Abstract
Objective
To assess the immunogenicity of pneumococcal 13-valent conjugate vaccination (PCV-13) in patients with rheumatoid arthritis receiving upadacitinib and background methotrexate (MTX).
Methods
Eligible patients from the phase 2 open-label extension trial BALANCE-EXTEND (NCT02049138) receiving stable dosing of upadacitinib 15 mg or 30 mg once daily plus background MTX were given PCV-13. Antibody titres were collected prevaccination and 4 and 12 weeks postvaccination. The primary endpoint was the proportion of patients with satisfactory humoral response to PCV-13, defined as a ≥2-fold increase in ≥6 of 12 pneumococcal antigens at 4 weeks postvaccination.
Results
Of 111 patients (upadacitinib 15 mg, N=87; 30 mg, N=24), 85.6% were women, 97.3% used concomitant MTX and 44.1% used oral corticosteroids. At 4 weeks, 67.5% (95% CI 57.4 to 77.5) of patients receiving upadacitinib 15 mg and 56.5% (36.3 to 76.8) receiving 30 mg had a satisfactory PCV-13 response. Responses were similar in patients who used or did not use concomitant corticosteroids. No deaths or serious adverse events were reported.
Conclusions
Approximately two-thirds of patients receiving upadacitinib 15 mg once daily achieved a satisfactory humoral response to PCV-13 despite receiving concomitant MTX. Concomitant corticosteroid use did not negatively affect PCV-13 response.
Keywords: antirheumatic agents, arthritis, rheumatoid, vaccination
Key messages.
Patients with rheumatoid arthritis have an elevated risk of infection; therefore, pneumococcal vaccination is recommended, particularly in those receiving immunosuppressive therapy.
This study showed that approximately two-thirds of patients receiving upadacitinib 15 mg once daily had a satisfactory humoral response to the pneumococcal 13-valent conjugate vaccine (PCV-13) despite receiving concomitant methotrexate.
Concomitant corticosteroid use did not appear to negatively affect antibody response to PCV-13.
These data suggest that it may not be necessary to temporarily stop upadacitinib treatment in patients receiving PCV-13.
Taking concomitant corticosteroids at doses typically used for RA is unlikely to impair response to PCV-13.
Introduction
Patients with rheumatoid arthritis (RA) are susceptible to infection because of weakened immune responses due to the underlying disease, comorbidities and immunosuppressants used to control RA activity.1 Streptococcus pneumoniae (pneumococcus) is a common cause of pneumonia, septicemia and meningitis, associated with morbidity and mortality.2 Therefore, pneumococcal vaccination is recommended in patients with RA receiving conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) or biologic DMARDs (bDMARDs).3
Several studies have evaluated pneumococcal vaccine response with DMARDs4 5 and, more recently, with Janus kinase (JAK) inhibitor treatment.6 7 Upadacitinib is an oral JAK inhibitor engineered to have greater selectivity for JAK1 versus JAK2, JAK3 and tyrosine kinase 2.8 Upadacitinib 15 mg once daily (QD) is approved in multiple countries for the treatment of RA. This analysis aimed to describe the humoral immune response to the pneumococcal 13-valent conjugate vaccine (PCV-13) in patients with RA receiving concomitant upadacitinib and methotrexate (MTX).
