Abstract
COVID-19 has been associated with central nervous system manifestations; however, cerebral venous thrombosis is rarely reported. A 34-year-old woman was admitted to the hospital with headache and recurrent seizures; she was recently discharged after COVID-19 pneumonia. Cranial magnetic resonance imaging and magnetic resonance venography showed cortical vein thrombosis in the right frontal lobe. SARS-CoV-2 RNA was detected in cerebrospinal fluid analysis. The patient was anticoagulated and put on antiepileptics. The most probable mechanism underlying the venous thrombosis is COVID-19-associated hypercoagulability. However, the relation between the viral RNA in cerebrospinal fluid analysis and the thrombosis is controversial.
Keywords: COVID-19, intracranial sinus thrombosis, seizures
Introduction
Coronavirus disease 2019 (COVID-19) is a cause of viral pneumonia. COVID-19 has also been associated with many central nervous system (CNS)-related manifestations including headache, anosmia, ageusia, dizziness, acute cerebrovascular disease, seizure, ataxia, acute disseminated encephalomyelitis (ADEM), and encephalitis.1,2 Coagulopathy is one of the main underlying mechanisms of COVID-19-related CNS disorders. 3 Herein, we report a patient, who presented with cortical venous thrombosis (CVT) and epileptic seizures following COVID-19-induced pneumonia.
Case
A 34-year-old woman had been hospitalized for COVID-19 pneumonia which was confirmed with a nasophargyngeal PCR and a non-enhanced, low-dose lung computerized tomography (CT) (Figure 1). After discharge she had a seizure on the 15th day following her COVID-19 diagnosis. On the 18th day, she admitted to the emergency department because of 2 recurrent motor seizures on the same day. On readmission, she had a transient (2 hours) left-sided hemiparesis following the motor seizures and right-sided frontal headache with photophobia in the postictal phase. Low molecular weight heparin (LMWH) had been prescribed for prophylaxis during discharge due to the elevated D-dimer level (0.94 mg/L; normal range < 0.55). However, the patient did not take the medication. Neurological examination was normal on the index admission and laboratory results were congruent with viral infection (leukocyte: 12.57 x 10^3 μL, neutrophil: 7.5 x 10^3 μL, lymphocyte: 3.97 x 10^3 μL, and C-reactive protein:76.2 mg/L). COVID-19 PCR test in the nasopharyngeal sample was negative on second hospitalization. Electroencephalography (EEG) showed delta waves in the right hemisphere, prominently in the fronto-temporal areas. On the 20th day, lumbar puncture was performed. Although CSF analysis was normal (leukocyte: 2/mm3, erythrocyte: 