Abstract
Stigma changes over time: it waxes and wanes through history, is manifested within humans who develop over time and is tied to statuses (such as attributes, illnesses and identities) that have varying courses. Despite the inherent fluidity of stigma, theories, research and interventions typically treat associations between stigma and health as stagnant. Consequently, the literature provides little insight into when experiences of stigma are most harmful to health and when stigma interventions should be implemented. In this Perspective, we argue that integrating time into stigma research can accelerate progress towards understanding and intervening in associations between stigma and health inequities. We situate time in relation to key concepts in stigma research, identify three timescales that are relevant for understanding stigma (historical context, human development and status course), and outline a time-based research agenda to improve scientists’ ability to understand and address stigma to improve health.
Subject terms: Psychology, Interdisciplinary studies, Diseases
Associations between stigma and health are typically treated as stagnant. In this Perspective, Earnshaw et al. argue that considering stigma in relation to historical, human development and status course timescales can advance progress in understanding and addressing stigma to improve health.
Introduction
Stigma is a social process that involves distinguishing people based on social statuses (such as attributes, illnesses and identities) and socially devaluing, discrediting and excluding individuals with those statuses1. Many statuses are stigmatized today, including those associated with oppressed groups, such as women and minoritized ethnic groups; physical and mental illnesses, such as HIV and schizophrenia; and social norm violations, such as drug use and sexual and gender diverse identities1–3. Stigma undermines health by preventing access to critical health-promoting resources (such as healthcare and employment) and acting as a pernicious stressor that leads to harmful affective, cognitive, behavioural and physiological responses among individuals1. Thus, stigma is a fundamental cause of health inequities4, that is, health differences in which stigmatized groups experience worse health or greater health risks than non-stigmatized groups5.
Stigma changes over time. At the societal level, the magnitude of stigma associated with various statuses has waxed and waned over the course of history. For example, sexism and homophobia have generally decreased in the United States over the past century6–8. By contrast, xenophobia towards Latinx, Muslim and Asian individuals has resurged during the recent political climate9 and the COVID-19 pandemic10, and HIV and COVID-19 have ushered in fresh waves of health-related stigma11–14. At the individual level, the impact of stigma changes across human development, such that people are more vulnerable or more resilient to stigma at different stages of their lives. For example, there is evidence that sexual and gender diversity stigma might improve as sexually and gender diverse individuals transition from youth into adulthood15,16.
In addition to changes in the experience and outcomes of stigma, stigmatized statuses themselves evolve over time. Some of these statuses change in ways that place individuals at risk for more frequent or pronounced experiences of stigma, such as when an individual’s symptoms of muscular dystrophy worsen and become visible17. Other stigmatized statuses might change in ways that lead to less frequent or pronounced experiences of stigma, such as when an individual loses weight18. Despite the inherent fluidity of stigma, and recent calls from theorists working on racism19 and health disparities20 to better account for time in these areas of research, stigma scientists often do not consider the temporal context of their work.
In this Perspective, we argue that integrating time into stigma research can accelerate progress towards understanding and intervening in associations between stigma and health inequities. We situate time in relation to key questions in stigma research, identify three timescales that are particularly important for understanding stigma (historical context, human development and status course) and outline a time-based research agenda to understand and address stigma to improve health. Accounting for time in stigma research can yield key insights into how experiences of stigma evolve, how pathways linking stigma with health change and when individuals are most vulnerable or resilient to the effects of stigma. Moreover, accounting for time in stigma interventions can help psychologists determine when stigma interventions are most needed, identify appropriate intervention targets for specific times and consider which stigma reduction tools will be most effective at which times.
Key questions about stigma
Scientists researching stigma have been asking key questions that have yielded important insights into associations between stigma and health. In this section, we outline these questions and situate the concept of time within this literature.
What is stigma and why does stigma exist?
Stigma is a social process that emerges at the co-occurrence of labelling, stereotyping, separation, status loss and discrimination within a power context21. This social process is theorized to exist, in part, because it serves societal functions, including to perpetuate exploitation and domination of some groups of people (such as minoritized ethnic groups, or women), enforce conformity to social norms by shaming or questioning the morality of other groups (such as people who use drugs or those with diverse sexual and gender identities) and encourage avoidance of people impacted by illness (such as people living with HIV or schizophrenia)2. Intersectionality suggests that various forms of stigma intersect and interact (for example, Black women living with HIV experience unique forms of stigma shaped by their race, gender and HIV status)22,23.
Who enacts and experiences stigma?
At the individual level, stigma is enacted and experienced by both people without stigmatized statuses (who are sometimes called ‘stigmatizers’, actors or perpetrators) and people with stigmatized statuses (who are sometimes called the ‘stigmatized’ or targets). Stigma is perpetuated via prejudice (negative emotions and feelings towards a person based on group membership), stereotypes (group-based beliefs applied to individuals) and discrimination (unfair or unjust treatment of group members)24,25. These stigma manifestations can be experienced with intention and awareness as explicit bias or without intention and awareness as implicit bias26–28. Moreover, individuals can perceive stigma, or hold perceptions of the extent to which others in their community engage in prejudice, stereotypes and discrimination towards people with stigmatized statuses29. Perceived stigma can influence the extent to which individuals (especially children) endorse stigma towards people with stigmatized statuses30, as well as the extent to which individuals with stigmatized statuses internalize stigma31,32 — that is, the extent to which they endorse prejudice and stereotypes associated with their stigmatized status and apply them to the self (also known as self-stigma)29,33–35.
Individuals living with stigmatized statuses are exposed to both experienced stigma (discrimination from others in the past or present) and anticipated stigma (expectations of discrimination in the future)29,33. These experiences range from chronic and everyday stressors (microaggressions) to acute and significant events (macroaggressions)36–39. The impact of experienced and anticipated stigma depends on the source of these experiences, such that stigma from family, healthcare providers, employers and others plays different roles in health outcomes40–42. For example, stigma from family members can undermine health outcomes by leading to psychological distress whereas stigma from healthcare providers can undermine health outcomes by leading people to avoid accessing needed medical treatment40,43.
Where does stigma occur?
Social-structural contexts shape individuals’ experiences and outcomes of stigma. Structural stigma spans conditions, cultural norms and policies at the societal and institutional levels that constrain the opportunities and resources of individuals living with stigmatized statuses44. At a macro level, culture fundamentally shapes stigma processes given that values and priorities shape the ways and extent to which statuses are stigmatized45,46. Societal-level examples of structural stigma include racial residential segregation47,48, same-sex marriage bans49,50, HIV criminalization policies51 and the war on drugs52–54. Institutional-level examples include HIV disclosure policies within employment settings55, zero-tolerance drug use policies in workplace settings and housing agencies56, and the lack of gender-neutral bathrooms and locker rooms in schools57. At more micro levels, stigma is shaped by social networks (individuals report more stigma when their interaction partners also report more stigma)58 and manifests uniquely in various spaces, places and/or locations. For example, theorists working on spatial stigma note that racism manifests in high-poverty, urban areas characterized by racial residential segregation59. Given that stigma is socially constructed within specific contexts, individuals may experience more or less pronounced stigma as they move between contexts. For example, an individual might be racialized, or considered to be a member of a minoritized ethnic group, in one country but not in another60 and a pregnant person may experience stigma in the workplace but not at home61.
How does stigma impact health?
Stigma plays a role in the risk for, development of and/or worsening of many diseases including mental health conditions (such as depression36,62,63 and anxiety36), behavioural health conditions (such as substance use disorders (SUDs)63,64), infectious diseases (such as HIV63,65 and tuberculosis63) and non-communicable diseases (such as cardiovascular disease66,67 and epilepsy63). Longitudinal and population-based studies further suggest that greater stigma is associated with greater risk of mortality68–71.
Stigma erodes the health of people with stigmatized statuses via two primary mediating pathways33. First, stigma at the individual and structural levels limits access to health-promoting resources, such as housing, healthcare, education, income and food4. For example, anticipated stigma among people with mental and physical health conditions undermines healthcare initiation and access35,72–75, stereotypes endorsed by food retailers lead to decisions to not stock or promote healthy foods in low-income neighbourhoods76 and racial residential segregation is associated with racial disparities in education and housing quality, employment opportunities and healthcare access47. Second, stigma leads to affective, cognitive, behavioural and physiological responses that undermine health33,46,77. For example, experienced and anticipated stigma leads to stress, which has a pronounced impact on mental and physical health4,78,79. Moreover, behavioural responses to stigma include maladaptive health behaviours, such as substance use80 and increased food consumption67,81.
Several characteristics of stigmatized statuses may shape individuals’ experiences of stigma and the ways in which stigma impacts health33,82,83. For example, individuals with statuses that are concealable (or can be hidden from others, such as HIV status) sometimes delay help-seeking to avoid discovery84. Stigma associated with statuses that are controllable (or perceived to be under the influence of the individual, such as weight status) is perceived by members of the general public to be more justified than stigma associated with statuses that are not controllable (such as a genetic health condition), and thus stigma associated with controllable statuses is sometimes stronger and more harmful33. Additionally, individuals with statuses reflective of a collective identity (or a larger group with shared identity, such as the Deaf community) might have access to social support and other health-promoting resources that enhance their resilience to stigma33.
When does stigma occur?
