Abstract
Objective/Background:
Over the past decade, multidisciplinary “toe and flow” programs have gained great popularity, with proven benefits in limb salvage. Many vascular surgeons have incorporated podiatrists into their practices. The viability of this practice model requires close partnership, hospital support, and financial sustainability. We intend to examine the economic values of podiatrists in a busy safety-net hospital in the Southwest United States.
Methods:
An administrative database that captured monthly operating room (OR) cases, clinic encounters, in-patient volume, and total work relative value units (wRVUs) in an established limb salvage program in a tertiary referral center were examined. The practice has a diverse patient population with >30% of minority patients. During a period of 3 years, there was a significant change in the number of podiatrists (from 1 to 4) within the program, whereas the clinical full-time employees for vascular surgeons remained relatively stable.
Results:
The limb salvage program experienced >100% of growth in total OR volumes, clinic encounters, and total wRVUs over a period of 4 years. A total of 35,591 patients were evaluated in a multidisciplinary limb salvage clinic, and 5535 procedures were performed. The initial growth of clinic volume and operative volume (P < .01) were attributed by the addition of vascular surgeons in year one. However, recruitment of podiatrists to the program significantly increased clinic and OR volume by an additional 60% and >40%, respectively (P < .01) in the past 3 years. With equal number of surgeons, podiatry contributed 40% of total wRVUs generated by the entire program in 2019. Despite the fact that that most of the foot and ankle procedures that were regularly performed by vascular surgeons were shifted to the podiatrists, vascular surgeons continued to experience an incremental increase in operative volume and >10% of increase in wRVUs.
Conclusions:
This study shows that the value of close collaboration between podiatry and vascular in a limb salvage program extends beyond a patient’s clinical outcome. A financial advantage of including podiatrists in a vascular surgery practice is clearly demonstrated.
Keywords: Diabetes, Economic, Financial, Limb salvage, Multidisciplinary
Peripheral arterial disease (PAD) affects approximately 8.5 million Americans older than 40 years of age and more than 20% of octogenarians.1 PAD is more prevalent among diabetics, up to 20-fold higher, compared with non-diabetics.2 Twenty-five percent of people with diabetes will have a diabetic foot ulcer (DFU) in their life-time.3 Even with advances in limb salvage techniques and wound care products, many of these patients with DFUs are faced with the possibility of a lower extremity amputation, and patients with critical limb-threatening ischemia are at the highest risk for limb loss. The 5-year mortality rate with a major amputation in patients with diabetes exceeds 70%.4,5
There are several models to provide focused integrated foot care that have shown to be beneficial in limb salvage.6 One such model is “toe and flow,” which integrates vascular surgery and podiatric surgery to deliver care. The idea is that podiatrists will screen diabetic patients and work as a “gatekeeper” if there are any risk factors for ulcer, infection, or ischemia and triage the patient to the appropriate specialty. A number of other disciplines are also involved in these models including internal medicine, infectious disease, and plastic and orthopedic surgery as well as orthotists and wound nurse care.
The integrated multidisciplinary team approach as a means to provide integrated foot care reduces amputation by 49% to 85%.7–9 Consequently, the “toe and flow” model has been adapted by many limb salvage practices. However, the success of a “toe and flow” team requires close partnership, hospital support, and financial sustainability. The financial viability of including podiatry in a vascular surgery practice remains unclear. This study is to evaluate the economic values of podiatric surgeons in an established limb salvage program of a busy safety-net hospital in the Southwest United States that has a large underprivileged population with a high prevalence of patients with diabetes.
METHODS
During a period of 5 years, there was a significant fluctuation in the composition of the Southern Arizona Limb Salvage Alliance (SALSA), an established integrated “toe and flow” team. Although there was an incremental increase in the number of vascular surgeons from 2 in 2015 and 2016 to a full complement of 4 in 2018, the clinical full-time employee (cFTE) remained relatively stable. The podiatry cFTE, however, changed from 1 in 2017 to 4 in 2019, and 50% of podiatric surgeons have advanced foot and ankle training for complex hindfoot surgeries. We evaluated an administrative database that captured monthly clinic visits, surgery volume, and inpatient volume from 2015 to 2019 in the vascular surgery department. Monthly total charges billed in the podiatry and vascular surgery service were also evaluated from 2015 to 2019. We looked at work relative value unit (wRVU) of vascular and podiatry surgery from 2016 to 2019. The administrative database does not contain patient information, procedural types, or date of service, and therefore was exempted from Institutional Review Board. Analysis of variance (ANOVA) was used to compare monthly volumes and charges over a period of 5 years. The Tukey multiple comparison test was used for individual comparison. A P-value of <.05 was considered significant.
