Background:
The study aimed to introduce a rib and costal cartilage harvesting surgery by transumbilical single-incision laparoscopy and evaluate its efficiency and safety.
Methods:
Patients who underwent rib and costal cartilage harvest under different approaches (direct open approach and transumbilical) were collected in this retrospective study. The differences in the pain scores [visual analog scale (VAS)], postoperative appearance, and complications were compared between the two groups at 1, 2, 3, and 7 days after surgery. In addition, based on the minimal clinically important difference and the generalized estimating equation, the differences were compared between the two groups in terms of the VAS score.
Results:
On postoperative day 1, the VAS scores of the direct open approach group and the transumbilical group were significantly different, that is, 7.29 and 6.10, respectively (P < 0.001). Also, the generalized estimating equation results were different (P < 0.001). An interaction was observed between different groups and days, that is, a statistical difference was observed in the VAS score between the two groups (P < 0.001). In terms of aesthetics and complications, patients from the transumbilical group had no scars on the chest wall and no obvious postoperative complications.
Conclusions:
Transumbilical single-incision laparoscopic surgery is an innovative surgical approach for harvesting ribs and costal cartilage, which leaves no scars on the skin of the chest wall and has the advantages of slight postoperative pain, quick recovery, and fewer complications. This novel surgery is beneficial to patients with higher aesthetic requirements.
Takeaways
Question: Surgical approach for harvesting ribs and costal cartilage, which leaves scars on the skin of the chest wall, is not ideal for cosmetic surgeries.
Findings: We created a new surgery method named “transumbilical single-incision laparoscopic surgery” for harvesting rib and costal cartilage, which left no scars on the skin of the chest wall.
Meaning: The transumbilical single-incision laparoscopic surgery has the advantages of slight postoperative pain, quick recovery, and few complications. It is especially beneficial for patients with higher aesthetic requirements and is worthy of vigorous promotion.
INTRODUCTION
The development of plastic surgery has changed from relying on doctors’ skills at the beginning to new technology and equipment innovation. In the reconstruction of maxillofacial deformities caused by congenital hereditary factors or traumatic factors and the need for facial plastic surgery due to psychological factors, ribs and costal cartilage play an irreplaceable role.1,2 For instance, in rhinoplasty surgery, to raise the height of the bridge of the nose, filling the material with a hardness similar to that of the original is essential.3 The commonly used clinical materials include silicone implants and hyaluronic acid.4–7 However, these exogenous materials have obvious disadvantages: (1) rejection reaction or infection8; (2) the bridge of the nose formed by silicone implants is unnatural, and light transmission is observed from the side view4; and (3) hyaluronic acid has a short duration, requiring repeated injections and forming reactive granulation tissue in the local injection area.6 Ribs and costal cartilage have a strong regenerative ability, and since they are derived from autologous tissues, there is no rejection. Therefore, ribs and costal cartilage are ideal implant materials for rhinoplasty.
Traditional surgery to harvest ribs and costal cartilage requires an incision in the chest wall, which forms scars.1,9 For some patients, scar hyperplasia may also occur, which negatively affects their appearance. When the ribs are damaged, some patients’ visual analog scale (VAS) score can reach 70–80 mm.10 Compared to the maxillofacial defects caused by congenital maxillofacial deformities or trauma, the imperfect facial aesthetics considered by patients’ psychological factors can influence the surgeon’s choice of methods of surgery. This could be attributed to patients’ high psychological expectations and desire to achieve the perfect presentation of their face and body through minimally invasive methods.11,12
The umbilicus is a physiological scar left after a person leaves the mother’s body. Owing to its sequestered location, it is now often used as a common approach for some abdominal surgery, such as transumbilical laparoscopic appendectomy,13 cholecystectomy,14 and sleeve gastrectomy.15 In such an operation, a puncture with multiple operating holes is inserted through the umbilicus, and then a lens and surgical instruments are inserted to assist in the operation. The highest advantage of this kind of operation is small damage, slight pain, quick postoperative recovery, and no scars.16,17
For patients with high aesthetic requirements who need maxillofacial plastic surgery, we attempted to use the umbilicus and the natural scar to design incisions for harvesting ribs and costal cartilage. Some studies demonstrated that ribs and costal cartilage are donor sites for rhinoplasty, genioplasty, cleft lip, and orbital deformities, whereas others used the umbilicus as an approach to harvest rib and costal cartilage.10,18–20 In this study, we performed several transumbilical single-incision laparoscopic surgery (TUSILS) for harvesting rib and costal cartilage and confirmed the feasibility and effectiveness of this operation. It provides theoretical guidance for harvesting ribs and costal cartilage with limited scars and improving the postoperative satisfaction of patients.
