Abstract
Objective
Social and structural factors, referred to as social determinants of health (SDH), create pathways or barriers to equitable sexual health, and information on these factors can provide critical insight into rates of diseases such as HIV. Our objectives were to describe and identify differences, by race/ethnicity and geography, in SDH among adults with HIV.
Methods
We conducted an ecological study to explore SDH among people with HIV diagnosed in 2017, by race/ethnicity and geography, at the census-tract level in the United States and Puerto Rico. We defined the least favorable SDH as the following: low income (<$40 000 in median annual household income), low levels of education (≥18% of residents have <high school diploma), high levels of poverty (≥19% of residents live below the federal poverty level), unemployment (≥6% of residents in the workface do not have a job), lack of health insurance (≥16% of residents lack health insurance), and vacant housing (≥15% of housing units are vacant).
Results
HIV diagnosis rates increased 1.4 to 4.0 times among men and 1.5 to 5.5 times among women as census-tract poverty levels increased, education levels decreased, income decreased, unemployment increased, lack of health insurance increased, and vacant housing increased. Among racial/ethnic groups by region and SDH, we observed higher HIV diagnosis rates per 100 000 population among non-Hispanic Black (49.6) and non-Hispanic White (6.5) adults in the South and among Hispanic/Latino (27.4) adults in the Northeast than in other regions. We observed higher HIV diagnosis rates per 100 000 population among non-Hispanic Black (44.3) and Hispanic/Latino (21.1) adults than among non-Hispanic White (5.1) adults.
Conclusion
Our findings highlight the importance of SDH in HIV infection and support the need for effective, targeted local interventions to specific populations based on HIV diagnoses and prevalence to prevent infection and reduce racial/ethnic disparities.
Keywords: HIV, epidemiology, racial/ethnic differences, social determinants of health, SDH
With approximately 40 000 HIV cases diagnosed each year from 2013 to 2017 in the United States, progress in reducing HIV transmission has slowed. 1 In 2017, Hispanic/Latino and non-Hispanic Black or African American (hereinafter, Black) males had HIV diagnosis rates 4 and 8 times the rate of non-Hispanic White (hereinafter, White) males, respectively; Hispanic/Latino and Black females had HIV diagnosis rates 3 and 15 times the rate of White females, respectively. 1
Racial/ethnic differences in HIV diagnoses and prevalence are well documented in the United States. 1 However, those differences cannot be fully explained by individual-level risk behaviors. Structural and societal factors, referred to as social determinants of health (SDH), create pathways or barriers to equitable good health—in particular, sexual health—and information on these factors can provide critical insight into rates of diseases such as HIV. 2,3 SDH are health care service, social, and physical environment factors that are not under the control of the individual, and they may explain overlapping risk factors common among populations and geographic areas that bear a disproportionate share of HIV diagnoses in the United States. 3,4
Black and Hispanic/Latino people are at increased risk for HIV because of SDH such as poverty, reduced access to health care, and low levels of education. 5 -11 Areas with high levels of poverty, low levels of household income, and low levels of health insurance coverage accounted for the highest HIV diagnosis rates among Black and Hispanic/Latino people in 2017. 12 The Ending the HIV Epidemic: A Plan for America initiative aims to reduce the number of new HIV infections by 75% in 5 years and by 90% in 10 years and sharpen prevention efforts to focus on HIV-related disparities in populations and geographic areas with substantial HIV burden in the United States. Continued insight into these disparities can inform the expansion of HIV prevention and treatment services and ultimately achieve the goals of reducing the number of new infections. 13 In addition, improving the measurement and monitoring of SDH and further clarifying their connection with HIV diagnosis rates could provide evidence to support and evaluate policy and program action. 3
This ecological study aims to explore SDH among people with HIV diagnosed in 2017, by race/ethnicity and geography, at the census-tract level in the United States and Puerto Rico. Our objective was to describe differences in SDH among racial/ethnic groups that may provide insight into the disparate rates of HIV diagnoses among these groups.
Methods
We used data from 2 sources: the Centers for Disease Control and Prevention (CDC) National HIV Surveillance System (NHSS) 1 and the US Census Bureau’s American Community Survey (ACS). 14 The NHSS is a population-based census of all people with diagnosed HIV infection in the United States and 6 dependent areas. This comprehensive national surveillance system uses a standard, robust statistical methodology that does not require statistical tests of significance. 1 We geocoded NHSS data to the census-tract level for address of residence at the time of diagnosis and subsequently linked these data at the census-tract level to SDH data from the ACS. NHSS is determined a public health activity and not subject to human subjects research, and, therefore, does not require institutional review board review or approval.
We included diagnoses of HIV infection in 2017 among Black, Hispanic/Latino, and White adults aged ≥18 reported to CDC by December 31, 2018. People categorized as Hispanic/Latino were of either race (Black or White).
We obtained census tract–level SDH data from the ACS 2013-2017 five-year estimates 14 for the following 6 SDH indicators: federal poverty status (percentage of residents who were living below the federal poverty level [FPL]), education (percentage of residents with <high school diploma), income (median annual household income), employment status (percentage of residents in the workforce without a job), health insurance coverage (percentage of residents without health insurance coverage), and vacant housing (percentage of housing units that were vacant). We included these indicators because they are generally recognized in the scientific literature as population determinants of health. Although other social determinants may affect health, research on SDH emphasizes the need to incorporate these structural and societal factors into analyses of public health data. 12 We categorized SDH indicators using empirically derived quartiles, determined by data from all census tracts in the United States and Puerto Rico. We focused on the outer quartiles (ie, the extremes) of each indicator. The SDH defined as least favorable were the lowest quartile of income (<$40 000 in median annual household income), lowest quartile of education (≥18% of residents with <high school education), highest quartile of poverty (≥19% of residents living below the FPL), highest quartile of unemployment (≥6% of residents in the workforce without a job), highest quartile without health insurance (≥16% of residents without health insurance coverage), and highest quartile of vacant housing (≥15% of vacant housing units). The SDH defined as most favorable were the highest quartile of income (≥$75 000 median annual household income), highest quartile of education (<6% of residents with <high school education), lowest quartile of poverty (<7% of residents living below the FPL), lowest quartile of unemployment (<2% of residents in the workforce without a job), lowest quartile without health insurance (<6% of residents without health insurance coverage), and lowest quartile of vacant housing (<5% of vacant housing units).
Analysis
Using NHSS data reported from the United States and Puerto Rico, we assessed the distribution of HIV diagnoses in 2017, by age group, transmission category, residence at diagnosis, sex at birth, and SDH indicators among Black, Hispanic/Latino, and White adults. We limited the numerator population to adults aged ≥18 whose HIV infection was diagnosed (ie, diagnosis as a surrogate for infection) and whose case record included a complete residential address. We based the population denominators on the ACS 2013-2017 five-year estimates of the racial/ethnic populations aged ≥18. 14 We computed the denominators used to calculate age-, sex-, and race/ethnicity-specific rates by applying the appropriate 5-year estimate. Because the ACS uses predetermined age categories and varying criteria for SDH variables, the denominators may differ among SDH variables.
We excluded cases or census tracts if the address was nonresidential (eg, military base, corrections facility), no census tract was associated with the case, no SDH information was available for the census tract, or the census tract from the surveillance data could not be matched to a census tract provided by the ACS. We calculated percentages and/or rates of HIV diagnoses per 100 000 population based on census tract by region, age group, transmission category, residence at diagnosis, and SDH indicators, and we stratified these data by sex and race/ethnicity. Reported numbers <12 and their accompanying rates should be interpreted with caution.
Regional data were based on the 4 US Census regions. Because Puerto Rico is a US territory, we categorized data for Puerto Rico separately when we examined data stratified by region. We either did not compare data for Puerto Rico or we did not show these data because of small numbers. We defined the area of residence as metropolitan (large metropolitan area with ≥500 000 population), urban (smaller metropolitan area with 50 000-499 999 population), or rural (nonmetropolitan area with <50 000 population). 15
We conducted an ecological analysis using SAS version 9.4 (SAS Institute, Inc) to describe the relationship between HIV diagnosis (numbers, rates, percentages) and SDH among people with HIV diagnosed in 2017 by sex and other characteristics (age, transmission category, residence at diagnosis), stratified by race/ethnicity and geography. We described differences in HIV diagnosis in terms of rates, except when describing differences by transmission category and residence at diagnosis, which we described in terms of percentages.
Results
In the United States and Puerto Rico, 30 287 HIV diagnoses among adults aged ≥18 had a geocoded residential address at diagnosis (approximately 81%, 92%, and 81% of all HIV diagnoses among Black, Hispanic/Latino, and White adults, respectively) in 2017. The HIV diagnosis rates per 100 000 population among Black (44.3) and Hispanic/Latino adults (21.1) were nearly 9 and 4 times that of White adults (5.1), respectively (Table 1).
Table 1.