SALSA team practice model.
For outpatient evaluation, vascular surgeons, podiatrists, and vascular lab are co-located in the same clinic area. At least 1 vascular and 1 podiatric surgeon are available at any given clinic time 5 days a week. For those patients who are scheduled to have both vascular and podiatry evaluations, both surgeon partners will evaluate the patients at the same time under a separate encounter. For those patients who did not anticipate a SALSA evaluation, but when it was determined to be necessary, the partner surgeon will examine the patients at the same time without re-locating the patients, and a separate clinic encounter will be generated to capture the workload. For inpatient consultation, podiatric surgeons are the initial consultants for any foot pathologies. The majority of podiatric cases are for limb salvage and wound care. Reconstructive hindfoot surgery by the SALSA team has been limited to diabetic foot pathology and performed by two of the podiatric surgeons (A.M.R., N.P.) who have formal foot/ankle trainings. Over the period of 4 years, we have established a collaborative agreement with the orthopedic department and shared podiatric emergencies. The SALSA team evaluates the majority of DFU-related pathologies, with 50% of foot infection calls in one hospital and 100% in the other, whereas orthopedic surgeons are fully responsible for trauma-related foot pathologies. Vascular surgeons are involved if there is a concern for poor healing or inadequate blood flow. Patient are co-managed by the SALSA team, and surgeries are coordinated between members of the team.
RESULTS
A total of 35,591 patient encounters in the SALSA clinic and 5535 operative procedures were performed during the period of 5 years. The entire department experienced >100% of growth in clinic visits, operative cases, and total wRVU by 2019 compared with 2015 (P < .01; Table). With the equal number of podiatric and vascular surgeons in 2019, podiatry contributes to 40% of total OR cases and in-patient encounters, as well as 70% of clinic encounters.
Table.
Yearly clinic encounters, OR cases, wRVUs, and inpatient consultations from 2015 to 2019
| Total numbers | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|---|---|---|---|---|
| Podiatrists, No. (cFTE) | 2 (1.6) | 3 (2.6) | 1 (0.9) | 3 (2.8) | 4 (3.8) |
| Vascular surgeons, No. (cFTE) | 2 (1.6) | 2 (1.6) | 4 (2.1) | 4 (2.6) | 4 (2.2) |
| Clinic encounters, No. | 4446 | 5723 | 7302 | 7452 | 11,724 |
| OR cases, No. | 839 | 861 | 1045 | 1151 | 1639 |
| wRVUs, No. | 19,810 | 21,780 | 27,096 | 31,844 | 43,227 |
| Inpatient consultations, No. | 1854 | 2757 |
cFTE, Clinical full-time employee; OR, operating room; SALSA, Southern Arizona Limb Salvage Alliance; wRVUs, work relative value units. From 2015 to 2019, the number of SALSA podiatrists fluctuated between 1 and 4.
The initial significant growth of clinic volume was driven by the addition of podiatrists and vascular surgeons in 2016 and 2017, respectively. Although the podiatry clinic volume was maintained during 2017 with the help of an outpatient Locum tenens podiatrist, the vascular surgery clinic volume experienced significant growth (Fig 1). The recruitment of podiatrists accelerated the growth trajectory of clinic volumes in 2019. Fig 1 depicts monthly clinic encounters from 2015 to 2019 for SALSA-Podiatry (Mean ± standard deviation [SD]: 120 ± 74, 332 ± 74, 380 ± 127, 366 ± 119, and 687 ± 154, respectively) and SALSA-Vascular (Mean ± SD: 298 ± 172, 145 ± 17, 229 ± 32, 255 ± 35, and 283 ± 42, respectively). In addition to outpatient clinic encounters, there was a significant increase in the in-patient consultation captures in 2019 compared with 2018 (podiatry: 99 ± 35 vs 32 ± 31 monthly; P < .01; vascular: 131 ± 37 vs 123 ± 30; P = NS), primarily driven by podiatric practice.
Fig 1.