METHODS
Source of the Patients
The patients were selected from the Department of Plastic and Reconstructive Surgery, Shanghai Ninth People’s Hospital Affiliated Shanghai Jiao Tong University School of Medicine. Before the operation, the patients were informed of the relevant information of the surgery, and informed consent was obtained from the patients and their families. The ethics committee of Shanghai Ninth People’s Hospital Affiliated Shanghai Jiao Tong University School of Medicine approved this study (SH9H-2021-T183-1).
Surgical Procedure
Eighth to tenth ribs and costal cartilage harvesting are an example to introduce the surgical procedure. The direct open approach of this surgery was as described previously.10
Preoperative Preparation
No special treatments such as skin preparation were required before the operation. After general anesthesia, the umbilicus was cleaned with an iodophor cotton ball before disinfection. After the abdomen was disinfected, the skin on both sides of the umbilicus was lifted with towel pliers to expose the depression of the umbilicus and disinfected again.
Transumbilical Approach
Towel pliers were used to lift up the bilateral sides of the umbilical margin and cut the umbilical skin longitudinally with a small sharp knife. The length of the incision was about 2 cm. Then, a multichannel single-port laparoscopic surgical trocar (Innovia IMD-LES-804) was inserted through the incision of the umbilicus, and carbon dioxide pneumoperitoneum was established (maintaining a constant pressure of 9–15 mm Hg), using a 5-mm laparoscopic lens and conventional laparoscopic instruments for surgery.
Surgical Operation
Combined with preoperative computed tomography, eighth to tenth costal cartilage was located, the electric hook was used to open the peritoneum and diaphragm, the costal cartilage was exposed, an ultrasonic knife was used to cut the rib or costal cartilage at 5 cm, and the rib or costal cartilage was removed from the single-hole trocar.
Umbilical Reconstruction
The longitudinal or T-shaped incision can form the most beautiful umbilicus in the umbilical reconstruction.21
Incision Closed
The peritoneum was closed with 2-0 absorbable sutures, and then the wound was washed with iodophor and saline. Ropivacaine was injected preperitoneally and subcutaneously, and finally, the aponeurosis and intradermal were sutured with 3-0 and 5-0 absorbable sutures, respectively.
The surgical procedure of TUSILS for harvesting rib and costal cartilage is illustrated in Figures 1 and 2.
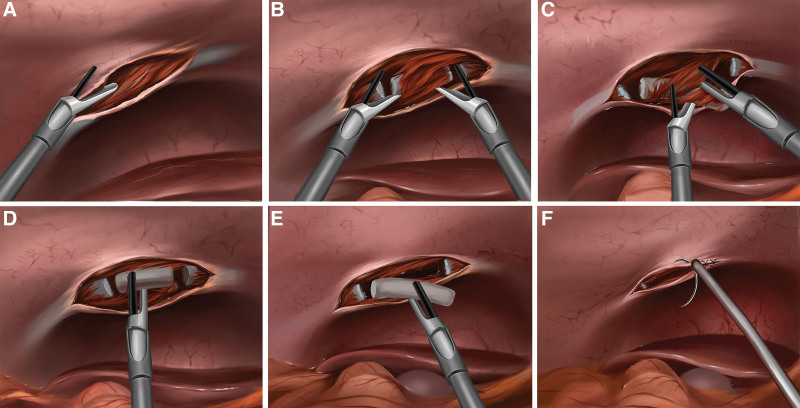
Fig. 1.
Schematic of TUSILS for harvesting rib and costal cartilage. A and B, The incision of peritoneum and the truncation of the rib or costal cartilage. C and D, The dissociation and exposure of the rib or costal cartilage. E and F, The extraction of the rib or costal cartilage and wound suture.