8/mm3, protein: 46 mg/dL, glucose: 52 mg/dL, IgG index: 0.49, and oligoclonal band was negative), clinical and EEG findings suggested viral encephalitis prompting CSF analysis for the presence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). SARS-CoV-2 RNA in the CSF was detected using the COVID-19 real-time reverse transcription polymerase chain reaction (real-time RT-PCR) kit (Bio-speedy, Bioeksen, Istanbul, Turkey). Viral RNA was achieved via one-step reverse transcription and real-time PCR targeting SARS-CoV-2-specific RNA-dependent RNA polymerase gene fragment. Real-time RT-PCR was performed on the LightCycler® 480 Instrument II using the following conditions: 45°C for 15 minutes and 95°C for 3 minutes, 45 cycles of amplification at 95°C for 5 seconds and 55°C for 35 seconds. SARS-CoV-2 RNA was not detected in the blood sample obtained simultaneously with the CSF. The negative controls included in every run to check for potential contamination were negative. Also, the positive and internal controls (RNase P gene) included in every run were detected as positive. According to the manufacturer, the threshold cycle (Ct) < 38 was positive for SARS-CoV-2 RT-PCR. CT value of SARS-CoV-2 in CSF was detected as 37. The limit of detection of the kit is 5.6 copies/reaction, and its analytical sensitivity and specificity are 99.4% and 99%. The kit has the same study protocol for nasopharyngeal aspirate, bronchoalveolar lavage, nasopharyngeal swab, oropharyngeal swab, and sputum samples, but the manufacturer does not have any preparation recommendations for CSF samples. The test was performed using the same protocol for the CSF sample. The CSF sample was tested twice. SARS-CoV-2 sequencing for confirmation could not be performed. In the studies, different PCR-based kits were used to detect SARS-CoV-2 RNA in CSF. 4
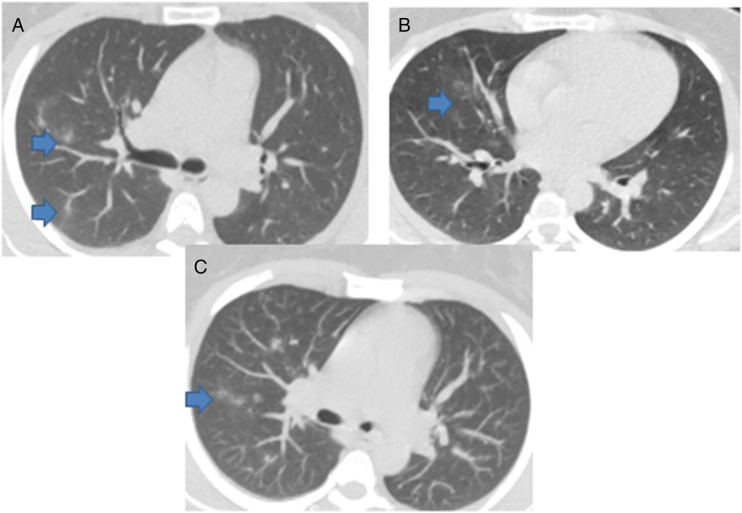
Figure 1.
(A-B) Non-enhanced axial chest CT and (C) axial MIP images show unilateral peripheral and central, solid ground glass mix type nodular opacities of right upper, lower, middle lobes (arrows).
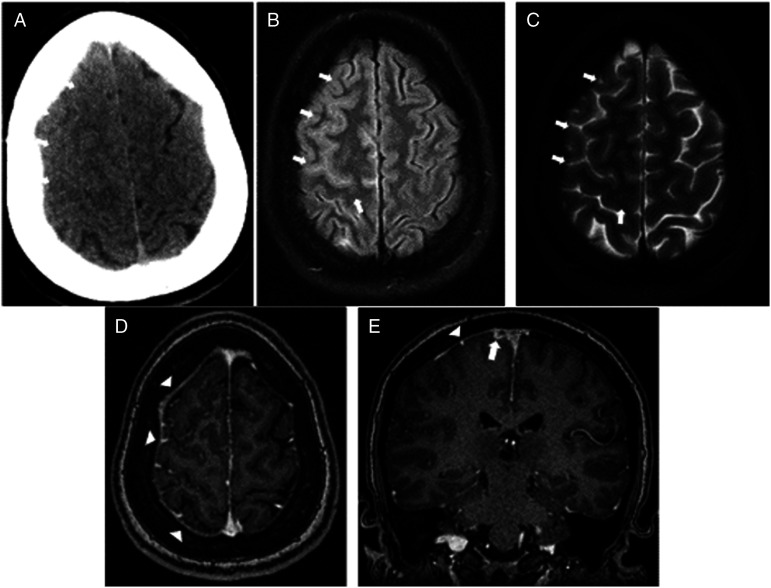
However, cranial CT (Figure 2A) on the first day of admission showed effacement of right frontal sulci. Cranial magnetic resonance imaging and magnetic resonance venography (Figure 2B-E and Figure 3) revealed acute thrombosed right cortical vein at the level of vertex, leading to a final diagnosis of CVT. The patient had no other risk factor for CVT. D-dimer level was high (0.94 mg/L; normal range < 0.55). ANA, anti dsDNA, and ENA profile were negative. The patient was started on levetiracetam and oral anticoagulation resulting in seizure control.