Methods
Patients
Patients from the ongoing, multicentre phase 2 open-label extension trial BALANCE-EXTEND (NCT02049138) were eligible to participate in this vaccine substudy. BALANCE-EXTEND included adults with active RA who had an inadequate response to an antitumour necrosis factor inhibitor or MTX and completed a preceding phase 2 randomised clinical trial of upadacitinib.9 10 In the substudy, patients were required to have received a stable dose of upadacitinib 15 mg or 30 mg QD and background MTX for ≥4 weeks prior to and after PCV-13 vaccination as specified in the protocol. Patients who used corticosteroids (CSs) had to remain on a stable dose of less than 10 mg/day of prednisone or equivalent CS therapy for ≥4 weeks after vaccination. In addition, patients must have met PCV-13 prescribing specifications as per local label requirements. Exclusion criteria were receipt of steroid injection within 4 weeks prior to vaccination, pneumococcal vaccination including PCV-13 at any time, any vaccination 4 weeks prior to and/or after the substudy vaccination visit, history of severe allergic reaction to any component of PCV-13 or pneumococcal infection within 6 months before the vaccination visit. Patients could initiate or change their dosage of oral or parenteral CSs, csDMARDs and background antirheumatic medications after 4 weeks postvaccination. The vaccine substudy was conducted following the principles of the Declaration of Helsinki and Good Clinical Practice guidelines. Ethical approval was provided by an institutional review board or ethics committee at each study site. Participating patients gave written informed consent.
Patient and public involvement
Patients and the public were not involved in the design or analysis of this study.
Study design
All enrolled patients receiving either upadacitinib 15 mg or 30 mg QD plus stable MTX were administered a single-dose 0.5 mL intramuscular injection of PCV-13 (Prevnar 13, Wyeth Pharmaceuticals, a subsidiary of Pfizer (Diphtheria CRM197 Protein)) according to the label.11 Blood samples for antibody titres were collected prevaccination (week 0) and postvaccination (weeks 4 and 12). Measurement of antibody concentrations was performed by ICON Central Laboratories (Farmingdale, New York). Adverse events (AEs) were collected up to 4 weeks postvaccination.
Immunogenicity and safety measures
The primary endpoint was the proportion of patients with satisfactory humoral response to PCV-13 at 4 weeks postvaccination. Similar to prior studies, a satisfactory humoral response was defined as a ≥2-fold increase in antibody concentration from prevaccination (week 0) in ≥6 of 12 pneumococcal antigens (1, 3, 4, 5, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F).12 13 Secondary endpoints included the proportion of patients with a satisfactory humoral response to PCV-13 at 12 weeks postvaccination and the geometric mean fold rise (GMFR) of antipneumococcal antibody levels to each of the 12 pneumococcal antigens compared with baseline at 4 and 12 weeks postvaccination. Antibody concentrations were measured against 12 pneumococcal antigens based on the availability of established assays by the study’s central lab at the time of protocol development. Safety was assessed by evaluating AEs, defined as an event with onset on or after vaccination and up to 30 days postvaccination.
Statistical analysis
The planned total sample size was 150 patients with 100 in the upadacitinib 15 mg QD group, to achieve a precision of estimation of 10% margin of error for the 95% CI of the 15 mg QD group, assuming a 60% satisfactory humoral response rate. All patients who were vaccinated with PCV-13 and received ≥1 dose of upadacitinib after vaccination were analysed. Patients were classified into two groups based on the upadacitinib 15 mg or 30 mg QD dose received at the vaccination visit. The proportion of patients achieving a satisfactory humoral response was presented as counts and percentages with 95% CIs calculated based on normal approximation. Subgroup analyses were also performed by age and concomitant CS use. The GMFR postvaccination and 95% CIs were calculated at weeks 4 and 12 for each pneumococcal antigen.
Results
Baseline patient characteristics
A total of 111 patients receiving ≥1 dose of upadacitinib (15 mg, N=87; 30 mg, N=24) were enrolled in the vaccine substudy. Most patients were women (85.6%) and white (98.2%) with a mean (SD) age of 58.4 (12.0) years. Patients had a median (range) duration of RA of 9.3 (3.4 to 35.0) years, mean (SD) Clinical Disease Activity Index of 6.0 (6.1), mean (SD) Disease Activity Score 28-joint count C reactive protein of 2.2 (1.0) and were receiving upadacitinib for a median (range) of 3.9 (3.0 to 4.9) years. Three patients (2.7%) included in this analysis did not meet the stated enrolment criteria as they were not receiving concomitant MTX. One patient changed their MTX dose from 20 mg to 10 mg weekly during the last 2 weeks of the substudy. Nearly half (44.1%) of patients used oral CSs at a median daily dose of 5.0 mg. Every patient received PCV-13 and continued upadacitinib during the first 4 weeks. Nearly all patients provided evaluable blood samples at appropriate time points (83 (95.4%)/23 (95.8%) and 79 (90.8%)/22 (91.7%) patients in the upadacitinib 15/30 mg groups at weeks 4 and 12, respectively).