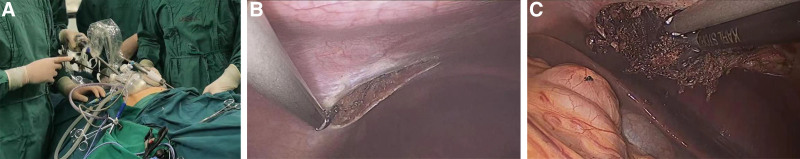
Fig. 2.
Intraoperative pictures of TUSILS for harvesting rib and costal cartilage. A, Transumbilical single-port endoscope. B, The peritoneum was cut with a harmonic ultrasonic knife. C, The muscles attached to the rib surface were cutoff to free the ribs.
Outcomes
Differences in VAS scores between the two groups at 1, 2, 3, and 7 days postsurgery;
Pain evaluation based on the minimal clinically important difference (MCID). The VAS score is the patient’s subjective self-evaluation of pain degree, with a score of 0–100 mm. Previous studies reported that in the pain assessment of VAS, 10 mm is the MCID, and 33 mm or less is the acceptable level of pain. These scores are used to calculate whether the patient’s VAS score change in the first 3 days after the surgery exceeds the MCID, which is 10 mm, to compare the differences in pain perception between the two groups postoperatively.
Comparison of differences in postoperative complications between the two groups (including infection, tissue damage, scars, and postoperative pain).
Statistical Analysis
Comparison of VAS Score
T-test was used to compare the differences in the VAS scores between the two groups. The chi-square test was used to check whether the two groups were balanced. A P value greater than 0.05 indicates that the groups were comparable.
Repeated Measurement Data Comparison Model
We compared the VAS scores of the two groups at 1, 2, 3, and 7 days after surgery and created a generalized estimating equation (GEE). In this model, the variables included group, timepoints, gender, age, and reason for surgery. The group and VAS-days were used as interactive factors to evaluate the difference in the trend of VAS scores between the two groups at various time points after surgery. A P value less than 0.05 indicated a statistical difference.
RESULTS
Patient Information
Between May 2020 and January 2021, a total of 54 patients were included in the current study. Among them, 27 patients (50%) underwent the TUSILS approach, and the remaining 27 patients (50%) underwent the direct open approach. The covariates of these two groups were balanced (P > 0.05 by chi-squared test) (Table 1).
Table 1.
Characteristics of Patients Who Underwent Rib or Costal Cartilage by TUSILS and Direct Open Approach
| Characteristic | TUSILS (N = 27) | Traditional Transcutaneous Approach (N = 27) | Overall (N = 54) | P* |
|---|---|---|---|---|
| Number (Percentage) | ||||
| Gender | 0.268 | |||
| Women | 14 (51.9) | 18 (66.7) | 32 (59.3) | |
| Men | 13 (48.1) | 9 (33.3) | 22 (40.7) | |
| Age [mean (SD)]† | 27.11 (5.97) | 28.15 (4.92) | 27.63 (5.44) | 0.489 |
| Reason for the surgery | 0.362 | |||
| Nose trauma repair | 21 (77.8) | 18 (66.7) | 39 (72.2) | |
| Rhinoplasty | 6 (22.2) | 9 (33.3) | 15 (27.8) | |
*The P value was calculated by chi-squared test.
†The P value was calculated by t-test.
Comparison of VAS Scores
At 1, 2, 3, and 7 days after surgery, the VAS scores of the TUSILS approach group were 6.10, 5.45, 4.40, and 2.98 cm, respectively, and those in the direct open approach group were 7.29, 5.54, 4.59, and 3.16 cm, respectively. On day 1 after the surgery, the VAS scores of the two groups were significantly different (P < 0.001, t-test) (Table 2).
Table 2.
Comparison of VAS Score between Two Groups
| VAS score [mean (SD)] | TUSILS | Traditional Transcutaneous Approach | P* |
|---|---|---|---|
| VAS-Day1 | 6.10 (0.62) | 7.29 (0.43) | <0.001 |
| VAS-Day2 | 5.45 (0.48) | 5.54 (0.90) | 0.667 |
| VAS-Day3 | 4.40 (0.63) | 4.59 (0.96) | 0.404 |
| VAS-Day7 | 2.98 (0.59) | 3.16 (0.67) | 0.298 |
*The P value was calculated by t-test.