Percentages and rates (per 100 000 population) of HIV diagnoses among Black or African American, Hispanic/Latino, and White adults aged ≥18, by sex and selected characteristics, United States and Puerto Rico, 2017 a
| Characteristic | Black or African American | Hispanic/Latino | White | All | ||||
|---|---|---|---|---|---|---|---|---|
| No. (%) | Rate | No. (%) | Rate | No. (%) | Rate | No. (%) | Rate | |
| Men | ||||||||
| Age group at diagnosis, y | ||||||||
| 18-24 | 2877 (29.1) | 120.0 | 1569 (20.6) | 43.3 | 1089 (15.6) | 12.5 | 5535 (22.6) | 37.6 |
| 25-34 | 3784 (38.2) | 129.1 | 3064 (40.2) | 62.2 | 2300 (32.9) | 18.3 | 9148 (37.3) | 44.8 |
| 35-44 | 1448 (14.6) | 57.8 | 1603 (21.0) | 36.6 | 1340 (19.1) | 11.4 | 4391 (17.9) | 23.5 |
| 45-54 | 1002 (10.1) | 39.4 | 960 (12.6) | 27.6 | 1351 (19.3) | 9.7 | 3313 (13.5) | 16.6 |
| 55-64 | 608 (6.1) | 28.3 | 319 (4.2) | 14.1 | 721 (10.3) | 5.1 | 1648 (6.7) | 8.8 |
| ≥65 | 177 (1.8) | 10.2 | 108 (1.4) | 5.7 | 200 (2.9) | 1.2 | 485 (2.0) | 2.4 |
| Transmission categoryb,c | ||||||||
| Male-to-male sexual contact | 7895 (79.8) | — | 6638 (87.1) | — | 5795 (82.8) | — | 20 328 (82.9) | — |
| Injection drug use | 309 (3.1) | — | 234 (3.1) | — | 347 (5.0) | — | 889 (3.6) | — |
| Male-to-male sexual contact and injection drug use | 216 (2.2) | — | 244 (3.2) | — | 495 (7.1) | — | 956 (3.9) | — |
| Heterosexual contact d | 1465 (14.8) | — | 502 (6.6) | — | 358 (5.1) | — | 2325 (9.5) | — |
| Other e | 11 (0.1) | — | 5 (0.1) | — | 6 (0.1) | — | 22 (0.1) | — |
| Residence area at diagnosisc,f | ||||||||
| Metropolitan | 8132 (82.2) | — | 6757 (88.6) | — | 5366 (76.7) | — | 20 255 (82.6) | — |
| Urban | 1204 (12.2) | — | 666 (8.7) | — | 1077 (15.4) | — | 2947 (12.0) | — |
| Rural | 494 (5.0) | — | 195 (2.6) | — | 540 (7.7) | — | 1229 (5.0) | — |
| Percentage of residents living below the federal poverty level | ||||||||
| <7.00 | 1134 (11.5) | 50.1 | 857 (11.2) | 26.3 | 1629 (23.3) | 5.8 | 3620 (14.8) | 10.8 |
| 7.00-10.99 | 1253 (12.7) | 57.1 | 1130 (14.8) | 32.3 | 1556 (22.2) | 8.3 | 3939 (16.1) | 16.1 |
| 11.00-18.99 | 2731 (27.6) | 69.7 | 2283 (30.0) | 37.5 | 2078 (29.7) | 10.3 | 7092 (28.9) | 23.5 |
| ≥19.00 | 4775 (48.3) | 82.5 | 3349 (43.9) | 43.8 | 1736 (24.8) | 16.2 | 9860 (40.2) | 40.8 |
| Percentage of residents with <high school diploma | ||||||||
| <6.00 | 1192 (12.1) | 64.8 | 904 (11.9) | 40.3 | 1951 (27.9) | 7.8 | 4047 (16.5) | 13.9 |
| 6.00-10.99 | 1965 (19.9) | 66.0 | 1105 (14.5) | 35.0 | 1954 (27.9) | 7.9 | 5024 (20.5) | 16.3 |
| 11.00-17.99 | 2739 (27.7) | 69.0 | 1460 (19.2) | 35.3 | 1585 (22.6) | 9.0 | 5784 (23.6) | 22.5 |
| ≥18.00 | 4000 (40.4) | 73.0 | 4154 (54.5) | 37.7 | 1511 (21.6) | 14.3 | 9665 (39.4) | 35.7 |
| Median annual household income, $ | ||||||||
| <40 000 | 4723 (47.7) | 83.2 | 2950 (38.7) | 44.7 | 1479 (21.1) | 13.8 | 9152 (37.3) | 39.8 |
| 40 000-53 999 | 2368 (23.9) | 68.5 | 2027 (26.6) | 37.2 | 1835 (26.2) | 9.6 | 6230 (25.4) | 22.2 |
| 54 000-74 999 | 1743 (17.6) | 60.2 | 1613 (21.2) | 33.1 | 2012 (28.7) | 8.6 | 5368 (21.9) | 17.2 |
| ≥75 000 | 1050 (10.6) | 50.3 | 1026 (13.5) | 28.9 | 1669 (23.8) | 6.8 | 3745 (15.3) | 12.5 |
| Percentage of residents in the workforce without a job | ||||||||
| <2.00 | 664 (6.7) | 46.9 | 684 (9.0) | 32.7 | 1103 (15.8) | 7.1 | 2451 (10.0) | 12.8 |
| 2.00-3.99 | 2178 (22.0) | 58.7 | 2245 (29.5) | 35.1 | 2734 (39.1) | 7.8 | 7157 (29.2) | 15.9 |
| 4.00-5.99 | 2593 (26.2) | 69.7 | 2265 (29.7) | 37.8 | 1886 (26.9) | 10.2 | 6744 (27.5) | 23.9 |
| ≥6.00 | 4461 (45.1) | 82.3 | 2429 (31.9) | 40.0 | 1278 (18.3) | 14.6 | 8168 (33.3) | 40.3 |
| Percentage of residents without health insurance | ||||||||
| <6.00 | 824 (8.3) | 44.7 | 720 (9.5) | 27.8 | 1495 (21.4) | 5.7 | 3039 (12.4) | 9.9 |
| 6.00-9.99 | 1499 (15.2) | 58.0 | 979 (12.8) | 31.5 | 1603 (22.9) | 7.8 | 4081 (16.6) | 15.5 |
| 10.00-15.99 | 2620 (26.5) | 66.1 | 1551 (20.4) | 35.6 | 1874 (26.8) | 10.2 | 6045 (24.7) | 22.6 |
| ≥16.00 | 4951 (50.0) | 85.7 | 4369 (57.3) | 41.9 | 2029 (29.0) | 16.1 | 11 349 (46.3) | 39.4 |
| Percentage of housing units that are vacant | ||||||||
| <5.00 | 1366 (13.8) | 54.9 | 1794 (23.5) | 30.0 | 1517 (21.7) | 7.2 | 4677 (19.1) | 15.8 |
| 5.00-8.99 | 2179 (22.0) | 64.7 | 2147 (28.2) | 37.5 | 1836 (26.2) | 8.7 | 6162 (25.1) | 20.4 |
| 9.00-14.99 | 2988 (30.2) | 75.6 | 2010 (26.4) | 41.0 | 1945 (27.8) | 10.3 | 6943 (28.3) | 25.0 |
| ≥15.00 | 3357 (33.9) | 77.1 | 1668 (21.9) | 43.2 | 1700 (24.3) | 10.2 | 6725 (27.4) | 27.1 |
| Subtotal | 9896 (100.0) | 69.4 | 7623 (100.0) | 37.1 | 7001 (100.0) | 9.0 | 24 520 (100.0) | 21.8 |
| Women | ||||||||
| Age group at diagnosis, y | ||||||||
| 18-24 | 490 (13.6) | 21.1 | 140 (13.7) | 4.1 | 136 (12.1) | 1.6 | 766 (13.3) | 5.5 |
| 25-34 | 988 (27.3) | 31.8 | 266 (26.0) | 5.9 | 330 (29.3) | 2.7 | 1584 (27.5) | 8.0 |
| 35-44 | 834 (23.1) | 29.7 | 233 (22.7) | 5.5 | 256 (22.7) | 2.2 | 1323 (22.9) | 7.1 |
| 45-54 | 671 (18.6) | 23.3 | 228 (22.2) | 6.6 | 230 (20.4) | 1.6 | 1129 (19.6) | 5.5 |
| 55-64 | 476 (13.2) | 18.6 | 117 (11.4) | 4.8 | 149 (13.2) | 1.0 | 742 (12.9) | 3.7 |
| ≥65 | 155 (4.3) | 6.0 | 41 (4.0) | 1.6 | 27 (2.4) | 0.1 | 223 (3.9) | 0.9 |
| Transmission category b,c | ||||||||
| Injection drug use | 268 (7.4) | — | 115 (11.2) | — | 343 (30.4) | — | 726 (12.6) | — |
| Heterosexual contact d | 3326 (92.0) | — | 908 (88.6) | — | 781 (69.3) | — | 5015 (87.0) | — |
| Other e | 21 (0.6) | — | 2 (0.2) | — | 4 (0.3) | — | 27 (0.5) | — |
| Residence area at diagnosis c,f | ||||||||
| Metropolitan | 2984 (82.6) | — | 877 (85.6) | — | 802 (71.1) | — | 4663 (80.9) | — |
| Urban | 434 (12.0) | — | 105 (10.2) | — | 215 (19.1) | — | 754 (13.1) | — |
| Rural | 165 (4.6) | — | 40 (3.9) | — | 106 (9.4) | — | 311 (5.4) | — |
| Percentage of residents living below the federal poverty level | ||||||||
| <7.00 | 370 (10.2) | 15.3 | 104 (10.2) | 3.1 | 223 (19.8) | 0.8 | 697 (12.1) | 2.0 |
| 7.00-10.99 | 448 (12.4) | 18.7 | 137 (13.4) | 4.0 | 224 (19.9) | 1.1 | 809 (14.0) | 3.2 |
| 11.00-18.99 | 968 (26.8) | 21.9 | 272 (26.5) | 4.6 | 328 (29.1) | 1.5 | 1568 (27.2) | 5.0 |
| ≥19.00 | 1828 (50.6) | 26.1 | 512 (50.0) | 6.6 | 353 (31.3) | 3.2 | 2693 (46.7) | 10.4 |
| Percentage of residents with <high school diploma | ||||||||
| <6.00 | 304 (8.4) | 14.8 | 85 (8.3) | 3.6 | 184 (16.3) | 0.7 | 573 (9.9) | 1.9 |
| 6.00-10.99 | 615 (17.0) | 18.0 | 134 (13.1) | 4.1 | 300 (26.6) | 1.2 | 1049 (18.2) | 3.2 |
| 11.00-17.99 | 1002 (27.7) | 21.2 | 188 (18.3) | 4.5 | 305 (27.0) | 1.6 | 1495 (25.9) | 5.4 |
| ≥18.00 | 1693 (46.9) | 27.9 | 618 (60.3) | 5.8 | 339 (30.1) | 3.2 | 2650 (46.0) | 9.6 |
| Median annual household income, $ | ||||||||
| <40 000 | 1811 (50.1) | 26.1 | 450 (43.9) | 6.7 | 335 (29.7) | 2.9 | 2596 (45.0) | 10.3 |
| 40 000-53 999 | 823 (22.8) | 21.3 | 276 (26.9) | 5.2 | 309 (27.4) | 1.5 | 1408 (24.4) | 4.8 |
| 54 000-74 999 | 621 (17.2) | 19.5 | 183 (17.9) | 3.8 | 292 (25.9) | 1.2 | 1096 (19.0) | 3.4 |
| ≥75 000 | 358 (9.9) | 16.1 | 116 (11.3) | 3.2 | 192 (17.0) | 0.8 | 666 (11.6) | 2.1 |
