Abstract
Rationale:
Loneliness is associated with negative health outcomes, such as cardiovascular disease, cognitive impairment, dementia, physical functional decline, depression, and increased mortality risk, among HIV-positive and HIV-negative older men who have sex with men (MSM). Given these negative health outcomes, it is imperative to identify factors that minimize loneliness in these vulnerable groups.
Objective:
We sought to examine whether social-environmental resiliencies–defined as an individual’s level of support, social bonding, and psychological sense of community among gay men–buffer against symptoms of loneliness.
Method:
We analyzed longitudinal data from 1,255 older MSM with and without HIV infection, all of whom were enrolled in the Multicenter AIDS Cohort Study (MACS). Using longitudinal latent class analysis (LLCA), we identified three underlying classes (Social Connectors, Non-community Connectors, and Social Isolates) in the social environment of the sample. We assessed the prevalence of loneliness by these latent classes. By lagging social environmental factors over time, we were able to examine the temporal relationships between latent classes and subsequent loneliness.
Results:
Consistent with our hypothesis, multivariate associations revealed that compared to Social Connectors with high levels of social support and social bonding and a strong perceived sense of community among gay men, Social Isolates (Prevalence Ratio (PR): 1.42; 95% CI: 1.08–1.88; p = 0.0120) and Non-community Connectors (PR: 1.34; 95% CI: 1.03–1.75; p = 0.0322) were more likely to experience loneliness after adjustment for covariates and baseline loneliness. There were no differences by HIV status.
Conclusions:
These longitudinal data allowed us to make causal inferences related to the social environmental resiliencies lowering the odds of loneliness among HIV-positive and HIV-negative older MSM. Developing individual-and community-level tailored interventions for these populations by leveraging social environmental resiliencies is key to reducing loneliness and promoting health.
Keywords: Social environment, Resilience, Older men who have sex with men, HIV/AIDS, Loneliness, Social support, Social bonding, Social cohesion
1. Introduction
Given that the life expectancy of people living with HIV (PLWH) has increased and that men who have sex with men (MSM) now account for nearly two-thirds of the HIV/AIDS epidemic in the United States (Centers for Disease, Control, and Prevention, 2016), it is imperative to understand how to promote the health of older MSM defined as 40 years and over in this study. Loneliness–defined as the feeling of isolation regardless of objective social network size (Keefe et al., 2006)–is a key health risk for HIV-positive and HIV-negative older MSM (Marziali et al., 2020; Rendina et al., 2019). This psychosocial challenge is of great concern to clinicians, public health officials, and gerontologists, given the numerous adverse health outcomes frequently associated with prolonged periods of loneliness: an increased incidence of cardiovascular disease (Valtorta et al., 2018; Xia and Li, 2018), cognitive impairment (Luchetti et al., 2020; Yang et al., 2020), dementia progression (Holwerda et al., 2014; Sutin et al., 2018), and depressive symptomatology (Bergman and Segel-Karpas, 2018; Ge et al., 2017). Additionally, a report of any loneliness symptoms, including mild symptoms, has been associated with functional decline and increased mortality risk (Henriksen et al., 2019; Holt-Lunstad et al., 2015). To minimize the risk of older MSM with and without HIV infection developing these adverse health outcomes, it is imperative to identify factors that minimize loneliness in these vulnerable groups.
To date, studies examining loneliness among older PLWH or the subpopulation of HIV-positive older MSM reveal that loneliness is a pressing public health problem among these populations (Greene et al., 2018; Jacobs and Kane, 2012; Karpiak et al., 2006; Leyva-Moral et al., 2019; Marziali et al., 2020; Mazonson et al., 2020; Rendina et al., 2019; Su et al., 2018; Yoo-Jeong et al., 2019). The Research on Older Adults with HIV (ROAH) study assessed loneliness among older adults living with HIV (Karpiak et al., 2006). Half of the respondents were Black, a third Latino, and about 14% White. The remaining 4% identified as Asian/Pacific Islander, American Indian, or multi-ethnic (Karpiak et al., 2006). The study used the 20-item version of the UCLA Loneliness Scale (Russell, 1996), which is designed to assess perceptions of inadequate support from a person’s social network. Results revealed an average score of 53 among participants (scores range from 20 to 80, with higher scores indicating a greater degree of loneliness) (Karpiak et al., 2006). A more recent study with older White (57%) and non-White/Latino participants (43%) living with HIV, who were primarily male, gay or bisexual, and in their mid-to-late 50s, demonstrated that 58% of them experienced some degree of loneliness (Greene et al., 2018). Lonely participants were more likely to report depression, alcohol, and tobacco use, and to have fewer relationships (Greene et al., 2018). In another study, 51% of older HIV-positive persons, the majority of whom were male (89%), gay (77%), and white (69%), were classified as lonely (Mazonson et al., 2020). The prevalence of loneliness was lower in the older age group (60 plus) compared to the “younger old” group (50–59 years) and may be explained by lower rates of depression and lower likelihood of feeling distant from friends among the older individuals (Mazonson et al., 2020). While previous studies demonstrate that loneliness is common among older HIV-positive MSM, these studies are limited in that none of them have a HIV-negative control group.
Given the high prevalence of loneliness among the older MSM population, particularly among HIV-positive older MSM, it is crucial to uncover more evidence about this public health concern and develop effective interventions aimed at reducing loneliness and promoting health. The concept of resilience has received growing attention in the public health literature. Efforts have increased to better understand how gay men promote and protect their health and well-being in the presence of adversity (Buttram, 2015; Herrick et al., 2011; Russell et al., 2003). Resilience is conceptualized as a process of adapting well in the face of adversity, trauma, tragedy, threats or significant sources of stress; this dynamic process involves the interplay of risk and protective factors (Masten and Powell, 2003; Yates and Masten, 2004). Although a risk factor such as loneliness is conceptualized as an adverse experience that can have negative effects on adaptive functioning and health, resiliencies that emanate from interpersonal and social environment sources may serve as protective factors against loneliness (Marziali et al., 2020; Rendina et al., 2019).
In particular, more evidence is needed to elucidate the role of resiliencies in the social environment such as social support, social networks, and social cohesion, which have been found to have a positive impact on health (Berkman and Glass, 2003; De Jesus et al., 2010; De Silva et al., 2005; Fiori et al., 2006; Ziersch et al., 2005). Social support is defined as having someone who can loan money, help out when sick, run errands, provide transportation, help with other tasks or take time to listen or to help deal with problems (Barrera, 1981). Social networks are the number and types of social connections one has including spouse/partner, close relatives and friends, and membership in church group or in other community organizations (Berkman and Syme, 1979). Social cohesion refers to the extent of connectedness and solidarity among groups (Kawachi and Berkman, 2000). These social environmental factors may increase resilience and in turn, may buffer against loneliness in persons living with HIV ages 40 years or older.
Several studies among HIV-positive MSM have demonstrated the positive impact of social environment resiliencies on health (Li et al., 2015; Ramirez-Valles et al., 2002, 2005; Rosario et al., 2001; Shao et al., 2018). One study showed that social support utilization–defined as the degree of utilizing various types of available support, such as seeking help from others and participating in social activities–was negatively associated with depression and anxiety among HIV-positive MSM in China (Shao et al., 2018). In another study, access to community resources was positively associated with perceived connectedness to the gay/bisexual community, and in turn was protective against loneliness among a sample of primarily White (84%), gay (77%) men, and HIV-negative (64%) (Li et al., 2015). Similarly, another study revealed that community involvement in AIDS and gay-related organizations among HIV-positive Latino gay men buffered against the adverse effects of stigma, depression, and loneliness (Ramirez-Valles et al., 2005). Other studies have shown that strong attachment to the gay community is protective for health (Li et al., 2015; Ramirez-Valles et al., 2002; Rosario et al., 2001). It offers protection by providing a sense of community and an opportunity to build social connections and systems of support that help combat loneliness. However, another study with Black MSM revealed that most of these men’s social support networks were comprised of family members or non-gay friends. Furthermore, social support as an element of resilience was experienced differently among Black MSM who did not have strong connections with the gay community compared to those who did (Buttram, 2015). While previous studies among MSM demonstrate the protective effect of resiliencies on health, the results of these studies were not specific to older MSM and all of the studies were cross-sectional. More information is needed on the effects of resiliencies on health in this sub-population of MSM.
In studies that examine older lesbian, gay, and bisexual (LGB) adults, social environmental factors were found to influence the level of loneliness. In a study that investigated older LGB, primarily White (89%) adults, both those living alone and those living with someone other than a partner reported higher degrees of loneliness compared with older LGB adults living with a partner or spouse (Kim and Fredriksen-Goldsen, 2016). Results revealed that social support, social network size, and internalized stigma partially accounted for the observed relationship between living arrangement and loneliness (Kim and Fredriksen-Goldsen, 2016). Another study reported that older, mostly White, LGB adults living alone are more likely to feel lonely than those living with others (Grossman et al., 2000). Furthermore, results revealed that an elevated risk of loneliness among these adults is associated with a lower level of satisfaction with the social support they receive (Grossman et al., 2000). Existing literature suggests that the relationship between living arrangement and loneliness may be because persons in non-partnered living arrangements have limited social resources (Grossman et al., 2000; Schnittker, 2007; Yeh and Lo, 2004). These studies, while relevant to older MSM, were limited in that they mainly focused on one particular dimension of the social environment and did not focus on participants’ HIV status.
