 2020), and Phase 3 (May–August 2020). Considering the small number of studies on older adults with chronic illnesses, these subgroup analyses were conducted separately only for two groups (COVID-19 and general public).
For studies of older COVID-19 patients, there was significant heterogeneity in estimated prevalence (I2 = 75%, p < 0.01). Therefore, potential sources of heterogeneity were tested. However, no significant difference was found between studies using different criteria (p = 0.95) or between patients from different regions (p = 0.87). In addition, although the prevalence of depressive symptoms for older COVID-19 patients was higher during Phase 2 of the pandemic (38%, 95% CI: 19%–62%)24,42,53 than in Phase 3 (29%, 95% CI: 17%–44%)58 and in Phase 1 (9%, 95% CI: 3%–25%),52 only a marginally significant difference was found (p = 0.06). Details of the comparisons were presented in Table 2. For studies dealing with older adults from general public (I2 = 99.5%, p < 0.01), we did not conduct quantitative comparisons to investigate estimates based on different assessment criteria as there were not enough studies for each assessment subgroup. Quantitative subgroup analysis on this subpopulation showed that no significant differences were found between older adults from different regions (p = 0.61) and between prevalence estimated in different phases of the pandemic (p = 0.11). Details of the comparisons were presented in Table 2.
Table 2.
Subgroup analysis for prevalence of depression.
| Population | No. of studies | Events | Total | Proportion (95% CI) | Heterogeneity | ||||
|---|---|---|---|---|---|---|---|---|---|
| I2 | Tau2 | Chi2(p) | |||||||
| COVID-19 patients | |||||||||
| Criteria | |||||||||
| SDS≥ 53 | 2 | 15 | 58 | 23% (6%–58%) | 88.3% | 0.949 | 8.56 (p < 0.01) | ||
| HADS-D≥ 8 | 2 | 15 | 37 | 30% (7%–71%) | 79.2% | 1.0771 | 4.81 (p < 0.05) | ||
| PHQ-9≥ 5 | 1 | 12 | 42 | 29% (17%–44%) | — | — | — | ||
| Between-groups | 0.11 (p = 0.95) | ||||||||
| Region | |||||||||
| Mainland China | 4 | 30 | 95 | 26% (10%–53%) | 80% | 1.0629 | 15 (p < 0.01) | ||
| Hong Kong China | 1 | 12 | 42 | 29% (17%–44%) | — | — | — | ||
| Between-groups | 0.03 (p = 0.87) | ||||||||
| Time phase | |||||||||
| Phase 1 | 1 | 3 | 32 | 9% (3%–25%) | — | — | — | ||
| Phase 2 | 3 | 27 | 63 | 38% (19%–62%) | 58.4% | 0.38 | 4.81 (p = 0.09) | ||
| Phase 3 | 1 | 12 | 42 | 29% (17%–44%) | — | — | — | ||
| Between-groups | 5.51 (p = 0.06) | ||||||||
| Older adults from general public | |||||||||
| Region | |||||||||
| Mainland China | 5 | 3030 | 6672 | 30% (21%–42%) | 94.8% | 0.2243 | 76.31 (p < 0.01) | ||
| Hong Kong China | 2 | 362 | 3557 | 22% (6%–57%) | 99.3% | 1.229 | 150.06 (p < 0.01) | ||
| Between-groups | 0.25 (p = 0.61) | ||||||||
| Time phase | |||||||||
| Phase 1 | 2 | 2838 | 6016 | 27% (1%–90%) | 0% | 1.1516 | 0 (p = 1.00) | ||
| Phase 2 | 2 | 79 | 184 | 41% (31%–53%) | 71.9% | 0.041 | 3.56 (p = 0.06) | ||
| Phase 3 | 2 | 457 | 3937 | 17% (7%–37%) | 99.5% | 0.5868 | 185.92 (p < 0.01) | ||
| Between-groups | 4.37 (p = 0.11) | ||||||||
Subgroup analyses in prevalence of anxiety symptoms during the COVID-19 pandemic
The homogeneity among samples of older COVID-19 patients reporting prevalence of anxiety were not significant (I2 = 0%, p = 0.55). However, further subgroup analysis showed that neither assessment criteria (p = 0.62) nor time phases of the pandemic (p = 0.58) can account for the heterogeneity. Details of the comparisons were presented in Table 2. Effect of regions on between-study heterogeneity was not tested as all the included patients within these samples were from Mainland China. Of the nine samples of older adults from general public (I2 = 99.5%, p = 0), we did not conduct quantitative comparisons to investigate estimates based on different assessment criteria as there were not enough studies for each assessment subgroup. Though date of data collection was unavailable in Ren, et al,55 quantitative subgroup analysis on the rest showed a significant difference (p < 0.01) among samples collected in different phases of the pandemic. Particularly, the prevalence of anxiety among older adults from general public was highest during the Phase 2 of the pandemic (45%, 95% CI: 38%–52%), followed by Phase 1 (25%, 95% CI: 12%–46%) and Phase 3 (7%, 95% CI: 6%–8%). Whereas, region was not a significant source of heterogeneity on prevalence of anxiety among older adults from general public (p = 0.78). Details of the comparisons were presented in Table 3.