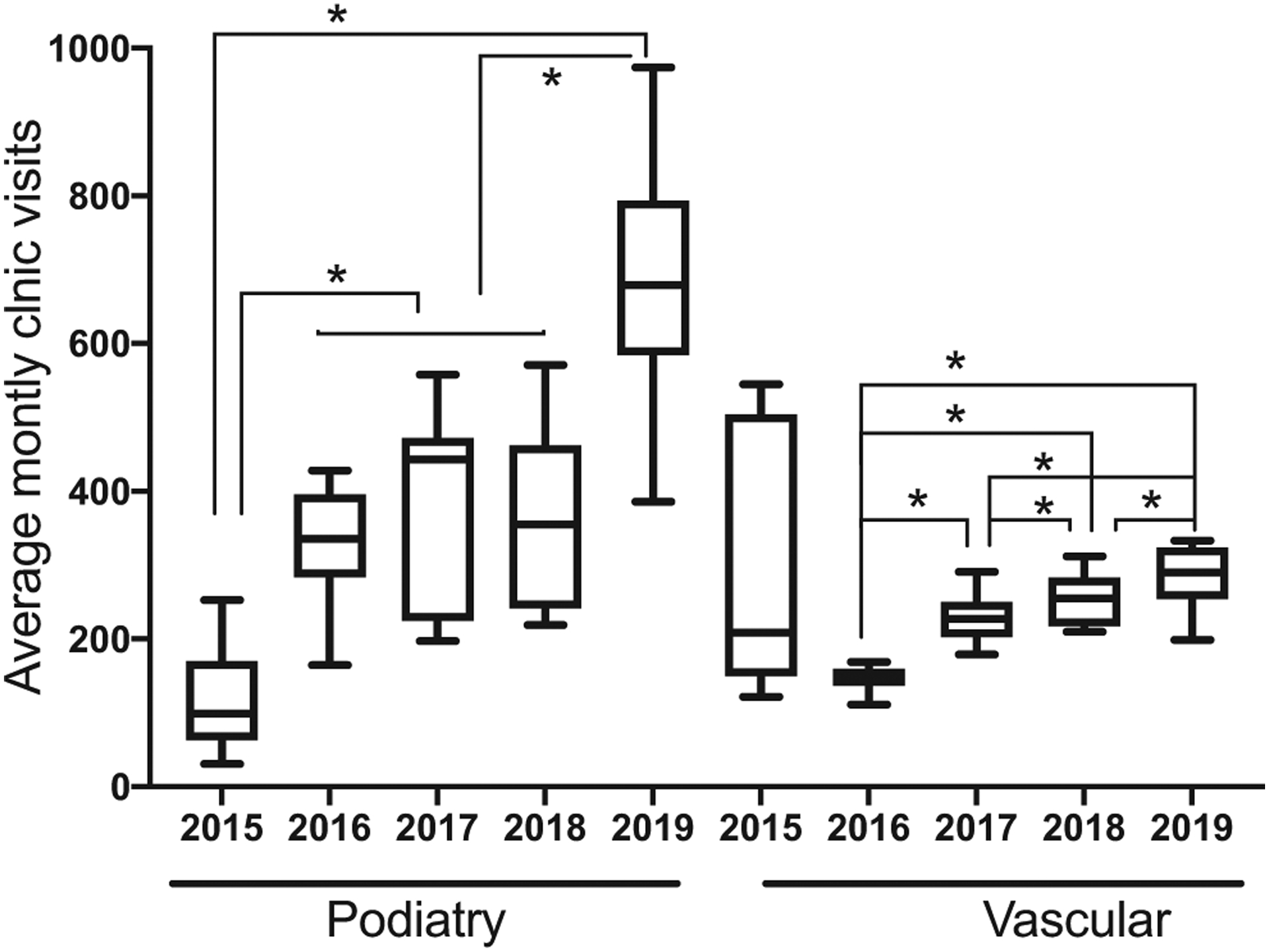
Average monthly clinic encounters shown in box and whiskers plot. The Southern Arizona Limb Salvage Alliance (SALSA) podiatry team had significant clinic volume growth in 2019 when the full complements of 4 podiatrists were recruited. The SALSA vascular team had significant (P < .05) yearly growth in outpatient clinic encounters since 2016. *P < .05.
OR volume nearly doubled over the period of 5 years (Fig 2). The initial significant growth was driven by the addition of vascular surgeons in 2017 compared with 2016 (vascular monthly mean ± SD: 66 ± 16 vs 37 ± 4; P < .01). The vascular OR volume continue to grow, albeit insignificantly, in 2018 and 2019 (monthly mean ± SD: 73 ± 12 and 79 ± 9) despite that minor amputations and procedures related to foot wounds were shifted to the new podiatrists. With the recruitment of the podiatrists, podiatric procedures doubled in 2019 and contributed to 40% of total OR volumes.
Fig 2.
