Abstract
HIV testing efforts increased in recent years to reduce the percentage of persons with HIV unaware of their infection and to detect HIV early. An analysis of CD4 data from national HIV surveillance indicates that diagnosis delays decreased during 2003-2011; on average, persons diagnosed in 2011 had been infected 5.6 years before their diagnosis compared with 7.0 years among those diagnosed in 2003. Diagnosis delays were longer among females, blacks, Hispanics/Latinos, and younger persons, but shorter among men who have sex with men, compared with their counterparts. Continued efforts to implement routine testing can help reduce diagnosis delays.
Across the United States, HIV testing efforts have increased in recent years to reduce the percentage of persons with HIV unaware of their infection and to detect HIV at earlier stages of disease.1 Persons aware of their HIV infection are less likely to transmit the virus and can enter HIV care to reduce morbidity and mortality.2 As a result of increased testing, the percentage of persons living with HIV aware of their infection has steadily increased over the years and an estimated 84% of persons living with HIV at the end of 2010 were aware of their infection.3 Early detection of HIV coupled with HIV care and treatment to achieve viral suppression enhances preservation of immune function and also reduces the potential transmission of the virus.4 However, while some jurisdictions have observed an increase in the mean CD4 count at diagnosis in recent years possibly indicating earlier detection of HIV5, overall about 25% of the persons newly diagnosed with HIV in 2011 were diagnosed with advanced disease (stage 3, AIDS, primarily based on CD4 <200 cells/μL as well as opportunistic illness).3 Actual delays between infection and HIV diagnosis have not been measured. We used data from the Centers for Disease Control and Prevention’s (CDC) National HIV Surveillance System to estimate the date of infection among persons diagnosed with HIV in 2003 through 2011 aged 13 years and older.
Based on the results of the first CD4 tests after HIV diagnosis reported to CDC through the end of 2012, and a CD4 depletion model for estimating the progression of HIV disease6,7, we determined the distribution of delay from HIV infection to HIV diagnosis. HIV is reportable in all 50 states and the District of Columbia. However, HIV reporting was implemented in the different jurisdictions over time and not all jurisdictions had complete reporting of initial CD4 test results during the years of interest. Therefore, we used data from 33 jurisdictions that had CD4 information within 3 months of HIV diagnosis on at least 50% of persons diagnosed each year, or where at least 85% of persons diagnosed during the entire time period had CD4 information by end of 2012. We modeled the delay between infection and diagnoses using CD4 data reported from the 33 jurisdictions (which represent about 60% of cases diagnosed in the United States during 2003-2011).
To account for cases without CD4 test results, we assigned a weight to each case with CD4 test information based on the proportion of cases with CD4 test results in each stratum, where the stratum is defined by year of diagnosis and status (ever diagnosed with AIDS, HIV death without AIDS, alive without AIDS diagnosis) at the end of 2011. The weight is simply the reciprocal of the proportion. To account for cases in the other 18 states without complete CD4 data, we extended the weight to each case with CD4 test information in the 33 jurisdictions based on the proportion of cases in the 33 jurisdictions to those in all states within each stratum, where the stratum is defined by year of diagnosis, sex, race/ethnicity, transmission category, and age at diagnosis. The reciprocal of this proportion multiplied by the previous weight gives the extended weight. The extended weight is then combined with the adjustment weights for delays in reporting of HIV diagnoses and for missing information on risk factors.8 The final weight is then used to model the delay from HIV infection to HIV diagnosis based on the first CD4 test results and the CD4 depletion model. We determined the mean and median number of years infected at the time of HIV diagnosis for cases diagnosed in each of the 9 years 2003-2011 and the overall cumulative distributions of diagnosis delay (from infection to diagnosis) by year of diagnosis.
On average, persons diagnosed with HIV infection in 2011 had been infected 5.6 years (95% confidence interval [CI] 5.5, 5.6) before their HIV diagnosis (median, 3.6 years) (Table). Males, in particular males with infection attributed to male-to-male sexual contact (men who have sex with men, MSM), had shorter delays between infection and diagnosis compared with females or compared with persons with infection attributed to other risk factors. Delays in diagnosis were longer among blacks/African Americans (hereinafter referred to as black) (5.8 years, 95% CI 5.7, 5.9) and Hispanic or Latinos (5.8 years, 95% CI 5.6, 6.0) compared with whites (5.0 years, 95% CI 4.9, 5.2) and among older persons compared with younger persons (e.g., 6.8 years among persons aged 55 years or older at diagnosis vs. 3.9 years among those aged 13-24 years).
Table.