Despite tackling the important questions related to stigma and health outlined above, research has focused less on the question of when stigma occurs. Asking when stigma occurs might lead to a more complete understanding of associations between stigma and health, including when experiences of stigma are most harmful to health and how pathways linking stigma with health change over time. Asking when stigma occurs might, additionally, lead to more effective solutions to intervene in stigma by informing when to deliver stigma intervention strategies, ultimately bringing society closer to health equity. Until a more complete understanding of stigma and health is developed and more effective strategies to eliminate stigma are developed, stigma will remain an intractable social problem extracting a costly toll on human health.
Time, stigma and health
Three timescales might be particularly relevant for understanding stigma and health: historical context, human development and stigma course. The choice of these timescales is inspired by bioecological systems theory, which emphasizes the interplay between proximal processes, context and historical time in human development85–87. In this section, we introduce each timescale and relevant theoretical frameworks.
Historical context
According to life course theory, human lives must be understood in relation to historical time because differences in birth year expose individuals to different historical contexts88. Individuals’ experiences of stigma are therefore fundamentally shaped by the historical context into which they are born. For example, a woman living in the United States in the nineteenth century likely experienced substantial structural-level sexism and overt macroaggressions: she could not own property, vote or work outside her home. She could be legally raped by her husband (or by her white slave owner if she was Black). A woman living in the United States in the twenty-first century experiences arguably less pronounced structural-level sexism given policy changes since the nineteenth century. However, she continues to experience harmful forms of structural sexism: she could earn lower wages at work than men, live in states with fewer women than men representatives in her legislature and lack access to abortion89. She could also continue to experience macroaggressions, such as sexual harassment, and microaggressions, such as not getting hired or receiving poor healthcare on the basis of her sex90.
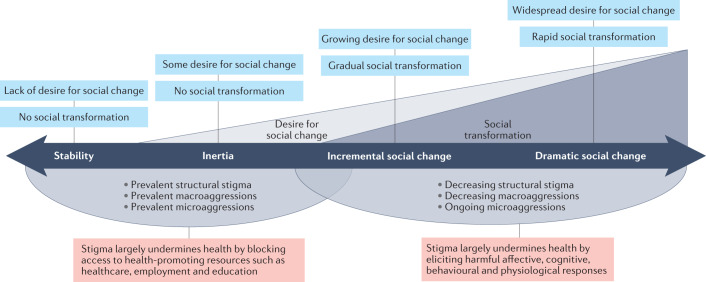
We hypothesize that stigma is continually being dismantled, maintained and/or created over time through social change processes. There are four contexts for social change that might shape experiences of stigma and individual-level outcomes, including health91 (Fig. 1). The contexts of stability and inertia are characterized by a lack of social change. In times of stability, there is a general lack of desire for social change and people are generally happy with the status quo. For example, few people currently call for an end to stigma towards sex offenders. In times of inertia, some members of society desire social change but not enough members desire change to initiate structural and/or individual-level transformation. For example, although Amnesty International has called for full decriminalization of consensual sex work92, widespread transformation of policies surrounding sex work and attitudes towards sex workers has arguably yet to occur.
Fig. 1. Stigma and historical context.
Societies move forwards and backwards through contexts of social change, represented by bidirectional arrow. Characteristics of each historical context described above timeline (blue). Ways in which individuals experience stigma and how stigma impacts health across historical contexts described below timeline (red). Figure assumes that stigma decreases over time, with times of stability associated with most stigma and times of dramatic social change associated with least stigma.
By contrast, contexts of incremental and dramatic social change are characterized by social transformation. In times of incremental social change, society evolves slowly and steadily in ways that do not threaten cultural identity. For example, there is currently slow evolution towards perceiving people with SUDs as people living with chronic health conditions rather than as criminals93, and stigmatizing policies such as the war on drugs are being increasingly critiqued as forms of stigmatization94,95. In times of dramatic social change, society evolves quickly and profoundly in ways that threaten cultural identity. For example, the Black Lives Matter movement is calling for dramatic systemic change to address racism and, in some places, ushering in structural changes96. Notably, contexts for social change are specific to individual stigmatized statuses. At one point in time within one society, there may be different contexts for social change related to sex offenders, sex workers, people with SUDs, Black people and people with other stigmatized statuses.
Research spanning generational statuses provides evidence that the historical context and the context of social change shape experiences and outcomes of stigma. For example, younger generations of Black Americans report experiencing a different form of racism, described as less overt yet still harsh, than older generations did97. Similarly, reductions in stigma associated with alcohol use disorders has resulted in younger generations initiating services for alcohol use disorders earlier than older generations98.
The pathways linking stigma with health outcomes might also evolve over time4. For example, as anti-discrimination laws that prohibit discrimination on the basis of stigmatized statuses are enacted, the primary mediating mechanism linking stigma with health might shift from overt discrimination preventing access to health-promoting resources, such as employment, housing and healthcare, to more subtle interpersonal experiences that result in stress4. Importantly, this change might be slow: even after anti-discrimination laws are enacted, more subtle and covert forms of interpersonal discrimination might continue to prevent access to health-promoting resources for some time.
The ways in which and extent to which stigma harms health are shaped by social change processes. Thus, differentiating between contexts for social change, including stability, inertia, and incremental and dramatic social change, is important for stigma and health research.
Human development
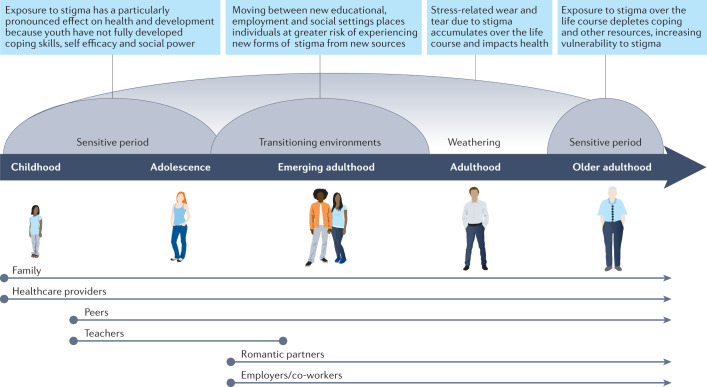
In addition to historical time, life course theory suggests that human lives must also be understood in relation to developmental processes and contexts88 (Fig. 2). As individuals age and transition between life stages and social environments, such as from school to work, sources of stigma and contexts in which stigma is experienced shift39,99. Life course theory suggests that properties of each life stage confer differential susceptibilities and resiliencies to stressors such as stigma20. Among children, stigma can take the form of bullying from peers on playgrounds100. As children age into adolescence, many begin experiencing more stigma from adults101, including discrimination from teachers and other adults in school settings102, shopkeepers and police103. Yet adolescents can be buffered from stigma by strong relationships with other adults such as parents and teachers104,105. Emerging adults experience significant transitions in social environments related to education, employment and interpersonal relationships106. These transitions might expose emerging adults to new forms of stigma from new sources, such as from college professors, employers and co-workers, and romantic partners. Yet emerging adults might also have greater ability to change where they live and work, and who they spend time with, than children and adolescents, allowing them to reduce their exposure to stigma in these contexts. Adults might experience more stigma from healthcare providers as they develop chronic diseases, bringing them into healthcare contexts more frequently107,108. As they age, older adults report increasing age discrimination109. Yet older adults have better emotion regulation abilities that protect them from the negative impacts of stigma110.
Fig. 2. Stigma and human development.
Vulnerabilities to stigma at each developmental period depicted above timeline (blue). Examples of sources of stigma across developmental stages depicted below timeline.
Evidence from developmental science indicates that the temporal context of adverse experiences during the life course has implications for both immediate and lasting health. Sensitive periods are developmental stages when social or environmental exposures can have especially pronounced effects on human development, and can be critical drivers of population-level health disparities20. We hypothesize that childhood and adolescence might be sensitive periods for stigma: although children and adolescents gain awareness of stigma as they develop metacognitive skills, or awareness of others’ thoughts and perceptions111, they have not fully developed coping capacity and skills, self-efficacy or social power112,113. They might therefore be more vulnerable to stigma than adults because they are less able to respond to stigma with resilience and resistance strategies. Moreover, adolescents undergoing identity versus role confusion, a stage when individuals grapple with questions of who they are and how they are similar to versus unique from others, might be more vulnerable to stigma114,115. Indeed, exposure to stigma early in life is associated with worse health outcomes than exposure later in life116.
Older age might be another sensitive period for stigma. According to the strength and vulnerability integration model110, older adults have accumulated psychological strengths such as emotion regulation abilities that are protective of their well-being. Yet older adults might also be more vulnerable to situations that elicit high levels of emotional arousal, and repeated exposure to stigma over the life course might deplete their coping resources over time, rendering them more vulnerable to stigma109. Additionally, older adults might be particularly vulnerable to several of the pathways whereby stigma undermines health, such as social isolation and less access to resources, as their social networks shrink and they become more dependent on others and social welfare systems110,117.
Finally, the weathering hypothesis suggests that stress-related wear and tear accumulates over the life course and results in substantial health inequities among stigmatized populations118,119. Thus, at the timescale of human development, associations between stigma and health might be influenced both by specific sensitive periods and by processes that unfold over the lifespan.