Table 3.
Subgroup analysis for prevalence of anxiety.
| Population | No. of studies | Events | Total | Proportion (95% CI) | Heterogeneity | ||||
|---|---|---|---|---|---|---|---|---|---|
| I2 | Tau2 | Chi2(p) | |||||||
| COVID-19 patients | |||||||||
| Criteria | |||||||||
| HADS-A ≥ 8 | 2 | 7 | 37 | 19% (9%–35%) | 0% | 0 | 0.92 (p = 0.34) | ||
| SAS ≥50 | 1 | 3 | 26 | 12% (4%–30%) | — | — | — | ||
| STAI-S ≥ 53 | 1 | 4 | 34 | 12% (4%–27%) | — | — | — | ||
| Between-groups | 0.96 (p = 0.62) | ||||||||
| Time phase | |||||||||
| Phase 2 | 2 | 10 | 63 | 16% (9%–27%) | 0% | 0 | 1.68 (p = 0.43) | ||
| Phase 3 | 3 | 4 | 34 | 12% (4%–27%) | — | — | — | ||
| Between-groups | 0.3 (p = 0.58) | ||||||||
| Older adults from general public | |||||||||
| Region | |||||||||
| Mainland China | 7 | 3558 | 6351 | 24% (13%–41%) | 95% | 0.8677 | 119.28 (p < 0.01) | ||
| Hong Kong China | 2 | 302 | 3557 | 20% (5%–56%) | 99.4% | 1.3912 | 164.73 (p < 0.01) | ||
| Between-groups | 0.08 (p = 0.78) | ||||||||
| Time phase | |||||||||
| Phase 1 | 4 | 3510 | 6196 | 25% (12%–46%) | 96.7% | 0.7572 | 89.85 (p < 0.01) | ||
| Phase 2 | 2 | 83 | 184 | 45% (38%–52%) | 0% | 0 | 0.01 (p = 0.91) | ||
| Phase 3 | 2 | 241 | 3436 | 7% (6%–8%) | 0% | 0 | 0 (p = 1.00) | ||
| Between-groups | 221.42 (p < 0.01) | ||||||||
Descriptive analysis of depressive and anxiety symptoms in older adults with chronic illnesses
Only two studies reporting prevalence of depressive and anxiety symptoms focused on older adults with chronic disease. The number of studies was too small to conduct quantitative subgroup analyses. Descriptively, a study21 collected data during Phase 2 in Hong Kong China, using PHQ-9 ≥ 10 as the indicator of depressive symptoms, reported an estimate of 40% (95% CI: 36%–44%). To identify anxiety symptoms, this study used assessment criteria of GAD-7 ≥ 5 and the prevalence rate was 27% (95% CI: 24%–31%). Another study56 on older adults with chronic illnesses was conducted in Mainland China. However, the date of data collection was unavailable. Using SDS ≥53 to identify depressive symptoms, they reported the prevalence estimate was 79% (95% CI: 31%–84%). To identify anxiety symptoms, they used criterion of SAS ≥50 and the estimated prevalence was 99% (95% CI: 9%–100%).