Number of years infected at the time of HIV diagnosis in 2003 and 2011, United States
| 2003 | 2011 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CD4 at diagnosis |
Number of years infected at time of diagnosis |
CD4 at diagnosis |
Number of years infected at time of diagnosis |
Percentage change |
|||||||||
| Mean | Median | Mean | 95% CI | Mean | Median | Mean | 95% CI | Mean | 95% CI | ||||
| Total | 325 | 5.4 | 7.0 | 6.9, | 7.1 | 395 | 3.6 | 5.6 | 5.5, | 5.6 | −20.7 | −22.2 | −19.3 |
| Transmission category | |||||||||||||
| Male | 320 | 5.2 | 6.8 | 6.7, | 6.9 | 391 | 3.5 | 5.4 | 5.3, | 5.5 | −20.8 | −22.4 | −19.1 |
| Male-to-male sexual contact | 336 | 4.5 | 6.2 | 6.1, | 6.3 | 404 | 3.2 | 5.0 | 4.9, | 5.0 | −19.6 | −21.5 | −17.6 |
| Injection drug use | 277 | 7.1 | 7.6 | 7.3, | 7.8 | 334 | 5.3 | 6.5 | 6.0, | 7.0 | −14.2 | −21.0 | −7.4 |
| Male-to-male sexual contact and injection drug use | 371 | 3.4 | 5.4 | 5.1, | 5.7 | 423 | 2.7 | 4.8 | 4.4, | 5.3 | −10.5 | −20.0 | −1.0 |
| Heterosexual contact | 257 | 9.0 | 9.8 | 9.4, | 10.1 | 314 | 5.9 | 8.1 | 7.7, | 8.5 | −17.0 | −22.1 | −11.9 |
| Female | 339 | 5.8 | 7.6 | 7.4, | 7.7 | 410 | 3.9 | 6.2 | 6.0, | 6.4 | −18.4 | −21.7 | −15.1 |
| Injection drug use | 334 | 5.6 | 6.7 | 6.4, | 7.0 | 398 | 4.8 | 6.0 | 5.4, | 6.6 | −10.6 | −19.8 | −1.4 |
| Heterosexual contact | 340 | 5.9 | 7.8 | 7.6, | 8.0 | 412 | 3.7 | 6.2 | 6.0, | 6.4 | −20.7 | −24.4 | −16.9 |
| Race/ethnicity | |||||||||||||
| Black/African American | 297 | 6.7 | 7.9 | 7.8, | 8.0 | 388 | 3.9 | 5.8 | 5.7, | 5.9 | −26.6 | −28.6 | −24.6 |
| Hispanic/Latino | 302 | 6.3 | 7.4 | 7.2, | 7.5 | 379 | 3.8 | 5.8 | 5.6, | 6.0 | −21.7 | −24.7 | −18.8 |
| White | 381 | 3.2 | 5.5 | 5.4, | 5.6 | 417 | 2.8 | 5.0 | 4.9, | 5.2 | −8.5 | −11.8 | −5.2 |
| Other | 329 | 4.9 | 6.6 | 6.3, | 6.9 | 385 | 3.8 | 5.7 | 5.3, | 6.0 | −14.5 | −21.0 | −7.9 |
| Age at diagnosis (years) | |||||||||||||
| 13-24 | 383 | 3.5 | 5.4 | 5.2, | 5.6 | 460 | 2.7 | 3.9 | 3.8, | 4.1 | −27.2 | −30.8 | −23.7 |
| 25-34 | 346 | 4.9 | 6.8 | 6.7, | 7.0 | 418 | 3.2 | 5.3 | 5.2, | 5.5 | −22.6 | −25.4 | −19.7 |
| 35-44 | 314 | 5.8 | 7.4 | 7.3, | 7.6 | 370 | 3.9 | 6.3 | 6.1, | 6.5 | −15.0 | −18.0 | −12.0 |
| 45-54 | 301 | 6.1 | 7.2 | 7.0, | 7.4 | 355 | 4.2 | 6.2 | 6.0, | 6.4 | −13.7 | −17.1 | −10.3 |
| 55+ | 265 | 7.5 | 7.7 | 7.4, | 8.0 | 316 | 5.6 | 6.8 | 6.5, | 7.1 | −11.7 | −16.3 | −7.0 |
From 2003 to 2011, the delays in infection to diagnosis decreased, with 50% of persons diagnosed in less than 3.6 years among those diagnosed in 2011 compared 5.4 years among those diagnosed in 2003 (Figure). However, the magnitude of the decrease over time differed among subgroups; the percent change was smaller among persons with infection attributed to injection drug use, whites, and older adults compared with their counterparts (Table 1).
Figure.