Vaccine immunogenicity
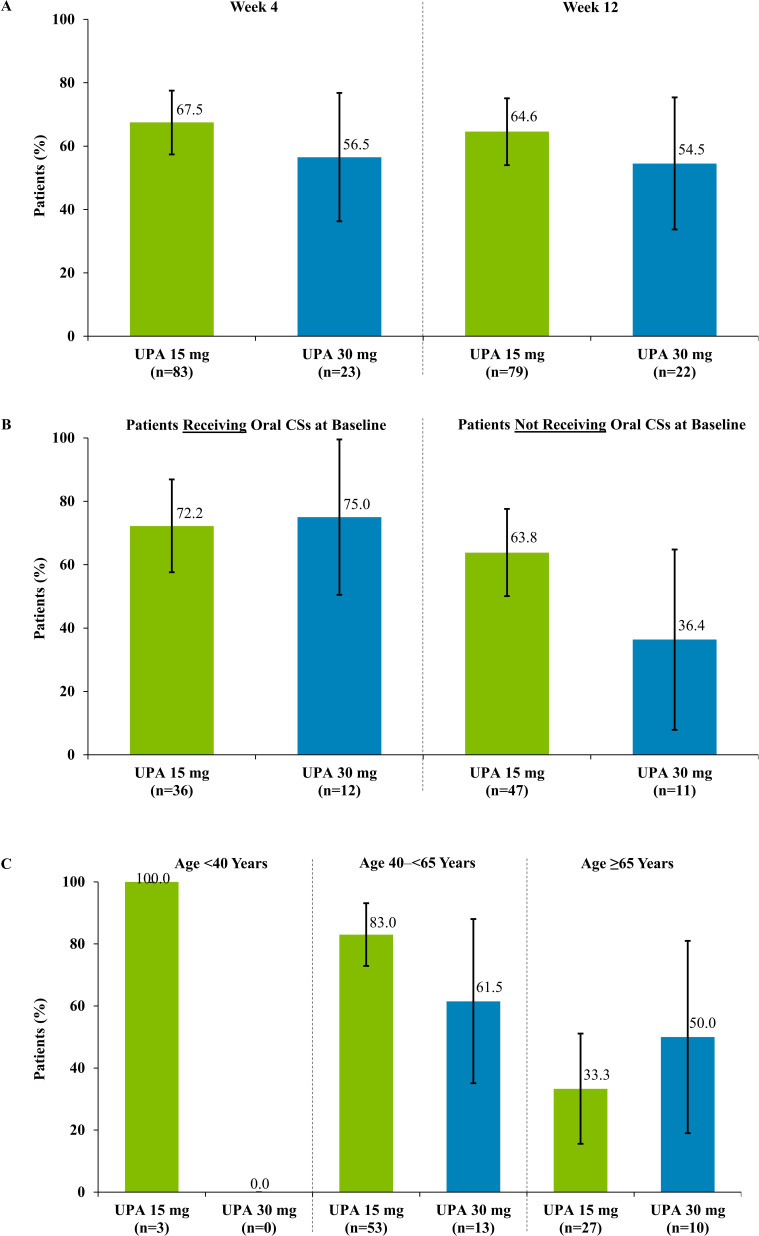
Satisfactory humoral response to PCV-13 at week 4 occurred in 67.5% (95% CI 57.4 to 77.5) of patients receiving upadacitinib 15 mg and 56.5% (36.3 to 76.8) receiving upadacitinib 30 mg. Similar responses were found at week 12, with 64.6% (54.0 to 75.1) of patients receiving upadacitinib 15 mg and 54.5% (33.7 to 75.4) receiving upadacitinib 30 mg achieving a satisfactory humoral response (figure 1A). No apparent difference in humoral response between patients receiving and not receiving concomitant CSs was observed (figure 1B). Humoral responses were numerically lower in older versus younger adults (figure 1C). Geometric mean increases in antibody levels compared with vaccination baseline values were observed for each of the 12 pneumococcal antigens at weeks 4 and 12 (table 1).