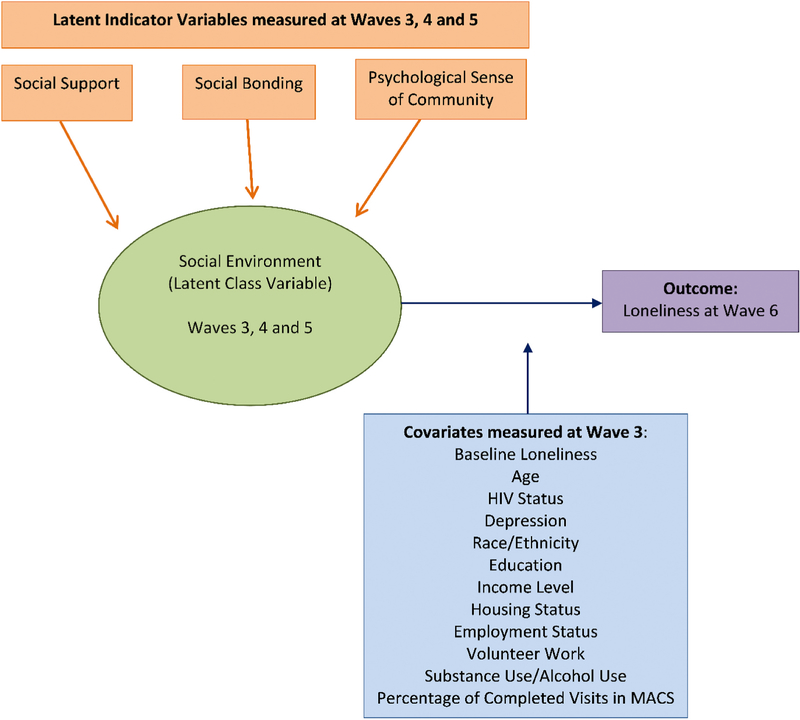
Given the dearth of longitudinal studies on loneliness among older MSM with and without HIV, this study aimed to fill this gap in the literature by examining the extent to which social environmental resiliencies–defined as an individual’s level of support, social bonding, and psychological sense of community–act as protective factors against loneliness over time among these subpopulations of MSM (Fig. 1). This study had a HIV-negative MSM group that acted as a control group. The objectives of this study among older MSM with and without HIV infection were to: (1) identify underlying classes of individuals based on their social environment using longitudinal latent class analysis; (2) assess the prevalence of loneliness by these underlying classes; and (3) examine whether there are differences in the prevalence of loneliness by HIV status. We hypothesized that aging MSM who report higher levels of social support and social bonding, and a stronger psychological sense of community among gay men will be less likely to experience loneliness than aging MSM who do not. We also hypothesized that there will not be differences by HIV status. Based on the resilience literature, we predicted that the impact of social-environmental resiliencies (i.e., social support, social networks, and social cohesion) on loneliness will be greater than the impact of HIV status.
Fig. 1.
Hypothesized model of the social environment resiliencies and loneliness among older MSM.
2. Method
2.1. Study population
The Multicenter AIDS Cohort Study (MACS) is a longitudinal study that examines the natural and treated history of HIV/AIDS among men who have sex with men (MSM) in Baltimore, Maryland/Washington, DC, Chicago, Illinois, Los Angeles, California, and Pittsburgh, Pennsylvania. Since 1984, 7,352 HIV-positive and -negative participants were enrolled over four time periods: 4,954 in 1984–85, 668 in 1987–1991, 1,350 in 2001–2003, and 380 in 2011–2019. MACS participants attended semiannual visits that involve an audio computer-assisted self-interview and a standardized clinic examination. Details on the study design appear elsewhere (Dudley et al., 1995; Kaslow et al., 1987). Study instruments can be found at http://www.mwccs.org.
2.2. Healthy Aging sub-study
The Healthy Aging sub-study, nested within the MACS, seeks to understand psychosocial resiliency factors that contribute to healthy aging among older MSM with and without HIV infection. The sub-study was conducted over six Waves (Table 1). Inclusion criteria for the study were that participants had to be at least 40 years old on or before April 2016, reported at least one incidence of sexual intercourse with another man since enrolling in the MACS, and completed at least two consecutive MACS visits before April 2016 (Meanley et al., 2019). There was a total of 1,318 MACS participants enrolled in the sub-study. Current analyses used data collected at Waves 3–6. The analytic sample included 1,255 HIV-positive and -negative MACS participants who completed surveys during those waves. Institutional Review Boards (IRB) at each study site approved the MACS and Healthy Aging sub-study protocols, and informed consent was obtained from all participants. Participants were also provided a nominal incentive for each completed survey (up to six) that was approved by each site’s IRB.
Table 1.
Healthy Aging sub-study enrollment wave and corresponding MACS visits and dates.
| Enrollment Wave | MACS Visit | MACS Visit Dates |
|---|---|---|
|
| ||
| 1 | 65 | April 2016–September 2016 |
| 2 | 66 | October 2016–March 2017 |
| 3 | 67 | April 2017–September 2017 |
| 4 | 68 | October 2017–March 2018 |
| 5 | 69 | April 2018–September 2018 |
| 6 | 70 | October 2018–March 2019 |
3. Measures
3.1. Indicators of social environment
We included three scales as indicators of the latent construct of social environment among MSM: 1) perceived social support; 2) social bonding as measured by the 24-item social provisions scale (Cutrona et al., 1987; Russell and Cutrona, 1984); and 3) psychological sense of community scale adapted to the gay male community (McMillan and Chavis, 1986; Proescholdbell et al., 2006). Data from these scales were obtained at Waves 3, 4, and 5.
Perceived Social Support.
Social support was defined as having someone who can loan money, help out when sick, run errands, provide transportation, help with other tasks, or take time to listen to help deal with problems. Participants were asked how much support they receive from the following people in the last 6 months: 1) Primary partners (e.g., boyfriend[s], girlfriend[s], spouse); 2) Biological family (e.g., mother, father, siblings, children); 3) Created family (e.g., friends in your life who you consider to be family; 4) Friends; 5) Acquaintances; 6) People in your church; 7) Coworkers; and 8) Others. Possible responses were “Not at all”, “Very little”, “Somewhat”, “Quite a bit”, “A great deal”, “Prefer not to say” and “N/A”. For the analysis, responses were collapsed into “Not at all/Very Little”, “Somewhat”, “A great deal/Quite a bit,” and “N/A”. “Prefer not to say” responses were coded as missing. The standardized Cronbach’s αs for Perceived Social Support at Waves 3, 4, and 5 were 0.823, 0.826, and 0.818, respectively.
Social Provisions Scale.
The 24-item Social Provisions Scale (SPS-24) was developed to measure the degree of social support through six subscales: 1) Emotional support or attachment; 2) Social integration; 3) Reassurance of worth; 4) Tangible help; 5) Orientation; and 6) Opportunity of nurturance. The scale items are detailed elsewhere (Cutrona et al., 1987; Russell and Cutrona, 1984). Possible responses to the items were “Strongly Agree”, “Agree”, “Disagree”, and “Strongly Disagree”. For the analysis, responses were collapsed into “Strongly Agree/Agree” and “Disagree/Strongly Disagree”. The standardized Cronbach as for Social Provisions Scales at Waves 3, 4, and 5 were 0.832, 0.860, and 0.834, respectively.
Psychological Sense of Community.
Psychological sense of community is the degree to which members of a community feel that they belong, feel that they matter to one another and to the group, and feel that their needs are met by the group (McMillan et al., 1986). This scale has been adapted to the gay male community (Proescholdbell et al., 2006). The following questions were asked: 1) How much do you feel you can get help from gay men if you need it? 2) How much do you feel that you help other people in the gay male community? 3) How much do you feel like you belong in the gay male community? 4) How much do you feel like you are a member of the gay male community? 5) How much do you feel like a part of the gay male community?; and 6) How many of your needs do you feel are met by the gay male community? Possible responses to items 1–5 were “None”, “A little”, “Some”, “A fair deal”, “A great deal”, and “prefer not to say”. For the analysis, these responses were collapsed into “None/a little”, “Some”, and “A fair deal/a great deal”. Possible responses to item 6 were “None”, “A few”, “About half”, “Most”, “All” and “Prefer not to say”. These responses were collapsed into “None/a few”, “About half”, “Most/All”. “Prefer not to say” responses were coded as missing. The standardized Cronbach’s as for Psychological Sense of Community at Waves 3, 4, and 5 were 0.930, 0.933, and 0.927, respectively.
4. Covariates
Covariates were obtained at wave 3.
HIV Status.
HIV status (“HIV-positive”/“HIV-negative”) was assessed using enzyme-linked immunosorbent assay and a confirmatory Western blot on all MACS participants at their baseline visit and at every visit for HIV-negative participants. HIV-positive participants include those who tested as such at baseline or seroconverted during study observation.
Percentage of Completed MACS Visits.
To assess for possible cohort effect on loneliness, we calculated the percentage of completed MACS study, adjusted for by MACS enrollment wave.
Sociodemographic Characteristics.