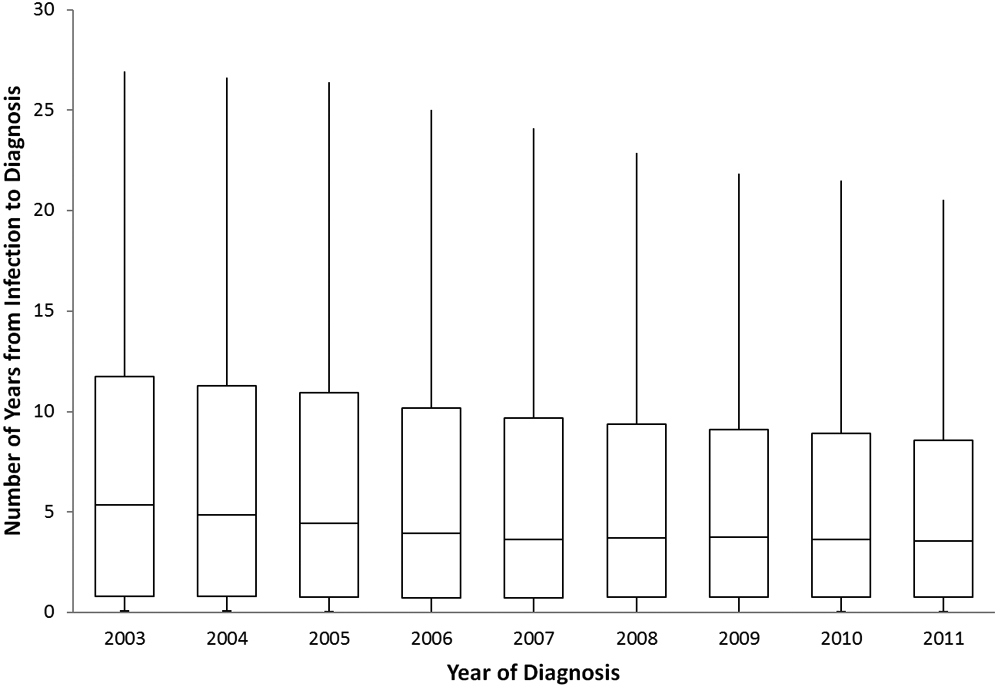
Number of years infected at HIV diagnosis, 2003-2011, United States
box plot of 25th percentile, median, and 75th percentile, with whiskers.
In 2006, CDC recommended routine testing for HIV in health care settings and testing at least annually for persons at high risk for HIV infection.9 Results from this analysis indicate that the time from infection to diagnosis has decreased in recent years, indicating better access to testing and corroborating findings from the National Health Interview Survey (NHIS) on increases among adults who report having ever tested for HIV.10 We also found that MSM, who comprise the majority of persons diagnosed with HIV, have a shorter interval from infection to diagnosis than their counterparts. Awareness of their HIV infection has increased among MSM and testing within the past year is high (67%).11,12 We found longer diagnosis delays among persons with infection attributed to heterosexual contact or injection drug use, although generally the percentage of persons with injection drug use aware of their infection is higher than among others, possibly because they tend to be older than persons with infection attributed to other modes of transmission.3,13
While the diagnosis delay was longer among blacks and Hispanics or Latinos compared to whites, the decrease in delay between 2003 and 2011 was larger among blacks and Hispanics or Latinos. Generally, testing rates are higher among blacks and Hispanics or Latinos compared with whites and the results may reflect efforts to improve access to testing among this population.1,10 Disparities in diagnosis delay coupled with lower retention in care and viral suppression and higher prevalence may add to higher transmission of HIV among blacks and poorer health outcomes.
The percentage of persons aware of their HIV infection is much lower among persons 13-24 years old compared with persons 25 years and older.3 However, persons diagnosed in this age group cannot have been infected for a long time compared with older persons who may have been living with HIV for longer periods of time, as reflected in our analysis. While national survey results indicate that overall HIV testing has not increased among this age group10, we found the largest percentage decrease in diagnosis delay among person diagnosed at age 13-24 years with possibly those at risk are testing earlier or more frequently. Improving early diagnosis and prompt linkage to care is important for all age groups to prevent further transmission of the virus and to reduce morbidity.
While our results indicate earlier diagnosis in recent years, this is in contrast to findings from a meta-analysis that did not show improvements in stage of disease at presentation to care.14 Delays in linkage to care after HIV diagnosis followed by regular care visits can undermine any gains from early diagnosis of HIV. Persons who are not in care do not benefit from risk-reduction counseling and cannot be offered HIV treatment. Current treatment guidelines recommend offering antiretroviral therapy to all persons with HIV infection regardless of stage of disease to reduce disease progression and prevent transmission of the virus to others.4
Our analyses are subject to several limitations. First, while good data exist to determine trends in diagnoses at late stage of disease, data on the actual stage of disease based on CD4 test results are more limited.3 Our results are based on 33 areas with adequate completeness of reporting of CD4 test results and may not be generalizable. However, additional analyses limited to a subset of jurisdictions with more complete CD4 information yielded similar results. Second, adjustment for reporting delays and missing risk factors may be inaccurate if factors associated with these were not accounted for in the model. In addition, the uncertainties associated with the diagnosis delay time estimates derived from the CD4 depletion model could be underestimated due to some restrictive assumptions, for example, the mean square root of CD4 count is linearly related to the time since infection. Therefore, the confidence intervals may not cover the true value with the desired confidence level.