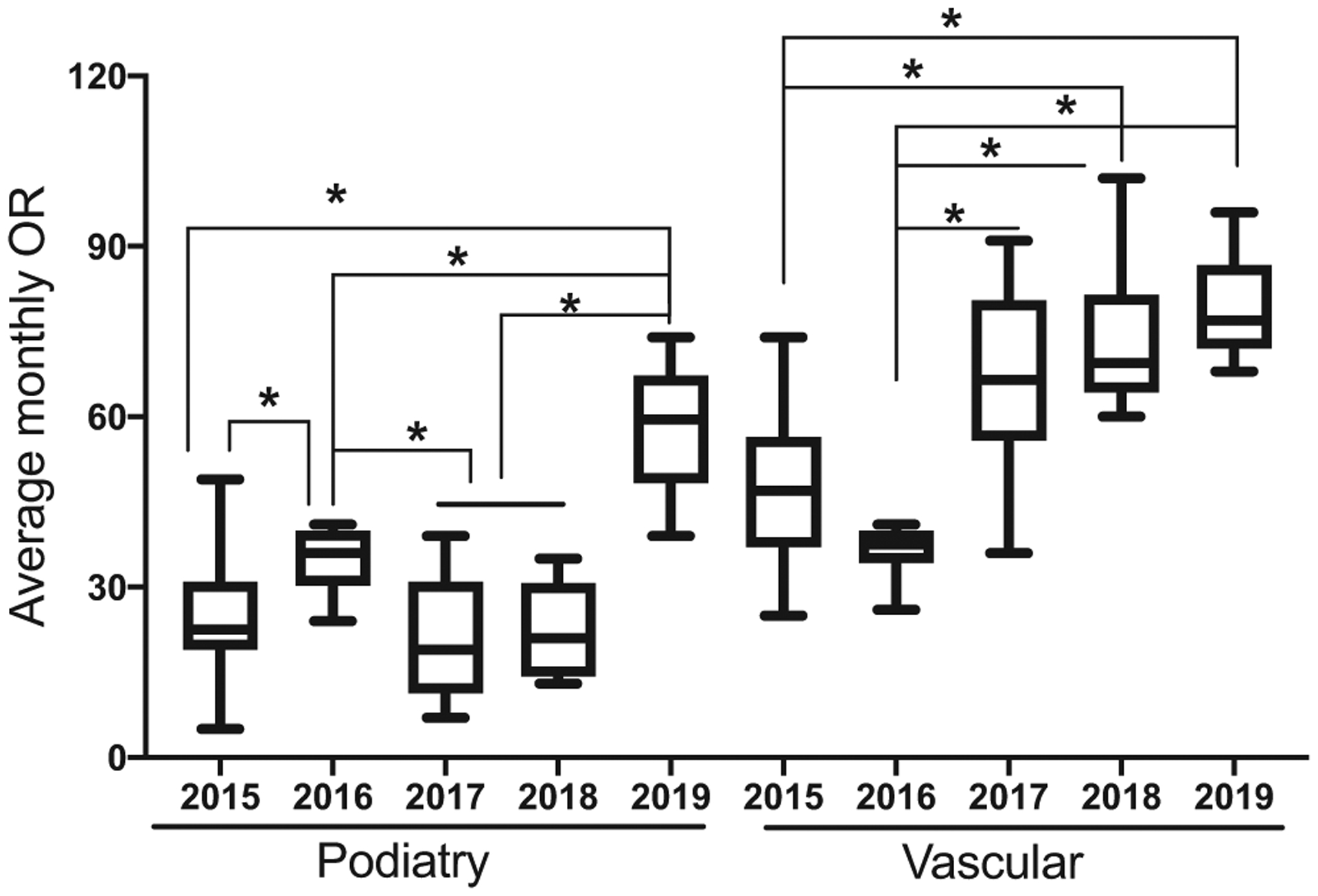
Box and whiskers plot showing mean monthly operating room (OR) cases performed by the Southern Arizona Limb Salvage Alliance (SALSA) team. There was a significant growth in vascular OR volume in 2017 and a steady increase at an average of 10% per year. Podiatry OR experienced a loss that coincided with loss of podiatrists, but had a significant growth in 2019. *P < .05.
Total annual wRVUs generated by the surgeons was 19,810 in 2015 and significantly increased to 43,227 in 2019 (P < .001; Fig 3). Similar to the change patterns of OR volumes and clinical encounters, the podiatry team had a significant increase in wRVUs in 2017 to 2018 compared with 2015, and a further increase in 2019 compared with the previous years (P < .01). Vascular wRVUs were significantly higher from 2017 to 2019 compared with 2016 (P < .01) and continued to have a 10% to 25% increase per year since 2017. By 2019, podiatry contributed to 40% of total wRVUs generated by the SALSA program. The total charges by the SALSA team in 2015 was $4.7 million, and this increased to $7.5 million in 2019. There was also an increase in hospital contribution margin even with the addition of provider salary supports (Fig 4), and the salary payment reflects a productivity (wRVU)-based compensation model. Although the charges by vascular surgeons were relatively stable since 2017, there was a significant increase in the charges generated by the podiatric surgeons (P < .01). By 2019, podiatry accounted for 40% of the total charges from the team.