Age was calculated from date of birth and date of survey administration at wave 3 and reported continuously in years. Race/ethnicity was self-reported and categorized into: 1) “White, non-Hispanic”; 2) “Black, non-Hispanic”; 3) “Hispanic”; and 4) “Other” (American Indian, Asian and Pacific Islander). Education was self-reported and categorized into: 1) “Less than High School”; 2) “High School Diploma”; 3) “Some or completed college” and 4) “Some or completed graduate education”. Participants reporting any part-time, full-time or self-employment were classified as being “Employed”, otherwise participants were considered “Not employed”. Income was self-reported and categorized into: 1) “Less than $29,999”; 2) “$30,000-$59,999”; and 3) “$60,000 or more”. Housing status was self-reported and categorized into: 1) “In your own home”; 2) “At your parent’s home”; 3) “Someone else’s home”; 3) “In shelter/welfare housing”; 4) “In rooming, boarding or halfway house”; 5) “Residential drug or alcohol facility”; and 6) “Other place”. For analysis purposes, housing status was collapsed into “In your own home” and “Not in your own home”.
Sexual Orientation.
Participants were asked to indicate their sexual orientation. The choices were “Gay”, “Bisexual”, “Heterosexual/Straight”, and “Other”.
Depressive symptoms.
Depressive symptoms were assessed using the Center for Epidemiological Studies Depression Scale (CES-D) (Radloff, 1977). Participants with a score greater than or equal to 16 were categorized as having “depressive symptoms”. Participants with a score less than 16 were categorized as having “no depressive symptoms”.
Volunteer Work.
Volunteer work was a dichotomous indicator (“Yes”/“No”) of any political, religious, charitable or unspecified volunteer activity.
Alcohol Use.
Self-report alcohol use was categorized into: 1) “None”; 2) “Low/Moderate (1–2 drinks/day)”; 3) “Moderate/Heavy (3–4 drinks/day)”; and 4) “Heavy (5 drinks/day)”
Substance Use.
Self-reported marijuana, popper, cocaine/crack and methamphetamine use (“Yes”/“No”) were included.
4.1. Outcome
Loneliness.
Loneliness was assessed using the UCLA 3-item Loneliness Scale (Hughes et al., 2004) at Waves 3 (baseline) and 6 (outcome). The questions were: 1) How often do you feel that you lack companionship?; 2) How often do you feel left out?; 3) How often do you feel isolated from others? The scale uses three response categories: “Hardly Ever” (scored 1); “Some of the Time” (scored 2); and “Often” (scored 3). Responses are summed and possible values ranged from 3 to 9. Higher scores indicated greater loneliness. Scores were then categorized into a dichotomous variable: “Not lonely” (<6) and “Lonely” (≥6) (Doménech-Abella et al., 2017; Steptoe et al., 2013). Loneliness at wave 6 (outcome) was modeled as an outcome while adjusting for loneliness at baseline.
4.2. Statistical analysis
Descriptive statistics by HIV status were generated using frequency/percentage and median/interquartile range (IQR) where appropriate. Distribution of responses to the scales were generated by wave (3, 4, and 5) and included as supplemental information. Longitudinal latent class analysis (LLCA) was used to identify mutually exclusive latent classes by modeling indicators of social environment over wave 3, 4, and 5. Missing values were assumed to be at random. Model selection was performed using a step-wise approach, testing up to five classes. Model fit statistics included Bayesian information criterion (BIC), entropy, the Lo-Mendel-Rubin Adjusted Likelihood Ratio Test (LMR LRT). In combination with a priori knowledge, the model with the optimal number of classes had lower BIC values, high entropy (≥0.7) and statistically significant LMR LRT p-value (<0.05) (Jung et al., 2008; Tein et al., 2013). Homogeneity (degree to which the item response probabilities are close to 0 or 1) and latent class separation (degree to which latent classes can be distinguished from one another) were also considered. Parameters estimated in LLCA were latent class membership probabilities and item response probabilities. Participants were assigned to classes for which they had the highest posterior probability of membership based on their responses to the indicators (items).
Descriptive statistics by the resulting latent classes were generated. Differences in distributions by latent class were evaluated by χ2, Fisher’s Exact test, and Wilcoxon Rank sum. The average item response probabilities across Waves 3, 4, and 5 were plotted by latent class as stacked bar charts. Poisson regression with robust error variance was used to assess the prevalence of loneliness at wave 6 using the social environment latent classes as the primary predictor and adjusting for covariates and loneliness at baseline. The primary predictor and each covariate were modeled independently. Additionally, an interaction between HIV status and the latent classes was also tested. Latent classes, core demographic variables (age, HIV status, race/ethnicity, and sexual orientation), loneliness at baseline, and any covariates and interactions with a p-value <0.10 in their respective bivariate model were included in the final adjusted model. Unadjusted and adjusted odds ratios (OR) along with their 95% confidence interval (CI) were reported. Statistical significance was set at p-value <0.05. Statistical analyses were performed in Mplus version 8.4 (Muthén and Muthén, 2020) and SAS version 9.4 (2014).
4.3. Missing values
We examined missing values in the two components of this analysis, LLCA and Poisson regression model with robust error variance. Out of the total 1,255 participants, there were two who were missing values on all indicator variables for the LLCA model and 435 missing at least the outcome variable or covariates for the Poisson regression model. In the LLCA procedure, missing values are addressed through maximum likelihood estimation and used all available information to estimate the parameters (Little and Rubin, 1989). Because there were only two participants were missing on all indicator variables, we felt it was reasonable to allow them to be dropped from the analysis. The Poisson regression model deleted any observations missing the outcome or at least one independent variable. We sought to determine the mechanism of missingness to ensure list-wise deletion is appropriate: 1) missing completely at random (MCAR), 2) missing at random (MAR) or 3) missing not at random (MNAR). We performed Little’s MCAR test for the missing outcome and covariates (Little, 1988). The MCAR test was statistically significant for (χ2 = 563.640; df = 47; p < 0.0001), indicating that the data were not MCAR and thus not appropriate for list-wise deletion. Since there is no formal test to distinguish MAR and MNAR, we concluded that in either case multiple imputation would be appropriate rather than allowing for listwise deletion, which can produce biased results (Sidi and Harel, 2018; van Ginkel et al., 2020). The chosen method of imputation was multiple imputation with fully conditional specification using the SAS procedure PROC MI. Because missing data were categorical, we used the logistic regression approach. The analysis was conducted in three stages: 1) multiply-impute the incomplete data 25 times using PROC MI; 2) analyze each imputed dataset using the Poisson regression model with robust error variance; 3) combining the results of each imputed dataset to obtain the model parameter estimates using PROC MIANALYZE. Subsequently, we compared the estimates from the multiply-imputed dataset to dataset with no imputation. It was worth noting that results from both analyses were similar.
5. Results
5.1. Population characteristics by HIV status
There were 631 (50.3%) HIV-negative and 624 (49.7%) HIV-positive participants. The overall median age was 61.0 (IQR: 55.0–66.0) years (HIV-negative: 63.0 years; HIV-positive 58.0 years). The overall median percentage of completed MACS visits was 86.2% (IQR:75.0%–96.6%) (HIV-negative: 79.5%; HIV-positive: 89.7%). The majority of participants were White, non-Hispanic (HIV-negative: 80.7%; HIV-positive: 58.0%), college educated (HIV-negative: 90.3%; HIV-positive: 81.4%), gay (HIV-negative: 89.2%; HIV-positive: 83.7%), live on their own (HIV-negative: 93.8%; HIV-positive: 84.8%), employed (HIV-negative: 58.2%; HIV-positive: 53.4%), and reported volunteer work (HIV-negative: 61.0%; HIV-positive: 55.6%). Many HIV-negative participants reported making $60,000 or more (41.7%), while many HIV-positive participants made less than $29,999 (40.1%). Most participants reported low to moderate drinking (HIV-negative: 59%; HIV-positive: 58.0%). Among HIV-negative participants, marijuana, popper, cocaine/crack and methamphetamine use was 20.6%, 17.1%, 3.3%, and 1.0%, respectively. HIV-positive participants reported marijuana, popper, cocaine/crack and methamphetamine use at 33.5%, 23.9%, 8.2%, and 6.4%, respectively. A quarter (25.2%) of HIV-positive participants and 17.6% of HIV-negative participants reported depressive symptoms. At baseline, the median loneliness score was 4.0 (IQR: 3.0–6.0) for HIV-negative participants and 5.0 (IQR: 3.0–6.0) for HIV-positive participants. At Wave 6, the median loneliness score was 4.0 (IQR: 3.0–6.0) for HIV-negative participants and 4.5 (IQR: 3.0–6.0) for HIV-positive participants (Table 2).
Table 2.