| Percentage of residents in the workforce without a job | ||||||||
| <2.00 | 191 (5.3) | 16.9 | 75 (7.3) | 4.0 | 137 (12.2) | 0.8 | 403 (7.0) | 2.1 |
| 2.00-3.99 | 724 (20.0) | 18.1 | 273 (26.6) | 4.3 | 402 (35.6) | 1.1 | 1399 (24.3) | 3.0 |
| 4.00-5.99 | 1011 (28.0) | 23.3 | 307 (30.0) | 5.1 | 321 (28.5) | 1.6 | 1639 (28.4) | 5.5 |
| ≥6.00 | 1688 (46.7) | 24.9 | 370 (36.1) | 5.9 | 268 (23.8) | 2.9 | 2326 (40.3) | 10.4 |
| Percentage of residents without health insurance | ||||||||
| <6.00 | 286 (7.9) | 14.8 | 90 (8.8) | 3.3 | 205 (18.2) | 0.7 | 581 (10.1) | 1.8 |
| 6.00-9.99 | 480 (13.3) | 16.5 | 147 (14.3) | 4.5 | 248 (22.0) | 1.1 | 875 (15.2) | 3.2 |
| 10.00-15.99 | 865 (23.9) | 18.7 | 218 (21.3) | 5.0 | 282 (25.0) | 1.5 | 1365 (23.7) | 4.8 |
| ≥16.00 | 1983 (54.9) | 29.3 | 570 (55.6) | 5.6 | 393 (34.8) | 3.0 | 2946 (51.1) | 9.9 |
| Percentage of housing units that are vacant | ||||||||
| <5.00 | 547 (15.1) | 19.6 | 233 (22.7) | 3.8 | 205 (18.2) | 0.9 | 985 (17.1) | 3.2 |
| 5.00-8.99 | 826 (22.9) | 21.1 | 265 (25.9) | 4.6 | 284 (25.2) | 1.3 | 1375 (23.8) | 4.3 |
| 9.00-14.99 | 1053 (29.1) | 22.9 | 277 (27.0) | 5.7 | 314 (27.8) | 1.6 | 1644 (28.5) | 5.6 |
| ≥15.00 | 1188 (32.9) | 24.1 | 250 (24.4) | 6.6 | 325 (28.8) | 1.9 | 1763 (30.6) | 6.8 |
| Subtotal | 3614 (100.0) | 22.2 | 1025 (100.0) | 5.0 | 1128 (100.0) | 1.4 | 5767 (100.0) | 4.9 |
| Total g | 13 510 (100.0) | 44.3 | 8648 (100.0) | 21.1 | 8129 (100.0) | 5.1 | 30 287 (100.0) | 13.1 |
aData collected from the Centers for Disease Control and Prevention National HIV Surveillance System 1 and the US Census Bureau’s American Community Survey. 14 Numbers <12 and rates based on these numbers should be interpreted with caution.
bData have been statistically adjusted to account for missing data on transmission.
cRates not calculated because of lack of denominator data.
dHeterosexual contact with a person known to have, or to be at high risk for, HIV infection.
eIncludes hemophilia, blood transfusion, perinatal exposure, and risk factor not reported or not identified.
fArea of residence defined as metropolitan (large metropolitan area with ≥500 000 population), urban (smaller metropolitan area with 50 000-499 999 population), or rural (nonmetropolitan area with <50 000 population). 15
gTotals may not be representative of all people with HIV in these areas during 2017.
Of the 24 520 men, the highest HIV diagnosis percentage (37.3%) and rate per 100 000 population (44.8) were among adults aged 25-34. Most HIV infections among men were attributed to male-to-male sexual contact (82.9%), and most men with an HIV diagnosis were metropolitan residents (82.6%). Diagnosis rates per 100 000 population among Black (69.4) and Hispanic/Latino (37.1) men were nearly 8 and 4 times that of White men (9.0), respectively.
Of the 5767 women, the highest HIV diagnosis percentage (27.5%) and rate per 100 000 population (8.0) were among women aged 25-34. Most HIV infections among women were attributed to heterosexual contact (87.0%), and most women with an HIV diagnosis were metropolitan residents (80.9%). Diagnosis rates per 100 000 population among Black (22.2) and Hispanic/Latino (5.0) women were nearly 16 and 4 times that of White women (1.4), respectively.
SDH and Geographic Characteristics and Differences in HIV Diagnoses
Regardless of sex, HIV diagnosis rates increased as the percentage of residents living below the FPL increased, the percentage of those with <high school diploma increased, the median annual household income decreased, the percentage of unemployed increased, the percentage of uninsured increased, and the percentage of vacant housing increased (Table 1).
HIV diagnosis rates were higher among men and women who lived in census tracts with the least favorable SDH than among men and women who lived in census tracts with the most favorable SDH (Table 1). Men and women who lived in census tracts with the highest percentage (≥16%) of uninsured residents had HIV diagnosis rates per 100 000 population that were 4 and nearly 6 times the rate of men and women who lived in census tracts with the lowest percentage (<6%) of uninsured residents (men, 39.4 vs 9.9; women, 9.9 vs 1.8). We observed a similar pattern of higher rates among men and women by race/ethnicity who lived in census tracts with other least favorable SDH, except among Hispanic/Latino men for education. Hispanic/Latino men who lived in census tracts with the highest percentage (≥18%) and lowest percentage (<6%) of residents with <high school education had similar diagnosis rates of 37.7 and 40.3, respectively.
We observed a similar pattern of higher HIV diagnosis rates per 100 000 population by sex and region among racial/ethnic groups who lived in census tracts with the least favorable SDH (Table 2). HIV diagnosis rates were highest among Black (49.6) and White (6.5) adults in the South and among Hispanic/Latino (27.4) adults in the Northeast. In the South, the HIV diagnosis rate among Black men who lived in census tracts with the highest unemployment percentage (≥6%) was 1.7 times the rate among Black men who lived in census tracts with the lowest unemployment percentage (<2%; 97.4 vs 56.1). Also in the South, HIV diagnosis rates among Black women who lived in census tracts with the highest poverty percentage (≥19%) or the largest percentage of residents with <high school education (>18%) were 1.9 times the rates among Black women who lived in tracts with the lowest (<7%) poverty percentage (30.0 vs 15.7) or lowest percentage (<6%) of residents with <high school diploma (31.8 vs 16.9), respectively. Similarly, the HIV diagnosis rate among White men in the South who lived in census tracts with the highest percentage (≥16%) of uninsured residents was 2 times the rate among White men who lived in census tracts with the lowest percentage (<6%) of uninsured residents (15.6 vs 7.8), and the rate among White women in the South who lived in census tracts with the highest percentage (≥18%) of residents with <high school diploma was 3 times the rate among White women who lived in census tracts with the lowest percentage (<6%) of residents with <high school diploma (3.0 vs 1.0). Also, in this region, HIV diagnosis rates among both Black men and women who lived in census tracts with the least favorable or most favorable SDH were higher than the rates among White men and women who lived in similar areas. The HIV diagnosis rates per 100 000 population among Black men who lived in census tracts with the highest (≥19%) or lowest (<7%) percentage of poverty (93.6 and 59.6, respectively) were nearly 6 and 7 times the rates among White men who lived in similar areas (16.3 and 8.5, respectively; Table 2). Similarly, the HIV diagnosis rates among Black women who lived in census tracts with the highest (≥18%) and lowest (<6%) percentage of residents with <high school diploma (31.8 and 16.9, respectively) were nearly 11 and 17 times the rates among White women who lived in similar areas (3.0 and 1.0, respectively; Table 2).
Table 2.