Figure 1.
Satisfactory humoral responses to PCV-13 at weeks 4 and 12 postvaccination (A) and effect of concomitant CSs (B) and age (C) on week 4 responses to PCV-13. Error bars indicate 95% CIs. Satisfactory humoral response was defined as ≥2 fold increase in antibody concentration from the vaccination baseline in ≥6 out of 12 pneumococcal antigens (1, 3, 4, 5, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F). Number of patients per treatment group was based on the availability of blood samples collected at weeks 4 and 12. CIs, confidence intervals; CSs, corticosteroids; PCV-13, pneumococcal 13-valent conjugate vaccine (Diphtheria CRM197 Protein); UPA, upadacitinib.
Table 1.
Anti-pneumococcal antibody levels at baseline and GMFR at weeks 4 and 12 after PCV-13 vaccination
| Antigen | UPA 15 mg QD | UPA 30 mg QD | ||||
| Baseline, µg/mL * (N=83) |
Week 4 GMFR (95% CI) (N=83) |
Week 12 GMFR (95% CI) (N=79) |
Baseline, µg/mL* (N=23) |
Week 4 GMFR (95% CI) (N=23) |
Week 12 GMFR (95% CI) (N=22) |
|
| 1 | 0.4 | 7.9 (6.1 to 10.2) | 8.1 (6.2 to 10.6) | 0.4 | 6.5 (4.0 to 10.7) | 6.5 (3.9 to 10.9) |
| 3 | 0.7 | 2.6 (2.1 to 3.2) | 2.3 (1.8 to 2.8) | 0.4 | 2.3 (1.5 to 3.5) | 2.2 (1.5 to 3.4) |
| 4 | 0.2 | 5.6 (4.3 to 7.4) | 5.2 (3.9 to 6.9) | 0.1 | 3.8 (2.3 to 6.4) | 3.4 (2.0 to 5.8) |
| 5 | 2.2 | 1.9 (1.5 to 2.4) | 1.8 (1.5 to 2.3) | 2.6 | 1.6 (1.1 to 2.4) | 1.6 (1.0 to 2.4) |
| 6B | 0.5 | 4.5 (3.3 to 6.1) | 3.9 (2.8 to 5.4) | 0.4 | 3.1 (1.7 to 5.5) | 3.3 (1.7 to 6.1) |
| 7F | 0.9 | 3.6 (2.8 to 4.5) | 3.3 (2.6 to 4.3) | 1.1 | 2.8 (1.8 to 4.4) | 3.0 (1.9 to 4.9) |
| 9V | 0.5 | 5.7 (4.3 to 7.6) | 6.2 (4.6 to 8.3) | 0.4 | 2.8 (1.6 to 4.8) | 2.9 (1.6 to 5.1) |
| 14 | 1.6 | 3.0 (2.4 to 3.7) | 2.8 (2.2 to 3.6) | 1.2 | 2.4 (1.6 to 3.7) | 2.4 (1.5 to 3.8) |
| 18C | 1.6 | 4.5 (3.5 to 5.8) | 4.4 (3.4 to 5.7) | 1.3 | 3.2 (2.0 to 5.2) | 3.5 (2.2 to 5.7) |
| 19A | 8.6 | 1.5 (1.3 to 1.7) | 1.4 (1.2 to 1.7) | 9.2 | 1.1 (0.8 to 1.5) | 1.2 (0.9 to 1.5) |
| 19F | 1.7 | 2.3 (1.8 to 2.8) | 2.2 (1.8 to 2.7) | 1.6 | 2.3 (1.5 to 3.5) | 2.0 (1.3 to 3.0) |
| 23F | 0.7 | 4.3 (3.3 to 5.7) | 4.1 (3.0 to 5.4) | 0.7 | 3.1 (1.9 to 5.2) | 3.3 (1.9 to 5.7) |
Patients with non-missing baseline and at least one post-baseline value were included in the analysis.