Status course
The sections above describe how experiences and outcomes of stigma can change over historical and developmental timescales. The status course timescale describes the extent to which stigmatized statuses can themselves change and evolve over time82. For example, individuals can develop or gain stigmatized statuses such as sexual and gender diverse identities, HIV, mental illnesses, weight and old age during their lifetime. Individuals can also lose stigmatized statuses, such as when they resolve a SUD, lose weight or transition from unemployed to employed. Additionally, associations between individuals’ identities and their stigmatized status can change over time, such as when individuals become aware that an aspect of the self, such as their gender or race, is stigmatized within society120.
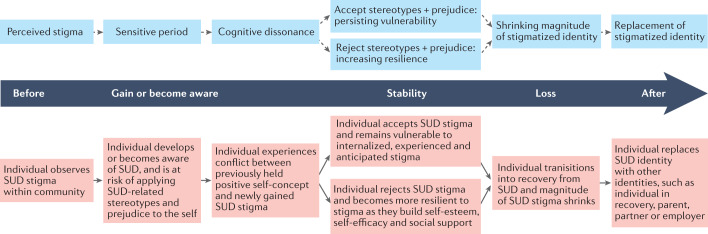
Experiences of stigma change alongside changes in stigmatized statuses31,32 and identities120,121 (Fig. 3). Modified labelling theory31 and the stage model of self-stigma32 suggest that individuals first develop perceived stigma, or an awareness that a particular status is stigmatized within society. Individuals who gain or become aware of a stigmatized status then begin the process of identity formation, involving self-discovery and exploration of their new identity122. They then enter a sensitive period during which they are at risk of applying the negative stereotypes and prejudice associated with the status to the self, thereby potentially rendering them vulnerable to internalized, experienced and anticipated stigma32. For example, longitudinal work suggests that internalized HIV and sexually transmitted infection stigma are particularly high immediately after an HIV or sexually transmitted infection diagnosis123,124. Individuals then move through a period of cognitive dissonance, during which conflict arises between their previously held positive self-concept and new internalized stigma125. For example, the self-perception of an individual who has gained weight that they are motivated and hard-working conflicts with the stereotype that people with obesity are lazy or weak-willed126.
Fig. 3. Stigma and status course.
Vulnerabilities to stigma across status course described above timeline (blue). Example of substance use disorder (SUD) stigma changing with status course described below timeline (red). Some individuals might not progress to next stage (dotted arrows).
Increasing dissonance might lead to existential crisis, which can be resolved by accepting or rejecting previously held stereotypes and prejudice125. If individuals accept stereotypes and prejudice, they remain vulnerable to internalized, experienced and anticipated stigma. If individuals reject stereotypes and prejudice, their internalized stigma decreases over time125. As internalized stigma decreases, individuals are able to accept their stigmatized status, integrate their new identity into their sense of self, and build self-esteem and self-efficacy120–122,127. These individuals can develop pride in their stigmatized status as they form social connections with others who share their status, and their identity associated with the status can become less central to their self-definition or balance with other identities121. Individuals can also become more resilient to stigma as they build self-esteem, self-efficacy and social support networks. For example, people in recovery from SUDs accumulate self-esteem128 and social support129 over time. This may explain why people in later stages of recovery report less psychological distress associated with experienced stigma than people in earlier stages130.
There has been less work on the process of losing a stigmatized status, perhaps because many stigmatized statuses (such as HIV) cannot be lost over time. Nevertheless, some common intrapersonal and interpersonal processes have been identified that facilitate transitions from a stigmatized status to a non-stigmatized status when stigmatized statuses are lost.
First, the identity theory of desistance131 and the Social Identity Model of Cessation Maintenance132 suggest that individuals begin to identify new ‘possible selves’, or ideas of what future versions of themselves might be, at the intrapersonal level as they lose stigmatized statuses. For example, people with SUDs begin to replace an existing stigmatized identity, such as ‘addict’, with a valued identity, such as ‘person in recovery’132. For some individuals, high levels of identification with the new possible selves or valued identities facilitates the process of evolving past the stigmatized identity132.
Second, engaging in behaviours that move them away from a stigmatized status might lead to less interpersonal reinforcement of that status18. For example, individuals experience less stigma from others as they lose weight, which provides social feedback that they are no longer viewed as members of a stigmatized group18.
Third, individuals’ identities as members of stigmatized groups become less salient (that is, thought about less frequently), and less central or important to self-definition, at the intrapersonal level as stigmatized statuses are reinforced less by others at the interpersonal level. Thus, the strength of identities associated with the stigmatized status might decrease133. The intrapersonal process of losing a stigmatized status might last years after the status is lost. Indeed, people continue to identify with a stigmatized status long after the status ceases to mark social interactions18. For example, some individuals who have lost weight continue to experience weight-related stigma18 and some individuals who have resolved a SUD continue to self-identify as ‘addicts’132.
Intersection of timescales
Changing stigmatized statuses are nested within developing humans, which are nested within evolving historical contexts. There is some precedence for studying intersecting timescales within stigma research, especially within the context of age–period–cohort effects which consider the intersections between historical context and human development99. However, to best understand how an individual will experience and be impacted by stigma, it is important to consider when they are experiencing stigma in relation to all three timescales.
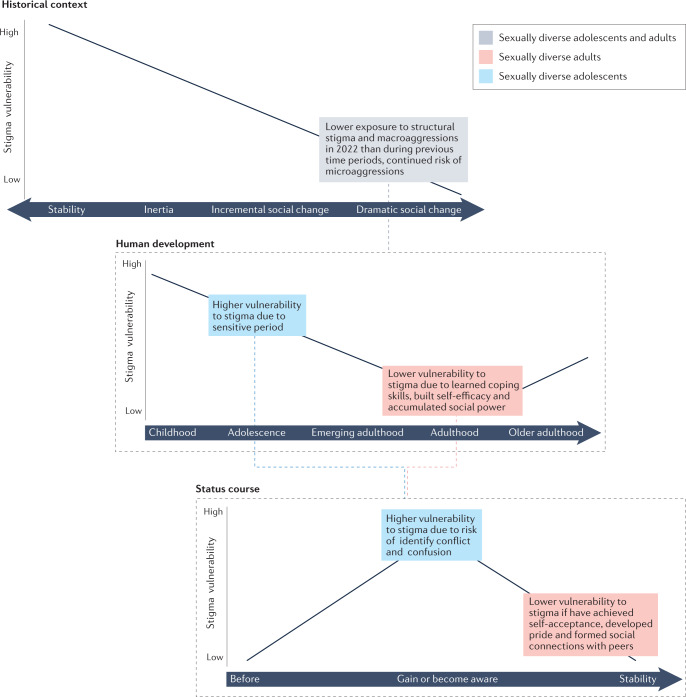
For example, consider sexually diverse adolescents living in the United States in 2022 (Fig. 4). Regarding the historical context, there is evidence that sexual diversity stigma is undergoing dramatic change in the United States. At the structural level, state Supreme Courts began finding bans on same-sex marriages unconstitutional in 2003 and the US Supreme Court ruled that all states must recognize same-sex marriage in 2015, thereby removing a pernicious form of structural stigma. The policy landscape surrounding sexual diversity rights continues to evolve8,134. Reflecting parallel changes at the individual level, the percentage of respondents to the General Social Survey who agreed that “homosexuals should have a right to marry” increased from 11% in 1990 to 68% in 2018 and that a “homosexual should be allowed to teach” rose from 65% to 88% during the same time period135. Considering only historical context, one might expect that sexually diverse adolescents are less harmed by stigma in the 2020s than they were in the 1990s.
Fig. 4. Intersecting timescales for sexually diverse adolescents and adults in 2022.
Status course timescale nested within developmental timescale, nested within historical context timescale. Stigma vulnerabilities among sexually diverse adolescents and adults (grey box), sexually diverse adolescents (blue boxes) and sexually diverse adults (red boxes). Magnitude of stigma vulnerabilities indicated at various time points (black lines).
However, despite benefiting from a historical context of decreasing stigma, sexually diverse adolescents continue to experience persistent health inequities111. This might be because their stage of development and status course continue to render adolescents vulnerable to stigma. Regarding human development, adolescence is a sensitive period for stigma because individuals are gaining awareness that others might hold prejudice towards and stereotypes about them, but have fewer coping and resilience resources to buffer them from experienced and anticipated stigma111. In addition, sexually diverse adolescents are often financially, legally and emotionally dependent on their families and have little control over their environments, such as which school they attend. It is possible that the same experiences of stigma that could be managed by changing a residence, friend group or workplace among adults cannot be addressed among adolescents who do not have full control of these aspects of their lives, thus making sexually diverse adolescents more vulnerable to stigma than sexually diverse adults.
Regarding the stigma course timescale, evidence suggests that youth first experience same-sex attraction around age 12 years, and realize and disclose their sexually diverse status around age 14 years (both of which are considerably younger ages than in older generations)111,136. Adolescents are, therefore, arguably in the early phases of stigmatized identity development, and might be experiencing identity conflict and confusion. This confers an additional layer of vulnerability to experiences of stigma. By contrast, sexually diverse adults might be more resilient to experiences of stigma given that they have had more time to reject stereotypes and prejudice associated with their stigmatized status32, as well as achieve self-acceptance, develop pride and form social connections with sexually diverse peers15.