Percentages and rates (per 100 000 population) of HIV diagnoses among Black or African American, Hispanic/Latino, and White adults aged ≥18, by sex, selected characteristics, and US Census region, United States, 2017 a
| Characteristic | Black or African American | Hispanic/Latino | White | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Northeast | Midwest | South | West | Northeast | Midwest | South | West | Northeast | Midwest | South | West | |
| Men | ||||||||||||
| Age group at diagnosis, y | ||||||||||||
| 18-24 | 22.5 (70.0) | 32.0 (114.9) | 30.3 (142.2) | 23.7 (91.4) | 20.4 (54.5) | 23.4 (35.7) | 19.2 (49.8) | 22.1 (36.7) | 13.7 (7.0) | 18.6 (9.9) | 15.4 (15.8) | 14.6 (15.9) |
| 25-34 | 34.4 (85.7) | 38.7 (120.4) | 38.5 (148.3) | 41.3 (118.0) | 41.6 (78.3) | 40.3 (46.2) | 40.3 (73.5) | 40.6 (51.3) | 35.1 (13.1) | 32.4 (12.6) | 31.7 (22.4) | 34.2 (23.0) |
| 35-44 | 16.6 (50.0) | 12.4 (45.7) | 14.6 (64.7) | 16.5 (57.0) | 20.0 (44.3) | 22.4 (28.0) | 21.9 (43.5) | 20.4 (30.1) | 19.1 (7.7) | 19.4 (7.9) | 18.8 (13.9) | 19.5 (14.5) |
| 45-54 | 14.8 (41.6) | 10.2 (37.3) | 9.2 (40.6) | 10.6 (35.4) | 12.2 (33.3) | 10.5 (18.8) | 12.7 (32.8) | 12.3 (22.4) | 18.6 (5.8) | 18.5 (6.5) | 19.8 (12.5) | 19.4 (12.8) |
| 55-64 | 8.8 (31.1) | 5.5 (23.7) | 5.8 (29.8) | 6.4 (26.0) | 4.4 (18.6) | 3.0 (9.0) | 4.4 (17.9) | 3.2 (9.2) | 10.3 (3.1) | 8.8 (3.0) | 11.2 (7.1) | 9.9 (6.2) |
| ≥65 | 2.9 (12.0) | 1.2 (6.5) | 1.7 (11.3) | 1.7 (8.7) | 1.5 (7.9) | 0.4 (1.8) | 1.5 (7.2) | 1.3 (4.8) | 3.3 (0.9) | 2.4 (0.8) | 3.2 (1.6) | 2.5 (1.3) |
| Transmission category b,c | ||||||||||||
| Male-to-male sexual contact | 70.2 (—) | 83.5 (—) | 79.9 (—) | 85.7 (—) | 83.2 (—) | 89.8 (—) | 88.3 (—) | 90.0 (—) | 82.0 (—) | 84.5 (—) | 81.9 (—) | 83.5 (—) |
| Injection drug use | 8.7 (—) | 3.0 (—) | 2.1 (—) | 3.1 (—) | 6.0 (—) | 2.2 (—) | 2.0 (—) | 2.4 (—) | 6.9 (—) | 5.4 (—) | 4.7 (—) | 4.2 (—) |
| Male-to-male sexual contact and injection drug use | 2.5 (—) | 2.7 (—) | 1.7 (—) | 4.9 (—) | 2.4 (—) | 3.4 (—) | 2.5 (—) | 4.6 (—) | 5.8 (—) | 6.5 (—) | 6.6 (—) | 8.9 (—) |
| Heterosexual contact d | 18.5 (—) | 10.3 (—) | 16.3 (—) | 6.3 (—) | 8.4 (—) | 4.5 (—) | 7.2 (—) | 3.0 (—) | 5.4 (—) | 3.5 (—) | 6.8 (—) | 3.3 (—) |
| Other e | 0.2 (—) | 0.4 (—) | 0.0 (—) | 0.1 (—) | 0.0 (—) | 0.1 (—) | 0.1 (—) | 0.1 (—) | 0.1 (—) | 0.2 (—) | 0.1 (—) | 0.1 (—) |
| Residence area at diagnosisc,f | ||||||||||||
| Metropolitan | 96.0 (—) | 86.5 (—) | 76.6 (—) | 96.4 (—) | 95.1 (—) | 83.1 (—) | 87.7 (—) | 89.6 (—) | 85.6 (—) | 69.5 (—) | 71.8 (—) | 85.9 (—) |
| Urban | 3.3 (—) | 11.7 (—) | 15.2 (—) | 3.1 (—) | 4.1 (—) | 11.1 (—) | 8.8 (—) | 8.5 (—) | 10.4 (—) | 17.2 (—) | 18.9 (—) | 10.4 (—) |
| Rural | 0.5 (—) | 1.9 (—) | 7.2 (—) | 0.5 (—) | 0.8 (—) | 5.7 (—) | 3.3 (—) | 1.9 (—) | 3.9 (—) | 13.3 (—) | 8.8 (—) | 3.8 (—) |
| Social determinants of health at census-tract level | ||||||||||||
| Percentage of residents living below the federal poverty level | ||||||||||||
| <7.00 | 13.1 (35.7) | 8.9 (43.5) | 11.7 (59.6) | 11.9 (37.5) | 10.7 (25.0) | 15.1 (21.4) | 12.9 (33.9) | 10.1 (20.4) | 33.1 (3.9) | 24.9 (4.1) | 21.6 (8.5) | 20.4 (6.9) |
| 7.00-10.99 | 12.1 (39.3) | 9.2 (44.5) | 13.2 (67.3) | 16.2 (50.1) | 12.9 (37.3) | 16.7 (24.2) | 15.7 (38.8) | 16.2 (26.8) | 19.2 (4.9) | 22.0 (5.4) | 21.9 (10.9) | 24.4 (10.7) |
| 11.00-18.99 | 25.9 (55.1) | 23.4 (62.4) | 28.7 (76.5) | 29.4 (61.8) | 27.9 (50.9) | 28.8 (25.9) | 32.1 (44.4) | 31.5 (30.0) | 23.7 (7.5) | 28.1 (7.4) | 31.4 (11.5) | 30.8 (13.2) |
| ≥19.00 | 48.8 (63.4) | 58.5 (75.6) | 46.4 (93.6) | 42.5 (86.2) | 48.6 (59.4) | 39.3 (42.2) | 39.3 (51.7) | 42.3 (39.2) | 24.0 (15.0) | 25.1 (12.8) | 25.1 (16.3) | 24.4 (20.4) |
| Percentage of residents with <high school diploma | ||||||||||||
| <6.00 | 7.0 (34.1) | 13.7 (57.1) | 12.2 (78.7) | 14.8 (52.3) | 8.0 (33.5) | 16.9 (32.0) | 14.1 (52.5) | 11.1 (33.4) | 30.9 (4.8) | 29.2 (5.5) | 24.4 (10.9) | 31.6 (9.6) |
| 6.00-10.99 | 15.9 (40.0) | 21.7 (62.0) | 20.6 (78.4) | 16.3 (47.4) | 11.4 (32.0) | 19.4 (25.9) | 17.5 (47.6) | 12.0 (25.8) | 29.5 (4.7) | 32.6 (5.5) | 26.7 (11.7) | 26.0 (9.8) |
| 11.00-17.99 | 30.2 (53.0) | 29.7 (64.8) | 27.4 (76.9) | 22.2 (62.5) | 18.2 (42.3) | 22.2 (29.8) | 21.4 (42.9) | 16.2 (27.6) | 20.9 (6.5) | 23.7 (7.1) | 24.8 (10.1) | 18.9 (11.2) |
| ≥18.00 | 46.9 (61.6) | 34.9 (67.3) | 39.7 (80.3) | 46.7 (71.5) | 62.4 (55.9) | 41.5 (29.2) | 47.0 (41.4) | 60.8 (32.7) | 18.9 (14.5) | 14.6 (11.2) | 24.1 (12.8) | 23.4 (21.2) |
| Median annual household income, $ | ||||||||||||
| <40 000 | 41.8 (63.8) | 58.6 (75.0) | 48.1 (92.8) | 33.5 (97.7) | 36.3 (58.0) | 37.9 (43.5) | 39.5 (53.5) | 31.7 (40.5) | 15.1 (11.3) | 23.4 (11.4) | 24.3 (14.0) | 16.8 (18.7) |
| 40 000-53 999 | 23.8 (55.2) | 20.8 (56.3) | 24.6 (76.3) | 24.7 (63.6) | 24.8 (50.5) | 29.2 (25.1) | 27.9 (42.6) | 28.2 (31.7) | 17.6 (5.8) | 29.7 (6.7) | 29.0 (11.4) | 23.0 (13.3) |
| 54 000-74 999 | 18.7 (43.0) | 14.1 (54.2) | 17.4 (69.0) | 24.0 (53.5) | 23.5 (44.4) | 23.0 (24.9) | 20.0 (38.9) | 23.8 (26.8) | 30.2 (5.8) | 30.7 (5.6) | 26.8 (11.2) | 30.1 (11.6) |
| ≥75 000 | 15.8 (41.4) | 6.6 (45.8) | 9.7 (58.2) | 17.7 (41.7) | 15.2 (31.5) | 9.9 (20.4) | 12.5 (35.1) | 16.4 (24.8) | 37.1 (4.8) | 16.2 (4.2) | 19.8 (9.2) | 29.9 (8.5) |
| Percentage of residents in the workforce without a job | ||||||||||||
| <2.00 | 4.0 (26.4) | 6.3 (37.3) | 7.4 (56.1) | 6.4 (38.0) | 4.8 (28.2) | 10.9 (24.5) | 12.9 (40.7) | 6.2 (24.3) | 12.4 (4.3) | 20.2 (5.1) | 17.3 (9.7) | 11.5 (8.0) |
| 2.00-3.99 | 19.4 (42.9) | 17.1 (50.9) | 23.8 (66.4) | 21.7 (48.9) | 27.8 (43.7) | 28.2 (25.0) | 35.1 (41.2) | 25.4 (27.9) | 40.6 (4.9) | 40.0 (5.4) | 39.5 (10.2) | 36.8 (9.9) |
| 4.00-5.99 | 25.7 (51.9) | 18.4 (61.4) | 27.3 (77.1) | 33.4 (69.0) | 28.3 (47.2) | 24.2 (26.1) | 31.3 (46.2) | 31.2 (31.2) | 27.7 (6.4) | 22.5 (7.3) | 27.4 (12.6) | 28.9 (12.4) |