Population characteristics by HIV status.
| HIV-Negative (n = 631) | HIV-Positive (n = 624) | Overall (n = 1,255) | |
|---|---|---|---|
|
| |||
| Age (years), Median (IQR) | 63.0 (57.0, 69.0) | 58.0 (53.0, 64.0) | 61.0 (55.0, 66.0) |
| Percentage of Completed Visits, Median (IQR) | 79.5 (75.5–93.1) | 89.7 (75.9–96.6) | 86.2 (75.0–96.6) |
| Race/Ethnicity, n (%) | |||
| White, non-Hispanic | 509 (80.7) | 362 (58.0) | 871 (69.4) |
| Black, non-Hispanic | 79 (12.5) | 171 (27.4) | 250 (19.9) |
| Hispanic | 32 (5.1) | 79 (12.7) | 111 (8.8) |
| Other | 11 (1.7) | 12 (1.9) | 23 (1.8) |
| Education, n (%) | |||
| Less than High School | 13 (2.1) | 31 (5.0) | 44 (3.5) |
| High School | 48 (7.6) | 85 (13.6) | 133 (10.6) |
| College | 301 (47.7) | 343 (55.0) | 644 (51.3) |
| Graduate School | 269 (42.6) | 165 (26.4) | 434 (34.6) |
| Sexual Orientation, n (%) | |||
| Gay | 562 (89.1) | 522 (83.7) | 1084 (86.4) |
| Bisexual | 18 (2.9) | 43 (6.9) | 61 (4.9) |
| Heterosexual/Straight | 20 (3.2) | 11 (1.8) | 31 (2.5) |
| Other | 10 (1.6) | 11 (1.8) | 21 (1.7) |
| Missing | 21 (3.3) | 37 (5.9) | 58 (4.6) |
| Depressive Symptoms, n (%) | |||
| Depressive symptoms (CES-D ≥16) | 111 (17.6) | 157 (25.2) | 268 (21.4) |
| No depressive symptoms (CES-D < 16) | 484 (76.7) | 432 (69.2) | 916 (73.0) |
| Missing | 36 (5.7) | 35 (5.6) | 71 (5.7) |
| Employment Status, n (%) | |||
| Employed | 367 (58.2) | 333 (53.4) | 700 (55.8) |
| Not Employed | 240 (38.0) | 271 (43.4) | 511 (40.7) |
| Missing | 24 (3.8) | 20 (3.2) | 44 (3.5) |
| Income Category, n (%) | |||
| Less than $29,999 | 150 (23.8) | 250 (40.1) | 400 (31.9) |
| $30,000 to $59,999 | 152 (24.1) | 153 (24.5) | 305 (24.3) |
| $60,000 or more | 263 (41.7) | 168 (26.9) | 431 (34.3) |
| Missing/do not wish to respond | 66 (10.5) | 53 (8.5) | 119 (9.5) |
| Housing Status, n (%) | |||
| In your own home | 592 (93.8) | 529 (84.8) | 1121 (89.3) |
| Not in your own home | 35 (5.5) | 79 (12.6) | 114 (9.1) |
| Prefer not to say | 1 (0.2) | 4 (0.6) | 5 (0.4) |
| Missing | 3 (0.5) | 12 (1.9) | 15 (1.2) |
| Volunteer Work, n (%) | |||
| No | 237 (37.6) | 257 (41.2) | 494 (39.4) |
| Yes | 385 (61.0) | 347 (55.6) | 732 (58.3) |
| Missing | 9 (1.4) | 20 (3.2) | 29 (2.3) |
| Alcohol Use, n (%) | |||
| None | 113 (17.9) | 124 (19.9) | 237 (18.9) |
| Low/Moderate | 378 (59.9) | 339 (54.3) | 717 (57.1) |
| Moderate/Heavy | 73 (11.6) | 90 (14.4) | 163 (13.0) |
| Heavy | 25 (4.0) | 29 (4.6) | 54 (4.3) |
| Missing | 42 (6.7) | 42 (6.7) | 84 (6.7) |
| Marijuana Use, n (%) | |||
| No | 459 (72.7) | 377 (60.4) | 836 (66.6) |
| Yes | 130 (20.6) | 209 (33.5) | 339 (27.0) |
| Missing | 42 (6.7) | 38 (6.1) | 80 (6.4) |
| Popper Use, n (%) | |||
| No | 483 (76.5) | 433 (69.4) | 916 (73.0) |
| Yes | 108 (17.1) | 149 (23.9) | 257 (20.5) |
| Missing | 40 (6.3) | 42 (6.7) | 82 (6.5) |
| Cocaine/Crack Use, n (%) | |||
| No | 569 (90.2) | 524 (84.0) | 1093 (87.1) |
| Yes | 21 (3.3) | 51 (8.2) | 72 (5.7) |
| Missing | 41 (6.5) | 49 (7.9) | 90 (7.2) |
| Methamphetamine Use, n (%) | |||
| No | 585 (92.7) | 543 (87.0) | 1128 (89.9) |
| Yes | 6 (1.0) | 40 (6.4) | 46 (3.7) |
| Missing | 40 (6.3) | 41 (6.6) | 81 (6.5) |
| Loneliness Scale Sum at wave 3, Median (IQR) | 4.0 (3.0, 6.0) | 5.0 (3.0, 6.0) | 4.0 (3.0, 6.0) |
| Loneliness Scale Sum at wave 6, Median (IQR) | 4.0 (3.0, 6.0) | 4.5 (3.0, 6.0) | 4.0 (3.0, 6.0) |
IQR=Interquartile Range.
5.2. Model selection
Model fit statistics for one to five class models are reported in Table 3. The five-class solution had the lowest BIC (132,470.947) and highest entropy (0.96). However, the LMR LRT was no longer statistically significant after the three classes, which indicates that the model does not improve beyond the three-class solution. In addition, the three-class model demonstrated higher homogeneity and latent class separation compared to higher class solutions. Ultimately, the optimal number of classes selected was three. The BIC, entropy, and LMR LRT p-value of the final three class model was 134,259.888, 0.959, and p = 0.0007, respectively. The classification probabilities for the most likely latent class membership by latent class were reported in Table 4.
Table 3.
Model fit selection.
| Number of Classes | Bayesian Information Criterion | Entropy | Lo-Mendel-Rubin Adjusted LRT |
|---|---|---|---|
|
| |||
| 1 | 150846.761 | 1.000 | - |
| 2 | 138820.365 | 0.941 | 0.0000 |
| 3 | 134259.888 | 0.959 | 0.0007 |
| 4 | 133313.833 | 0.955 | 0.6297 |
| 5 | 132470.947 | 0.960 | 0.3721 |
LRT = Likelihood ratio test.
Table 4.
Classification probabilities for the most likely latent class membership by latent class.
| 1 | 2 | 3 | |
|---|---|---|---|
|
| |||
| 1 | 0.988 | 0.012 | 0.000 |
| 2 | 0.014 | 0.980 | 0.006 |
| 3 | 0.002 | 0.016 | 0.981 |
5.3. Latent classes of social environment
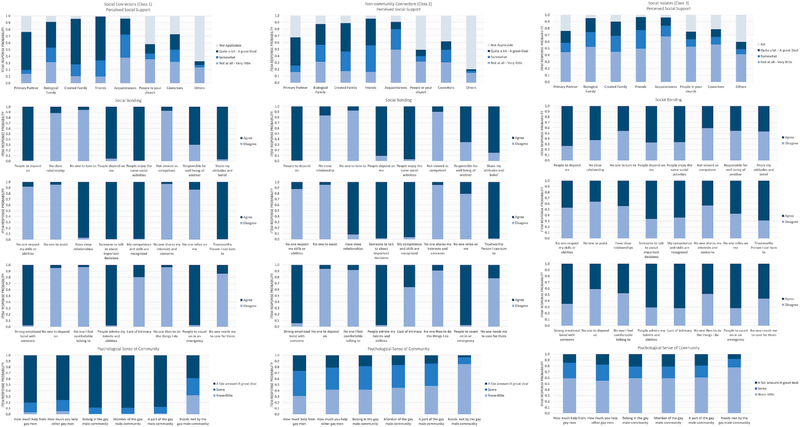
Three mutually exclusive latent classes emerged from this analytic sample. Class 1 (41.7%), or Social Connectors, is described as those who receive “a great deal” or “quite a bit” of support from primary partners, biological family, created family, and friends, and feel supported “somewhat” by acquaintances. They also have a high degree of social bonding from their networks and have a high sense of community among gay men. Class 2 (39.2%), or Non-community Connectors, is characterized by participants who tend to receive “somewhat” to “a great deal” of support from primary partners, biological family, created family and friends. Similar to Class 1, they also have a high degree of social bonding from their networks. However, they tend to perceive “none/a little” to “some” sense of community among gay men. Class 3 (19.1%), Social Isolates, is characterized by participants who mostly do not receive support from primary partners, biological family, created family, friends, acquaintances, people from church, coworkers or others. Compared to the other classes, Social Isolates tend to have a lower degree of social bonding from their networks and, similarly to Class 2, tend to perceive “none/a little” to “some” sense of community among gay men. Fig. 2 illustrates the distribution of the item response probabilities by class.
Fig. 2.
Social environment latent profile plot.
5.4. Population characteristics by latent classes
Social Connectors (Class 1) had a median age of 62.0 years (IQR: 56.0–67.0) and completed a median of 86.2% of their MACS visits (IQR: 75.0%–96.5%). Most were White non-Hispanic (75.1%), college educated (90.4%), identified as gay (91.8%), and lived on their own (92.4%). Less than half had an annual income greater than $60,000 per year (43.8%). More than half were HIV-negative (56.2%), currently employed (62.5%), volunteered (69.2%), and reported low to moderate drinking (59.5%). Marijuana, popper, cocaine/crack and methamphetamine use was at 31.2%, 25.4%, 4.4% and 3.4%, respectively. Depressive symptoms were reported in 12.2% of Social Connectors and the median loneliness scale sum at baseline and at wave 6 was 3.0 (IQR: 3.0–5.0).
Non-community Connectors (Class 2) had a median age of 61.0 years (IQR: 55.0–66.0) and completed a median of 86.2% of their MACS visits (IQR: 75.0%–96.5%). Most were White non-Hispanic (73.1%), college educated (87.1%), identified as gay (85.1%), and lived on their own (91.9%). A little over a third made more than $60,000 per year (34.6%) and approximately half were HIV-positive (51.7%) and reported volunteer activities (51.9%). More than half were employed (55.8%) and reported low to moderate drinking (58.5%). Marijuana, popper, cocaine/crack and methamphetamine use was at 21.2%, 16.1%, 4.3% and 2.0%, respectively. Depressive symptoms were reported in 17.3% of Non-community Connectors and the median loneliness scale sum at baseline and wave 6 was 5.0 (IQR: 3.0–6.0) and 4.0 (IQR: 3.0–6.0), respectively.