Fig 3.
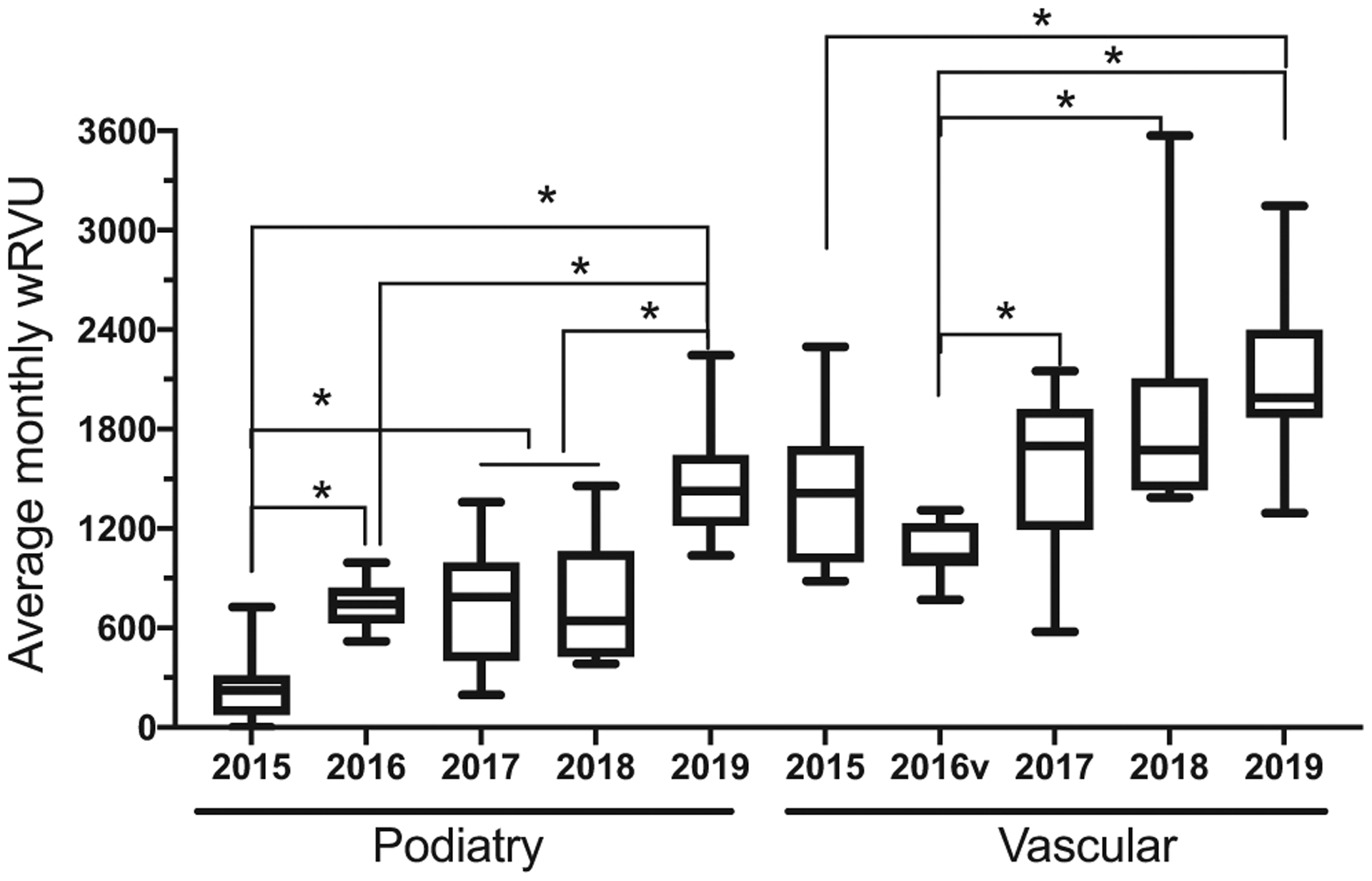
Box and whisker plot shows monthly average work relative value units (wRVUs) generated by podiatry and vascular teams. The podiatry team had a significant increase in wRVUs in 2016 to 2018 compared with 2015, and a further increase in 2019 compared with the previous years. Vascular wRVUs were significantly higher from 2017 to 2019 compared with 2016 and continued to have a 10% to 25% increase per year since 2017. *P < .05.
Fig 4.