Pain Evaluation based on the MCID
Comparison of Differences in Perceived Pain Changes (MCID = 10 mm)
The estimated marginal mean (EMM) of the daily VAS score obtained by GEE was 6.633, 5.435, 4.437, and 3.013. A significant difference was noted between the two EMMs (P < 0.001), and the difference in pain perception between the two groups reached 10 mm MCID (Fig. 3).
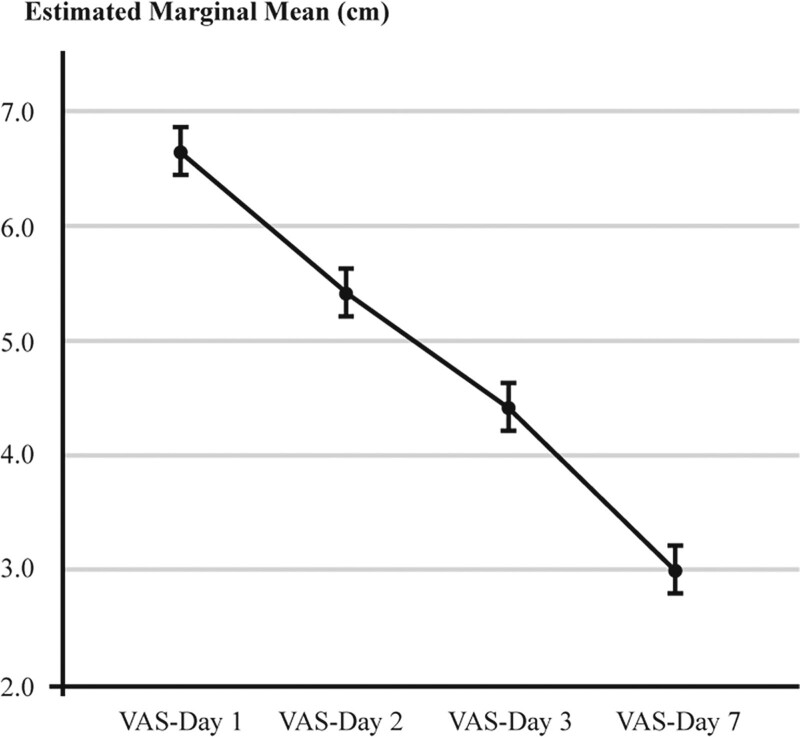
Fig. 3.
Comparison of differences in perceived pain changes. The EMM of the daily VAS score obtained by GEE was 6.633, 5.435, 4.437, and 3.013, respectively. A significant difference was observed between the two EMMs (P < 0.001).
Comparison of VAS Scores on Day 7 Postsurgery
On postoperative day 7, the number of patients with VAS scores less than 33 mm in the TUSILS approach, and the direct open approach groups were 16 (59.3%) and 17 (63.0%), respectively (P = 0.78, chi-squared test) (Table 3).
Table 3.
VAS Scores on Day 7 after Surgery
| VAS-Day7 | TUSILS | Traditional Transcutaneous Approach | P* |
|---|---|---|---|
| ≥33 mm | 11 (40.7) | 10 (37.0) | 0.78 |
| <33 mm | 16 (59.3) | 17 (63.0) |
*The P value was calculated by chi-squared test.
Generalized Estimating Equation
According to GEE, the mean VAS scores of the two groups showed a significant downward trend after the operation (P < 0.001). In addition, the mean VAS score of the TUSILS approach group was lower on day 1 after the surgery (Pgroup × time < 0.001), but no significant difference was observed in the mean VAS score between the two groups at 2, 3, and 7 days after the surgery (P > 0.05) (Fig. 4).