*Baseline geometric mean antibody levels among patients with available week 4 data.
CI, confidence interval; GMFR, geometric mean fold rise; PCV-13, pneumococcal 13-valent conjugate vaccine (Diphtheria CRM197 Protein); QD, once daily; UPA, upadacitinib.
Safety
No serious AEs, AEs leading to discontinuation of upadacitinib or death were reported.
Overall, 18 patients (16.2%) experienced an AE during 30 days postvaccination (table 2). Most events were mild in severity (88.9%); one event each of moderate upper respiratory tract infection and superficial thrombophlebitis was reported with upadacitinib 15 mg. Within 30 days postvaccination, two AEs were considered possibly related to upadacitinib: one case of diverticulitis with upadacitinib 15 mg and one case of anaemia with upadacitinib 30 mg. Within 1-day postvaccination, two patients experienced fever, and one patient each experienced vaccination-site pain and headache (all receiving upadacitinib 15 mg).
Table 2.
Safety through 30 days postvaccination with PCV-13
| Event, n (%) | UPA 15 mg QD (N=87) |
UPA 30 mg QD (N=24) |
| Any AE | 15 (17.2) | 3 (12.5) |
| AEs occurring in >1 patient | ||
| Fever | 2 (2.3) | 0 |
| Nasopharyngitis | 3 (3.4) | 0 |
| Onychomycosis | 2 (2.3) | 0 |
| Upper respiratory tract infection | 1 (1.1) | 1 (4.2) |
| Serious AE | 0 | 0 |
| AE leading to discontinuation of study drug | 0 | 0 |
| AE with reasonable possibility of being related to UPA* | 1 (1.1) | 1 (4.2) |
| Death | 0 | 0 |
*As assessed by the investigator.
AE, adverse event; PCV-13, pneumococcal 13-valent conjugate vaccine (Diphtheria CRM197 Protein); QD, once daily; UPA, upadacitinib.
Discussion
This study assessed humoral immune responses to PCV-13 in patients with RA receiving upadacitinib and MTX. Treatment with MTX, the standard of care for RA, has been shown to diminish antibody response following pneumococcal7 14 15 and influenza vaccination.7 Current guidelines recommend pneumococcal vaccination before starting a csDMARD or bDMARD3 in addition to applying a prime-boost vaccination strategy (PCV-13 followed by 23-valent pneumococcal polysaccharide vaccine (PPSV-23; Pneumovax)) to potentially improve antibody response.16 However, the clinical question remains whether it is necessary to temporarily stop JAK inhibitor and/or MTX treatment prior to vaccination.
Importantly, we found that about two-thirds of patients receiving upadacitinib 15 mg QD mounted a satisfactory humoral response to PCV-13 at 4 and 12 weeks postvaccination, despite 97% receiving concomitant MTX. Our results were broadly consistent with pneumococcal vaccine humoral responses in patients with RA treated with other JAK inhibitors, biologics or placebo.4 6 7 In studies of patients with RA receiving other JAK inhibitors, 68% achieved a satisfactory humoral response to PCV-13 with baricitinib with or without MTX,6 and 66% achieved a satisfactory humoral response to PPSV-23 with tofacitinib plus MTX.7 In addition, humoral response rates in the present study were similar to those reported by Nived et al5 for patients with RA not receiving DMARDs (52%) and healthy adults (55%); however, the study only assessed antibody concentrations for pneumococcal antigens 6B and 23F and was limited by small sample size.