| ≥6.00 | 50.9 (60.9) | 58.3 (76.2) | 41.6 (97.4) | 38.5 (71.4) | 39.1 (53.0) | 36.7 (38.8) | 20.7 (48.6) | 37.1 (34.7) | 19.3 (11.0) | 17.4 (11.7) | 15.7 (15.5) | 22.7 (17.9) |
| Percentage of residents without health insurance | ||||||||||||
| <6.00 | 15.5 (35.9) | 12.0 (45.0) | 6.0 (59.3) | 8.9 (33.3) | 15.3 (33.1) | 16.7 (27.3) | 4.4 (37.7) | 8.1 (24.3) | 46.8 (4.8) | 29.6 (4.5) | 12.0 (7.8) | 19.7 (7.4) |
| 6.00-9.99 | 24.1 (50.0) | 21.3 (58.2) | 11.8 (67.0) | 16.3 (49.1) | 17.9 (44.7) | 16.1 (24.6) | 7.6 (40.1) | 12.8 (25.9) | 25.4 (5.6) | 28.3 (5.8) | 17.4 (8.9) | 27.4 (11.1) |
| 10.00-15.99 | 33.6 (59.8) | 32.7 (68.6) | 23.3 (68.3) | 28.8 (63.9) | 23.8 (49.0) | 21.4 (27.3) | 15.7 (40.6) | 24.7 (30.1) | 17.2 (8.2) | 25.4 (8.2) | 30.4 (11.0) | 26.0 (11.3) |
| ≥16.00 | 26.8 (60.6) | 34.0 (75.4) | 58.9 (91.3) | 46.0 (82.3) | 43.0 (54.5) | 45.8 (32.9) | 72.2 (45.9) | 54.4 (34.6) | 10.6 (13.5) | 16.8 (13.4) | 40.2 (15.6) | 27.0 (20.4) |
| Percentage of housing units that are vacant | ||||||||||||
| <5.00 | 21.5 (50.8) | 10.8 (43.9) | 10.8 (62.5) | 31.2 (51.0) | 26.5 (43.7) | 20.0 (23.5) | 15.1 (32.3) | 37.1 (26.6) | 25.3 (4.8) | 24.6 (5.0) | 13.7 (9.1) | 31.7 (9.8) |
| 5.00-8.99 | 30.2 (53.1) | 17.3 (55.1) | 20.1 (73.3) | 33.3 (60.4) | 33.3 (47.7) | 24.6 (23.9) | 25.1 (40.5) | 33.7 (34.4) | 30.3 (6.0) | 28.6 (6.2) | 22.1 (10.7) | 29.7 (11.8) |
| 9.00-14.99 | 27.9 (52.7) | 25.9 (63.6) | 32.5 (85.1) | 24.3 (82.2) | 25.2 (45.4) | 34.1 (34.5) | 31.6 (46.7) | 19.8 (36.4) | 26.5 (6.9) | 28.0 (7.4) | 31.1 (12.1) | 22.5 (13.9) |
| ≥15.00 | 20.4 (51.8) | 46.0 (77.7) | 36.6 (84.1) | 11.3 (75.2) | 14.9 (53.7) | 21.4 (37.0) | 28.2 (56.1) | 9.4 (31.2) | 17.9 (5.9) | 18.8 (7.4) | 33.0 (12.2) | 16.0 (11.7) |
| Subtotal | 100.0 (51.7) | 100.0 (63.8) | 100.0 (78.7) | 100.0 (61.2) | 100.0 (46.7) | 100.0 (29.0) | 100.0 (44.0) | 100.0 (30.9) | 100.0 (5.8) | 100.0 (6.3) | 100.0 (11.3) | 100.0 (11.4) |
| Women | ||||||||||||
| Age group at diagnosis, y | ||||||||||||
| 18-24 | 9.9 (16.0) | 16.4 (19.3) | 14.0 (24.0) | 12.9 (16.4) | 8.1 (4.5) | 14.8 (2.7) | 15.7 (5.8) | 18.8 (3.2) | 10.1 (0.9) | 15.4 (1.3) | 12.7 (2.6) | 8.5 (1.1) |
| 25-34 | 22.5 (27.1) | 33.8 (31.4) | 28.0 (35.6) | 20.8 (19.0) | 24.4 (9.6) | 27.8 (3.9) | 27.0 (7.2) | 27.1 (3.6) | 26.4 (1.7) | 30.3 (1.9) | 28.8 (3.9) | 32.0 (2.6) |
| 35-44 | 24.3 (32.6) | 22.8 (23.6) | 22.6 (31.4) | 25.3 (27.4) | 23.6 (10.2) | 16.7 (2.5) | 23.1 (6.4) | 23.1 (3.4) | 16.9 (1.2) | 22.1 (1.4) | 24.3 (3.4) | 23.0 (2.0) |
| 45-54 | 21.6 (26.8) | 13.5 (14.0) | 18.7 (25.8) | 19.5 (19.9) | 25.6 (12.8) | 29.6 (6.3) | 18.8 (6.5) | 20.5 (3.7) | 29.1 (1.5) | 15.9 (0.9) | 19.5 (2.3) | 20.5 (1.6) |
| 55-64 | 16.1 (23.4) | 11.0 (12.4) | 12.4 (19.1) | 17.8 (20.8) | 14.6 (10.4) | 3.7 (1.2) | 10.8 (5.5) | 8.7 (2.3) | 14.9 (0.8) | 15.4 (0.8) | 12.0 (1.3) | 13.5 (0.9) |
| ≥65 | 5.7 (7.5) | 2.7 (3.0) | 4.3 (6.9) | 3.7 (4.3) | 3.7 (2.6) | 7.4 (3.0) | 4.6 (2.2) | 1.8 (0.5) | 2.7 (0.1) | 1.0 (0.0) | 2.7 (0.2) | 2.5 (0.1) |
| Transmission categoryb,c | ||||||||||||
| Injection drug use | 11.4 (—) | 9.5 (—) | 5.5 (—) | 10.7 (—) | 13.9 (—) | 12.2 (—) | 7.3 (—) | 16.2 (—) | 40.1 (—) | 33.1 (—) | 26.4 (—) | 32.5 (—) |
| Heterosexual contact d | 88.2 (—) | 89.1 (—) | 94.1 (—) | 87.9 (—) | 85.4 (—) | 87.6 (—) | 92.7 (—) | 83.7 (—) | 59.6 (—) | 66.5 (—) | 73.5 (—) | 66.7 (—) |
| Other e | 0.4 (—) | 1.4 (—) | 0.4 (—) | 1.4 (—) | 0.7 (—) | 0.2 (—) | 0.1 (—) | 0.1 (—) | 0.3 (—) | 0.5 (—) | 0.2 (—) | 0.8 (—) |
| Residence area at diagnosisc,f | ||||||||||||
| Metropolitan | 95.0 (—) | 85.1 (—) | 77.3 (—) | 95.0 (—) | 93.5 (—) | 68.5 (—) | 85.8 (—) | 86.9 (—) | 79.1 (—) | 70.8 (—) | 65.2 (—) | 82.5 (—) |
| Urban | 5.0 (—) | 11.4 (—) | 14.9 (—) | 3.7 (—) | 4.1 (—) | 14.8 (—) | 8.7 (—) | 11.4 (—) | 15.5 (—) | 18.5 (—) | 22.6 (—) | 12.0 (—) |
| Rural | 0 (—) | 3.5 (—) | 6.4 (—) | 1.2 (—) | 2.4 (—) | 16.7 (—) | 4.8 (—) | 1.8 (—) | 5.4 (—) | 10.8 (—) | 11.3 (—) | 5.5 (—) |
| Social determinants of health at census-tract level | ||||||||||||
| Percentage of residents living below the federal poverty level | ||||||||||||
| <7.00 | 13.6 (17.7) | 8.7 (13.4) | 9.6 (15.7) | 10.8 (10.9) | 8.9 (4.0) | 14.8 (2.4) | 11.6 (3.8) | 11.4 (2.2) | 32.4 (0.6) | 15.4 (0.4) | 17.8 (1.3) | 20.5 (0.8) |
| 7.00-10.99 | 11.7 (17.8) | 9.1 (13.5) | 12.6 (20.4) | 19.1 (17.6) | 13.0 (7.3) | 16.7 (2.8) | 16.1 (5.3) | 12.7 (2.1) | 14.2 (0.6) | 16.9 (0.6) | 20.4 (1.8) | 25.5 (1.2) |
| 11.00-18.99 | 23.0 (21.1) | 24.6 (18.8) | 28.0 (23.3) | 29.5 (18.1) | 19.9 (7.1) | 38.9 (4.1) | 30.4 (5.7) | 32.3 (3.0) | 26.4 (1.4) | 30.8 (1.2) | 31.5 (2.1) | 22.5 (1.1) |
| ≥19.00 | 51.7 (26.8) | 57.6 (19.1) | 49.9 (30.0) | 40.7 (22.7) | 58.1 (12.4) | 29.6 (3.8) | 41.9 (7.5) | 43.7 (4.0) | 27.0 (2.8) | 36.9 (2.8) | 30.3 (3.5) | 31.5 (3.0) |
| Percentage of residents with <high school diploma | ||||||||||||
| <6.00 | 6.0 (13.4) | 10.6 (12.6) | 8.6 (16.9) | 8.3 (9.7) | 6.5 (4.9) | 14.8 (3.0) | 9.4 (4.3) | 8.7 (2.4) | 19.6 (0.5) | 19.0 (0.5) | 12.7 (1.0) | 22.0 (0.7) |
| 6.00-10.99 | 14.3 (16.2) | 20.5 (16.3) | 16.5 (18.9) | 21.6 (19.0) | 8.5 (4.5) | 24.1 (3.7) | 17.4 (5.9) | 11.4 (2.3) | 32.4 (0.8) | 26.7 (0.7) | 25.3 (2.0) | 26.0 (1.1) |
| 11.00-17.99 | 29.7 (1.9) | 31.3 (18.0) | 26.7 (22.3) | 25.7 (20.6) | 16.3 (7.1) | 22.2 (3.6) | 22.7 (6.0) | 12.7 (2.1) | 22.3 (1.1) | 26.7 (1.2) | 31.3 (2.3) | 18.0 (1.2) |
| ≥18.00 | 50.1 (28.3) | 37.7 (20.8) | 48.2 (31.8) | 44.4 (19.6) | 68.7 (11.5) | 38.9 (3.3) | 50.6 (6.3) | 67.3 (3.6) | 25.7 (3.4) | 27.7 (3.3) | 30.7 (3.0) | 34.0 (3.6) |
| Median annual household income, $ | ||||||||||||
| <40 000 | 45.9 (27.3) | 58.2 (19.0) | 51.6 (29.5) | 30.7 (24.2) | 46.8 (12.6) | 33.3 (4.5) | 38.3 (7.1) | 34.1 (4.3) | 18.9 (2.3) | 38.5 (2.7) | 31.2 (3.2) | 24.5 (3.0) |