Social Isolates (Class 3) had a median age of 58.0 years (IQR: 52.0–63.0) and completed a median of 86.2% of their MACS visits (IQR: 69.9%–93.1%). Most were college educated (73.6%), identified as gay (77.0%), and lived on their own (77.7%). More than half were HIV-positive (58.2%), unemployed (56.5%), and made less than $29,999 per year (59.0%). Approximately half were White non-Hispanic (49.0%), volunteered (47.7%), and reported low to moderate drinking (49.4%). Marijuana, popper, cocaine/crack and methamphetamine use was at 30.1%, 18.8%, 11.7% and 7.5%, respectively. Depressive symptoms were reported in 49.8% of Social Isolates and the median loneliness scale sum at baseline and wave 6 was 7.0 (IQR: 5.0–9.0). The differences in distribution of the covariates by latent class were statistically significant (Table 5).
Table 5.
Characteristics by latent class.
| Social Connectors | Non-community Connectors | Social Isolates | P-value | |
|---|---|---|---|---|
|
|
|
|
|
|
| N (%) | 523 (41.7) | 491 (39.2) | 239 (19.1) | |
|
| ||||
| Age (years), Median (IQR) | 62.0 (56.0, 67.0) | 61.0 (55.0, 66.0) | 58.0 (52.0, 63.0) | <0.0001 |
| Percentage of Completed Visits, Median (IQR) | 86.2 (75.0–96.5) | 86.2 (75.0–96.5) | 86.2 (69.9–93.1) | 0.0830 |
| HIV Status, n (%) | ||||
| Positive | 229 (43.8) | 254 (51.7) | 139 (58.2) | 0.0006 |
| Negative | 294 (56.2) | 237 (48.3) | 100 (41.8) | |
| Race/Ethnicity, n (%) | ||||
| White, non-Hispanic | 393 (75.1) | 359 (73.1) | 117 (49.0) | <0.0001 |
| Black, non-Hispanic | 76 (14.5) | 91 (18.5) | 83 (34.7) | |
| Hispanic | 46 (8.8) | 29 (5.9) | 36 (15.1) | |
| Other | 8 (1.5) | 12 (2.4) | 3 (1.3) | |
| Education, n (%) | ||||
| Less than High School | 9 (1.7) | 14 (2.9) | 21 (8.8) | <0.0001 |
| High School | 41 (7.8) | 49 (10.0) | 42 (17.6) | |
| College | 261 (49.9) | 256 (52.1) | 126 (52.7) | |
| Graduate School | 212 (40.5) | 172 (35.0) | 50 (20.9) | |
| Sexual Orientation, n (%) | ||||
| Gay | 480 (91.8) | 418 (85.1) | 184 (77.0) | <0.0001 |
| Bisexual | 19 (3.6) | 27 (5.5) | 15 (6.3) | |
| Heterosexual/Straight | 2 (0.4) | 12 (2.4) | 17 (7.1) | |
| Other | 9 (1.7) | 7 (1.4) | 5 (2.1) | |
| Missing | 13 (2.5) | 27 (5.5) | 18 (7.5) | |
| Depressive Symptoms, n (%) | ||||
| Depressive symptoms (CES-D ≥16) | 64 (12.2) | 85 (17.3) | 119 (49.8) | <0.0001 |
| No depressive symptoms (CES-D < 16) | 432 (82.6) | 374 (76.2) | 109 (45.6) | |
| Missing | 27 (5.2) | 32 (6.5) | 11 (4.6) | |
| Employment Status, n (%) | ||||
| Employed | 327 (62.5) | 274 (55.8) | 99 (41.4) | <0.0001 |
| Not Employed | 182 (34.8) | 193 (39.3) | 135 (56.5) | |
| Missing | 14 (2.7) | 24 (4.9) | 5 (2.1) | |
| Income Category, n (%) | ||||
| Less than $29,999 | 112 (21.4) | 146 (29.7) | 141 (59.0) | <0.0001 |
| $30,000 to $59,999 | 134 (25.6) | 124 (25.3) | 47 (19.7) | |
| $60,000 or more | 229 (43.8) | 170 (34.6) | 32 (13.4) | |
| Missing/do not wish to respond | 48 (9.2) | 51 (10.4) | 19 (7.9) | |
| Housing Status, n (%) | ||||
| In your own home | 483 (92.4) | 451 (91.9) | 185 (77.4) | <0.0001 |
| At your parent’s home | 34 (6.5) | 34 (6.9) | 46 (19.2) | |
| Prefer not to say | 0 (0.0) | 3 (0.6) | 2 (0.8) | |
| Missing | 6 (1.1) | 3 (0.6) | 6 (2.5) | |
| Volunteer Work, n (%) | ||||
| No | 158 (30.2) | 225 (45.8) | 110 (46.0) | <0.0001 |
| Yes | 362 (69.2) | 255 (51.9) | 114 (47.7) | |
| Missing | 3 (0.6) | 11 (2.2) | 15 (6.3) | |
| Alcohol Use, n (%) | ||||
| None | 82 (15.7) | 86 (17.5) | 69 (28.9) | 0.0005 |
| Low/Moderate | 311 (59.5) | 287 (58.5) | 118 (49.4) | |
| Moderate/Heavy | 78 (14.9) | 62 (12.6) | 23 (9.6) | |
| Heavy | 24 (4.6) | 17 (3.5) | 13 (5.4) | |
| Missing | 28 (5.4) | 39 (7.9) | 16 (6.7) | |
| Marijuana Use, n (%) | ||||
| No | 331 (63.3) | 351 (71.5) | 153 (64.0) | 0.0017 |
| Yes | 163 (31.2) | 104 (21.2) | 72 (30.1) | |
| Missing | 29 (5.5) | 36 (7.3) | 14 (5.9) | |
| Popper Use, n (%) | ||||
| No | 359 (68.6) | 376 (76.6) | 180 (75.3) | 0.0019 |
| Yes | 133 (25.4) | 79 (16.1) | 45 (18.8) | |
| Missing | 31 (5.9) | 36 (7.3) | 14 (5.9) | |
| Cocaine/Crack Use, n (%) | ||||
| No | 466 (89.1) | 434 (88.4) | 192 (80.3) | 0.0002 |
| Yes | 23 (4.4) | 21 (4.3) | 28 (11.7) | |
| Missing | 34 (6.5) | 36 (7.3) | 19 (7.9) | |
| Methamphetamine Use, n (%) | ||||
| No | 473 (90.4) | 446 (90.8) | 208 (87.0) | 0.0020 |
| Yes | 18 (3.4) | 10 (2.0) | 18 (7.5) | |
| Missing | 32 (6.1) | 35 (7.1) | 13 (5.4) | |
| Loneliness Scale Sum at wave 3, Median (IQR) | 3.0 (3.0, 5.0) | 5.0 (3.0, 6.0) | 7.0 (5.0, 9.0) | <0.0001 |
| Loneliness Scale Sum at wave 6, Median (IQR) | 3.0 (3.0, 5.0) | 4.0 (3.0, 6.0) | 7.0 (5.0, 9.0) | <0.0001 |
IQR=Interquartile range.
5.5. Bivariate associations of social environment latent classes and covariates on loneliness
Bivariate analysis revealed that the association of latent social classes on loneliness outcome measure was statistically significant. Age, percentage of completed MACS visits, sexual orientation, depressive symptoms, income category, housing status, and methamphetamine use had either a statistically significant (p < 0.05) or marginally significant (p < 0.10) association with loneliness. The interaction between HIV status and latent class was not statistically significant. Ultimately, the latent classes, age, HIV status, percentage of completed MACS visits, race/ethnicity, sexual orientation, depressive symptoms, income level, housing status, cocaine/crack use, methamphetamine use, and baseline loneliness were included in the final multivariate model (Table 6).
Table 6.