Risk of bias assessment and publication bias
The average risk of bias score of the 17 included studies was 6.71 (range = 6–8) (see Supplementary Materials 4). Based on the results, the majority of included studies employed appropriate statistical methods, used validated measurement tools, and had adequate response rates, their most common limitations were: (a) inappropriate sample frame24,42,53,54,56–60; (b) inappropriate sampling methods41,42,53–63; and (c) insufficient sample size 24,52–56,58,60–63 Visual inspection of the funnel plots (see Supplementary Materials 5 and 6) and the nonsignificant results of Egger’s tests (depressive symptoms: bias = −2.4337, t = −0.72, p > 0.05; anxiety symptoms: bias = −4.92, t = −1.43, p > 0.05; see Supplementary Materials 7 and 8) indicated absence of asymmetry in funnel plots. These results provided evidence that there was no publication bias in our included studies.
Discussion
To our knowledge, this work was the first systematic review and meta-analysis that assessed the prevalence of depressive and anxiety symptoms among older COVID-19 patients, generally healthy older adults, and older adults with chronic disease during the COVID-19 pandemic. The majority of included studies employed appropriate statistical methods, used validated measurement tools, and had adequate response rates; however, they might have had deficiencies in sample frame, sampling method and sample size. After analyzing data from 17 studies with 11,237 older participants, we found that during the COVID-19 pandemic, depressive and anxiety symptoms were common among Chinese older adults, especially among those with chronic illness.
The overall prevalence of depressive symptoms was 27%, 26%, and 61% in older COVID-19 patients, older adults from general public, and older adults with chronic illnesses, respectively. Though a between-group comparison was not significant, the large absolute difference between older adults with chronic illnesses and those without suggested a need for further study. For anxiety symptoms, the prevalence was 14%, 23%, and 85% for older COVID-19 patients, older adults from general public, and older adults with chronic illnesses, respectively. Similarly, anxiety was much more prevalent among older adults with chronic illnesses than among older COVID-19 patients and those from general public, though the difference was not significant. Chronic illnesses, such as hypertension, heart disease, diabetes, and osteoarthropathy, can cause great inconvenience to older adults’ daily lives, and suffering from these chronic diseases has been found to be a significant factor leading to depression and anxiety among older adults.66, 67 After the outbreak of COVID-19, China quickly instituted a massive lockdown, and this may have cut down access to regular clinic visits and medicine for chronic disease patients.13, 14 With chronic illnesses and deteriorated health conditions, they are more prone to be infected by the virus and, worse still, they may face higher death rates due to fatal comorbidities if infected.12 Besides, chronic disease patients may actively seek information about COVID-19 virus due to their past disease history, while with limited resources, they might form an incomplete and one-sided picture of the pandemic.68 As older adults in the two included studies21,56 focused on chronic illnesses patients were recruited from clinical care settings with more than one chronic illness, the above factors can possibly account for their peculiarly high prevalence of depressive and anxiety symptoms.
However, when compared with the 25.55% prevalence of depression during 2010–2019,69 the 25.2% prevalence of anxiety in 201670 and 11.77% prevalence of anxiety in 201871 among Chinese older adults, there seems to be no substantial increase of depressive and anxiety symptoms among older adults without chronic disease after the outbreak of COVID-19, even after having been infected. These findings were consistent with some previous studies.24,72 As older adults are entering their twilight years, they are motivated by a limited remaining lifetime to pursue life meaning and satisfaction to gain more positive emotional experience; therefore, they are able to cope with the life-threatening virus with better emotional regulation and strategies.73 Besides, as suggested by the Strength and Vulnerability Integration model (SAVI),74 older adults may demonstrate higher levels of resilience and life strength facing the pandemic because of their rich life experience.
Subgroup analysis revealed that among older adults from general public, the prevalence of anxiety symptoms was significantly different across phases of the pandemic. Specifically, anxiety symptoms were more prevalent during Phase 2, followed by Phase 1 and then Phase 3. Similarly, among COVID-19 patients, prevalence of depressive symptoms was highest during Phase 2 of the pandemic, compared with Phases 3 and 1, though the difference was only marginally significant. According to Pasnau and Fawzy,75 such findings may indicate that during the early stage of the pandemic, older adults showed uncertainty toward the virus while hoping for quick recovery. However, due to the fluctuations of the pandemic and its later negative impacts, older adults might have become more depressed and anxious as their optimism waned and prolonged stress resulted in exhaustion. But from May 2020 on, the Chinese situation was well controlled due to the efforts of the government and the public. This might have assured the older population, who might then have shown fewer depressive and anxiety symptoms.