Considering the example of sexually diverse adolescents illustrates the importance of integrating multiple timescales into stigma and health research. Although they live in a historical context characterized by dramatic social change, which should confer some protections from stigma, today’s sexually diverse adolescents remain vulnerable to stigma because of their stage of human development and status course (that is, their early stage of stigmatized identity development). Taking all three timescales into account is important for both understanding and intervening in associations between stigma and health among sexually diverse adolescents.
A time-based research agenda
Psychologists and other social scientists have achieved remarkable innovations over the past several decades in research methods for studying time137,138. Yet, according to meta-analyses, only a minority of studies focused on associations between stigma and health use longitudinal methods34,73,139,140. Moreover, decades of research have yielded a toolbox of evidence-based strategies to intervene and reduce stigma, such as through education, contact between people with and without stigmatized statuses, and policy change141–145. However, there has been little research on when these stigma reduction tools should be implemented to maximize their efficacy. In this section, we outline research questions that might lead to a better understanding of the role of time in associations between stigma and health inequities, and ways to leverage time to better intervene to reduce these associations (see Table 1).
Table 1.
Summary and comparison of timescales for stigma and health research
| Historical context | Human development | Stigma course | |
|---|---|---|---|
| Concept | The extent to which and ways in which statuses are stigmatized change over time; thus, the impact of stigma on health and processes linking stigma with health change over time | The ways in which individuals experience stigma and the extent to which stigma impacts health change across the lifespan | The ways in which individuals experience stigma and the extent to which stigma impacts health change in relation to the course of stigmatized statuses |
| Examples | Declines in sexual diversity stigma in the second half of the twentieth century and beginning of the twenty-first century | Childhood and adolescence are sensitive periods, when experiences of stigma have particularly profound effects on health and development | People living with HIV experience higher internalized stigma immediately following HIV diagnosis |
| Emergence of HIV-related stigma in the 1980s and COVID-19 stigma in the 2020s | According to the weathering hypothesis, older adults are vulnerable to the effects of accumulated stress due to stigma | Individuals who enter recovery from substance use disorders (SUDs) replace a stigmatized identity (‘addict’) with a valued identity (‘person in recovery’) | |
| Research questions | How do experiences of stigma differ within various historical contexts? | How do experiences of stigma evolve across the life course? | How do experiences of stigma change alongside the course of stigmatized statuses, including status gains and losses? |
| During which social change contexts is stigma most harmful to health? | At which developmental stages are individuals most vulnerable to the harmful effects of stigma on health? | As individuals gain and lose stigmatized statuses, when are they most vulnerable to the impacts of stigma? | |
| When and how do pathways linking stigma with health change over time? | For how long do experiences of stigma impact health? | ||
| Research methods | Multilevel methods | Life course histories | Mixture modelling |
| Longitudinal policy analysis | Longitudinal studies | Moderation analyses | |
| Integrative data analysis | |||
| Implications for interventions | During times when stigma is not changing at structural or individual levels, interventions that promote resilience to stigma among individuals with stigmatized statuses might be most effective | Deliver stigma interventions during stages of human development when individuals are most vulnerable to stigma | Address internalized stigma in the weeks and months following the development of a new stigmatized status |
| During times when stigma is changing at structural and/or individual levels, stigma reduction might be most effective | Stigma interventions delivered early in life might promote well-being later in life | Individuals might continue to be impacted by stigma even after they have lost a stigmatized status | |
| Intervention strategies should be leveraged to address the cumulative effects of experienced and anticipated stigma among people who have lived with stigmatized statuses for long periods of time |
Questions and methods
We propose three cross-cutting research questions that can be asked in relation to each timescale. First, research should investigate how experiences of stigma evolve over time. We hypothesize that the ways in which stigma manifests at the structural and individual levels might differ depending on the time period. For example, individuals might experience more macroaggressions during historical contexts of stability and more microaggressions during contexts of dramatic social change; they might experience stigma-based bullying from peers during childhood and hiring discrimination from employers during adulthood. Time-specific measures of stigma are available (for example, the Perceptions of Racism in Children and Youth scale is designed to measure race-based stigma among children and youth146), but more are needed to best capture unique experiences of stigma occurring at specific times. Additionally, the extent to which individuals experience stigma might change over time. For example, individuals might experience more stigma as they develop a SUD and less stigma as they enter into recovery. Growth curve modelling could be used to chart stigma manifestations prospectively over time.
Second, research should examine how the pathways linking stigma with health change over time. For example, we hypothesize that during younger developmental stages when individuals’ capacity for coping is still growing, experiences of stigma might have a strong impact on health via stress and maladaptive behavioural and psychological responses. At later developmental stages, stigma might have a more profound impact on health by undermining access to resources such as income and health insurance. Longitudinal studies that span the full life course are rare and challenging to conduct, particularly with hard-to-reach populations. Cohort sequential design147 and integrative data analysis148 offer methodological approaches for pooling data across multiple, independent samples to study individual development over time. Longitudinal mediation analyses can be used to explore pathways linking stigma with health during different time periods.
Last, scientists should determine when individuals are most vulnerable to the effects of stigma, and when they are most resilient. For example, the hopelessness theory of depression suggests that stressors are more likely to generate symptoms of hopelessness and depression when they are viewed as highly stable and global149. Thus, it is possible that experiences of stigma are more distressing during historical contexts of stability. To determine when experiences of stigma are most harmful in relation to the historical context, research methods that can characterize evolving historical contexts are needed. Longitudinal methods that quantify the rate of change at the structural level, such as via policy change, and the individual level, such as via attitude change, could help classify historical contexts. Multilevel models allow for the modelling of piecewise growth, which can allow scientists to estimate periods of both stability and social change. Moreover, novel methods that explore trends in people’s digital footprints, such as Google search terms and social media posts, could offer innovative strategies for characterizing current and changing historical contexts150–152. Multilevel methods can be used to study individual-level experiences of stigma in varying historical contexts. For example, research on age–period–cohort effects using multilevel modelling demonstrates that the health of Black Americans improved with the abolition of Jim Crow (state and local laws that enforced racial segregation in the Southern United States)153. We additionally hypothesize that individuals might be more vulnerable to stigma during sensitive periods, such as during childhood, adolescence and older adulthood as well as when they first gain a new stigmatized status. Longitudinal methods can be used to more precisely identify sensitive periods across human development and stigma course.
Implications for interventions
We additionally propose three cross-cutting implications for interventions in relation to each timescale. First, scientists conducting interventions should determine when stigma interventions are most needed. Although it is arguably always appropriate to attempt to intervene to reduce stigma and improve health, there might be times when stigma interventions are particularly needed because the impacts of stigma are especially harmful. For example, as noted above, childhood and adolescence might be sensitive periods during which stigma could have a particularly pronounced impact on health. Moreover, early exposures to stressors including stigma can have long-term impacts on health16,99. Thus, it might be particularly important to intervene at early ages to promote lifetime well-being. Stigma interventions for youth are becoming more numerous, yet remain small in number and unevenly distributed across stigmatized statuses, locations and social contexts100,154. Thus, there are sizeable gaps in existing interventions to address stigma during childhood and adolescence.
Second, scientists should consider appropriate intervention targets for specific times. It is possible that some intervention targets are more or less feasible during certain time periods. For example, resilience interventions are designed to reduce internalized stigma and inoculate individuals against the negative effects of stigma on health65,78. These interventions might be more effective than interventions that challenge dominant narratives during historical contexts of stability and inertia because they do not require change within structures or individuals without stigmatized statuses. By contrast, interventions that challenge dominant narratives that support stigma processes might be more feasible during contexts of incremental and dramatic social change when individuals might be more receptive to strategies that call stereotypes into question and promote social change155.
Last, we recommend evaluating which stigma reduction tools will be most effective at which times. For example, cognitive behavioural therapy and acceptance and commitment therapy, which have been shown to reduce internalized stigma and shame141,156, might be particularly important in the weeks and months following the gain of new stigmatized status when internalized stigma might be particularly high. Similarly, values affirmation interventions, which increase the salience and centrality of valued identities141, might accelerate progress towards identity synthesis and pride, and so might be most effective after individuals gain a new stigmatized status. Intervention strategies that bolster coping, reduce social isolation and/or facilitate access to resources might become increasingly important over the lifespan to buffer individuals from the cumulative effects of experienced and/or anticipated stigma from others. As individuals lose stigmatized statuses, values affirmation interventions could help individuals recognize new valued identities, such as person in recovery from a SUD, or focus on existing valued identities, such as mother, friend or volunteer, enabling lost stigmatized identities to decrease in importance. Interventions might additionally be needed to address the mental, physical, economic and other sequalae of stigma after stigmatized statuses are lost.
Conclusion
As a social process that waxes and wanes throughout history, is manifested within individuals who develop over time and is tied to statuses that have varying courses, stigma is constantly changing. However, theories, empirical approaches and intervention strategies generally treat stigma as static. We propose that better integrating time into stigma research will provide a more complete understanding of associations between stigma and health, and improve the ability to intervene to reduce stigma to promote health equity. Previous theorists have called on scientists to consider the three timescales of historical context91, human development19,99 or stigma course31,32,82,131. However, attending to timescales independently could yield incomplete understanding of individuals’ experiences and outcomes of stigma111. We therefore suggest considering these timescales simultaneously.