Bivariate and multivariate associations of Latent Class on Loneliness at Wave 6.
| Bivariate Analysis |
Multivariate Analysis |
|||
|---|---|---|---|---|
| Prevalence Ratio (95% CI) | P-value | Prevalence Ratio (95% CI) | P-value | |
|
| ||||
| Latent Class | ||||
| Non-community Connectors | 1.68 (1.34–2.09) | <.0001 | 1.34 (1.03–1.75) | 0.0322 |
| Social Isolate | 3.14 (2.55–3.86) | <.0001 | 1.42 (1.08–1.88) | 0.012 |
| Social Connectors | Referent | – | ||
| Age (per 10-year increase) | 0.92 (0.88–1.02) | 0.0001 | 0.96 (0.92–1.00) | 0.0594 |
| Percentage of Completed Visits (per 10 increase) | 0.96 (0.91–1.00) | 0.0516 | 0.85 (0.60–1.19) | 0.3373 |
| HIV Status | ||||
| Positive | 1.12 (0.95–1.32) | 0.1786 | 1.08 (0.79–1.47) | 0.6304 |
| Negative | Referent | – | Referent | – |
| Race/Ethnicity | ||||
| Black, non-Hispanic | 1.15 (0.95–1.39) | 0.1592 | 1.00 (0.82–1.21) | 0.9895 |
| Hispanic | 1.07 (0.81–1.41) | 0.6432 | 0.90 (0.70–1.16) | 0.4002 |
| Other | 0.70 (0.31–1.54) | 0.3721 | 0.68 (0.39–1.16) | 0.1562 |
| White, non-Hispanic | Referent | – | Referent | – |
| Education | ||||
| Less than High School | 1.25 (0.83–1.88) | 0.2882 | – | – |
| High School | 1.06 (0.80–1.41) | 0.6934 | – | – |
| College | 1.13 (0.94–1.35) | 0.2023 | – | – |
| Graduate School | Referent | – | – | – |
| Sexual Orientation, n () | ||||
| Bisexual | 1.33 (0.98–1.81) | 0.0645 | 1.19 (0.92–1.53) | 0.1797 |
| Heterosexual/Straight | 0.92 (0.51–1.66) | 0.7776 | 0.72 (0.42–1.23) | 0.2251 |
| Other | 1.28 (0.79–2.07) | 0.3170 | 1.24 (0.78–1.99) | 0.3595 |
| Gay | Referent | – | ||
| Depressive Symptoms | ||||
| Depressive symptoms (CES-D ≥16) | 2.69 (2.31–3.14) | <.0001 | 1.37 (1.18–1.59) | <.0001 |
| No depressive symptoms (CES-D < 16) | Referent | – | Referent | – |
| Employment Status | ||||
| Not Employed | 1.07 (0.91–1.27) | 0.4035 | – | – |
| Employed | Referent | – | – | – |
| Income Category | ||||
| Less than $29,999 | 1.69 (1.38–2.07) | <.0001 | 1.21 (1.00–1.46) | 0.0499 |
| $30,000 to $59,999 | 1.34 (1.06–1.68) | 0.0145 | 1.16 (0.95–1.42) | 0.1373 |
| $60,000 or more | Referent | – | Referent | – |
| Housing Status | ||||
| Somewhere else | 1.34 (1.06–1.69) | 0.0159 | 1.29 (1.05–1.59) | 0.0171 |
| In your own home | Referent | – | Referent | – |
| Marijuana Use, n () | ||||
| Yes | 1.13 (0.94–1.36) | 0.1892 | – | – |
| No | Referent | – | – | – |
| Popper Use, n () | ||||
| Yes | 1.01 (0.83–1.24) | 0.9141 | – | – |
| No | Referent | – | – | – |
| Cocaine/Crack Use, n () | ||||
| Yes | 1.26 (0.94–1.70) | 0.1253 | – | – |
| No | Referent | – | – | – |
| Methamphetamine Use, n () | ||||
| Yes | 1.36 (0.98–1.89) | 0.07 | 1.01 (0.77–1.32) | 0.9638 |
| No | Referent | – | Referent | – |
| Volunteer Work | ||||
| No | 1.06 (0.90–1.26) | 0.4744 | – | – |
| Yes | Referent | – | – | – |
| Alcohol Use | ||||
| Low/Moderate | 0.88 (0.72–1.08) | 0.2142 | – | – |
| Moderate/Heavy | 0.85 (0.64–1.11) | 0.235 | – | – |
| Heavy | 0.85 (0.55–1.32) | 0.4706 | – | – |
| None | Referent | – | – | – |
| Baseline (wave 3) Loneliness | ||||
| Yes (≥6) | 5.73 (4.65–7.06) | <.0001 | 4.74 (3.70–6.07) | <.0001 |
| No (<6) | Referent | – | Referent | – |
5.6. Multivariate associations of social environment latent classes and covariates on loneliness
Compared to Social Connectors, Social Isolates (Prevalence Ratio (PR): 1.42; 95% CI: 1.08–1.88; p = 0.0120) and Non-community Connectors (PR: 1.34; 95% CI: 1.03–1.75; p = 0.0322) were more likely to experience loneliness at wave 6 after adjustment for covariates and baseline loneliness (Table 5). Participants reporting depressive symptoms (vs. no depressive symptoms; PR: 1.37; 95% CI: 1.18–1.59; p < 0.0001), income of less than $29,999 per year (vs $60,000 or more; PR: 1.21; 95% CI 1.00–1.46; p = 0.0499) and living “somewhere else” (vs. living “in your own home; PR:1.29; 95% CI: 1.05–1.59; p = 0.0171) were also more likely to report loneliness.
6. Discussion
Our results were consistent with our original hypothesis and clearly demonstrated that the social environmental resiliencies impacted loneliness among older MSM, even after controlling for covariates and baseline loneliness. Consistent with our main hypothesis, aging MSM who reported a higher level of social support, a higher degree of social bonding, and a stronger psychological sense of community among gay men were less likely to experience loneliness than aging MSM who did not. To our knowledge, this longitudinal study is the first to examine the relationship between loneliness and social environmental resiliencies among older HIV-positive and HIV-negative MSM. We utilized longitudinal latent class analysis to identify mutually exclusive latent classes by modeling indicators of social environment.
Compared to Social Connectors (who reported receiving a lot of social support, had a high degree of social bonding from their networks, and perceived a strong sense of community among gay men), Social Isolates (who lacked social support, had a low degree of social bonding and a weak sense of community) and Non-community Connectors (who were like the first class except that they felt a weak sense of community among gay men) had a higher prevalence of loneliness. These findings corroborate prior studies that examined the relationship between specific social environmental factors and loneliness among older MSM. For example, Kim and Fredriksen-Goldsen et al. (2016) and Grossman (2010) reported that social support accounted for more variance in loneliness than the objective evaluation of social connectedness (e.g., network size). A resilience framework provides a lens through which to examine the psychosocial health and well-being of older MSM. The fact that the majority of MSM in this study maintained and relied on strong social networks that provided high levels of social support and social bonding (both Social Connectors and Non-community Connectors) reflects considerable resilience over time, given the homophobic stigma and discrimination faced by many MSM across their lifetime. These supportive relationships buffered against symptoms of loneliness among these older MSM with and without HIV infection.
Consistent with the literature, social-environmental resiliencies may present differently among non-White and non-gay identifying MSM (Buttram, 2015). Our study findings revealed that there was a larger representation of Social Isolates, compared to Social Connectors and Non-community Connectors, who were non-White, non-gay identifying, and HIV-positive older MSM (Table 5). They received little social support from family, friends, or others, have a low degree of social bonding from their networks, and perceived a weak sense of community among gay men. Social Isolates were also more likely to be unemployed, make less than $29,999 per year, not have gone to college or graduate school, not live in their own home, have depressive symptoms, and report using more alcohol, cocaine/crack, and methamphetamine. This group of older MSM reported experiencing loneliness, operationalized as often lacking companionship, feeling left out, and isolated from others. Interestingly, compared to Social Connectors, fewer non-community Connectors and Social Isolates reported participating in volunteer activities (Table 5). These findings have important implications for interventions designed to promote the development of resilience among this population, including facilitating volunteer opportunities, as discussed further below in the implications section.
6.1. Limitations and strengths of the study
The study has some limitations. First, although the sample size is adequate, we used convenience sampling for our recruitment design, and our sample consists of mostly White, non-Hispanic MSM, thereby reducing the generalizability of our findings. Our study design should, therefore, be replicated with larger, alternative community samples of ethnically/racially diverse older MSM to understand more about loneliness across a heterogeneous group of older MSM. Future studies are needed to explore any differences across the social-environmental resiliencies of non-White and White older MSM and gay and non-gay identifying older MSM. For example, a deeper understanding of how being a Black and non-gay identifying older MSM intertwines in having multiple group memberships, some of which are marginalized and some which are not. These patterns of marginalization and nonmarginalized group memberships may influence the quantity and quality of social networks and the degree of social support one receives from family, friends, coworkers, church members, and others, especially in the context where typically, behaviors or identities associated with being gay are stigmatized. Second, future waves of longitudinal data will allow us to examine how social environmental resiliencies change over time and what factors are associated with maintaining positive social relationships in older age among MSM.
Notwithstanding these limitations, the study also has several strengths. A major strength of this study is that by lagging social environmental factors over time, we were able to examine temporal relationships between latent classes and loneliness. The longitudinal data, therefore, allowed us to make causal inferences related to the social-environmental resiliencies reducing loneliness among older MSM. Our longitudinal study also included HIV-negative older MSM who served as a control group. Furthermore, rather than examining one specific aspect of the social environment, we investigated multidimensional aspects of the social environments (i.e., social support, social bonding, and psychological sense of community among gay men). It is important to note that these social environmental resiliencies were among those identified during the formative phase of this study by a heterogenous group that not only included MSM health researchers and experts, but MSM community members themselves, who chose factors deemed important and relevant to the lives of MSM.
6.2. Implications for practice
Models of successful aging clearly acknowledge the importance of identifying factors that are modifiable through interventions to promote the health and well-being of older adults. By identifying and harnessing the resiliencies already used by some aging MSM to reduce loneliness, we can develop and test interventions to diminish loneliness and promote health among MSM who do not yet have these resiliencies. The results of our study revealed that the symptoms of loneliness among older MSM with and without HIV infection can be buffered by social environmental resiliencies, that is, a highly supportive social network, social bonding with and from a social network, and a strong attachment with the gay male community.
These results provide useful information for the development and testing of individual- and community-level tailored interventions aimed at buffering against loneliness and promoting health among older MSM, especially among MSM who are socially disconnected (like the Social Isolates in this study). As demonstrated in our study, Social Isolates are MSM who lack a supportive social network, lack social bonding from their networks, and have little to no psychological sense of community among gay men. Increased attention needs to be paid to this socially disconnected group who may also experience elevated risks of mental and physical problems but not be able to find necessary support within their social networks. Older HIV-positive and HIV-negative MSM may have different social support networks, given that HIV-positive men have access to a pre-existing support network of HIV/AIDS services and resources.