Figure 2.
Demonstration of sulcal effacement of right frontal cerebral sulci at the level of vertex and unsuppressed CSF signal representing the meningeal irritation (short arrows). (A) Non-enhanced axial head CT, (B) axial FLAIR, (C) axial T2-WI (D) contrasted volumetric axial T1-WI shows mild dural enhancement (arrowheads), and (E) contrasted MPR coronal T1-WI shows dural enhancement (arrowhead) and filling defect of cortical vein (short arrow).
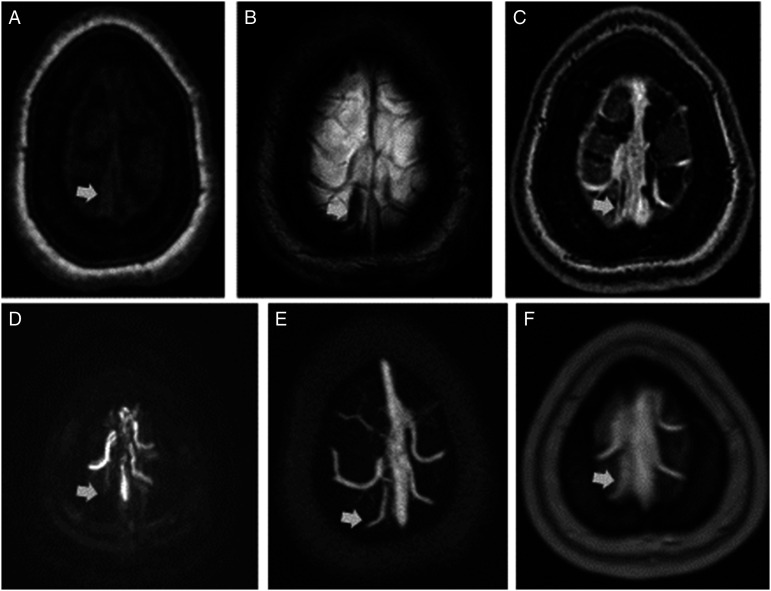
Figure 3.
(A) Non-enhanced axial T1-WI, (B) axial SWI MIP, (C) contrasted T1-WI, (D) phase contrast MRV axial MIP reconstruction show thrombosed right cortical vein, and (E and F) contrasted MRV and contrasted T1-WI (short arrows) demonstrate the partial filling defect of thrombosed cortical vein after medication
Discussion
Although viral encephalitis was initially suspected in this case due to SARS-CoV-2 RNA positivity, seizures, and abnormal EEG findings suggestive of acute encephalopathy, neuroimaging features clearly exhibited CVT. Non-inflammatory CSF findings, congruence of EEG findings with the side of the infarct side, and regression of symptoms under anti-coagulant medication further supported this final diagnosis. It is conceivable that the isolated CVT in our case, in the absence of other risk factors, is secondary to coagulopathy related to COVID-19. Our case emphasizes the notion that increased liability to coagulation, a common feature of COVID-19, may persist after cessation of the respiratory symptoms and nasopharyngeal positivity of SARS-CoV-2 leading to vascular complications.