Concomitant CS use did not appear to negatively affect PCV-13 antibody response, and age-related decreases in humoral immune response to pneumococcal vaccination were observed in line with findings from previous studies.4 6 Overall, PCV-13 vaccination was well tolerated, and no serious AEs were reported.
Several limitations should be acknowledged. Small sample sizes of the upadacitinib 30 mg may limit the comparisons of the two dose groups, and similarly, small sample sizes in the subgroups receiving versus not receiving concomitant CSs may have limited the power of this analysis. In addition, no control group was evaluated. Our findings may not be generalisable to patients with RA receiving other commonly administered vaccines (eg, influenza vaccine) while on therapy.
In summary, satisfactory humoral response to PCV-13 was attained through 12 weeks postvaccination in most patients with RA receiving upadacitinib 15 mg QD plus MTX, irrespective of CS use. Future studies should assess whether temporary discontinuation of either upadacitinib or MTX (or both) would further enhance the immune response to PCV-13, particularly in older adults who are more likely to have a less robust response.15
Acknowledgments
AbbVie and the authors thank the patients, study sites, and investigators who participated in this clinical trial. Julia Zolotarjova, MSc, MWC, of AbbVie Inc., provided medical writing assistance for the development of this publication.
Footnotes
Contributors: JIV, ED, CG, AF, BH, YL, JK and AK were involved in the acquisition of data. All authors were involved in the analysis and interpretation of the data, drafting the article, revising it for critically important content and approving the final version of manuscript.
Funding: AbbVie Inc. (North Chicago, IL, USA) funded this study and participated in the study design, research, analysis, data collection, interpretation of data, review and approval of the publication. All authors had access to relevant data and participated in the drafting, review and approval of this publication. No honoraria or payments were made for authorship.
Competing interests: KW has received consulting fees and/or grant/research support from AbbVie, AstraZeneca, Bristol-Myers Squibb, Eli Lilly and Company, Galapagos, Gilead, GlaxoSmithKline, Novartis, Pfizer, Regeneron, Roche, Sanofi and UCB; and is an editorial board member of RMD Open.JI Vargas has received honoraria from AbbVie and fees from AbbVie as Principal Investigator in the study. ED has received fees from AbbVie as Principal Investigator in the study. CG has received fees from AbbVie as Principal Investigator in the study. AF, BH, YL and JK are employees of AbbVie and may own stocks or options. AK has received consulting fees and/or honoraria from AbbVie, Amgen, Boehringer Ingelheim, Eli Lilly and Company, Flexion, Genzyme, Gilead, Horizon, Janssen, Merck, Novartis, Pfizer, Regeneron, Sanofi, Sanofi Aventis, SUN Pharma Advanced Research, and UCB; owns stocks or options in Amgen, Gilead, GlaxoSmithKline, Novartis, Pfizer, and Sanofi; his institution received fees from AbbVie for his role as a Principal Investigator in the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by IRB: Advarra IRB Organization Number (IORG): 0000635IRB Registration Number: 00000971 Participants gave informed consent to participate in the study before taking part.