| 40 000-53 999 | 21.4 (21.9) | 22.4 (17.8) | 22.8 (22.3) | 27.0 (20.1) | 21.1 (8.5) | 40.7 (4.2) | 32.5 (6.8) | 28.8 (3.2) | 25.0 (1.4) | 28.2 (0.9) | 30.5 (2.1) | 19.5 (1.2) |
| 54 000-74 999 | 18.5 (19.3) | 13.9 (16.1) | 16.9 (21.3) | 22.8 (14.8) | 21.5 (8.0) | 14.8 (1.9) | 16.6 (4.3) | 23.1 (2.6) | 26.4 (0.8) | 24.6 (0.7) | 24.8 (1.9) | 30.0 (1.3) |
| ≥75 000 | 14.3 (17.4) | 5.6 (12.4) | 8.6 (16.7) | 19.5 (14.6) | 10.6 (4.1) | 11.1 (2.5) | 12.5 (4.4) | 14.0 (2.0) | 29.7 (0.6) | 8.7 (0.3) | 13.5 (1.1) | 26.0 (0.8) |
| Percentage of residents in the workforce without a job | ||||||||||||
| <2.00 | 2.8 (13.4) | 6.4 (16.9) | 5.7 (17.6) | 5.4 (16.6) | 4.5 (5.7) | 13.0 (3.6) | 10.6 (4.7) | 4.4 (2.0) | 8.1 (0.5) | 18.0 (0.7) | 12.2 (1.2) | 9.5 (0.7) |
| 2.00-3.99 | 17.8 (18.1) | 16.8 (15.7) | 20.6 (18.7) | 27.0 (19.3) | 21.5 (6.5) | 38.9 (4.0) | 32.3 (5.0) | 25.8 (2.8) | 39.9 (0.8) | 28.2 (0.6) | 38.0 (1.8) | 33.0 (1.0) |
| 4.00-5.99 | 23.3 (20.1) | 21.1 (19.1) | 29.6 (25.3) | 38.6 (22.6) | 23.6 (7.3) | 22.2 (2.8) | 35.9 (7.1) | 32.3 (3.1) | 29.7 (1.1) | 23.1 (1.1) | 28.9 (2.4) | 31.5 (1.5) |
| ≥6.00 | 56.1 (26.7) | 55.7 (18.0) | 44.1 (29.5) | 29.1 (14.0) | 50.4 (12.1) | 25.9 (3.2) | 21.2 (6.7) | 37.6 (3.4) | 22.3 (2.1) | 30.8 (3.0) | 20.9 (3.7) | 26.0 (2.3) |
| Percentage of residents without health insurance | ||||||||||||
| <6.00 | 17.8 (19.8) | 9.7 (11.4) | 5.0 (15.8) | 6.6 (8.2) | 13.4 (5.3) | 13.0 (2.4) | 4.1 (4.4) | 5.7 (1.6) | 46.0 (0.8) | 19.5 (0.4) | 10.5 (1.2) | 19.0 (0.8) |
| 6.00-9.99 | 18.5 (16.4) | 20.1 (15.7) | 9.8 (17.5) | 19.1 (17.5) | 18.3 (8.2) | 20.4 (3.6) | 6.3 (4.2) | 14.0 (2.7) | 23.7 (0.9) | 28.7 (0.9) | 16.8 (1.5) | 29.0 (1.3) |
| 10.00-15.99 | 31.9 (23.0) | 31.3 (17.2) | 20.1 (18.2) | 25.3 (16.5) | 28.5 (10.5) | 25.9 (3.9) | 15.7 (5.3) | 21.0 (2.5) | 19.6 (1.5) | 26.7 (1.3) | 27.9 (1.8) | 19.0 (0.9) |
| ≥16.00 | 31.8 (30.8) | 38.9 (22.9) | 65.2 (30.8) | 49.0 (23.7) | 39.8 (9.9) | 40.7 (3.5) | 74.0 (6.4) | 59.4 (3.7) | 10.8 (2.3) | 25.1 (3.0) | 44.9 (3.1) | 33.0 (2.9) |
| Percentage of housing units that are vacant | ||||||||||||
| <5.00 | 21.5 (21.6) | 15.1 (18.2) | 11.5 (20.7) | 33.6 (15.4) | 24.4 (7.1) | 25.9 (3.5) | 15.9 (4.3) | 40.6 (2.8) | 28.4 (0.9) | 17.4 (0.5) | 10.3 (1.2) | 34.5 (1.2) |
| 5.00-8.99 | 28.2 (21.1) | 16.8 (15.1) | 21.3 (23.2) | 36.1 (18.7) | 30.9 (8.2) | 22.2 (2.5) | 24.6 (5.2) | 30.6 (3.0) | 28.4 (0.9) | 29.2 (0.9) | 21.2 (1.8) | 30.5 (1.3) |
| 9.00-14.99 | 31.1 (24.9) | 25.9 (17.9) | 30.4 (24.3) | 18.7 (18.6) | 27.6 (9.5) | 25.9 (3.1) | 31.1 (6.2) | 23.1 (4.1) | 24.3 (1.0) | 21.0 (0.8) | 33.9 (2.3) | 19.5 (1.3) |
| ≥15.00 | 19.5 (22.2) | 42.2 (18.7) | 36.8 (27.0) | 11.6 (30.3) | 17.1 (12.4) | 25.9 (5.4) | 28.4 (8.0) | 5.7 (2.0) | 18.9 (1.1) | 32.3 (1.9) | 34.6 (2.3) | 15.5 (1.3) |
| Subtotal | 100.0 (22.5) | 100.0 (17.7) | 100.0 (24.4) | 100.0 (18.2) | 100.0 (8.7) | 100.0 (3.4) | 100.0 (5.9) | 100.0 (3.0) | 100.0 (0.9) | 100.0 (0.9) | 100.0 (2.0) | 100.0 (1.3) |
| Total g | 100.0 (35.9) | 100.0 (39.3) | 100.0 (49.6) | 100.0 (39.9) | 100.0 (27.4) | 100.0 (16.7) | 100.0 (25.1) | 100.0 (17.0) | 100.0 (3.3) | 100.0 (3.5) | 100.0 (6.5) | 100.0 (6.3) |
aData collected from the Centers for Disease Control and Prevention National HIV Surveillance System 1 and the US Census Bureau’s American Community Survey. 14 Numbers <12 and rates based on these numbers should be interpreted with caution. Census data by race and transmission category were not available for Puerto Rico; numbers and rates for Puerto Rico are not shown but are included in the total.
bData have been statistically adjusted to account for missing data on transmission.
cRates not calculated because of lack of denominator data.
dHeterosexual contact with a person known to have, or to be at high risk for, HIV infection.
eIncludes hemophilia, blood transfusion, perinatal exposure, and risk factor not reported or not identified.
fArea of residence defined as metropolitan (large metropolitan area with ≥500 000 population), urban (smaller metropolitan area with 50 000-499 999 population), or rural (nonmetropolitan area with <50 000 population). 15
gTotals may not be representative of all people with HIV in these areas during 2017.
In the Northeast, the HIV diagnosis rate per 100 000 population among Hispanic/Latino men who lived in census tracts with the highest percentage (≥19%) of poverty was 2.4 times the rate among Hispanic/Latino men who lived in census tracts with the lowest percentage (<7%) of poverty (59.4 vs 25.0, respectively), and the rates among Hispanic/Latino women who lived in census tracts with the highest percentage (≥19%) of poverty or lowest median annual household income (<$40 000; 12.4 and 12.6, respectively) were 3 times the rates among Hispanic/Latino women who lived in census tracts with the lowest percentage (<7%) of poverty or highest median annual household income (≥$75 000; 4.0 and 4.1, respectively). In addition, the HIV diagnosis rates among Hispanic/Latino men and women who lived in census tracts with the least favorable SDH or the most favorable SDH were higher than the rates among White men and women who lived in similar areas, respectively. The rates among Hispanic/Latino men who lived in census tracts with the lowest (<5%) or highest (≥16%) percentage of vacant housing (43.7 and 53.7, respectively) were 9 times the rates among White men who lived in similar areas (4.8 and 5.9, respectively; Table 2). The HIV diagnosis rates among Hispanic/Latino women who lived in census tracts with the lowest (<2%) or highest (≥6%) percentage of unemployment (5.7 and 12.1, respectively) were 11 and nearly 6 times the rates among White women who lived in similar areas (0.5 and 2.1, respectively). Although the Northeast had higher HIV diagnosis rates among Hispanic/Latino adults than other regions, rates by SDH were similarly high in the South.