Longitudinal methods such as growth curve modelling, cohort sequential design and integrative data analysis are needed to best answer questions of how experiences of stigma and pathways linking stigma to health evolve over time, and when individuals are most vulnerable and resilient to the effects of stigma. New methods might be needed to study the intersection of all three timescales to enable insight into how changing stigmatized statuses within developing humans and evolving historical contexts shape experiences and outcomes of stigma.
Integrating time into stigma research and answering the questions outlined above have implications for interventions. Specifically, it will be important to determine when stigma interventions are most needed, consider appropriate intervention targets for specific times and evaluate which stigma reduction tools will be most effective at which times. Determining when to use which tools and when to replace tools that are no longer effective due to a changing temporal context are critical next steps in collective efforts to address stigma and promote health equity.
There are certainly additional timescales to be considered beyond those we have identified and discussed here. For example, research utilizing ecological momentary assessment and daily diaries has yielded important insights into stigma processes on a more granular temporal scale than the timescales we focused on here157,158. Moreover, we discussed stigma processes generally, across a wide range of stigmatized statuses and social-structural contexts. However, there are important ways in which stigmatized statuses are unique that might limit the generalizability of findings across stigmatized groups82,83. For example, the stigma-related processes involved in gaining and losing weight versus developing and resolving a SUD likely differ18,132. Similarly, associations between timescales, stigma processes and health outcomes likely differ across social-structural contexts given that stigma is socially constructed. Finally, we primarily focused on stigma processes experienced by individuals living with stigmatized statuses. This focus is guided by the goal of understanding when stigma will be most harmful to the health of individuals with stigmatized statuses, and when to intervene to protect and improve the health of individuals with stigmatized statuses. However, developmental intergroup theory30 and other theoretical and empirical work4,91 provide important insights into the interactions between time and stigma processes among individuals without stigmatized statuses. Considering time in various ways, and across a range of individuals and socio-cultural contexts, will accelerate the field’s ability to understand stigma and intervene to promote health equity.
Acknowledgements
This article was supported by the National Institutes of Health (NIH) under award numbers K01DA042881 (V.A.E.), K01DA047918 (R.J.W.) and T32MH074387 (N.M.B.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author contributions
All authors contributed to article conceptualization, the first author prepared the first draft, and all authors contributed to revising the manuscript.
Peer review
Peer review information
Nature Reviews Psychology thanks Paula Brochu, Sarah Whitton and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Major, B., Dovidio, J. F. & Link, B. G. The Oxford Handbook of Stigma, Discrimination, and Health (Oxford Univ. Press, 2018).
- 2.Phelan JC, Link BG, Dovidio JF. Stigma and prejudice: one animal or two? Soc. Sci. Med. 2008;67:358–367. doi: 10.1016/j.socscimed.2008.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benuto, L. T., Duckworth, M. P., Masuda, A. & O’Donohue, W. Prejudice, Stigma, Privilege, and Oppression: A Behavioral Health Handbook (Springer Nature, 2020).
- 4.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am. J. Public Health. 2013;103:813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braveman P. Health disparities and health equity: concepts and measurement. Annu. Rev. Public Health. 2006;27:167–194. doi: 10.1146/annurev.publhealth.27.021405.102103. [DOI] [PubMed] [Google Scholar]
- 6.Baunach DM. Decomposing trends in attitudes toward gay marriage, 1988–2006. Soc. Sci. Q. 2011;92:346–363. doi: 10.1111/j.1540-6237.2011.00772.x. [DOI] [PubMed] [Google Scholar]
- 7.Bolzendahl CI, Myers DJ. Feminist attitudes and support for gender equality: opinion change in women and men, 1974–1998. Soc. Forces. 1998;83:759–790. doi: 10.1353/sof.2005.0005. [DOI] [Google Scholar]
- 8.Angelo, P. J. & Bocci, D. The changing landscape of global LGBTQ+ rights. Council on Foreign Relationshttps://www.cfr.org/article/changing-landscape-global-lgbtq-rights (2021).
- 9.Lee, E. America for Americans (Basic Books, 2019).
- 10.Reny TT, Barreto MA. Xenophobia in the time of pandemic: othering, anti-Asian attitudes, and COVID-19. Polit. Groups Identities. 2020 doi: 10.1080/21565503.2020.1769693. [DOI] [Google Scholar]
- 11.Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect. Dis. 2020;20:782. doi: 10.1016/S1473-3099(20)30498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herek GM, Capitanio JP. Public reactions to AIDS in the United States: a second decade of stigma. Am. J. Public. Health. 1993;83:574–577. doi: 10.2105/AJPH.83.4.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991–1999. Am. J. Public Health. 2002;92:371–377. doi: 10.2105/AJPH.92.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Logie CH, Turan JM. How do we balance tensions between COVID‑19 public health responses and stigma mitigation? Learning from HIV research. AIDS Behav. 2020;24:2003–2006. doi: 10.1007/s10461-020-02856-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asakura K, Craig SL. ‘It gets better’ … but how? Exploring resilience development in the accounts of LGBTQ adults. J. Hum. Behav. Soc. Environ. 2014;24:253–266. doi: 10.1080/10911359.2013.808971. [DOI] [Google Scholar]
- 16.Birkett M, Newcomb ME, Mustanski B. Does it get better? A longitudinal analysis of psychological distress and victimization in lesbian, gay, bisexual, transgender, and questioning youth. J. Adolesc. Heal. 2015;56:280–285. doi: 10.1016/j.jadohealth.2014.10.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boström K, Ahlström G. Living with a chronic deteriorating disease: the trajectory with muscular dystrophy over ten years. Disabil. Rehabil. 2009;26:1388–1398. doi: 10.1080/0963-8280400000898. [DOI] [PubMed] [Google Scholar]
- 18.Granberg EM. “Now my ‘old self’ is thin”: stigma exits after weight loss. Soc. Psychol. Q. 2011;74:29–52. doi: 10.1177/0190272511398020. [DOI] [Google Scholar]
- 19.Gee GC, Hing A, Mohammed S, Tabor DC, Williams DR. Racism and the life course: taking time seriously. Am. J. Public. Health. 2019;109:43–47. doi: 10.2105/AJPH.2018.304766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jones NL, et al. Life course approaches to the causes of health disparities. Am. J. Public. Health. 2019;109:48–55. doi: 10.2105/AJPH.2018.304738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Link BG, Phelan JC. Conceptualizing stigma. Annu. Rev. Sociol. 2001;27:363–385. doi: 10.1146/annurev.soc.27.1.363. [DOI] [Google Scholar]
- 22.Berger, M. T. Workable Sisterhood: The Political Journey of Stigmatized Women with HIV/AIDS (Princeton Univ. Press, 2004).
- 23.Jackson-Best F, Edwards N. Stigma and intersectionality: a systematic review of systematic reviews across HIV/AIDS, mental illness, and physical disability. BMC Public Health. 2018;18:919. doi: 10.1186/s12889-018-5861-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Corrigan, P. W., Bink, A. B. & Schmidt, A. in Oxford Handbook of Stigma, Discrimination, and Health (eds Major, B., Dovidio, J. F. & Link, B. G.) 413–428 (Oxford Univ. Press, 2018).
- 25.Brewer, M. B. in Social Psychology: Handbook of Basic Principles (eds. Kruglanski A. W. & Higgins, E. T.) 695–715 (Guilford Press, 2007).
- 26.Dovidio, J. & Gaertner, S. in Advances in Experimental Social Psychology Vol. 36 (ed. Zanna, M. P.) 1–52 (Elsevier, 2004).
- 27.Phelan JC, et al. A comparison of status and stigma processes: explicit and implicit appraisals of “mentally ill people” and “uneducated people”. Stigma Heal. 2019;4:213–224. doi: 10.1037/sah0000106. [DOI] [Google Scholar]
- 28.Ashford RD, Brown AM, McDaniel J, Curtis B. Biased labels: an experimental study of language and stigma among individuals in recovery and health professionals. Subst. Use Misuse. 2019;54:1376–1384. doi: 10.1080/10826084.2019.1581221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fox AB, Earnshaw VA, Taverna EC, Vogt D. Conceptualizing and measuring mental illness stigma: the Mental Illness Stigma Framework and critical review of measures. Stigma Heal. 2018;3:348–376. doi: 10.1037/sah0000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bigler RS, Liben LS. Developmental intergroup theory: explaining and reducing children’s social stereotyping and prejudice. Curr. Dir. Psychol. Sci. 2007;16:162–166. doi: 10.1111/j.1467-8721.2007.00496.x. [DOI] [Google Scholar]
- 31.Link BG, et al. A modified labeling theory approach to mental disorders: an empirical assessment. Am. Sociol. Rev. 1989;54:400–423. doi: 10.2307/2095613. [DOI] [Google Scholar]
- 32.Corrigan PW, Rao D. On the self-stigma of mental illness: stages, disclosure, and strategies for change. Can. J. Psychiatry. 2012;57:464–469. doi: 10.1177/070674371205700804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Major, B., Dovidio, J. F., Link, B. G. & Calabrese, S. K. in The Oxford Handbook of Stigma, Discrimination, and Health (eds Major, B., Dovidio, J. F. & Link, B. G.) 3–29 (Oxford Univ. Press, 2018).