For the population of older MSM who are living with HIV, a comprehensive tailored approach, incorporating screening for loneliness, psychosocial and mental health assessments, as well as traditional clinical assessments, is necessary to reduce loneliness and improve health outcomes in this growing population. Providers at HIV/AIDS service organizations and other grassroots organizations will need to develop more programs and services (e.g., home visits, day centers that individuals can regularly attend, organized social groups/clubs for MSM) that mitigate loneliness experienced by many older MSM with HIV and help them cope with aging with HIV. Also, it will be crucial to create a supportive community for this population, comprised of other older MSM with HIV who can offer emotional, tangible, and informational support via peer-led education and health communication. Other volunteers from the wider community can also be invited to be part of the support network for aging MSM who are living with HIV. These diverse social networks can provide valuable opportunities for social interaction and engagement, thereby reducing loneliness among this population.
Policymakers must also act to eliminate discriminatory practices and policies against members of the wider lesbian, gay, bisexual, transgender, and queer (LGBTQ) community in different realms including employment, housing, adoption and child custody, and access to quality health care and other services. These harmful practices and policies hinder social integration and can potentially exacerbate loneliness and social isolation. With equal rights and protections, members of LGBTQ can more easily be integrated into their neighborhoods and larger communities, which can also provide resources and serve as sources of emotional and tangible support to reduce loneliness. In addition, policymakers should focus on capacity building and integration of HIV and geriatric service networks. We can learn and generalize from these interventions that aim to protect against loneliness and promote the health of HIV-positive older MSM to HIV-negative aging MSM.
The people most in need of social support and resources are likely the hardest to reach because of their social disconnectedness, which means that as a first step, targeted efforts are needed to identify those lonely individuals through existing social services as well as through new community outreach initiatives. Second, service providers can create a community of support comprised of mentors and volunteers from the MSM community and the community at large, who can offer tangible and emotional support to diminish loneliness. Community activities such as organized social groups/clubs (e.g., book club), volunteer opportunities, and social events for aging MSM would also provide opportunities for social connection.
7. Conclusions
The current study offers evidence for the theoretical and practical significance of social-environmental resiliencies already adopted by many aging MSM with and without HIV to protect against loneliness. These findings can inform the development of potentially efficacious interventions to diminish loneliness among aging MSM. Older MSM are a unique and vulnerable, yet resilient population; leveraging social-environmental resiliencies is key to reducing loneliness and promoting health in this population.
Acknowledgments
This study is funded by the National Institute for Minority Health Disparities [grant R01 MD010680 Plankey & Friedman]. The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH). MWCCS (Principal Investigators): Atlanta CRS (Ighovwerha Ofotokun, Anandi Sheth, and Gina Wingood), U01-HL146241; Baltimore CRS (Todd Brown and Joseph Margolick), U01-HL146201; Bronx CRS (Kathryn Anastos and Anjali Sharma), U01-HL146204; Brooklyn CRS (Deborah Gustafson and Tracey Wilson), U01-HL146202; Data Analysis and Coordination Center (Gypsyamber D’Souza, Stephen Gange and Elizabeth Golub), U01-HL146193; Chicago-Cook County CRS (Mardge Cohen and Audrey French), U01-HL146245; Chicago-Northwestern CRS (Steven Wolinsky), U01-HL146240; Connie Wofsy Women’s HIV Study, Northern California CRS (Bradley Aouizerat, Phyllis Tien, and Jennifer Price), U01-HL146242; Los Angeles CRS (Roger Detels), U01-HL146333; Metropolitan Washington CRS (Seble Kassaye and Daniel Merenstein), U01-HL146205; Miami CRS (Maria Alcaide, Margaret Fischl, and Deborah Jones), U01-HL146203; Pittsburgh CRS (Jeremy Martinson and Charles Rinaldo), U01-HL146208; UAB-MS CRS (Mirjam-Colette Kempf, Jodie Dionne-Odom, and Deborah Konkle-Parker), U01-HL146192; UNC CRS (Adaora Adimora), U01-HL146194. The MWCCS is funded primarily by the National Heart, Lung, and Blood Institute (NHLBI), with additional co-funding from the Eunice Kennedy Shriver National Institute Of Child Health & Human Development (NICHD), National Institute On Aging (NIA), National Institute Of Dental & Craniofacial Research (NIDCR), National Institute Of Allergy And Infectious Diseases (NIAID), National Institute Of Neurological Disorders And Stroke (NINDS), National Institute Of Mental Health (NIMH), National Institute On Drug Abuse (NIDA), National Institute Of Nursing Research (NINR), National Cancer Institute (NCI), National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Institute on Deafness and Other Communication Disorders (NIDCD), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute on Minority Health and Health Disparities (NIMHD), and in coordination and alignment with the research priorities of the National Institutes of Health, Office of AIDS Research (OAR). MWCCS data collection is also supported by UL1-TR000004 (UCSF CTSA), P30-AI-050409 (Atlanta CFAR), P30-AI-050410 (UNC CFAR), and P30-AI-027767 (UAB CFAR).
The authors are indebted to the participants of the Multicenter AIDS Cohort Study [MACS] Healthy Aging Study. The authors thank the staff at the four sites for implementation support John Welty, Montserrat Tarrago, and Katherine McGowan for data support of this study.
References
- Barrera M, Sandler IN, Ramsey TB, 1981. Preliminary development of a scale of social support: studies on college students. Am. J. Community Psychol. 58, 304–309. [Google Scholar]
- Bergman YS, Segel-Karpas D, 2018. Future time perspective, loneliness, and depressive symptoms among middle-aged adults: a mediation model. J. Affect. Disord. 241, 173–175. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, 2003. Social integration, social networks, social support, and health. In: Berkman LF, Kawachi I (Eds.), Social Epidemiology. Oxford University Press, pp. 137–173. [Google Scholar]
- Berkman LF, Syme SL, 1979. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am. J. Epidemiol. 109 (2), 186–204. [DOI] [PubMed] [Google Scholar]
- Buttram ME, 2015. The social environmental elements of resilience among vulnerable African American/Black men who have sex with men. J. Hum. Behav. Soc. Environ. 25 (8), 923–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease, Conatrol, and Prevention, 2016. CDC Fact Sheet: Today’s HIV/AIDS Epidemic. https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/todaysepidemic-508.pdf.
- Cutrona CE, Russell D, Jones WH, Perlman D, 1987. The provisions of social relationships and adaptation to stress. In: Jones WH, Perlman DD (Eds.), Advances in Personal Relationships. JAI Press, pp. 37–67. [Google Scholar]
- De Jesus M, Puleo E, Shelton RC, Emmons KM, 2010. Associations between perceived social environment and neighborhood safety: health implications. Health Place 16, 1007–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Silva MJ, McKenzie K, Harpham T, Huttly SR, 2005. Social capital and mental illness: a systematic review. J. Epidemiol. Community 59, 619–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doménech-Abella J, Lara E, Rubio-Valera M, Olaya B, Moneta MV, Rico-Uribe LA, Ayuso-Mateos JL, Mundó J, Haro JM, 2017. Loneliness and depression in the elderly: the role of social network. Soc. Psychiatr. Psychiatr. Epidemiol. 52 (4), 381–390. [DOI] [PubMed] [Google Scholar]
- Dudley J, Jin S, Hoover D, Metz S, Thackeray R, Chmiel J, 1995. The multicenter AIDS cohort study: retention after 9½ years. Am. J. Epidemiol. 142 (3), 323–330. [DOI] [PubMed] [Google Scholar]
- Fiori KL, Antonucci TC, Cortina KS, 2006. Social network typologies and mental health among older adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 61, 25–32. [DOI] [PubMed] [Google Scholar]
- Ge L, Yap CW, Ong R, Heng BH, 2017. Social isolation, loneliness and their relationship with depressive symptoms: a population-based study. PloS One 12 (8), e0182145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene M, Hessol NA, Perissinotto C, Zepf R, Parrott AH, Foreman C, Whirry R, Gandhi M, Malcolm J, 2018. Loneliness in older adults living with HIV. AIDS Behav. 22 (5), 1475–1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman A, D’Augelli A, Hershberger S, 2000. Social support networks of lesbian, gay, and bisexual adults 60 years of age and older. J. Gerontol. 55B, P171–P179. [DOI] [PubMed] [Google Scholar]
- Henriksen J, Larsen ER, Mattisson C, Andersson NW, 2019. Loneliness, health and mortality. Epidemiol. Psychiatr. Sci. 28 (2), 234–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrick AL, Lim SH, Wei C, Smith H, Guadamuz T, Friedman MS, Stall R, 2011. Resilience as an untapped resource in behavioral intervention design for gay men. AIDS Behav. 15 (Suppl. 1), S25–S29. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D, 2015. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect. Psychol. Sci. 10 (2), 227–237. [DOI] [PubMed] [Google Scholar]
