Abstract
Intense investigation into the predictors and determinants of post-acute sequelae of SARS-CoV-2 infection (PASC), including ‘long COVID’, is underway. Recent studies provide clues to the mechanisms that might drive this condition, with the goal of identifying host or virus factors that can be intervened upon to prevent or reverse PASC.
Keywords: SARS-CoV-2, post-acute sequelae of SARS-CoV-2 (PASC), post-acute COVID syndrome (PACS), long COVID, immunology
Abbreviations: PASC, post-acute sequelae of SARS-CoV-2 infection; PACS, post-acute COVID syndrome; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; COVID-19, coronavirus disease 2019; EBV, Epstein-Barr virus; IFN, interferon
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection can lead to systemic symptoms, which in most people resolve within a few weeks. A poorly characterized subset of individuals, however, have persistent symptoms that last for many weeks or longer. The syndrome has many names, including ‘post-acute sequelae of SARS-CoV-2 infection’ (PASC) and ‘post-acute coronavirus disease (COVID) syndrome’ (PACS), but is more widely known as ‘long COVID’. Due in part to the formation of a very powerful and effective advocacy community, the US Congress recently allocated over $1 billion dollars for the study of PASC. The National Institutes of Health (NIH) is now implementing a massive program [Researching COVID to Enhance Recovery (RECOVER); www.recovercovid.org]; the UK and other countries already have several ongoing initiatives. The study of PASC has become a major research priority that will presumably lead to discoveries relevant to other post-infectious syndromes, many of which are similar to PASC.
There are dozens of epidemiologic studies, most leveraging electronic medical records, describing the natural history of PASC. In general, these studies have found that sex, severity of initial COVID-19, the presence of certain comorbidities (including obesity, diabetes, and chronic lung disease), and socioeconomic status can affect the risk of an individual with COVID-19 developing PASC. Newer clinical and translational studies are beginning to explore its pathogenesis, providing clues about some of the mechanistic pathways that might contribute to this condition.
We can now expect the emergence of major scientific efforts addressing the pathogenesis of PASC. In one of the first systematic studies, a large collaborative group organized by the Institute for Systems Biology (Seattle, WA, USA) performed a longitudinal multi-omic systems biology analysis of over 200 individuals who were followed for 2–3 months after acute infection [1]. Several factors were associated with the development of PASC, including pre-existing diabetes mellitus, high-level SARS-CoV-2 viremia, and Epstein-Barr virus (EBV) reactivation during acute infection. The investigators also identified the presence of certain autoantibodies, including those targeting type I interferons (IFNs), that could predict PASC. Their observations suggest plausible mechanisms by which SARS-CoV-2 infection can cause persistent symptoms. For example, a higher degree of SARS-CoV-2 viremia likely reflects higher tissue viral burden and increased likelihood of end-organ damage. Higher viremia might also be associated with immunologic perturbations that could lead to organ dysfunction; some of these might persist beyond early convalescence. The relationships for other factors are less clear, for example, EBV viremia may more plausibly reflect the severity of initial illness rather than represent a causal mechanism of PASC, although the recent observation that EBV reactivation might lead to multiple sclerosis suggests this virus can contribute to autoimmune syndromes [2]. Furthermore, the identification of a relationship with anti-IFN antibodies, previously shown to be important in acute COVID-19 [3], suggests another mechanism that may tie together an impaired antiviral response, an enhanced inflammatory response, and generation of downstream autoimmune processes.