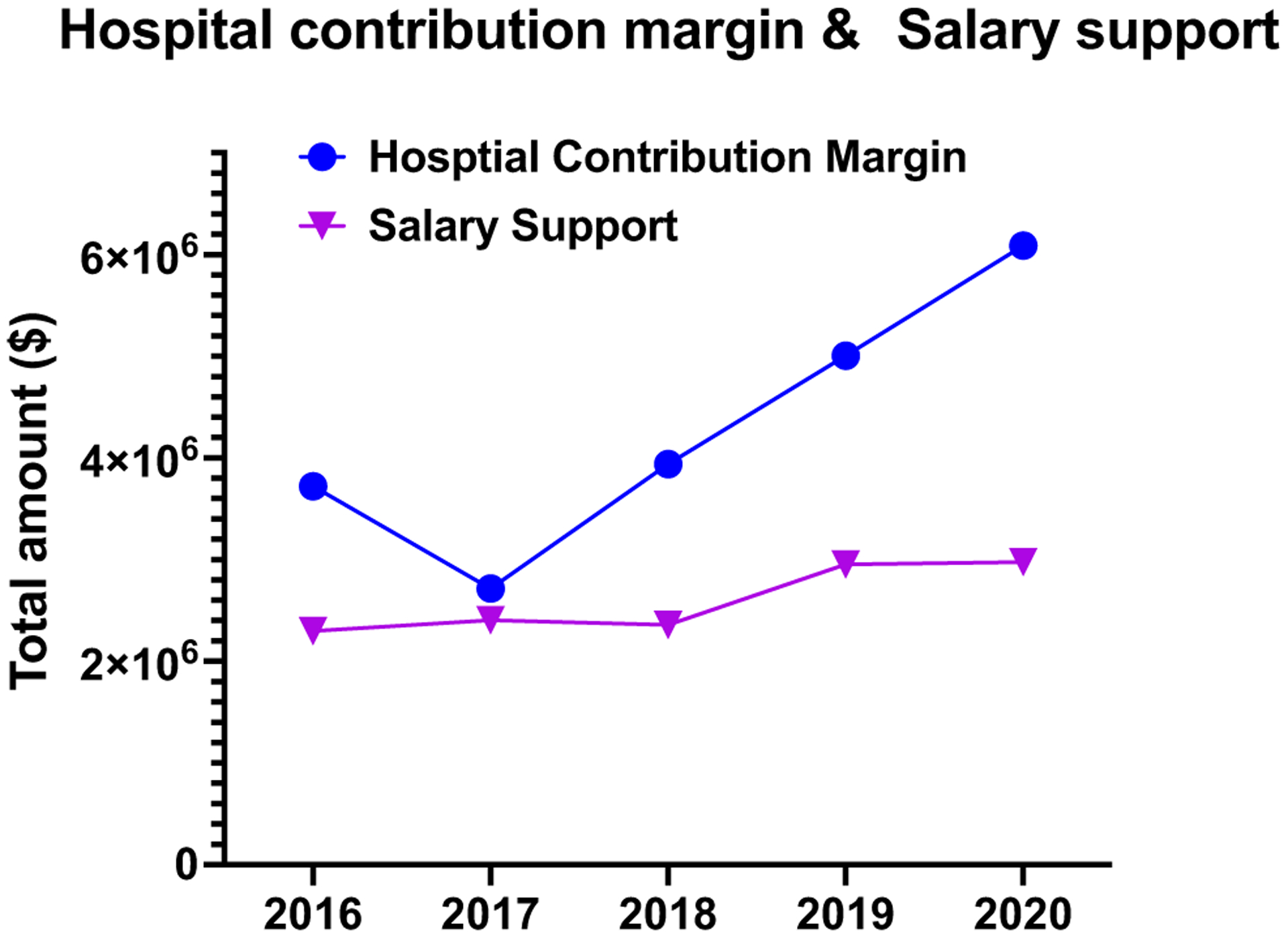
Line graph depicts hospital contribution margin and total provider salary support from 2016 to 2020.
DISCUSSION
Podiatry plays a central role in DFU prevention and limb preservation.7 Many systematic reviews have shown that multidisciplinary teams have lower major amputation rates10–12 as well as the clinical benefits of a podiatrist in a diabetic limb salvage team.13–16 In our SALSA “toe and flow” model, podiatric surgeons are recruited into a vascular surgery division. We have previously showed that this alliance has improved clinical outcomes and decreased lower extremity amputations.17 This study highlighted the financial benefit of including podiatry in a limb salvage team. To the best of our knowledge, this is the first study that describes the impact of podiatric surgeons on the volume of a “toe and flow” team.