COVID-19 has been associated with many CNS manifestations including acute ischemic cerebrovascular disease. 1 However cerebral vein thrombosis is rarely reported. In a retrospective, single-centered, observational analysis, out of 221 COVID-19 patients, 11 (5%) had arterial ischemic stroke and only 1 (0.5%) had cerebral venous sinus thrombosis (CVST). 5 In another case report, the patient had CVST as the presenting symptom of the COVID-19 infection. 6 These reported cases had significantly increased D-dimer and C-reactive protein levels, potentially suggesting an inflammation-induced hypercoagulable state resulting in stroke. Although precise mechanisms of COVID-19-associated vascular thrombosis are still unknown, endotheliitis induced by systemic inflammation may be one of the underlying factors.7-9
Our case also shows one of the rare demonstrations of the presence of SARS-CoV-2 in the CSF. More importantly, our case underscores that SARS-CoV-2 may persist in the CSF, while not present in the nasopharyngeal swab. There is evidence suggesting that SARS-CoV-2 has the potential to invade the CNS like SARS-CoV-1. There are only a few reported cases with neurological manifestations, in whom, CSF examination could be performed. SARS-CoV-2 PCR positivity in CSF is mostly reported in cases with encephalopathy or encephalitis-meningitis; however, headache and seizures have also been recorded. 4 Furthermore, 2 COVID-19 cases with concomitant stroke were reported to have negative CSF SARS-CoV-2 PCR results, 10 suggesting that this association might be coincidental. In a post-mortem case report, SARS-CoV-2 was detected in neural and capillary endothelial cells of the frontal lobe, but not in the CSF sample. Authors suggest that this may be due to the fact that SARS-CoV-2 is mainly cell‐bound, spreading from cell‐to‐cell and presumably found in CSF at concentrations below the level of detection of the testing method. 11 In this context, our case provides some evidence as to the relation between stroke and COVID-19 infection and shows that SARS-CoV-2 may remain detectable levels in the CSF. However, a cause-effect relationship between SARS-CoV-2 PCR positivity and venous thrombosis cannot be extrapolated.
In conclusion, hypercoagulability, which is a well-known complication of COVID-19, may persist and potentially lead to vascular complications even after cessation of respiratory symptoms. SARS-CoV-2 may exist in the CSF even when absent in the upper respiratory tract without necessarily causing encephalitis or meningitis symptoms. It is difficult to interpret the relation between SARS-CoV-2 and vascular complications. Post-mortem studies of the future cases may illuminate the potential role of virus-induced hypercoagulability and/or endothelial inflammation in neurological presentations of COVID-19
Acknowledgments
We are indebted to Ethem Murat Arsava and Erdem Tüzün, for their excellent discussion of the case and helpful review of the manuscript.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Nurdan Göçgün https://orcid.org/0000-0002-4605-6718
Miray Atacan Yaşgüçlükal https://orcid.org/0000-0002-9529-1343
References
- 1.Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with Coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683-690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giacomelli A, Pezzati L, Conti F, et al. Self-reported olfactory and taste disorders in patients with severe acute respiratory Coronavirus 2 infection: A cross-sectional study. Clin Infect Dis. 2020;71(15):889-890. doi: 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145-147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis A, Frontera J, Placantonakis DG, et al. Cerebrospinal fluid in COVID-19: A systematic review of the literature. J Neurol Sci. 2021;421:117316. doi: 10.1016/j.jns.2021.117316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Y, Li M, Wang M, et al. Acute cerebrovascular disease following COVID-19: A single center, retrospective, observational study. Stroke and Vascular Neurology. 2020;5:279-284. doi: 10.1136/svn-2020-000431.Published online July 2, 2020:svn-2020-000431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christopher Hughes C, Tom Nichols T, Martin Pike M, Christian Subbe C, Salah Elghenzai S. Cerebral venous sinus thrombosis as a presentation of COVID-19. European Journal of Case Reports in Internal Medicine. 2020;7(5):1691. doi: 10.12890/2020_001691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417-1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen G, Wu D, Guo W, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130(5):2620-2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033-1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al Saiegh F, Ghosh R, Leibold A, et al. Status of SARS-CoV-2 in cerebrospinal fluid of patients with COVID-19 and stroke. J Neurol Neurosurg Psychiatr. 2020;91(8):846-848. doi: 10.1136/jnnp-2020-323522. [DOI] [PubMed] [Google Scholar]
- 11.Paniz‐Mondolfi A, Bryce C, Grimes Z, et al. Central nervous system involvement by severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2). J Med Virol. 2020;92(7):699-702. doi: 10.1002/jmv.25915. [DOI] [PMC free article] [PubMed] [Google Scholar]