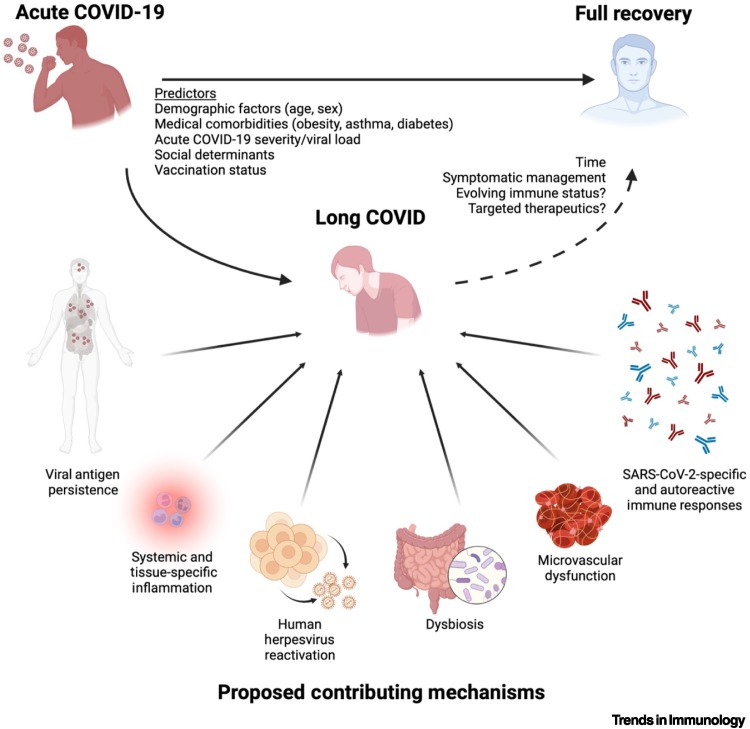
In a different analysis of several hundred individuals during acute infection and up to a year later [4], Cervia and colleagues identified a distinct SARS-CoV-2 specific immunoglobulin signature during acute infection among those who went on to develop PASC. Specifically, they found that reduced IgM and IgG3 titers during acute infection were a risk factor for PASC, which the authors suggest might be related to reduced production of type I IFNs resulting in a failure of isotype switching. Using these laboratory measurements in combination with certain clinical factors (e.g., age, asthma history, number of acute COVID-19 symptoms), the team generated a prediction model to identify those who developed PASC [4]. In yet another recent study, Liu and colleagues found differences in the gut microbiome associated with neuropsychiatric and pulmonary PASC symptoms [5]. These studies add to a growing body of literature suggesting that a combination of virus and host factors, including potential viral antigen persistence (preliminary) [6], residual inflammation [7,8], microvascular dysregulation [9], and autoimmune phenomena [10] might contribute to PASC (Figure 1 ).
Figure 1.
Predictors and proposed pathophysiologic mechanisms of long coronavirus disease (COVID).
Studies to date have identified certain factors that predict whether an individual with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection will fully recover or develop post-acute sequelae, including the persistent symptoms that characterize long COVID. Shown here are several mechanisms with evidence supported by recent studies of individuals with post-acute sequelae of SARS-CoV-2 infection (PASC) [1,4., 5., 6., 7., 8., 9., 10.]. These include tissue persistence of viral antigen, systemic and tissue-localized inflammatory responses, reactivation of human herpesviruses (e.g., Epstein-Barr virus), alterations in the gut microbiome, issues related to clotting, and the interplay between SARS-CoV-2-specific and autoreactive immunity. Some individuals with long COVID will spontaneously recover over time, possibly due to resolution of these factors and/or evolving immune status. The confirmation of these mechanisms in individuals with PASC may lead to therapeutics targeting the pathophysiology of this condition, with the goal of allowing more individuals to achieve full recovery. Figure created with BioRender.com
These studies are not without limitations. Volunteers have disproportionately been previously hospitalized with severe COVID-19, despite the fact that the vast majority of those who acquire SARS-CoV-2 (including those with PASC) are not hospitalized. This makes it difficult to distinguish the virus-specific contribution from the well-established effects of hospitalization and/or critical illness. PASC has not been measured in a consistent way and many participants would not meet the WHO case definition for PASC. Furthermore, few studies have attempted to ascertain the severity of PASC symptoms and/or their impact on quality of life, which might be a more relevant outcome than their presence or absence. The inclusion of objective physiologic measurements (e.g., cardiopulmonary or neurologic function, tissue-based measurements) will be an essential element in further studies that seek to identify the physiologic drivers of PASC symptoms. Finally, each study addresses different clinical phenotypes of PASC, which are presumed to exist but have not been rigorously defined. Overall, the heterogeneity in approaches to recruitment and measurement makes it challenging to construct one cohesive story from these individual contributions. For this reason, disentangling the causes of PASC will require substantial coordination in defining outcomes and identifying biomarkers. Such efforts are now beginning, including the nascent US RECOVER meta-cohort.