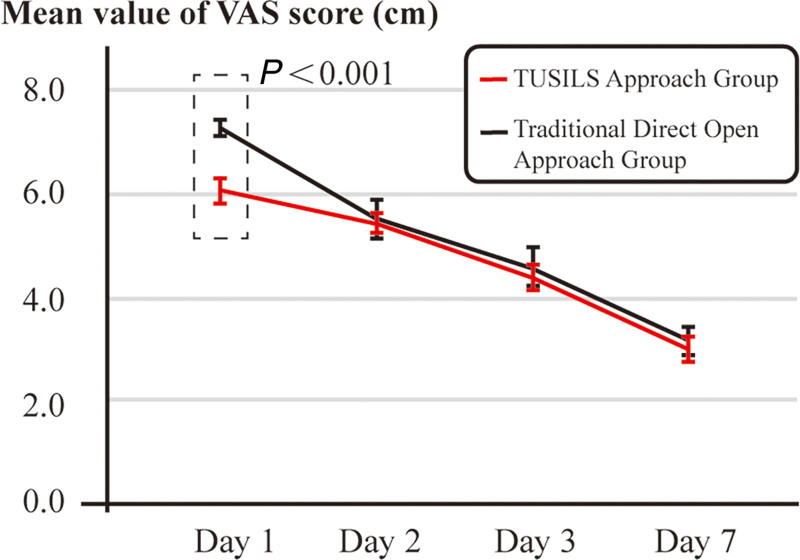
Fig. 4.
Mean VAS scores generated by GEE. The mean VAS scores of the two groups showed a downward trend after the operation (P < 0.001). On day 1 after surgery, the mean VAS score of the TUSILS approach group was lower than that of the direct open approach group (P group × time < 0.001).
Complications
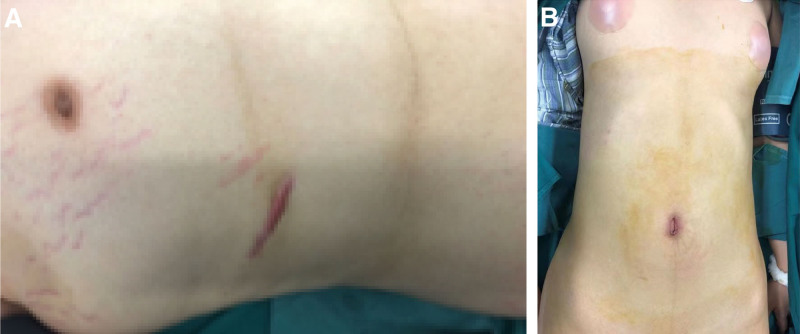
Scars
Compared to the direct open approach group, the TUSILS approach group did not have any additional incisions or scars except the umbilicus. The scar of the umbilicus was about 1.5 cm, sequestered in the umbilical folds (Fig. 5).
Fig. 5.
Comparison of the postoperative scars between the two groups. A, Skin scars on the chest wall in the direct open approach group. B, Occult scar on the umbilicus in the TUSILS approach group.
Aesthetics and Function
The length of the ribs or costal cartilage obtained by the TUSILS approach was about 5 cm without damage or distortion.
Infection and Injury
Only one patient developed a local infection in the TUSILS approach group after surgery, which was cured by antibiotic treatment, and no postoperative infection or diaphragm injury was observed.
Others
The operation did not affect the patient’s diet. No obvious pain was presented in the incision of the umbilicus, and the stitches did not require removal.
DISCUSSION
TUSILS for harvesting rib and costal cartilage is a technical improvement in surgery that is beneficial to patients. It proposes not only a new method of rib and costal cartilage harvesting but also the process of surgery. As surgeons have become specialized and surgical methods and instruments are individualized, the development of cross-category surgery is restricted. Although young doctors will undergo multidisciplinary training at the resident stage, it is difficult for them to have complete access to different fields. Especially for doctors with extensive clinical experience, the knowledge of other disciplines they acquired 5 or 10 years ago still stays, although the cognition of their discipline has not been pursued. This study is a combination of the ideas of other surgeons and plastic surgeons with great contingency. The present innovative strategy and its results have promoted multidisciplinary exchanges.