- 34.Del Rosal E, González-Sanguino C, Bestea S, Boyd J, Muñoz M. Correlates and consequences of internalized stigma assessed through the Internalized Stigma of Mental Illness Scale for people living with mental illness: a scoping review and meta-analysis from 2010. Stigma Heal. 2021;6:324–334. doi: 10.1037/sah0000267. [DOI] [Google Scholar]
- 35.Hammarlund R, Crapanzano K, Luce L, Mulligan L, Ward K. Review of the effects of self-stigma and perceived social stigma on the treatment-seeking decisions of individuals with drug- and alcohol-use disorders. Subst. Abuse Rehabil. 2018;9:115–136. doi: 10.2147/SAR.S183256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am. J. Public Health. 2003;93:200–208. doi: 10.2105/AJPH.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Olkin R, Hayward H, Abbene MS, VanHeel G. The experiences of microaggressions against women with visible and invisible disabilities. J. Soc. Issues. 2019;75:757–785. doi: 10.1111/josi.12342. [DOI] [Google Scholar]
- 38.Eaton LA, et al. HIV microaggressions: a novel measure of stigma-related experiences among people living with HIV. J. Behav. Med. 2020;43:34–43. doi: 10.1007/s10865-019-00064-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Compton-Lilly C. Microaggressions and macroaggressions across time: the longitudinal construction of inequality in schools. Urban. Educ. 2020;55:1315–1349. doi: 10.1177/0042085919893751. [DOI] [Google Scholar]
- 40.Earnshaw V, Smith L, Copenhaver M. Drug addiction in the context of methadone maintenance therapy: an investigation into understudied sources of stigma. Int. J. Ment. Health Addict. 2013;11:110–122. doi: 10.1007/s11469-012-9402-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rice WS, et al. A mixed methods study of anticipated and experienced stigma in health care settings among women living with HIV in the United States. AIDS Patient Care STDs. 2019;33:184–195. doi: 10.1089/apc.2018.0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kalichman SC, Katner H, Banas E, Hill M, Kalichman MO. Cumulative effects of stigma experiences on retention in HIV care among men and women in the rural Southeastern United States. AIDS Patient Care STDs. 2020;34:484–490. doi: 10.1089/apc.2020.0144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Earnshaw VA, Quinn DM, Park CL. Anticipated stigma and quality of life among people living with chronic illnesses. Chronic Illn. 2012;8:79–88. doi: 10.1177/1742395311429393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hatzenbuehler ML, Link BG. Introduction to the special issue on structural stigma and health. Soc. Sci. Med. 2014;103:1–6. doi: 10.1016/j.socscimed.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 45.Yang LH, et al. Culture and stigma: adding moral experience to stigma theory. Soc. Sci. Med. 2007;64:1524–1535. doi: 10.1016/j.socscimed.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 46.Misra S, et al. Systematic review of cultural aspects of stigma and mental illness among racial and ethnic minority groups in the United States: implications for interventions. Am. J. Community Psychol. 2021 doi: 10.1002/ajcp.12516. [DOI] [PubMed] [Google Scholar]
- 47.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404–416. doi: 10.1016/S0033-3549(04)50068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bluthenthal RN. Structural racism and violence as social determinants of health: conceptual, methodological and intervention challenges. Drug Alcohol Depend. 2021 doi: 10.1016/j.drugalcdep.2021.108681. [DOI] [PubMed] [Google Scholar]
- 49.Pachankis JE, Bränström R. Hidden from happiness: structural stigma, sexual orientation concealment, and life satisfaction across 28 countries. J. Consult. Clin. Psychol. 2018;86:403–415. doi: 10.1037/ccp0000299. [DOI] [PubMed] [Google Scholar]
- 50.Hatzenbuehler ML. Structural stigma: research evidence and implications for psychological science. Am. Psychol. 2016;71:742–751. doi: 10.1037/amp0000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tran NK, Hatzenbuehler ML, Goldstein ND. Potential relationship between HIV criminalization and structural stigma related to sexual orientation in the United States. J. Acquir. Immune Defic. Syndr. 2019;80:106–108. doi: 10.1097/QAI.0000000000001961. [DOI] [PubMed] [Google Scholar]
- 52.Watson RJ, Eaton LA, Maksut JL, Rucinski KB, Earnshaw VA. Links between sexual orientation and disclosure among Black MSM: sexual orientation and disclosure matter for PrEP awareness. AIDS Behav. 2020;24:39–44. doi: 10.1007/s10461-019-02696-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.El-Bassel N, Shoptaw S, Goodman-Meza D, Ono H. Addressing long overdue social and structural determinants of the opioid epidemic. Drug Alcohol. Depend. 2021;222:108679. doi: 10.1016/j.drugalcdep.2021.108679. [DOI] [PubMed] [Google Scholar]
- 54.Bolster-Foucault C, Fane BHM, Blair A. Structural determinants of stigma across health and social conditions: a rapid review and conceptual framework to guide future research and intervention. Heal. Promot. Chronic Dis. Prev. Can. 2021;41:85–115. doi: 10.24095/hpcdp.41.3.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sprague L, Simon S, Sprague C. Employment discrimination and HIV stigma: survey results from civil society organisations and people living with HIV in Africa. Af. J. AIDS Res. 2011;10:311–324. doi: 10.2989/16085906.2011.637730. [DOI] [PubMed] [Google Scholar]
- 56.Lopez, K. & Reid, D. Discrimination against patients with substance use disorders remains prevalent and harmful: the case for 42 CFR part 2. Health Aff.https://www.healthaffairs.org/do/10.1377/hblog20170413.059618/full/ (2020).
- 57.Earnshaw VA, et al. LGBTQ bullying: translating research to action in pediatrics. Pediatrics. 2017;140:e20170432. doi: 10.1542/peds.2017-0432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Takada S, et al. The social network context of HIV stigma: population-based, sociocentric network study in rural Uganda. Soc. Sci. Med. 2019;233:229–236. doi: 10.1016/j.socscimed.2019.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Keene DE, Padilla MB. Spatial stigma and health inequality. Crit. Public Health. 2014;24:392–404. doi: 10.1080/09581596.2013.873532. [DOI] [Google Scholar]
- 60.LaVeist TA. Beyond dummy variables and sample selection: what health services researchers ought to know about race as a variable. Health Serv. Res. 1994;29:1–16. [PMC free article] [PubMed] [Google Scholar]
- 61.Fox AB, Quinn DM. Pregnant women at work: the role of stigma in predicting women’s intended exit from the workforce. Psychol. Women Q. 2015;39:226–242. doi: 10.1177/0361684314552653. [DOI] [Google Scholar]
- 62.Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc. Sci. Med. 2010;71:2150–2161. doi: 10.1016/j.socscimed.2010.09.030. [DOI] [PubMed] [Google Scholar]
- 63.Kane JC, et al. A scoping review of health-related stigma outcomes for high-burden diseases in low- and middle-income countries. BMC Med. 2019;17:1–40. doi: 10.1186/s12916-019-1250-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Earnshaw VA. Stigma and substance use disorders: a clinical, research, and advocacy agenda. Am. Psychol. 2020;75:1300–1311. doi: 10.1037/amp0000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am. Psychol. 2013;68:225–236. doi: 10.1037/a0032705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Panza GA, et al. Links between discrimination and cardiovascular health among socially stigmatized groups: a systematic review. PLoS ONE. 2019;14:1–27. doi: 10.1371/journal.pone.0217623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Puhl R, Suh Y. Health consequences of weight stigma: implications for obesity prevention and treatment. Curr. Obes. Rep. 2015;4:182–190. doi: 10.1007/s13679-015-0153-z. [DOI] [PubMed] [Google Scholar]
- 68.Farmer HR, Wray LA, Thomas JR. Do race and everyday discrimination predict mortality risk? Evidence from the Health and Retirement Study. Gerontol. Geriatr. Med. 2019;5:233372141985566. doi: 10.1177/2333721419855665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nystedt TA, Rosvall M, Lindström M. The association of self-reported discrimination to all-cause mortality: a population-based prospective cohort study. SSM Popul. Heal. 2019;7:100360. doi: 10.1016/j.ssmph.2019.100360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hatzenbuehler ML, Rutherford C, McKetta S, Prins SJ, Keyes KM. Structural stigma and all-cause mortality among sexual minorities: differences by sexual behavior? Soc. Sci. Med. 2020;244:112463. doi: 10.1016/j.socscimed.2019.112463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kashyap R, Behrman J. Gender discrimination and excess female under-5 mortality in India: a new perspective using mixed-sex twins. Demography. 2020;57:2143–2167. doi: 10.1007/s13524-020-00909-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Earnshaw VA, et al. Internalized HIV stigma, ART initiation and HIV-1 RNA suppression in South Africa: exploring avoidant coping as a longitudinal mediator. J. Int. AIDS Soc. 2018;21:e25198. doi: 10.1002/jia2.25198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Katz IT, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J. Int. AIDS Soc. 2013;16:18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schnyder N, Panczak R, Groth N, Schultze-Lutter F. Association between mental health-related stigma and active help-seeking: systematic review and meta-analysis. Br. J. Psychiatry. 2017;210:261–268. doi: 10.1192/bjp.bp.116.189464. [DOI] [PubMed] [Google Scholar]
- 75.Babel RA, Wang P, Alessi EJ, Raymond HF, Wei C. Stigma, HIV risk, and access to HIV prevention and treatment services among men who have sex with men (MSM) in the United States: a scoping review. AIDS Behav. 2021;25:3574–3604. doi: 10.1007/s10461-021-03262-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Earnshaw VA, Karpyn A. Understanding stigma and food inequity: a conceptual framework to inform research, intervention, and policy. Transl. Behav. Med. 2020;10:1350–1357. doi: 10.1093/tbm/ibaa087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Earnshaw VA, et al. HIV stigma, depressive symptoms, and substance use. AIDS Patient Care STDs. 2020;34:275–280. doi: 10.1089/apc.2020.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Meyer IH. Identity, stress, and resilience in lesbians, gay men, and bisexuals of color. Couns. Psychol. 2010;38:442–454. doi: 10.1177/0011000009351601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rüsch N, et al. A stress-coping model of mental illness stigma: I. Predictors of cognitive stress appraisal. Schizophr. Res. 2009;110:59–64. doi: 10.1016/j.schres.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.English D, Rendina HJ, Parsons JT. The effects of intersecting stigma: a longitudinal examination of minority stress, mental health, and substance use among Black, Latino, and multiracial gay and bisexual men. Psych. Viol. 2018;8:669–679. doi: 10.1037/vio0000218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Puhl RM, et al. Internalization of weight bias: implications for binge eating and emotional well-being. Obesity. 2007;15:19–23. doi: 10.1038/oby.2007.521. [DOI] [PubMed] [Google Scholar]
- 82.Jones, E. E., Farina, A., Hastorf, A. H., Markus, H. & Scott, R. A. Social Stigma: The Psychology of Marked Relationships (W. H. Freeman, 1984).