Such efforts to develop a more focused understanding of the complex biology of PASC are a crucial step toward the goal of preventing or reversing this condition. The mechanisms outlined here naturally lead to testable hypotheses regarding treatment. These include strategies aimed at reducing the titers of acute viremia, such as post-infection therapeutic vaccination, antiviral drugs, and/or monoclonal antibodies. Notably, the emerging literature suggests that infection after vaccination (‘breakthrough infection’) is associated with a lower risk of PASC than infection in those who are unvaccinated; this provides indirect evidence that better control of acute infection may prevent longer term complications. Immunomodulators that disrupt potentially harmful inflammatory or autoimmune processes should also be tested. Ultimately, understanding PASC will require investigation that leverages the full research armamentarium (epidemiologic, clinical, translational, and basic science studies) to understand the incidence, prevalence, and causal determinants of the condition and, eventually, interventional trials to determine how best to treat it.
Acknowledgments
Acknowledgments
M.J.P. is supported on K23AI157875 and by the UCSF Resource Allocation Program. M.J.P. and S.G.D. are investigators in the NIH RECOVER Consortium.
Declaration of interests
The authors have no interests to declare.
References
- 1.Su Y., et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell. 2022 doi: 10.1016/j.cell.2022.01.014. Published online January 25, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bjornevik K., et al. Longitudinal analysis reveals high prevalence of Epstein-Barr virus associated with multiple sclerosis. Science. 2022;375:296–301. doi: 10.1126/science.abj8222. [DOI] [PubMed] [Google Scholar]
- 3.Calabrese L.H., et al. Type I interferon, anti-interferon antibodies, and COVID-19. Lancet Rheumatol. 2021;3:e246–e247. doi: 10.1016/S2665-9913(21)00034-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cervia C., et al. Immunoglobulin signature predicts risk of post-acute COVID-19 syndrome. Nat. Commun. 2022;13:446. doi: 10.1038/s41467-021-27797-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu Q., et al. Gut microbiota dynamics in a prospective cohort of patients with post-acute COVID-19 syndrome. Gut. 2022;71:544–552. doi: 10.1136/gutjnl-2021-325989. [DOI] [PubMed] [Google Scholar]
- 6.Chertow D., et al. SARS-CoV-2 infection and persistence throughout the human body and brain. Res. Square. 2021 doi: 10.21203/rs.3.rs-1139035/v1. Published online December 20, 2021. [DOI] [Google Scholar]
- 7.Peluso M.J., et al. Markers of immune activation and inflammation in individuals with postacute sequelae of severe acute respiratory syndrome coronavirus 2 infection. J. Infect. Dis. 2021;224:1839–18488. doi: 10.1093/infdis/jiab490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phetsouphanh C., et al. Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection. Nat. Immunol. 2022;23:210–216. doi: 10.1038/s41590-021-01113-x. [DOI] [PubMed] [Google Scholar]
- 9.Pretorius E., et al. Persistent clotting protein pathology in long COVID/post-acute sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovasc. Diabetol. 2021;20:172. doi: 10.1186/s12933-021-01359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seeßle J., et al. Persistent symptoms in adult patients one year after COVID-19: a prospective cohort study. Clin. Infect. Dis. 2021;5 doi: 10.1093/cid/ciab611. [DOI] [PMC free article] [PubMed] [Google Scholar]