The major concern of the surgeon is the efficacy of surgery. Traditionally, successful surgery means a high cure rate and a low recurrence rate, especially in those diseases that have not been truly “conquered.” However, with the advancement of science and technology, and the continuous development of surgical techniques, plastic surgery should be considered more than curing the disease and understanding the spiritual needs of the patients. Thus, the inconsistency of subjective and objective evaluations and doctor-patient evaluations of the same medical behavior could be avoided.22 Pain as a symptom has a high degree of subjectivity and individual differences, and its evaluation results are affected by many factors, such as visual information.23,24 In the current study, although there is little difference in the ribs taken out by the two groups of patients, the TUSILS group had significantly lower VAS scores on postoperative day 1. Moreover, on days 1 and 2, a smaller downward trend was observed in VAS scores compared to the direct open approach group. This could be attributed to the absence of surface wounds and drainage tubes, which allow the patients to feel that their body has not been damaged severely visually. It also implies psychologically that such small injuries do not cause severe pain. Moreover, this kind of psychological suggestion to patients may be strengthened by focusing on their wound-free skin surface, which encourages patients to face postoperative pain with a positive attitude. Nonetheless, such subtle psychological changes require in-depth research. On postoperative days 2 and 3, the pain in the traditional group continued to decrease, but the proportion of patients with continuous pain reduction in the TUSILS approach group was not satisfactory, and the VAS values of postoperative days 2 and 3 were similar between the two groups. In the TUSILS group, the subjective feelings of pain and the true degree of pain on postoperative day 1 of the patients had a certain degree of deviation, which led to the judgment of the VAS score being lower than the real pain degree and lower than the traditional group. Therefore, this resulted in little difference in VAS between postoperative days 1 and 2. Our data also supported such speculation. Autologous bone transplantation has many advantages: natural appearance, low infection rate, and less foreign body reaction. Rib transplantation is the most commonly used surgical procedure in clinical practice. In a previous study, we found that the in situ splitting approach for obtaining a rib significantly reduces the complications compared to the traditional approach (6.67% versus 44.44%).10 In the same study, we also found that on days 2 and 3, the VAS scores of the in situ splitting approach were significantly lower than the traditional approach, showing better surgical tolerance and quality of life. Therefore, the in situ splitting approach for harvesting ribs and costal cartilage is the best choice to repair facial deformities. In addition, the in situ splitting approach avoids complications, such as pleural injury and pneumothorax, during the operation. As the postoperative pain of the in situ splitting approach is less, patients can receive rehabilitation training earlier to avoid postoperative complications. During the 12-month follow-up, the rib recovery of patients with an in situ splitting approach was significantly better than that of the traditional approach (41.45% versus 94.12%), which highlights the importance of periosteum in rib repair.18
Ribs have critical application and research value in many plastic surgery operations. For instance, in the study of using ribs to repair orbit defects, no significant difference was observed between the in situ splitting and the traditional approach in the volume reduction of the donor site when the ribs were removed, illustrating the safety of the in situ splitting approach.18 In addition to orbital repair, ribs and costal cartilage are also used for rhinoplasty. Previously, we used the natural curvature of the costal cartilage to repair the nasal base and the chin at the same time with a piece of costal cartilage. After trimming the shape of the costal cartilage, the remaining costal cartilage could be used to make a fine adjustment to the shape of the nose and chin, which could simultaneously take into account the shape and proportion of the middle and lower parts of the face.19 Also, the autologous ribs and costal cartilage are proven as satisfactory graft donors in the repair surgery of patients with cleft lip.20 Unlike the traditional treatment of the cleft lip and palate with the iliac bone as a donor, ribs and costal cartilage can be used to repair alveolar clefts and nasal deformities, greatly reducing the damage to the donor site and reducing the number of operations. In these studies, the evaluation described is applicable as it can assess the surgery objectively and comprehensively based on the subjective feelings of the patient. As the operation matures, the postoperative pain caused by psychological factors should be under intensive focus.
In plastic surgery, minimally invasive surgery is one of the major pursuits of doctors and patients and is crucial with respect to the orbit, nose, lips, and chin. Presently, ribs as a donor site is relatively mature in plastic surgery, and we are now focusing on patients’ subjective feelings after surgery. Since Fearon and Cotton applied costal cartilage to treat subglottic stenosis in 1972, ribs and cost cartilage have been widely used in the field of plastic surgery.25 Ribs and costal cartilage have always been used as good graft materials because their source of homology minimizes the rejection reaction after surgery.8 The traditional incision approach for ribs and costal cartilage harvesting has always been designed on the chest wall. If the patient needs a defect repair after maxillofacial trauma, a larger amount of costal cartilage can be harvested to repair a wide range of defects. However, in plastic surgery, if the patient’s expectations are high and do not want to add new incisions in other parts of the body, then rib and costal cartilage grafts are often not the first options for the patient, which makes the development of this type of surgery limited.