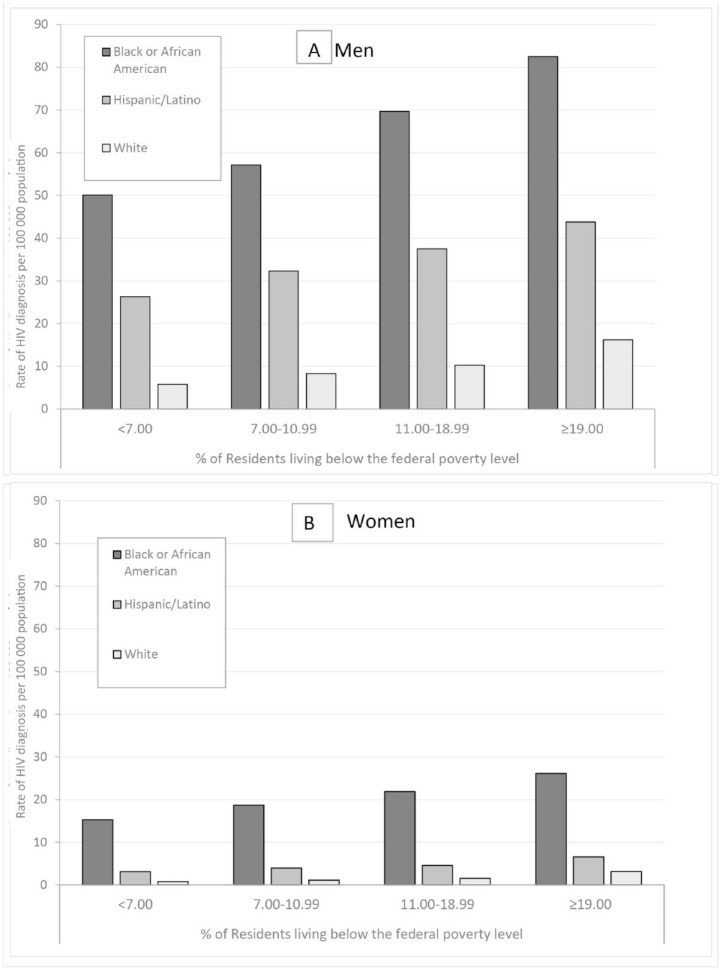
HIV diagnosis rates per 100 000 population by SDH among Black and Hispanic/Latino adults were higher than rates among White adults (Table 2). Among Black men, rates were 8 and 5 times the rates of White men who lived in census tracts with the lowest (<7%) and highest (≥19%) percentages of poverty (Black men: 50.1 and 82.5, respectively; White men: 5.8 and 16.2, respectively; Figure A). Among Hispanic/Latino men, rates were nearly 5 and 3 times the rates of White men who lived in census tracts with the lowest (<7%) and highest (≥19%) percentages of poverty (Hispanic/Latino men: 26.3 and 43.8, respectively; White men: 5.8 and 16.2, respectively; Figure A). Among Black women, HIV diagnosis rates were 19 and 8 times the rates of White women in census tracts with the lowest (<7%) and highest (≥19%) percentages of poverty (Black women: 15.3 and 26.1, respectively; White women: 0.8 and 3.2, respectively; Figure B). Among Hispanic/Latino women, HIV diagnosis rates were nearly 4 and 2 times the rates of White women who lived in census tracts with the lowest (<7%) and highest (≥19%) percentages of poverty (Hispanic/Latino women: 3.1 and 6.6, respectively; White women: 0.8 and 3.2, respectively; Figure B).
Figure.
HIV diagnosis rates by race/ethnicity and federal poverty level, United States and Puerto Rico, 2017. (A) Men. (B) Women. Poverty levels were categorized using empirically derived quartiles determined by data from all census tracts in the United States and Puerto Rico. Data collected from the Centers for Disease Control and Prevention National HIV Surveillance System 1 and the US Census Bureau’s American Community Survey. 14
Discussion
To our knowledge, this is the first ecological, census tract–level analysis that provides exploratory insight into racial/ethnic and regional differences in HIV diagnoses and SDH in the United States and Puerto Rico. We observed an overall pattern of disparity between HIV diagnosis rates and SDH, by race/ethnicity and geography. Unsurprisingly, among racial/ethnic groups, HIV diagnosis rates were higher among adults who lived in census tracts with the least favorable SDH than among adults who lived in census tracts with the most favorable SDH. By region, Black and White adults were disproportionately affected in the South and Hispanic/Latino adults were disproportionately affected in the Northeast. When we compared rates by SDH among racial/ethnic groups, Black and Hispanic/Latino adults were disproportionately affected by HIV compared with White adults.
These findings of higher HIV diagnosis rates in areas with the least favorable SDH suggest that these social and structural factors play a role in the HIV epidemic. Our findings are consistent with previous research that found that HIV diagnosis rates increased as the community socioeconomic position decreased, placing people, especially women and some racial/ethnic groups, at higher risk for infection than others. 16 -19 Other analyses in single US jurisdictions found that neighborhoods with higher levels of poverty, on average, had higher HIV diagnosis rates. 20,21 People with lower levels of education and income are more likely than their more educated, higher-income counterparts to lack job opportunities and experience worse health outcomes. 21,22 Consequently, SDH can affect how people may access and receive preventive or care services for HIV, ultimately increasing their risk for infection or HIV-associated complications.
Black and White adults are disproportionately affected by HIV in the South and Hispanic/Latino adults in the Northeast. 1 Persistent disparities in HIV infection rates, caused by social and structural factors among these groups in these regions, are well documented. 2,9,12,20 -28 Furthermore, among people with undocumented immigration status, language barriers, fear resulting from immigration status or potential deportation, and socioeconomic factors can lead to problems accessing health care. 29 -31 Our findings of racial/ethnic and geographic differences in HIV diagnosis rates highlight the need for investments based on local HIV health equity needs that support culturally appropriate sexual health campaigns and prioritization of interventions among people living in socioeconomically and medically disadvantaged areas. 2,9,17,32
Our results also show that Black and Hispanic/Latino adults, compared with White adults, continue to be disproportionately affected by HIV (except among Hispanic/Latino men for education). HIV prevention among these groups is affected by social and structural factors. Poverty can decrease access to prevention and care services, including preexposure prophylaxis and routine HIV testing, treatment, and care, or contribute to economic instability (food insecurity, inadequate housing, homelessness, lack of health insurance) that can increase the risk for HIV transmission. 11,12,20,21,23,26,31,33 -35 Black and Hispanic/Latino adults were more likely than White adults to live in disadvantaged neighborhoods, where conditions—such as a lack of sexual partners as a result of incarceration or deportation, disproportionate levels of sexually transmitted infections including HIV, and low rates of community viral suppression—can increase the transmission rates of HIV and sexually transmitted infections. 2,16,31,33,36,37 Among Hispanic/Latino men, we suspect the lack of relationship between neighborhood education and HIV may be mediated by factors such as Hispanic/Latino descent, varying immigration policies, migration, and Medicaid expansion; we did not assess these factors in this analysis, and they may contribute to this biased effect among education levels in this group. 38 -41 Despite the availability of tools to prevent HIV transmission, innovative strategies are needed to overcome several factors, including lack of HIV awareness; lack of access to testing, treatment, and prevention; HIV-related stigma and homophobia; and increasing trends in injection drug use among racial/ethnic groups. 13 These efforts, in addition to addressing SDH, are critical to reduce new HIV infections consistent with the goals of Healthy People 2030 and the Ending the HIV Epidemic initiative. 12,13,42,43
Limitations
Our analysis had several limitations. First, diagnoses of HIV infection do not represent incidence or new infections. The time from infection to diagnosis varies by individual and can affect reporting of diagnoses to the surveillance system. Hence, residence at HIV diagnosis may not be the residence at the time HIV infection was acquired. Second, data were limited to people whose residence at diagnosis was complete and could be geocoded; therefore, results may not reflect the entire population of Black, Hispanic/Latino, and White adults with HIV diagnosed in those areas. Third, SDH information is not available at the individual level; we used census tract–level data as a snapshot of the environment in which adults with diagnosed HIV infection lived at the time of diagnosis. Because the data are a snapshot, some SDH indicators may be correlated (eg, lack of education is associated with both poverty and low income in the United States), but we did not analyze correlations between SDH indicators in this study. Thus, the conclusions and findings should be interpreted with caution and not inferred at the individual level. Lastly, the data used for computing race-specific rates may include Hispanic/Latino (except for non-Hispanic/Latino White) and should be interpreted with caution. The ACS does not provide age- and sex-specific SDH variables stratified by ethnicity in its 2013-2017 estimates, except for White people (ie, non-Hispanic/Latino White). The rates and number of people reported in each race category may include people whose ethnicity was not reported. Hispanic/Latino people accounted for 3.7% of the denominator for Black people (2.9% when Puerto Rico is excluded).
Conclusion
Focusing on disparities in rates of HIV infection is appropriate not only for achieving national goals but also for equitable health in HIV-related outcomes. Our findings contribute to the current literature that highlights the importance of SDH in HIV infection and supports the need for effective, targeted social and structural interventions to specific populations at high risk of HIV to prevent infection and reduce racial/ethnic disparities. Future studies should continue to explore single-level and examine multilevel factors of SDH on HIV among racial/ethnic groups at the census-tract level to help direct prevention and care services. Addressing disparities in HIV diagnosis rates by strengthening community–public health partnerships, promoting community empowerment, and implementing strategies of increased testing, care, and prevention efforts with peer navigation for people either living with HIV or at greater risk for HIV are vital to advancing progress for ending the HIV epidemic in the United States.