- 83.Pachankis JE, et al. The burden of stigma on health and well-being: a taxonomy of concealment, course, disruptiveness, aesthetics, origin, and peril across 93 stigmas. Personal Soc. Psychol. Bull. 2018;44:451–474. doi: 10.1177/0146167217741313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Quinn, D. M. in The Oxford Handbook of Stigma, Discrimination, and Health (eds Major, B., Dovidio., J. F. & Link, B. G.) 287–299 (Oxford Univ. Press, 2018).
- 85.Bronfenbrenner, U. The Ecology of Human Development: Experiments by Nature and Design Vol. 148 (Harvard Univ. Press, 1979).
- 86.Bronfenbrenner U, Ceci SJ. Nature-nurture reconceptualized in developmental perspective: a bioecological model. Psychol. Rev. 1994;101:568–586. doi: 10.1037/0033-295X.101.4.568. [DOI] [PubMed] [Google Scholar]
- 87.Rosa EM, Tudge J. Urie Bronfenbrenner’s theory of human development: its evolution from ecology to bioecology. J. Fam. Theory Rev. 2013;5:243–258. doi: 10.1111/jftr.12022. [DOI] [Google Scholar]
- 88.Elder GH. Time, human agency, and social change: perspectives on the life course. Soc. Psychol. Q. 1994;57:4–15. doi: 10.2307/2786971. [DOI] [Google Scholar]
- 89.Homan P. Structural sexism and health in the United States: a new perspective on health inequality and the gender system. Am. Sociol. Rev. 2019;84:486–516. doi: 10.1177/0003122419848723. [DOI] [Google Scholar]
- 90.Lewis, J. A. in APA Handbook of the Psychology of Women: History, Theory, and Battlegrounds (eds Travis, C. B. & White, J. W.) 381–397 (American Psychological Association, 2018).
- 91.de la Sablonnière R. Toward a psychology of social change: a typology of social change. Front. Psychol. 2017;8:1–20. doi: 10.3389/fpsyg.2017.00397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Amnesty International. Global movement votes to adopt policy to protect human rights of sex workers. Amnesty Internationalhttps://www.amnesty.org/en/latest/news/2015/08/global-movement-votes-to-adopt-policy-to-protect-human-rights-of-sex-workers (2015).
- 93.Arria AM, Mclellan AT. Evolution of concept, but not action, in addiction treatment. Subst. Use Misuse. 2012;47:1041–1048. doi: 10.3109/10826084.2012.663273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.United Nations Office on Drugs and Crime. 2008 World Drug Report. UNODChttps://www.unodc.org/documents/wdr/WDR_2008/WDR_2008_eng_web.pdf (2008).
- 95.Lewis J, Earp BD. Pathways to drug liberalization: racial justice, public health, and human rights. Am. J. Bioeth. 2021 doi: 10.1080/15265161.2021.1940370. [DOI] [PubMed] [Google Scholar]
- 96.Levin, S. What does ‘defund the police’ mean? The rallying cry sweeping the US explained. The Guardianhttps://www.theguardian.com/us-news/2020/jun/05/defunding-the-police-us-what-does-it-mean (2020).
- 97.Brown KD. Race as a durable and shifting idea: how Black millennial preservice teachers understand race, racism, and teaching. Peabody J. Educ. 2018;93:106–120. doi: 10.1080/0161956X.2017.1403183. [DOI] [Google Scholar]
- 98.Bourdon JL, et al. Characterization of service use for alcohol problems across generations and sex in adults with alcohol use disorder. Alcohol. Clin. Exp. Res. 2020;44:746–757. doi: 10.1111/acer.14290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Gee GC, Walsemann KM, Brondolo E. A life course perspective on how racism may be related to health inequities. Am. J. Public Health. 2012;102:967–974. doi: 10.2105/AJPH.2012.300666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Earnshaw VA, et al. Stigma-based bullying interventions: a systematic review. Dev. Rev. 2018;48:178–200. doi: 10.1016/j.dr.2018.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Greene ML, Way N, Pahl K. Trajectories of perceived adult and peer discrimination among Black, Latino, and Asian American adolescents: patterns and psychological correlates. Dev. Psychol. 2006;42:218–236. doi: 10.1037/0012-1649.42.2.218. [DOI] [PubMed] [Google Scholar]
- 102.Farkas G. Racial disparities and discrimination in education: what do we know, how do we know it, and what do we need to know? Teach. Coll. Rec. 2003;105:1119–1146. doi: 10.1111/1467-9620.00279. [DOI] [Google Scholar]
- 103.Rosenbloom SR, Way N. Experiences of discrimination among African American, Asian American, and Latino adolescents in an urban high school. Youth Soc. 2004;35:420–451. doi: 10.1177/0044118X03261479. [DOI] [Google Scholar]
- 104.Gibbons FX, et al. Exploring the link between racial discrimination and substance use: what mediates? What buffers? J. Pers. Soc. Psychol. 2010;99:785–801. doi: 10.1037/a0019880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Earnshaw VA, et al. Teacher involvement as a protective factor from the association between race-based bullying and smoking initiation. Soc. Psychol. Educ. 2014;17:197–209. doi: 10.1007/s11218-014-9250-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. Am. Psychol. 2000;55:469–480. doi: 10.1037/0003-066X.55.5.469. [DOI] [PubMed] [Google Scholar]
- 107.Earnshaw VA, Quinn DM. The impact of stigma in healthcare on people living with chronic illnesses. J. Health Psychol. 2012;17:157–168. doi: 10.1177/1359105311414952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Emlet CA. “You’re awfully old to have this disease”: experiences of stigma and ageism in adults 50 years and older living with HIV/AIDS. Gerontologist. 2006;46:781–790. doi: 10.1093/geront/46.6.781. [DOI] [PubMed] [Google Scholar]
- 109.Marchiondo LA, Gonzales E, Williams LJ. Trajectories of perceived workplace age discrimination and long-term associations with mental, self-rated, and occupational health. J. Gerontol. Soc. Sci. 2019;74:655–663. doi: 10.1093/geronb/gbx095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Charles ST. Strength and vulnerability integration: a model of emotional well-being across adulthood. Psychol. Bull. 2010;136:1068–1091. doi: 10.1037/a0021232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Russell ST, Fish JN. Sexual minority youth, social change, and health: a developmental collision. Res. Hum. Dev. 2019;16:5–20. doi: 10.1080/15427609.2018.1537772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zimmer-Gembeck MJ, Skinner EA. The development of coping across childhood and adolescence: an integrative review and critique of research. Int. J. Behav. Dev. 2011;35:1–17. doi: 10.1177/0165025410384923. [DOI] [Google Scholar]
- 113.Vasquez-Tokos J, Norton-Smith K. Talking back to controlling images: Latinos’ changing responses to racism over the life course. Ethn. Racial Stud. 2017;40:912–930. doi: 10.1080/01419870.2016.1201583. [DOI] [Google Scholar]
- 114.Erikson, E. H. Childhood and Society (Norton, 1963).
- 115.Erikson, E. H. Identity: Youth and Crisis (Norton, 1968).