Since Wheeless26 carried out the first transumbilical laparoscopic tubal ligation in 1969, TUSILS has been gradually used in clinical practice with satisfactory effects. Since the umbilicus is the only scar left after a person leaves the mother’s body, we can apply this scar to plastic surgery. Harvesting ribs and costal cartilage under TUSILS can resolve the issue of scars on the chest wall; our team has verified the effectiveness and feasibility of this operation. Compared to traditional open surgery, the advantages of TUSILS for harvesting ribs and costal cartilage are as follows: (1) the umbilical incision is about 1.5–2 cm and is covered by wrinkles. Compared to the traditional chest wall incision, it is concealed and aesthetic; (2) the smaller incision lessens the postoperative pain, the wound recovers rapidly, and the subjective experience is better; (3) one of the complications of traditional costal cartilage harvest surgery is pleural injury, which can lead to pneumothorax, whereas the diaphragm can be viewed directly under TUSILS to avoid severe complications, such as diaphragm injury and pneumothorax. In the 27 patients who underwent TUSILS included in our study, the ribs were completely removed without causing any auxiliary damage to the adjacent organs, and only a very hidden umbilical wound was left that could heal quickly.
Nevertheless, TUSILS for harvesting ribs and costal cartilage has some drawbacks, but it also points out a new direction for the progress of surgery. First, single-port surgical instruments are more difficult to operate than traditional three-port laparoscopes, and the operator needs a learning curve. Since most plastic surgeons do not have such operation skills, they need to cooperate with a doctor who is familiar with endoscopy or can master this skill after a long learning period. Although this has increased the difficulty of surgery promotion, it can improve the safety of patients, making the learning worthwhile. Second, the current laparoscopic instruments are not designed for rib harvesting, and there are problems, such as lack of motion protection and difficulty while directly measuring the length of the ribs. This requires innovative surgical medical equipment. Third, due to the limitations of the current medical equipment, we have not yet been able to perform the in situ splitting approach of the ribs under TUSILS; currently, the ribs can be taken out completely. This aspect will be investigated in future studies.
In conclusion, TUSILS is an innovative surgical approach to harvesting the ribs and costal cartilage, which has the advantages of no scars on the chest wall skin, slight postoperative pain, quick recovery, and fewer complications. Thus, this novel surgery is beneficial to patients with high aesthetic requirements.
Footnotes
Published online 7 March 2022.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Cochran CS. Harvesting rib cartilage in primary and secondary rhinoplasty. Clin Plast Surg. 2016;43:195–200. [DOI] [PubMed] [Google Scholar]
- 2.Wee JH, Park MH, Oh S, et al. Complications associated with autologous rib cartilage use in rhinoplasty: a meta-analysis. JAMA Facial Plast Surg. 2015;17:49–55. [DOI] [PubMed] [Google Scholar]
- 3.Ho OYM, Ku PKM, Tong MCF. Rhinoplasty outcomes and trends. Curr Opin Otolaryngol Head Neck Surg. 2019;27:280–286. [DOI] [PubMed] [Google Scholar]
- 4.Kim IS. Augmentation rhinoplasty using silicone implants. Facial Plast Surg Clin North Am. 2018;26:285–293. [DOI] [PubMed] [Google Scholar]
- 5.Manavbasi I, Agaoglu G. Silicon template for nasal tip graft. Ann Plast Surg. 2006;56:226. [DOI] [PubMed] [Google Scholar]
- 6.Bravo BSF, Bravo LG, Mariano Da Rocha C, et al. Evaluation and proportion in nasal filling with Hyaluronic Acid. J Clin Aesthet Dermatol. 2018;11:36–40. [PMC free article] [PubMed] [Google Scholar]