Furthermore, region was not a significant source of heterogeneity for studies reporting prevalence of depressive and anxiety symptoms among COVID-19 patients and older adults from the general public. This might be because emotional stability, resilience and life strength are common among older people26,76; thus, when facing this pandemic,2 they reacted similarly regardless of where they lived. Though subgroup analysis showed that there was no significant difference between different assessment criteria, we did find a pattern of higher prevalence of depressive symptoms based on the criteria of PHQ-9 ≥ 5 and HADS-D ≥ 8 than other criteria among COVID-19 patients and older adults from the general public. The similar prevalence recognized by these two criteria was consistent with previous study.77 However, with higher prevalence recognized, scales of PHQ-9 and HADS-D may be less valid as one study78 suggested that, raising cut-offs to 8–11 for PHQ-9 can increase its validity but at the cost of lower prevalence and more potential missing cases.
This meta-analysis has several limitations. First, we only included “depression” and “anxiety” in original search terms, and relevant adjectives such as depressive or depressed were missing. A complementary search was conducted in Google Scholar using updated search terms (shown as the Method section) and the results showed that no qualified studies were omitted. Second, heterogeneity of variance still existed even after subgroup analyses were conducted, the small number of included studies would probably take the blame. Furthermore, quantitative analysis was not available for older adults with chronic illnesses as there were only two included studies. Therefore, results for this subpopulation were tentative and future studies were needed to gain deeper insight.
This study has several strengths and implications for clinical services. Having taken cultural factors into consideration, we only focused on the Chinese older population. Our research has focalized implications for Chinese geriatric mental health services in the post-pandemic period as well as future public health disasters. Specifically, we found depressive and anxiety symptoms were prevalent in older populations, especially among older adults with chronic illnesses. As psychological services for older adults in China are limited, these results call for massive, early and effective deployment of mental health aid for Chinese older adults to prevent the later outbreak of mental health problems. Particularly, special attention should be paid to those with chronic illnesses.
In conclusion, our study provides a snapshot of the mental health impact of the COVID-19 pandemic on Chinese older adults with different health conditions. During the pandemic, roughly one fourth of older adults in general population and of older adults infected by COVID-19 reported depressive symptoms (26% and 27%, respectively), while prevalence of depressive symptoms was as high as 61% among the older adults with chronic illnesses. Anxiety was also prevalent among older adults during the pandemic (14% for COVID-19 patients; 23% for adults in the general public). The presence of anxiety symptoms was especially high among older adults with chronic disease (85%) and among older adults from the general public during the phase 2 of the pandemic (45%). Considering the negative psychological impacts of the pandemic, large-scale and timely mental health services for older adults are necessary to prevent the outbreak of a mental health tsunami following the acute phase of the pandemic. Particular attention should be paid to older adults with chronic diseases and more studies focusing on mental health are needed on this subpopulation.
Supplemental Material
Supplemental Material, sj-pdf-1-jgp-10.1177_08919887221078556 for Prevalence of depressive and anxiety symptoms among Chinese older adults during the COVID-19 pandemic: A systematic review and meta-analysis by Yifei Yan, Xiayu Du, Lizu Lai, Zhihong Ren and Hua Li in Journal of Geriatric Psychiatry and Neurology
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Self-determined Research Funds of Central China Normal University grant number CCNU20TD001 and the Key Program of Institute of Wuhan Studies of Jianghan University grant number IWHS20201007.
Supplemental material: Supplemental material for this article is available online.