- Holwerda TJ, Deeg DJ, Beekman ATF, van Tilburg TG, Stek ML, Jonker C, Schoevers RA, 2014. Feelings of loneliness, but not social isolation, predict dementia onset: results from the Amsterdam Study of the Elderly (AMSTEL). J. Neurol. Neurosurg. Psychiatr. 85 (2), 135–142. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT, 2004. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res. Aging 26 (6), 655–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs RJ, Kane MN, 2012. Correlates of loneliness in midlife and older gay and bisexual men. J. Gay Lesb. Soc. Serv. 24, 40–61. [Google Scholar]
- Jung T, Wickrama KA, 2008. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass 2 (1), 302–317. [Google Scholar]
- Karpiak SE, Shippy RA, Cantor MH, 2006. Research on Older Adults with HIV. AIDS Community Research Initiative of America, New York. https://www.health.ny.gov/diseases/aids/providers/conferences/docs/roah_final_report.pdf. [Google Scholar]
- Kaslow RA, Ostrow DG, Detels R, Phair JP, Polk BF, Rinaldo CR Jr., 1987. The Multicenter AIDS Cohort Study: rationale, organization, and selected characteristics of the participants. Am. J. Epidemiol. 126 (2), 310–318. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Berkman L, 2000. Social cohesion, social capital, and health. In: Berkman LF, Kawachi I (Eds.), Social Epidemiology. Oxford University Press, pp. 174–190. [Google Scholar]
- Keefe J, Andrew M, Fancey P, Hall M, 2006. May 15). Final report: A Profile of Social Isolation in Canada. Nova Scotia Centre on Aging, Mount Saint Vincent University. https://www.health.gov.bc.ca/library/publications/year/2006/keefe_social_isolation_final_report_may_2006.pdf. [Google Scholar]
- Kim H-J, Fredriksen-Goldsen KI, 2016. Living arrangement and loneliness among lesbian, gay, and bisexual older adults. Gerontol. 56 (3), 548–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyva-Moral JM, Martínez-Batlle F, Vázquez-Naveira M, Hernández-Fernández J, Villar-Salgueiro M, 2019. The experience of growing old while living with HIV in Spain: a phenomenological study. J. Assoc. Nurses AIDS Care 30 (1), 111–118. [DOI] [PubMed] [Google Scholar]
- Li MJ, Hubach RD, Dodge B, 2015. Social milieu and mediators of loneliness among gay and bisexual men in rural Indiana. J. Gay Lesb. Ment. Health 19, 331–346. [Google Scholar]
- Little RJA, 1988. A test of missing completely at random for multivariate data with missing values. J. Am. Stat. Assoc. 83 (404), 1198–1202. [Google Scholar]
- Little RJA, Rubin DB, 1989. The analysis of social science data with missing values. Socio. Methods Res. 18 (2–3), 292–326. [Google Scholar]
- Luchetti M, Terracciano A, Aschwanden D, Lee JH, Stephan Y, Sutin AR, 2020. Loneliness is associated with risk of cognitive impairment in the survey of health, ageing and retirement in europe. Int. J. Geriatr. Psychiatr. 35 (7), 794–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marziali ME, Armstrong HL, Closson K, McLinden T, Wang L, Barath J, Harris M, Roth EA, Moore DM, Lachowsky NJ, Hogg RS, Sang JM, Card KG, 2020. Loneliness and self-rated physical health among gay, bisexual and other men who have sex with men in Vancouver, Canada. J. Epidemiol. Community 74 (7), 553–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, Powell JL, 2003. A resilience framework for research, policy, and practice. In: Luthar SS (Ed.), Resilience and Vulnerability. Cambridge University Press, pp. 1–28. [Google Scholar]
- Mazonson P, Berko J, Loo T, et al. , 2020. Loneliness among older adults living with HIV: the “older old” may be less lonely than the “younger old”. AIDS Care. 10.1080/09540121.2020.1722311. Feb 1–8. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- McMillan DW, Chavis DM, 1986. Sense of community: a definition and theory. J. Community Psychol. 14 (1), 6–23. [Google Scholar]
- Meanley SP, Stall RD, Dakwar O, Egan JE, Friedman MR, Haberlen SA, Okafor C, Teplin LA, Plankey MW, 2019. Characterizing experiences of conversion therapy among middle-aged and older Men who have Sex with Men from the Multicenter AIDS Cohort Study (MACS). Sex. Res. Soc. Pol. 17 (2), 334–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO, 2020. Mplus Version 8.4. Authors, Los Angeles, CA, 2020. [Google Scholar]
- Proescholdbell RJ, Roosa MW, Nemeroff CJ, 2006. Component measures of psychological sense of community among gay men. J. Community Psychol. 34 (1), 9–24. [Google Scholar]
- Radloff LS, 1977. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1 (3), 385–401. [Google Scholar]
- Ramirez-Valles J, 2002. The protective effects of community involvement for HIV risk behavior: a conceptual framework. Health Educ. Res. 17, 389–403. [DOI] [PubMed] [Google Scholar]
- Ramirez-Valles J, Fergus S, Reisen CA, Poppen PJ, Zea MC, 2005. Confronting stigma: community involvement and psychological wellbeing among HIV-positive Latino gay men. Hisp. J. Behav. Sci. 27 (1), 101–119. [Google Scholar]
- Rendina HJ, Weaver L, Millar BM, López-Matos J, Parsons JT, 2019. Psychosocial well-being and HIV-related immune health outcomes among HIV-positive older adults: support for a biopsychosocial model of HIV stigma and health. J. Int. Assoc. Phys. AIDS Care 18, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosario M, Hunter J, Maguen S, Gwadz M, Smith R, 2001. The coming-out process and its adaptational and health-related associations among gay, lesbian, and bisexual youths: stipulation and exploration of a model. Am. J. Community Psychol. 29, 133–160. [DOI] [PubMed] [Google Scholar]
- Russell DW, 1996. UCLA loneliness scale (version 3): reliability, validity and factor structure. J. Pers. Assess. 66 (1), 20–40. [DOI] [PubMed] [Google Scholar]
- Russell DW, Cutrona CE, 1984. Social Provisions Scale. Iowa State University Press. [Google Scholar]
- Russell GM, Richards JA, 2003. Stressor and resilience factors for lesbians, gay men, and bisexuals confronting antigay politics. Am. J. Community Psychol. 31 (3–4), 313–328. [DOI] [PubMed] [Google Scholar]
- SAS, 2014. Version 9.4. SAS Institute Inc, Cary, NC. [Google Scholar]
- Schnittker J, 2007. Look (closely) at all the lonely people: age and the social psychology of social support. J. Aging Health 19, 659–682. [DOI] [PubMed] [Google Scholar]
- Shao B, Song B, Feng S, Lin Y, Du J, Shao H, Chi Z, Yang Y, Wang F, 2018. The relationship of social support, mental health, and health-related quality of life in human immunodeficiency virus-positive men who have sex with men: from the analysis of canonical correlation and structural equation model: a cross-sectional study. Medicine 97 (30), e11652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidi Y, Harel O, 2018. The treatment of incomplete data: reporting, analysis, reproducibility, and replicability. Soc. Sci. Med. 209, 169–173. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Shankar A, Demakakos P, Wardle J, 2013. Social isolation, loneliness, and all-cause mortality in older men and women. Proc. Natl. Acad. Sci. U.S.A. 110 (15), 5797–5801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su X, Zhou AN, Li J, Shi L, Huan X, Yan H, Wei C, 2018. Depression, loneliness, and sexual risk-taking among HIV-negative/unknown men who have sex with men in China. Arch. Sex. Behav. 47, 1959–1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, Stephan Y, Luchetti M, Terracciano A, 2018. Loneliness and risk of dementia. J. Gerontol. B Psychol. Sci. Soc. Sci. 75 (7), 1414–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tein JY, Coxe S, Cham H, 2013. Statistical power to detect the correct number of classes in latent profile analysis. Struct. Equ. Model. 20 (4), 640–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valtorta NK, Kanaan M, Gilbody S, Hanratty B, 2018. Loneliness, social isolation and risk of cardiovascular disease in the English Longitudinal Study of Ageing. European Journal of Preventive Cardiology 25 (13), 1387–1396. [DOI] [PubMed] [Google Scholar]
- van Ginkel JR, Linting M, Rippe RC, van der Voort A, 2020. Rebutting existing misconceptions about multiple imputation as a method for handling missing data. J. Pers. Assess. 102 (3), 297–308. [DOI] [PubMed] [Google Scholar]
- Xia N, Li H, 2018. Loneliness, social isolation, and cardiovascular health. Antioxidants Redox Signal. 28 (9), 837–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang R, Wang H, Edelman LS, Tracy EL, Demiris G, Sward KA, Donaldson GW, 2020. Loneliness as a mediator of the impact of social isolation on cognitive functioning of Chinese older adults. Age Ageing 49 (4), 599–604. [DOI] [PubMed] [Google Scholar]
- Yates TM, Masten AS, 2004. Fostering the future: resilience theory and the practice of positive psychology. In: Linley PA, Joseph S (Eds.), Positive Psychology in Practice. Wiley, pp. 521–539. [Google Scholar]
- Yeh S, Lo S, 2004. Living alone, social support, and feeling lonely among the elderly. SBP (Soc. Behav. Pers.) 32, 129–138. [Google Scholar]
- Yoo-Jeong M, Hepburn K, Holstad M, Haardörfer R, Waldrop-Valverde D, 2019. Correlates of loneliness in older persons living with HIV. AIDS Care 32 (7), 869–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziersch AM, Baum FE, Macdougall C, Putland C, 2005. Neighbourhood life and social capital: the implications for health. Soc. Sci. Med. 60 (1), 71–86. [DOI] [PubMed] [Google Scholar]