Several studies have highlighted the economic value of podiatric physicians in treating DFU. One such study has shown that commercially insured patients would have an average cost savings of nearly $20K if they saw a podiatrist annually.18 Sloan et al showed that podiatric medicine involvement was associated with reduced downstream expenditures and lower incidence of amputation in Medicare patients with diabetes.19 Given the significant socioeconomic burden of DFU,20 the gatekeeper role of podiatrists in routine foot care and early management of DFU becomes ever more important. In addition to the values added to patient care and the health care system, this study clearly outlines the economic value of podiatrists to a limb salvage team in a multidisciplinary practice. The significant increase in clinical volume reflects a growing and sustainable limb salvage practice.
Although the “toe and flow” model has gained popularity, many limb salvage practices are still hesitant to recruit podiatrists. Concern for expenses, call coverage, and volume loss may contribute to the barriers. We observed continuous clinic and OR volume expansion among vascular surgeons despite an addition of podiatric surgeons from 1 to 4. As expected, wound debridement and minor amputations have largely been performed by the podiatry surgery service (data not shown), but despite this shift of procedures away from vascular surgeons, there was a significant increase in vascular and endovascular procedures over the years. We attribute this increase to the overall volume increase and increase in screening by our podiatry colleagues for PAD. Podiatrists can help to screen patients in a limb salvage team and triage the patients to appropriate service lines. This practice reduces some burden of patient screening by other service lines including vascular surgery, which frees up resources for vascular surgeons to take care of vascular conditions that may lead to higher wRVUs and OR volume. In fact, the addition of podiatrists has led to an increase in elective podiatry procedures including preventative foot surgery in diabetic patient population.
Admittedly, financial profitability is difficult to assess due to multiple factors, such as payer-mix index, accuracy of coding and coding capture, and downstream revenues. Like all physicians, the podiatrists are compensated based on clinical productivity and the fair market value deemed by the health care system, which is determined from the results of various physician compensation surveys, such as SullivanCotter, Medical Group Management Association, and American Medical Group Association. There is a persistent increase in the hospital contribution margin since 2017. Although the growth of the hospital contribution margin is disproportionally higher than the growth in salary support, other expenses related to the practice plan are not included. There are also several other limitations related to the studies. We focused on the economic values of podiatrists in a limb salvage practice. Although the clinical benefits of including podiatrists in our limb salvage practice have been shown,17 we did not evaluate the clinical outcomes in this study. Patient satisfaction and quality of life were not examined either. In addition, we did not separate foot and ankle procedures that could have been performed by vascular surgeons if there were no podiatrist to accurately reflect the number of OR cases being shifted away from vascular surgeons. However, the overall OR volumes were significantly increased for both vascular surgeons and podiatric surgeons with the addition of podiatric surgeons. The ability to continue expanding the team highlighted the profitability of the program and pragmatic growth.
CONCLUSIONS
In conclusion, DFUs and PAD are complex pathologies that require a team approach to achieve optimal outcomes. This study shows that the value of close collaboration between podiatry and vascular in a limb salvage program extends beyond a patient’s clinical outcome and that a “toe and flow” model is financially viable for a hospital system. This study contributes to the paucity of literature that helps to justify podiatric recruitment in a health care system.
ARTICLE HIGHLIGHTS.
Type of Research: Retrospective, observational
Key Findings: There is a significant economic advantage of including podiatrists in a vascular surgery practice in a safety-net hospital with a large portion of underprivileged population. Recruitment of podiatrists contributed to >100% growth of the practice. With an equal number of podiatric and vascular surgeons, podiatry contributes 40% of total operating room and in-patient volumes, and 70% of clinic volumes.
Take Home Message: The value of close collaboration between podiatry and vascular in a limb salvage program extends beyond a patient’s clinical outcome, and a “toe and flow” model is financially viable for a hospital system.