ORCID iDs
Yifei Yan https://orcid.org/0000-0001-9014-6262
References
- 1.Su Z, Mcdonnell D, Ahmad J, et al. Time to stop the use of ‘Wuhan virus’, ‘China virus’ or ‘Chinese virus’ across the scientific community. Br Med J Glob Health 2020; 5(9): 3746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . WHO director-general’s opening remarks at the. Media briefing on COVID-19–11 March 2020. Geneva, Switzerland: World Health Organization, https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-COVID-19—11-march-202 (2020, accessed 23 May 2021). [Google Scholar]
- 3.World Health Organization . WHO coronavirus (COVID-19) dashboard. Geneva, Switzerland: World Health Organization. https://covid19.who.int/ (2020, Accessed20 April 2020). [Google Scholar]
- 4.BDC News . COVID-19 may cause global Tsunami of mental health problems, 2020. Sudbury, MA: BDC News, http://bdc-tv.com/COVID-19-may-cause-global-tsunami-of-mental-health-problems/ (2020, accessed23 May 2021). [Google Scholar]
- 5.Riedel-Heller S, Richter D. COVID-19 pandemic and mental health of the general public: is there a tsunami of mental disorders? Psychiatrische Praxis 2020; 47(8): 452–456. [DOI] [PubMed] [Google Scholar]
- 6.National Health Commission . Notice on the issuance of guidelines for emergency psychological crisis intervention in the novel coronavirus pneumonia epidemic. Beijing, China: National Health Commission, http://www.nhc.gov.cn/jkj/s3577/202001/6adc08b966594253b2b791be5c3b9467.shtml (2020, accessed 23 May 2021). [Google Scholar]
- 7.World Health Organization . COVID-19 and the need for action on mental health, 2020, https://www.un.org/sites/un2.un.org/files/un_policy_brief-covid_and_mental_health_final.pdf (2020, accessed 23 May 2021). [Google Scholar]
- 8.Standing Committee of the National People’s Congress . Law of the people’s republic of China on the protection of the rights and interests of the elderly, http://pkulaw.cn/fulltext_form.aspx?Gid=328224 (2018, accessed 29 December 2018). [Google Scholar]
- 9.Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health 2020; 5(5): e256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clark A, Jit M, Warren-Gash C, et al. How many are at increased risk of severe COVID-19 disease? rapid global, regional and national estimates for 2020. BMJ 2020. 10.1101/2020.04.18.20064774. [DOI] [Google Scholar]
- 11.Wu Z, Mcgoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA 2020; 323: 1239–1242. [DOI] [PubMed] [Google Scholar]
- 12.Cheng Y, Li J, Peng Z, et al. Analysis on prevention and control of some infectious diseases in the elderly aged 60 years and above in China and countermeasure recommendation. Chin J Epidemiol 2020; 42(1): 28–32. [DOI] [PubMed] [Google Scholar]
- 13.Vahia IV. COVID-19, aging, and mental health: lessons from the first six months. Am J Geriatr Psychiatry 2020; 28(7): 691–694, DOI: 10.1016/j.jagp.2020.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Webb L. COVID‐19 lockdown: a perfect storm for older people’s mental health. J Psychiatry Ment Health Nurs 2021; 28(2): 300, DOI: 10.1111/jpm.12644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brooke J, Jackson D. Older people and COVID-19: isolation, risk and ageism. J Clin Nurs 2020; 29(13–14): 2044–2046, DOI: 10.1111/jocn.15274 [DOI] [PubMed] [Google Scholar]
- 16.Borelli WV, Xavier LDL, Ornell F, et al. The hidden stigma of aging and COVID-19: aggravating factors and strategies to mitigate the impact of the pandemic in older adults, a text mining analysis. Aging Ment Health 2021;1-9. doi: 10.1080/13607863.2021.1910793. [DOI] [PubMed] [Google Scholar]
- 17.Zhao W, Zhang Y, Liu X, et al. Comorbid depressive and anxiety symptoms and frailty among older adults: findings from the West China health and aging trend study. J Affect Disord 2020; 277: 970–976, DOI: 10.1016/j.jad.2020.08.070 [DOI] [PubMed] [Google Scholar]
- 18.National Health Commission . Normal epidemic prevention and control should pay attention to the mental health of key population (Transcript of the press conference on May 15, 2020). Beijing, China: National Health Commission, http://www.nhc.gov.cn/xcs/s3574/202005/e25ee419ae2746c88cdcd641acf73410.shtml (2020, accessed 23 May 2021). [Google Scholar]