Acknowledgments
The authors thank our local, tribal, territorial, and state health department jurisdictions; this article would not have been possible without their contributions. The authors also thank Mi Chen and Baohua Wu for their valuable analytic contributions to the NHSS Geocoding and Data Linkage project, and Azfar-E-Alam Siddiqi for his critical review of this article. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Shacara Johnson Lyons, MSPH  https://orcid.org/0000-0002-7539-4169
https://orcid.org/0000-0002-7539-4169
Zanetta Gant, PhD, MS  https://orcid.org/0000-0003-2558-8237
https://orcid.org/0000-0003-2558-8237
Chan Jin, PhD  https://orcid.org/0000-0002-5954-1579
https://orcid.org/0000-0002-5954-1579
Ndidi Nwangwu-Ike, MPH  https://orcid.org/0000-0003-4667-3086
https://orcid.org/0000-0003-4667-3086
References
- 1. Centers for Disease Control and Prevention . Diagnoses of HIV infection in the United States and dependent areas, 2017. HIV Surveill Rep. 2018;29:1-129. [Google Scholar]
- 2. Elmore K., Bradley ELP., Lima AC. et al. Trends in geographic rates of HIV diagnoses among Black females in the United States, 2010-2015. J Womens Health. 2019;28(3):410-417. 10.1089/jwh.2017.6868 [DOI] [PubMed] [Google Scholar]
- 3. Song R., Hall HI., Harrison KM., Sharpe TT., Lin LS., Dean HD. Identifying the impact of social determinants of health on disease rates using correlation analysis of area-based summary information. Public Health Rep. 2011;126(suppl 3):70-80. 10.1177/00333549111260S312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gant Z., Gant L., Song R., Willis L., Johnson AS. A census tract–level examination of social determinants of health among Black/African American men with diagnosed HIV infection, 2005-2009—17 US areas. PLoS One. 2014;9(9): 10.1371/journal.pone.0107701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention . HIV and Hispanics/Latinos. Updated October 13, 2020. Accessed February 5, 2019. https://www.cdc.gov/hiv/group/racialethnic/hispaniclatinos/index.html
- 6. Centers for Disease Control and Prevention . HIV and African Americans. Updated May 18, 2020. Accessed February 5, 2019. https://www.cdc.gov/hiv/group/racialethnic/africanamericans/index.html
- 7. Caiola C., Barroso J., Docherty SL. Black mothers living with HIV picture the social determinants of health. J Assoc Nurses AIDS Care. 2018;29(2):204-219. 10.1016/j.jana.2017.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bose S. Demographic and spatial disparity in HIV prevalence among incarcerated population in the US: a state-level analysis. Int J STD AIDS. 2018;29(3):278-286. 10.1177/0956462417724586 [DOI] [PubMed] [Google Scholar]
- 9. Sutton MY., Gray SC., Elmore K., Gaul Z. Social determinants of HIV disparities in the southern United States and in counties with historically Black colleges and universities (HBCUs), 2013-2014. PLoS One. 2017;12(1): 10.1371/journal.pone.0170714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pouget ER., Kershaw TS., Niccolai LM., Ickovics JR., Blankenship KM. Associations of sex ratios and male incarceration rates with multiple opposite-sex partners: potential social determinants of HIV/STI transmission. Public Health Rep. 2010;125(4 suppl):70-80. 10.1177/00333549101250S411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ransome Y., Kawachi I., Braunstein S., Nash D. Structural inequalities drive late HIV diagnosis: the role of Black racial concentration, income inequality, socioeconomic deprivation, and HIV testing. Health Place. 2016;42:148-158. 10.1016/j.healthplace.2016.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention . Social determinants of health among adults with diagnosed HIV infection, 2017. Part A: census tract–level social determinants of health and diagnosed HIV infection—United States and Puerto Rico. Part B: county-level social determinants of health, selected care outcomes, and diagnosed HIV infection—41 states and the District of Columbia. HIV Surveill Suppl Rep. 2019;24(4):1-134. [Google Scholar]
- 13. Fauci AS., Redfield RR., Sigounas G., Weahkee MD., Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321(9):844-845. 10.1001/jama.2019.1343 [DOI] [PubMed] [Google Scholar]
- 14. US Census Bureau . American Community Survey: 2013-2017 5-year estimates. December 7, 2018. Accessed February 5, 2019. https://www.census.gov/programs-surveys/acs/news/data-releases/2017/release.html
- 15. Office of Management and Budget . Revised delineations of metropolitan statistical areas, micropolitan statistical areas, and combined statistical areas, and guidance on uses of the delineations of these areas. OMB Bulletin 17-01. Published August 15, 2017. Accessed February 5, 2019. http://www.whitehouse.gov/sites/whitehouse.gov/files/omb/bulletins/2017/b-17-01.pdf
- 16. Braveman P. The question is not: “is race or class more important?” J Epidemiol Community Health. 2005;59(12): [PMC free article] [PubMed] [Google Scholar]
- 17. Braveman PA., Cubbin C., Egerter S. et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294(22):2879-2888. 10.1001/jama.294.22.2879 [DOI] [PubMed] [Google Scholar]
- 18. Braveman PA., Egerter SA., Mockenhaupt RE. Broadening the focus: the need to address the social determinants of health. Am J Prev Med. 2011;40(1 Suppl 1):S4-S18. 10.1016/j.amepre.2010.10.002 [DOI] [PubMed] [Google Scholar]
- 19. Braveman PA., Egerter SA., Woolf SH., Marks JS. When do we know enough to recommend action on the social determinants of health? Am J Prev Med. 2011;40(1 Suppl 1):S58-S66. 10.1016/j.amepre.2010.09.026 [DOI] [PubMed] [Google Scholar]
- 20. Wiewel EW., Bocour A., Kersanske LS., Bodach SD., Xia Q., Braunstein SL. The association between neighborhood poverty and HIV diagnoses among males and females in New York City, 2010-2011. Public Health Rep. 2016;131(2):290-302. 10.1177/003335491613100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gibson C., Grande K., Schumann C., Gasiorowicz M. Census tract poverty and racial disparities in HIV rates in Milwaukee County, Wisconsin, 2009-2014. AIDS Behav. 2018;22(9):2994-3002. 10.1007/s10461-018-2064-y [DOI] [PubMed] [Google Scholar]
- 22. Barr D. Health Disparities in the United States: Social Class, Race, Ethnicity, and the Social Determinants of Health. 3rd ed. Johns Hopkins University Press; 2019. [Google Scholar]
- 23. An Q., Prejean J., McDavid Harrison K., Fang X. Association between community socioeconomic position and HIV diagnosis rate among adults and adolescents in the United States, 2005 to 2009. Am J Public Health. 2013;103(1):120-126. 10.2105/AJPH.2012.300853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Williams DR., Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood). 2005;24(2):325-334. 10.1377/hlthaff.24.2.325 [DOI] [PubMed] [Google Scholar]
- 25. Buot M-LG., Docena JP., Ratemo BK. et al. Beyond race and place: distal sociological determinants of HIV disparities. PLoS One. 2014;9(4): 10.1371/journal.pone.0091711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Watson M., Johnson SD., Zhang T., Oster AM. Characteristics of and trends in HIV diagnoses in the Deep South region of the United States, 2012-2017. AIDS Behav. 2019;23(Suppl 3):224-232. 10.1007/s10461-019-02659-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. An Q., Hernandez A., Prejean J. et al. Geographic differences in HIV infection among Hispanics or Latinos—46 states and Puerto Rico, 2010. MMWR Morb Mortal Wkly Rep. 2012;61(40):805-809. [PubMed] [Google Scholar]
- 28. Xia Q., Braunstein SL., Wiewel EW., Hadler JL., Torian LV. Persistent racial disparities in HIV infection in the USA: HIV prevalence matters. J Racial Ethn Health Disparities. 2017;4(1):87-93. 10.1007/s40615-015-0205-9 [DOI] [PubMed] [Google Scholar]
- 29. Demeke HB., Johnson AS., Wu B., Nwangwu-Ike N., King H., Dean HD. Differences between U.S.-born and non–U.S.-born Black adults reported with diagnosed HIV infection: United States, 2008-2014. J Immigr Minor Health. 2019;21(1):30-38. 10.1007/s10903-018-0699-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Deane KD., Parkhurst JO., Johnston D. Linking migration, mobility and HIV. Trop Med Int Health. 2010;15(12):1458-1463. 10.1111/j.1365-3156.2010.02647.x [DOI] [PubMed] [Google Scholar]
- 31. Loue S. Preventing HIV, eliminating disparities among Hispanics in the United States. J Immigr Minor Health. 2006;8(4):313-318. 10.1007/s10903-006-9001-2 [DOI] [PubMed] [Google Scholar]
- 32. Sullivan PS., Purcell DW., Grey JA. et al. Patterns of racial/ethnic disparities and prevalence in HIV and syphilis diagnoses among men who have sex with men, 2016: a novel data visualization. Am J Public Health. 2018;108(suppl 4):S266-S273. 10.2105/AJPH.2018.304762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Williams DR., Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood). 2005;24(2):325-334. 10.1377/hlthaff.24.2.325 [DOI] [PubMed] [Google Scholar]
- 34. Williams DR., Seth P., Walker T. et al. HIV testing and outcomes among Hispanics/Latinos—United States, Puerto Rico, and U.S. Virgin Islands, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(40):1099-1103. 10.15585/mmwr.mm6540a2 [DOI] [PubMed] [Google Scholar]
- 35. Essuon AD., Zhao H., Wang G., Collins N., Karch D., Rao S. HIV testing outcomes among Blacks or African Americans—50 local U.S. jurisdictions accounting for the majority of new HIV diagnoses and seven states with disproportionate occurrences of HIV in rural areas, 2017. MMWR Morb Mortal Wkly Rep. 2020;69(4):97-102. 10.15585/mmwr.mm6904a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Dailey AF., Johnson AS., Wu B. HIV care outcomes among Blacks with diagnosed HIV—United States, 2014. MMWR Morb Mortal Wkly Rep. 2017;66(4):97-103. 10.15585/mmwr.mm6604a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ibragimov U., Beane S., Adimora AA. et al. Relationship of racial residential segregation to newly diagnosed cases of HIV among Black heterosexuals in US metropolitan areas, 2008-2015. J Urban Health. 2019;96(6):856-867. 10.1007/s11524-018-0303-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Levison JH., Levinson JK., Alegría M. A critical review and commentary on the challenges in engaging HIV-infected Latinos in the continuum of HIV care. AIDS Behav. 2018;22(8):2500-2512. 10.1007/s10461-018-2187-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ohl ME., Perencevich E. Frequency of human immunodeficiency virus (HIV) testing in urban vs. rural areas of the United States: results from a nationally-representative sample. BMC Public Health. 2011;11(1): 10.1186/1471-2458-11-681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dolwick Grieb SM., Desir F., Flores-Miller A., Page K. Qualitative assessment of HIV prevention challenges and opportunities among Latino immigrant men in a new receiving city. J Immigr Minor Health. 2015;17(1):118-124. 10.1007/s10903-013-9932-3 [DOI] [PubMed] [Google Scholar]
- 41. Kaiser Family Foundation . Current status of Medicaid expansion decisions: interactive map. Published 2019. Accessed June 21, 2019. http://kff.org/health-reform/slide/current-status-of-the-medicaid-expansion-decision
- 42. Johnson S., Gold MR., Baciu A. Rethinking the leading health indicators for Healthy People 2030. JAMA Health Forum. Published May 20, 2020. Accessed February 5, 2021. https://jamanetwork.com/channels/health-forum/fullarticle/2766503 [DOI] [PubMed]
- 43. Centers for Disease Control and Prevention . Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2018. HIV Surveill Suppl Rep. 2020;25(2):1-104. [Google Scholar]