Footnotes
Presented at the Thirty-fifth Annual Meeting of the Western Vascular Society, Santa Monica, Calif, September 26–29, 2020.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
REFERENCES
- 1.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. ; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation 2020;141: e139–596. [DOI] [PubMed] [Google Scholar]
- 2.Olinic DM, Spinu M, Olinic M, Homorodean C, Tataru DA, Liew A, et al. Epidemiology of peripheral artery disease in europe: VAS educational paper. Int Angiol 2018;37:327–34. [DOI] [PubMed] [Google Scholar]
- 3.Apelqvist J, Larsson J. What is the most effective way to reduce incidence of amputation in the diabetic foot? Diabetes Metab Res Rev 2000;16(Suppl 1):S75–83. [DOI] [PubMed] [Google Scholar]
- 4.Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med 2017;376:2367–75. [DOI] [PubMed] [Google Scholar]
- 5.Robbins JM, Strauss G, Aron D, Long J, Kuba J, Kaplan Y. Mortality rates and diabetic foot ulcers: is it time to communicate mortality risk to patients with diabetic foot ulceration? J Am Podiatr Med Assoc 2008;98:489–93. [DOI] [PubMed] [Google Scholar]
- 6.Rogers LC, Andros G, Caporusso J, Harkless LB, Mills JL Sr, Armstrong DG. Toe and flow: essential components and structure of the amputation prevention team. J Vasc Surg 2010;52:23S–7S. [DOI] [PubMed] [Google Scholar]
- 7.Kim PJ, Attinger CE, Evans KK, Steinberg JS. Role of the podiatrist in diabetic limb salvage. J Vasc Surg 2012;56:1168–72. [DOI] [PubMed] [Google Scholar]
- 8.van Acker K, Leger P, Hartemann A, Chawla A, Siddiqui MK. Burden of diabetic foot disorders, guidelines for management and disparities in implementation in Europe: a systematic literature review. Diabetes Metab Res Rev 2014;30:635–45. [DOI] [PubMed] [Google Scholar]
- 9.Driver VR, Goodman RA, Fabbi M, French MA, Andersen CA. The impact of a podiatric lead limb preservation team on disease outcomes and risk prediction in the diabetic lower extremity: a retrospective cohort study. J Am Podiatr Med Assoc 2010;100:235–41. [DOI] [PubMed] [Google Scholar]
- 10.Albright RH, Manohar NB, Murillo JF, Kengne LAM, Delgado-Hurtado JJ, Diamond ML, et al. Effectiveness of multidisciplinary care teams in reducing major amputation rate in adults with diabetes: a systematic review & meta-analysis. Diabetes Res Clin Pract 2020;161: 107996. [DOI] [PubMed] [Google Scholar]
- 11.Buggy A, Moore Z. The impact of the multidisciplinary team in the management of individuals with diabetic foot ulcers: a systematic review. J Wound Care 2017;26:324–39. [DOI] [PubMed] [Google Scholar]
- 12.Musuuza J, Sutherland BL, Kurter S, Balasubramanian P, Bartels CM, Brennan MB. A systematic review of multidisciplinary teams to reduce major amputations for patients with diabetic foot ulcers. J Vasc Surg 2020;71:1433–46.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Canavan RJ, Unwin NC, Kelly WF, Connolly VM. Diabetes- and nondiabetes-related lower extremity amputation incidence before and after the introduction of better organized diabetes foot care: continuous longitudinal monitoring using a standard method. Diabetes Care 2008;31:459–63. [DOI] [PubMed] [Google Scholar]
- 14.Litzelman DK, Slemenda CW, Langefeld CD, Hays LM, Welch MA, Bild DE, et al. Reduction of lower extremity clinical abnormalities in patients with non-insulin-dependent diabetes mellitus. A randomized, controlled trial. Ann Intern Med 1993;119:36–41. [DOI] [PubMed] [Google Scholar]
- 15.Lavery LA, Wunderlich RP, Tredwell JL. Disease management for the diabetic foot: effectiveness of a diabetic foot prevention program to reduce amputations and hospitalizations. Diabetes Res Clin Pract 2005;70:31–7. [DOI] [PubMed] [Google Scholar]
- 16.Patout CA Jr, Birke JA, Horswell R, Williams D, Cerise FP. Effectiveness of a comprehensive diabetes lower-extremity amputation prevention program in a predominantly low-income African-American population. Diabetes Care 2000;23:1339–42. [DOI] [PubMed] [Google Scholar]
- 17.Armstrong DG, Bharara M, White M, Lepow B, Bhatnagar S, Fisher T, et al. The impact and outcomes of establishing an integrated interdisciplinary surgical team to care for the diabetic foot. Diabetes Metab Res Rev 2012;28:514–8. [DOI] [PubMed] [Google Scholar]
- 18.Carls GS, Gibson TB, Driver VR, Wrobel JS, Garoufalis MG, Defrancis RR, et al. The economic value of specialized lower-extremity medical care by podiatric physicians in the treatment of diabetic foot ulcers. J Am Podiatr Med Assoc 2011;101:93–115. [DOI] [PubMed] [Google Scholar]
- 19.Sloan FA, Feinglos MN, Grossman DS. Receipt of care and reduction of lower extremity amputations in a nationally representative sample of U.S. elderly. Health Serv Res 2010;45:1740–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet 2005;366:1719–24. [DOI] [PubMed] [Google Scholar]