- 19.Yang Y, Li W, Zhang Q, et al. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry 2020; 7(4): e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krendl AC, Perry BL. The impact of sheltering-in-place during the COVID-19 pandemic on older adults’ social and mental well-being. J Gerontol Ser B Psychol Sci Soc Sci 2020; 76(2): e53–e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong SYS, Zhang D, Sit RWS, et al. Impact of COVID-19 on loneliness, mental health, and health service utilisation: a prospective cohort study of older adults with multimorbidity in primary care. Br J Gen Pract 2020; 70(700): e817–e824. DOI: 10.3399/bjgp20X713021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qiu J, Shen B, Zhao M, et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry 2020; 33(2): e100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang C, Song W, Hu X, et al. Depressive, anxiety, and insomnia symptoms between population in quarantine and general population during the COVID-19 pandemic: a case-controlled study. BMC Psychiatry 2021; 21(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cai X, Hu X, Otte EI, et al. Psychological distress and its correlates among COVID-19 survivors during early convalescence across age groups. Am J Geriatr Psychiatry 2020; 28(10): 1030–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Tilburg TG, Steinmetz S, Stolte E, et al. Loneliness and mental health during the COVID-19 pandemic: a study among dutch older adults. J Gerontol Ser B Psychol Sci Soc Sci 2020; 76(7): e249–e255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hamm ME, Brown PJ, Karp JF, et al. Experiences of American older adults with pre-existing depression during the beginnings of the COVID-19 pandemic: a multicity, mixed-methods study. Am J Geriatr Psychiatry 2020; 28(9): 924–932, DOI: 10.1016/j.jagp.2020.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lind M, Bluck S, McAdams D. More vulnerable? the life story approach highlights older peoples’ potential for strength during the pandemic. J Gerontol B Psychol Sci Soc Sci 2020; 76(2): e45–e48. DOI: 10.1093/geronb/gbaa105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang MY, Liu XL, Guo H, et al. Mental health of middle-aged and elderly population during outbreak of coronavirus disease 2019. Chin J Mult Organ Dis Elder 2020; 19(4): 241–245. [Google Scholar]
- 29.Liu TB, Chen XY, Miao GD, et al. Suggestions on diagnostic criteria and prevention of SARS related mental disorders. J Clin Psychol Med 2003; 3: 188–191. [Google Scholar]
- 30.Zhao Y-J, Jin Y, Rao WW, et al. The prevalence of psychiatric comorbidities during the SARS and COVID-19 epidemics: a systematic review and meta-analysis of observational studies. J Affective Disord 2021; 287(6): 145–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deng J, Zhou F, Hou W, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID‐19 patients: a meta‐analysis. Ann New York Acad Sci 2020; 1486(1): 90–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salari N, Khazaie H, Hosseinian-Far A, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health 2020; 18(100): 100–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Necho M, Tsehay M, Birkie M, et al. Prevalence of anxiety, depression, and psychological distress among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Int J Soc Psychiatry 2021; 67: 892–906. [DOI] [PubMed] [Google Scholar]
- 34.Alegria A, Hasin D, Nunes E, et al. Comorbidity of generalized anxiety disorder and substance use disorders: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry 2010; 71(09): 1187–1195. DOI: 10.4088/JCP.09m05328gry [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beekman ATF, Penninx BWJH, Deeg DJH, et al. The impact of depression on the well‐being, disability and use of services in older adults: a longitudinal perspective. Acta Psychiatr Scand 2010; 105(1): 20–27. [DOI] [PubMed] [Google Scholar]
- 36.Bourland SL, Stanley MA, Snyder AG, et al. Quality of life in older adults with generalized anxiety disorder. Aging Ment Health 2000; 4(4): 315–323. DOI: 10.1080/713649960 [DOI] [Google Scholar]
- 37.Dong L, Freedman VA, Mendes de Leon CF. The association of comorbid depression and anxiety symptoms with disability onset in older adults. Psychosomatic Med 2020; 82(2): 158–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol 2009; 5(1): 363–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wilkinson P, Ruane C, Tempest K. Depression in older adults. BMJ 2018; 363: k4922. DOI: 10.1136/bmj.k4922 [DOI] [PubMed] [Google Scholar]