- 7.Jung GS. Minimally invasive rhinoplasty technique using a hyaluronic acid filler and polydioxanone threads: an effective combination. Facial Plast Surg. 2019;35:109–110. [DOI] [PubMed] [Google Scholar]
- 8.Mohammadi S, Ghourchian S, Izadi F, et al. Porous high-density polyethylene in facial reconstruction and revision rhinoplasty: a prospective cohort study. Head Face Med. 2012;8:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ohara K, Nakamura K, Ohta E. Chest wall deformities and thoracic scoliosis after costal cartilage graft harvesting. Plast Reconstr Surg. 1997;99:1030–1036. [DOI] [PubMed] [Google Scholar]
- 10.Zhang L, Sun XM, Jin R, et al. A study of the morbidity involved in whole rib harvesting and in situ splitting rib harvesting surgery. J Craniofac Surg. 2016;27:876–879. [DOI] [PubMed] [Google Scholar]
- 11.Asimakopoulou E, Zavrides H, Askitis T. Plastic surgery on body image, body satisfaction and self-esteem. Acta Chir Plast. 2020;61:3–9. [PubMed] [Google Scholar]
- 12.Bradbury E. The psychology of aesthetic plastic surgery. Aesthetic Plast Surg. 1994;18:301–305. [DOI] [PubMed] [Google Scholar]
- 13.Switzer NJ, Gill RS, Karmali S. The evolution of the appendectomy: from open to laparoscopic to single incision. Scientifica (Cairo). 2012;2012:895469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roberts KE, Solomon D, Duffy AJ, et al. Single-incision laparoscopic cholecystectomy: a surgeon’s initial experience with 56 consecutive cases and a review of the literature. J Gastrointest Surg. 2010;14:506–510. [DOI] [PubMed] [Google Scholar]
- 15.Wang L, Zheng X, Sang Q, et al. Single-incision transumbilical laparoscopic sleeve gastrectomy with a stomach retractor in 20 superobese patients-a video vignette. Obes Surg. 2020;30:5179–5181. [DOI] [PubMed] [Google Scholar]
- 16.Tyagi S, Sinha R, Tyagi A. Single incision laparoscopic cholecystectomy: less scar, less pain. J Minim Access Surg. 2017;13:118–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Canes D, Desai MM, Aron M, et al. Transumbilical single-port surgery: evolution and current status. Eur Urol. 2008;54:1020–1029. [DOI] [PubMed] [Google Scholar]
- 18.Sun XM, Ye LX, Jin R, et al. Survey of in situ splitting rib harvesting surgery for orbital deformity: follow-up. J Craniofac Surg. 2018;29:1224–1226. [DOI] [PubMed] [Google Scholar]
- 19.Zhang L, Ma WS, Bai JP, et al. Comprehensive application of autologous costal cartilage grafts in rhino- and mentoplasty. J Craniofac Surg. 2019;30:2174–2177. [DOI] [PubMed] [Google Scholar]
- 20.Zhang L, Wei S, Qi L, et al. Simultaneous correction of complex secondary deformities of cleft lip using autogenous costal cartilage combined with rib grafts. J Craniofac Surg. 2020;31:497–500. [DOI] [PubMed] [Google Scholar]
- 21.Sisti A, Huayllani MT, Boczar D, et al. Umbilical reconstruction techniques: a literature review. Aesthetic Plast Surg. 2021;45:1078–1096. [DOI] [PubMed] [Google Scholar]
- 22.Garimella R, Koenig HG, Larson DL, et al. Of these, faith, hope, and love: assessing and providing for the psychosocial and spiritual needs of burn patients. Clin Plast Surg. 2017;44:893–902. [DOI] [PubMed] [Google Scholar]
- 23.Loeser JD, Melzack R. Pain: an overview. Lancet. 1999;353:1607–1609. [DOI] [PubMed] [Google Scholar]
- 24.Kaciroti N, DosSantos MF, Moura B, et al. Sensory-discriminative three-dimensional body pain mobile app measures versus traditional pain measurement with a visual analog scale: validation study. JMIR Mhealth Uhealth. 2020;8:e17754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gallagher TQ, Hartnick CJ. Costal cartilage harvest. Adv Otorhinolaryngol. 2012;73:39–41. [DOI] [PubMed] [Google Scholar]
- 26.Wheeless CR. A rapid, inexpensive and effective method of surgical sterilization by laparoscopy. J Reprod Med. 1969;3:65–69.. [Google Scholar]