- 116.Cuevas AG, et al. Developmental timing of initial racial discrimination exposure is associated with cardiovascular health conditions in adulthood. Ethn. Health. 2020;63:1–14. doi: 10.1080/13557858.2019.1613517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lu P, Shelley M, Liu Y-L. Re-examining the poverty cycle in middle and late adulthood: evidence from the Health and Retirement Study 2002–2014. Int. J. Soc. Welf. 2020;30:140–151. doi: 10.1111/ijsw.12454. [DOI] [Google Scholar]
- 118.Geronimus AT, Hicken M, Keene D, Bound J. ‘Weathering’ and age patterns of allostatic load scores among blacks and whites in the United States. Am. J. Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Forde AT, Crookes DM, Suglia SF, Demmer RT. The weathering hypothesis as an explanation for racial disparities in health: a systematic review. Ann. Epidemiol. 2019;33:1–18.e3. doi: 10.1016/j.annepidem.2019.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Worrell FC, Cross WE, Vandiver BJ. Nigrescence theory: current status and challenges for the future. J. Multicult. Couns. Devel. 2001;29:201–213. doi: 10.1002/j.2161-1912.2001.tb00517.x. [DOI] [Google Scholar]
- 121.Cass VC. Homosexual identity formation: a theoretical model. J. Homosex. 1984;20:143–167. doi: 10.1300/J082v04n03_01. [DOI] [PubMed] [Google Scholar]
- 122.Rosario M, Schrimshaw EW, Hunter J. Different patterns of sexual identity development over time: Implications for the psychological adjustment of lesbian, gay, and bisexual youths. J. Sex. Res. 2011;48:3–15. doi: 10.1080/00224490903331067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Eaton LA, et al. Experiences of stigma and health care engagement among Black MSM newly diagnosed with HIV/STI. J. Behav. Med. 2018;41:458–466. doi: 10.1007/s10865-018-9922-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chan BT, et al. Trajectories of HIV-related internalized stigma and disclosure concerns among ART initiators and noninitiators in South Africa. Stigma Heal. 2019;4:433–441. doi: 10.1037/sah0000159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Martz E. A philosophical perspective to confront disability stigmatization and promote adaptation to disability. J. Loss Trauma. 2004;9:139–158. doi: 10.1080/15325020490423343. [DOI] [Google Scholar]
- 126.Tomiyama AJ, et al. How and why weight stigma drives the obesity ‘epidemic’ and harms health. BMC Med. 2018;16:1–6. doi: 10.1186/s12916-018-1116-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Romero AJ, Edwards LM, Fryberg SA, Orduña M. Resilience to discrimination stress across ethnic identity stages of development. J. Appl. Soc. Psychol. 2014;44:1–11. doi: 10.1111/jasp.12192. [DOI] [Google Scholar]
- 128.Kelly JF, Greene MC, Bergman BG. Beyond abstinence: changes in indices of quality of life with time in recovery in a nationally representative sample of U.S. adults. Alcohol. Clin. Exp. Res. 2018;42:770–780. doi: 10.1111/acer.13604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kelly JF, Stout RL, Magill M, Tonigan JS. The role of Alcoholics Anonymous in mobilizing adaptive social network changes: a prospective lagged mediational analysis. Drug Alcohol Depend. 2011;114:119–126. doi: 10.1016/j.drugalcdep.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Vilsaint CL, Hoffman LA, Kelly JF. Perceived discrimination in addiction recovery: assessing the prevalence, nature, and correlates using a novel measure in a U.S. national sample. Drug Alcohol Depend. 2020;206:107667. doi: 10.1016/j.drugalcdep.2019.107667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Paternoster R, Bushway S. Desistance and the ‘feared self’: toward an identity theory of criminal desistance. J. Crim. Law Criminol. 2009;99:1103–1156. [Google Scholar]
- 132.Frings D, Albery IP. The Social Identity Model of Cessation Maintenance: formulation and initial evidence. Addict. Behav. 2015;44:35–42. doi: 10.1016/j.addbeh.2014.10.023. [DOI] [PubMed] [Google Scholar]
- 133.Quinn DM, Earnshaw VA. Understanding concealable stigmatized identities: the role of identity in psychological, physical, and behavioral outcomes. Soc. Issues Policy Rev. 2011;5:160–190. doi: 10.1111/j.1751-2409.2011.01029.x. [DOI] [Google Scholar]
- 134.Valenti A. LGBT employment rights in an evolving legal landscape: the impact of the Supreme Court’s decision in Bostock v. Clayton County, Georgia. Empl. Responsib. Rights J. 2021;33:3–23. doi: 10.1007/s10672-020-09359-7. [DOI] [Google Scholar]
- 135.Smith, T. W., Davern, M., Freese, J. & Morgan, S. General Social Surveys, 1972–2018. General Social Survey Data Explorer (GSS, 2020).
- 136.Bishop MD, Fish JN, Hammack PL, Russell ST. Sexual identity development milestones in three generations of sexual minority people: a national probability sample. Dev. Psychol. 2020;56:2177–2193. doi: 10.1037/dev0001105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Bolger, N. & Laurenceau, J.-P. Intensive Longitudinal Methods (Guilford Press, 2013).
- 138.Menard, S. Longitudinal Research (Sage, 2002).
- 139.Paradies Y, Ben J, Denson N, Elias A, Priest N. Racism as a determinant of health: a systematic review and meta-analysis. PLoS ONE. 2015;10:e0138511. doi: 10.1371/journal.pone.0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Rueda S, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open. 2016;6:e011453. doi: 10.1136/bmjopen-2016-011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Cook JE, Purdie-Vaughns V, Meyer IH, Busch JTA. Intervening within and across levels: a multilevel approach to stigma and public health. Soc. Sci. Med. 2014;103:101–109. doi: 10.1016/j.socscimed.2013.09.023. [DOI] [PubMed] [Google Scholar]
- 142.Chaudoir SR, Wang K, Pachankis JE. What reduces sexual minority stress? A review of the intervention “toolkit”. J Soc Issues. 2017;73:586–617. doi: 10.1111/josi.12233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Nyblade L, et al. Stigma in health facilities: why it matters and how we can change it. BMC Med. 2019;17:1–15. doi: 10.1186/s12916-019-1256-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Rao D, et al. A systematic review of multi-level stigma interventions: state of the science and future directions. BMC Med. 2019;17:1–11. doi: 10.1186/s12916-018-1244-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J. Int. AIDS Soc. 2013;16:18734. doi: 10.7448/IAS.16.3.18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Pachter LM, Szalacha LA, Bernstein BA, Garcia Coll C. Perceptions of Racism in Children and Youth (PRaCY): properties of a self-report instrument for research on children’s health and development. Ethn. Heal. 2010;15:33–46. doi: 10.1080/13557850903383196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Prinzie, P. & Onghena, P. in Encyclopedia of Statistics in Behavioral Science (eds Everitt, B. S. & Howell, D.) 319–322 (Wiley, 2005).
- 148.Curran PJ, et al. Advancing the study of adolescent substance use through the use of integrative data analysis. Eval. Health Prof. 2018;41:216–245. doi: 10.1177/0163278717747947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Alloy LB, Metalsky GI, Hartlage S. The hopelessness theory of depression: attributional aspects. Br. J. Clin. Psychol. 1988;27:5–21. doi: 10.1111/j.2044-8260.1988.tb00749.x. [DOI] [PubMed] [Google Scholar]
- 150.Chae DH, et al. Association between an internet-based measure of area racism and Black mortality. PLoS ONE. 2015;10:1–12. doi: 10.1371/journal.pone.0122963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Robinson P, Turk D, Jilka S, Cella M. Measuring attitudes towards mental health using social media: investigating stigma and trivialisation. Soc. Psychiatry Psychiatr. Epidemiol. 2019;54:51–58. doi: 10.1007/s00127-018-1571-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Hatzenbuehler, M. L. in The Oxford Handbook of Stigma, Discrimination, and Health (eds Major, B., Link, B. G. & Dovidio, J. F.) 105–121 (Oxford Univ. Press, 2017).
- 153.Krieger N, et al. Jim Crow and premature mortality among the US Black and White population, 1960–2009. Epidemiology. 2014;33:395–401. doi: 10.1097/EDE.0000000000000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Hartog K, et al. Stigma reduction interventions for children and adolescents in low- and middle-income countries: systematic review of intervention strategies. Soc. Sci. Med. 2020;246:112749. doi: 10.1016/j.socscimed.2019.112749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Hardeman RR, Karbeah J. Examining racism in health services research: a disciplinary self-critique. Health Serv. Res. 2020;55:777–780. doi: 10.1111/1475-6773.13558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Luoma JB, Kohlenberg BS, Hayes SC, Fletcher L. Slow and steady wins the race: a randomized clinical trial of acceptance and commitment therapy targeting shame in substance use disorders. J. Consult. Clin. Psychol. 2012;80:43–53. doi: 10.1037/a0026070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Carels RA, Rossi J, Solar C, Selensky JC. An ecological momentary assessment of weight stigma among weight loss participants. J. Health Psychol. 2019;24:1155–1166. doi: 10.1177/1359105317692855. [DOI] [PubMed] [Google Scholar]
- 158.Livingston NA, Heck NC, Szalda-Petree A, Cochran BN. Ecological momentary assessment of daily discrimination experiences and nicotine, alcohol, and drug use among sexual and gender minority individuals. J. Couns. Clin. Psychol. 2017;85:1131–1143. doi: 10.1037/ccp0000252. [DOI] [PMC free article] [PubMed] [Google Scholar]