- 40.Wang ZH, Qi SG, Zhang H, et al. Impact of the COVID-19 epidemic on anxiety among the elderly in community. Natl Med J China 2020; 100(40): 3179–3185. [DOI] [PubMed] [Google Scholar]
- 41.Wu M, Han H, Lin T, et al. Prevalence and risk factors of mental distress in China during the outbreak of COVID: a national cross-sectional survey. Brain Behav 2020; 10(11): e01818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang J, Yang Z, Wang X, et al. The relationship between resilience, anxiety, and depression among patients with mild symptoms of COVID in China: a cross-sectional study. J Clin Nurs 2020; 29(21): 4020–4029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang A, Kong D, Jiang L, et al. Understanding the effectiveness of psychosocial services for anxiety and depression in Chinese older adults: a systematic review and meta-analysis of controlled trials. Gerontologist 2019; 60(1): e76–e92. [DOI] [PubMed] [Google Scholar]
- 44.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Plos Med 2009; 6(7): e1000100. DOI: 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Munn Z, Moola S, Lisy K, et al. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Health 2015; 13(3): 147–153. [DOI] [PubMed] [Google Scholar]
- 46.Altman DG. Practical Statistics for Medical Research. London, UK: Chapman & Hall, 1991. [Google Scholar]
- 47.Lin L, Chu H. Meta-analysis of proportions using generalized linear mixed models. Epidemiology 2020; 31(5): 713–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Warton DI, Hui F. The arcsine is asinine: the analysis of proportions in ecology. Ecology 2011; 92(1): 3–10. [DOI] [PubMed] [Google Scholar]
- 49.Schwarzer G, Chemaitelly H, Abu-Raddad LJ, et al. Seriously misleading results using inverse of Freeman-Tukey double arcsine transformation in meta-analysis of single proportions. Res Synth Method 2019; 10(3): 476–483, DOI: 10.1002/jrsm.1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315(7109): 629–634. DOI: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Choi EPH, Hui BPH, Wan EYF. Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health 2020; 17(10): 3740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dai LL, Wang X, Jiang TC, et al. Anxiety and depressive symptoms among COVID-19 patients in Jianghan Fangcang Shelter Hospital in Wuhan, China. PLoS One 2020; 15(8): e0238416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li X, Tian J, Xu Q. The associated factors of anxiety and depressive symptoms in COVID-19 patients hospitalized in Wuhan, China. Psychiatr Q 2021; 92: 879–887. DOI: 10.1007/s11126-020-09865-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li Q, Zhang HF, Zhang M, et al. Prevalence and risk factors of anxiety, depression, and sleep problems among caregivers of people living with neurocognitive disorders during the COVID-19 pandemic. Front Psychiatry 2021; 11: 590343. DOI: 10.3389/fpsyt.2020.590343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ren Y, Cheng SP, Yang YX. Status quo of depression and its influencing factors in elderly people at home during outbreak of novel coronavirus pneumonia. J Mod Clin Med 2020; 46(6): 449–452. [Google Scholar]
- 56.Zhang JL, Sun R, Yang J. Anxiety and depression in elderly patients during epidemic of coronavirus disease 2019 and its influencing factors. Chin J Mult Organ Dis Elder 2020; 19(4): 246–250. [Google Scholar]
- 57.Wong FHC, Liu T, Leung DKY, et al. Consuming information related to COVID-19 on social media among older adults and its association with anxiety, social trust in information, and COVID-safe behaviors: cross-sectional telephone survey. J Med Internet Res 2021; 23(2): e26570. DOI: 10.2196/26570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fong BYF, Wong MCS, Law VTS, et al. Relationships between physical and social behavioural changes and the mental status of homebound residents in Hong Kong during the COVID-19 pandemic. Int J Environ Res Public Health 2020; 17(18): 6653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liang W, Duan Y, Shang B, et al. Precautionary behavior and depression in older adults during the COVID-19 pandemic: an online cross-sectional study in Hubei, China. Int J Environ Res Public Health 2021; 18(4): 1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liu X, Luo WT, Li Y, et al. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect Dis Poverty 2020; 9(3): 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chen SH, Dai JM, Hu Q, et al. Public anxiety and its influencing factors in the initial outbreak of COVID-19. Fudan Univ J Med Sci 2020; 47(3): 385–391. [Google Scholar]