In summary, the time from HIV infection to diagnosis has decreased in recent years but diagnosis delays continue to be substantial for some population groups. Delays in diagnosis can lead to missed opportunities for HIV care and treatment to reduce morbidity and prolong the time a person is unaware of their infection, which increases the potential for HIV transmission. Health care providers may still provide risk-based testing rather than offering routine testing at patient encounters as recommended by testing guidelines.15 For care and treatment to effectively reduce incidence, a high proportion of persons need to be diagnosed within the first year of infection.16 Continued efforts to assure implementation of routine testing can help both reduce the number of persons unaware of their infection and delays in diagnosis.
Disclaimer:
The findings and conclusions in this study are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Source of support:
US Government work
REFERENCES
- 1.Centers for Disease Control and Prevention. Results of the Expanded HIV Testing Initiative — 25 Jurisdictions, United States, 2007–2010. MMWR. 2011;60:805–810. [PubMed] [Google Scholar]
- 2.Hall HI, Holtgrave DR, Maulsby C. HIV transmission rates from persons living with HIV who are aware and unaware of their infection. AIDS. 2012;26:887–896. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2011. HIV Surveillance Supplemental Report 2013;18(No. 5). http://www.cdc.gov/hiv/library/reports/surveillance/. Published October 2013. Accessed May 29, 2014. [Google Scholar]
- 4.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. Department of Health and Human Services. May 1, 2014; E2. Available at: http://www.aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf. [Google Scholar]
- 5.San Francisco Department of Public Health. HIV/AIDS Epidemiology Annual Report, 2012. Available at: http://www.sfdph.org/dph/comupg/oprograms/hivepisec/default.asp. Accessed May 30, 2014.
- 6.Lodi S, Phillips A, Touloumi G, et al. Time from human immunodeficiency virus seroconversion to reaching CD4+ Cell Count Thresholds <200, <350, and <500 Cells/mm3: Assessment of Need Following Changes in treatment guidelines. Clin Infect Dis. 2011. Oct;53(8):817–25. [DOI] [PubMed] [Google Scholar]
- 7.Lodi S, Phillips A, Touloumi G, et al. CD4 decline in seroconverter and seroprevalent individuals in the precombination of antiretroviral therapy era. AIDS. 2010;24:2697–2704. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. HIV Surveillance Report Vol. 23. Diagnosis of HIV infection and AIDS in the United States and dependent areas, 2011. Published on February 28, 2013. Available at: http://www.cdc.gov/hiv/surveillance/resources/reports/2011report/index.htm. [Google Scholar]
- 9.CDC. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR. 2006;55(No. RR-14). [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. HIV Testing Trends in the United States, 2000-2011. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; January 2013:1–35. Available at: http://www.cdc.gov/hiv/pdf/testing_trends.pdf. Accessed June 2, 2014. [Google Scholar]
- 11.Centers for Disease Control and Prevention. HIV Testing and Risk Behaviors Among Gay, Bisexual, and Other Men Who Have Sex with Men — United States. MMWR. 2013;62(47):958–962. [PMC free article] [PubMed] [Google Scholar]
- 12.Wejnert C, Le B, Rose C, et al. HIV infection and awareness among men who have sex with men—20 cities, United States, 2008 and 2011. PLoS One. 2013;8:e76878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. NCHHSTP Atlas. Accessed on 06/17/2014.
- 14.Lesko CR, Cole SR, Zinski A, Poole C, Mugavero MJ. A Systematic Review and Meta-regression of Temporal Trends in Adult CD4+ Cell Count at Presentation to HIV Care, 1992-2011. Clin Infect Dis. 2013;57:1027–1037. [DOI] [PubMed] [Google Scholar]
- 15.McNaghten AD, Valverde EE, Blair JM, Johnson CH, Freedman MS, et al. Routine HIV Testing among Providers of HIV Care in the United States, 2009. PLoS ONE. 2013;8(1): e51231. doi: 10.1371/journal.pone.0051231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burns DN, DeGruttola V, Pilcher CD, Kretzschmar M,. Gordon CM, Flanagan EH, Duncombe C, Cohen MS, on behalf of the NIH-BMGF Finding Persons Unaware of their HIV Infection Workshop. Toward an Endgame: Finding and Engaging People Unaware of Their HIV-1 Infection in Treatment and Prevention. Aids Research And Human Retroviruses. 2014;30:217–224. [DOI] [PMC free article] [PubMed] [Google Scholar]