References
- 1.Listing J, Gerhold K, Zink A. The risk of infections associated with rheumatoid arthritis, with its comorbidity and treatment. Rheumatology 2013;52:53–61. 10.1093/rheumatology/kes305 [DOI] [PubMed] [Google Scholar]
- 2.Henriques-Normark B, Tuomanen EI. The pneumococcus: epidemiology, microbiology, and pathogenesis. Cold Spring Harb Perspect Med 2013;3:a010215. 10.1101/cshperspect.a010215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh JA, Saag KG, SL BJ. American College of rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res 2015;2016:1–25. [DOI] [PubMed] [Google Scholar]
- 4.Bingham CO, Rizzo W, Kivitz A, et al. Humoral immune response to vaccines in patients with rheumatoid arthritis treated with tocilizumab: results of a randomised controlled trial (VISARA). Ann Rheum Dis 2015;74:818–22. 10.1136/annrheumdis-2013-204427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nived P, Saxne T, Geborek P, et al. Antibody response to 13-valent pneumococcal conjugate vaccine is not impaired in patients with rheumatoid arthritis or primary Sjögren's syndrome without disease modifying treatment. BMC Rheumatol 2018;2:12. 10.1186/s41927-018-0019-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Winthrop KL, Bingham CO, Komocsar WJ, et al. Evaluation of pneumococcal and tetanus vaccine responses in patients with rheumatoid arthritis receiving baricitinib: results from a long-term extension trial substudy. Arthritis Res Ther 2019;21:102. 10.1186/s13075-019-1883-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Winthrop KL, Silverfield J, Racewicz A, et al. The effect of tofacitinib on pneumococcal and influenza vaccine responses in rheumatoid arthritis. Ann Rheum Dis 2016;75:687–95. 10.1136/annrheumdis-2014-207191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parmentier JM, Voss J, Graff C, et al. In vitro and in vivo characterization of the JAK1 selectivity of upadacitinib (ABT-494). BMC Rheumatol 2018;2:23. 10.1186/s41927-018-0031-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kremer JM, Emery P, Camp HS, et al. A phase IIb study of ABT-494, a selective JAK-1 inhibitor, in patients with rheumatoid arthritis and an inadequate response to anti-tumor necrosis factor therapy. Arthritis Rheumatol 2016;68:2867–77. 10.1002/art.39801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Genovese MC, Smolen JS, Weinblatt ME, et al. Efficacy and safety of ABT-494, a selective JAK-1 inhibitor, in a phase IIb study in patients with rheumatoid arthritis and an inadequate response to methotrexate. Arthritis Rheumatol 2016;68:2857–66. 10.1002/art.39808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.U.S. Food Drug and Administration . Prevnar 13 prescribing information, 2017. Available: https://www.fda.gov/files/vaccines%2C%20blood%20%26%20biologics/published/Package-Insert-Prevnar-13.pdf [Accessed 23 Jun 2021].
- 12.Orange JS, Ballow M, Stiehm ER, et al. Use and interpretation of diagnostic vaccination in primary immunodeficiency: a working group report of the Basic and Clinical Immunology Interest Section of the American Academy of Allergy, Asthma & Immunology. J Allergy Clin Immunol 2012;130:S1–24. 10.1016/j.jaci.2012.07.002 [DOI] [PubMed] [Google Scholar]
- 13.Daly TM, Hill HR. Use and clinical interpretation of pneumococcal antibody measurements in the evaluation of humoral immune function. Clin Vaccine Immunol 2015;22:148–52. 10.1128/CVI.00735-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kapetanovic MC, Nagel J, Nordström I, et al. Methotrexate reduces vaccine-specific immunoglobulin levels but not numbers of circulating antibody-producing B cells in rheumatoid arthritis after vaccination with a conjugate pneumococcal vaccine. Vaccine 2017;35:903–8. 10.1016/j.vaccine.2016.12.068 [DOI] [PubMed] [Google Scholar]
- 15.Rasmussen SL, Fuursted K, Nielsen KA, et al. Pneumococcal antibody protection in patients with autoimmune inflammatory rheumatic diseases with varying vaccination status. Scand J Rheumatol 2020;49:353–60. 10.1080/03009742.2020.1732459 [DOI] [PubMed] [Google Scholar]
- 16.CDC . Recommended adult immunization schedule, 2021. Available: https://www.cdc.gov/vaccines/schedules/downloads/adult/adult-combined-schedule.pdf [Accessed 27 Jun 2021].