- 62.Chen L, Zhao H, Razin D, et al. Anxiety levels during a second local COVID-19 pandemic breakout among quarantined people: a cross sectional survey in China. J Psychiatr Res 2021; 135: 37–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yan F, Li YQ, Qi H, et al. Analysis of anxiety status among Beijing residents during the coronavirus disease 2019 outbreak. Capital J Public Health 2020; 14(3): 140–144. [Google Scholar]
- 64.Allan SM, Bealey R, Birch J, et al. The prevalence of common and stress-related mental health disorders in healthcare workers based in pandemic-affected hospitals: a rapid systematic review and meta-analysis. Eur Journal Psychotraumatol 2021; 11(1): 1810903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.World Health Organization . China situation. Geneva, Switzerland: World Health Organization. https://covid19.who.int/region/wpro/country/cn (2020, accessed 20 April 2021). [Google Scholar]
- 66.Liu CP, Zhang X, Jin Y, et al. A community-based survey on prevalence of anxiety-depression disorder in elderly inhibitants with chronic diseases. Chin J Mult Organ Dis Elder 2010; 9(1): 38–40. [Google Scholar]
- 67.Bi Y-H, Pei J-J, Hao C, et al. The relationship between chronic diseases and depression in middle-aged and older adults: a 4-year follow-up study from the China health and retirement longitudinal study. J Affective Disord 2021; 289: 160–166. [DOI] [PubMed] [Google Scholar]
- 68.Wang MM, Tian SR, Wu RX, et al. Investigation on anxiety and psychological resilience of the elderly during the epidemic. Health Vocational Educ 2021; 39(3): 139–141. [Google Scholar]
- 69.Rong J, Ge YH, Meng NN, et al. Prevalence rate of depression in Chinese elderly from 2010 to 2019: a meta-analysis. Chin J Evidence-Based Med 2020; 20(1): 26–31. [Google Scholar]
- 70.Dong XL, Sun WM, Yuan YF. Status and influencing of anxiety among community elderly in Jiangxi. Mod Prev Med 2016; 43(13): 2378–2381. [Google Scholar]
- 71.Kou XJ, Gong CP, Liu XJ, et al. Anxiety and depression status and influencing factors of community elderly in Wuhan. Chin J Gerontol 2018; 38(10): 2529–2531. [Google Scholar]
- 72.Carstensen LL Shavit YZ and Barnes JT. Age advantages in emotional experience persist even under threat from the COVID-19 pandemic. Psychol Sci 2020;31:1374-1385. 10.31124/advance.13022042.v1. [DOI] [PubMed] [Google Scholar]
- 73.Carstensen L, Fung H, Charles S. Socioemotional selectivity theory and the regulation of emotion in the second half of life. Motiv Emot 2003; 27: 103–123. DOI: 10.1023/a:1024569803230 [DOI] [Google Scholar]
- 74.Charles ST. Strength and vulnerability integration: a model of emotional well-being across adulthood. Psychol Bull 2010; 136(6): 1068–1091. DOI: 10.1037/a0021232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pasnau RO, Fawzy FI. Stress and psychiatry. In: Sadock BJ, Sadock VA, Ruiz P. (eds) Kaplan and Sadock’s Comprehensive Textbook of Psychiatry. Philadelphia: Wolters Kluwer Health, 1989. [Google Scholar]
- 76.Rutherford BR, Choi CJ, Chrisanthopolous M, et al. The COVID-19 pandemic as a traumatic stressor: mental health responses of older adults with chronic PTSD. Am J Geriatr Psychiatry 2020; 29(2): 105–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Maja H, Jayanti C, Annika N, et al. Comparison of two self-rating scales to detect depression: hads and phq-9. Br J Gen Pract 2009; 59: e283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Manea L, Gilbody S, Mcmillan D. Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): a meta-analysis. CMAJ: Can Med Assoc Journal 2012; 184(3): E191–E196. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-jgp-10.1177_08919887221078556 for Prevalence of depressive and anxiety symptoms among Chinese older adults during the COVID-19 pandemic: A systematic review and meta-analysis by Yifei Yan, Xiayu Du, Lizu Lai, Zhihong Ren and Hua Li in Journal of Geriatric Psychiatry and Neurology